Abstract
Introduction
Acetaminophen and topical diclofenac (AtopD) have complementary mechanisms of action and are therefore candidates for combination use in osteoarthritis (OA) pain. However, an evidence gap exists on their combination use in OA pain. This study aimed to assess the effects of this combination and compare its performance relative to monotherapies on pain score reduction and opioid-sparing effect by leveraging evidence from acute pain setting using a model-based meta-analysis (MBMA).
Methods
A literature search was conducted using the MEDLINE database to identify randomized controlled trials (RCTs) studying the combination for acute pain. Subsequently, an MBMA of RCTs was implemented in conjunction with extrapolation principles to infer efficacy in the population of interest. Pain score reduction and opioid-sparing effect (OSE) were selected as the measures of efficacy.
Results
A total of 11 RCTs encompassing 1396 patients were included. Exploratory evaluation revealed AtopD combination to show greater pain score reduction versus acetaminophen monotherapy. However, pain score reduction was more susceptible to confounding by opioid patient-controlled analgesia (PCA) than OSE. Therefore, a parsimonious MBMA evaluating OSE was developed from 5 of the 11 RCTs (n = 353 patients). The analysis revealed a statistically significant interaction coefficient, suggesting a reduction of 32% in opioid use with the combination versus acetaminophen monotherapy. Differences in the effect size of the combination were less conclusive versus diclofenac monotherapy.
Conclusion
Our results indicate greater pain reduction and opioid-sparing efficacy for the AtopD combination versus acetaminophen monotherapy. Given the similar pain pathways and mechanisms of action of the two drugs in acute and mild-to-moderate OA pain, comparable beneficial effects from the combination therapy may be anticipated following extrapolation to chronic OA pain. Prospective RCTs and real-world studies in OA pain are needed to confirm the differences in the efficacy of the combination treatment observed in our study.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40122-023-00569-z.
Keywords: Acetaminophen, Diclofenac, Combination therapy, Model-based meta-analysis, Osteoarthritis, Acute pain
Key Summary Points
| Why carry out this study? |
| Effective management of mild-to-moderate osteoarthritis (OA) pain remains suboptimal despite the availability of several pharmacologic treatments. |
| Acetaminophen and topical diclofenac have complementary mechanisms of action and are therefore promising candidates for use in combination analgesia in OA pain; however, evidence on their efficacy in OA is lacking. |
| We conducted a model-based meta-analysis (MBMA) to infer the efficacy of the combination versus monotherapies by leveraging evidence from acute pain. |
| What was learned from this study? |
| Our study indicates greater pain reduction and opioid-sparing effect for the combination treatment versus acetaminophen monotherapy in acute pain. |
| Considering the similar pathogenesis in acute and mild-to-moderate OA pain, comparable treatment benefits may be expected with the use of the combination on extrapolation to OA pain. |
Introduction
Pain is an important health problem that causes substantial reduction in quality of life. Pain is categorized on the basis of clinical characteristics and underlying mechanisms into nociceptive pain (i.e., originating from tissue damage), neuropathic pain (i.e., resulting from nerve damage), and idiopathic pain, which has no identified cause. Understanding these differences is crucial when tailoring treatment to achieve optimal pain relief [1]. Osteoarthritis (OA) is a major cause of chronic pain and disability in older adults and currently affects more than 500 million people worldwide [2]. In the absence of a curative therapy, symptomatic drugs remain the mainstay for pain management in OA. However, acetaminophen provides inadequate relief and oral non-steroidal anti-inflammatory drugs (NSAIDs) are associated with significant gastrointestinal and cardiovascular adverse events, which limit their long-term use in the elderly [3, 4]. On the other hand, even though opioids are widely used in clinical practice if other analgesics provide insufficient pain relief or are contraindicated, their efficacy in OA is controversial. In addition, long-term opioid use is associated with serious risk of addiction and overdose deaths [5]. Therefore, an unmet need still exists for effective and well-tolerated treatments.
Mounting evidence suggests that when the pathophysiology of a medical condition is mediated by multiple pathways such as in OA pain, use of rational combinations of analgesic drugs acting through different mechanisms can provide effective pain relief at reduced individual doses while also minimizing side effects in the long term [6]. The combination of analgesics is also recommended by major clinical practice guidelines for pain, including the World Health Organization and the American College of Rheumatology [7].
Acetaminophen and topical diclofenac (AtopD) have complementary mechanism of action (MoA) and are therefore promising candidates for use in combination analgesia. Although acetaminophen MoA is not completely understood, prevailing evidence suggests it to mediate central analgesic effect by activating descending serotonergic pathways [8]. By contrast, diclofenac, a non-selective cyclooxygenase inhibitor, alters peripheral pain transmission pathways by its anti-inflammatory mechanisms [9–12]. Combining topical diclofenac with oral acetaminophen could also be a useful strategy to address the limitations of acetaminophen monotherapy, which has recently been shown to have insufficient efficacy as a single agent in the treatment of OA [13]. It may also be suitable for patients averse to oral NSAIDs as a result of comorbidities [4, 14]. Moreover, several clinical practice guidelines in OA recommend concomitant use of topical NSAIDs with acetaminophen in case of inadequate pain relief with acetaminophen monotherapy [15, 16]. Therefore, it can be hypothesized that the AtopD combination may show greater efficacy than either acetaminophen or topical diclofenac alone in the management of OA pain. However, while ample clinical evidence exists on the monotherapies of acetaminophen or topical diclofenac in OA pain, there is a gap in clinical evidence supporting their use as a combination therapy [17]. Consequently, further research is needed to assess the efficacy of the combination therapy in OA pain.
Model-based meta-analysis (MBMA) has become an increasingly important quantitative tool to inform drug development decisions and address clinical questions for which direct evidence is not available [18–20]. In the absence of individual patient-level data, MBMA allows not only direct and indirect comparison of drug treatments, like network meta-analysis, but also represents a robust regression-based technique for the evaluation of various clinical pharmacology questions, including dose–response, drug interaction, covariates effects, and/or endpoint bridging. MBMA is increasingly being used to determine overall treatment effect, a drug–drug combination effect, or an optimal dose compared against comparator drug in a specific disease or indication [18, 21–25]. It is one of the approaches available for the implementation of model-informed drug development (MIDD), a concept for evidence generation which has gained recognition across drug regulatory authorities [26–28].
It is also worth acknowledging that a high degree of overlap exists between acute and chronic pain states, both with regard to their chronology and pathophysiology [29, 30]. Moreover, various acute pain and mild-to-moderate OA pain are recognized as nociceptive in nature [31–34]. Given the gap in clinical evidence in OA pain, here we have attempted to leverage published summary-level data on the combination therapy in acute pain indications identified through literature search. Hence, this study aimed to assess the effects of AtopD combination and compare its performance relative to acetaminophen or topical diclofenac monotherapy on pain score reduction and opioid-sparing effect using an MBMA.
Methods
Literature Search and Data Extraction
A literature review was conducted to identify randomized controlled trials (RCTs) investigating the efficacy of AtopD combination in acute pain. The MEDLINE database was searched from inception up to April 2022 using the keywords—“acetaminophen”, “NSAIDs”, “diclofenac”, and “acute pain”—for RCTs published in English. In addition, the reference lists of all identified articles were searched by hand to identify cited articles not captured by electronic searches. The detailed search strategy is presented in Supplementary Table S1. All published RCTs evaluating the efficacy of acetaminophen with oral or topical diclofenac in acute pain were included for analysis (Supplementary Table S2).
Two independent researchers reviewed all abstracts and selected potentially eligible studies. Full texts of these studies were then retrieved and examined thoroughly for eligibility. A data collection form was prepared to extract all relevant information from the included studies. One reviewer was responsible for the extraction of the relevant information, whereas the second reviewer conducted random checks to review the quality of data extraction.
Endpoints
The endpoints of interest were pain score reduction on the numerical rating scale (NRS) or visual analog scale (VAS) and opioid-sparing effect (OSE), defined as a reduced opioid dose without loss of analgesic efficacy.
Statistical Analysis
Model Development
After an initial exploratory analysis, opioid-sparing effect was selected as the endpoint to be evaluated in the MBMA, as it showed a lower likelihood of bias than pain score reduction to assess the combined effect of acetaminophen and diclofenac versus either drug alone from RCTs allowing opioid patient-controlled analgesia (PCA). The opioid-sparing effect was modeled using the following MBMA structure, generally adopted for measures that are likely to follow a continuous Gaussian distribution [18, 21–23]:
| 1 |
where the consumption of opioids () within trial i and arm j is described as a function of (i) placebo response (), (ii) f(Drug,θ) characterizing the drug effect (for acetaminophen or diclofenac) using the fixed-effect model parameter (θ), and (iii) representing the residual error.
The residual (within-trial) variability, , was assumed to be normally distributed with a mean of 0 and variance , which represents the precision associated with each measurement. is the standard deviation of the outcome in the arm j of trial i for the endpoint and N is the associated sample size. Note that represents the standard error (SE) of the mean. In this model for between-trial variability, the trial-specific placebo response for the endpoint at primary time in trial () was described by an unstructured (or non-parametric) model considering the variability is determined by a substantial number of unexplained factors and thus likely to be highly non-Gaussian in distribution.
For the opioid-sparing effect of the combination of acetaminophen and diclofenac, an additive effect based on pharmacological principles for pharmacodynamic response was assumed, and an interaction term was used to account for non-additivity of both drugs.
The combination treatment effect was captured using the following structure:
| 2 |
where f(acetaminophen) and f(diclofenac) are the effect of each drug as monotherapy, and is the interaction coefficient. The parameter described non-additivity and characterized the type of interaction while also quantifying its magnitude. Estimates of γ not significantly different from 0 indicated that the combined effect was the sum of the two individual drug effects. However, negative values of γ indicated that the improvement, i.e., reduction in opioid dose or opioid use, was more than the sum of the two individual drug effects. In contrast, positive values of γ indicated a less than additive effect.
Model Evaluation
Candidate models were evaluated on the basis of the likelihood ratio test and maximum likelihood criteria [Akaike information criterion (AIC); statistical significance was achieved when p < 0.05], with observed response plotted against population- and trial-specific predictions as diagnostics for the assessment of the goodness-of-fit (e.g., precision, absence of bias). Forest plots were used to compare model predictions for each study arm with observed values along with their 95% confidence intervals (CI). Additionally, partial residual plots were used as graphical assessment to compare model predicted values with normalized observed values. This normalization was performed to ensure consistency between model prediction and the observed data. Confidence intervals for the expected treatment outcome were computed by resampling a total of 1000 sets of final MBMA model parameter estimates from the variance–covariance matrix of the final model. All analyses and simulations were conducted using generalized least squares regression function (gnls) provided in the nlme package in R (version 3.5.3 or higher, 64 bit running on Windows 10 Professional, SP1).
Compliance with Ethics Guidelines
The analysis in this article is based on previously conducted studies and does not involve any new studies with human participants or animal performed by any of the authors.
Results
Study Inclusion and Characteristics in Acute Pain
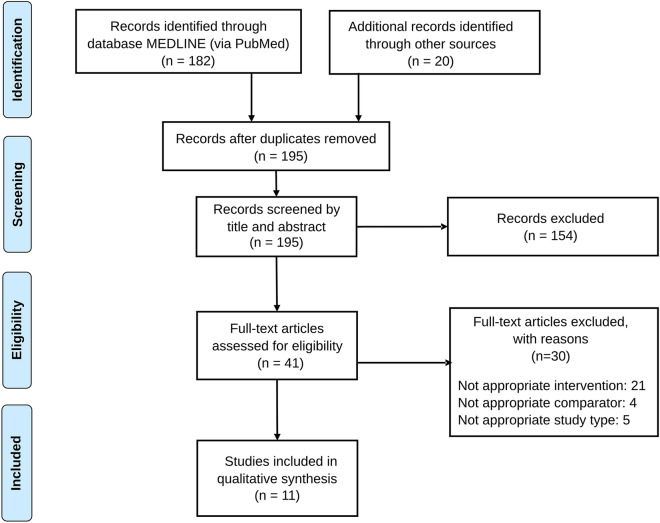
The literature review yielded 195 articles, 154 of which were excluded as they lacked relevant interventions or outcomes or population, or were non-clinical or observational studies, resulting in 41 articles assessed for eligibility by full review. Of these, 30 were excluded after full text review. Finally, a total of 11 RCTs investigating the effect of systemic acetaminophen and diclofenac combination in acute pain were selected for the evaluation of the effect of the combination (Fig. 1). Of the 11 studies that met the inclusion criteria, 10 were conducted in acute postoperative pain and a single study was conducted in acute musculoskeletal pain (Table 1).
Fig. 1.
Flowchart of the screening and selection process of RCTs on the combination of acetaminophen and diclofenac in acute pain setting
Table 1.
Characteristics of the studies on the combination of acetaminophen and diclofenac in acute pain
| Study | Population | Indication | Endpoint | No. of patients | Treatments | ROA | PCA | PCA unit |
|---|---|---|---|---|---|---|---|---|
| Matthews et al., 1984 [63] | Adults | Dental surgery | VAS | 27 |
ace 500 mg; ace 500 mg + dic 50 mg |
Oral | ND | NA |
| Montgomery et al., 1996 [64] | Women | Elective gynecological surgery | VAS | 59 |
ace 1500 mg; ace 1500 mg + dic 100 mg; dic 100 mg |
Rectal | Morphine | Mean mg |
| Breivik et al., 1999 [35] | Adults | Oral surgery | VAS | 72 |
ace 1000 mg; ace 1000 mg + dic 100 mg; dic 100 mg |
Oral | Codeine/paracetamol | % |
| Beck et al., 2000 [65] | Women | Hysterectomy pain | VAS | 65 |
ace 1200 mg; ace 1200 mg + dic 100 mg; ace 2400 mg |
Rectal | Morphine | Mean mg |
| Siddik et al., 2001 [61] | Women | Cesarean pain | VAS at rest | 80 |
ace 2000 mg; ace 2000 mg + dic 100 mg; dic 100 mg; placebo 0 mg |
Intravenous; rectal | Morphine | Mean mg |
| Hiller et al., 2004 [66] | Adults | Tonsillectomy | VAS (0–3) | 71 |
ace 2000 mg; ace 2000 mg + dic 75 mg; dic 75 mg |
Intravenous | Oxycodone | Mean mg |
| Woo et al., 2005 [67] | Adults | Musculoskeletal injury | VAS at rest | 229 |
ace 1000 mg; ace 1000 mg + dic 25 mg; dic 25 mg |
Oral | No | NA |
| Munishankar et al., 2008 [68] | Women | Cesarean pain | VAS at rest | 78 |
ace 1000 mg; ace 1000 mg + dic 100 mg; dic 100 mg |
Oral | Morphine | Mean mg |
| Riad et al., 2007 [69] | Children | Postoperative pain | Pain rating scale (0–5) | 108 |
ace 880 mg; ace 908 mg + dic 22.7 mg; dic 23.7 mg |
Rectal | Morphine | Mean mg |
| Hannam et al., 2014 [36] | Children | Postoperative pain | VAS | 496 |
ace NA mg; ace NA mg + dic NA mg; dic NA mg |
Oral/rectal; oral | No | NA |
| Elzaki et al., 2016 [70] | Adults | Post-endodontic pain | NRS | 111 |
ace 1000 mg; ace 1000 mg + dic 50 mg; placebo 0 mg |
Oral | Ibuprofen | Mean mg |
ROA route of administration, PCA patient-controlled analgesia, ND no data, NA not applicable, VAS visual analog scale, NRS numerical rating scale, ace acetaminophen, dic diclofenac
Exploratory Analysis
As revealed from an exploratory analysis of the data, 8 out of the 11 RCTs showed beneficial effect of the combination for pain score reduction in comparison to acetaminophen monotherapy. On the other hand, 5 out of the 11 RCTs showed beneficial effect of the combination versus diclofenac monotherapy (Supplementary Fig. S1). However, only two studies reported statistically significant differences in the efficacy of the combination for the management of acute pain versus acetaminophen or diclofenac monotherapy [35, 36]. Due to high heterogeneity in the pain scale and/or pain score definition used across the studies, the ratio of observed mean pain score reduction with acetaminophen and diclofenac combination compared to either drug alone was used to demonstrate the magnitude of the combination effect (Supplementary Table S3). Nevertheless, no consistent beneficial effect was observed for the combination treatment on pain score reduction, compared to either drug alone, particularly for studies allowing subjects to use opioids as PCA. In this context, use of opioid-sparing effect was found to show a lower likelihood of bias than pain score reduction to assess the combined effect of acetaminophen and diclofenac (> 1 ratio) versus either drug alone (Supplementary Fig. S2).
Model Development and Assessment of Opioid-Sparing Effect
A parsimonious MBMA model was developed on the basis of five eligible studies in acute pain reporting mean opioid PCA consumption (in mg) to quantify the opioid-sparing effect of the combination (Table 2 and Supplementary Fig. S3). Supplementary Table S4 presents the key steps involved in model development. The final model showed adequate performance in predicting opioid use across most study arms (Supplementary Fig. S4). Acetaminophen and diclofenac monotherapies were modeled independently initially before introducing the combination therapy data in the analysis. The effect of the combination was characterized using an interaction term as described in Eq. (2) in the “Methods” section. The model was able to show a statistically significant interaction coefficient accounting for non-additivity between both drugs on opioid-sparing effect (Table 3). The positive γ value indicated that the beneficial opioid-sparing effect of the combination was less than the sum of the two individual drug effects.
Table 2.
Characteristics of the studies considered for the analysis of opioid-sparing effect in acute pain
| Study | Population | Indication | No. of subjects | Opioid PCA | Reported PCA unit | Included in the final analysis |
|---|---|---|---|---|---|---|
| Montgomery et al., 1996 [64] | Women | Elective gynecological surgery | 59 | Morphine | mg | Yes |
| Breivik et al., 1999 [35]a | Adults | Oral surgery | 72 | Codeine/paracetamol | % | No |
| Beck et al., 2000 [65] | Women | Hysterectomy pain | 65 | Morphine | mg | Yes |
| Siddik et al., 2001 [61] | Women | Cesarean pain | 80 | Morphine | %/mg | Yes |
| Hiller et al., 2004 [66] | Adults | Tonsillectomy | 71 | Oxycodone | %/mg | Yes |
| Munishankar et al., 2008 [68] | Women | Cesarean pain | 78 | Morphine | mg | Yes |
| Riad et al., 2007 [69]b | Children | Postoperative pain | 108 | Morphine | mg | No |
PCA patient-controlled analgesia
aExcluded as only a limited % of subjects used PCA in each treatment arm
bExcluded as the population comprised children
Table 3.
Estimated parameters from the parsimonious model of opioid-sparing effect
| Parameter | Parameter description | Estimate [95% CI] | RSE % | Absolute (mg) |
|---|---|---|---|---|
| e.ace | Drug effect of acetaminophen | − 18.9 [− 31.4 to − 6.43] | 29% | − 18.9 |
| e.dic | Drug effect of diclofenac | − 28.4 [− 40.7 to − 16.2] | 19% | − 28.4 |
| γ* | Interaction between acetaminophen and diclofenac | 0.025 [0.0148 to 0.0353] | 18% |
A γ of 0 indicates that the combined effect was the sum of the two individual drug effects. A positive γ indicates that the resulting opioid-sparing effect was less than the sum of the effects of the two individual drugs, while a negative γ indicates a more than additive effect
ace acetaminophen, dic diclofenac, RSE residual standard error
The resulting placebo-adjusted opioid-sparing effect (mean and 95% CI) is presented in Fig. 2 and Supplementary Table S5. The final model predicted about 32% less opioid use with the combination than acetaminophen monotherapy based on the mean point estimate. However, the beneficial effect of the combination was less pronounced vs. diclofenac monotherapy. Due to limited number of studies, no further analysis was performed to differentiate opioid PCA use based on the type of surgical intervention (for instance, opioid PCA use was generally lower for tonsillectomy pain than pain after gynecological surgery).
Fig. 2.
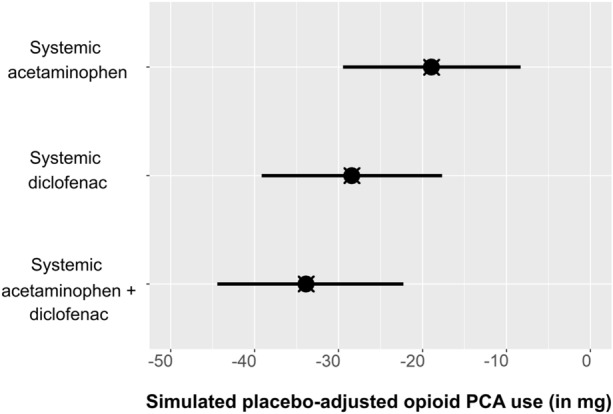
Simulated placebo-adjusted opioid PCA use (in mg) for acetaminophen and diclofenac monotherapies and their combination assuming a typical placebo response (64.7 mg). Symbols indicate maximum likelihood model predictions and error bars represent 95% CI of resampling parameter estimates from the final model variance–covariance matrix 1000 times. PCA patient-controlled analgesia, CI confidence interval
Discussion
Pain in osteoarthritis is a complex phenomenon that encompasses both inflammatory and non-inflammatory pain signaling pathways at peripheral and central levels of the nervous system [37, 38]. Thus, it is not surprising that no single drug provides adequate pain relief while demonstrating optimal risk–benefit ratio in the long term. Consequently, successful approaches may require targeting several pathways at the same time [39, 40]. In this context, combination therapy of AtopD can be a promising strategy to achieve effective analgesia with an adequate safety profile considering that, at the recommended therapeutic doses, both drugs are devoid of any major risk of serious adverse events in the subset of the population most prone to OA.
Acetaminophen, included in the World Health Organization’s List of Essential Medicines, is one of the most widely used analgesic and antipyretic medications globally owing to its high tolerability profile when compared with other analgesics, particularly in high-risk populations such as adults with comorbidities [41, 42]. It was historically the first-line pain medication for OA [43] before a few recent publications reported doubts over its efficacy in OA pain [3]. Although acetaminophen rarely causes adverse effects in healthy individuals when used episodically at ≤ 4 g/day, doses exceeding the recommended daily maximum can result in liver toxicity [42]. Topical NSAIDs, including diclofenac, have become valuable treatment options for the OA population, to whom oral NSAIDs are contraindicated [44]. Topical NSAIDs have shown comparable efficacy to oral NSAIDs but exhibit better safety profile due to their considerably lower systemic exposure. Therefore, they are nowadays recommended as first-line medication by most OA clinical practice guidelines before resorting to oral NSAIDs. The most common adverse effects of topical NSAIDs are local site reactions [45].
A multi-mechanistic therapeutic approach has greater potential to provide optimal analgesia in OA which involves multiple pain pathways [6]. Acetaminophen plus topical diclofenac is a rational combination that is based on the complementary pharmacodynamics (i.e., different mechanisms of action) of the two drugs. In general, both drugs act by suppressing nociceptive signaling via inhibition of cyclooxygenase (COX), an enzyme involved in the conversion of arachidonic acid to prostaglandins, which mediate inflammation and pain. However, each drug acts via a slightly different mechanism. While topical diclofenac acts peripherally to inhibit prostaglandin synthesis at the site of nociception, acetaminophen inhibits prostaglandin synthesis mainly in the central nervous system [46, 47]. As a result, the combination might work by blocking pain transmission at peripheral and central nervous system and thus provide greater analgesia than each drug alone [47].
Although the combination treatment is commonly used, i.e., with more than one-quarter of patients using topical NSAIDs with oral non-opioid analgesics such as acetaminophen in real-world settings [48], there is limited literature available on the combination of acetaminophen and topical NSAIDs [17]. Only one RCT of 4-week duration was found that showed significantly greater pain reduction with the combination versus acetaminophen or placebo [49]. Moreover, a qualitative systematic review focused on pain intensity scores and supplemental analgesic requirements in acute postoperative pain in adults showed the combination of acetaminophen and NSAIDs to be more effective than acetaminophen or NSAIDs alone in more than 60% of studies [50]. In addition, a pharmacokinetic–pharmacodynamic study in children with acute postoperative pain also found combination treatment with lower doses of acetaminophen and diclofenac to provide comparable analgesia to monotherapies [36]. Furthermore, several previous studies have investigated the effect of combining oral NSAIDs and acetaminophen in OA and have shown the combinations provide additional pain-relieving activity, thereby leading to a dose-sparing effect and improved safety versus monotherapies [51–53]. These findings seem to support the recommendations of several prominent OA clinical guidelines, which endorse the use of topical NSAIDs concomitantly with acetaminophen [15, 16]. However, there are no previous studies on the AtopD combination in OA pain. Our study represents therefore an attempt to integrate existing data and extrapolate findings from acute to chronic pain.
While a trend for beneficial effect was observed for the combination on pain score reduction compared to either drug alone, the combination effect was confounded by use of opioid PCA in the studies. Our MBMA of RCTs identified in acute postoperative pain revealed further reduction of opioid use in studies allowing PCA with the combination treatment versus acetaminophen monotherapy. Despite several reports showing opioids to exhibit minimal efficacy in chronic OA pain [54, 55], opioid prescribing in clinical practice continues unabated [56]. In this context, the beneficial potential of the combination therapy to reduce opioid consumption by 32% vs. acetaminophen monotherapy cannot be underemphasized when considering the substantial health risks of adverse outcomes associated with opioid usage, including the development of opioid use disorder (dependency and addiction), overdose fatalities, respiratory depression, falls, and their negative effects on gastrointestinal (nausea, constipation), endocrine, immune, and nervous systems (dizziness, somnolence, and fatigue) [57]. In addition, opioid use is associated with significantly greater structural damage and faster progression of degenerative changes when compared with controls. In fact, opioid users also exhibited significantly greater pain, worse symptoms, and lower quality of life than controls, which suggests inadequate pain control by opioids [58].
Whilst our findings indicate that combination therapy has a greater opioid-sparing effect when compared with diclofenac monotherapy, the beneficial effect was lesser in magnitude when compared with acetaminophen. This finding is in agreement with a previous clinical study which reported the combination of paracetamol and ibuprofen to exhibit significant efficacy vs. acetaminophen but not against ibuprofen monotherapy in chronic knee pain [53].
To our knowledge, this is the first MBMA to evaluate and synthesize clinical evidence on the efficacy of the combination of acetaminophen and topical diclofenac in acute pain. Inferences from the results are made on the basis of extrapolation principles, which suggest the potential therapeutic value of the combined use of these two commonly recommended analgesics in mild-to-moderate OA pain. Furthermore, extrapolation of the findings appears to be supported by clinical practice. The majority of trials in OA pain, which included topical or oral diclofenac in one of their treatment arms, allowed acetaminophen as rescue therapy [59, 60], suggesting that the combination is generally perceived to be beneficial and well tolerated.
Adding topical diclofenac to acetaminophen could also be a potential approach to mitigate safety concerns with acetaminophen by allowing its use at lower dosages. Eventually, it could also delay the progression to oral NSAIDs and opioids in clinical settings. Undoubtedly, insights from this MBMA open the door for a potential treatment option for the ever-increasing aging population suffering from OA, especially those who have cardiovascular and gastrointestinal comorbidities and hence may not transition to stronger analgesics such as oral NSAIDs and opioids.
We acknowledge the limitation of our analysis, which is based on summary-level data only. In this regard, it was not possible to fully assess the combination effect. We also recognize the implications of the restricted inclusion criteria, based on studies having acetaminophen or diclofenac in one of their treatment arms. Inclusion of studies on other NSAIDs could have provided further insight into the anti-inflammatory effect and possibly helped in understanding whether the observed differences are a class effect. From a technical perspective, it should be noted that the combination effect was estimated by adding treatment effect onto the non-parametric placebo response. As there was only one placebo-controlled trial to inform placebo response on the opioid-sparing effect in acute pain [61], this may have introduced some degree of estimation bias. This limitation may be further compounded by the few studies available, and relatively small sample size. Consequently, we cannot rule out the impact of study-level variation on model precision, as suggested by the wide range of simulated confidence intervals. From a clinical perspective, the severity of acute pain caused by different types of surgery should not be overlooked, as it may drive large variation in the consumption of opioids (e.g., cesarean pain required higher dose of PCA vs. tonsillectomy). This effect could not be fully accounted for in the current parsimonious model because of the limited number of clinical studies. Lastly, our analysis might be subject to publication bias. However, considering acetaminophen and diclofenac have a long history of use, we believe that the chance of publication bias is low.
Conclusions
Available data from published RCTs suggest that the combination of acetaminophen and diclofenac yields greater pain reduction and opioid-sparing effect versus acetaminophen monotherapy in acute pain treatment. On the basis of our findings, a beneficial effect for the combination can be expected in the treatment of mild-to-moderate OA pain considering the pharmacologically complementary mechanism of action of the two drugs and considerable overlap in the pathophysiology of acute and chronic inflammatory pain. In conclusion, additional evidence from RCTs is urgently needed to investigate the efficacy of combination therapy in comparison to monotherapies in mild-to-moderate OA pain. Such studies should be complemented by research based on biomarkers and quantitative systems pharmacology [62], which could be used to evaluate the clinical significance of pharmacodynamic interactions between the drugs and to further optimize combination regimens and as well as define doses, inclusion criteria, and endpoints to be evaluated in prospective clinical trials.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our gratitude for Aneta Gomulka-Pilat, Joanna Jarosz, Paulina Pierzchala from Certara evidence & access at Krakow for literature data support. We thank the participants of the original studies upon which this analysis is based.
Author Contributions
Design and analysis: Vidhu Sethi, Li Qin, Eugène Cox, Oscar Della Pasqua. Initial drafting of manuscript: Vidhu Sethi, Li Qin, Oscar Della Pasqua, Iñaki F. Trocóniz. Critical review and revision: All authors. Approval of final draft for submission: All authors.
Funding
The study and the Rapid Service fee were funded by Haleon (formerly GSK Consumer Healthcare).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Disclosures
Vidhu Sethi: employee and shareholder of Haleon. Oscar Della Pasqua: employee and shareholder of GlaxoSmithKline. Li Qin: employee and shareholder of Certara. Eugène Cox: former employee and shareholder of Certara; current employee of University Leiden, the Netherlands. Iñaki F. Trocóniz: No competing interests to disclose.
Ethical Approval
The analysis in this article is based on previously conducted studies and does not involve any new studies with human participants or animal performed by any of the authors.
Footnotes
The original online version of this article was revised to include the ORCID and correct the affiliation details for author Oscar Della Pasqua.
Change history
2/19/2024
The original online version of this article was revised to include the ORCID and correct the affiliation details for author Oscar Della Pasqua.
References
- 1.Thakur M, Dickenson AH, Baron R. Osteoarthritis pain: nociceptive or neuropathic? Nat Rev Rheumatol. 2014;10(6):374–380. doi: 10.1038/nrrheum.2014.47. [DOI] [PubMed] [Google Scholar]
- 2.Long H, Liu Q, Yin H, et al. Prevalence trends of site-specific osteoarthritis from 1990 to 2019: findings from the global burden of disease study 2019. Arthritis Rheumatol. 2022;74(7):1172–1183. doi: 10.1002/art.42089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leopoldino AO, Machado GC, Ferreira PH, et al. Paracetamol versus placebo for knee and hip osteoarthritis. Cochrane Database Syst Rev. 2019;2(2):Cd013273. doi: 10.1002/14651858.CD013273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper C, Chapurlat R, Al-Daghri N, et al. Safety of oral non-selective non-steroidal anti-inflammatory drugs in osteoarthritis: what does the literature say? Drugs Aging. 2019;36(Suppl 1):15–24. doi: 10.1007/s40266-019-00660-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deveza LA, Hunter DJ, Van Spil WE. Too much opioid, too much harm. Osteoarthr Cartilage. 2018;26(3):293–295. doi: 10.1016/j.joca.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Altman RD. Pain relief in osteoarthritis: the rationale for combination therapy. J Rheumatol. 2004;31(1):5–7. [PubMed] [Google Scholar]
- 7.Paladini A, Varrassi G. Multimodal pharmacological analgesia in pain management. In: Waisundara VY, Banjari I, Balkić J, editors. Pain management-practices, novel therapies and bioactives. London: IntechOpen; 2020. [Google Scholar]
- 8.Anderson BJ. Paracetamol (acetaminophen): mechanisms of action. Paediatr Anaesth. 2008;18(10):915–921. doi: 10.1111/j.1460-9592.2008.02764.x. [DOI] [PubMed] [Google Scholar]
- 9.Shah S, Mehta V. Controversies and advances in non-steroidal anti-inflammatory drug (NSAID) analgesia in chronic pain management. Postgrad Med J. 2012;88(1036):73–78. doi: 10.1136/postgradmedj-2011-130291. [DOI] [PubMed] [Google Scholar]
- 10.Brewer AR, McCarberg B, Argoff CE. Update on the use of topical NSAIDs for the treatment of soft tissue and musculoskeletal pain: a review of recent data and current treatment options. Phys Sportsmed. 2010;38(2):62–70. doi: 10.3810/psm.2010.06.1784. [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence (NICE). Osteoarthritis in over 16s: diagnosis and management, Guideline No. NG226. 2022. https://www.nice.org.uk/guidance/ng226/resources/osteoarthritis-in-over-16s-diagnosis-and-management-pdf-66143839026373. Accessed 4 May 2023. [PubMed]
- 12.Bruyere O, Honvo G, Veronese N, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) Semin Arthritis Rheum. 2019;49(3):337–350. doi: 10.1016/j.semarthrit.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Bannuru R, Dasi U, McAlindon T. 558 Reassessing the role of acetaminophen in osteoarthritis: systematic review and meta-analysis. Osteoarthr Cartilage. 2010;18:S250. doi: 10.1016/S1063-4584(10)60585-7. [DOI] [Google Scholar]
- 14.McCarberg B, Tenzer P. Complexities in the pharmacologic management of osteoarthritis pain. Curr Med Res Opin. 2013;29(5):539–548. doi: 10.1185/03007995.2013.785391. [DOI] [PubMed] [Google Scholar]
- 15.Bruyère O, Cooper C, Pelletier JP, et al. An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally: a report from a task force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) Semin Arthritis Rheum. 2014;44(3):253–263. doi: 10.1016/j.semarthrit.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 16.Geenen R, Overman CL, Christensen R, et al. EULAR recommendations for the health professional's approach to pain management in inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77(6):797–807. doi: 10.1136/annrheumdis-2017-212662. [DOI] [PubMed] [Google Scholar]
- 17.Bell J, Sethi V, Siddiqui K, Conaghan PG. AB0808 combination of oral paracetamol and topical NSAIDs for osteoarthritis pain: a systematic scoping review of the literature. New Jersey: BMJ; 2019. [Google Scholar]
- 18.Mandema JW, Cox E, Alderman J. Therapeutic benefit of eletriptan compared to sumatriptan for the acute relief of migraine pain—results of a model-based meta-analysis that accounts for encapsulation. Cephalalgia. 2005;25(9):715–725. doi: 10.1111/j.1468-2982.2004.00939.x. [DOI] [PubMed] [Google Scholar]
- 19.D'Agate S, Wilson T, Adalig B, et al. Model-based meta-analysis of individual international prostate symptom score trajectories in patients with benign prostatic hyperplasia with moderate or severe symptoms. Br J Clin Pharmacol. 2020;86(8):1585–1599. doi: 10.1111/bcp.14268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D'Agate S, Chavan C, Manyak M, et al. Model-based meta-analysis of the time to first acute urinary retention or benign prostatic hyperplasia-related surgery in patients with moderate or severe symptoms. Br J Clin Pharmacol. 2021;87(7):2777–2789. doi: 10.1111/bcp.14682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mandema JW, Gibbs M, Boyd RA, Wada DR, Pfister M. Model-based meta-analysis for comparative efficacy and safety: application in drug development and beyond. Clin Pharmacol Ther. 2011;90(6):766–769. doi: 10.1038/clpt.2011.242. [DOI] [PubMed] [Google Scholar]
- 22.Maringwa J, Sardu ML, Hang Y, et al. Characterizing effects of antidiabetic drugs on heart rate, systolic and diastolic blood pressure. Clin Pharmacol Ther. 2021;109(6):1583–1592. doi: 10.1002/cpt.2130. [DOI] [PubMed] [Google Scholar]
- 23.Qin L, Zhang N, Ishigami J, et al. Dyskalemia risk associated with fixed-dose anti-hypertensive medication combinations. J Hum Hypertens. 2022;36(11):989–995. doi: 10.1038/s41371-021-00600-w. [DOI] [PubMed] [Google Scholar]
- 24.Witjes H, Khatri A, Diderichsen PM, Mandema J, Othman AA. Meta-analyses of clinical efficacy of risankizumab and adalimumab in chronic plaque psoriasis: supporting evidence of risankizumab superiority. Clin Pharmacol Ther. 2020;107(2):435–442. doi: 10.1002/cpt.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan P, Peskov K, Song X. Applications of model-based meta-analysis in drug development. Pharm Res. 2022;39(8):1761–1777. doi: 10.1007/s11095-022-03201-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marshall S, Madabushi R, Manolis E, et al. Model-informed drug discovery and development: current industry good practice and regulatory expectations and future perspectives. CPT Pharmacometr Syst Pharmacol. 2019;8(2):87–96. doi: 10.1002/psp4.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madabushi R, Seo P, Zhao L, Tegenge M, Zhu H. Review: Role of model-informed drug development approaches in the lifecycle of drug development and regulatory decision-making. Pharm Res. 2022;39(8):1669–1680. doi: 10.1007/s11095-022-03288-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Food and Drug Administration. Meta-analyses of randomized controlled clinical trials to evaluate the safety of human drugs or biological products guidance for industry. US Department of Health and Human Services. 2018. https://www.fda.gov/media/117976/download. Accessed 4 May 2023.
- 29.McCormick T, Frampton CJA, Medicine IC. Assessment of acute and chronic pain. Anaesth Intens Care Med. 2019;20(8):405–409. doi: 10.1016/j.mpaic.2019.05.010. [DOI] [Google Scholar]
- 30.Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–2097. doi: 10.1016/S0140-6736(21)00393-7. [DOI] [PubMed] [Google Scholar]
- 31.Wu X, Wei X, Jiang L, Cai J, Ju M, Zheng X. Is lidocaine patch beneficial for postoperative pain: a meta-analysis of randomized clinical trials. Clin J Pain. 2023;39(9):484–490. doi: 10.1097/AJP.0000000000001135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matsutani N, Kawamura M. Successful management of postoperative pain with pregabalin after thoracotomy. Surg Today. 2014;44(4):712–715. doi: 10.1007/s00595-013-0743-x. [DOI] [PubMed] [Google Scholar]
- 33.European Medicines Agency. Guideline on the clinical development of medicinal products intended for the treatment of pain. 2017. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-development-medicinal-products-intended-treatment-pain-first-version_en.pdf. Accessed 4 May 2023.
- 34.Cazzola M, Atzeni F, Boccassini L, Cassisi G, Sarzi-Puttini P. Physiopathology of pain in rheumatology. Reumatismo. 2014;66(1):4–13. doi: 10.4081/reumatismo.2014.758. [DOI] [PubMed] [Google Scholar]
- 35.Breivik EK, Barkvoll P, Skovlund E. Combining diclofenac with acetaminophen or acetaminophen-codeine after oral surgery: a randomized, double-blind single-dose study. Clin Pharmacol Ther. 1999;66(6):625–635. doi: 10.1016/S0009-9236(99)90073-5. [DOI] [PubMed] [Google Scholar]
- 36.Hannam JA, Anderson BJ, Mahadevan M, Holford NH. Postoperative analgesia using diclofenac and acetaminophen in children. Paediatr Anaesth. 2014;24(9):953–961. doi: 10.1111/pan.12422. [DOI] [PubMed] [Google Scholar]
- 37.Perrot S. Osteoarthritis pain. Best Pract Res Clin Rheumatol. 2015;29(1):90–97. doi: 10.1016/j.berh.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 38.Salaffi F, Ciapetti A, Carotti M. The sources of pain in osteoarthritis: a pathophysiological review. Reumatismo. 2014;66(1):57–71. doi: 10.4081/reumatismo.2014.766. [DOI] [PubMed] [Google Scholar]
- 39.Raffa RB, Clark-Vetri R, Tallarida RJ, Wertheimer AI. Combination strategies for pain management. Expert Opin Pharmacother. 2003;4(10):1697–1708. doi: 10.1517/14656566.4.10.1697. [DOI] [PubMed] [Google Scholar]
- 40.van Laar M, Pergolizzi JV, Jr, Mellinghoff HU, et al. Pain treatment in arthritis-related pain: beyond NSAIDs. Open Rheumatol J. 2012;6:320–330. doi: 10.2174/1874312901206010320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Conaghan PG, Arden N, Avouac B, Migliore A, Rizzoli R. Safety of paracetamol in osteoarthritis: what does the literature say? Drugs Aging. 2019;36(Suppl 1):7–14. doi: 10.1007/s40266-019-00658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alchin J, Dhar A, Siddiqui K, Christo PJ. Why paracetamol (acetaminophen) is a suitable first choice for treating mild to moderate acute pain in adults with liver, kidney or cardiovascular disease, gastrointestinal disorders, asthma, or who are older. Curr Med Res Opin. 2022;38(5):811–825. doi: 10.1080/03007995.2022.2049551. [DOI] [PubMed] [Google Scholar]
- 43.Majeed MH, Sherazi SAA, Bacon D, Bajwa ZH. Pharmacological treatment of pain in osteoarthritis: a descriptive review. Curr Rheumatol Rep. 2018;20(12):88. doi: 10.1007/s11926-018-0794-5. [DOI] [PubMed] [Google Scholar]
- 44.Honvo G, Leclercq V, Geerinck A, et al. Safety of topical non-steroidal anti-inflammatory drugs in osteoarthritis: outcomes of a systematic review and meta-analysis. Drugs Aging. 2019;36(Suppl 1):45–64. doi: 10.1007/s40266-019-00661-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rannou F, Pelletier JP, Martel-Pelletier J. Efficacy and safety of topical NSAIDs in the management of osteoarthritis: evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(4 Suppl):S18–21. doi: 10.1016/j.semarthrit.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 46.D'Arcy Y, Mantyh P, Yaksh T, et al. Treating osteoarthritis pain: mechanisms of action of acetaminophen, nonsteroidal anti-inflammatory drugs, opioids, and nerve growth factor antibodies. Postgrad Med. 2021;133(8):879–894. doi: 10.1080/00325481.2021.1949199. [DOI] [PubMed] [Google Scholar]
- 47.Altman RD. A rationale for combining acetaminophen and NSAIDs for mild-to-moderate pain. Clin Exp Rheumatol. 2004;22(1):110–117. [PubMed] [Google Scholar]
- 48.Jackson H, Barnett LA, Jordan KP, et al. Patterns of routine primary care for osteoarthritis in the UK: a cross-sectional electronic health records study. BMJ Open. 2017;7(12):e019694. doi: 10.1136/bmjopen-2017-019694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yoo BCS, Lee MS, Moon HB. Treatment of knee osteoarthritis with ketoprofen (Ketotop): a double-blind placebo-controlled randomized trial. J Korean Rheum Assoc. 1996;3(1):70–75. [Google Scholar]
- 50.Ong CK, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110(4):1170–1179. doi: 10.1213/ANE.0b013e3181cf9281. [DOI] [PubMed] [Google Scholar]
- 51.Murphy JE, Donald JF, Layes MA. Analgesic efficacy and acceptability of fenoprofen combined with paracetamol and compared with dihydrocodeine tartrate in general practice. J Int Med Res. 1978;6(5):375–380. doi: 10.1177/030006057800600504. [DOI] [PubMed] [Google Scholar]
- 52.Seideman P, Samuelson P, Neander G. Naproxen and paracetamol compared with naproxen only in coxarthrosis. Increased effect of the combination in 18 patients. Acta Orthop Scand. 1993;64(3):285–288. doi: 10.3109/17453679308993626. [DOI] [PubMed] [Google Scholar]
- 53.Doherty M, Hawkey C, Goulder M, et al. A randomised controlled trial of ibuprofen, paracetamol or a combination tablet of ibuprofen/paracetamol in community-derived people with knee pain. Ann Rheum Dis. 2011;70(9):1534–1541. doi: 10.1136/ard.2011.154047. [DOI] [PubMed] [Google Scholar]
- 54.Welsch P, Petzke F, Klose P, Häuser W. Opioids for chronic osteoarthritis pain: an updated systematic review and meta-analysis of efficacy, tolerability and safety in randomized placebo-controlled studies of at least 4 weeks double-blind duration. Eur J Pain. 2020;24(4):685–703. doi: 10.1002/ejp.1522. [DOI] [PubMed] [Google Scholar]
- 55.Osani MC, Lohmander LS, Bannuru RR. Is there any role for opioids in the management of knee and hip osteoarthritis? A systematic review and meta-analysis. Arthritis Care Res (Hoboken) 2021;73(10):1413–1424. doi: 10.1002/acr.24363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thorlund JB, Turkiewicz A, Prieto-Alhambra D, Englund M. Opioid use in knee or hip osteoarthritis: a region-wide population-based cohort study. Osteoarthr Cartilage. 2019;27(6):871–877. doi: 10.1016/j.joca.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 57.Gewandter JS, Smith SM, Dworkin RH, et al. Research approaches for evaluating opioid sparing in clinical trials of acute and chronic pain treatments: initiative on methods, measurement, and pain assessment in clinical trials recommendations. Pain. 2021;162(11):2669–2681. doi: 10.1097/j.pain.0000000000002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bodden J, Joseph GB, Schirò S, et al. Opioid users show worse baseline knee osteoarthritis and faster progression of degenerative changes: a retrospective case–control study based on data from the osteoarthritis initiative (OAI) Arthritis Res Ther. 2021;23(1):146. doi: 10.1186/s13075-021-02524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Courtney P, Doherty M. Key questions concerning paracetamol and NSAIDs for osteoarthritis. Ann Rheum Dis. 2002;61(9):767–773. doi: 10.1136/ard.61.9.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stewart M, Cibere J, Sayre EC, Kopec JA. Efficacy of commonly prescribed analgesics in the management of osteoarthritis: a systematic review and meta-analysis. Rheumatol Int. 2018;38(11):1985–1997. doi: 10.1007/s00296-018-4132-z. [DOI] [PubMed] [Google Scholar]
- 61.Siddik SM, Aouad MT, Jalbout MI, Rizk LB, Kamar GH, Baraka AS. Diclofenac and/or propacetamol for postoperative pain management after cesarean delivery in patients receiving patient controlled analgesia morphine. Reg Anesth Pain Med. 2001;26(4):310–315. doi: 10.1053/rapm.2001.21828. [DOI] [PubMed] [Google Scholar]
- 62.Taneja A, Oosterholt SP, Danhof M, Della PO. Biomarker exposure-response relationships as the basis for rational dose selection: lessons from a simulation exercise using a selective COX-2 inhibitor. J Clin Pharmacol. 2016;56(5):609–621. doi: 10.1002/jcph.629. [DOI] [PubMed] [Google Scholar]
- 63.Matthews RW, Scully CM, Levers BG. The efficacy of diclofenac sodium (Voltarol) with and without paracetamol in the control of post-surgical dental pain. Br Dent J. 1984;157(10):357–359. doi: 10.1038/sj.bdj.4805486. [DOI] [PubMed] [Google Scholar]
- 64.Montgomery JE, Sutherland CJ, Kestin IG, Sneyd JR. Morphine consumption in patients receiving rectal paracetamol and diclofenac alone and in combination. Br J Anaesth. 1996;77(4):445–447. doi: 10.1093/bja/77.4.445. [DOI] [PubMed] [Google Scholar]
- 65.Beck DH, Schenk MR, Hagemann K, Doepfmer UR, Kox WJ. The pharmacokinetics and analgesic efficacy of larger dose rectal acetaminophen (40 mg/kg) in adults: a double-blinded, randomized study. Anesth Analg. 2000;90(2):431–436. doi: 10.1213/00000539-200002000-00035. [DOI] [PubMed] [Google Scholar]
- 66.Hiller A, Silvanto M, Savolainen S, Tarkkila P. Propacetamol and diclofenac alone and in combination for analgesia after elective tonsillectomy. Acta Anaesthesiol Scand. 2004;48(9):1185–1189. doi: 10.1111/j.1399-6576.2004.00473.x. [DOI] [PubMed] [Google Scholar]
- 67.Woo WW, Man SY, Lam PK, Rainer TH. Randomized double-blind trial comparing oral paracetamol and oral nonsteroidal antiinflammatory drugs for treating pain after musculoskeletal injury. Ann Emerg Med. 2005;46(4):352–361. doi: 10.1016/j.annemergmed.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 68.Munishankar B, Fettes P, Moore C, McLeod GA. A double-blind randomised controlled trial of paracetamol, diclofenac or the combination for pain relief after caesarean section. Int J Obstet Anesth. 2008;17(1):9–14. doi: 10.1016/j.ijoa.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 69.Riad W, Moussa A. Pre-operative analgesia with rectal diclofenac and/or paracetamol in children undergoing inguinal hernia repair. Anaesthesia. 2007;62(12):1241–1245. doi: 10.1111/j.1365-2044.2007.05248.x. [DOI] [PubMed] [Google Scholar]
- 70.Elzaki WM, Abubakr NH, Ziada HM, Ibrahim YE. Double-blind randomized placebo-controlled clinical trial of efficiency of nonsteroidal anti-inflammatory drugs in the control of post-endodontic pain. J Endod. 2016;42(6):835–842. doi: 10.1016/j.joen.2016.02.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.