Abstract
Background
Despite their higher risk of developing severe disease, little is known about the burden of influenza in Portugal in children aged < 5 years old. This study aims to cover this gap by estimating the clinical and economic burden of severe influenza in children, in Portugal, during ten consecutive influenza seasons (2008/09-2017/18).
Methods
We reviewed hospitalizations in children aged < 5 years old using anonymized administrative data covering all public hospitals discharges in mainland Portugal. The burden of hospitalization and in-hospital mortality directly coded as due to influenza was supplemented by the indirect burden calculated from excess hospitalization and mortality (influenza-associated), estimated for four groups of diagnoses (pneumonia or influenza, respiratory, respiratory or cardiovascular, and all-cause), through cyclic regression models integrating the incidence of influenza. Means were reported excluding the H1N1pdm09 pandemic (2009/10).
Results
The mean annual number of hospitalizations coded as due to influenza was 189 (41.3 cases per 100,000 children aged < 5 years old). Hospitalization rates decreased with increasing age. Nine-in-ten children were previously healthy, but the presence of comorbidities increased with age. Children stayed, on average, 6.1 days at the hospital. Invasive mechanical ventilation was used in 2.4% of hospitalizations and non-invasive in 3.1%. Influenza-associated excess hospitalizations between 2008 and 2018 were estimated at 1,850 in pneumonia or influenza, 1,760 in respiratory, 1,787 in respiratory or cardiovascular, and 1,879 in all-cause models. A total of 95 influenza-associated excess deaths were estimated in all-cause, 14 in respiratory or cardiovascular, and 9 in respiratory models. Over ten years, influenza hospitalizations were estimated to have cost the National Health Service at least €2.9 million, of which 66.5% from healthy children.
Conclusions
Influenza viruses led to a high number of hospitalizations in children. Most were previously healthy. Results should lead to a reflection on the adequate preventive measures to protect this age group.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12879-023-08685-z.
Keywords: Influenza, Burden, Excess, Mortality, Hospitalization, Children, Healthy, Portugal
Background
Every year, influenza viruses are estimated to infect between 5 and 10% of adults and 20–30% of children across the globe, causing substantial morbidity and mortality [1]. Influenza’s clinical manifestations can range from asymptomatic to severe illness, often [2]triggering complications in children, such as primary viral or secondary bacterial pneumonia, seizures, sinusitis, acute otitis media, exacerbations of existing respiratory conditions, amongst others [2–4].
Although [1]annual influenza vaccination in children aged 6–59 months is recommended by the World Health Organization, some countries – such as Portugal – recommend it only for high-risk children [3, 5–8]. There are few studies in Europe focused on understanding the burden of influenza in children and characterizing the severe cases that lead to hospitalization and even death [9, 12], despite evidence suggesting that children aged < 5 years old may have the highest hospitalizations rates amongst all age groups [10].
In our study, we aimed to estimate the epidemiological and economic burden of severe influenza in children aged < 5 years old in Portugal, during ten consecutive influenza seasons (2008/09-2017/18). Secondary objectives included the description of the clinical and demographic characteristics of hospitalized children, as well as outcomes and severity indicators of the episodes. The burden of hospitalization and in-hospital mortality directly due to influenza (i.e., coded as due to influenza) as calculated from the National Health Service (NHS) discharge data was supplemented by the burden calculated from excess hospitalization and mortality indirectly due to influenza (influenza associated) and related costs.
Methods
The Burden of Acute Respiratory Infections (BARI) study is a multidimensional real-world evidence study assessing the clinical and economic burden of acute respiratory infections (influenza and respiratory syncytial virus) in Spain and Portugal [10–15]. Here we report results for the burden of severe influenza in children aged < 5 years old in Portugal, measured through hospitalizations and deaths. Results for other age groups are reported by Froes et al. (2022) [10].
The following approach was used: (i) a direct method of estimating seasonal influenza incidence, based on the number of NHS hospitalizations with influenza-specific International Classification of Diseases (ICD) codes; (ii) an indirect method of estimating excess hospitalizations and deaths using broader groups of ICD codes in time-series ecological models [10].
Data sources
Hospital discharge data
Anonymized administrative data on hospitalizations (January 2008–December 2018) were provided by the Administração Central do Sistema de Saúde (Health System Central Administration), which collects administrative and clinical data for all hospitalization episodes in Portuguese public hospitals, including information on diagnoses and procedures performed during hospital stay, which are coded using the ICD-9-CM and ICD-10-CM/PCS. These data were also used to describe the in-hospital case fatality risk based on discharge status, corresponding to the hospitalization episodes coded as due to influenza that resulted in in-hospital death during the respective episode.
Death certificate data
The analysis of influenza-associated excess mortality used data on daily deaths listed in the death certificate for children aged < 5 years old per cause obtained from the Instituto Nacional de Estatística (INE, National Statistics Institute) in July 2020. The data were aggregated into weekly counts [16]. The coding for primary death from the death certificate was used.
Influenza activity data
The primary predictor of influenza excess hospitalizations and deaths was the overall weekly incidence rate of influenza-like-illness (ILI), which was obtained from the Instituto Nacional de Saúde Doutor Ricardo Jorge (National Institute of Health Doutor Ricardo Jorge) in July 2020 [17].
Demographic data
Data on age-specific annual resident population estimates were downloaded from INE’s website [16] to compute rates of cases per 100,000 people.
Statistical analysis
An ecological approach was used to estimate the number of influenza-associated excess hospitalizations, deaths, and hospitalization costs by using different Poisson cyclic regression models (time series), where cause-specific hospitalization and mortality data were explained by the ILI incidence, as well as time trends and seasonal terms, using a log link (moving average, broken down by season, with a one-week lag for hospitalizations and three-week lag for deaths) [10, 11, 18].
The number of influenza-associated hospitalizations or deaths was defined for each epidemic season by the sum of the weekly excesses. The seasons were defined from September to June of each year, as standard for the Northern Hemisphere. Cases per 100,000 people were computed by dividing the estimated influenza cases by the Portuguese population aged < 5 years old. Means were reported only for nine seasons, excluding the H1N1pdm09 pandemic (2009/10). Three-year means, including the most recent seasons (2015/16 to 2017/18), were also included.
The correlation between the values predicted by the model and those observed indicated the performance of the model, using Pearson’s correlation. The mean absolute percentage error, defined as the average of the percentage difference between predicted and observed values for all weeks, was also computed. All analyses were performed using SAS 9.4.
Case definition
Hospitalizations coded as due to Influenza
Data were extracted from administrative databases from 2008 to 2018 that contained all NHS hospitalization records in mainland Portugal for children aged < 5 years old. Influenza episodes were defined as those coded with ICD-9 487 or 488; or ICD-10 J09, J10, or J11 in any primary or secondary diagnosis field [10, 19]. Diagnostics information during the influenza episode was also used to identify children who had at least one medical condition regarded as a risk factor for severe influenza (respiratory or lung disease, cardiovascular disease, immunocompromised, and other conditions – Down syndrome, diabetes mellitus, chronic liver/kidney disease, neuromuscular impairment), in any primary or secondary diagnosis field, as detailed in Table S1.
Mechanical ventilation was used as surrogate indicator of Intensive Care Unit (ICU) admissions, as these are not separately identified in the database [14, 20].
Excess hospitalization and mortality
Influenza-associated excess hospitalization was computed for four groups of diagnoses, according to the primary diagnosis, namely pneumonia or influenza (P&I, ICD-9: 480–488, 517.1; or ICD-10: J09–J18), respiratory (R, ICD-9: 460–519; or ICD-10: J00–J99), respiratory or cardiovascular (R&C, ICD-9: 390–459, 460–519; or ICD-10: I00–I99, J00–J99), and all-cause (any ICD-9/10 diagnosis). Influenza-associated excess mortality was computed for the same groups of diagnoses according to the cause of death listed on the death certificate.
Cost estimation
Only direct costs were estimated using a diagnosis-related group-based budget allocation model. Hospitalization costs were computed by multiplying each cost weight with the Portuguese fixed cost multiplier and funding price applicable for the 2018 year [10]. The cost of excess hospitalization was computed by multiplying the number of estimated excess hospitalizations by the mean cost per hospitalization by cause.
Ethical considerations
The study was conducted following the ethical principles of the Declaration of Helsinki and as per local regulations, including privacy laws. Data were provided anonymized and may be used for research purposes without the approval of an ethics committee or informed consent. In addition, the protocol of the BARI study was validated by a panel of clinical experts, classified by the Agency of Medicines and Medical Devices as an observational study and approved by the Ethics Committee of Hospital Clinic de Barcelona (HCB/2020/1132), who waived the need for participant consent.
Results
Descriptive statistics for unmodeled hospitalizations and deaths
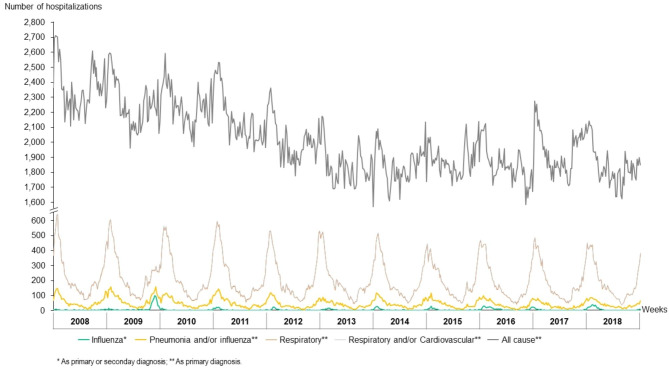
In 2018, Portugal had a resident population of 10.3 million, of which 4.2% (0.4 million) were aged < 5 years old [21]. During the study period, a total of 1.0 million all-cause hospitalizations were registered in children aged < 5 years old in Portuguese public hospitals. R&C, R, and P&I diagnoses accounted for 10.3%, 10.2%, and 2.2% of hospitalizations, respectively. The evolution of the weekly hospitalizations per groups of causes throughout the study period is displayed in Fig. 1. A total of 3,490 children aged < 5 years old have died in Portugal over the same period. R&C, R, and P&I diagnoses accounted for 3.7%, 2.2%, and 1.1% of deaths, respectively.
Fig. 1.
Weekly hospitalizations in children aged < 5 years old, by groups of ICD-9/10 codes, in Portuguese public hospitals, between 1st January 2008–31st December 2018
Hospitalizations coded as due to Influenza
Hospitalization rate
A total of 2,319 influenza hospitalizations were registered in children aged < 5 years old between seasons 2008/09 and 2017/18, of which 843 (36.4%) during the last three seasons. The maximum number of influenza hospitalizations was observed in 2009/10, the H1N1 pandemic season. Excluding this atypical season, the mean annual number of hospitalizations per season was 189, corresponding to 41.3 cases per 100,000 children (Table 1). Influenza hospitalization rates decreased as age increased (Table 2). Influenza was the primary discharge diagnosis in 73.6%1 of the observed influenza hospitalizations, and a secondary discharge diagnosis in the remaining ones (Table 1).
Table 1.
Number and characteristics of hospitalizations coded as due to influenza in children aged < 5 years old by epidemic season in Portuguese public hospitals between 2008/09 and 2017/18 seasons
| Season | N | Ratec | Influenza as primary diagnosis (%) | Mean LoS (days) |
In-hospital case fatality risk (%) | Use of supple-mental oxygen (%) | Use of non-invasive MV (%) | Use of invasive MV (%) | Mean hospitalization cost per patiente (€) | With comor-bidities (%) |
|---|---|---|---|---|---|---|---|---|---|---|
|
2008/ 2009 |
117 | 22.8 | 86.3 | 4.4 | 0.0 | 17.9 | 0.9 | 0.9 | 780 | 5.1 |
|
2009/ 2010 |
617 | 123.5 | 82.7 | 5.1 | 0.2 | 17.8 | 0.6 | 2.1 | 1,232 | 8.4 |
|
2010/ 2011 |
158 | 32.2 | 74.7 | 6.6 | 0.6 | 34.2 | 3.2 | 3.2 | 1,576 | 5.7 |
|
2011/ 2012 |
128 | 26.6 | 68.0 | 6.8 | 0.0 | 31.3 | 1.6 | 4.7 | 1,295 | 17.2 |
|
2012/ 2013 |
122 | 26.3 | 73.8 | 6.6 | 0.8 | 41.8 | 3.3 | 4.9 | 2,471 | 13.1 |
|
2013/ 2014 |
180 | 40.0 | 70.0 | 7.0 | 0.0 | 32.2 | 3.3 | 1.1 | 1,253 | 10.0 |
|
2014/ 2015 |
154 | 35.3 | 66.2 | 5.3 | 0.0 | 32.5 | 3.2 | 1.3 | 967 | 12.3 |
|
2015/ 2016 |
340 | 79.4 | 75.3 | 6.0 | 0.3 | 38.2 | 2.4 | 2.9 | 1,307 | 12.9 |
|
2016/ 2017 |
170 | 39.9 | 70.0 | 6.3 | 0.0 | 40.6 | 2.9 | 1.8 | 1,209 | 12.4 |
|
2017/ 2018 |
333 | 77.4 | 76.0 | 5.9 | 0.0 | 33.0 | 5.1 | 1.8 | 1,005 | 10.8 |
| 9-year meana | 189 | 41.3 | 73.6 | 6.1 | 0.2 | 34.3 | 3.1 | 2.4 | 1,278 | 11.2 |
| 3-year meanb | 281 | 65.6 | 74.5 | 6.0 | 0.1 | 36.7 | 3.6 | 2.3 | 1,174 | 12.0 |
Abbreviations: LoS: Length of stay; MV: Mechanical ventilation; N: Number of hospitalizations coded as due to influenza
a Includes the following seasons: 2008/09, 2010/11, 2011/12, 2012/13, 2013/14, 2014/15, 2015/16, 2016/17, 2017/18. Excludes season 2009/10, since it was affected by the 2009 influenza A (H1N1) pandemic; b Includes the most recent seasons, namely 2015/16, 2016/17, 2017/18; c Rate of hospitalizations coded as due to influenza per 100,000 children aged < 5 years old; d Discharges to long-term hospital care, specialized care, post-hospital care, palliative care, transference to other institution with inpatient care or home care; e Includes > 1 influenza hospitalization/patient
Table 2.
Summary of the characteristics of the hospitalizations coded as due to influenza in children aged < 5 years old by age group and presence of comorbidities in Portuguese public hospitals between 2008/09 and 2017/18 seasons
| Variable | Age Group (in months) | Aged < 5 years old with comorbidities | Aged < 5 years old without comorbidities |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–5 | 6–11 | 12–23 | 24–35 | 36–47 | 48–59 | < 24 | 24–59 | 0–59 | |||
| Share of hospitalizations (% of hospitalizations) | |||||||||||
| 9 years meana | 32.5 | 17.7 | 24.0 | 11.8 | 8.1 | 5.8 | 74.3 | 25.7 | 100.0 | 11.2 | 88.8 |
| 3 years meanb | 30.4 | 18.7 | 25.1 | 12.2 | 7.5 | 6.0 | 74.3 | 25.7 | 100.0 | 12.0 | 88.0 |
| Hospitalization rate (hospitalizations per 100,000 children) c | |||||||||||
| 9 years meana | 139.4 | 75.7 | 50.3 | 24.5 | 16.5 | 11.6 | 78.6 | 17.4 | 41.3 | NA | NA |
| 3 years meanb | 196.7 | 121.4 | 81.7 | 40.2 | 25.0 | 19.9 | 120.4 | 28.4 | 65.6 | NA | NA |
| Mean LoS (in days) | |||||||||||
| 9 years meana | 6.1 | 6.3 | 6.4 | 5.7 | 6.4 | 4.6 | 6.2 | 5.7 | 6.1 | 12.8 | 5.2 |
| 3 years meanb | 5.2 | 6.5 | 7.1 | 5.5 | 6.0 | 5.1 | 6.2 | 5.6 | 6.0 | 11.9 | 5.2 |
| In-hospital case fatality risk (% of hospitalizations) | |||||||||||
| 9 years meana | 0.0 | 0.0 | 0.0 | 0.5 | 0.7 | 1.0 | 0.0 | 0.7 | 0.2 | 0.5 | 0.1 |
| 3 years meanb | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 2.0 | 0.0 | 0.5 | 0.1 | 0.0 | 0.1 |
| Use of supplemental oxygen (% of hospitalizations) | |||||||||||
| 9 years meana | 28.3 | 44.2 | 39.4 | 35.3 | 30.4 | 19.2 | 35.7 | 30.1 | 34.3 | 48.7 | 32.4 |
| 3 years meanb | 29.7 | 46.8 | 42.9 | 35.0 | 28.6 | 27.5 | 38.5 | 31.3 | 36.7 | 51.5 | 34.6 |
| Use of non-invasive mechanical ventilation (% of hospitalizations) | |||||||||||
| 9 years meana | 5.2 | 2.7 | 1.2 | 2.5 | 3.6 | 1.0 | 3.3 | 2.5 | 3.1 | 7.9 | 2.5 |
| 3 years meanb | 6.3 | 2.5 | 1.4 | 2.9 | 4.8 | 2.0 | 3.7 | 3.2 | 3.6 | 6.9 | 3.1 |
| Use of invasive mechanical ventilation (% of hospitalizations) | |||||||||||
| 9 years meana | 3.6 | 2.0 | 1.7 | 1.5 | 1.4 | 3.0 | 2.6 | 1.8 | 2.4 | 9.9 | 1.5 |
| 3 years meanb | 2.7 | 1.9 | 2.4 | 1.0 | 1.6 | 3.9 | 2.4 | 1.8 | 2.3 | 8.9 | 1.3 |
| Mean hospitalization cost per patient d (€) | |||||||||||
| 9 years meana | 1,678 | 1,282 | 925 | 1,050 | 1,165 | 1,048 | 1,339 | 1,086 | 1,278 | 3,812 | 953 |
| 3 years meanb | 1,150 | 1,513 | 1,008 | 1,171 | 940 | 1,095 | 1,194 | 1,086 | 1,174 | 2,612 | 972 |
Abbreviations: LoS: length of stay; NA: Not available
a Includes the following seasons: 2008/09, 2010/11, 2011/12, 2012/13, 2013/14, 2014/15, 2015/16, 2016/17, 2017/18. Excludes season 2009/10, since it was affected by the 2009 influenza A (H1N1) pandemic; b Includes the most recent seasons, namely 2015/16, 2016/17, 2017/18; c Rate of hospitalizations coded as due to influenza per 100,000 children; d Includes > 1 influenza hospitalization/patient
Demographic and clinical characteristics
The male to female ratio was 1.3, with boys accounting for 56.2% of influenza hospitalizations1. Children aged bellow 12 months of age accounted for 50.2% of hospitalizations (Table 2)1. Children without known predisposing risk factors for severe influenza infection accounted for 88.8% of influenza hospitalizations1 (Table 2). The share of influenza hospitalized children with a reported comorbidity increased with age. Comorbidities were observed in 7.8%, 10.3%, 9.5%, 15.4%, 17.4% and 23.2% of influenza hospitalizations in children aged 0–5, 6–11, 12–23, 24–35, 36–47 and 48–59 months of age, respectively1. Respiratory or lung disease was the most common comorbidity, closely followed by cardiovascular disease (Figure S1).
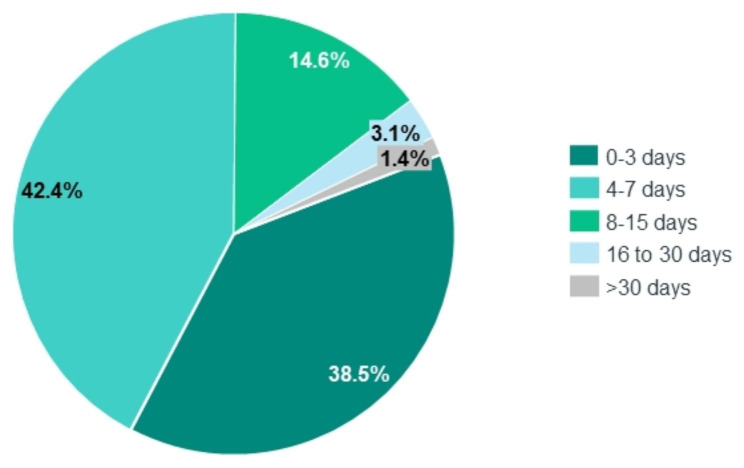
Severity indicators
The mean length of stay (LoS) stood at 6.1 days, increasing to 12.8 in children with comorbidities1 (Table 2). Most children (42.4%) were hospitalized during 4–7 inpatient days (Fig. 2) 1. The mean LoS was lower in children aged between 48 and 59 months of age (4.6 days) and ranged between 5.7 and 6.4 days in the other age groups1 (Table 2). Invasive mechanical ventilation was used in 2.4% of influenza hospitalizations, non-invasive ventilation in 3.1% and oxygen supplementation in 34.3%1 (Table 1). During the study period, four deaths were observed among the 2,319 influenza hospitalizations. Excluding the pandemic season, the mean in-hospital case fatality risk was 0.2%. On average, children with comorbidities had more severe influenza hospitalization episodes than those without comorbidities, measured by the LoS, use of mechanical ventilation, oxygen supplementation and in-hospital case fatality risk (Table 2).
Fig. 2.
Percentage of hospitalizations diagnosed as due to influenza in children aged < 5 years old by length-of-stay at the hospital, in Portuguese public hospitals, between 2008/09 and 2017/18
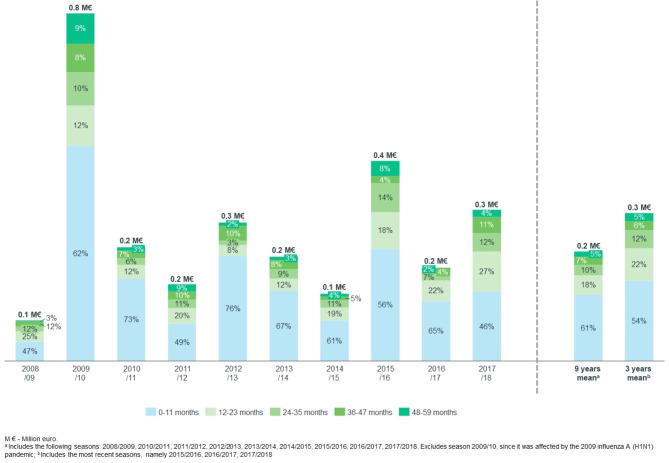
Direct cost
Over ten years, the 2,319 hospitalizations coded as due to influenza in children aged < 5 years old cost the Portuguese NHS €2.9 million. Costs varied considerably according to the epidemic season, from €0.1 million in 2008/09 to €0.8 million in 2009/10 (Fig. 3). The mean direct annual cost over nine seasons was €0.2 million1, of which 60.6%, 17.6%, 9.7%, 7.4% and 4.7% were generated by children aged 0–11, 12–23, 24–35, 36–47 and 48–59 months of age, respectively1 (Fig. 3). Children without registered comorbidities, accounted for 66.5% of all influenza direct hospitalization costs1. Mean per hospitalized children aged < 5 years old was €1,278 (Table 1)1. The mean cost of hospitalization was €953 in children without comorbidities, increasing fourfold in children with comorbidities (Table 1)1.
Fig. 3.
Direct cost of hospitalizations coded as due to influenza in children aged < 5 years old by months of age and epidemic season, in Portuguese public hospitals, between 2008/09 and 2017/18 (million €)
Influenza-associated excess hospitalization
Estimated excess hospitalization
The influenza-associated excess hospitalizations in children aged < 5 years old between 2008 and 2018 were estimated at 1,850 in the P&I, 1,760 in the R, 1,787 in the R&C, and 1,879 in the all-cause model (Table 3). The all-cause hospitalizations model had an inferior performance, as detailed in Supplementary Materials (Table S2). The model using P&I hospitalizations estimated influenza-associated excess hospitalizations in all seasons, except for 2012/13. The absolute and relative influenza-associated excess hospitalizations is presented in Table 3 for all groups of diagnoses and seasons.
Table 3.
Estimated influenza-associated excess hospitalizations in children aged < 5 years old, in absolute number of cases and per 100,000 children, by group of diagnoses and epidemic season in Portuguese public hospitals between 2008/09 and 2017/18 seasons
| 2008/ 2009 | 2009/ 2010 | 2010/ 2011 | 2011/ 2012 | 2012/ 2013 | 2013/ 2014 | 2014/ 2015 | 2015/ 2016 | 2016/ 2017 | 2017/ 2018 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| P&I | N | 119 | 570 | 183 | 40 | -b | 259 | 84 | 278 | 101 | 215 |
| 95% CI | 40–207 | 512–629 | 115–262 | -28 to 103 | -266 to -119 | 198–312 | 27–135 | 207–334 | 40–155 | 132–281 | |
| Ratea | 23.0 | 112.6 | 37.0 | 8.2 | -b | 56.8 | 19.0 | 64.4 | 23.8 | 50.1 | |
| R | N | -b | 95 | -b | -b | -b | 367 | -b | 646 | -b | 652 |
| 95% CI | -1313 to -658 | -171 to 374 | -1147 to -533 | -412 to 99 | -1740 to -1158 | 152–596 | -1287 to -817 | 373–895 | -382 to 109 | 351–929 | |
| Ratea | -b | 18.8 | -b | -b | -b | 80.5 | -b | 149.3 | -b | 152.2 | |
| R&C | N | -b | 93 | -b | -b | -b | 381 | -b | 652 | -b | 662 |
| 95% CI | -1339 to -689 | -176 to 371 | -1166 to -556 | -405 to 105 | -1754 to -1169 | 165–613 | -1,292 to -820 | 377–909 | -387 to 105 | 364–942 | |
| Ratea | -b | 18.3 | -b | -b | -b | 83.4 | -b | 150.8 | -b | 154.7 | |
| All-cause | N | -b | -b | 922 | 214 | -b | -b | -b | 743 | -b | -b |
| 95% CI | -2442 to -1097 | -994 to 145 | 323–1576 | -428 to 862 | -4506 to -3112 | -1718 to -516 | -1934 to -928 | 72-1382 | -1380 to -335 | -1147 to 297 | |
| Ratea | -b | -b | 186.4 | 44.0 | -b | -b | -b | 171.8 | -b | -b |
Abbreviations: CI - Confidence interval (of the N); N - Number of excess hospitalizations; R – Respiratory; R&C - Respiratory or cardiovascular; P&I - Pneumonia or influenza
a Rate of influenza-associated excess hospitalizations per 100,000 children aged < 5 years old; b No influenza-associated excess hospitalizations estimated in this season
Estimated direct cost from the excess hospitalization
The direct cost of influenza-associated excess hospitalizations in children aged < 5 years old between 2008 and 2018 was estimated at €1.8 million in the P&I, €1.5 million in the R, €1.6 million in the R&C, and €1.6 million in the all-cause model.
Influenza-associated excess mortality
We estimated a total of 95 influenza-associated excess deaths in children aged < 5 years old between 2008 and 2018 in the all-cause model, 14 in the R&C, and 9 in the R models (Table 4). The analysis was not performed for the P&I diagnoses as the number of total P&I deaths (40 deaths between 2008 and 2018) was not sufficient to perform the statistical analysis. The performance of the models for each group of diagnoses is presented in Table S2. In this age group, the accuracy is higher in the all-cause deaths model.
Table 4.
Estimated influenza-associated excess deaths in children aged < 5 years old, in absolute number of cases and per 100,000 children, by group of diagnoses and epidemic season in Portugal between 2008/09 and 2017/18 seasons
| 2008/ 2009 | 2009/ 2010 | 2010/ 2011 | 2011/ 2012 | 2012/ 2013 | 2013/ 2014 | 2014/ 2015 | 2015/ 2016 | 2016/ 2017 | 2017/ 2018 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| P&I | N | -c | |||||||||
| 95% CI | |||||||||||
| Ratea | |||||||||||
| R | N | 4.0 | 0.5 | 4.7 | -b | -b | 0.0 | -b | -b | -b | 0.1 |
| 95% CI | 3.2–5.7 | -1.0 to 2.1 | 4.1–7.1 | -2.9 to 1.4 | -2.9 to 2.0 | -0.5 to 2.1 | -0.9 to 1.6 | -0.8 to 2.7 | -1.8 to 1.2 | 1.3-5.0 | |
| Ratea | 0.8 | 0.1 | 0.9 | -b | -b | 0.0 | -b | -b | -b | 0.0 | |
| R&C | N | 4.3 | 0.3 | 4.6 | -b | -b | 1.5 | 1.5 | 0.4 | -b | 1.1 |
| 95% CI | 2.6–5.9 | -1.7 to 2.4 | 2.9–6.7 | -3.2 to 2.6 | -2.7 to 2.4 | -0.2 to 3.6 | 0.4–3.4 | -1.0 to 3.5 | -1.4 to 2.1 | 0.3–4.8 | |
| Ratea | 0.8 | 0.1 | 0.9 | -b | -b | 0.3 | 0.3 | 0.1 | -b | 0.3 | |
| All-cause | N | 9.2 | 7.8 | 7.0 | 21.0 | 8.4 | 9.0 | 7.4 | 15.5 | 6.4 | 3.1 |
| 95% CI | -2.9 to 20.4 | -3.5 to 19.8 | -4.4 to 18.3 | 10.1 to 31.7 | -4.0 to 20.9 | -1.3 to 18.7 | -1.4 to 15.8 | 4.1 to 25.7 | -2.3 to 15.0 | -9.5 to 15.6 | |
| Ratea | 1.8 | 1.5 | 1.4 | 4.3 | 1.8 | 2.0 | 1.7 | 3.6 | 1.5 | 0.7 | |
Abbreviations: CI - Confidence interval (of the N); N - Number of excess deaths; R – Respiratory; R&C - Respiratory or cardiovascular; P&I - Pneumonia or influenza
a Rate of influenza-associated excess deaths per 100,000 children aged < 5 years old; b No influenza-associated excess deaths estimated in this season; c Not estimated due to the low number of deaths in children aged < 5 years old in this group of diagnoses
The model has estimated influenza-associated excess all-cause deaths in all seasons. Season 2011/12 was estimated to have been the most fatal, with 21 (95% CI: 10–32) influenza-associated all-cause deaths in children aged < 5 years old (4.3 per 100,000 children). The absolute and relative influenza-associated excess deaths is presented in Table 4 for all groups of diagnoses and seasons.
Discussion
This was the first study exploring the characteristics of children under five years of age that were hospitalized for influenza in Portugal, and estimating the morbidity and mortality caused by influenza over ten seasons. We found that influenza viruses led to a high number of hospitalizations in children, especially in those under 24 months of age and who were previously healthy. These results should support an evidence-based reflection on the adequate preventive measures to protect this age group.
Influenza hospitalization rates
Excluding the 2009/10 H1N1 pandemic, the mean annual number of hospitalizations per season was 189, corresponding to 41.3 cases per 100,000 children, which is bellow general estimates for high-income countries [22]. Influenza hospitalization rates for Portugal were approximately half the estimates published for France [9] and Poland [23] – where differences may be partially explained by the included seasons and by cases treated in the emergency services, which were not accounted for in our study [9, 23] – and were also lower than the ones reported for Spain using the same methodology and period of analysis [11]. Future studies should explore the possible causes for these lower rates.
Characteristics of children hospitalized due to Influenza
Three-fourths of hospitalized children were aged < 24 months. Unsurprisingly, hospitalization rates decreased with increasing age [24, 25]. Across all age groups, we found that most children hospitalized for influenza were previously healthy, which is consistent with studies from other European countries [9, 25]. The presence of comorbidities increased with age, ranging from 7.8% in children aged 0–5 months to 23.2% in children aged 48–59 months of age.
Severity of hospitalizations
The study reveals a non-negligible use of mechanical ventilation during hospitalizations coded as due to influenza (2.4% invasive and 3.1% non-invasive ventilation), potentially reflecting the cases requiring care at the ICU. These are not far from those reported by Tillard et al. (2022) for France, where 2.2% of children aged < 24 months hospitalized for influenza were admitted to ICU [9]. Mean in-hospital case fatality risk was also within reported ranges [11, 23]. [14]
Influenza-associated excess hospitalization and mortality
The study highlights the complexity of estimating the burden of influenza in children. [28]The total number of hospitalizations coded as due to influenza (2,319) over ten seasons was higher than the estimated influenza-associated excess hospitalizations in all groups of diagnoses – which ranged from 1,760 to 1,879 -, as the models were not able to detect influenza-associated excess hospitalizations in all seasons. Similar conclusions would be reached if we contrasted other published estimates with the hospitalizations coded as due to influenza obtained from our study, for the comparable years [26]. As expected, the excess morbidity and mortality estimates varied across the ten seasons and four groups of diagnoses. More studies are needed to establish which cause-specific data are more adequate when estimating morbidity and mortality due to influenza in children [27] and weekly ILI incidence rates specific for children aged < 5 years old are needed to improve the models’ performance, as different weekly trends in the virus circulations are expected across age groups [28].
Findings from our study raise the question on the extent of the under-detection of influenza amongst the younger Portuguese population. In 2015/16 and 2017/18 we estimated around 650 annual influenza-attributed excess R&C hospitalizations, almost the double from the ones coded as due to influenza, results which appear more aligned with international estimates on the rate of influenza hospitalizations [9, 22, 23]. Furthermore, all models estimated a higher number of influenza-associated excess deaths – ranging from 9 to 95 over the total period – in comparison with the four deaths that had been observed during the hospitalizations coded as due to influenza.
[29]In terms of mortality, we have estimated a mean of 2.1 influenza-associated all-cause deaths per children aged < 5 years old1, which is lower than the one estimated by Nunes et al. (2.6) between 1980 and 2004 [29]. It is however higher than the one reported more recently by Nielsen et al. in the pooled estimates of mortality attributable to influenza in children aged < 5 years old in 24 European countries, which varied between 0.4 and 1.1 [30], and higher than the 1.5 reported by Pumarola et al. (2023) for Spain, using the same methodology and period of analysis [11]. Comparison of results with those from other studies is challenging as there are few studies reporting results of excess hospitalization and mortality modelling in children – in Portugal and in other European countries – and as they are sensitive to methodological and temporal differences.
Future studies would benefit from better surveillance data in this age group, with age-stratified data and with information on whether hospitalized children had been vaccinated. Generating more comprehensive evidence contributes to a better understanding of the implications that influenza may have to public health and may help to generate awareness and strengthen preventive policies.
Economic burden of Influenza
[4, 33–37]Although the mean cost of hospitalization was fourfold in children with comorbidities than in those without them, the total cost to the NHS of influenza hospitalizations was mainly driven by children without comorbidities. These results should be considered when assessing whether the current immunization strategies – targeting only high-risk children in Portugal - are sufficient to address the clinical and economic burden of influenza infection across all children and other indirectly affected age groups. Studies demonstrate that the vaccine effectiveness against influenza-related hospitalizations is high in children [31]. Moreover, children – especially schoolchildren, can also be a vehicle of transmission of the influenza virus across the community [3, 32]. Understanding the impact and cost-effectiveness from the extension of influenza vaccination to all children aged 6 months to 5 years of age put in place in the USA, Canada and by several European countries would be advisable [5, 7, 9, 33].
Limitations
The results reported in this study should be interpreted considering its limitations. The administrative data from hospitalizations did not include laboratory data nor information on whether the children had been vaccinated for influenza. It is also subject to coding errors or missing information. Hospitalization data includes all NHS hospitalizations, but not those in the private sector. However, the mortality data are representative of the country, as all deaths registered in the nation were used.
The excess morbidity and mortality modeled with ILI cannot strictly be attributed to influenza alone as our time-series models used ILI incidence as an indicator of influenza activity, without additional control variables [18, 34]. [41]Other variables could have also been used, such as temperature and laboratory data on the circulation of other respiratory viruses [35, 36]. Future studies would benefit from considering other respiratory viruses, namely the respiratory syncytial virus which was estimated by Rodrigues et al. (2019) to have an impact on children all-cause mortality in Portugal twice as high as the one from influenza in season 2016/2017 [37]. Furthermore, as previously addressed, the age-stratified weekly ILI incidence rates were not available for the complete study period limiting the predictive capability of the models [28]. Another limitation from our study is that the age groups used in our time series models were not stratified for 0–23 and 24–59 months of age, although the first group represents most of the hospitalizations coded as influenza [38].
Regarding the economic burden of influenza, our study covers only the tip of the iceberg, as only direct costs of hospitalizations in the NHS were considered, thus excluding children treated in the private and in the outpatient setting, both increasing in recent years. Indirect costs of lost productivity from parents or caregivers were not computed, although they may be generated even by milder cases that do not require hospitalization [39].
Conclusions
Results from the BARI study confirm the high burden of severe influenza in children under 5 years old in Portugal, mostly driven by those without comorbidities. The findings of this study suggest that strategies targeting only high-risk children will provide an inadequate protection and ability to reduce the clinical and economic burden of influenza infection.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
NA.
Abbreviations
- BARI
Burden of Acute Respiratory Infections
- CI
Confidence Interval
- ICD
International Classification of Diseases
- ILI
Influenza-like illness
- INE
Instituto Nacional de Estatística
- LoS
Length of stay
- MV
Mechanical ventilation
- NHS
National Health Service
- P&I
Pneumonia and/or influenza
- R
Respiratory
- R&C
Respiratory and/or cardiovascular
Author contributions
All the authors contributed to the critical analysis and the discussion of the study results, as well as to redacting and revising the manuscript. MC and HL conducted technical analysis of the BARI study.
Funding
The BARI study was funded by Sanofi.
Data Availability
The data that support the study’s findings are available from IQVIA, but there are restrictions on their availability because they were used under license for the current study and thus are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from IQVIA.
Declarations
Competing interests
CG and HB are Sanofi employees. MC and HL are IQVIA employees. GJ reports personal fees from Sanofi outside the submitted work. FF reports Advisory Board and personal fees from Sanofi, Pfizer, MSD, Gilead and personal fees or non-financial support from Bial, AstraZeneca, GSK, Novartis, Boehringer Ingelheim, Tecnifar, Lilly, Bayer and Roche outside the submitted work. ACA and CG have no conflicts of interest to declare.
Ethics approval and consent to participate
The study was conducted following the ethical principles of the Declaration of Helsinki and as per local regulations, including privacy laws. Data were provided anonymized and may be used for research purposes without the approval of an ethics committee or informed consent. In addition, the protocol of the BARI study was validated by a panel of clinical experts, classified by the Agency of Medicines and Medical Devices as an observational study, and approved by the Ethics Committee of Hospital Clinic de Barcelona (Comité de Ética de la Investigación con medicamentos del Hospital Clínic de Barcelona, HCB/2020/1132), which waived the need for participant consent as the study fulfills the criteria established on Orden SAS/3470/2009.
Consent for publication
NA.
Authors’ information (optional)
NA.
Footnotes
Mean for nine seasons (2008/2009 to 2017/2018), i.e., excluding the H1N1pdm09 pandemic (2009/10).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Organization WH. Vaccines against influenza WHO position paper—November 2012. In: Weekly Epidemiological Record = Relevé épidémiologique hebdomadaire vol. 87; 2012: 461–476. [PubMed]
- 2.Zambon M. Influenza surveillance and laboratory diagnosis. Textbook of Influenza 2013:229–49.
- 3.Nayak J, Hoy G, Gordon A. Influenza in children. Cold Spring Harbor Perspectives in Medicine 2021, 11(1). [DOI] [PMC free article] [PubMed]
- 4.Neuzil KM, Wright PF, Mitchel EF, Jr, Griffin MR. The burden of Influenza Illness in children with Asthma and other chronic medical conditions. Pediatrics. 2000;137(6):856–64. doi: 10.1067/mpd.2000.110445. [DOI] [PubMed] [Google Scholar]
- 5.Grohskopf LA. Prevention and Control of Seasonal Influenza with vaccines: recommendations of the Advisory Committee on Immunization practices—United States, 2022–23 Influenza season. MMWR Recommendations and Reports 2022, 71. [DOI] [PMC free article] [PubMed]
- 6.Organization WH. Seasonal influenza vaccines: an overview for decision-makers. 2020.
- 7.Seasonal influenza vaccination strategies. [https://www.ecdc.europa.eu/en/seasonal-influenza/prevention-and-control/vaccines/vaccination-strategies].
- 8.Saúde D-G. Campanha de Vacinação Sazonal contra a Gripe: OutonoInverno 2022–2023. In., vol. 007/2022; 2022.
- 9.Tillard C, Chazard E, Faure K, Bartolo S, Martinot A, Dubos F. Burden of Influenza Disease in children under 2 years of age hospitalized between 2011 and 2020 in France. J Infect. 2022;84(2):145–50. doi: 10.1016/j.jinf.2021.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Froes F, Carmo M, Lopes H, Bizouard G, Gomes C, Martins M, Bricout H, de Courville C, de Sousa JC, Rabaçal C, et al. Excess hospitalizations and mortality associated with seasonal Influenza in Portugal, 2008–2018. BMC Infect Dis. 2022;22(1):726. doi: 10.1186/s12879-022-07713-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pumarola T, Díez-Domingo J, Martinón-Torres F, Redondo Margüello E, de Lejarazu Leonardo RO, Carmo M, Bizouard G, Drago G, López-Belmonte J, Bricout H. Excess hospitalizations and mortality associated with seasonal Influenza in Spain, 2008–2018. BMC Infect Dis. 2023;23(1):86. doi: 10.1186/s12879-023-08015-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gil-de-Miguel Á, Martinón-Torres F, Díez-Domingo J, de Lejarazu Leonardo RO, Pumarola T, Carmo M, Drago G, López-Belmonte JL, Bricout H, de Courville C. Clinical and economic burden of physician-diagnosed Influenza in adults during the 2017/2018 epidemic season in Spain. BMC Public Health. 2022;22(1):2369. doi: 10.1186/s12889-022-14732-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martinón-Torres F, Carmo M, Platero L, Drago G, López-Belmonte JL, Bangert M, Díez-Domingo J, Garcés-Sánchez M. Clinical and economic burden of respiratory syncytial virus in Spanish children: the BARI study. BMC Infect Dis. 2022;22(1):759. doi: 10.1186/s12879-022-07745-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandeira T, Carmo M, Lopes H, Gomes C, Martins M, Guzman C, Bangert M, Rodrigues F, Januário G, Tomé T. Burden and severity of children’s hospitalizations by respiratory syncytial virus in Portugal, 2015–2018. Influenza Other Respir Viruses. 2023;17(1):e13066. doi: 10.1111/irv.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gil-de-Miguel Á, Díez-Domingo J, Martinón-Torres F, Margüello ER, de Lejarazu Leonardo RO, Pumarola T, de Sousa JC, Rabaçal C, Raposo J, Cordeiro CR. Addressing Influenza’s underestimated burden–Iberian experts call to action. BMC Infect Dis. 2023;23(1):308. doi: 10.1186/s12879-023-08277-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Instituto Nacional de Estatística: Óbitos gerais, diários, por causa de morte. In.: INE. Received in. July 2020; 2020.
- 17.Instituto Nacional de Saúde Doutor Ricardo Jorge. : Taxa de incidência de síndrome gripal semanal. In.: INSA. Received in July 2020.; 2020.
- 18.Lemaitre M, Carrat F, Rey G, Miller M, Simonsen L, Viboud C. Mortality burden of the 2009 A/H1N1 Influenza pandemic in France: comparison to seasonal Influenza and the A/H3N2 pandemic. PLoS ONE. 2012;7(9):e45051–1. doi: 10.1371/journal.pone.0045051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton MA, Calzavara A, Emerson SD, Djebli M, Sundaram ME, Chan AK, Kustra R, Baral SD, Mishra S, Kwong JC. Validating International classification of Disease 10th revision algorithms for identifying Influenza and respiratory syncytial virus hospitalizations. PLoS ONE. 2021;16(1):e0244746. doi: 10.1371/journal.pone.0244746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mendes-da-Silva A, Gonçalves-Pinho M, Freitas A, Azevedo I. Trends in hospitalization for acute bronchiolitis in Portugal: 2000–2015. Pulmonology. 2019;25(3):154–61. doi: 10.1016/j.pulmoe.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Instituto Nacional de Estatística: População residente em Portugal. In.: INE. Retrieved in. July 2020; 2020.
- 22.Wang X, Li Y, O’Brien KL, Madhi SA, Widdowson MA, Byass P, Omer SB, Abbas Q, Ali A, Amu A, et al. Global burden of Respiratory Infections associated with seasonal Influenza in children under 5 years in 2018: a systematic review and modelling study. The Lancet Global Health. 2020;8(4):e497–e510. doi: 10.1016/S2214-109X(19)30545-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hospitalization of Children Aged <5 Years Due to Influenza: Study Based on the National Hospitalization Registry. Children (Basel, Switzerland) 2022, 9(7). [DOI] [PMC free article] [PubMed]
- 24.Cromer D, Van Hoek AJ, Jit M, Edmunds WJ, Fleming D, Miller E. The burden of Influenza in England by age and clinical risk group: a statistical analysis to inform vaccine policy. J Infect. 2014;68(4):363–71. doi: 10.1016/j.jinf.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 25.Hauge SH, Bakken IJ, De Blasio BF, Håberg SE. Risk conditions in children hospitalized with Influenza in Norway, 2017–2019. BMC Infect Dis. 2020;20(1):1–9. doi: 10.1186/s12879-020-05486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodrigues E, Machado A, Silva S, Nunes B. Excess Pneumonia and Influenza hospitalizations associated with Influenza epidemics in Portugal from season 1998/1999 to 2014/2015. Influenza Other Respir Viruses. 2018;12(1):153–60. doi: 10.1111/irv.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmidt SS, Iuliano AD, Vestergaard LS, Mazagatos-Ateca C, Larrauri A, Brauner JM, Olsen SJ, Nielsen J, Salomon JA, Krause TG. All‐cause versus cause‐specific excess deaths for estimating Influenza‐associated mortality in Denmark, Spain, and the United States. Influenza and other respiratory viruses 2022. [DOI] [PMC free article] [PubMed]
- 28.Rodrigues AP, Silva S, Torres AR, Guiomar R, Pechirra P, Cristóvão P, Baltazar N. Mortalidade atribuível Ao vírus sincicial respiratório em Portugal entre 2014 e 2018. Instituto Nac De Saúde Doutor Ricardo Jorge Observações Bol Epidemiológico 2019, Número 25(Artigos breves nº2).
- 29.Nunes B, Viboud C, Machado A, Ringholz C, Rebelo-de-Andrade H, Nogueira P, Miller M. Excess mortality associated with Influenza epidemics in Portugal, 1980 to 2004. PLoS ONE. 2011;6(6):e20661. doi: 10.1371/journal.pone.0020661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nielsen J, Vestergaard LS, Richter L, Schmid D, Bustos N, Asikainen T, Trebbien R, Denissov G, Innos K, Virtanen MJ, et al. European all-cause excess and influenza-attributable mortality in the 2017/18 season: should the burden of Influenza B be reconsidered? Clin Microbiol Infect. 2019;25(10):1266–76. doi: 10.1016/j.cmi.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 31.Kalligeros M, Shehadeh F, Mylona EK, Dapaah-Afriyie C, van Aalst R, Chit A, Mylonakis E. Influenza vaccine effectiveness against influenza-associated hospitalization in children: a systematic review and meta-analysis. Vaccine. 2020;38(14):2893–903. doi: 10.1016/j.vaccine.2020.02.049. [DOI] [PubMed] [Google Scholar]
- 32.Worby CJ, Chaves SS, Wallinga J, Lipsitch M, Finelli L, Goldstein E. On the relative role of different age groups in Influenza epidemics. Epidemics. 2015;13:10–6. doi: 10.1016/j.epidem.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agency UHS. The national influenza immunisation programme 2022 to 2023: information for healthcare practitioners. In., vol. Published 20 September 2022; 2022.
- 34.Czaja CA, Miller L, Colborn K, Cockburn MG, Alden N, Herlihy RK, Simões EAF. State-level estimates of excess hospitalizations and deaths associated with Influenza. Influenza Other Respir Viruses. 2020;14(2):111–21. doi: 10.1111/irv.12700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leung VKY, Wong JY, Barnes R, Kelso J, Milne GJ, Blyth CC, Cowling BJ, Moore HC, Sullivan SG. Excess respiratory mortality and hospitalizations associated with Influenza in Australia, 2007–2015. Int J Epidemiol. 2021;51(2):458–67. doi: 10.1093/ije/dyab138. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen J, Krause TG, Mølbak K. Influenza-associated mortality determined from all-cause mortality, Denmark 2010/11-2016/17: the FluMOMO model. Influenza Other Respir Viruses. 2018;12(5):591–604. doi: 10.1111/irv.12564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodrigues A, Silva S, Torres R, Guiomar R, Pechirra P, Cristovão P, Nunes B. Respiratory syncytial virus attributable mortality in Portugal between 2014 and 2018. 2019.
- 38.Organization WH. Global epidemiological surveillance standards for influenza. 2013.
- 39.Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, Bridges CB, Grijalva CG, Zhu Y, Bernstein DI. The underrecognized burden of Influenza in young children. N Engl J Med. 2006;355(1):31–40. doi: 10.1056/NEJMoa054869. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the study’s findings are available from IQVIA, but there are restrictions on their availability because they were used under license for the current study and thus are not publicly available. Data are, however, available from the authors upon reasonable request and with permission from IQVIA.