Abstract
Purpose:
To quantify the impact of the COVID-19 pandemic on surgical volumes performed by fellowship-trained glaucoma subspecialists.
Methods:
This retrospective cohort analysis of the CMS Medicare Public Use File extracted all glaucoma surgeries including micro-invasive glaucoma surgeries, trabeculectomy, goniotomy, lasers, and cataract surgery performed by fellowship-trained glaucoma surgeons in rural and urban areas between 2016 and 2020. Predicted estimates of 2020 surgical volumes were created utilizing linear squares regression. Percent change between predicted and observed 2020 surgical volume estimates was analyzed. Statistical significance was achieved at p<0.05.
Results:
In 2020, fellowship trained glaucoma surgeons operated mostly in urban areas (N=810, 95%). A 29% and 31% decrease in predicted cataract surgery volumes in urban and rural areas was observed. Glaucoma surgeries experienced a 36% decrease from predicted estimates (N=56,781). MIGS experienced a 86% and 75% decrease in rural and urban areas respectively. Trabeculectomy in rural areas experienced a 16% increase relative to predicted estimates while urban areas experienced a decrease of 3% (p>0.05). The number of goniotomies decreased by 10% more in rural areas than in urban areas (−22% and −12%, respectively). Laser procedures decreased by 8% more in urban areas than in rural areas (−18% and −10%, respectively).
Conclusions:
Among glaucoma-trained surgeons, glaucoma surgeries experienced a greater volume loss than cataract surgeries. In urban US areas, relative reductions in MIGS and goniotomy volumes in urban areas may have been compensated by greater laser and trabeculectomy volumes. Trabeculectomies in rural areas was the only group exceeding predicted estimates. Glaucoma subspecialists may utilize these findings when planning for future events and in overcoming any remaining unmet need in terms of glaucoma care.
Keywords: glaucoma, COVID-19, surgery, Medicare, rural, urban
Précis
The change in glaucoma surgical volumes due to the COVID-19 pandemic was not uniform across procedure types and unequal between rural and urban practice locations.
Introduction
The COVID-19 pandemic challenged existing models of ophthalmic care delivery.1 A recent review demonstrated the field of ophthalmology experienced the greatest loss of clinical volume early in the pandemic relative to all medical specialties.1 Ophthalmic clinical volumes declined 81% during March and April of 2020 compared to the corresponding months in 2019.2 Surgical volumes also experienced a substantial decline of 97% and 88% for cataract and glaucoma surgeries, respectively.2
A plethora of surgical and non-surgical medical specialties report similar findings. Radiologic imaging volumes for PET/CT in low-surge academic medical systems decreased relative to screening modalities including breast screening and DEXA scanning.3 Approximately 526,000 to 538,000 cases of total knee and hip arthroplasties were performed nationally in 2020, representing a 47% decrease relative to the prior 3-year average.4 Elective cases of adult cardiac surgery experienced a greater reduction in volume relative to non-elective cases (66% versus 53%); the Mid-Atlantic and New England regions experienced greater volume loss and mortality during the first COVID-19 surge.5 Otolaryngologists also experienced significant volume losses for a variety of ear, nose, and throat procedures, including flexible nasendoscopy.6,7
Urban-rural designations are characterized as important determinants of healthcare utilization during the pandemic.1 Specifically, Medicare Advantage beneficiaries residing in rural isolated, small rural, and large rural areas utilized telemedicine visits significantly less than beneficiaries residing in urban areas (adjusted incidence rate ratio (IRR) 0.822, 0.754, 0.711, all p<0.05).1 Preclusion of use of important diagnostic tools, reduced follow-up for disease monitoring, and a substantial reduction in performance of glaucoma surgery occurred.8 US counties with high-poverty indices were disproportionately influenced by less utilization of telehealth services.1 Importantly, these studies also directly comment on an expected ophthalmologic challenge of delayed patient care secondary to the pandemic for ophthalmic diseases, including retinal disease and glaucoma.1 While prior Medicare analyses have highlighted geographical variation in glaucoma subtype diagnoses and utilization for various glaucoma surgeries , analyses centered on exposing nuances associated with the Rural Urban Community Areas (RUCA) classification system are limited in number and can theoretically provide expiation for ecological biases likely present in prior studies.9,10
While prior studies provide evidence of how the COVID-19 pandemic has affected other medical specialties,3–6 additional granularity within the scope of ophthalmic practice remains an area of unresolved uncertainty.1 In the context of a dynamic clinical practice landscape during the COVID-19 pandemic, the subsequent reduction in clinical and surgical volumes relative to most other medical specialties,2 and a further unmet impetus to identify at-risk regions subsequent to the pandemic, we performed an analysis of Centers for Medicare and Medicaid Services (CMS) physician payment data. This analysis aims to characterize the influence of the COVID-19 pandemic on glaucoma surgery volumes among presumed fellowship-trained glaucoma surgeons in rural and urban US areas.
Materials and Methods
Given the use of publicly available data, this analysis does not constitute human-subjects research and was exempt from IRB review. The CMS Physician and Other Supplier Public Use File (PUF) is a nationally representative compendium containing geography- and National Provider Identification-associated claims data for all services, procedures, and surgeries performed for Medicare Part B beneficiaries.11 Data suppression is used to protect patient confidentiality by excluding services rendered to fewer than 10 beneficiaries for any year by a given provider. Ophthalmologists were identified using the Provider type field in the PUF data. Between 2016 and 2020, the PUF data was queried using Current Procedural Terminology (CPT) codes associated with micro-invasive glaucoma surgery (MIGS) (CPT Codes 65820, 66174, 66711, 0191T, 0449T, 0474T, 0253T), trabeculectomy (CPT codes 66170, 66172, 0192T/, glaucoma drainage implant (66180, 66185, 66179), office-based laser procedures (65855, 66761, 66762), and cataract surgery (66982, 66984). CPT code 66183 was not considered trabeculectomy nor MIGS due to confounding caused by cross-billing for both surgical types under one CPT code; however, 66183 was included in total surgery counts. The decision to include cataract surgery for overall surgical volume was made because it is the most performed surgery in ophthalmology.
Fellowship-trained glaucoma surgeons were identified via a manual review of National Provider Identification (NPI) numbers. After confirmation of ophthalmology as the specialty of training, each NPI was manually searched within publicly available data, including physician profiles, hospital/private practice websites, etc., to determine fellowship training in glaucoma (as of September 2022). Only glaucoma surgeons performing at least 11 traditional, incisional glaucoma procedures (trabeculectomy, glaucoma drainage implant, and office-based laser procedures) for Medicare beneficiaries within any given year during our study time interval were included within our analysis. Based on this criteria, glaucoma surgeons newly entering practice, retiring, or re-locating practice from urban to rural or vice-versa, were accounted for in our analysis on a year-to-year basis.
The US Health Resources and Services Administration – Federal Office of Rural Health Policy and the US Department of Agriculture Economic Research Service (FORHP) designed the RUCA classification system to organize the US into 10 primary and 21 secondary sub-county classes based on population density, urbanization, and daily commute.12 Areas designated as metropolitan or secondary flow to a larger urbanized area of at least 50,000 residents were deemed as Urban. Micropolitan areas, small town cores, rural areas were designated as rural.6,7 The RUCA system allows for comparisons between rural and urban US areas at the subcounty level. Precise provider practice locations were extracted from the CMS PUF and, like prior studies, categorized as either urban or rural.13 Among fellowship-trained glaucoma surgeons, cumulative volumes per procedural category per year were determined after stratification by RUCA-designated urban or rural area of surgical practice. Categorization of RUCA codes and number of glaucoma surgeons enlisted in each category are provided in Table 1.
Table 1.
The number of fellowship-trained glaucoma surgeons providing services to patients subscribed to fee-for-service Medicare based on Rural-Urban Commuting Area (RUCA).
| Number of Glaucoma Surgeons by RUCA Code in 2020 | |
|---|---|
|
| |
| Urban | 810 |
| Metropolitan area core: primary flow within an urbanized area of 50,000 and greater | 802 |
| Metropolitan area high commuting: primary flow 30% or more to a urbanized area of 50,000 and greater | 3 |
| Secondary flow 30% to <50% to a larger urbanized area of 50,000 and greater | 5 |
|
| |
| Rural | 42 |
| Micropolitan area core: primary flow within an urban cluster of 10,000 to 49,999 | 37 |
| Micropolitan high commuting: primary flow 30% or more to a urban cluster of 10,000 to 49,999 | 2 |
| Rural areas: primary flow to a tract outside a urbanized area of 50,000 and greater or UC | 2 |
| Small town core: primary flow within an urban cluster of 2,500 to 9,999 | 1 |
|
| |
| Total | 852 |
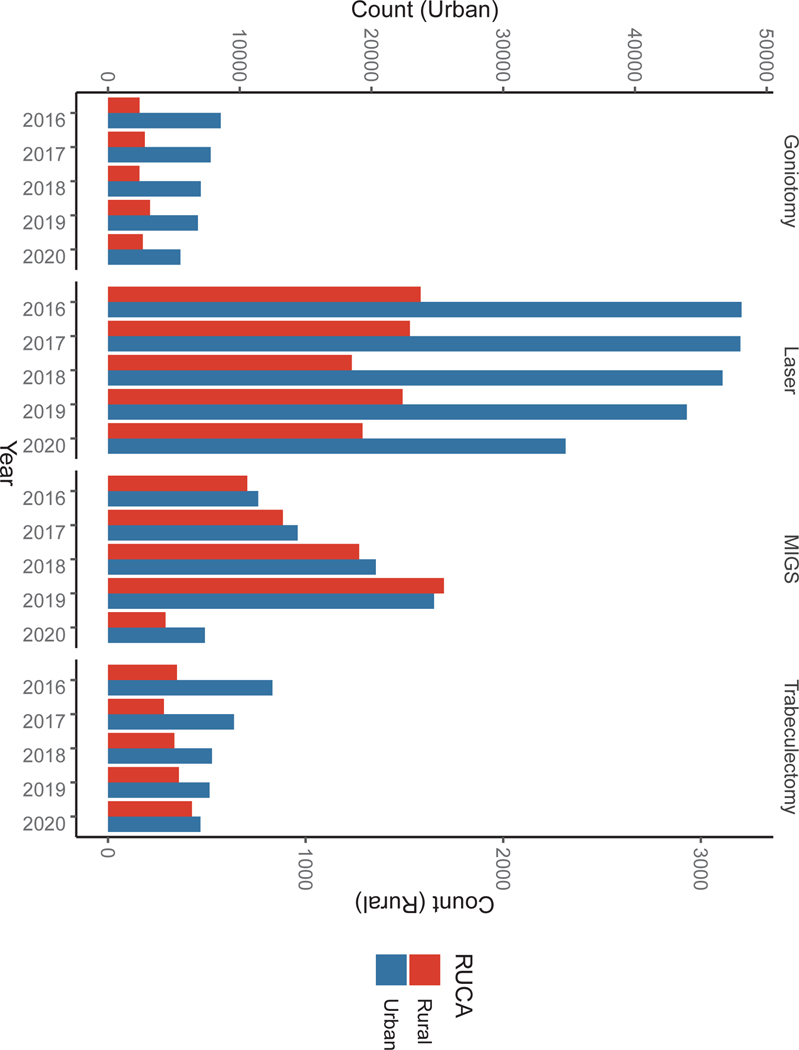
Using procedural volumes from Calendar year (CY) 2016 to CY2019, univariate ordinary least squares regression was used to predict volume for those procedures in CY2020. Figure 1 demonstrates relative volume trends across our 5-year time frame for urban and rural areas, separately; the right y-axis corresponds to rural volumes, and the left y-axis corresponds to urban volumes. The percent change between observed and predicted estimates was used as a metric of the pandemic’s influence on surgical volumes in CY2020. If the observed estimate was not within the 95% confidence interval for the predicted estimate, statistical significance was achieved at p<0.05. Statistical analyses were performed using IBM SPSS Version 29 (Armonk, NY).
Figure 1.
Change in surgical volumes of fellowship-trained glaucoma surgeons between 2016 and 2020, broken down by procedure type and by rural-urban practice location. Given large differences in the number of procedures by region, the right y-axis corresponds to rural volumes, and the left y-axis corresponds to urban volumes.
Results
In 2020, fellowship-trained glaucoma surgeons were predominantly practicing in US urban areas (N=810, 95%) compared to rural areas (Table 1). In 2020, cataract surgery accounted for the majority of total surgical volume (N=142,836, 71%) among glaucoma surgeons. The predicted number of all surgeries, including cataract removal, in 2020 in urban and rural areas was 265,107 and 20,151, respectively. However, only 185,222 and 14,395 surgeries were performed in 2020; this represents a 29% and 31% decrease from predicted volumes in urban and rural areas, respectively (p<0.05, p<0.05). A total of 88,311 glaucoma surgeries were predicted to be performed in 2020; however, only 56,781 glaucoma surgeries were observed (−36%, p<0.05). MIGS suffered the greatest loss relative to all other surgeries; relative to urban areas, rural areas experienced an additional 11% decrease in MIGS volume (−75%, p<0.05; −86%, p=0.05, respectively). Trabeculectomy in rural areas was the only procedure exceeding predicted 2020 estimates and did so by 16% (p>0.05); urban revealed a decrease by 3% (p>0.05). Volumes of goniotomy decreased by 10% more in rural areas relative to urban areas (−22%, p<0.05; −12%, p<0.05, respectively). Lasers decreased by 8% more in urban areas relative to rural areas (18%, p<0.05; 10%, p>0.05, respectively). Additional outcomes are included in Table 2.
Table 2.
Volumes of glaucoma procedures by type and by rural versus urban location from 2016 to 2020, Surgical types were defined via Current Procedural Terminology codes. Rural Urban Commuting Areas, defined by the US Census Bureau. The percent change was calculated as [Observed 2020 volume minus Predicted 2020 volume] divided by Predicted2020 volume.
| Impact of the COVID-19 Pandemic on Surgical Volumes Among Glaucoma Subspecialists, 2016–2020 | |||||||
|---|---|---|---|---|---|---|---|
| Surgery Type | Year | Beta (95% CI) | Percent Change | ||||
| 2016 | 2017 | 2018 | 2019 | 2020 | |||
|
| |||||||
| All Surgeries | |||||||
| urbanb | 234,102 | 240,339 | 245,035 | 257,591 | 185,222 | 7,516 (2,352, 12,679) | −31%* |
| ruralb | 16,442 | 16,968 | 17,947 | 19,220 | 14,395 | 931 (420, 1,441) | −29%* |
| MIGSc | |||||||
| urban | 11,404 | 14,403 | 20,333 | 24,748 | 7,353 | 4,596 (2,935, 6,256) | −75%* |
| rural | 705 | 885 | 1,271 | 1,700 | 291 | 337 (160, 513) | −86%* |
| Trabeculectomy | |||||||
| urban | 9,182 | 6,940 | 6,207 | 4,666 | 3,328 | −1,428 (2,387, 4,089) | −3% |
| rural | 186 | 143 | 187 | 140 | 151 | −9.4 (76, 185) | 16% |
| Goniotomy | |||||||
| urban | 8,561 | 7,795 | 7,046 | 6,829 | 5,497 | −595 (−999, −189) | −12%* |
| rural | 160 | 186 | 159 | 213 | 176 | 13 (−31, 58) | −22%* |
| Lasers | |||||||
| urban | 48,093 | 48,002 | 46,650 | 43,935 | 34,735 | −1,383 (−3,168, 402) | −18%* |
| rural | 1,582 | 1,528 | 1,234 | 1,491 | 1,288 | −57 (−377, 263) | −10% |
indicates statistical significance at P-value < 0.05.
Discussion
In 2020, a total of 199,617 glaucoma surgeries were performed, including cataract removal, among fellowship-trained glaucoma subspecialists for Medicare Fee-for-Service Part B beneficiaries; this represents a 31% decrease in surgical volume relative to the mean of the prior 4 years (mean 261,911, 2016–2019). In 2020, the percent change in total surgical volume between predicted and observed estimates in rural versus urban US areas for Medicare beneficiaries was −31% and −29%, respectively (p<0.05, p<0.05). MIGS experienced the greatest loss in volume in 2020; however, rural areas (−86%, p<0.05) were impacted more than urban areas (−75%, p<0.05). Goniotomy volumes portrayed similar findings with rural areas (−22%, p<0.05) experiencing a greater deficit relative to urban areas (−12%, p<0.05). Laser procedures were the only glaucoma surgery observed to decrease in urban areas (−18%, p<0.05) relative to rural areas (−10%, p>0.05). Interestingly, trabeculectomy performed in rural areas was the only surgical category exceeding predicted estimates (16%, p>0.05). Collectively, our findings demonstrate substantial variation in glaucoma surgical volumes during the COVID-19 pandemic. Identifying at-risk regions, such as RUCA-defined rural US regions, may aid glaucoma surgeons in alleviating disease burden secondary to the COVID-19 pandemic.1,14 The broad implication regarding the independent influence of geographical region on surgical volumes due to heightened prevalence of ophthalmic disease in rural or otherwise disadvantaged areas is a documented area of uncertainty.14,15 Prior studies determined that the lesser density of ophthalmologists in rural areas is not necessarily associated with greater surgical volumes.15 While many mechanisms exist to explain geographical variations, identifying specific areas with an unmet burden to “bridge the divide” remains an evolving, important area of medical practice.
The COVID-19 pandemic highlighted substantial challenges for the field of ophthalmology in terms of deferred care.1 Relative to most other medical specialties, such as psychiatry, neurology, and endocrinology, utilization of telemedicine, clinical volumes, and delivery of surgical care in ophthalmology declined significantly during 2020.1 While attempts were made to reduce this burden subsequent to COVID-19, it is imperative to further discriminate which US areas are preferentially impacted to aid in clinical efforts and policy advocacy. Within our analysis, RUCA-defined rural areas, relative to urban areas, experienced an additional 11% decrease in MIGS volume based on predicted estimates (rural −86%, p<0.05; urban −75%, p<0.05). Similarly, a 10% additional decrease in receipt of goniotomy was noted for rural areas versus urban areas (−22%, p<0.05; −12%, p<0.05). Laser volumes dropped more in urban areas than rural areas (percent change difference 8%). In contrast, trabeculectomies exceeded predicted estimates by 16% in rural areas. Paradoxically, the number of trabeculectomies performed in rural areas during the first year of the pandemic was greater than the prior year (2019). Collectivity, these findings indicate that while substantial reductions in nearly every surgical category occurred, glaucoma subspecialists demonstrated a relative preference for trabeculectomy in rural areas during the pandemic. This important observation is likely a compensatory approach to feasibly continue providing glaucoma care in the context of the COVID-19 pandemic.
While MIGS volume dropped in both rural and urban environments during 2020, the relatively greater declivity in rural areas may be expiated by historical trends. Since the widespread adoption of MIGS, specific US areas were observed to favor MIGS relative to other US areas.10 Between 2002 and 2008, the Northeast had the highest glaucoma surgery rate at 36.9 surgeries per 10,000 individuals; this finding is in tandem with the Northeast also possessing the strongest predilection for traditional glaucoma surgeries compared to MIGS.10 Interestingly, the highest MIGS rates were observed in South Dakota (95%), Wyoming (94%), and Oklahoma (94%), which are states containing vast rural areas.10 Indeed, our analysis supports this notion as rural areas, relative to urban areas, experienced a 24% greater increase in MIGS volume between 2016 and 2019. The “practice-style” hypothesis postulates clinical and surgical decision-making is dependent on individualized physician experience and judgment and partially elucidates why geographical variation in diagnostic and service patterns exist.9 In this context, it is possible that surgeons servicing rural areas utilize MIGS more frequently for reasons related to the level of subspecialization and ease of performance. Interpretation of these findings with recent reimbursement decisions by CMS Medicare should be exercised with caution.16 These rural US areas were likely affected as part of the broader decline in glaucoma surgery volume during the pandemic. Consequently, greater pre-pandemic MIGS rates in rural versus urban areas may be the reason for the significantly greater reduction in rural MIGS volume observed in our analysis.
The pre-pandemic approach to ophthalmologic practice may be challenged by an evolved, more efficient strategy due to mandatory remote placement of non-clinical/surgical staff, telecommuting from less expensive facilities, and other relevant efforts to maximize capacity through learned efficiency.17,18 Understanding potential clinical volume decreases associated with future public health emergencies may optimize the next ophthalmologic response. For example, if glaucoma surgical volume is expected to decrease by 35% for a 10-week stretch and glaucoma clinical volume by 50% for a 12-week stretch, then a tailored approach to anticipate and optimize this reduced demand can be considered.
By virtue of a 100% sample of Medicare Fee-for-Service Part B data, this analysis is strengthened via its reliance on a large sample that is otherwise representative of ophthalmic practice patterns in those aged 65 years and older. However, Medicare beneficiaries subscribed to Medicare Advantage Plans are not included in publicly available data and consist of approximately 46%of the entire Medicare population.19 The PUF does not contain individual patient demographic data nor clinical metrics of interest including intraocular pressures, prior surgical histories, nor medication/surgical outcomes. While Medicare payment data analyses are previously published,9,10ophthalmic analyses centered on exposing nuances associated with the RUCA classification system are limited in number. This analysis is also ecologically biased as nuanced service utilization patterns are likely revealed when exploring sub-RUCA schemas, including county level, zip-code level, state-level, and region-level classification systems. Future analyses may focus on multi-level modeling to ascertain sub-regional nuances in the world of glaucoma surgery pre-, post-, and during the COVID-19 pandemic. Also, the data used within our analysis does not allow timewise discrimination on a smaller interval than by calendar year; future studies assessing the pandemic’s influence may utilize data allowing for more tailored time frames such as between March 2020 to March 2021, which may more accurately reflect the start and end of the pandemic. The challenge to this kind of work is the relatively small number of procedures performed in more rural settings.
In conclusion, this nationally representative CMS Medicare analysis demonstrates the influence of the COVID-19 pandemic on surgical volume in urban versus rural areas in a fellowship-trained glaucoma subspecialist only cohort. Rural US areas, relative to urban areas, suffered a greater loss of procedural volumes by falling significantly short of predicted surgical volume estimates during the first year of the pandemic. Glaucoma surgeons may reconcile these findings with their surgical preferences in tandem with geographical locale of at-risk populations.
Acknowledgments
This was presented at the American Glaucoma Society Annual Meeting, 2023 in Austin, Texas.
Footnotes
Conflict of Interest: no conflicting relationship exists for any author.
References
- 1.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, et al. Variation In Telemedicine Use And Outpatient Care During The COVID-19 Pandemic In The United States. Health Aff (Millwood) 2021;40(2):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eyewire. Analysis: Ophthalmology Lost More Patient Volume Due to COVID-19 Than Any Other Specialty. [Strata Decision Technology web site; ]. May 11, 2020. Available at: https://eyewire.news/articles/analysis-55-percent-fewer-americans-sought-hospital-care-in-march-april-due-to-covid-19/?c4src=article:infinite-scroll. Accessed February 20, 2023. [Google Scholar]
- 3.Norbash AM, Moore AV Jr, Recht MP, et al. Early-Stage Radiology Volume Effects and Considerations with the Coronavirus Disease 2019 (COVID-19) Pandemic: Adaptations, Risks, and Lessons Learned. J Am Coll Radiol 2020;17(9):1086–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forte ML. Not Yet Available: Cheap Data for Nationally Representative Estimates: Commentary on an article by Heckmann Nathanael D., MD, et al. : “Elective Inpatient Total Joint Arthroplasty Case Volume in the United States in 2020. Effects of the COVID-19 Pandemic”. J Bone Joint Surg Am 2022;104(13):e59. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen TC, Thourani VH, Nissen AP, et al. The Effect of COVID-19 on Adult Cardiac Surgery in the United States in 717 103 Patients. Ann Thorac Surg 2022;113(3):738–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loizidou A, Tatla TS, Harvey I et al. COVID-VU – ENT-UK national survey of flexible nasendoscopy in the upper aerodigestive tract amidst the COVID-19 pandemic. BMC Health Serv Res 22, 625 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson JA, Lubek JE, Amin N, et al. Impact of the Novel Coronavirus 2019 (COVID-19) Pandemic on Head and Neck Cancer Care. Otolaryngol Head Neck Surg 2022;166(1):93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Aswad LA, Elgin CY, Patel V, et al. Real-Time Mobile Teleophthalmology for the Detection of Eye Disease in Minorities and Low Socioeconomics At-Risk Populations. Asia Pac J Ophthalmol (Phila) 2021;10(5):461–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cassard SD, Quigley HA, Gower EW et al. Regional variations and trends in the prevalence of diagnosed glaucoma in the Medicare population. Ophthalmology 2012;119(7):1342–1351. [DOI] [PubMed] [Google Scholar]
- 10.Ma AK, Lee JH, Warren JL, et al. GlaucoMap - Distribution of Glaucoma Surgical Procedures in the United States. Clin Ophthalmol 2020;14:2551–2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.. Centers for Medicare & Medicaid Services. [CMS website]. January 1, 2023. Available at: https://www.cms.gov February 20, 2023.
- 12.Health Resources & Services Administration. Federal Office of Rural Health Policy. [HRSA web site; ]. January 1, 2023. https://www.hrsa.gov/about/organization/bureaus/forhp. Accessed February 20, 2023. [Google Scholar]
- 13.Patel RA, Torabi SJ, Kayastha D, et al. Medicare Utilization and Reimbursement Variation Between Rural and Urban Otolaryngologists [published online ahead of print, 2022 Jul 19]. Otolaryngol Head Neck Surg 2022;1945998221113550. [DOI] [PubMed] [Google Scholar]
- 14.Assistant Secretary for Planning and Evaluation: Office of Health Policy. Medicare Beneficiaries’ use of Telehealth in 2020: Trends by Beneficiary Characteristics and Location. [HHS web site; ]. January 1, 2023. https://aspe.hhs.gov/sites/default/files/documents/a1d5d810fe3433e18b192be42dbf2351/medicare-telehealth-report.pdf. Accessed February 20, 2023. [Google Scholar]
- 15.Cai CX, Klawe J, Ahmad S, et al. Geographic variations in gender differences in cataract surgery volume among a national cohort of ophthalmologists. J Cataract Refract Surg 2022;48(9):1023–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ophthalmology Management. THE FUTURE OF MIGS. [Ophthalmology Management web site; ]. January 1, 2023. https://www.ophthalmologymanagement.com/issues/2022/march-2022/the-future-of-migs. Accessed February 20, 2023. [Google Scholar]
- 17.Davenport MS, Bruno MA, Iyer RS, et al. ACR Statement on Safe Resumption of Routine Radiology Care During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Am Coll Radiol 2020;17(7):839–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fan Q, Wang H, Kong W, et al. The Implications on Future Ophthalmic Care During and Post-COVID-19. Front Public Health 2021;9:653708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fierce Healthcare. MedPAC: Majority of Medicare beneficiaries to be on MA by 2023, but coding issues remain rampant. January 14, 2022. [MedPac web site]. Accessed February 20, 2023.