Abstract
Background:
The association of historical redlining policies—a marker of structural racism—with contemporary heart failure (HF) risk among Black and White individuals is not well-established.
Methods:
We aimed to evaluate the association of redlining with the risk of HF among White and Black race Medicare beneficiaries. Zip-code level redlining was determined by the proportion of historically redlined areas using the Mapping Inequality Project within each Zip-code. The association between higher Zip-code redlining proportion (Quartile 4 vs. Quartiles 1–3) and HF risk were assessed separately among Black and White Medicare beneficiaries using generalized linear mixed models adjusted for potential confounders, including measures of Zip-code level Social Deprivation Index (SDI).
Results:
2,388,955 Medicare beneficiaries (Black N=801,452; White N=1,587,503; mean age: 71 years; men: 44.6%) were included. Among Black beneficiaries, living in Zip-codes with higher redlining proportion (Q4 vs. Q1-3) was associated with increased risk of HF after adjusting for age, sex, and comorbidities (RR [95% CI]: 1.08 [1.04–1.12], P<0.001). This association remained significant after further adjustment for area-level SDI (RR [95% CI]: 1.04 [1.002–1.08], P=0.04). A significant interaction was observed between redlining proportion and SDI (P-interaction<0.01) such that higher redlining proportion was significantly associated with HF risk only among socioeconomically distressed regions (above median SDI). Among White beneficiaries, redlining was associated with a modestly lower risk of HF after adjustment for age, sex, and comorbidities (RR [95% CI]: 0.94 [0.89–0.99], P=0.02).
Conclusions:
Historical redlining is associated with an increased risk of HF among Black patients. Contemporary Zip-code level SDOH modifies the relationship between redlining and HF risk, with the strongest relationship between redlining and HF observed in the most socioeconomically disadvantaged communities.
Keywords: Redlining policies, socioeconomic distress, structural racism, racial disparities, heart failure
INTRODUCTION
Heart failure (HF) affects 6.2 million people in the US and disproportionately impacts individuals of Black race.1 Black patients are diagnosed at earlier ages, have worse health status, and are more frequently hospitalized than their White counterparts.1–4 These racial disparities have been attributed to differences in access to healthcare and exposure to adverse social determinants of health (SDOH), though their relationship to upstream macro-social factors is not well understood.5,6
Structural racism—which encompasses “historical, cultural, institutional and interpersonal” discriminatory practices against Black and other underrepresented racial and ethnic communities—underlies race-related health disparities in the US and has been identified by the American Heart Association as a key target of research aimed to address disparities in cardiovascular health.7 However, the pervasive nature of structural racism has resulted in challenges in studying and quantifying its effects on health.
In this setting, the study of “redlining”, discriminatory housing practices enacted in the 1930s, may help explain the persistent impacts of structural racism on health among Black and other minoritized individuals today. Many present-day differences in neighborhood environments can be attributed to such policies that became institutionalized following the US Federal Government’s creation of the Home Owners’ Loan Corporation (HOLC), which graded neighborhoods across an investment risk spectrum based on neighborhood racial and ethnic makeup.8,9 Redlining practices led to the designation of neighborhoods with a high proportion of Black and other underrepresented racial and ethnic groups as high-risk areas for investment (indicated in red in HOLC maps), leading to systematic disinvestment in communities of color and denial of mortgages and homeownership to generations of Black adults and individuals of other racial minority groups.10,11 Despite the passage of the Fair Housing Act of 1968 to combat the practice of redlining, contemporary data demonstrate that historically redlined neighborhoods continue to experience more poverty, urban violence, poorer air quality, less resilient housing markets, and less access to fresh foods than non-redlined neighborhoods.12,13 Furthermore, residents of historically redlined communities have been demonstrated to have shorter life expectancies and worse cardiovascular health than their counterparts, reflecting the persisting impacts of structural racism on health.14,15
Racial disparities in HF incidence and outcomes have been attributed to differences in exposure to risk factors for HF and socioeconomic disadvantage. However, the contribution of structural discrimination as captured in redlining practices to racial disparities in HF incidence has not previously been described.16 Moreover, the extent to which this relationship is explained by current SDOH factors has not been evaluated. Accordingly, we examined the association of historical redlining with the incidence of HF among Medicare beneficiaries after adjustment for known confounding by risk factor burden. We additionally assessed interactions by contemporary area-level measures of SDOH to assess the degree to which such factors modify the relationship between historical redlining and contemporary health outcomes.
METHODS
Data used for the study are covered under a data use agreement with the Centers for Medicare and Medicaid Services and are not available for distribution by the authors, but they may be obtained with an approved data use agreement.
Study cohort
We identified self-reported non-Hispanic White and non-Hispanic Black beneficiaries with available residential Zip-codes from the Medicare Beneficiary Summary Files between 2014 and 2019 and linked their data with the available Zip-code level redlining data (N=1044 Zip-codes).17 Individuals of other races were excluded due to low numbers available for analysis within the Medicare cohort for Zip-code level analysis. Beneficiaries with a history of HF or myocardial infarction in the preceding two years, less than two years of Medicare coverage before the study start date, or who were enrolled in a Medicare Advantage plan, and who were younger than 40 years were excluded. At the Zip-code level, 2922 Zip-codes had available data on redlining. Of these, we excluded Zip-codes that had greater than 50% missingness of HOLC scores (N=1833), significant overlap of A and D HOLC areas in the same Zip-code (N=21) (see description below), and those with fewer than 10 beneficiaries from a specific race (N=24), resulting in a total of 1044 Zip-codes included in the final analysis. Of note, because some Zip-codes contained White beneficiaries only (N=23) or Black beneficiaries only (N=2), the total number of Zip-codes included varied by race group in the final analysis. The detailed cohort derivation for our study is shown in eFigure-1. Medicare Beneficiary Summary Files were used to extract patients’ age, sex, self-reported race, enrollment dates and residential Zip-codes. A lookback period of two years was used to determine patients’ comorbidities based on all international classification of diseases (ICD) codes submitted in any claim and using Elixhauser’s method.18,19 Developed and validated in administrative datasets, the Elixhauser’s Comorbidity Index uses a comprehensive set of 30 comorbidity measures to provide a weighted index score which may impact the risk of hospitalization and mortality in longitudinal studies.19 The Institutional Review Board at the Cleveland Clinic approved the study with waiver of informed consent.
Zip-code level redlining measures
Primary measure (Zip-code level redlining proportion):
The primary exposure of interest was beneficiary residential Zip-code redlining proportion, defined as the percentage of a given Zip-code exposed to historical redlining practices at the date of enrollment. The redlining proportion was obtained from The Mapping Inequality Project.17 In summary, HOLC mortgage security risk maps from the 1930s were digitized and overlaid with 2010 census tracts using ArcGIS. Within each Zip-code, the proportion of HOLC risk category-D (corresponding to “Hazardous” census tracts and indicated by red in historical maps) was calculated as a ratio of total Zip-code area. Because modern Zip-code boundaries do not exactly overlay 1930s census tract maps, it was possible for a single census tract to contribute HOLC grades to multiple Zip-codes, and for a single Zip-code to be comprised of multiple census tracts. As a result, it was common for a single Zip-code to receive contributions from multiple census tracts of different HOLC residential security grades. Furthermore, because not all areas within a Zip-code received a corresponding HOLC-graded census tract, it was possible for a single Zip-code to have a large degree of HOLC score missingness. Given the possibility of a high degree of missingness within a single Zip-code, we excluded Zip-codes that had greater than 50% missingness of HOLC scores as described above. The proportion of category D census tracts within each Zip-code was assessed continuously and categorically as quartiles, with quartile 4 representing the highest proportion of redlined area at the Zip-code level.
Secondary measure (weighted mean HOLC score):
We additionally calculated Zip-code level HOLC scores by using the weighted mean of HOLC residential security grades and the relative area within each Zip-code boundary to evaluate consistency in our results across different approaches to measuring redlining at the Zip-code level. In this approach, each HOLC risk category was assigned a numeric value as follows: (grade-A “Best”: 1), (grade-B “Still Desirable”: 2), (grade-C “Definitely Declining”: 3), and (grade-D “Hazardous”: 4). For example, if a Zip-code was comprised of two census tracts of equal size of 50%, with one contributing grade-A (1 point) and one contributing grade-B (2 points), the Zip-codes would receive a HOLC score of 1.5. As a second example, if a Zip-code had one grade-A census tract contributing 35%, one grade-B census tract contributing 35%, and 30% missing data, the weighted HOLC score would be calculated only using the known data, thus resulting in a score 1.5. We excluded Zip-codes which had both grade-A and grade-D census tracts contributing, as the weighted mean scores are not representative of the true degree of redlining occurring within the Zip-code. Zip-codes were then stratified into quartiles based on HOLC score, where Q4 indicated the highest HOLC score (most hazardous or least desirable neighborhoods).
Zip-code-level SDOH parameters
Residential Zip-codes for Medicare beneficiaries were linked to an index of Zip-code-level socioeconomic deprivation. The Social Deprivation Index (SDI) is a composite measure of Zip-code-level deprivation based on 7 demographic characteristics collected in the American Community Survey including poverty rate, education, employment, housing (percentage living in rented or crowded housing units), household characteristics (single-parent households), and access to transportation. Scores range from 0–100 and represent percentile rank in relation to other surveyed Zip-codes, with higher scores corresponding to higher socioeconomic distress. For the present analysis, high versus low socioeconomic deprivation at the Zip-code level was identified using data-derived median thresholds.
Study outcomes
The key outcome of interest was incident HF as identified by hospitalization with a primary diagnosis of HF through December 2019. The primary diagnosis of HF was determined as admission to the hospital with ICD-9 (428.*, 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93) or ICD-10 codes (I50.*, I11.0, I13.0, I13.2), consistent with prior approaches.20 Patients were followed and censored at the time of event, death, Medicare dis-enrollment, or end of the study.
To assess the robustness of the observed association between redlining and HF, a falsification endpoint analysis was also performed for the outcome of hip fracture as defined by hospitalization with primary diagnosis codes for hip fracture (ICD-9 Code: 820*, 821 or ICD-10 code: S72*).
Statistical Methods
The unit of analysis for the present study was Zip-code. As described above, redlining was assessed continuously as the category D census tracts proportion of the total Zip-code area (0–100%) and by quartiles, where quartile 4 reflected “redlined Zip-codes” with the highest proportion of redlined area within a Zip-code and quartiles 1–3 representing “non-redlined Zip-codes” with relatively low levels of redlining. We evaluated Zip-code level patient and neighborhood SDOH characteristics (SDI scores) in redlined and non-redlined Zip-codes. Patient characteristics were reported for each as the median (25th and 75th percentile) of the Zip-code-level proportions (for categorical patient characteristics) and Zip-code-level median (25th, 75th percentile) of Zip-code-level means (for continuous patient characteristics) and compared across the 2 groups using the Kruskal-Wallis test. Crude incidence rates of HF among beneficiaries of Black and White race were calculated for redlined and non-redlined Zip-codes. The association between residing in redlined Zip-codes (Q4) vs. the other three quartiles (Q1-Q3) and risk of HF was assessed by constructing generalized linear mixed models using Poisson distribution and log link, with new onset HF as the outcome, patient characteristics as a fixed effect, Zip-code as a random intercept, and the log time in follow up to the event, death or censoring as an offset term. The models were constructed separately among Black and White beneficiaries considering the well-established differences in the experience of structural racism and adverse SDOH burden among Black vs. White race individuals. The models were adjusted for the following covariates, Model-1: age, sex; Model-2: age, sex, and comorbidities defined by the Elixhauser algorithm. The association between continuous redlining proportion and risk of HF was also assessed using similar models and restricted cubic splines with adjustment for age, sex, and comorbidities (3 knots).
To evaluate the contribution of Zip-code level SDOH parameters toward the association between redlining and HF risk, additional models were constructed including variables in Model-2 and SDI score (Model-3). There was no evidence of collinearity between redlining proportion and SDI (variance inflation factor=1.4). We evaluated the proportional contribution of neighborhood-level SDOH factors to the observed association between redlining and HF risk by evaluating the change in the parameter estimate with and without adjustment for SDI.21 Interaction between SDI score and redlining status was assessed in Model-3. If significant interaction was noted, SDI-stratified (above and below median) analysis was performed to evaluate the association of redlining with incident HF across strata of SDI in each race group separately, adjusting for age, sex, and comorbidities.
We additionally repeated primary analyses assessing the relationship of redlining with the risk of HF using an alternate measure of redlining incorporating all HOLC grades to generate a continuous HOLC score for each Zip-code. The association between living in Zip-codes with high HOLC score (Q4 vs. Q1-3) and the risk of HF was assessed separately among Black and White beneficiaries using the models described above. Finally, we conducted falsification endpoint analyses evaluating the association of categorical and continuous measures of the Zip-code proportion with risk of hip fractures using adjusted generalized mixed models and restricted cubic splines with the same adjustments as Model-2. The analysis was performed using SAS version 9.4 (SAS Institute, Inc, Cary, NC), R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria), and GraphPad Prism version 8. A 2-sided P value <0.05 was considered statistically significant.
RESULTS
Baseline Characteristics
The study included 2,388,955 Medicare beneficiaries (Black race N=801,452; White race N=1,587,503; mean[SD] age=71.2[11.6]; men=44.6%) with a median follow-up time of 6 years (total follow-up 12,427,571 person-years). The median Zip-code-level redlining proportion varied by quartile, with redlined Zip-codes reflecting 78.3% (IQR: 61.0, 97.2%) redlined proportion in the highest quartile versus only 3.4% (IQR: 0, 17.6%) in the lower three quartiles in non-redlined Zip-codes. Black (vs. White) beneficiaries in the study were younger and more commonly lived in redlined Zip-codes (27.7% vs. 15.8%). Black beneficiaries residing in redlined (vs. non-redlined) Zip-codes demonstrated a higher prevalence of some comorbidities, including COPD, CKD, and anemia (Table-1). White beneficiaries residing in redlined (vs. non-redlined) Zip-codes also had a higher prevalence of comorbidities such as diabetes, hypertension, anemia, CKD, and liver disease (Table-1). Among both White and Black Medicare beneficiaries, SDI scores were higher in redlined Zip-codes as compared to non-redlined Zip-codes (Table-1). There was a modest correlation between redlining proportion and SDI scores (r=0.40) in the overall study cohort.
Table 1:
Patient characteristics of White and Black Medicare beneficiaries across redlining quartiles.
| Black race (N=801,452) | White race (N=1,587,503) | |||||
|---|---|---|---|---|---|---|
| Not redlined Q1-Q3 | Redlined Q4 |
P value | Not redlined Q1-Q3 | Redlined Q4 |
P value | |
|
Percent redlined area (median, 25th-75th) |
3.6 (0–18.3) | 78.2 (61. 0–96.2) | 3.4 (0–17.6) | 78.3 (61–96.7) | ||
| Number of Zip-codes | 765 | 256 | 783 | 259 | ||
| Number of Beneficiaries | 579,767 | 221,685 | 1,337,330 | 250,173 | ||
| SDI (median, 25th-75th) | 77 (47.5–92) | 95 (81–98) | <0.001 | 75.5 (46–92) | 94 (80–98) | <0.001 |
| Zip-code Level Patient Characteristics [median (25th-75th percentile)] | ||||||
| Age, years | 67.6 (64.9–70) | 67.9 (65.6–69.3) | 0.8 | 72.5 (70.4–74) | 70.5 (68.1–72.4) | <0.001 |
| Male (%) | 46 (42.1–52) | 47.1 (43.3–51.8) | 0.2 | 45.2 (43–48) | 49.2 (45.2–53.5) | <0.001 |
| Diabetes (%) | 8.8 (7.2–10.6) | 9.1 (8–10.5) | 0.07 | 5.3 (3.9–6.8) | 6.4 (4.4–8.7) | <0.001 |
| Hypertension (%) | 18.8 (16.3–22) | 19.3 (17.2–21.9) | 0.07 | 15.6 (13.6–17.9) | 16.2 (13.4–20) | 0.03 |
| Anemia (%) | 7.3 (5.7–9.1) | 7.6 (6.3–9) | 0.03 | 4.9 (4–6.1) | 5.6 (4.3–7.3) | <0.001 |
| CKD (%) | 4.6 (3.5–5.7) | 4.9 (4.2–5.8) | 0.006 | 2.4 (1.9–2.9) | 2.6 (1.9–3.5) | 0.006 |
| COPD (%) | 5.9 (4.2–7.7) | 6.4 (5.1–7.6) | 0.004 | 5.2 (3.8–7.4) | 6.8 (4.5–10.2) | <0.001 |
| CAD (%) | 4 (3–5.2) | 4 (3.1–5) | 0.7 | 4.7 (3.8–5.7) | 4.5 (3.6–6.1) | 0.9 |
| Liver disease (%) | 1.1 (0.6–1.8) | 1.3 (0.8–1.8) | 0.03 | 0.9 (0.6–1.4) | 1.3 (0.8–2.1) | <0.001 |
| Stroke (%) | 1.6 (1–2.2) | 1.5 (1–2) | 0.1 | 1.4 (1.0–1.7) | 1.3 (0.9–2) | 0.6 |
| Prior pacemaker (%) | 0.3 (0–0.5) | 0.3 (0–0.5) | 0.08 | 0.6 (0.4–0.8) | 0.6 (0.2–0.8) | 0.006 |
| Peripheral vascular disease (%) | 2 (1.4–2.7) | 2.2 (1.7–2.7) | 0.03 | 1.9 (1.4–2.4) | 2 (1.4–2.7) | 0.07 |
| Valvular disease (%) | 0.8 (0.3–1.3) | 0.8 (0.6–1.3) | 0.5 | 1.5 (1.2–2) | 1.4 (0.9–1.7) | <0.001 |
| Metastatic tumor (%) | 0.5 (0–0.7) | 0.5 (0.3–0.8) | 0.003 | 0.5 (0.4–0.7) | 0.5 (0.2–0.7) | 0.06 |
| Tumor without metastasis (%) | 1.2 (0.6–1.6) | 1.1 (0.7–1.5) | 0.3 | 1.2 (1–1.5) | 1.2 (0.8–1.6) | 0.3 |
Redlining quartiles 1–3 represents non-redlined Zip-codes, while quartile 4 reflect Zip-codes with the highest proportion of redlined census tracts.
Patient characteristics are reported as the median (25th-75th percentile) of the Zip-code-level proportions (for categorical patient characteristics) and median (25th-75th percentile) of Zip-code-level means (for continuous patient characteristics).
Abbreviations: SDI - Social Deprivation Index; CKD - chronic kidney disease; COPD - chronic obstructive pulmonary disease; CAD - coronary artery disease.
Association of Redlining with Risk of HF among Beneficiaries of Black and White Race
Among Black beneficiaries, the unadjusted cumulative incidence of HF was higher among those living in redlined (vs. non-redlined) Zip-codes (1035 vs. 992 events per 100,000 person-years). In age and sex-adjusted analysis, living in Zip-codes with higher redlining proportion (Q4 vs. Q1-3) was significantly associated with a higher risk of HF (RR[95%CI]: 1.09[1.05–1.13] P<0.001, Model-1). This association persisted after adjusting for comorbidities (RR[95%CI]: 1.08[1.04–1.12] P<0.001, Model-2 Table-2). Similar patterns of association were observed using a continuous measure of redlining proportion with a higher risk of HF among beneficiaries living in areas with a greater proportion of redlining (RR[95% CI]: 1.04[1.03–1.06], P<0.001) (Figure-1, Table S1).
Table 2:
Adjusted association between Zip-code-level redlining proportion with the risk of heart failure in White and Black beneficiaries.
| Beneficiaries of Black Race | Beneficiaries of White Race | |||
|---|---|---|---|---|
| RR (95% CI) | P Value | RR (95% CI) | P-Value | |
| Model 1 | 1.09 (1.05–1.13) | <0.001 | 0.94 (0.88–0.99) | 0.02 |
| Model 2 | 1.08 (1.04–1.12) | <0.001 | 0.94 (0.89–0.99) | 0.02 |
| Model 3 | 1.04 (1.002–1.08) | 0.04 | 0.90 (0.85–0.95) | <0.001 |
Zip-code-level redlining proportion assessed categorically as Quartile 4 (highest proportion of redlined area) compared to Quartiles 1–3 (reference, lowest proportion of redlined area).
Model 1 includes age + sex. Model 2 includes model 1 + comorbidities. Model 3 includes age, sex, comorbidities + Social Deprivation Index.
Models are generalized linear models, with patients’ variables as fixed effects, Zip-code as random intercept, with Poisson distribution and log time patient was alive as offset term.
Abbreviations: RR = risk ratio. CI = confidence interval.
Figure 1:
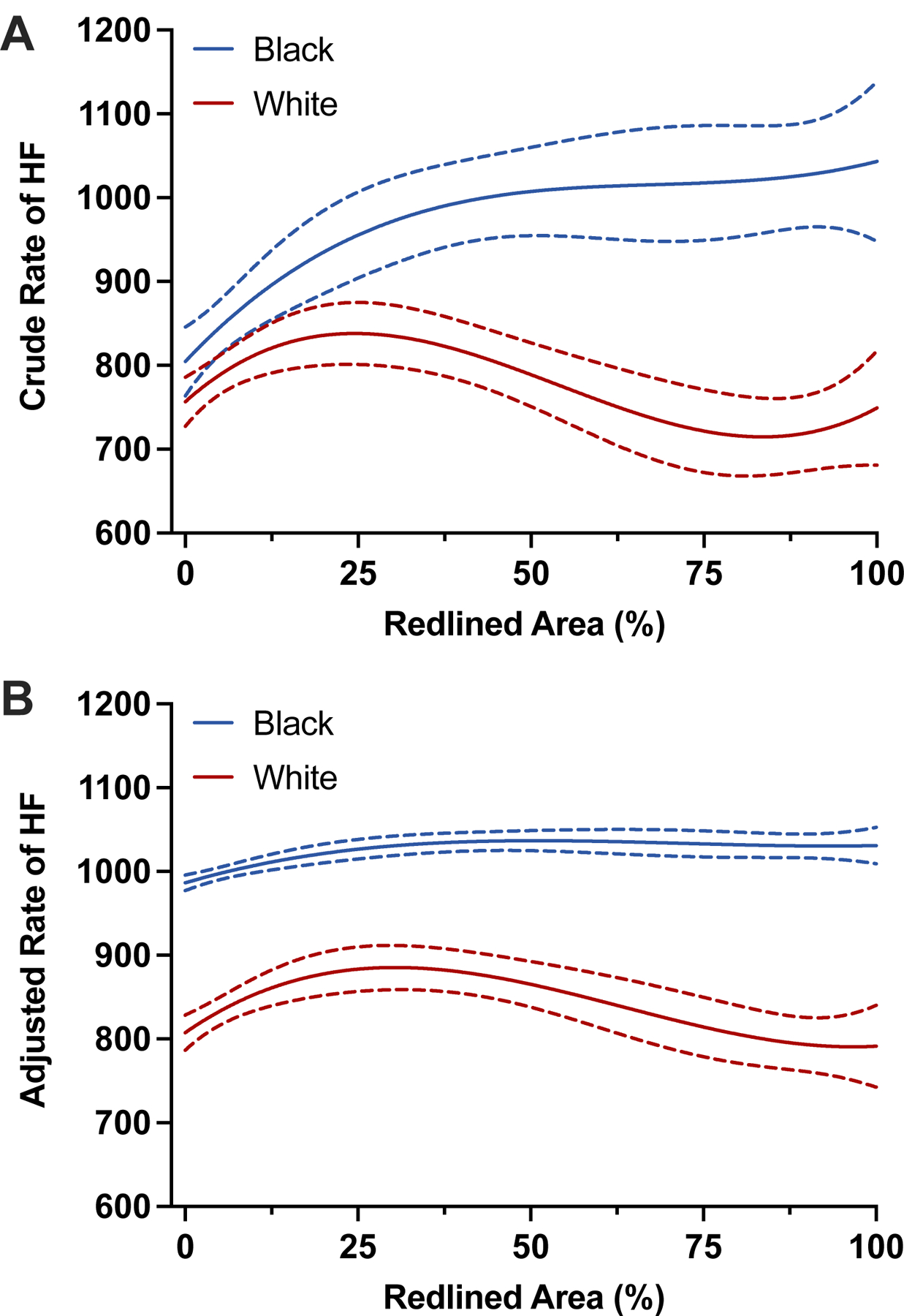
Association between Zip code-level redlining proportion and risk of heart failure
Caption: Spline plots show the relationship between continuous redlining proportion and the crude rate (panel A) and adjusted rate (panel B – adjusted for age, sex, and comorbidity burden) of heart failure among Black (blue) and White (red) beneficiaries. HF rates are calculated per 100,000 person-years.
Among White beneficiaries, the unadjusted cumulative incidence of HF was modestly lower for those living in redlined (vs. non-redlined) Zip-codes (747 vs. 809 events per 100,000 person-years). In adjusted models, living in Zip-codes with high redlining proportion was associated with a modestly lower risk of HF after adjustment for age, sex, and comorbid diseases (Q4 vs. Q3-Q1, RR[95% CI]: 0.94[0.89–0.99], P=0.02, Model-2 Table-2). A similar pattern of results was observed in continuous analysis of redlining with a modest, statistically insignificant association between redlining proportion and risk of HF after adjustment for age, sex, and comorbidity burden (Figure-1, Table S1).
Contribution of Contemporary SDOH to Historical Redlining associated risk of HF
Among Black beneficiaries, the relationship between living in redlined Zip-codes and HF risk attenuated in magnitude but remained statistically significant after adjustment for SDI (RR[95% CI]: 1.04[1.002–1.08], P=0.04, Model-3 Table-2]. A similar pattern of results was noted using continuous measures of redlining proportions (Table S1). SDI accounted for 50% of the association between the highest redlining Zip-codes and HF risk. The interaction between redlining quartile and SDI score was significant for HF among Black beneficiaries (P-interaction<0.001). In stratified analysis by SDI, living in redlined Zip-codes was significantly associated with a higher risk of HF only among socioeconomically distressed regions (above median SDI) but not for Zip-codes with SDI below the median levels. Figure-2, Table-3). In the fully adjusted model with the continuous redlining score, redlining remained significantly associated with HF risk in Black beneficiaries after adjusting for SDI score, though the relationship was attenuated (RR[95% CI]: 1.02[1.01–1.04], P=0.004, Model-3 Table S1).
Figure 2:

Association between Zip code-level redlining proportion and risk of heart failure among individuals above and below median Social Deprivation Index (SDI) score
Caption: Spline curves demonstrating the risk of HF among White (panel A) and Black (panel B) Medicare beneficiaries among those above the median SDI (blue) or below the median SDI (red). The models are adjusted for age, sex, and comorbidities. HF rates are calculated per 100,000 person-years.
Table 3:
Association between the categorical measure of Zip-code-level redlining proportion (Q4 vs. Q1-3) and risk of heart failure across strata (above and below median) of Social Deprivation Index scores.
| Black beneficiaries | White beneficiaries | |||||
|---|---|---|---|---|---|---|
| RR (95% CI) | P value | P-interaction | RR (95% CI) | P value | P-interaction | |
| Below Median SDI | 1.03 (0.98–1.09) | 0.2 | <0.001 | 0.82 (0.74–0.91) | <0.001 | 0.002 |
| Above Median SDI | 1.05 (1.00–1.10) | 0.05 | 0.92 (0.87–0.98) | 0.01 | ||
Separate models were constructed for beneficiaries of Black and White race and for each stratum of Social Deprivation Index. Models were adjusted for age, sex, and comorbidities.
Abbreviations: SDI – Social Deprivation Index, RR – Risk Ratio, CI – Confidence Interval.
White participants living in redlined Zip-codes had a modestly lower risk of HF after accounting for SDI [RR[95% CI]: 0.90[0.85–0.95], P<0.001, Model-3 Table-2]. The interaction between redlining categories and SDI score was also significant for the risk of HF among White beneficiaries (P-interaction=0.002). In stratified analysis by SDI strata, higher redlining proportions were associated with a lower risk of HF across both SDI strata, with a stronger association noted among Zip-codes with the lowest levels of socioeconomic distress (Figure-2, Table-3).
Association of HOLC score and risk of HF
We additionally evaluated the relationship between the weighted mean HOLC score and the risk of HF, where the Q4 Zip-code corresponded to communities deemed more hazardous by HOLC grading, and Q1-3 corresponded to more desirable communities based on the HOLC grading. Consistent with primary analysis, among Black adults, higher HOLC score was significantly associated with a higher risk of HF after adjustment for age, sex, and comorbidities (Q4 vs. Q1-3, RR[95%CI]: 1.08[1.04–1.12], P<0.001, Model-2 Table S2]. This association was attenuated but remained significant after further adjustment for the SDI score. Among White beneficiaries, a higher HOLC score was associated with a modestly lower risk of HF in the most adjusted model (Table S2).
Falsification Endpoint analysis
We observed no significant association between redlining and incidence of hip fracture at the Zip-code level among Black patients when adjusting for age, sex, and comorbidities (Black race: RR[95% CI]: 1.04[0.98–1.10], P=0.2). Among White patients, a modest inverse relationship was observed between Zip-code level redlining and risk of hip fractures (White race: RR[95%CI]: 0.95[0.92–0.99], P=0.01) (Table S3).
DISCUSSION
In this study, we observed several important findings. Notably, more than a quarter of Black beneficiaries resided in historically redlined areas, compared to only 15.7% of White beneficiaries. Among Black Medicare beneficiaries, living in Zip-codes with a high proportion of redlining area was significantly associated with a higher risk of HF. This association was largely driven by the higher burden of adverse SDOH in Zip-codes with high levels of redlining, though the relationship between redlining and HF risk was strongest among Black beneficiaries living in the most socially disadvantaged Zip-codes. Furthermore, the association between living in communities with more redlining and the risk of HF persisted after adjustment for cardiovascular risk factors and socioeconomic risk factors among Black beneficiaries, highlighting the unique contribution of discriminatory redlining practices on the risk of HF among Black adults decades later. In contrast, among White beneficiaries, a modest inverse relationship was observed between higher Zip-code level proportion of redlining and risk of HF.
This study builds upon a growing body of literature implicating structural racism and racist policies in modern disparities in health. Prior work has demonstrated that Black individuals residing in historically redlined communities are exposed to greater levels of environmental pollutants, residential segregation, and reduced access to green spaces and health services.22–26 In turn, associations between historical redlining and health have been observed starting at birth and extending throughout individuals’ lifespans with an increased risk of asthma, cancer, higher post-operative mortality and complication rates, and reduced life expectancy.15,22,27–30 Moreover, a recent study by Mujahid et al. evaluated the impacts of historical redlining on cardiovascular health and found that Black individuals living in historically redlined communities had lower cardiovascular health scores and reported more adverse health behaviors and risk factors than those living in areas not affected by prior redlining.31
Our findings extend these observations to the risk of HF, whereby we observed an increased risk of HF for Black adults living in Zip-codes where redlining was prevalent. Consistent with prior observations of chronic disinvestment in redlined communities, we observed a greater concentration of socioeconomic distress in redlined Zip-codes that contributed to the relationship between redlining and incident HF risk. This disparity in socioeconomic disadvantage across redlining categories reflects how neighborhood characteristics may drive poorer access to education, employment, wealth, and health and contribute to disparities in healthcare access.32 We also found that adverse SDOH at the Zip-code level accounted for a large proportion of the increased risk of HF among Black individuals living in redlined areas.
However, among Black individuals, in fully adjusted models accounting for a wide array of SDOH, the relationship between redlining and HF risk remained significant, suggesting that the effects of redlining may extend beyond traditional SDOH. Additionally, the highest risk of HF was observed among Black beneficiaries living in redlined Zip-codes with the highest levels of socioeconomic distress, demonstrating how the persisting impacts of redlining may be felt most in the most disadvantaged communities. This residual risk, although modest at the Zip-code level, may be related to the impacts of residential segregation, which has been shown to associate with adverse cardiovascular outcomes in non-Hispanic Black communities, chronic discrimination, disparities in healthcare delivery, and other unmeasured risks.33–35 Prior studies have elucidated how exposure to chronic discrimination may contribute to adverse cardiometabolic health by means of upregulated stress pathways,36 reduced access to healthcare and resources, and increased unhealthy behaviors.34,37 Moreover, persistent gaps in cardiovascular mortality between Black and White adults have been demonstrated in wealthy communities and among highly educated Black men, suggesting that while cardiovascular outcomes may be influenced by socioeconomic disparities, the impact of structural racism on health disparities likely extends beyond the neighborhood and individual wealth.38,39 Notably, the risk conferred by redlining was unique to HF and was not observed for the outcome of hip fractures, supporting the conclusion that the neighborhood environment is of particular importance to cardiovascular health, which may be more influenced by long-term exposure to psychosocial stress, socioeconomic disadvantage, and reduced access to healthcare.
The relationship between redlining and the risk of HF notably varied by race such that the risk of HF among White individuals living in redlined Zip-codes was modestly lower than in non-redlined Zip-codes after adjustment for socioeconomic factors. This observation is consistent with prior literature demonstrating null or protective effects of racial segregation on cardiovascular health among White individuals living in predominantly White neighborhoods, and inter-neighborhood differences that are primarily mediated by differences in socioeconomic factors.31,34 Redlining policies targeted Black and other minoritized individuals by design, limiting the ability of Black families to generate wealth through homeownership and driving a persistent wealth gap by race.40 Furthermore, the modest inverse effect of redlining seen in the most adjusted models for White beneficiaries may reflect the effects of gentrification, leading to an influx of well-educated, high-income White residents with a low cardiovascular morbidity burden to low-income primarily underrepresented racial and ethnic communities, or of competing risk of disease among the most disadvantaged White individuals.
Policy Implications:
Our study has important policy implications. We find that legacies of residential segregation continue to impact disparities in cardiovascular health today, driven and amplified by socioeconomic disadvantage. These findings highlight the need for aggressive social interventions targeting improvement in neighborhood-level SDOH, particularly in disadvantaged communities, to lower the risk of HF. Efforts to expand affordable housing access in historically “desirable” neighborhoods for individuals from low-income and underrepresented racial and ethnic groups and to reinvest in disadvantaged communities through favorable tax benefits or incentives may help to shift historical residential patterns and provide the groundwork for infrastructure growth, particularly within predominantly Black communities. State and local governments should also consider an equitable approach to investing in the public services and goods available to residents of historically redlined areas and initiate policies to protect housing and rental markets in Black communities at risk of gentrification, displacement, and the ensuing disruption of social networks that risk exacerbating underlying disparities in HF risk among Black individuals.41 Finally, healthcare organizations in historically redlined and disadvantaged areas may facilitate access to benefits programs and federal and state tax incentives and offer structured education and mentoring for their constituents to assist in community wealth building and engagement.42
In addition to targeted investment in historically redlined areas, direct policy action aimed at preventing ongoing disparities in lending may be needed. Although the practice of redlining was officially ended by the Fair Housing Act, disparities in lending persist in some parts of the US, and were recently identified by the US Department of Justice as a priority in addressing a growing gap in homeownership between White and Black Americans.43 Policy interventions such as the Community Reinvestment Act of 1977 have aimed to directly address gaps in lending and have helped ease disparities, but enforcement of fair lending practices remains suboptimal and poses an ongoing health risk to future generations of Black and minority Americans.44
Our study has multiple strengths, including the use of a large claims-based dataset reflecting a nationally representative cohort of US adults with validated HF outcomes. Moreover, in this study, we present a novel approach to linking granular outcomes data with existing neighborhood-level measures of structural racism and socioeconomic disparities, providing a unique insight into the relationship between indices of structural racism and health outcomes. This study also has several limitations. First, HOLC scores were only one of the multiple policy approaches used to systematically reduce access to homeownership, credit lines, and insurance for Black individuals. Prior work has found that HOLC maps were neither the first nor the best sources of information about real estate risk levels.8 As such, this measure of redlining likely does not capture the full extent of discriminatory lending policies and serves as only one proxy for assessing the impacts of structural racism. Second, although we present two unique approaches to the measurement of redlining at the Zip-code level with consistency in our findings across both, each represents an approximation of this exposure and cannot exactly quantify redlining, which in practice was conducted at the census-tract level based on century-old zoning maps. Third, our study also has limitations owing to missingness in redlining data at the Zip-code level particularly in rural and less populous regions of the US where redlining maps are either unavailable or current Zip-code designations are subject to missingness. Although this limits the generalizability of our findings to areas where historical redlining maps are available, the study of redlining as a predominantly urban phenomenon is also reflective of the historical reality of this particular form of housing discrimination and captures the persistent effect of this policy on individuals continuing to live in redlined communities. Fourth, though we attempt to adjust for individual comorbidities and established socioeconomic distress indices, we cannot exclude the possibility of residual confounding by unmeasured risks. Fifth, our study is limited in its ability to assess patient-level social factors, thus we are unable to assess prior tenure in a redlined Zip-code or lifetime HF risk associated with redlining. Finally, as the focus of our study was an exploration of structural drivers of HF disparities in the Black population, we did not examine data on differences among other racial and ethnic groups who may have been impacted by discriminatory lending and residential segregation due to inadequate numbers for Zip-code level analysis in the Medicare cohort.
In summary, historical redlining policies differentially affect HF risk by race in the US, with redlining conferring a significantly higher risk of HF among Black individuals. Drivers of historic redlining policies include adverse SDOH factors, but these factors do not fully explain the increased HF risk in Black patients. Future work to further explore the unique impacts of systemic racism on health disparities among Black populations is warranted.
Supplementary Material
CLINICAL PERSPECTIVE.
What is New?
Black patients living in Zip codes exposed to historical redlining practices experience a higher risk of heart failure than those living in non-redlined areas.
The higher risk of heart failure among Black patients living in redlined Zip codes is largely driven by the high burden of adverse social determinants of health. These findings highlight one of the mechanisms by which structural racism has contributed to ongoing disparities in cardiovascular health.
What are the Clinical Implications?
Additional research is needed to understand the individual-level effects of exposure to residential social deprivation and redlining over the course of a lifetime to better identify individuals most in need of social intervention to address HF risk.
Targeted public health policy aimed at addressing residential disparities in HF risk by increasing access to “desirable” neighborhoods for Black individuals and by reinvesting in communities exposed to historical redlining practices is needed to lower the risk of HF in this population and address racial disparities in HF outcomes.
Sources of Funding:
The current research was partly funded by philanthropic gifts by the Haslam Family, Bailey Family, and Khouri family to the Cleveland Clinic (PI: Dr. Desai). Dr. Pandey has received research support from the National Institute on Aging Grant for Early Medical/Surgical Specialists’ Transition To Aging Research Grant (1R03AG067960-01), and the National Institute on Minority Health and Disparities (R01MD017529). Dr. Powell-Wiley is funded by the Division of Intramural Research at the National Heart, Lung, and Blood Institute and the Intramural Research Program of the National Institute on Minority Health and Health Disparities.
ABBREVIATIONS
- HF
heart failure
- SDOH
social determinants of health
- HOLC
Home Owners’ Loan Corporation
- ICD
International Classification of Diseases
- SDI
Social Deprivation Index
Footnotes
Disclosures: Dr. Desai is a consultant for Medtronic and Bristol Myers Squibb. He is on the executive steering committee of a trial sponsored by Bristol Myers Squibb. Dr. Pandey has received grant funding outside the present study from Applied Therapeutics and Gilead Sciences; has received honoraria outside of the present study as an advisor/consultant for Tricog Health Inc and Lilly, USA, Rivus, and Roche Diagnostics, and has received nonfinancial support from Pfizer and Merck. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institute on Minority Health and Health Disparities; the National Institutes of Health; or the U.S. Department of Health and Human Services. The remaining authors have nothing to disclose.
REFRENCES
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 2.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khariton Y, Nassif ME, Thomas L, Fonarow GC, Mi X, DeVore AD, Duffy C, Sharma PP, Albert NM, Patterson JH, et al. Health Status Disparities by Sex, Race/Ethnicity, and Socioeconomic Status in Outpatients With Heart Failure. JACC: Heart Failure 2018;6:465–473. doi: 10.1016/j.jchf.2018.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nayak A, Hicks AJ, Morris AA. Understanding the Complexity of Heart Failure Risk and Treatment in Black Patients. Circ Heart Fail 2020;13:e007264. doi: 10.1161/CIRCHEARTFAILURE.120.007264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White-Williams C, Rossi LP, Bittner VA, Driscoll A, Durant RW, Granger BB, Graven LJ, Kitko L, Newlin K, Shirey M. Addressing Social Determinants of Health in the Care of Patients With Heart Failure: A Scientific Statement From the American Heart Association. Circulation 2020;141:e841–e863. doi: doi: 10.1161/CIR.0000000000000767 [DOI] [PubMed] [Google Scholar]
- 6.Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Willis M, et al. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 7.Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to Action: Structural Racism as a Fundamental Driver of Health Disparities: A Presidential Advisory From the American Heart Association. Circulation 2020;142:e454–e468. doi: doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 8.Hillier AE. Redlining and the Home Owners’ Loan Corporation. Journal of Urban History 2003;29:394–420. doi: 10.1177/0096144203029004002 [DOI] [Google Scholar]
- 9.Rothstein R The color of law : a forgotten history of how our government segregated America First edition. ed. New York ; London: Liveright Publishing Corporation, a division of W.W. Norton & Company; 2017. [Google Scholar]
- 10.Faber J Contemporary echoes of segregationist policy: Spatial marking and the persistence of inequality. Urban Studies 2020;58:1067–1086. doi: 10.1177/0042098020947341 [DOI] [Google Scholar]
- 11.Richardson J, Mitchell B, Meier H, Lynch E, Edlebi J. Redlining and neighborhood health https://ncrc.org/holc-health/. 2020. Accessed February 1, 2023.
- 12.Jacoby SF, Dong B, Beard JH, Wiebe DJ, Morrison CN. The enduring impact of historical and structural racism on urban violence in Philadelphia. Social Science & Medicine 2018;199:87–95. doi: 10.1016/j.socscimed.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McClure E, Feinstein L, Cordoba E, Douglas C, Emch M, Robinson W, Galea S, Aiello AE. The legacy of redlining in the effect of foreclosures on Detroit residents’ self-rated health. Health & Place 2019;55:9–19. doi: 10.1016/j.healthplace.2018.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mujahid MS, Gao X, Tabb LP, Morris C, Lewis TT. Historical redlining and cardiovascular health: The Multi-Ethnic Study of Atherosclerosis. Proceedings of the National Academy of Sciences 2021;118:e2110986118. doi: 10.1073/pnas.2110986118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang SJ, Sehgal NJ. Association of historic redlining and present-day health in Baltimore. PLoS One 2022;17:e0261028. doi: 10.1371/journal.pone.0261028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JA. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nelson RK, Winling L, Marciano R, Connolly N, Ayers EL. Mapping inequality https://dsl.richmond.edu/panorama/redlining/#loc=4/41.146/−100.986&text=downloads. 2017. Accessed February 1, 2023.
- 18.Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying Increased Risk of Readmission and In-hospital Mortality Using Hospital Administrative Data: The AHRQ Elixhauser Comorbidity Index. Med Care 2017;55:698–705. doi: 10.1097/MLR.0000000000000735 [DOI] [PubMed] [Google Scholar]
- 19.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 20.Mentias A, Desai MY, Vaughan-Sarrazin MS, Rao S, Morris AA, Hall JL, Menon V, Hockenberry J, Sims M, Fonarow GC, et al. Community-Level Economic Distress, Race, and Risk of Adverse Outcomes After Heart Failure Hospitalization Among Medicare Beneficiaries. Circulation 2022;145:110–121. doi: 10.1161/CIRCULATIONAHA.121.057756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mora S, Cook N, Buring JE, Ridker PM, Lee IM. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation 2007;116:2110–2118. doi: 10.1161/CIRCULATIONAHA.107.729939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nardone A, Casey JA, Morello-Frosch R, Mujahid M, Balmes JR, Thakur N. Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study. Lancet Planet Health 2020;4:e24–e31. doi: 10.1016/S2542-5196(19)30241-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res 2012;47:1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Essien UR, Youmans QR. Burning in “Other Suns”: The Effects of Residential Segregation on Cardiovascular Health. Circ Cardiovasc Qual Outcomes 2022;15:e008694. doi: 10.1161/CIRCOUTCOMES.121.008694 [DOI] [PubMed] [Google Scholar]
- 25.Nardone A, Rudolph KE, Morello-Frosch R, Casey JA. Redlines and Greenspace: The Relationship between Historical Redlining and 2010 Greenspace across the United States. Environ Health Perspect 2021;129:17006. doi: 10.1289/EHP7495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch EE, Malcoe LH, Laurent SE, Richardson J, Mitchell BC, Meier HCS. The legacy of structural racism: Associations between historic redlining, current mortgage lending, and health. SSM Popul Health 2021;14:100793. doi: 10.1016/j.ssmph.2021.100793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diaz A, O’Reggio R, Norman M, Thumma JR, Dimick JB, Ibrahim AM. Association of Historic Housing Policy, Modern Day Neighborhood Deprivation and Outcomes After Inpatient Hospitalization. Ann Surg 2021;274:985–991. doi: 10.1097/SLA.0000000000005195 [DOI] [PubMed] [Google Scholar]
- 28.Krieger N, Van Wye G, Huynh M, Waterman PD, Maduro G, Li W, Gwynn RC, Barbot O, Bassett MT. Structural Racism, Historical Redlining, and Risk of Preterm Birth in New York City, 2013–2017. Am J Public Health 2020;110:1046–1053. doi: 10.2105/AJPH.2020.305656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krieger N, Wright E, Chen JT, Waterman PD, Huntley ER, Arcaya M. Cancer Stage at Diagnosis, Historical Redlining, and Current Neighborhood Characteristics: Breast, Cervical, Lung, and Colorectal Cancers, Massachusetts, 2001–2015. Am J Epidemiol 2020;189:1065–1075. doi: 10.1093/aje/kwaa045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nardone AL, Casey JA, Rudolph KE, Karasek D, Mujahid M, Morello-Frosch R. Associations between historical redlining and birth outcomes from 2006 through 2015 in California. PLoS One 2020;15:e0237241. doi: 10.1371/journal.pone.0237241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mujahid MS, Gao X, Tabb LP, Morris C, Lewis TT. Historical redlining and cardiovascular health: The Multi-Ethnic Study of Atherosclerosis. Proc Natl Acad Sci U S A 2021;118. doi: 10.1073/pnas.2110986118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sims M, Kershaw KN, Breathett K, Jackson EA, Lewis LM, Mujahid MS, Suglia SF, American Heart Association Council on E, Prevention, Council on Quality of C, et al. Importance of Housing and Cardiovascular Health and Well-Being: A Scientific Statement From the American Heart Association. Circ Cardiovasc Qual Outcomes 2020;13:e000089. doi: 10.1161/HCQ.0000000000000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Breathett K, Liu WG, Allen LA, Daugherty SL, Blair IV, Jones J, Grunwald GK, Moss M, Kiser TH, Burnham E, et al. African Americans Are Less Likely to Receive Care by a Cardiologist During an Intensive Care Unit Admission for Heart Failure. JACC Heart Fail 2018;6:413–420. doi: 10.1016/j.jchf.2018.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kershaw KN, Osypuk TL, Do DP, De Chavez PJ, Diez Roux AV. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Circulation 2015;131:141–148. doi: 10.1161/CIRCULATIONAHA.114.011345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reddy NM, Mayne SL, Pool LR, Gordon-Larsen P, Carr JJ, Terry JG, Kershaw KN. Exposure to Neighborhood-Level Racial Residential Segregation in Young Adulthood to Midlife and Incident Subclinical Atherosclerosis in Black Adults: The Coronary Artery Risk Development in Young Adults Study. Circ Cardiovasc Qual Outcomes 2022;15:e007986. doi: 10.1161/CIRCOUTCOMES.121.007986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: an assessment of the evidence. Am J Public Health 2003;93:243–248. doi: 10.2105/ajph.93.2.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Panza GA, Puhl RM, Taylor BA, Zaleski AL, Livingston J, Pescatello LS. Links between discrimination and cardiovascular health among socially stigmatized groups: A systematic review. PLoS One 2019;14:e0217623. doi: 10.1371/journal.pone.0217623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bucholz EM, Ma S, Normand SL, Krumholz HM. Race, Socioeconomic Status, and Life Expectancy After Acute Myocardial Infarction. Circulation 2015;132:1338–1346. doi: 10.1161/CIRCULATIONAHA.115.017009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Azap RA, Nolan TS, Gray DM 2nd, Lawson K, Gregory J, Capers Qt, Odei JB, Joseph JJ. Association of Socioeconomic Status With Ideal Cardiovascular Health in Black Men. J Am Heart Assoc 2021;10:e020184. doi: 10.1161/JAHA.120.020184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boen C, Keister L, Aronson B. Beyond Net Worth: Racial Differences in Wealth Portfolios and Black-White Health Inequality across the Life Course. J Health Soc Behav 2020;61:153–169. doi: 10.1177/0022146520924811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith GS, Breakstone H, Dean LT, Thorpe RJ Jr. Impacts of Gentrification on Health in the US: a Systematic Review of the Literature. J Urban Health 2020;97:845–856. doi: 10.1007/s11524-020-00448-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.South E, Venkataramani A, Dalembert G. Building Black Wealth - The Role of Health Systems in Closing the Gap. N Engl J Med 2022;387:844–849. doi: 10.1056/NEJMms2209521 [DOI] [PubMed] [Google Scholar]
- 43.Justice Department Announces New Initiative to Combat Redlining. The United States Department of Justice https://www.justice.gov/opa/pr/justice-department-announces-new-initiative-combat-redlining. 2021.
- 44.Capps K How the Fair Housing Act Failed Black Homeowners https://www.bloomberg.com/news/articles/2018-04-11/50-years-after-the-fair-housing-act-redlining-persists. 2018. Accessed February 1, 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


