Abstract
Introduction
Sinuvertebral nerve overactivation is one of the mechanisms of neck pain caused by cervical disc herniation. Radiofrequency ablation (RFA) of sinuvertebral nerves has shown efficacy for the treatment of discogenic low back pain. However, relatively few studies evaluated the efficacy of RFA of sinuvertebral nerves for the treatment of chronic neck pain caused by cervical disc herniation.
Methods
Clinical data were retrospectively collected from 168 patients diagnosed with cervical disc herniated neck pain from January 1, 2019, to September 1, 2022, who were treated with computed tomography (CT)-guided cervical disc RFA of at the Pain Medicine Center of Zhejiang Provincial People’s Hospital. A 22-G RFA needle (Inomed, Emmendingen, Germany) was inserted between the carotid artery and trachea to the intervertebral disc under the direction of CT the scanner. Depending on the position of the protruding nucleus pulposus or the rupture of the annulus fibrosus, the needle was inserted into the posterior side of the intervertebral disc until the tip of the needle reached the target position. The numeric rating scale (NRS) score, pain relief and appearance of complications after RFA were evaluated.
Results
A total of 168 patients underwent CT-guided RFA for cervical disc herniation. The average duration of pain was 67.07 ± 70.42 months. At 6 months of follow-up, the median preoperative NRS score decreased significantly from preoperative 5.41 ± 1.08 to postoperative 1.341 ± 1.25 at 1 month, 1.4 ± 1.38 at 3 months and 1.72 ± 1.41 at 6 months after RFA (p < 0.01). The numbers of patients with ≥ 50% of their neck pain relieved were 84% (141/168), 87% (147/168), 87% (147/168) and 79% (133/168) at 1 day, 1 month, 3 months and 6 months after RFA, respectively. No serious complications related to treatment or long-term complications were observed.
Conclusions
This study highlights that CT-guided RFA targeting the edge of cervical disc herniation to destroy the sinuvertebral nerves can effectively relieve neck pain, and the computed tomography (CT)-guided RFA treatment strategy has the advantages of having few complications.
Keywords: Radiofrequency ablation, Sinuvertebral nerve, Chronic neck pain, Cervical disc herniation
Key Summary Points
| Why carry out this study? |
| Chronic neck pain has clinical manifestations of pain in the head, neck, shoulder and upper limbs as well as pain associated with numbness |
| Neck pain seriously affects physical and mental health as well as quality of life of patients and increases health care costs |
| The purpose of this study was to evaluate pain relief and the occurrence of complications of CT-guided radiofrequency ablation (RFA) targeting the edge of herniation of the cervical disc to destroy the sinuvertebral nerves for the treatment of cervical pain |
| What was learned from the study? |
| This study highlights that CT-guided RFA targeting the edge of cervical disc herniation to destroy the sinuvertebral nerves can effectively relieve neck pain |
| The overactivation of sinuvertebral nerves is one of the mechanisms of neck pain caused by herniated cervical disc. RFA of sinuvertebral nerves has shown efficacy for the treatment of discogenic low back pain |
Introduction
Neck pain is a chronic pain with clinical manifestations of pain in the head, neck, shoulder and upper limbs as well as pain associated with numbness [1–4]. Neck pain seriously affects physical and mental health as well as the quality of life of patients of and increase health care costs [5–8]. Chronic neck pain leads to functional abnormalities in sensorimotor processing, emotion, cognition and memory. Neck pain has a global prevalence of 3551 people and 352 years lived with disability per 100,000 people [9]. Cervical intervertebral disc herniation is one of the most common causes of neck pain [10–14].
Despite such a high prevalence, the relationship between cervical disc herniation and clinical pain and neuropathology is still unclear. Previous studies have shown that neck pain and low back pain induced by disc herniation may be due to stimulation of the sinuvertebral nerves located on the posterolateral edge of intervertebral discs, which produces aseptic inflammation within the annulus of degenerative discs and induced pain [15–19].
Radiofrequency ablation (RFA) is an interventional therapy for the treatment of specific pain syndromes. There are studies that have evaluated the RFA of the sinuvertebral nerve for the treatment of low back pain with good effect; however, due to surgery-related anatomic limitations and the risk of thermal injury associated with the technique to the cervical nerve root [18, 20], few studies have evaluated the RFA of the sinuvertebral nerve for the treatment of neck pain.
In the present study, we retrospectively analyzed the efficacy and safety of a new approach of computed tomography (CT)-guided RFA of the herniated edge of cervical discs to destroy the sinuvertebral nerve for the treatment of neck pain without radiculopathy.
Methods
Study Participants
This study was approved and waived the requirement for informed consent by the Ethics Committee of the Zhejiang Provincial People’s Hospital. This study was designed as a retrospective clinical trial conducted from January 1, 2019, to September 30, 2022. The electronic medical records of patients treated with CT-guided cervical disc RFA at the Pain Medicine Center of Zhejiang Provincial People’s Hospital were reviewed. Patients were included only when they met all the following criteria: (1) chronic axial or referred neck pain; (2) cervical magnetic resonance imaging showed mild cervical disc herniation consistent with patient symptoms; (3) failure of conservative treatments; (4) underwent magnetic resonance imaging (MRI) of the brain prior to treatment. Patients who had: (1) pain intensity (numeric rating scale [NRS] score) was < 4; (2) with radiculopathy, spinal cord compression and/or myelopathy; (3) duration of the pain was < 6 months; (4) previous cervical spine surgery at the same cervical level was excluded in this study.
All included patients were discussed before surgery by senior pain physicians who considered neck pain caused by cervical disc herniation. Consent was obtained from all patients.
Surgical Procedures
The procedures were performed by two senior pain physicians (Shun Li and Bin Ru).
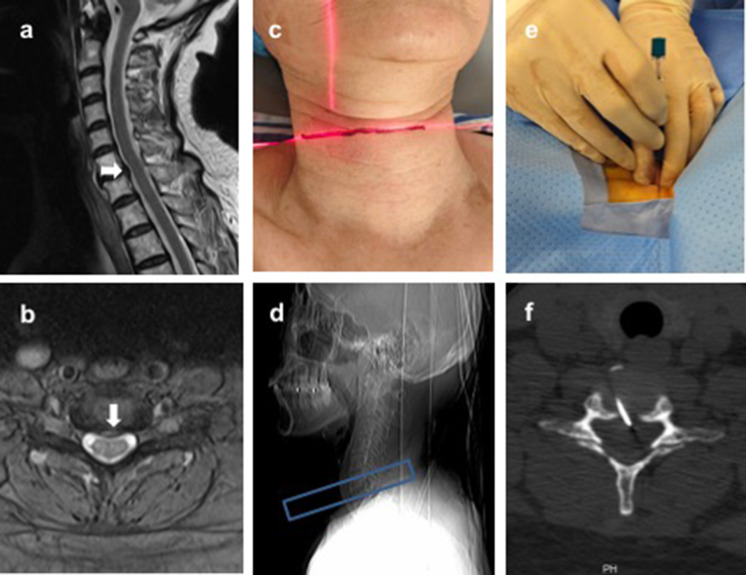
The enrolled patients underwent preoperative cervical spine MRI examinations. Based on symptoms and MRI results, senior pain physicians determined on which disc to operate. When the patient’s MRI showed that there was only a single plane of disc herniation, we only performed radiofrequency ablation of the intervertebral disc of the corresponding plane; however, when the patient’s MRI showed a multiplane disc herniation, we performed a sensory test on this herniated disc, and when the sensory test could induce the patient’s usual symptoms, we performed radiofrequency ablation of the intervertebral disc of that plane. The patients were placed in the supine position on the CT gantry table. A wide piece of tape was applied to secure the head to prevent head movement during the operation. Heart and respiratory rate, three-lead electrocardiography and fingertip digital oximetry were monitored throughout the surgical procedure. The sagittal CT image was used to locate the target position (Fig. 1a). The axial CT image was used to determine the puncture approach (Fig. 1b). After identifying the target point (Fig. 1c, d), the carotid arteries and trachea were pushed to the sides to avoid injury, and then the skin and subcutaneous soft tissue were locally anesthetized with 0.5 ml of 1% lidocaine (Tiancheng Co., Hebei, China). A 22-G RFA needle (Inomed, Emmendingen, Germany) was then inserted between the carotid artery and the trachea to the intervertebral disc (Fig. 1e). After puncture of the intervertebral disc, the position of the needle tip was checked again on the axial CT image. Next, depending on the position of the protruding nucleus pulposus or the rupture of the annulus fibrosus, we proceeded to insert the needle into the posterior side of the intervertebral disc until the tip of the needle reached the target position (Fig. 1f). The schematic diagram of RFA is shown in Fig. 2.
Fig. 1.
Radiofrequency ablation (RFA) of cervical intervertebral discs guided by computed tomography (CT). a, b Magnetic resonance imaging before RFA surgery showed mild central cervical disc herniation (white arrow) at C6–7. c, d CT scanner guidance was used to locate the target plane for cervical puncture. Blue box, scanning area. e After the surgeon has pushed the carotid artery and trachea to the sides, the radiofrequency needle is inserted into the intervertebral disc. f Under the guidance of CT, the radiofrequency needle reaches the position of the intervertebral disc herniation
Fig. 2.
Scheme illustration of radiofrequency ablation (RFA) for cervical intervertebral disc herniation target. a Sagittal view; b Axial view
The RFA procedure was performed using the R-2000B radiofrequency lesion generator (Beiqi, Beijing, China). Sensory tests were performed at 50 Hz and < 1.5 V before applying RFA. If preoperative pain or tingling occurred under simulation, called a positive sensory test, and there was no simultaneous abnormal sensation in the extremities, the placement of the needle tip was considered appropriate and safe. After the sensory test, motor stimulation was performed at 2 Hz and up to 2 V. If there was no abnormal response in the limbs, called a negative motor test, it indicated that there was still a safe distance between the tip of the needle and the cervical spinal cord, which reconfirmed that the tip was in a safe position. Patients with positive sensory test and negative motor test received temperature step-up RFA at 50 °C, 60 °C, 70 °C and 80 °C for 15 s followed by RFA for 180 s at 85 °C. If the patient reported any discomfort during the RFA process, the physician immediately stopped the operation and reconfirmed the position of the needle tip by CT scanner.
The treating physician visited in person 2 h after surgery, the interventional radiology nurse followed up by phone 3–4 days after the RFA surgery, and the treating physician followed up in person or by phone from 1 day to 6 months.
Outcome Analysis
The primary outcome included the mean difference in baseline pain intensity levels at 1 day, 1, 3 and 6 months after RFA treatment measured using an 11-point NRS. Pain relief rate was measured during 6 months of follow-up to assess functional status. Complications such as bleeding, paresthesia, and infection were recorded.
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS), version 23 (INM Corp., Armonk, NY, USA).
Before statistical analysis, the Kolmogorov-Smirnov test was used to determine the normality of the data distribution. Continuous data following a normal distribution are expressed as mean ± standard deviation (SD) and were compared between groups using an independent t-test. Nonnormally distributed data were described by median (interquartile range [IQR]). Descriptive statistics are shown as mean, SD, median and interquartile range, or numbers. To detect a statistically significant change in the value of the NRS score value in the posttreatment period compared to the pretreatment period, we used the Wilcoxon signed rank test. A two-tailed p < 0.05 was considered statistically significant.
Results
Patient Characteristics
From January 2019 to September 2022, a total of 213 patients were treated with CT-guided cervical disc RFA at Zhejiang People’s Hospital. Twelve patients had a previous cervical spine surgical history, five patients with a neck pain duration < 6 months, six patients with baseline NRS scores < 4, and five patients with radiculopathy, spinal cord compression or myelopathy, and two patients with intracranial space-occupying lesions were excluded from this study. Therefore, 183 patients with chronic neck pain caused by cervical disc herniation underwent RFA treatment for cervical disc herniation targets under the guidance of CT. However, 15 patients were subsequently excluded from this study because of loss to follow-up. Finally, 168 patients remained in this study for analysis (Fig. 3; Table 1).
Fig. 3.
Flow diagram of patients in this study. NRS numeric rating scale, RFA radiofrequency ablation
Table 1.
Demographics and characteristics of the included patients
| Variable | Value |
|---|---|
| Number of patients | 168 |
| Age [years, mean (SD)] | 51.92 (10.81) |
| Gender (male/female), n (%) | 49 (29)/119 (71) |
| Medical records, n (%) | |
| Migraine | 17 (10) |
| Hypertension | 39 (23) |
| Hyperlipidemia | 3 (2) |
| Osteoporosis | 10 (6) |
| Diabetes mellitus | 21 (12) |
| Neck pain duration (months) | 66.55 (66.73) |
| Location of pain | |
| Neck | 12 (7) |
| Neck base shoulder top | 101 (59) |
| Neck and head | 29 (17) |
| Neck, shoulder and head | 29 (17) |
| Previous conservative treatment, (%) | |
| Analgesics, n (%) | 152 (90) |
| Physiotherapy, n (%) | 72 (43) |
| Intervention, n (%) | 15 (9) |
| Duration of operation [mean (SD)] | 50.83 (10.2) |
SD standard deviation
Pre- and Postoperative NRS Scores
The mean preoperative NRS score was 6 (4, 6), and the median NRS scores (IQR) were 2 (1, 3), 1 (0, 2), 1 (0, 2) and 1 (1, 3) at 1 day, 1 month, 3 months and 6 months after RFA surgery treatment (Table 2). The NRS score within 6 months after RFA was significantly lower than before RFA surgery (p < 0.001) (Table 2, Fig. 4). Most patients experienced significant relief from neck pain after RFA treatment. In particular, according to the pain relief evaluation, the pain relief rate was 84% (141/168), 87% (147/168), 87% (147/168), and 79% (133/168) at 1 day, 1, 3 and 6 months after RFA treatment, respectively (Table 2).
Table 2.
Evaluation of pain relief in patients with neck pain caused by cervical disc herniation after RFA treatment
| Pre RFA (baseline) | 1 day after RFA | 1 month after RFA | 3 months after RFA | 6 months after RFA | p | |
|---|---|---|---|---|---|---|
| NRS scores, median (IQR) | 6 (4, 6) | 2 (1, 3) | 1 (0, 2) | 1 (0, 2) | 1 (1, 3) | < 0.001 |
| Pain relief after RFA | ||||||
| < 50% | 27 (16) | 21 (13) | 21 (13) | 35 (21) | ||
| ≥ 50% | 141 (84) | 147 (87) | 147 (87) | 133 (79) | ||
| = 100% | 27 (16) | 50 (30) | 51 (30) | 37 (22) | ||
IQR interquartile range, NRS numeric rating scale, RFA radiofrequency ablation
Fig. 4.
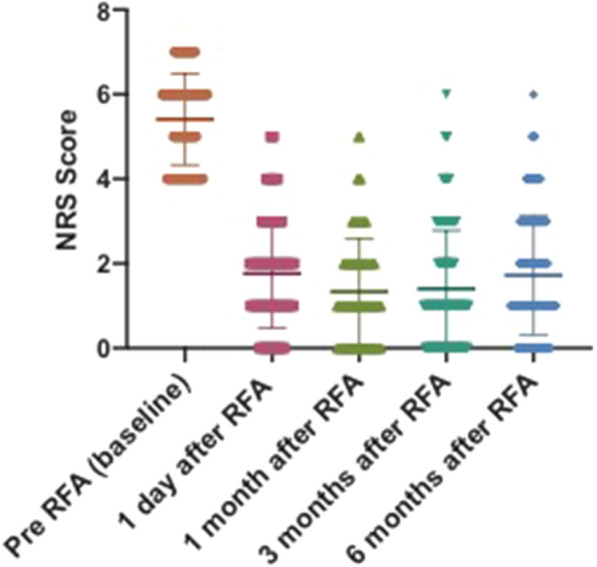
Numeric rating scale (NRS) scores of patients at varying time intervals as indicated. RFA: radiofrequency ablation
Complications
A total of 18 patients reported soreness at the needle insertion site, but this disappeared 2 weeks after surgery, suggesting that it was not associated with nerve root injury. This complication may be due to repeated punctures for the RFA operations. In the present study, there were no serious complications related to RFA treatment, such as bleeding, paresthesias or infection, in this study.
Discussion
In the present study, we observed the excellent therapeutic efficacy of CT-guided cervical disc RFA for the treatment of neck pain induced by cervical disc herniation, suggesting that method may be a promising treatment. To our knowledge, this is the first report of CT-guided RFA therapy for cervical disc herniation aimed at relieving neck pain by destroying sinuvertebral nerves, and the results showed that this treatment strategy is promising. Although the study was retrospective, the inclusion of > 160 patients makes the results even more convincing.
Cervical disc herniation is one of the most common causes of neck pain [21]. Current clinical treatment includes conservative treatment (medication and physical therapy), epidural injections (interlaminar or transforaminal), minimally invasive techniques and classical surgery (anterior cervical surgery, cervical disc replacement, anterior cervical fusion surgery or artificial cervical intervertebral disc replacement). In most cases, nonoperative treatment is effective. However, some patients do not respond to conservative treatment. For patients with cervical disc herniation, minimally invasive techniques are the preferred choice to reduce risk and reduce hospital stay. Intervertebral discectomy under intervertebral foramen endoscope is widely used for the treatment of patients with cervical disc herniation complicated with radiculopathy, spinal cord compression and/or myelopathy by removing the source of spinal cord compression, resulting in rapid relief of symptoms of axial neck pain and radiculopathy or myelopathy simultaneously. Although for most patients, the intervertebral foramen endoscope strategy is safe and effective, it can induce complications such as scar adhesion and decreased vertebral stability in the long term due to disc destruction and spine structure.
For patients with mild cervical intervertebral disc herniation, the intervertebral foramen endoscope is not the first choice. Many efforts have been made to develop more minimally invasive surgery. Cervical percutaneous discectomy by chemonucleolysis is one of the effective percutaneous disc treatments that aims to partially dissolve the nucleus pulposus, decrease intradiscal pressure and induce disc shrinkage with the advantages of shorter hospitalization, less tissue disruption, less risk, less or no postoperative adhesions, no skin scar, no risk of instability and shorter recovery period. However, chymopapain may induce an anaphylactic reaction [13], and pure ethanol had a short-lived effect with rapid leakage [22].
Cervical discs receive innervation posteriorly from sinuvertebral nerves, laterally from the vertebral nerve and anteriorly from sympathetic trunks [16, 23].
According to anatomy textbooks, the sinuvertebral nerve arises bilaterally from the ventral ramus of each spinal nerve just distal to the dorsal root ganglia, supplying both proprioceptive and nociceptive fibers. It is formed by the union of a somatic root from the ventral ramus and an autonomic root provided by the gray ramus (A). The sinuvertebral nerve takes a recurrent course and reenters the spinal canal through the intervertebral foramen. Kojima et al. reported that the nerve divides into superficial and deep networks around the longitudinal posterior ligament, providing sensation to the posterior annulus [24]. In healthy patients, the sinuvertebral nerves are located in the three outer layers of the annulus fibrosus, penetrating about 3 mm through the anulus [25, 26]. However, in degenerative discs, sinuvertebral nerves penetrate into the inner one third layer of the annulus fibrosus, even the nucleus pulposus [1, 27]. Sinuvertebral nerves have been found to be associated with discogenic low back pain in most previous research [18, 19]. In recent years, researchers have found that sinuvertebral nerves were associated with cervicogenic headaches [28, 29].
RFA, known as radiofrequency ablation, was first described by Kirschner in the early 1930s with thermocoagulation of the Gasserian ganglion for the treatment of trigeminal neuralgia [30]. The continuous radiofrequency current created a focal thermal lesion in a neural pathway with the goal of interrupting nociception. RFA has been widely applied for the treatment of specific pain syndromes. For example, Lord et al. demonstrated that percutaneous radiofrequency neurotomy could be used successfully for chronic cervical zygapophyseal joint pain [31]. RFA is also used for the treatment of back pain induced by degenerative disc disease. Kim et al. reported that RFA of the sinuvertebral nerves relieved paravertebral muscle spasms in patients with chronic discogenic back pain.
Compared to interventions for lumbar back pain treatment, neck pain treatment is challenging because of surgically related anatomic limitations and the risk of technique-associated thermal injury to the cervical nerve root [18, 20]. With the development of the image, CT guidance provides a clear review of the vessels and intervertebral discs, allowing for precise and safe positioning of a needle tip during the RFA procedure. The application of CT-guided interventional therapy for the treatment of neck pain induced by cervical disc degeneration has been widely accepted. However, few studies have evaluated the pain relief and complications of CT-guided RFA by targeting sinuvertebral nerves for the treatment of neck pain induced by cervical disc herniation.
Complications such as nerve root injury during the procedure were the major concern regarding its application at the cervical level. In the present study, none of the patients showed signs of nerve root injury symptoms during or after RFA treatment. A total of 18 patients reported soreness at the needle insertion site, but it disappeared 2 weeks postoperatively, suggesting that it is not associated with nerve root injury. Some limitations of the study need to be acknowledged. First, we only followed up all patients for a 6-month postoperative period, so we cannot claim that the technique was effective at relieving this kind of pain for a much longer period. Second, although the NRS score pain rating system was widely used as a gauge, we cannot eliminate the subjective preference of patients for their own pain ratings.
Conclusions
In summary, CT-guided RFA targeting the edge of the herniated cervical disc to destroy the sinuvertebral nerves can effectively relieve neck pain, and the CT-guided RFA treatment strategy has the advantages of having few complications. However, due to the limitations of this study, multicenter, prospective and randomized controlled trials are necessary to confirm these results.
Acknowledgments
Medical Writing/Editorial Assistance
Nannan Zhang completed to the writing of the manuscript under the guidance of Bin Ru. During the writing of this manuscript, American Journal Experts (AJE; part of Springer Nature) was used to edit the language of this manuscript. The authors funded the AJE service.
Author Contributions
BR and SL brought forward the subject of this study and guided the writing; NZ, JH, WC and WL were significant contributors to data acquisition and manuscript writing. All authors read and approved the final manuscript.
Funding
The study was supported by the Natural Science Foundation of Zhejiang Province (LQ23H300009, LQ22H090015, 2021ZA010 and LGD22H07004), the Department of Education of Zhejiang Province (Y202044330). The Rapid Service Fee was funded by the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
Nannan Zhang, Jiaqi Hu, Wenjun Cai, Wenlong Liu, Shun Li and Bin Ru have declared that no competing interest exists.
Ethical Approval
This study was approved, and the requirement for informed consent was waived by the Ethics Committee of Zhejiang Provincial People’s Hospital.
Footnotes
Nannan Zhang and Jiaqi Hu contributed equally to this work.
Contributor Information
Shun Li, Email: 13732208930@163.com.
Bin Ru, Email: 1148449287@qq.com.
References
- 1.Peng B, DePalma MJ. Cervical disc degeneration and neck pain. J Pain Res. 2018;11:2853–2857. doi: 10.2147/JPR.S180018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015;90(2):284–299. doi: 10.1016/j.mayocp.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 3.García-Cosamalón J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? J Anat. 2010;217(1):1–15. doi: 10.1111/j.1469-7580.2010.01227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henschke N, Kamper SJ, Maher CG. The epidemiology and economic consequences of pain. Mayo Clin Proc. 2015;90(1):139–147. doi: 10.1016/j.mayocp.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 5.Manchikanti L, Pampati V, Parr Iii A, et al. Cervical interlaminar epidural injections in the treatment of cervical disc herniation, post surgery syndrome, or discogenic pain: cost utility analysis from randomized trials. Pain Physician. 2019;22(5):421–431. doi: 10.36076/ppj/2019.22.421. [DOI] [PubMed] [Google Scholar]
- 6.Cohen SP, Hooten WM. Advances in the diagnosis and management of neck pain. BMJ. 2017;358:j3221. doi: 10.1136/bmj.j3221. [DOI] [PubMed] [Google Scholar]
- 7.Prablek M, Gadot R, Xu DS, Ropper AE. Neck pain: differential diagnosis and management. Neurol Clin. 2023;41(1):77–85. doi: 10.1016/j.ncl.2022.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Cabrera-Martos I, Rodríguez-Torres J, López-López L, Prados-Román E, Granados-Santiago M, Valenza MC. Effects of an active intervention based on myofascial release and neurodynamics in patients with chronic neck pain: a randomized controlled trial. Physiother Theory Pract. 2022;38(9):1145–1152. doi: 10.1080/09593985.2020.1821418. [DOI] [PubMed] [Google Scholar]
- 9.Safiri S, Kolahi AA, Hoy D, et al. Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ. 2020;368:m791. doi: 10.1136/bmj.m791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eloqayli H. Cervical discogenic pain treatment with percutaneous jellified ethanol: preliminary experience. Biomed Res Int. 2019;2019:2193436. doi: 10.1155/2019/2193436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujimoto K, Miyagi M, Ishikawa T, et al. Sensory and autonomic innervation of the cervical intervertebral disc in rats: the pathomechanics of chronic discogenic neck pain. Spine (Phila Pa 1976) 2012;37(16):1357–1362. doi: 10.1097/BRS.0b013e31824ba710. [DOI] [PubMed] [Google Scholar]
- 12.Bogduk N. The anatomy and pathophysiology of neck pain. Phys Med Rehabil Clin N Am. 2011;22(3):367–vii. doi: 10.1016/j.pmr.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Sayhan H, Beyaz SG, Ülgen AM, Yuce MF, Tomak Y. Long-term clinical effects of DiscoGel for cervical disc herniation. Pain Physician. 2018;21(1):E71–E78. [PubMed] [Google Scholar]
- 14.Yang L, Yang C, Pang X, et al. Mechanoreceptors in diseased cervical intervertebral disc and vertigo. Spine (Phila Pa 1976) 2017;42(8):540–546. doi: 10.1097/BRS.0000000000001801. [DOI] [PubMed] [Google Scholar]
- 15.Ohtori S, Miyagi M, Inoue G. Sensory nerve ingrowth, cytokines, and instability of discogenic low back pain: a review. Spine Surg Relat Res. 2018;2(1):11–17. doi: 10.22603/ssrr.2016-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shayota B, Wong TL, Fru D, et al. A comprehensive review of the sinuvertebral nerve with clinical applications. Anat Cell Biol. 2019;52(2):128–133. doi: 10.5115/acb.2019.52.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shimohata K, Hasegawa K, Onodera O, Nishizawa M, Shimohata T. The clinical features, risk factors, and surgical treatment of cervicogenic headache in patients with cervical spine disorders requiring surgery. Headache. 2017;57(7):1109–1117. doi: 10.1111/head.13123. [DOI] [PubMed] [Google Scholar]
- 18.Kim JY, Kim HS, Wu PH, Jang IT. Alleviating paravertebral muscle spasm after radiofrequency ablation treatment of hypersensitive basivertebral and sinuvertebral nerves for chronic discogenic back pain. Pain Physician. 2021;24(6):E883–E892. doi: 10.36076/ppj.2021.24.E883. [DOI] [PubMed] [Google Scholar]
- 19.Quinones S, Konschake M, Aguilar LL, et al. Clinical anatomy of the lumbar sinuvertebral nerve with regard to discogenic low back pain and review of literature [published correction appears in Eur Spine J. 2021 Aug;30(8):2409] Eur Spine J. 2021;30(10):2999–3008. doi: 10.1007/s00586-021-06886-1. [DOI] [PubMed] [Google Scholar]
- 20.Kim HS, Wu PH, Jang IT. Lumbar degenerative disease part 1: anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: a prospective case series and review of literature. Int J Mol Sci. 2020;21(4):1483. doi: 10.3390/ijms21041483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oh CH, Kim DY, Ji GY, et al. Cervical arthroplasty for moderate to severe disc degeneration: clinical and radiological assessments after a minimum follow-up of 18 months—Pfirrmann grade and cervical arthroplasty. Yonsei Med J. 2014;55(4):1072–1079. doi: 10.3349/ymj.2014.55.4.1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stagni S, de Santis F, Cirillo L, et al. A minimally invasive treatment for lumbar disc herniation: DiscoGel® chemonucleolysis in patients unresponsive to chemonucleolysis with oxygen-ozone. Interv Neuroradiol. 2012;18(1):97–104. doi: 10.1177/159101991201800113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang G, Zhang Z, Liu J, Cheng L. Comparison of the effect of diagnosing discogenic low back pain by sinuvertebral nerve block versus discoblock a retrospective cohort study. Eur Spine J. 2023;32(6):2093–2100. doi: 10.1007/s00586-023-07732-2. [DOI] [PubMed] [Google Scholar]
- 24.Kojima Y, Maeda T, Arai R, Shichikawa K. Nerve supply to the posterior longitudinal ligament and the intervertebral disc of the rat vertebral column as studied by acetylcholinesterase histochemistry. II. Regional differences in the distribution of the nerve fibres and their origins. J Anat. 1990;169:247–255. [PMC free article] [PubMed] [Google Scholar]
- 25.Kim HS, Wu PH, Jang IT. Narrative review of pathophysiology and endoscopic management of basivertebral and sinuvertebral neuropathy for chronic back pain. J Korean Neurosurg Soc. 2023;66(4):344–355. doi: 10.3340/jkns.2022.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edgar MA. The nerve supply of the lumbar intervertebral disc [published correction appears in J Bone Jt Surg Br. 2008 Apr;90(4):543] J Bone Jt Surg Br. 2007;89(9):1135–1139. doi: 10.1302/0301-620X.89B9.18939. [DOI] [PubMed] [Google Scholar]
- 27.Peng B, Wu W, Hou S, Li P, Zhang C, Yang Y. The pathogenesis of discogenic low back pain. J Bone Jt Surg Br. 2005;87(1):62–67. doi: 10.1302/0301-620X.87B1.15708. [DOI] [PubMed] [Google Scholar]
- 28.Hu JQ, Zhang J, Ru B, et al. Computed tomography-guided radiofrequency ablation of cervical intervertebral discs for the treatment of refractory cervicogenic headache: a retrospective chart review. Headache. 2022;62(7):839–847. doi: 10.1111/head.14361. [DOI] [PubMed] [Google Scholar]
- 29.Slipman CW, Lipetz JS, Jackson HB, Plastaras CT, Vresilovic EJ. Outcomes of therapeutic selective nerve root blocks for whiplash induced cervical radicular pain. Pain Physician. 2001;4(2):167–174. doi: 10.36076/ppj.2001/4/167. [DOI] [PubMed] [Google Scholar]
- 30.Grandhi RK, Kaye AD, Abd-Elsayed A. Systematic review of radiofrequency ablation and pulsed radiofrequency for management of cervicogenic headaches. Curr Pain Headache Rep. 2018;22(3):18. doi: 10.1007/s11916-018-0673-9. [DOI] [PubMed] [Google Scholar]
- 31.Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996;335(23):1721–1726. doi: 10.1056/NEJM199612053352302. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.