Abstract
Introduction
Sleep deficit or poor sleep leads to ill-health, whereas sleep deprivation for longer periods of time increases the risk of developing adverse conditions associated with poor quality of life, and high socioeconomic impact. The treatments for sleep disturbances include melatonin and over-the-counter medicines like diphenhydramine and doxylamine, all of which have negative side effects. Valerian (Valeriana officinalis L.) is a traditional herb and the most preferred alternate sleep solution to manage sleep complaints.
Methods
Eighty adult subjects with sleep complaints were randomized in 1:1 ratio to receive either V. officinalis extract (VE) or placebo for 8 weeks in a double-blind, placebo-controlled, parallel, clinical study. Primary efficacy endpoints included the Pittsburgh Sleep Quality Index (PSQI) and sleep latency using wrist actigraphy (WA), as well as a number of secondary endpoints, including sleep parameters such as actual sleep time and sleep efficiency using WA, the Epworth Sleepiness Scale (ESS), the Beck Anxiety Inventory (BAI), the Visual Analogue Scale (VAS) for the feeling of waking up refreshed, and a tertiary endpoint of sleep parameters using polysomnography (PSG) in a subset of 20 subjects per group. Safety parameters included physical examination, vital sign measurements, hematology, and clinical chemistry tests. Adverse events and serious adverse events were monitored throughout the study period.
Results
Seventy-two subjects (35 and 37 subjects in the placebo and VE groups, respectively) completed the study and were included in the efficacy assessments. On Days 14, 28, and 56, the PSQI Total Score in the VE group decreased significantly (p < 0.05) compared to the placebo group. Further, the VE group showed significant improvements (p < 0.05) in sleep latency and actual sleep time on Days 3, 14, 28, and 56, and sleep efficiency on Days 14, 28, and 56, as evaluated by WA. There was a decrease (p < 0.05) in anxiety (BAI) on Days 14, 28, and 56, daytime drowsiness (ESS) on Days 28 and 56, and an increased feeling of waking up refreshed (VAS) on Days 28 and 56 compared to placebo. PSG results carried out in subset of subjects revealed significant improvements (p < 0.05) in total sleep time, sleep latency, and sleep efficiency on Day 56 in the VE group compared to the placebo group. No safety concerns were observed throughout the study.
Conclusion
VE supplementation significantly improved various subjective and objective parameters of sleep in young subjects with mild insomnia symptoms, such as overall sleep quality, sleep latency, sleep efficiency, and total sleep time. We also observed decreased anxiety and daytime sleepiness, and improved feeling of being refreshed after waking up with VE supplementation. VE was found to be safe and well tolerated throughout the study.
Trial Registration
Clinical Trials Registry of India: CTRI/2022/05/042818.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12325-023-02708-6.
Keywords: Anxiety, Insomnia, PSQI, Sleep quality, Valerian, VAS
Key Summary Points
| Why carry out this study? |
| Poor quality sleep and sleep deprivation are linked to many diseases and negative socioeconomic issues |
| Over-the-counter medications like melatonin, diphenhydramine, and doxylamine are used for sleep disorders but they come with detrimental side effects |
| Valerian (Valeriana officinalis L.) is a traditional herb that helps to address various sleep-related complaints. A new valerian extract formulation (commercially known as Sleeproot®) has been developed and was studied for its efficacy and safety in this clinical trial |
| What was learned from the study? |
| This study found a significant improvement in overall sleep quality, latency, efficiency, total sleep time, decreased anxiety, and daytime sleepiness, and increased satisfaction with waking up feeling refreshed in young subjects with mild insomnia symptoms and no comorbidities. Safety and tolerability of valerian extract was demonstrated through our study results |
| Unlike other valerian studies, our results demonstrated the effectiveness of standardized valerian extract through objective and subjective sleep parameters |
Introduction
Insomnia is a common sleep disorder with sleep deficit or poor sleep quality affecting one-third of the adult population worldwide. Sleep deprivation for longer periods of time has serious consequences on health, associated with poor quality of life, lowered work place performance, and compromised safety, leading to increased cost in health care [1–6]. Studies have shown a direct relationship between inadequate sleep and development of metabolic diseases such as diabetes, obesity, hypertension, cardiovascular diseases, and depression [7–14], and consequences such as road accidents, work-related injuries, and loss of life [15–17]. Severe cases of sleep-associated conditions are reported in about 10–15% of adults which rises to 25% in the elderly [18]. Insomnia is found in up to 69% of patients attending primary care clinics and is widely prevalent in subjects with chronic medical conditions [19].
Approximately 40% of adults use over-the-counter medications or alcohol to manage sleep issues. Although melatonin is the most commonly used sleep aid, meta-analysis of human clinical studies indicate only a modest improvement of sleep parameters by melatonin [20]. Side effects of melatonin are mild in nature but include daytime sleepiness, headache, nausea, and dizziness. Although melatonin is secreted by the body and is a natural ingredient of the biological system with a primary role of management of circadian rhythm in the body, emerging evidence indicates that it is associated with a multitude of physiological systems that are unrelated to sleep and associated with interactions with the cardiovascular, reproductive, endocrine, and metabolic systems [21]. Common prescription drugs that are used for chronic sleep disorders include benzodiazepines, anti-histamines, anti-depressants, chloral hydrate, barbiturates, etc. [22]. Although benzodiazepines are known to improve insomnia, clinical benefits are marginal, with undesirable adverse effects such as cognitive impairment and an increased risk of motor vehicle accidents, falls, and fractures from chronic use [23, 24]. Buspirone, a serotonergic prescription drug used for anxiety disorders, has cardiovascular adverse effects [25]. Hence, alternate approaches, such as complementary medicines including herbal extracts, have been extensively explored to address insomnia and other sleep-related disorders [26, 27].
Root extract of valerian (Valeriana officinalis L.), a perennial herb, has been used as sedative since antiquity [28, 29] and is used primarily for management of sleep-related conditions across the world, including the Americas and Europe [30, 31]. The root extract of valerian (VE) exhibits anti-oxidant, antimicrobial, anti-inflammatory, sedative, anxiolytic, tranquilizing, spasmolytic, anticonvulsant, cytoprotective, and neuroprotective activities [32]. Valerian extract reduced sleep latency and improved sleep architecture and sleep perception of insomnia in healthy volunteers and patients suffering from sleep disorders [33, 34]. Two constituents of valerian, namely, volatile oils and valepotriates, potentially account for its activity [28, 31, 35]. Many preclinical and clinical studies have demonstrated valerian as an effective alternative treatment for insomnia [33, 34].
The current study evaluates higher potency standardized VE on sleep in subjects with sleep complaints after supplementation for 8 weeks in a randomized, double-blind, placebo-controlled, clinical interventional study. Objective evaluations of sleep using medical assistance have been performed in clinical laboratory settings using advanced technologies, such as polysomnography (PSG), electroencephalograms, electrocardiograms, etc., [36–39]. We used the most widely used subjective tool, i.e., the Pittsburgh Sleep Quality Index (PSQI) questionnaire, objective tools like wrist actigraphy bands and PSG, to measure various sleep parameters, such as overall sleep quality, sleep latency, sleep efficiency, actual sleep time, and sleep stages. Further, validated questionnaires were used to measure daytime sleepiness, anxiety, and feeling of waking up refreshed.
Methods
Study Material
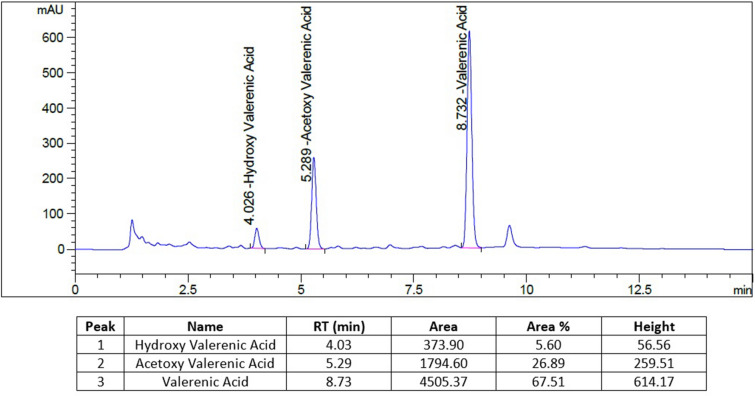
Spray-dried powder of VE (commercially known as Sleeproot®) consists of the hydro-alcoholic extract of valerian roots 26.23% (OmniActive Health Technologies, Mumbai, India), cellulose polymer 73.27% (Novo Excipients, Navi Mumbai, India), and colloidal silicon dioxide 0.5% (Daksh Medicare, Mumbai, India). The final composition consists of 2% total valerenic acid as established by HPLC (Fig. 1). The placebo contained microcrystalline cellulose.
Fig. 1.
Chromatogram of valerenic acid obtained by HPLC
Study Design and Procedures
This was a clinical interventional trial that lasted for a total of 56 days and consisted of a randomized, double-blind, placebo-controlled, parallel design. Participants were adults who had mild insomnia symptoms without any comorbidities. Before beginning the study, a written approval was received from the BGS Global Institute of Medical Sciences Institutional Ethics Committee in Bengaluru, India. The investigation was included in the Clinical Trials Registry of India (CTRI/2022/05/042818) as a registered study. The research was carried out in accordance with the standards that were mandated by the Indian Council of Medical Research's regulatory regulations, as well as their ethical guidelines, the International Council for Harmonization Guidance on Good Clinical Practice (E6R2), and the Declaration of Helsinki.
Each participant gave their signed, informed, and voluntary consent to participate in the study before they were enrolled. During the screening period, information such as a person's age, gender, current medications, and medical history was gathered. Subjects who were eligible were given either VE capsules (containing 200 mg of valerian extract) or placebo capsules. The random assignment was carried out in a ratio of 1:1. The participants were told to take one capsule 1 h before bedtime, and at the same time every day for a period of 56 days. An independent expert who was not involved in the study used R software version 4.2.1 to build the randomization schedule using a block randomization method with a block size of 4.
The study visits that were planned included a screening/baseline visit, randomization visit, and follow-up visits on Days 3, 14, 28, and 56. The subjects were accommodated at the designated study site for a period of three consecutive days during each scheduled visit. These visits occurred on specific days, namely Days − 3 to − 1, 1−3, 12−14, 26−28, and 54−56. During the house visits, participants were instructed to consistently wear a wrist actigraphy device for a duration of three consecutive nights. This was carried out in order to evaluate sleep latency, total sleep time, and sleep efficiency. Each visit utilized an average of 3 days' worth of data. Overnight PSG was conducted on two separate occasions, specifically on Days 1 and 56, within a subset population consisting of 40 participants. This subset population was further divided into two groups, with 20 subjects receiving VE and the remaining 20 subjects receiving a placebo. The purpose of the PSG was to evaluate various sleep parameters, including total sleep time, sleep latency, sleep efficiency, and sleep stages, which encompass non-rapid eye movement phases 1, 2, and 3, and rapid eye movement.
Inclusion/Exclusion Criteria
Subjects who met all the following criteria were included in the study: healthy male or female adults aged 18–50 years (both limits inclusive); BMI of 18.5–29.9 kg/m2 (both limits inclusive); PSQI score of 5 and above; insomnia severity index score of 14 and below; BAI score of 15 and below; subjects who agreed to maintain their usual level of activity throughout the trial period and willing to refrain from vigorous physical activity within 2 h of bedtime; subjects who agreed to maintain their usual dietary habits and level of exercise, i.e., maintain their usual life-style throughout the trial period; subjects who agreed to consume the study product 60 min before bed throughout the study period; subjects who agreed to refrain from taking any medications or preparations to improve sleep (herbal, dietary supplements, homeopathic preparations, etc.) during the study; subjects who agreed to consume no more than 4 servings of caffeine substances per day and no caffeine within 6 h of bedtime; and subjects who agreed to stay weight stable during the study period.
Subjects who met any of the following criteria were excluded from the study: individuals who were allergic to the study product or had a history of being allergic to it; who had cancer; laboratory abnormalities that researchers thought were risky or could make it difficult to collect data; uncontrolled high blood pressure at the screening visit (systolic blood pressure > 160 mm Hg or diastolic blood pressure > 100 mm Hg); taking hypnotics, antihistamines, antidepressants, antipsychotics, anticonvulsants, centrally acting corticosteroids, opioid painkillers, or prescribed sleep medications; had a history of drug and/or alcohol abuse at the time of enrolment; were pregnant, nursing, or planning a pregnancy during the study period; had received any investigational medication or device within 3 months of study entry; or whom the investigator believed had a chronic medical condition that could affect energy or fatigue levels.
Safety and Efficacy Parameters
Efficacy parameters included questionnaire-based assessments like the PSQI, the Epworth Sleepiness Scale (ESS), the Beck Anxiety Inventory (BAI), and the Visual Analogue Scale (VAS) for the feeling of waking up refreshed, as well as objective sleep assessments using wrist actigraphy, and PSG.
Safety parameters included physical examination, vital signs measurement, hematology (total leukocyte count, red blood cell count, hemoglobin, hematocrit, mean cell volume, mean cell hmoglobin, mean cell hemoglobin concentration, platelet count, neutrophils, lymphocytes, eosinophils, monocytes, and basophils) and clinical chemistry tests (aspartate aminotransferase, alanine transaminase and serum creatinine). Adverse events (AEs) and serious adverse events (SAEs) were monitored throughout the study period.
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a self-reporting questionnaire designed to evaluate sleep quality and disruptions within a period of 1 month. The initial four items are formulated as open-ended questions, whereas items 5–19 are assessed using a 4-point Likert scale. The scores of individual items contribute to the formation of seven components. The sleep quality of an individual is assessed by calculating a composite score, which ranges from 0 to 21. This number is derived by summing the seven component scores, where larger scores are indicative of poorer sleep quality. The PSQI questionnaire was administered during the first assessment, as well as during follow-up visits on Days 14 and 28, and at the end of the study on Day 56.
Wrist Actigraphy
Actigraphy devices worn on the wrist record movement data that can be used to estimate sleep parameters using specialized computer software algorithms. The participants undertook wrist actigraphy testing at the study site and were instructed to wear a wrist actigraphy device (MotionWatch 8; CamNtech, Cambridge, UK) for three consecutive nights as per the study protocol. The mean change was evaluated at baseline, Days 3, 14, and 28, and the end of the study (Day 56).
Beck Anxiety Inventory (BAI)
BAI is a self-reported questionnaire that measures 21 prevalent somatic and cognitive anxiety symptoms. The BAI comprises 21 items with Likert scales spanning from 0 to 3 and total scores ranging from 0 to 63. The BAI scores are categorized as follows: minimal anxiety (0–7 points), mild anxiety (8–15 points), moderate anxiety (16–25 points), and severe anxiety (30–63 points). The BAI questionnaire was administered at the beginning of the investigation, on Days 3, 14, and 28, and at the end of the study (Day 56).
Epworth Sleepiness Scale (ESS)
The ESS is a brief questionnaire designed to assess levels of drowsiness during the day. Each respondent rates themselves on 8 items that assess their “likelihood of dozing or falling asleep” in everyday scenarios; scores range from 0 to 3. The ESS score, which is the sum of all the components, can be anywhere from 0 to 24. The ESS questionnaire was administered during baseline, Days 3, 14, and 28, and the end of the study (Day 56).
Feeling of waking up refreshed as assessed by the visual analogue scale (VAS)
The VAS is an instrument which measures a characteristic or attitude that spans a continuum of values. Researchers who study sleep frequently use VAS to evaluate various aspects of sleep, daytime functioning, and the effects of therapeutic interventions on these variables. The most elementary VAS is a horizontal line of fixed length, typically 10 cm or 100 mm. The extremities are defined as the extreme limits of the parameter being measured (feeling of waking up refreshed), from left to right (best to worst). The VAS score is determined by measuring the distance, in centimeters, from the left end of the line to the subject’s mark.
Polysomnography (PSG)
PSG records multiple sleep-related signals by employing various measurement techniques simultaneously and continuously to record neurophysiological, cardiorespiratory, and other physiological and physical parameters, usually overnight. PSG provides quantitative documentation of abnormalities of sleep and wakefulness and their transition, and of organ dysfunctions that are influenced by the sleep state. The subjects underwent PSG in-house at the study site on Day − 1 and Day 56 overnight.
Prohibited medications or supplements
Subjects were prohibited to take any medications or preparations to improve sleep (herbal, dietary supplements, homeopathic preparations, etc.), anxiolytics, anti-depressants, antipsychotics, anticonvulsants, antihypertensive, centrally acting corticosteroids, opioid pain relievers, hypnotics, and/or prescribed sleep medications. Subjects who had received prohibited concomitant medications or products were discontinued from the study at the discretion of the investigator. Data from these subjects were evaluated up to the first dose of the prohibited concomitant medication or treatment.
Determination of Sample Size
A sample size of 80 subjects was considered sufficient to detect a clinically important difference between groups with 90% power and a 5% level of significance. Assuming a standard deviation (SD) of 2.98 at the end of treatment, 36 subjects per group would be sufficient to detect a mean difference of 1.58 in PSQI between the two groups with 90% power and a 0.05 two-sided level of significance. Considering a drop-out rate of 10%, the sample size was calculated to be 80 subjects (40 in each arm).
Statistical Analysis
Statistical analyses were carried out using R software version 4.2.1. The results for the continuous endpoints were summarized using descriptive statistics such as frequency, mean, median, standard error, 95% confidence interval (for normal distribution), and median with the 25th and 75th percentiles (for non-normal distribution). The evaluations encompassed the primary, secondary, and tertiary efficacy objectives, for which both actual values and mean change from baseline values were calculated. Paired t tests were utilized to evaluate the analysis within the group. Independent t tests were utilized to evaluate the between-group analysis for the actual and mean change values. A significance level of p < 0.05 was deemed to indicate statistical significance.
The categorical variables were summarized by calculating the frequencies and percentages. The evaluation of the comparisons between the treatment groups was conducted using either the Pearson’s Chi-square test or Fisher’s exact test, depending on the appropriateness of each test. The analyses were performed exclusively on the safety population.
A p value of less than 0.05 and a 95% confidence interval were both used to determine statistical significance for inferential tests. Additionally, a two-tailed hypothesis was employed for testing.
In general, missing data remained missing and were not included in the analyses. Data were analyzed for a per-protocol population.
Efficacy Endpoints Evaluation
Efficacy endpoints included evaluation of overall sleep quality by PSQI, sleep latency, actual sleep time and sleep efficiency by wrist actigraphy, anxiety by BAI, daytime sleepiness by ESS, and feeling of waking up refreshed by VAS, and of total sleep time, sleep latency, sleep efficiency, and sleep stages by PSG. Evaluations were performed from baseline to the end of the study visit (Day 56). Mean changes for PSQI were assessed from baseline against Days 14, 28, and 56. For other parameters, the assessments were carried out from baseline against Days 3, 14, 28, and 56 of the consumption of the products under investigation .
Safety Endpoints Evaluation
Safety analyses were performed using hematology and biochemistry assessments, the incidence of AEs/SAEs, physical examination, and vital signs measurements for all the randomized subjects who received at least one dose of the studied supplement. Descriptive statistics [n (number of subjects), mean, standard deviation, median, minimum and maximum] for continuous safety variables and frequency and the percentage for categorical safety variables such as adverse events were summarized by treatment.
Results
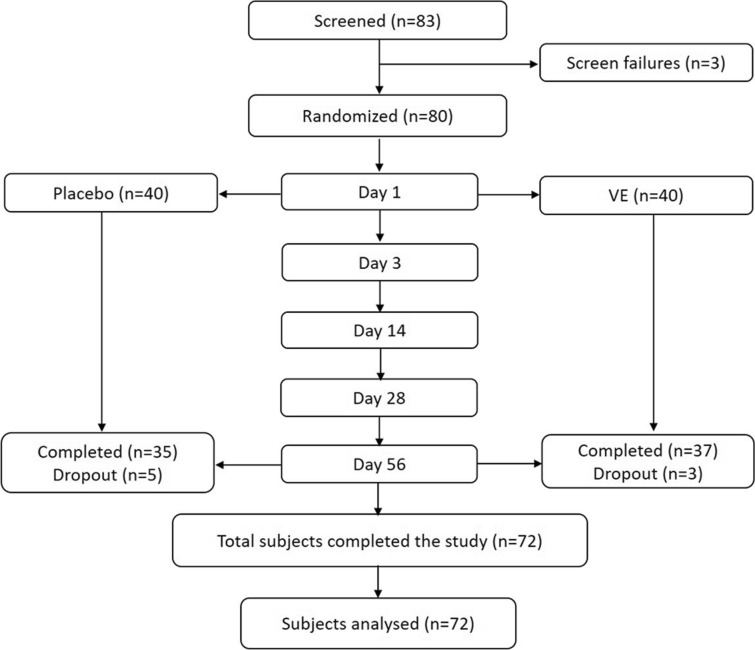
Overall, 83 subjects were screened, and 3 of them failed to meet the study’s inclusion criteria and were declared as screen failures (Fig. 2). A total of 80 subjects were randomized into a 1:1 ratio, i.e., 40 subjects per group. Of the 80 randomized subjects, 72 (35 subjects in the placebo group and 37 subjects in the VE group) completed the study and were included for the efficacy assessments. Five subjects from the placebo group and three subjects from the VE group were lost to follow-up and were treated as having withdrawn from the study.
Fig. 2.
CONSORT diagram
The demographic parameters of subjects at baseline are presented in Table 1. The mean age of participants (± SE) in the placebo group was 33.57 ± 1.06 years and in the VE group was 35.35 ± 0.92 years. The gender distribution was 16 males and 19 females in the placebo group and 15 males and 22 females in the VE group. The mean BMI (± SE) for the placebo group was 24.96 ± 0.51 kg/m2 and 25.48 ± 0.52 kg/m2 for the VE group.
Table 1.
Baseline demographics summary of study participants
| Particulars | Placebo (n = 35), mean ± SE | VE (n = 37), mean ± SE |
|---|---|---|
| Age (years) | 33.57 ± 1.06 | 35.35 ± 0.92 |
| Male, n (%) | 16 (45.71%) | 15 (40.54%) |
| Female, n (%) | 19 (54.29%) | 22 (59.46%) |
| BMI (kg/m2) | 24.96 ± 0.51 | 25.48 ± 0.52 |
| Pittsburgh sleep quality index (PSQI) | 11.43 ± 0.22 | 11.89 ± 0.20 |
| Sleep latency (min) by WA | 74.26 ± 5.24 | 89.39 ± 8.20 |
| Actual sleep time (min) by WA | 339.80 ± 6.40 | 306.09 ± 7.61 |
| Sleep efficiency (%) by WA | 72.87 ± 1.15 | 66.40 ± 1.67 |
| Beck anxiety inventory (BAI) | 11.57 ± 0.24 | 11.30 ± 0.22 |
| Epworth sleepiness scale (ESS) | 8.74 ± 0.32 | 8.65 ± 0.25 |
| VAS (feeling of waking up refreshed) | 7.29 ± 0.13 | 6.98 ± 0.15 |
Percentages are based on the number of subjects in the specified treatment
SE standard error, WA wrist actigraphy
Efficacy Results
Pittsburgh Sleep Quality Index (PSQI)
A significant (p < 0.05) decrease in PSQI total score was observed for the VE group compared to placebo from baseline on Day 14 (− 1.30 ± 0.24 for VE vs. − 0.31 ± 0.22 placebo), Day 28 (− 1.62 ± 0.20 for VE vs. 0.00 ± 0.27 placebo), and Day 56 (− 2.05 ± 0.23 for VE vs. − 0.09 ± 0.28 placebo) (Fig. 3).
Fig. 3.
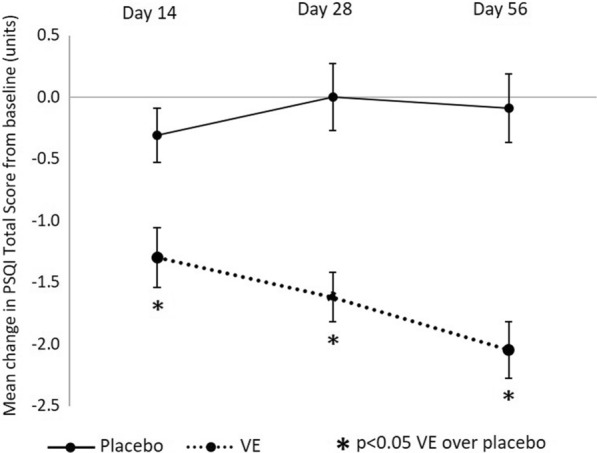
Summary results of placebo versus VE mean change from baseline in PSQI total score (units)
Further, subdomain analysis of PSQI revealed that subjects in the VE group showed significant (p < 0.05) improvements in PSQI for: subjective sleep quality and sleep latency on Days 14, 28, and 56; sleep duration and habitual sleep efficiency on Days 28 and 56; and daytime dysfunction on Day 14 compared to placebo. No significant differences were observed between the groups in PSQI for the sleep disturbance subscale.
Sleep Latency (Minutes) as assessed by Wrist Actigraphy
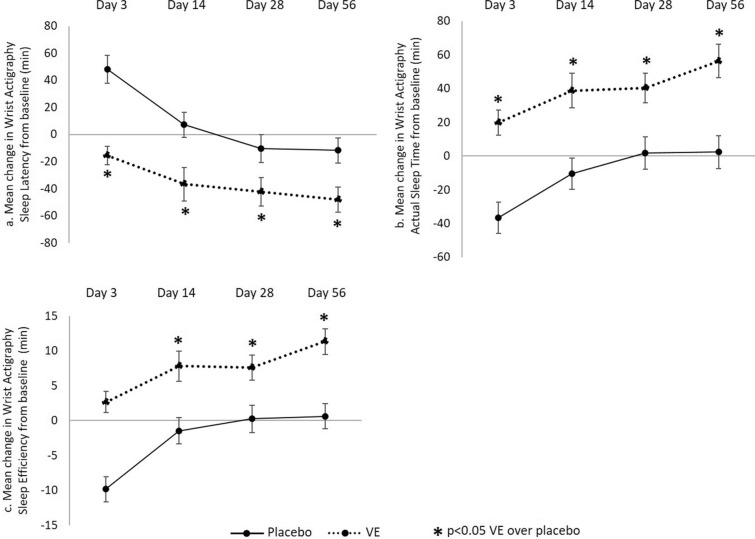
A significant (p < 0.05) decrease in sleep latency from baseline was recorded in case of the VE group on Day 3 (− 15.51 ± 6.79 for VE vs. 48.08 ± 10.27 placebo), Day 14 (− 36.67 ± 12.40 for VE vs. 7.25 ± 9.27 placebo), Day 28 (− 42.43 ± 10.48 for VE vs. − 10.37 ± 10.33 placebo), and Day 56 (− 48.03 ± 9.23 for VE vs. − 11.73 ± 9.31 placebo) compared to placebo (Fig. 4a).
Fig. 4.
Summary results of placebo versus VE mean change from baseline by wrist actigraphy in: a sleep latency (min); b actual sleep time (min); and c sleep efficiency (min)
Actual Sleep Time (Minutes) as assessed by Wrist Actigraphy
A significant (p < 0.05) increase in the actual sleep time was recorded in the VE group compared to placebo from baseline on Day 3 (19.80 ± 7.37 for VE vs. − 36.59 ± 9.14 placebo), Day 14 (38.76 ± 10.31 for VE vs. − 10.35 ± 9.31 placebo), Day 28 (40.30 ± 8.89 for VE vs. 1.65 ± 9.61 placebo), and Day 56 (56.31 ± 9.89 for VE vs. 2.33 ± 9.84 placebo) (Fig. 4b).
Sleep efficiency (%) as assessed by Wrist Actigraphy
A significant (p < 0.05) increase in sleep efficiency was recorded in the VE group from baseline compared to placebo on Day 14 (7.81 ± 2.17 for VE vs. − 1.46 ± 1.90 placebo), Day 28 (7.60 ± 1.82 for VE vs. 0.23 ± 1.95 placebo), and Day 56 (11.33 ± 1.85 for VE vs. 0.61 ± 1.80 placebo). (Fig. 4c).
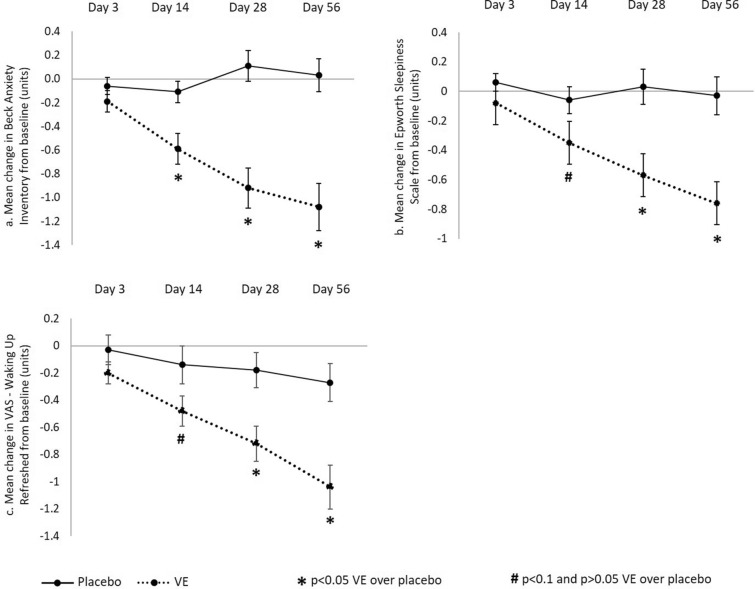
Anxiety Levels as Assessed by Beck Anxiety Inventory (BAI)
A significant (p < 0.05) decrease in anxiety score from baseline was observed for VE group compared to placebo on Day 14 (− 0.59 ± 0.13 for VE vs. − 0.11 ± 0.09 placebo), Day 28 (− 0.92 ± 0.17 for VE vs. 0.11 ± 0.13 placebo), and Day 56 (− 1.08 ± 0.20 for VE vs. 0.03 ± 0.14 placebo), and a non-significant decrease was observed on Day 03 (− 0.19 ± 0.09 for VE vs. − 0.06 ± 0.07 placebo) (Fig. 5a).
Fig. 5.
Summary results of placebo versus VE mean change from baseline in: a Beck Anxiety Inventory (units); b Epworth Sleepiness Scale (units); and c VAS waking up refreshed (units)
Daytime Sleepiness as Assessed by Epworth Sleepiness Scale (ESS)
A significant (p < 0.05) decrease in the daytime sleepiness from baseline was recorded for the VE group compared to placebo on Day 28 (− 0.57 ± 0.14 for VE vs.0.03 ± 0.12 placebo), and Day 56 (− 0.76 ± 0.16 for VE vs. − 0.03 ± 0.13 placebo), and a decreasing trend (p = 0.0522) on Day 14 (− 0.35 ± 0.12 for VE vs. − 0.06 ± 0.09 placebo) (Fig. 5b).
Feeling of Waking Up Refreshed as Assessed by VAS Scale
A significant (p < 0.05) improvement (decrease) in the waking up refreshed feeling from baseline was recorded for the VE group compared to placebo on Day 28 (− 0.72 ± 0.13 for VE vs. − 0.18 ± 0.13 placebo), and Day 56 (− 1.04 ± 0.16 for VE vs. − 0.27 ± 0.14 in placebo group), a decreasing trend (p = 0.0646) on Day 14 (− 0.48 ± 0.11 for VE vs. − 0.14 ± 0.14 placebo), and a non-significant decrease on Day 3 (− 0.20 ± 0.08 for VE vs. − 0.03 ± 0.11 placebo) (Fig. 5c).
Polysomnography (PSG)
Total Sleep Time (in Minutes) Assessed by PSG
A significant (p < 0.05) increase in total sleep time from baseline was seen in the VE group compared to placebo on Day 56 (75.21 ± 34.05 in VE vs. − 74.58 ± 31.33 placebo) (Fig. 6a).
Fig. 6.
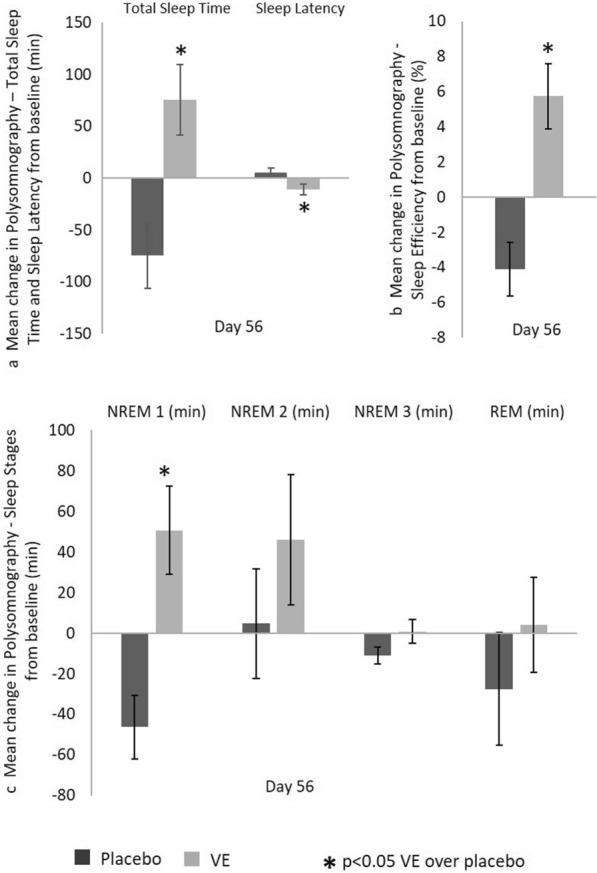
Summary of placebo versus VE PSG results. Mean change from baseline in: a total sleep time and sleep latency (min); b sleep efficiency (%); and c sleep stages (min)
Sleep Latency (in Minutes) assessed by PSG
A significant (p < 0.05) decrease in sleep latency from baseline was seen in the VE group compared to placebo on Day 56 (− 10.89 ± 4.98 in VE vs. 5.34 ± 4.17 placebo) (Fig. 6a).
Sleep Efficiency (Percent) Assessed by PSG
A significant (p < 0.05) increase in the sleep efficiency from baseline was seen in the VE group compared to placebo on Day 56 (5.74 ± 1.87 in VE vs. − 4.11 ± 1.53 placebo) (Fig. 6b).
Non-Rapid Eye Movement 1 (in Minutes) Assessed by PSG
A significant (p < 0.05) increase in non-rapid eye movement 1 sleep from baseline was observed in the VE group compared to placebo on Day 56 (50.74 ± 21.75 in VE vs. 46.24 ± 15.63 placebo) (Fig. 6c).
Non-rapid Eye Movement 2 (Minutes) Assessed by PSG
A non-significant increase in non-rapid eye movement 2 sleep from baseline was observed in the VE group compared to placebo on Day 56 (46.21 ± 32.17 in VE vs. 4.79 ± 27.00 placebo) (Fig. 6c).
Non-rapid Eye Movement 3 (Minutes) assessed by PSG
No significant difference was seen between the VE and placebo groups for non-rapid eye movement 3 sleep on Day 56 from baseline (0.84 ± 5.88 in VE group compared to − 10.92 ± 4.26 in placebo) (Fig. 6c).
Rapid Eye Movement (Minutes) Assessed by PSG
A non-significant increase in rapid eye movement sleep from baseline was observed for the VE group compared to placebo on Day 56 (4.24 ± 23.37 in VE vs. − 27.55 ± 27.73 in placebo) (Fig. 6c).
The absolute values and mean change values ± standard error values for the primary, secondary, and tertiary endpoints are presented in the Supplementary Material.
Safety Results
All the randomized subjects were included in the safety analysis. Throughout the trial, no clinically significant differences in vital signs, physical examination, or hematological and biochemical parameters were seen in any of the groups.
During the study, total of 12 AEs were reported by 8 (10%) subjects: 5 were reported by 3 (7.5%) subjects in the VE group, and 7 by 5 (12.5%) subjects in the placebo group. Subjects in the VE group reported one event each of upper respiratory tract infection, sore throat, headache, viral fever, and loose motion, while two events of fever and one each of upper respiratory tract infection, sore throat, headache, gastritis, and common cold were reported by subjects in the placebo group. Fever, upper respiratory tract infection, sore throat, and headache were the most common AEs experienced by two (2.5%) subjects overall.
All the AEs reported by the subjects were mild in severity and resolved, and the causality of the AEs was deemed by the investigator not to be related to the products under investigation. None of the subjects reported an SAE or was withdrawn from the study due to an AE or SAE.
In total, 14 (17.5%) subjects (7 each in the VE and placebo groups) used at least one concomitant mediation during the course of the study. The most commonly used medications included paracetamol. Overall, the safety and tolerability of the VE was confirmed by the safety assessments in the study.
Discussion
Sleep deprivation for longer periods of time may impact quality of life, cognitive performance [3–5, 40], and increase the risk of metabolic disorders such as hypertension, cardiovascular diseases, and diabetes [41, 42]. Supplementation with synthetic melatonin is used worldwide to treat insomnia and other sleep-related conditions. However, melatonin is only moderately effective in clinical studies, associated with daytime sleepiness and concerns have been raised about the possible long-term effects of taking it [20, 21]. Most commonly prescribed sleep solutions, based on benzodiazepine and non-benzodiazepine hypnotic drugs, are associated with adverse effects while providing modest improvements in sleep benefits. Valerian root extract is one of the most popular herbal supplements used for improving sleep. Several human clinical studies have not only established the safety of the valerian extract but also demonstrated overall improvement in multiple sleep-related parameters. However, several meta-analyses of published clinical studies have failed to establish consistent sleep benefits of valerian, probably due to flawed study design, use of valerian extract that is not well characterized or containing very low active content, suboptimal doses, or suboptimal measures for the efficacy of interventions [43]. In the current study, we have used a VE with 2% total valerenic acid content compared to the 0.5–0.8% used in most of the preparations explored in the past. Further, we have used both subjective and objective sleep parameters to measure the sleep efficacy using PSQI, wrist actigraphy, and PSG. Through a double-blind, placebo-controlled, parallel study, we have demonstrated that VE supplementation that contains 2% total valerenic acid at a 200-mg dose for 56 days significantly improved various subjective and objective parameters of sleep, including overall sleep quality, sleep latency, sleep efficiency, and total sleep time, in young subjects with mild insomnia symptoms and without comorbidities. Further, VE supplementation helped to reduce anxiety and daytime sleepiness, and improved the feeling of being refreshed after waking up in the morning. Throughout the study, VE was found to be safe and well tolerated.
Sleep assessment methods influence the outcome of sleep intervention studies. Few studies that used PSG, actigraphy, and sleep diaries concurrently to measure sleep parameters have reported that actigraphy and PSQI score yield comparable estimates of sleep to that of PSG [44]. PSG directly measures brain electrophysiology and is considered as the “gold standard” for many sleep outcomes [45], but has challenges in terms of cost and ease of use. We observed significant improvements in sleep parameters with VE supplementation over placebo as measured through PSG on Day 56, with increased total sleep time and decreased sleep latency associated with improved sleep efficiency. Both wrist actigraphy and PSQI score showed comparable results to that of PSG on Day 56 post-supplementation, which is a strong validation of the effectiveness of VE for management of sleep. We also observed similar improvements for sleep latency, actual sleep time, and sleep efficiency over placebo as early as 14 and 28 days post-VE supplementation, as measured by wrist actigraphy and PSQI. However, we observed relatively longer sleep latency, but still significant, compared to placebo, in the case of wrist actigraphy versus PSG for both the VE and placebo groups. Multiple published human studies that reported excellent concordance in sleep parameters endpoints with wrist actigraphy and PSG also reported longer sleep latency in the case of actigraphy [46]. It is believed that, as actigraphy monitors body movements to measure sleep, it may overestimate sleep latency due to body movements during sleep or disturbed sleep. In our study, wrist actigraphy demonstrated improved sleep latency and actual sleep time with VE as early as 3 days post-supplementation, thus providing an early indicator of positive sleep responses.
Multiple clinical studies have demonstrated the sleep benefits of valerian, with significant improvements in insomnia [47] and several sleep parameters [48–50]. The effectiveness of valerian as a single herb or in combination with other herbs has also been reported to provide benefits in cases of sleep issues associated with anxiety, obsessive compulsive disorders, cognitive dysfunctions, depression, hypertension, premenstrual syndrome, and sleep issues post-surgery [43, 51–54]. Valerenic acid from valerian is considered responsible for sedative activities through modulation of GABAA receptor function [31], inhibition of enzymatic breakdown of GABA, enhanced benzodiazepine binding [55], or partial agonistic activities against the 5-HT5a receptor, as demonstrated through experimental studies [35]. Valepotriates from valerian are believed to possess an anxiolytic effect. VE significantly (p < 0.05) increased the sleep duration with shorter sleep latency which was comparable to melatonin through modulation of GABA and 5-HT5a receptor expression in brain tissues in a pentobarbital-induced sleep model in mice (manuscript in preparation).
Our study limitation was that our subjects entered the study with higher sleep latency issues, as evident from baseline sleep latency time from wrist actigraphy and PSQI, suggesting that they possibly had mild to moderate insomnia symptoms as against our target for subjects with mild insomnia symptoms. Nevertheless, we saw significant effects on sleep latency with VE compared to placebo. Further, we used a simplistic statistical methodology for the data analysis which included paired t tests for within-group analysis and independent t tests for between-group analysis.
Conclusion
Our results indicate that VE with 2% valerenic acid showed significant improvements in overall sleep quality, latency, efficiency, total sleep time, decreased anxiety and daytime sleepiness, and increased feeling refreshed after waking up in young subjects with mild insomnia symptoms and without comorbidities. Unlike other studies, our results demonstrated significant improvements from both subjective and objective evaluations. Also, the safety and tolerability of VE was confirmed by the safety assessments in the study subjects.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the participants of the study.
Medical Writing and Editorial Assistance
The authors didn’t use any medical writing and editorial assistance for this article.
Author Contributions
Harshith Chandra Shekhar and Jestin V Thomas contributed to the study conception and design. Study conduct, subject recruitment and data collection were performed at study centre by Harshith Chandra Shekhar. Study was monitored in blinded fashion by Lincy Joshua. Statistical analysis and study report were prepared by Jestin V Thomas. Overall study data interpretation was carried out by Harshith Chandra Shekhar and Jestin V Thomas. The first draft of the manuscript was written by Harshith Chandra Shekhar and Jestin V Thomas. All authors provided their inputs, read and approved the final manuscript.
Funding
This study and the journal’s Rapid Service Fee was supported by OmniActive Health Technologies Limited (Mumbai, India).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethical Approval
A written approval was obtained from BGS Global Institute of Medical Sciences Institutional Ethics Committee, Bengaluru, India, before commence of the study. The study was registered with the Clinical Trials Registry of India (CTRI/2022/05/042818). The study was conducted as per the regulatory requirements of the Indian Council of Medical Research, ethical guidelines, International Council for Harmonization Guidance on Good Clinical Practice (E6R2) and the Declaration of Helsinki. A voluntary informed consent was obtained, in written, from every participant before enrolling in the study.
References
- 1.Kumar VM. Sleep and sleep disorders. Indian J Chest Dis Allied Sci. 2008;50(1):129. [PubMed] [Google Scholar]
- 2.Luyster FS, Strollo PJ, Jr, Zee PC, Walsh JK. Sleep: a health imperative. Sleep. 2012;35(6):727–734. doi: 10.5665/sleep.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medic G, Wille M, Hemels ME. Short-and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151–161. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olesen J, Gustavsson A, Svensson M, Wittchen HU, Jönsson B, Group CS, et al. The economic cost of brain disorders in Europe. Eur J Neurol. 2012;19(1):155–162. doi: 10.1111/j.1468-1331.2011.03590.x. [DOI] [PubMed] [Google Scholar]
- 5.Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. J Clin Sleep Med. 2015;11(8):931–952. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Staner L. Sleep and anxiety disorders. Dialogues Clin Neurosci. 2022;5(3):249–258. doi: 10.31887/DCNS.2003.5.3/lstaner. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonnet MH. Effect of sleep disruption on sleep, performance, and mood. Sleep. 1985;8(1):11–19. doi: 10.1093/sleep/8.1.11. [DOI] [PubMed] [Google Scholar]
- 8.Dinges DF, Douglas SD, Hamarman S, Zaugg L, Kapoor S. Sleep deprivation and human immune function. Adv Neuroimmunol. 1995;5(2):97–110. doi: 10.1016/0960-5428(95)00002-J. [DOI] [PubMed] [Google Scholar]
- 9.Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006;166(16):1768–1774. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- 10.Kasasbeh E, Chi DS, Krishnaswamy G. Inflammatory aspects of sleep apnea and their cardiovascular consequences. South Med J. 2006;99(1):58–68. doi: 10.1097/01.smj.0000197705.99639.50. [DOI] [PubMed] [Google Scholar]
- 11.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91(11):881–884. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz DJ, Kohler WC, Karatinos G. Symptoms of depression in individuals with obstructive sleep apnea may be amenable to treatment with continuous positive airway pressure. Chest. 2005;128(3):1304–1309. doi: 10.1378/chest.128.3.1304. [DOI] [PubMed] [Google Scholar]
- 13.Zimmerman M, McGlinchey JB, Young D, Chelminski I. Diagnosing major depressive disorder I: a psychometric evaluation of the DSM-IV symptom criteria. J Nerv Ment Dis. 2006;194(3):158–163. doi: 10.1097/01.nmd.0000202239.20315.16. [DOI] [PubMed] [Google Scholar]
- 14.Makarem N, Shechter A, Carnethon MR, Mullington JM, Hall MH, Abdalla M. Sleep duration and blood pressure: recent advances and future directions. Curr Hypertens Rep. 2019;21(5):33. doi: 10.1007/s11906-019-0938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hillman DR, Murphy AS, Antic R, Pezzullo L. The economic cost of sleep disorders. Sleep. 2006;29(3):299–305. doi: 10.1093/sleep/29.3.299. [DOI] [PubMed] [Google Scholar]
- 16.Leger D. The cost of sleep-related accidents: a report for the National Commission on sleep disorders research. Sleep. 1994;17(1):84–93. doi: 10.1093/sleep/17.1.84. [DOI] [PubMed] [Google Scholar]
- 17.Stoller MK. Economic effects of insomnia. Clin Ther Int Peer-Rev J Drug Ther. 1994;6:873–897. [PubMed] [Google Scholar]
- 18.Rama AN, Cho SC, Kushida CA. Sleep: a comprehensive handbook. Amsterdam: Wiley; 2006. Normal human sleep; pp. 3–10. [Google Scholar]
- 19.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30(3):274–280. [PubMed] [Google Scholar]
- 20.Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: melatonin for the treatment of primary sleep disorders. PLoS ONE. 2013;8(5):e63773. doi: 10.1371/journal.pone.0063773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boutin JA, Kennaway DJ, Jockers R. Melatonin: facts, extrapolations and clinical trials. Biomolecules. 2023;13(6):943. doi: 10.3390/biom13060943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schroeck JL, Ford J, Conway EL, Kurtzhalts KE, Gee ME, Vollmer KA, et al. Review of safety and efficacy of sleep medicines in older adults. Clin Ther. 2016;38(11):2340–2372. doi: 10.1016/j.clinthera.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 23.Longo LP, Johnson B. Addiction: Part I .Benzodiazepines—side effects, abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121–2128. [PubMed] [Google Scholar]
- 24.Stewart SA. The effects of benzodiazepines on cognition. J Clin Psychiatry. 2005;66(2):9–13. [PubMed] [Google Scholar]
- 25.Hanson RC, Braselton JP, Hayes DC, Snyder RW, White JB, Deitchman D. Cardiovascular and renal effects of buspirone in several animal models. Gen Pharmacol. 1986;17(3):267–274. doi: 10.1016/0306-3623(86)90040-6. [DOI] [PubMed] [Google Scholar]
- 26.Gooneratne NS. Complementary and alternative medicine for sleep disturbances in older adults. Clin Geriatr Med. 2008;24(1):121–138. doi: 10.1016/j.cger.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Antoniades J, Jones K, Hassed C, Piterman L. Sleep… naturally: a review of the efficacy of herbal remedies for managing insomnia. Altern Complement Ther. 2012;18(3):136–140. doi: 10.1089/act.2012.18310. [DOI] [Google Scholar]
- 28.Houghton PJ. The biological activity of valerian and related plants. J Ethnopharmacol. 1988;22(2):121–142. doi: 10.1016/0378-8741(88)90123-7. [DOI] [PubMed] [Google Scholar]
- 29.Hobbs C. Valerian: a literature review. HerbalGram. 1989;21:19–34. [Google Scholar]
- 30.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. In: Seminars in integrative medicine. Elsevier; 2004. pp. 54–71. [PubMed]
- 31.Houghton PJ. The scientific basis for the reputed activity of valerian. J Pharm Pharmacol. 1999;51(5):505–512. doi: 10.1211/0022357991772772. [DOI] [PubMed] [Google Scholar]
- 32.Nandhini S, Narayanan KB, Ilango K. Valeriana officinalis: a review of its traditional uses, phytochemistry and pharmacology. Asian J Pharm Clin Res. 2018;11(1):36–41. doi: 10.22159/ajpcr.2018.v11i1.22588. [DOI] [Google Scholar]
- 33.Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: a meta-analysis of treatment efficacy. Arn J. 1994;151:1172–1180. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- 34.Bent S, Padula A, Moore D, Patterson M, Mehling W. Valerian for sleep: a systematic review and meta-analysis. Am J Med. 2006;119(12):1005–1012. doi: 10.1016/j.amjmed.2006.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pilerood SA, Prakash J. Nutritional and medicinal properties of valerian (Valeriana officinalis) herb: a review. Int J Food Sci Nutr Diet. 2013;1:25–33. [Google Scholar]
- 36.Becker NB, Martins RIS, de Neves JS, Chiodelli R, Rieber MS. Sleep health assessment: a scale validation. Psychiatry Res. 2018;259:51–55. doi: 10.1016/j.psychres.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 37.Hoey LM, Fulbrook P, Douglas JA. Sleep assessment of hospitalised patients: a literature review. Int J Nurs Stud. 2014;51(9):1281–1288. doi: 10.1016/j.ijnurstu.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 38.Ibáñez V, Silva J, Cauli O. A survey on sleep assessment methods. PeerJ. 2018;6:e4849. doi: 10.7717/peerj.4849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15(4):259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Colten HR, Altevogt BM, Institute of Medicine (US) Committee on Sleep Medicine and Research. Extent and health consequences of chronic sleep loss and sleep disorders. In: Sleep disorders and sleep deprivation: an unmet public health problem. National Academies Press (US); 2006 [cited 2023 Mar 3]. https://www.ncbi.nlm.nih.gov/books/NBK19961/. [PubMed]
- 41.Paillard T. Detrimental effects of sleep deprivation on the regulatory mechanisms of postural balance: a comprehensive review. Front Hum Neurosci. 2023;17:1146550. doi: 10.3389/fnhum.2023.1146550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Fam Med Prim Care. 2016;5(4):780. doi: 10.4103/2249-4863.201153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shinjyo N, Waddell G, Green J. Valerian root in treating sleep problems and associated disorders—a systematic review and meta-analysis. J Evid Based Integr Med. 2020;25:2515690X2096732. doi: 10.1177/2515690X20967323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaplan KA, Talbot LS, Gruber J, Harvey AG. Evaluating sleep in bipolar disorder: comparison between actigraphy, polysomnography, and sleep diary. Bipolar Disord. 2012;14(8):870–879. doi: 10.1111/bdi.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J, Jr, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28(4):499–523. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]
- 46.Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139(6):1514–1527. doi: 10.1378/chest.10-1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taavoni S, Ekbatani N, Kashaniyan M, Haghani H. Effect of valerian on sleep quality in postmenopausal women: a randomized placebo-controlled clinical trial. Menopause. 2011;18(9):951–955. doi: 10.1097/gme.0b013e31820e9acf. [DOI] [PubMed] [Google Scholar]
- 48.Schulz H, Stolz C, Müller J. The effect of valerian extract on sleep polygraphy in poor sleepers: a pilot study. Pharmacopsychiatry. 1994;27(04):147–151. doi: 10.1055/s-2007-1014295. [DOI] [PubMed] [Google Scholar]
- 49.Kuhlmann J, Berger W, Podzuweit H, Schmidt U. The influence of valerian treatment on’reaction time, alertness and concentration’in volunteers. Pharmacopsychiatry. 1999;32(06):235–241. doi: 10.1055/s-2007-991100. [DOI] [PubMed] [Google Scholar]
- 50.Leathwood PD, Chauffard F, Heck E, Munoz-Box R. Aqueous extract of valerian root (Valeriana officinalis L.) improves sleep quality in man. Pharmacol Biochem Behav. 1982;17(1):65–71. doi: 10.1016/0091-3057(82)90264-7. [DOI] [PubMed] [Google Scholar]
- 51.Howell D, Oliver TK, Keller-Olaman S, Davidson JR, Garland S, Samuels C, et al. Sleep disturbance in adults with cancer: a systematic review of evidence for best practices in assessment and management for clinical practice. Ann Oncol. 2014;25(4):791–800. doi: 10.1093/annonc/mdt506. [DOI] [PubMed] [Google Scholar]
- 52.Ahmadi M, Khalili H, Abbasian L, Ghaeli P. Effect of valerian in preventing neuropsychiatric adverse effects of efavirenz in HIV-positive patients: a pilot randomized, placebo-controlled clinical trial. Ann Pharmacother. 2017;51(6):457–464. doi: 10.1177/1060028017696105. [DOI] [PubMed] [Google Scholar]
- 53.Moghadam ZB, Rezaei E, Gholami RS, Kheirkhah M, Haghani H. The effect of valerian root extract on the severity of pre menstrual syndrome symptoms. J Tradit Complement Med. 2016;6(3):309–315. doi: 10.1016/j.jtcme.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pinheiro MLP, Alcântara CEP, de Moraes M, de Andrade ED. Valeriana officinalis L. for conscious sedation of patients submitted to impacted lower third molar surgery: a randomized, double-blind, placebo-controlled split-mouth study. J Pharm Bioallied Sci. 2014;6(2):109. doi: 10.4103/0975-7406.129176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ortiz JG, Nieves-Natal J, Chavez P. Effects of Valeriana officinalis extracts on [3 H] flunitrazepam binding, synaptosomal [3 H] GABA uptake, and hippocampal [3 H] GABA release. Neurochem Res. 1999;24:1373–1378. doi: 10.1023/A:1022576405534. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.