Abstract
Background
Cardiovascular diseases (CVD), including coronary heart disease (CHD), display a higher prevalence in men than women. This study aims to evaluate the variations in the intestinal microbiota between men and women afflicted with CHD and delineate these against a non-CVD control group for each sex.
Methods
Our research was conducted in the framework of the CORDIOPREV study, a clinical trial which involved 837 men and 165 women with CHD. We contrasted our findings with a reference group of 375 individuals (270 men, 105 women) without CVD. The intestinal microbiota was examined through 16S metagenomics on the Illumina MiSeq platform and the data processed with Quiime2 software.
Results
Our results showed a sex-specific variation (beta diversity) in the intestinal microbiota, while alpha-biodiversity remained consistent across both sexes. Linear discriminant analysis effect size (LEfSe) analysis revealed sex-centric alterations in the intestinal microbiota linked to CVD. Moreover, using random forest (RF) methodology, we identified seven bacterial taxa—g_UBA1819 (Ruminococcaceae), g_Bilophila, g_Subdoligranulum, g_Phascolarctobacterium, f_Barnesiellaceae, g_Ruminococcus, and an unknown genus from the Ruminococcaceae family (Ruminococcaceae incertae sedis)—as key discriminators between men and women diagnosed with CHD. The same taxa also emerged as critical discriminators between CHD-afflicted and non-CVD individuals, when analyzed separately by sex.
Conclusion
Our findings suggest a sex-specific dysbiosis in the intestinal microbiota linked to CHD, potentially contributing to the sex disparity observed in CVD incidence.
Trial registration Clinical Trials.gov.Identifier NCT00924937.
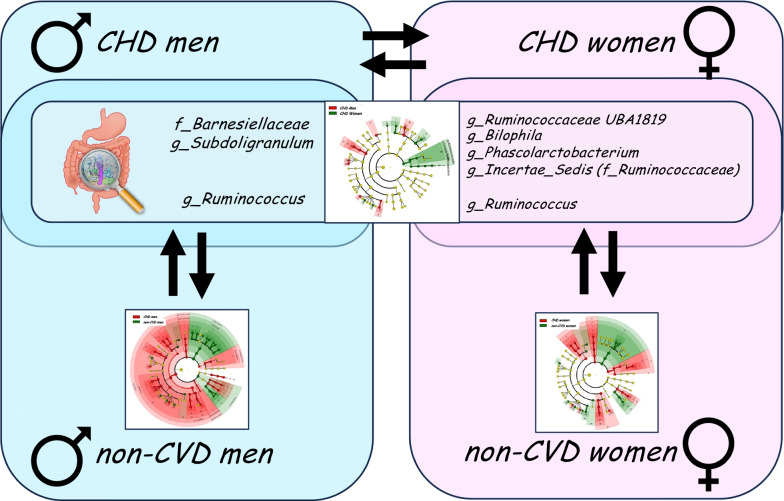
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13293-024-00582-7.
Keywords: Gut microbiota, Dysbiosis, Sexual dimorphism, Cardiovascular diseases, CORDIOPREV
Highlights
The incidence of cardiovascular disease is influenced by sex and appears with greater frequency in men than women.
We hypothesized that the alterations in the intestinal microbiota associated with cardiovascular disease are different in men and women, which could influence the processes that interconnect intestinal microbiota and cardiovascular disease.
Our results suggest that the dysbiosis of the intestinal microbiota associated with coronary heart disease seems to be partially sex-specific.
The identification of the mechanisms responsible for sexual dimorphism in the incidence of metabolic and cardiovascular disease is of particular importance when developing effective strategies and therapies aimed at reducing their incidence and recurrence, which should be sex-specific.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13293-024-00582-7.
Plain language summary
The frequency with which cardiovascular diseases occur differs in men and women as it appears with greater frequency in men. Moreover, it has been known for years that the community of bacteria living in our intestine, also known as the gut microbiota, influences the development of these diseases. Indeed, nowadays it known the influence of the intestinal microbiota in the development of atherosclerosis, the pathological process which is responsible for the three main causes of cardiovascular diseases: coronary heart disease, cerebrovascular disease and peripheral arterial disease. This study shows the differences in the community of bacteria living in the gut of men and those living in the gut of women, so that these differences could explain, at least in part, the differences in the frequency with which cardiovascular diseases appear between men and women. Our results suggest that the dysbiosis of the intestinal microbiota associated with CHD seems to be partially sex-specific, which may influence the sexual dimorphism in its incidence. Moreover, the identification of the mechanisms responsible for sexual dimorphism in the incidence of metabolic and cardiovascular disease is of particular importance when developing effective strategies and therapies aimed at reducing their incidence and recurrence. Indeed, the strategies and therapies used to treat the dysbiosis of the gut microbiota should be sex-specific.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13293-024-00582-7.
Background
Cardiovascular disease (CVD) is a leading cause of mortality in western nations, with incidence rates displaying a notable sex-based dichotomy—men exhibit a higher prevalence compared to women [1]. In recent years, mounting evidence has underscored the role of the intestinal microbiota in the onset of atherosclerosis, the pathological underpinning of the three primary CVD manifestations: coronary heart disease (CHD), cerebrovascular disease, and peripheral arterial disease [2, 3].
The composition of the intestinal microbiota depends on the sex, in addition to other factors such as age, genetic background and the nutritional habits of the host organism [4–7]. In fact, intestinal microbiota transplant experiments in germ-free mice have demonstrated that the sex of the recipient animal shapes the composition of the intestinal microbiota [8].
Factors such as age, genetics, dietary habits, and notably, sex, significantly influence the composition of the intestinal microbiota [4–7]. Studies using germ-free mice have confirmed that the sex of the recipient animal contributes to shaping the gut microbiota [8]. Moreover, growing evidence has indicated that differences in intestinal microbial architecture between sexes may contribute to sex-based disparities in various pathological conditions, such as autoimmune and metabolic diseases [9–12]. This sex-specific influence is evident in our recent findings on the differential composition of gut microbiota in men and women with metabolic syndrome (MetS), which could partly explain the sex-based incidence of this syndrome [13].
In light of these insights, this study hypothesizes that the gut microbiota alterations associated with CVD differ between sexes, potentially influencing CVD-linked processes like endotoxemia, lipid and cholesterol metabolism, and the production of microbial-origin metabolites [2, 3]. Our goal is to examine the differential intestinal microbiota in men and women with CHD, within a population reflecting this disease's sexual dimorphism (CORDIOPREV study, 837 men and 165 women) [14]. We will compare these findings with a non-CVD reference population, living in the same geographical locale as the CORDIOPREV cohort, to account for shared confounding factors such as lifestyle, dietary habits, and genetic background.
Methods
Study population
The current work was conducted in framework of the CORDIOPREV study (Clinical Trials.gov.Identifier: NCT00924937, Registered 19 June 2009, https://classic.clinicaltrials.gov/ct2/show/NCT00924937), an ongoing prospective, randomized, open, controlled trial in 1002 patients with coronary heart disease (CHD) who had their last coronary event over six months before enrolling, and who followed two different dietary models (a low-fat diet and the Mediterranean diet) over a period of seven years in addition to conventional treatment for CHD [14]. CORDIOPREV inclusion and exclusion criteria can be summarized as follows: patients were eligible if they were over 20 years old but under 75, had established CHD without clinical events in the last 6 months, were thought to be capable of following a long-term dietary intervention, and did not have severe diseases, diseases of the digestive tract that involve episodes of diarrhea or an estimated life expectancy of less than seven years. Detailed inclusion and exclusion criteria have been previously described [15]. Fecal samples were available at baseline for a total of 726 patients from which 682 had not received treatment with antibiotics within 1 month before baseline sample collection. Moreover, 3 samples were discarded because low sequencing quality (N = 679).
As reference of non-CVD population, we used the cohort of 375 non-CVD individuals enrolled in the ONCOVER study as healthy controls (http://www.proyecto-oncover.es/), which represents a population without CVD recruited among the free-living population without oncological diseases or disabling diseases or whose severity implied a life expectancy of less than three years from the same geographical location as the population of CORDIOPREV study, who share many of the co-founding factors such as lifestyle, dietary habits and genetic background with the study population. Fecal samples were available for a total of 338 patients from which 329 had not received treatment with antibiotics within 1 month before baseline sample collection. Both studies, CORDIOPREV and ONCOVER, have been approved by the Reina Sofia (Cordoba) University Hospital Ethics and Research Committees. All the participants agreed to their inclusion in these studies. Their trial protocols and all the amendments were approved by the Reina Sofia University Hospital Clinical Research Ethics Committee, following the Helsinki Declaration and good clinical practice.
Clinical plasma parameters
Blood was collected in tubes containing EDTA to give a final concentration of 0.1% EDTA. The plasma was separated from the red blood cells by centrifugation at 1500×g for 15 min at 4 ºC. Analytes in the frozen samples, blinded to the team members, were analyzed centrally by members of the laboratory research team at the Lipid and Atherosclerosis Unit at Reina Sofia University Hospital. The clinical plasma parameters were measured as previously described [6].
Intestinal microbiota analysis
DNA extraction from feces was performed using the QIAamp DNAStool Mini Kit Handbook (QIAGEN, Hilden, Germany), following the manufacturer’s instructions. The intestinal microbiota was examined through 16S metagenomics on the Illumina MiSeq platform (Illumina, San Diego, CA, USA) and the data processed with Quiime2 software as previously described [16]. The sequences obtained in this study have been submitted to NCBI Sequence Read Archive (SRA) under the accession numbers PRJNA1000902 and PRJNA1000795. Further, sequencing data were analyzed and visualized using QIIME2 [17], using the DADA2 method [18]. We evaluated the bacterial alpha- [19] and beta-diversity [20], this latter analyzed by permutational multivariate analysis of variance (PERMANOVA). Taxonomy was assigned to the high-quality reads using q2‐feature‐classifier [21] with a sequence identity threshold of 99% interrogating the sequences with the SILVA database [22]. Linear discriminant analysis (LDA) effect size (LEfSe) was used to compare groups at baseline and visualize the results using taxonomic bar charts and cladograms [23]. In this analysis, to exclude bacterial taxa that were not present in the majority of samples, a cut-off for exclusion was fixed; only bacterial taxa containing sequence reads in at least 75% of total samples were considered. The Chi-square test was applied to establish differences in bacterial presence/absence in bacterial taxa containing sequence reads in at least 50% of the samples in at least one of the experimental groups. Multiple comparisons in the large-scale expression analyses were assessed by False Discovery Rate (FDR) using the Benjamini and Hochberg method. P-values < 0.05 and Q-values < 0.1 were considered statistically significant. To study the potential functionality of the gut microbiota, PICRUSt2 (Phylogenetic Investigation of Communities by Reconstruction of Unobserved States) analysis of 16S sequences was performed to predicate and identify differentially enriched pathways. Thus, PICRUSt2 [24] was used to impute MetaCyc pathway abundance from the original taxonomic assignment. Further, metabolic pathway data were compared by STAMP [25], a graphical software package that provides statistical hypothesis tests and exploratory plots for functional profiles. Data were compared by two-sided Welch’s t-test and filtered for false discoveries using the Benjamini–Hochberg method (Q-value filter > 0.1) and an effect size filter higher than 0.01.
Statistical analysis
The statistical analysis of the data was carried out with SPSS statistical software (IBM SPSS Statistics version 28.0). One-way ANOVA was performed to calculate the statistical differences of the quantitative anthropometric and metabolic variables between groups. P-values < 0.05 were considered statistically significant. R software, version 4.2.3 (R Foundation for Statistical Computing, http://www.R-project.org/) for the random forest classifier carried out using the script of the caret package in R. To obtain more precise curves and assess the performance of the models, we used repeated tenfold cross-validation. The cross-validation error curves (average of ten validation sets each) and performance were averaged. The different taxonomic taxa were normalized by centering and scaling. The predictive value of each variable in the random forest models was calculated by Mean Decrease in Accuracy. The model’s performance was further evaluated through the AUC on the test set. pROC R package was used to calculate the confidence intervals for ROC curves.
Results
Baseline characteristics of the study participants
Based on sex (Table 1), we found CHD men to be younger compared to CHD women (P < 0.05). Interestingly, this sex-based differences in CHD patients were absent in non-CVD subjects. Conversely, higher triacylglycerides, along with increased fasting glucose and insulin levels, were observed in non-CVD men compared to non-CVD women (P < 0.05), a distinction absents among CHD patients. Men consistently demonstrated a higher waist circumference, blood pressure, and lower HDL-c than women across both CHD patients and non-CVD subjects. Differences in anthropometric and metabolic variables between CHD and non-CVD subjects are presented in Table 2.
Table 1.
Baseline characteristic of the participants with available fecal samples in the study according to the sex
| CHD patients | Non-CVD subjects | |||||
|---|---|---|---|---|---|---|
| Men | Women | P-value | Men | Women | P-value | |
| N (men/women) | 567 | 112 | n.a | 242 | 87 | n.a |
| Age (years) | 59.1 ± 0.4 | 62.8 ± 0.8 | < 0.001 | 59.2 ± 0.6 | 59.6 ± 0.9 | 0.711 |
| BMI (kg/m2) | 31.1 ± 0.2 | 31.2 ± 0.5 | 0.821 | 29.5 ± 0.3 | 29.0 ± 0.6 | 0.393 |
| WC (cm) | 106.1 ± 0.5 | 99.0 ± 1.2 | < 0.001 | 101.9 ± 0.7 | 93.6 ± 1.7 | < 0.001 |
| HDL-c (mg/dL) | 41.2 ± 0.4 | 47.5 ± 1.2 | < 0.001 | 43.7 ± 0.6 | 54.7 ± 1.3 | < 0.001 |
| LDL-c (mg/dL) | 88.2 ± 1.1 | 91.7 ± 2.8 | 0.190 | 132.8 ± 2.0 | 130.9 ± 2.9 | 0.612 |
| TAG (mg/dL) | 136.5 ± 2.9 | 136.0 ± 7.3 | 0.953 | 122.1 ± 3.9 | 97.4 ± 4.6 | 0.001 |
| Fasting glucose (mg/dL) | 112.9 ± 1.6 | 115.8 ± 4.9 | 0.482 | 104.9 ± 1.4 | 93.8 ± 1.5 | < 0.001 |
| Fasting insulin (mU/l) | 10.5 ± 0.4 | 10.8 ± 1.2 | 0.764 | 8.8 ± 0.4 | 6.7 ± 0.5 | 0.008 |
| HbA1c (%) | 6.63 ± 0.05 | 6.74 ± 0.13 | 0.409 | 5.75 ± 0.20 | 5.47 ± 0.07 | 0.408 |
| Systolic BP (mmHg) | 137.6 ± 0.8 | 141.7 ± 1.9 | 0.046 | 142.5 ± 1.2 | 136.9 ± 2.3 | 0.021 |
| Diastolic BP (mmHg) | 77.5 ± 0.5 | 74.2 ± 0.9 | 0.004 | 84.6 ± 0.7 | 78.5 ± 1.2 | < 0.001 |
Values correspond to the mean ± SEM
BMI body mass index, WC waist circumference, HDL-c high density lipoprotein-cholesterol, LDL-c low density lipoprotein-cholesterol, TAG triacylglycerides, BP blood pressure
The statistical differences between groups were evaluated by one-way ANOVA
Table 2.
Baseline characteristic of the participants in the study with available fecal samples
| CHD vs non-CVD in population | CHD vs non-CVD in men | CHD vs non-CVD in women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CHD | Non-CVD | P-value | CHD | Non-CVD | P-value | CHD | Non-CVD | P-value | |
| N (men/women) | 679 (567/112) | 329 (242/87) | < 0.001 | 567 | 242 | n.a | 112 | 87 | n.a |
| Age (years) | 59.7 ± 0.4 | 59.3 ± 0.5 | 0.508 | 59.1 ± 0.4 | 59.2 ± 0.6 | 0.889 | 62.8 ± 0.8 | 59.6 ± 0.9 | 0.011 |
| BMI (kg/m2) | 31.1 ± 0.2 | 29.4 ± 0.3 | < 0.001 | 31.1 ± 0.2 | 29.5 ± 0.3 | < 0.001 | 31.2 ± 0.5 | 29.0 ± 0.6 | 0.006 |
| Waist circumference (cm) | 104.9 ± 0.4 | 99.8 ± 0.7 | < 0.001 | 106.1 ± 0.5 | 101.9 ± 0.7 | < 0.001 | 99.0 ± 1.2 | 93.6 ± 1.7 | 0.007 |
| HDL-cholesterol (mg/dL) | 42.3 ± 0.4 | 46.6 ± 0.6 | < 0.001 | 41.2 ± 0.4 | 43.7 ± 0.6 | 0.001 | 47.5 ± 1.2 | 54.7 ± 1.3 | < 0.001 |
| LDL-cholesterol (mg/dL) | 88.7 ± 1.0 | 132.3 ± 1.6 | < 0.001 | 88.2 ± 1.1 | 132.8 ± 2.0 | < 0.001 | 91.7 ± 2.8 | 130.9 ± 2.9 | < 0.001 |
| Triglycerides (mg/dL) | 136.4 ± 2.7 | 115.5 ± 3.2 | < 0.001 | 136.5 ± 2.9 | 122.1 ± 3.9 | 0.005 | 136.0 ± 7.3 | 97.4 ± 4.6 | < 0.001 |
| Fasting glucose (mg/dL) | 113.4 ± 1.5 | 102.0 ± 1.1 | < 0.001 | 112.9 ± 1.6 | 104.9 ± 1.4 | 0.002 | 115.8 ± 4.9 | 93.8 ± 1.5 | < 0.001 |
| Fasting insulin (mU/L) | 10.5 ± 0.4 | 8.3 ± 0.4 | < 0.001 | 10.5 ± 0.4 | 8.8 ± 0.4 | 0.015 | 10.8 ± 1.2 | 6.7 ± 0.5 | 0.003 |
| HbA1c (%) | 6.65 ± 0.05 | 5.67 ± 0.15 | < 0.001 | 6.63 ± 0.05 | 5.75 ± 0.20 | < 0.001 | 6.74 ± 0.13 | 5.47 ± 0.07 | < 0.001 |
| Systolic BP (mmHg) | 138.3 ± 0.8 | 141.2 ± 1.0 | 0.029 | 137.6 ± 0.8 | 142.5 ± 1.2 | 0.001 | 141.7 ± 1.9 | 136.9 ± 2.3 | 0.119 |
| Diastolic BP (mmHg) | 76.9 ± 0.4 | 83.1 ± 0.6 | < 0.001 | 77.5 ± 0.5 | 84.6 ± 0.7 | < 0.001 | 74.2 ± 0.9 | 78.5 ± 1.2 | 0.005 |
Values correspond to the mean ± SEM
BMI body mass index, HDL-c high density lipoprotein-cholesterol, LDL-c low density lipoprotein-cholesterol, TAG triacylglycerides, BP blood pressure
The statistical differences between groups were evaluated by one-way ANOVA
Diversity of the gut microbiota according to the sex
There were no significant differences in alpha diversity indices (Shannon, Simpson (1-D), observed features and Faith's phylogenetic diversity) between male and female CHD patients. However, both Shannon and Simpson alpha diversity indices were lower in CHD men compared to non-CVD men, and similarly lower in CHD women compared to non-CVD women (P = 0.007, P = 0.003, P = 0.004, and P = 0.005, respectively) (Table 3). In contrast, we found significant sex-based distinctions in beta-diversity among CHD patients, which held true across Jaccard and Bray–Curtis distances (qualitative and quantitative measures, respectively), as well as Unweighted and Weighted Unifrac distances (also qualitative and quantitative, considering bacterial phylogeny) (all, P < 0.05). Similar significant differences were found between CHD and non-CVD subjects, within each sex (Table 3).
Table 3.
Alpha- and beta-diversity indexes
| CHD men vs CHD women | CHD men vs non-CVD men | CHD women vs non-CVD women | Non-CVD men vs non-CVD women | |
|---|---|---|---|---|
| N | 567/112 (men/women) | 567/242 (CVD/non-CVD) | 112/87 (CVD/non-CVD) | 242/87 (men/women) |
| Alpha diversity | ||||
| Shannon | 0.199 | 0.007 (lower in CVD) | 0.004 (lower in CVD) | 0.639 |
| Simpson (1-D) | 0.408 | 0.003 (lower in CVD) | 0.005 (lower in CVD) | 0.559 |
| Observed_features | 0.741 | 0.871 | 0.355 | 0.510 |
| Faith-fd | 0.612 | 0.386 | 0.421 | 0.107 |
| Beta diversity | ||||
| Jaccard | 0.001 | 0.001 | 0.001 | 0.001 |
| Bray–Curtis | 0.001 | 0.001 | 0.001 | 0.001 |
| Unweighted_unifrac | 0.001 | 0.001 | 0.001 | 0.001 |
| Weighted_unifrac | 0.001 | 0.001 | 0.002 | 0.002 |
CHD coronary heart disease, CVD cardiovascular disease, Faith-fd Faith’s phylogenetic diversity
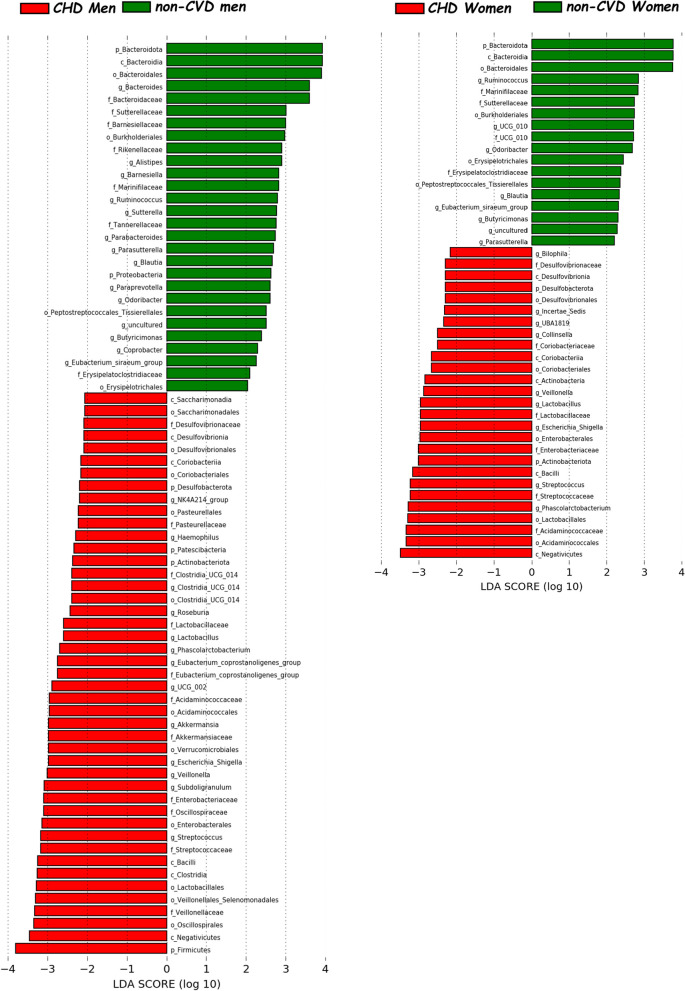
Differences in the gut microbiota composition according to the sex: LEfSe analysis
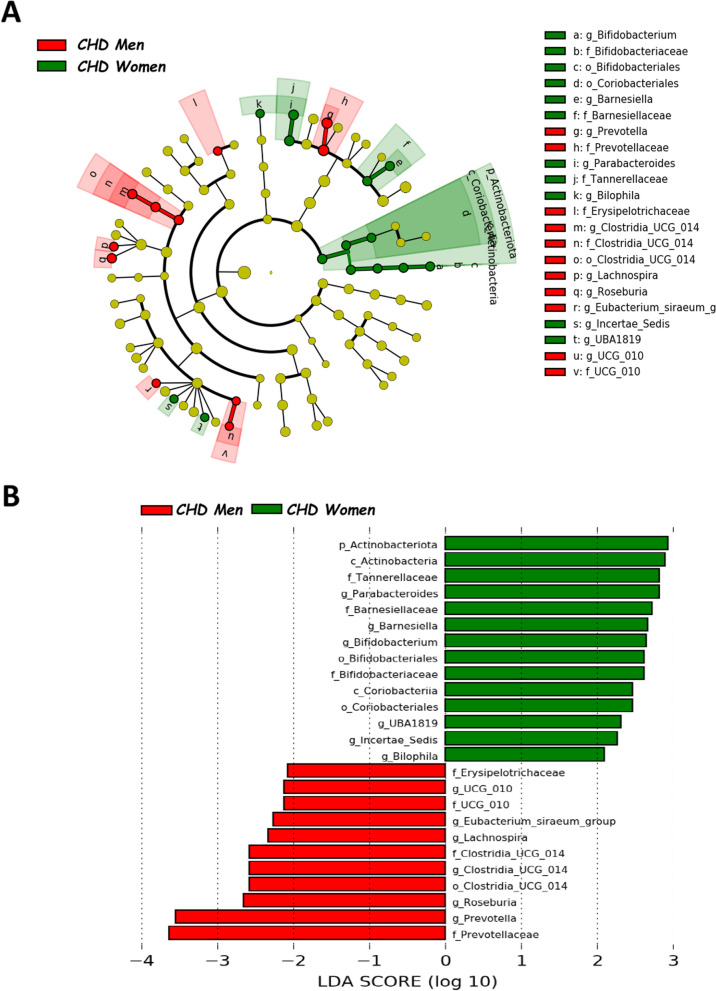
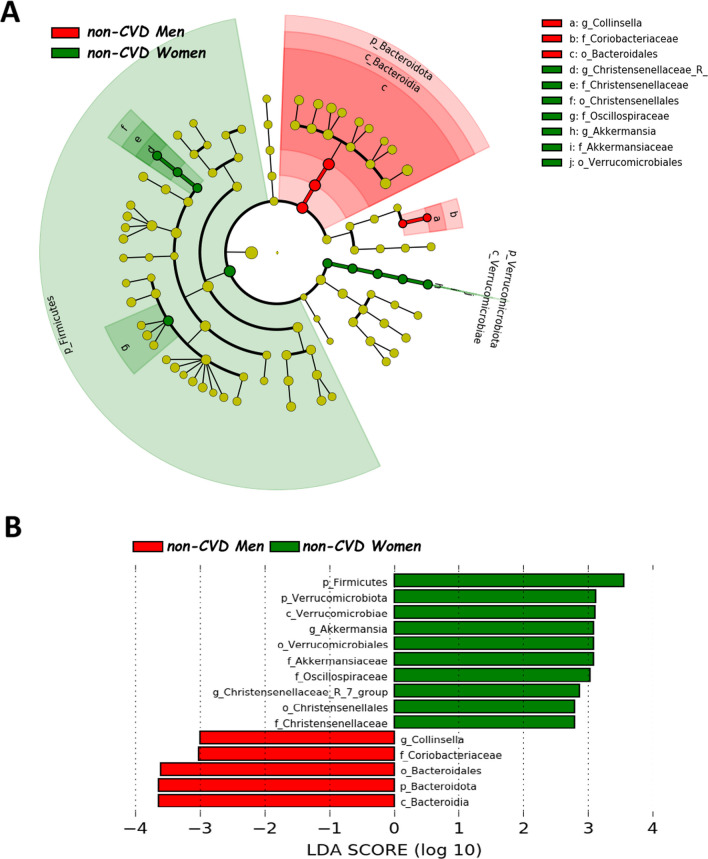
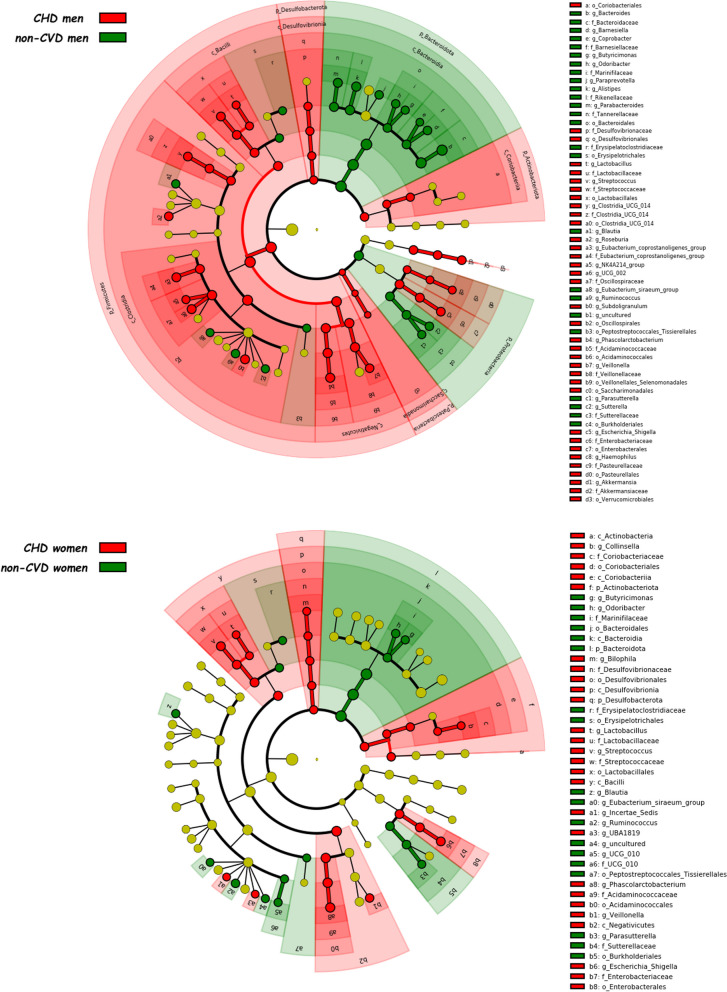
We employed LEfSe to identify taxonomic variations between the gut microbiota of male and female CHD patients. The intestinal microbiota of CHD men was characterized by a preponderance of Clostridia_UCG_014 order (also Clostridia_UCG_014 family and Clostridia_UCG_014 genus), UCG_010 family (also UCG_010 genus), Prevotellaceae (also Prevotella genus) and Erysipelotrichaceae families, and Eubacterium_siraeum_group, Lachnospira, and Roseburia genera. By contrast, the gut microbiota of CHD women was characterized by a preponderance of Actinobacteriota phylum (also Actinobacteria class), Coriobacteriia class (also Coriobacteriales order), Bifidobacteriales order (also Bifidobacteriaceae family and Bifidobacterium genus), Barnesiellaceae (also Barnesiella genus) and Tannerellaceae families, and Parabacteroides, UBA1819 (Ruminococcaceae), Ruminococcaceae incertae sedis and Bilophila genera (Fig. 1). Moreover, we also analyzed the differences in taxonomic composition between non-CVD subjects according to the sex (Fig. 2). Additionally, we noted differences in taxonomic composition between CHD patients and non-CVD subjects, examined separately for each sex (Figs. 3, 4).
Fig. 1.
Differently abundant taxa in CHD patients according to the sex, based on LEfSe analysis. The colors represent the group in which the indicated taxa are more abundant compared to the other group. In a taxonomic cladogram, each successive circle represents a different phylogenetic level. A Cladogram: the order from the center to the outside is phylum, class, family and genus levels. Differing taxa are listed on the right side of the cladogram. B Linear discriminant analysis. The most differently abundant taxa between sexes are represented in a bar graph according to the LDA score (log 10), an estimation of the effect size. Only taxa meeting a P < 0.05 and LDA score significant threshold |> 2| are shown. g_UBA1819: g_UBA1819 (Ruminococcaceae); g_Incertae Sedis: Ruminococcaceae incertae sedis; f_UCG_010: f_UCG_010 (Oscillospirales). CHD coronary heart disease patients
Fig. 2.
Differently abundant taxa in non-CVD patients according to the sex, based on LEfSe analysis. The colors represent the group in which the indicated taxa are more abundant compared to the other group. In a taxonomic cladogram, each successive circle represents a different phylogenetic level. A Cladogram: the order from the center to the outside is phylum, class, family and genus levels. Differing taxa are listed on the right side of the cladogram. B Linear discriminant analysis. The most differently abundant taxa between sexes are represented in a bar graph according to the LDA score (log 10), an estimation of the effect size. Only taxa meeting a P < 0.05 and LDA score significant threshold |> 2| are shown. g_UBA1819: g_UBA1819 (Ruminococcaceae); g_Incertae Sedis: Ruminococcaceae incertae sedis; f_UCG_010: f_UCG_010 (Oscillospirales). non-CVD non-cardiovascular disease individuals
Fig. 3.
Differently abundant taxa between CHD patients and non-CVD subjects in men and women separately identified using LEfSe analysis. The colors represent the group in which the indicated taxon is more abundant compared to the other group. In a taxonomic cladogram, each successive circle represents a different phylogenetic level. The order from the center to the outside is phylum, class, family and genus levels. Differing taxa are listed on the right side of the cladogram. CHD coronary heart disease patients, non-CVD non-cardiovascular disease individuals
Fig. 4.
Linear discriminant analysis between CHD patients and non-CVD subjects in men and women separately. The most differently abundant taxa between sexes are represented in a bar graph according to the LDA score (log 10), an estimation of the effect size and in a taxonomic cladogram. Only taxa meeting a P < 0.05 and LDA score significant threshold |> 2| are shown. CHD coronary heart disease patients, non-CVD non-cardiovascular disease individuals
Differences in the frequency of presence-absence according to the sex
We examined the frequency bacterial genera between sexes and found significant differences in the occurrence of 14 bacterial genera between male and female CHD patients (P < 0.05 and Q < 0.1 in Chi-square test). In addition, frequency differences were observed for 35 bacterial genera between CHD men and non-CVD men, and 18 bacterial genera between CHD women and non-CVD women. Thirteen genera were distinct between CHD patients and non-CVD subjects for both sexes (Fig. 5).
Fig. 5.
Differences in the frequency of presence-absence according to the sex: qualitative analysis. The Chi-square test was applied to establish differences in bacterial presence/absence at genus level
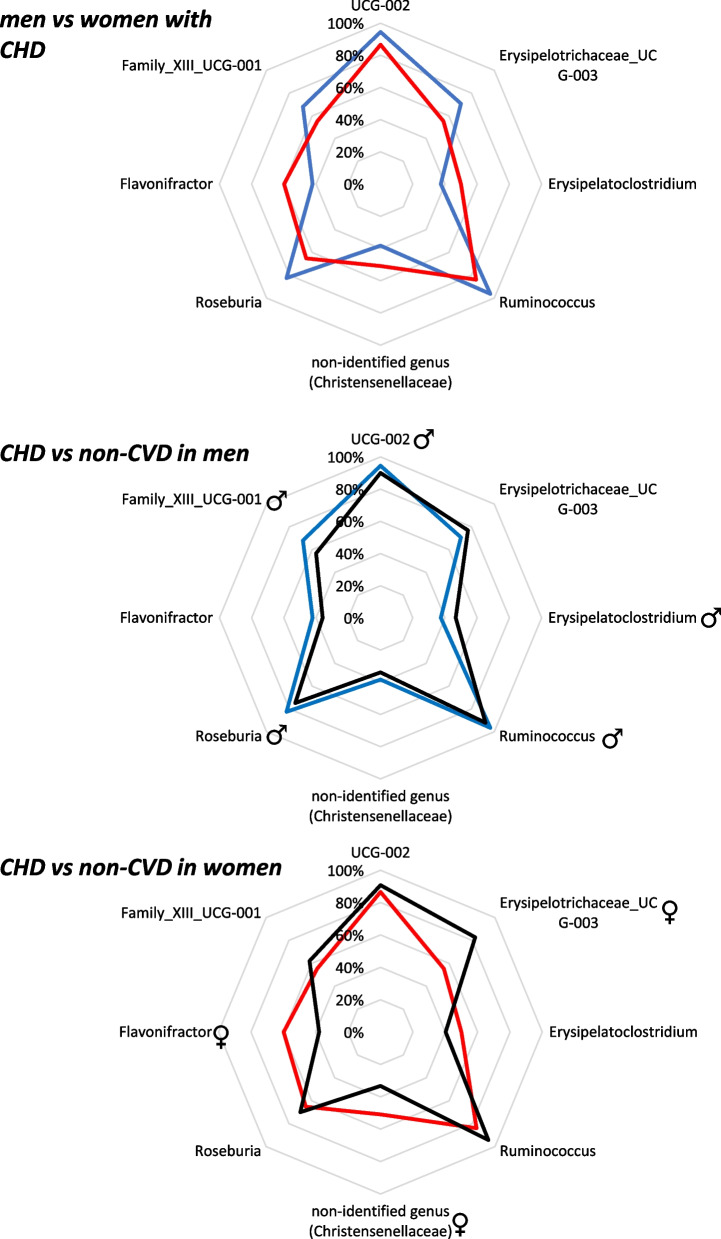
Identification of discriminant bacterial taxa according to the sex: data modeling
A random forest classifier was used to evaluate the different taxonomic taxa normalized on the datasets and their performance evaluated through the AUC of the 20 bacterial taxa most important identified by each model: (i) men and women with CHD and sex as factor (men vs women with CHD model: AUC of 73.0 (CI 67.8–78.2); (ii) men with CHD and men without CVD, and the presence of CVD as factor (CHD men vs non-CVD men model: AUC of 88.5 (CI 85.7–91.4); (iii) women with CHD and women without CVD, and the presence of CVD as factor (CHD women vs non-CVD women model: AUC of 89.4 (CI 85.0–93.9). The 20 bacterial taxa most important identified by each model are shown in Table 4.
Table 4.
Variable importance of the RF models
| Men vs women with CHD model | Importance | CHD men vs non-CVD men model | Importance | CHD women vs non-CVD women model | Importance | ||||
|---|---|---|---|---|---|---|---|---|---|
| g_UBA1819 (Ruminococcaceae) | ♀ | 100.00 | o_Peptostreptococcales_Tissierellales | ♀ | 100.00 | f_Coriobacteriaceae | ♂ | 100.00 | |
| g_Ruminococcus | 83.28 | g_Blautia | 89.11 | c_Negativicutes | ♂ | 80.17 | |||
| g_Bilophila | ♀ | 67.04 | c_Negativicutes | ♀ | 88.56 | o_Peptostreptococcales_Tissierellales | ♂ | 77.78 | |
| g_Coprobacter | 50.15 | f_Coriobacteriaceae | ♀ | 80.76 | f_UCG_010 (Oscillospirales) | 73.80 | |||
| g_Barnesiella | 44.85 | f_Streptococcaceae | ♀ | 76.89 | g_UCG_010 | 68.48 | |||
| g_Alistipes | 43.62 | g_Collinsella | ♀ | 68.36 | g_Collinsella | ♂ | 58.08 | ||
| g_Phascolarctobacterium | ♀ | 41.33 | o_Lactobacillales | ♀ | 67.19 | Ruminococcaceae incertae sedis | 57.79 | ||
| g_Paraprevotella | 38.80 | g_Streptococcus | ♀ | 60.19 | g_Ruminococcus | ♂ | 41.54 | ||
| f_Ruminococcaceae | 37.38 | g_Ruminococcus | ♀ | 57.57 | c_Coriobacteriia | ♂ | 37.40 | ||
| f_Barnesiellaceae | ♂ | 37.28 | g_Subdoligranulum | 54.89 | f_Streptococcaceae | ♂ | 37.17 | ||
| g_Eubacterium_siraeum_group | 36.53 | c_Bacteroidia | 54.28 | o_Coriobacteriales | 35.78 | ||||
| g_Subdoligranulum | ♂ | 36.22 | f_Sutterellaceae | ♀ | 53.39 | o_Lactobacillales | ♂ | 35.33 | |
| g_Parabacteroides | 34.08 | g_UCG_002 (Oscillospiraceae) | 48.34 | p_Actinobacteriota | 32.72 | ||||
| o_Oscillospirales | 33.61 | o_Burkholderiales | ♀ | 47.15 | g_Streptococcus | ♂ | 31.54 | ||
| f_Anaerovoracaceae | 32.19 | f_Oscillospiraceae | 45.45 | o_Burkholderiales | ♂ | 28.56 | |||
| f_Tannerellaceae | 31.97 | p_Bacteroidota | 44.97 | g_UBA1819 (Ruminococcaceae) | 28.23 | ||||
| f_Prevotellaceae | 31.86 | p_Firmicutes | 44.59 | f_Butyricicoccaceae | 27.22 | ||||
| g_Butyricimonas | 31.73 | o_Bacteroidales | 42.07 | g_Bilophila | 27.11 | ||||
| Ruminococcaceae incertae sedis | ♀ | 31.22 | f_Barnesiellaceae | 41.18 | g_Phascolarctobacterium | 26.92 | |||
| f_Rikenellaceae | 31.17 | c_Coriobacteriia | ♀ | 40.66 | f_Sutterellaceae | ♂ | 26.08 | ||
The sex-specific alterations in gut microbiota related to CHD were selected according to the following criteria: (1) bacterial taxa critical to distinguishing CHD men from non-CVD men or bacterial taxa critical to distinguishing CHD women from non-CVD women (2) bacterial taxa that significantly differentiated CHD men and CHD women. Men vs Women with CHD model: ♂, bacterial taxa that significantly differentiated CHD men and CHD women, which was also present among the main important variables on the CHD men vs non-CVD men model (in bold). ♂ bacterial taxa that significantly differentiated CHD men and CHD women, which was also present among the main important variables on the model CHD women vs non-CVD women model (in bold). CHD men vs non-CVD men model: bold, specific taxa in men model (these taxa did not appear in the CHD women vs non-CVD women model, and they are therefore specific to distinguishing CHD men from non-CVD men). ♂, taxa also present among the main important variables on the CHD women vs non-CVD women model. CHD women vs non-CVD women model: bold, specific taxa in women model (these taxa did not appear in the CHD men vs non-CVD men model, and they are therefore specific to distinguishing CHD women from non-CVD women). ♂, taxa also present among the main important variables on the CHD men vs non-CVD men model
Seven discriminant bacterial taxa, g_UBA1819 (Ruminococcaceae), g_Bilophila, g_Subdoligranulum, g_Phascolarctobacterium, f_Barnesiellaceae, g_Ruminococcus, and Ruminococcaceae incertae sedis, were identified as crucial in distinguishing between CHD men and women, which were also significant in distinguishing between CHD and non-CVD subjects for at least one of the sexes. However, g_Ruminococcus was especially significant in distinguishing between CHD and non-CVD individuals, in both sexes (Table 5).
Table 5.
Sex-specific alterations in gut microbiota related to CHD
| Men vs women with CHD RF model | CHD patients vs non-CVD individuals in RF models for men and women separately |
|---|---|
| g_UBA1819 (Ruminococcaceae) | Bacterial taxa identified by RF to distinguishing CHD women from non-CVD women |
| g_Bilophila | Bacterial taxa identified by RF to distinguishing CHD women from non-CVD women |
| g_Phascolarctobacterium | Bacterial taxa identified by RF to distinguishing CHD women from non-CVD women |
| f_Barnesiellaceae | Bacterial taxa identified by RF to distinguishing CHD men from non-CVD men |
| g_Subdoligranulum | Bacterial taxa identified by RF to distinguishing CHD men from non-CVD men |
| Ruminococcaceae incertae sedis | Bacterial taxa identified by RF to distinguishing CHD women from non-CVD women |
The sex-specific alterations in gut microbiota related to CHD were selected according to the following criteria: (1) bacterial taxa critical to distinguishing CHD men from non-CVD men or bacterial taxa critical to distinguishing CHD women from non-CVD women (CHD patients vs non-CVD individuals in models for men and women separately). (2) Bacterial taxa that significantly differentiated CHD men and CHD women (men vs women with CHD model column). CHD coronary heart disease, CVD cardiovascular disease, RF random forest
Gut microbiota functionality in coronary heart disease patients according to the sex
PICRUSt2 analysis of 16S sequences was used to study the potential function of gut microbiota. Further, STAMP software was employed to impute MetaCyc pathway abundance from the original taxonomic assignment. Data were compared by two-sided Welch’s t-test and filtered for false discoveries using the Benjamini–Hochberg method (Q-value filter > 0.1) and an effect size filter higher than 0.01 as difference between proportions. Our analysis revealed differences in the abundance of 196 MetaCyc pathways between non-CVD men and non-CVD women, after correcting for multiple comparisons P-values < 0.05 and Q-values < 0.1. By contrast, we observed differences in the abundance of 18 MetaCyc pathways between CHD men and CHD women, after correcting for multiple comparisons P-values < 0.05 and Q-values < 0.1 (Additional file 1: Fig. S1). MetaCyc pathways differentially abundant between groups are shown in Additional file 2: Table S1.
Discussion
This study identifies distinctions in gut bacterial composition between men and women diagnosed with coronary heart disease (CHD). Not only do these differences appear in bacterial composition, but they also exist in terms of beta diversity. Our data modeling technique using random forests (RF) helped us pinpoint significant discriminant bacterial taxa between men and women with CHD. Furthermore, when comparing CHD patients to non-CVD individuals, we noted that some microbial alterations associated with CHD differ between men and women.
Numerous studies underscore the influential role of gut microbiota in CVD development [2, 3]. Such alterations, often termed dysbiosis, include imbalances in bacterial taxa abundance and a reduced microbial diversity linked to CVD [26]—observations also made in our study when comparing CHD patients with non-CVD individuals. Of note, both CHD patients with non-CVD individuals were recruited from the same geographical location and share many of the co-founding factors such as lifestyle, dietary habits and genetic background.
The gut microbiota composition varies with sex [6, 7, 24], which suggests these differences may account for the sex-based discrepancies in CVD incidence. Indeed, several studies propose that such sex-differences could explain the sexual dimorphism observed in autoimmune and metabolic diseases [9–13].
In our study, we noted sex-specific changes in gut microbiota associated with CVD, along with other alterations linked to CVD, but independent of the sex. We utilized a linear discriminant analysis effect size to identify the most discriminant sex-specific alterations in gut microbiota related to CHD. Furthermore, our RF data modeling approach helped identify bacterial taxa that significantly differentiated men from women with CHD and also highlighted taxa critical to distinguishing CHD from non-CVD in sex-segregated models. In addition, the analysis of metagenome prediction of the gut microbiota functionality showed a reduction in number of MetaCyc pathways differently represented between sexes in CHD patients as compared with the number of pathways differently represented between sexes in non-CVD individuals. These results are in line with the reduced microbial diversity linked to CVD [26], also observed in our study; presumably in CHD patients, sex-differences in functionality are also reduced as the diversity in term of functionality is lower in CVD patients than in non-CVD individuals.
Specific alterations in men's intestinal microbiota connected with CHD included a decrease in the abundance of the Barnesiellaceae family, a bacterial taxon associated with CVD [27, 28], and its abundance has been shown to negatively correlate with carotid–femoral pulse wave velocity, a measure of arterial stiffness [29]. Also, we observed an increase in the Subdoligranulum genus, a taxon thought to be beneficial [30], yet its use as a probiotic has failed to show any beneficial effects in preclinical models [31].
On the other hand, alterations in women's intestinal microbiota linked to CHD involved an increase in the abundance of UBA1819 (Ruminococcaceae), Bilophila, and Phascolarctobacterium genera, along with an unknown genus from the Ruminococcaceae family (Ruminococcaceae incertae sedis). The UBA1819 (Ruminococcaceae) genus is connected to rheumatoid arthritis [32, 33], a chronic inflammatory disease like CVD [34], and negatively associated with lactulose and mannitol ratio, an indicator of intestinal barrier dysfunction [35]. A higher abundance in women with CHD compared to men suggests a lower intestinal barrier dysfunction, which may help reduce the CVD incidence in women. Bilophila is a sulfite-reducing and hydrogen sulfide-producing genus. This latter triggers direct inflammation, exerts genotoxic and cytotoxic effects on epithelial cells, and impairs gut barrier [36], and therefore involved in the chronic inflammation related with cardiometabolic diseases [37, 38]. Phascolarctobacterium a bacterial taxon that has been positively associated to CVD [28]. Even a preclinical study showed that the abundance of this taxon was associated to changes in cardiac structure and function [39].
However, it is worth noting that not all alterations in the gut microbiota connected to CVD were found to be different between sexes. In addition to sex-specific changes, we discovered modifications in the gut microbiota associated with CHD common to both sexes. These pertained to bacterial taxa such as Streptococcus and Ruminococcus genera or Sutterellaceae and Coriobacteriaceae families, which have previously been associated with CVD [40–46]. Of note, the abundance of this bacterial genus was reduced in CHD men as compared with non-CVD men and it was reduced in CHD women as compared with non-CVD women, and additionally, more abundant in CHD men than CHD women. However, the abundance difference was slightly, not detected by LefSe analysis, but enough to be detected in random forest model between CHD men and CHD women.
Taken together, these observations suggest that the abundance of different bacterial taxa related with CVD are differentially altered according to sex, which somehow may influence the sexual dimorphism in its incidence.
Our study has the limitation of an unbalanced number of men and women. In fact, this population was included in the CORDIOPREV study without any type of selection, therefore representing the sexual dimorphism existent in CHD, and any attempt to balance the number of men and women may introduce a bias. In addition, the differences observed herein regarding microbiota architecture may stem from the actual differences in sex hormone levels in elder men and women. On the other hand, it might reflect the residual influence of the dramatic differences in sex steroid profiles early in life between sexes, which may have a persistent effect on gut microbiota over time.
Perspectives and significance
In summary, our findings suggest that the dysbiosis of the gut microbiota associated with CHD may have sex-specific elements, which could potentially affect the sex-based differences in its incidence. It is of paramount importance to understand the mechanisms behind this sexual dimorphism in the incidence of metabolic and cardiovascular diseases as this could guide the development of effective strategies and therapies aimed at reducing their prevalence and recurrence. Indeed, our results imply that strategies and therapies designed to address gut microbiota dysbiosis should consider sex-specific implications.
Supplementary Information
Additional file 1: Figure S1. Functional characterization between CHD patients according to the sex based on PICRUSt2 analysis. CHD: coronary heart disease patients. Bar chart showing the functional difference between CHD men and CHD women. Data were compared by two-sided Welch’s t-test and filtered for false discoveries using the Benjamini–Hochberg method by using the STAMP software.
Additional file 2: Table S1. Functional characterization. Correspondence between BioCyc ID and MetaCyc Pathway nomenclature.
Acknowledgements
The CIBEROBN is an initiative of the Instituto de Salud Carlos III, Madrid, Spain. Antonio Camargo is supported by an ISCIII research contract (Programa Miguel-Servet CP14/00114 and CPII19/00007), and by the Servicio Andaluz de Salud-Junta de Andalucia (Nicolas Monardes Programme Contract C1-0001-2022). The funders had no role in the design and performance of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication. We would like to acknowledge the Biobank at the ‘Sistema Sanitario Público de Andalucía (Córdoba, Andalusia, Spain) for providing the human biological samples. We would also thank to the EASP (Escuela Andaluza de Salud Publica), Granada, Spain, which performed the randomization process for this study.
Author contributions
AC, JL-M, JMO: conceptualization. HG-F, APA-L, JL-Mo, DL-C, JLR-C, FMG-M, JDTP: methodology. HG-F, APA-L, JL-Mo, DR-C, JLR-C, HM-A, FMG-M, JDTP: formal analysis. HG-F, APA-L, JL-Mo, DL-C, JLR-C, FMG-M, JDTP, DR-C: investigation and data curation. AC, JL-M, JL-Mo, HM-A, DR-C: resources. HG-F, APA-L, JL-Mo, HM-A: writing—original draft. AC, JL-M, JMO, JD-L, PP-M, MMM: writing—review and editing. DR-C, MMM, JMO, JD-L, PP-M: visualization. AC, JL-M, JD-L, PP-M, MMM, JMO: supervision. JL-M, AC: funding acquisition. JL-M, AC: project administration.
Funding
The CORDIOPREV study is supported by the Fundacion Patrimonio Comunal Olivarero (Cordioprev-CEAS, 1/2016 to JL-M). The main sponsor was not involved in the design or carrying out the study, and its participation was limited to funding and providing the olive oil used in the study. We also received additional funding from CEAS (Centro de Excelencia en Investigacion sobre Aceite de Oliva), Junta de Andalucia (Consejeria de Salud, Consejeria de Agricultura y Pesca, Consejeria de Innovacion, Ciencia y Empresa), Diputaciones de Jaen y Córdoba, and Ministerio de Medio Ambiente, Medio Rural y Marino, and the Spanish Government. The CORDIOPREV study is supported by the Ministerio de Ciencia e Innovación, Spain, through the grants AGL2012/39615, PIE14/00005, and PIE14/00031 assigned to J.L.-M.; AGL2015-67896-P to J.L.-M. and A.C.; Grant PID2019-104362RB-Ioo funded by MCIN/AEI/10.13039/501100011033 to J.L.-M.; by the Instituto de Salud Carlos III grants CP14/00114, PI19/00299, DTS19/00007 and PI22/00925 to A.C.; by the Consejería de Salud y Familias, Junta de Andalucía (PI-0055-2021 to A.C.); also, by the ‘Consejeria de Innovación, Ciencia y Empresa, Proyectos de Investigación de Excelencia’, Junta de Andalucía via grant CVI-7450 and PY20_00256 obtained by J.L.-M.; and co-funded by the European Union.
Availability of data and materials
Collaborations with the Cordioprev Study are open to Biomedical Institutions, always after an accepted proposal for scientific work. Depending on the nature of the collaboration, electronic data, hard copy data, or biological samples should be provided. All collaborations will be made after a collaboration agreement. Terms of the collaboration agreement will be specific for each collaboration, and the extent of the shared documentation (i.e., deidentified participant data, data dictionary, biological samples, hard copy, or other specified data sets) will be also specifically set on the light of each work.
Declarations
Ethics approval and consent to participate
The Reina Sofia (Cordoba) University Hospital Ethics and Research Committees approved the study protocols that were performed in accordance with the Declaration of Helsinki and good clinical practice. All the participants agreed to their inclusion in these studies, and a written informed consent was obtained from all patients involved in the study.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Helena Garcia-Fernandez and Antonio P. Arenas-de Larriva equally contributed to this work.
Jose Lopez-Miranda and Antonio Camargo equally contributed to this work.
Contributor Information
Jose Lopez-Miranda, Email: jlopezmir@uco.es.
Antonio Camargo, Email: antonio.camargo@imibic.org.
References
- 1.Brown JR, O'Connor GT. Coronary heart disease and prevention in the United States. N Engl J Med. 2010;362(23):2150–2153. doi: 10.1056/NEJMp1003880. [DOI] [PubMed] [Google Scholar]
- 2.Witkowski M, Weeks TL, Hazen SL. Gut microbiota and cardiovascular disease. Circ Res. 2020;127(4):553–570. doi: 10.1161/CIRCRESAHA.120.316242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jonsson AL, Backhed F. Role of gut microbiota in atherosclerosis. Nat Rev Cardiol. 2017;14(2):79–87. doi: 10.1038/nrcardio.2016.183. [DOI] [PubMed] [Google Scholar]
- 4.Tims S, Derom C, Jonkers DM, Vlietinck R, Saris WH, Kleerebezem M, et al. Microbiota conservation and BMI signatures in adult monozygotic twins. ISME J. 2013;7(4):707–717. doi: 10.1038/ismej.2012.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saraswati S, Sitaraman R. Aging and the human gut microbiota-from correlation to causality. Front Microbiol. 2014;5:764. doi: 10.3389/fmicb.2014.00764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haro C, Rangel-Zuniga OA, Alcala-Diaz JF, Gomez-Delgado F, Perez-Martinez P, Delgado-Lista J, et al. Intestinal microbiota is influenced by gender and body mass index. PLoS ONE. 2016;11(5):e0154090. doi: 10.1371/journal.pone.0154090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dominianni C, Sinha R, Goedert JJ, Pei Z, Yang L, Hayes RB, et al. Sex, body mass index, and dietary fiber intake influence the human gut microbiome. PLoS ONE. 2015;10(4):e0124599. doi: 10.1371/journal.pone.0124599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang JJ, Wang J, Pang XY, Zhao LP, Tian L, Wang XP. Sex differences in colonization of gut microbiota from a man with short-term vegetarian and inulin-supplemented diet in germ-free mice. Sci Rep. 2016;6:36137. doi: 10.1038/srep36137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cross TL, Kasahara K, Rey FE. Sexual dimorphism of cardiometabolic dysfunction: gut microbiome in the play? Mol Metab. 2018;15:70–81. doi: 10.1016/j.molmet.2018.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elderman M, de Vos P, Faas M. Role of microbiota in sexually dimorphic immunity. Front Immunol. 2018;9:1018. doi: 10.3389/fimmu.2018.01018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaliannan K, Robertson RC, Murphy K, Stanton C, Kang C, Wang B, et al. Estrogen-mediated gut microbiome alterations influence sexual dimorphism in metabolic syndrome in mice. Microbiome. 2018;6(1):205. doi: 10.1186/s40168-018-0587-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Markle JG, Frank DN, Mortin-Toth S, Robertson CE, Feazel LM, Rolle-Kampczyk U, et al. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013;339(6123):1084–1088. doi: 10.1126/science.1233521. [DOI] [PubMed] [Google Scholar]
- 13.Santos-Marcos JA, Haro C, Vega-Rojas A, Alcala-Diaz JF, Molina-Abril H, Leon-Acuna A, et al. Sex differences in the gut microbiota as potential determinants of gender predisposition to disease. Mol Nutr Food Res. 2019;63(7):e1800870. doi: 10.1002/mnfr.201800870. [DOI] [PubMed] [Google Scholar]
- 14.Delgado-Lista J, Alcala-Diaz JF, Torres-Pena JD, Quintana-Navarro GM, Fuentes F, Garcia-Rios A, et al. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): a randomised controlled trial. Lancet. 2022;399(10338):1876–1885. doi: 10.1016/S0140-6736(22)00122-2. [DOI] [PubMed] [Google Scholar]
- 15.Delgado-Lista J, Perez-Martinez P, Garcia-Rios A, Alcala-Diaz JF, Perez-Caballero AI, Gomez-Delgado F, et al. CORonary Diet Intervention with Olive oil and cardiovascular PREVention study (the CORDIOPREV study): Rationale, methods, and baseline characteristics: a clinical trial comparing the efficacy of a Mediterranean diet rich in olive oil versus a low-fat diet on cardiovascular disease in coronary patients. Am Heart J. 2016;177:42–50. doi: 10.1016/j.ahj.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santos-Marcos JA, Barroso A, Rangel-Zuniga OA, Perdices-Lopez C, Haro C, Sanchez-Garrido MA, et al. Interplay between gonadal hormones and postnatal overfeeding in defining sex-dependent differences in gut microbiota architecture. Aging (Albany NY) 2020;12(20):19979–20000. doi: 10.18632/aging.104140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet CC, Al-Ghalith GA, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019;37(8):852–857. doi: 10.1038/s41587-019-0209-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJ, Holmes SP. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13(7):581–583. doi: 10.1038/nmeth.3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammer Ø, Harper DAT, Ryan PD. PAST: paleontological statistics software package for education and data analysis. Palaeontol Electron. 2001;4(1):9. [Google Scholar]
- 20.Lozupone C, Knight R. UniFrac: a new phylogenetic method for comparing microbial communities. Appl Environ Microbiol. 2005;71(12):8228–8235. doi: 10.1128/AEM.71.12.8228-8235.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bokulich NA, Kaehler BD, Rideout JR, Dillon M, Bolyen E, Knight R, et al. Optimizing taxonomic classification of marker-gene amplicon sequences with QIIME 2's q2-feature-classifier plugin. Microbiome. 2018;6(1):90. doi: 10.1186/s40168-018-0470-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quast C, Pruesse E, Yilmaz P, Gerken J, Schweer T, Yarza P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590. doi: 10.1093/nar/gks1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12(6):R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Douglas GM, Maffei VJ, Zaneveld JR, Yurgel SN, Brown JR, Taylor CM, et al. PICRUSt2 for prediction of metagenome functions. Nat Biotechnol. 2020;38(6):685–688. doi: 10.1038/s41587-020-0548-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parks DH, Tyson GW, Hugenholtz P, Beiko RG. STAMP: statistical analysis of taxonomic and functional profiles. Bioinformatics. 2014;30(21):3123–3124. doi: 10.1093/bioinformatics/btu494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang L, Wang S, Zhang Q, He C, Fu C, Wei Q. The role of the gut microbiota in health and cardiovascular diseases. Mol Biomed. 2022;3(1):30. doi: 10.1186/s43556-022-00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sawicka-Smiarowska E, Bondarczuk K, Bauer W, Niemira M, Szalkowska A, Raczkowska J, et al. Gut microbiome in chronic coronary syndrome patients. J Clin Med. 2021;10:21. doi: 10.3390/jcm10215074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valentini V, Silvestri V, Bucalo A, Marraffa F, Risicato M, Grassi S, et al. A possible link between gut microbiome composition and cardiovascular comorbidities in psoriatic patients. J Pers Med. 2022;12:7. doi: 10.3390/jpm12071118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menni C, Lin C, Cecelja M, Mangino M, Matey-Hernandez ML, Keehn L, et al. Gut microbial diversity is associated with lower arterial stiffness in women. Eur Heart J. 2018;39(25):2390–2397. doi: 10.1093/eurheartj/ehy226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cani PD, Moens de Hase E, Van Hul M. Gut microbiota and host metabolism: from proof of concept to therapeutic intervention. Microorganisms. 2021;9(6):1302. doi: 10.3390/microorganisms9061302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang X, Liu H, Li Y, Huang S, Zhang L, Cao C, et al. Altered gut bacterial and metabolic signatures and their interaction in gestational diabetes mellitus. Gut Microbes. 2020;12(1):1–13. doi: 10.1080/19490976.2020.1840765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen J, Wright K, Davis JM, Jeraldo P, Marietta EV, Murray J, et al. An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Med. 2016;8(1):43. doi: 10.1186/s13073-016-0299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Picchianti-Diamanti A, Panebianco C, Salemi S, Sorgi ML, Di Rosa R, Tropea A, et al. Analysis of gut microbiota in rheumatoid arthritis patients: disease-related dysbiosis and modifications induced by etanercept. Int J Mol Sci. 2018;19:10. doi: 10.3390/ijms19102938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Agca R, Smulders Y, Nurmohamed M. Cardiovascular disease risk in immune-mediated inflammatory diseases: recommendations for clinical practice. Heart. 2022;108(1):73–79. doi: 10.1136/heartjnl-2019-316378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Musa MA, Kabir M, Hossain MI, Ahmed E, Siddique A, Rashid H, et al. Measurement of intestinal permeability using lactulose and mannitol with conventional five hours and shortened two hours urine collection by two different methods: HPAE-PAD and LC-MSMS. PLoS ONE. 2019;14(8):e0220397. doi: 10.1371/journal.pone.0220397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scanlan PD, Shanahan F, Marchesi JR. Culture-independent analysis of desulfovibrios in the human distal colon of healthy, colorectal cancer and polypectomized individuals. FEMS Microbiol Ecol. 2009;69(2):213–221. doi: 10.1111/j.1574-6941.2009.00709.x. [DOI] [PubMed] [Google Scholar]
- 37.Feng Z, Long W, Hao B, Ding D, Ma X, Zhao L, et al. A human stool-derived Bilophila wadsworthia strain caused systemic inflammation in specific-pathogen-free mice. Gut Pathog. 2017;9:59. doi: 10.1186/s13099-017-0208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang Y, Zhang X, Chen D, Lu J, Gong Q, Fang J, et al. Causal associations between gut microbiome and cardiovascular disease: a Mendelian randomization study. Front Cardiovasc Med. 2022;9:971376. doi: 10.3389/fcvm.2022.971376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gutierrez-Calabres E, Ortega-Hernandez A, Modrego J, Gomez-Gordo R, Caro-Vadillo A, Rodriguez-Bobada C, et al. Gut microbiota profile identifies transition from compensated cardiac hypertrophy to heart failure in hypertensive rats. Hypertension. 2020;76(5):1545–1554. doi: 10.1161/HYPERTENSIONAHA.120.15123. [DOI] [PubMed] [Google Scholar]
- 40.Luedde M, Winkler T, Heinsen FA, Ruhlemann MC, Spehlmann ME, Bajrovic A, et al. Heart failure is associated with depletion of core intestinal microbiota. ESC Heart Fail. 2017;4(3):282–290. doi: 10.1002/ehf2.12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kazemian N, Mahmoudi M, Halperin F, Wu JC, Pakpour S. Gut microbiota and cardiovascular disease: opportunities and challenges. Microbiome. 2020;8(1):36. doi: 10.1186/s40168-020-00821-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Troseid M, Andersen GO, Broch K, Hov JR. The gut microbiome in coronary artery disease and heart failure: current knowledge and future directions. EBioMedicine. 2020;52:102649. doi: 10.1016/j.ebiom.2020.102649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang Z, Mei X, Jiang Y, Chen T, Zhou Y. Gut microbiota in heart failure patients with preserved ejection fraction (GUMPTION Study) Front Cardiovasc Med. 2021;8:803744. doi: 10.3389/fcvm.2021.803744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lakshmanan AP, Al Zaidan S, Bangarusamy DK, Al-Shamari S, Elhag W, Terranegra A. Increased relative abundance of ruminoccocus is associated with reduced cardiovascular risk in an obese population. Front Nutr. 2022;9:849005. doi: 10.3389/fnut.2022.849005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nakajima A, Mitomo S, Yuki H, Araki M, Seegers LM, McNulty I, et al. Gut microbiota and coronary plaque characteristics. J Am Heart Assoc. 2022;11(17):e026036. doi: 10.1161/JAHA.122.026036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rahman MM, Islam F, Or-Rashid MH, Mamun AA, Rahaman MS, Islam MM, et al. The gut microbiota (microbiome) in cardiovascular disease and its therapeutic regulation. Front Cell Infect Microbiol. 2022;12:903570. doi: 10.3389/fcimb.2022.903570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Functional characterization between CHD patients according to the sex based on PICRUSt2 analysis. CHD: coronary heart disease patients. Bar chart showing the functional difference between CHD men and CHD women. Data were compared by two-sided Welch’s t-test and filtered for false discoveries using the Benjamini–Hochberg method by using the STAMP software.
Additional file 2: Table S1. Functional characterization. Correspondence between BioCyc ID and MetaCyc Pathway nomenclature.
Data Availability Statement
Collaborations with the Cordioprev Study are open to Biomedical Institutions, always after an accepted proposal for scientific work. Depending on the nature of the collaboration, electronic data, hard copy data, or biological samples should be provided. All collaborations will be made after a collaboration agreement. Terms of the collaboration agreement will be specific for each collaboration, and the extent of the shared documentation (i.e., deidentified participant data, data dictionary, biological samples, hard copy, or other specified data sets) will be also specifically set on the light of each work.