Abstract
Background:
Hospital readmissions remain a significant and pressing issue in our healthcare system. In 2010, the Affordable Care Act helped establish the Hospital Readmissions Reduction Program, which incentivized reducing readmission rates by instituting penalties. Hospital readmission, specifically unplanned, refers to a patient returning to the hospital shortly after discharge due to the same or a related medical condition, signaling potential issues in initial care, discharge processes, or post-hospitalization management. For this study, we defined readmission as a return to the hospital within 30 days. In 2018, Staten Island University Hospital started a multidisciplinary and coordinated initiative to reduce patient readmissions. The approach involved the departments of emergency medicine, medicine, cardiology, case management, nursing, pharmacy, and transitional care management. This study aimed to determine if this approach reduced 30-day readmissions.
Methods:
This case-control retrospective study reviewed electronic health records between January 2018 and November 2019. Readmission rates within 30 days of index discharge were compared between patients who received transitional care management before and after establishing a multidisciplinary communication of transitional care. Readmission rates were unadjusted and adjusted for patient demographics and predisposed risk for readmission and compared across demographics and select clinical characteristics.
Results:
A total of 772 patients were included in the analyses; 323 were in the control group (41.8%), and 449 were in the intervention group (58.2%). After the hospital adopted the workflow for multidisciplinary communication of transitional care, there was 45.2% less adjusted incidence of readmission, or approximately seven fewer overall readmissions per 100 patients (16.4% readmission vs 9.0% readmission; incident rate ratio, 0.55; 95% CI: 0.34–0.88).
Conclusions:
Multidisciplinary communication approaches led by emergency medicine can help reduce readmissions significantly. Adopting a structured communication workflow can enhance co-managing patients with a high risk of readmission between the emergency department and hospital medicine teams.
Keywords: Hospital readmissions, reduction initiative, healthcare utilization
Introduction
High hospital readmission rates, accounting for over $17.4 billion in annual national healthcare spending, remain significant. 1 A small fraction of patients, often labeled as “super-utilizers” or “high-frequency patients,” are responsible for a disproportionate amount of this spending. These individuals, characterized by frequent emergency department (ED) visits and complex healthcare needs, represent less than 1% of patients but account for 21% of federal healthcare spending.
Special attention and effort have been delegated over the past few years to identify psychosocial elements contributing to readmissions. In 2010, the Affordable Care Act helped establish the Hospital Readmissions Reduction Program (HRRP), which incentivizes reducing readmission rates by instituting penalties and a star rating system. 2 As a result, hospitals nationwide began developing strategies to address high readmission rates directly. In 2010, 599 US hospitals enrolled in national initiatives to reduce readmission for heart failure patients. Despite the demonstrated effectiveness of various strategies, such as medication reconciliation, arranging follow-up visits, and direct communication with primary care physicians, less than 30% of hospitals have implemented these methods. 3
Hospitals continue to intensify efforts to reduce readmission through organizational strategies. In 2010, Mount Sinai Medical Center in New York City attempted a team-based, high-continuity approach by creating the Preventable Admissions Care Team (PACT) Clinic to improve care specifically for super-utilizers. Patients who had frequent hospital visits were identified from the emergency department. These patients were referred to the PACT Clinic’s multidisciplinary team for medical intervention, social work, and counseling. The PACT team reduced 30-day readmission by 43% and ED visits by 54% for super-utilizers. 4
Much of the current literature on reducing hospital readmissions focuses on improving communication and collaboration during the handoff between inpatient providers and community providers at discharge.3,5,6 Less attention has been paid to the communication and collaboration between ED physicians and hospitalists when patients return to the ED.7–10 This is an important area to explore, as readmissions from the ED can be particularly costly and burdensome for patients and healthcare systems.
Goals of this investigation
The purpose of this study was to evaluate if there was a reduction in 30-day readmissions in select patient populations at a large teaching hospital from an initiative that focused on multidisciplinary communication and collaboration between ED physicians and hospitalists when patients return to the ED.
Materials and methods
Study design and setting
This retrospective pre-post study reviewed electronic health records (EHRs) of patients treated at Northwell Health’s ED at SIUH. SIUH is a 700-bed tertiary-care teaching hospital in Staten Island, NY. The ED at SIUH has a census of nearly 100,000 patient visits annually, with an estimated 75% discharge rate. The study included pre- and post-intervention periods that were approximately 1 year each. The pre-intervention period reviewed EHRs of patients treated at the SIUH ED between January 1, 2018, and October 1, 2018, before the SIUH Readmission Reduction Initiative was implemented. Intervention patients were treated at the same ED facility between November 1, 2018, and November 1, 2019, during which the SIUH Readmission Reduction Initiative evaluated in this study occurred. This study was reviewed and deemed exempt by Northwell Health’s Institutional Review Board because the data used were routinely collected as part of patient care and were de-identified for analyses (IRB #21-0600). Informed consent was not sought for the present study because the study was a retrospective chart review. The requirement for written informed consent was waived by the IRB. This study followed the REporting of studies Conducted using Observational Routinely collected health Data (RECORD) guidelines. 11 This study used the best practices of Northwell Health’s Institutional Review Board to de-identify and protect patient data.
In 2018, Staten Island University Hospital (SIUH) started its initiative to reduce patient readmissions. The Readmission Reduction initiative screened patients ⩾65 years of age with fee for service (FFS) Medicare insurance for admission diagnosis of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), pneumonia (PN), acute myocardial infarction (MI), or cerebrovascular accident (CVA). This readmission reduction program was a coordinated, multidisciplinary effort between the departments of emergency medicine, medicine, cardiology, case management, nursing, pharmacy, and Northwell Health Solutions. Patients who met the criteria were “tagged” during hospitalization and followed along specific care pathways by the inpatient team to ensure a safe transition to the outpatient setting. Care pathways included the involvement of case management teams, home care services, disease process education, early follow-up appointments within 1 week after discharge, and a patient navigator as an outpatient for at least 30 days. These efforts aimed to ensure appropriate home support and medical follow-up and aid in the early identification of barriers to care and patient engagement about their chronic illness. The initiative uses organized methods that are feasible and reproducible by other facilities to reduce readmission for high-frequency patients.
Data query process
Health records were identified via an electronic query. We utilized the hospital’s Electronic Health Records (EHR) system as our primary data source. To extract the relevant records, we developed a specialized query to identify patients who met our predefined inclusion criteria. Our query focused on identifying patients readmitted to the ED within 30 days of their initial discharge. This time frame was chosen to concentrate on short-term readmissions. The extracted data were then de-identified. Then, the data was integrated into a secure, structured database. Each patient visit was considered distinct and eligible for inclusion if it met independent criteria for the study.
Inclusion criteria
Age: Patients aged 65 or older. This age group was identified since the RRI specifically screened patients ⩾65 for readmission.
Insurance: Enrolled in Medicare Fee-For-Service (FFS). This insurance status was included since the RRI initiative screened patients with FFS Medicare insurance for readmission.
Diagnosis: Patients with a final index discharge diagnosis of either COPD exacerbation, acute CHF, PN, MI, or CVA. These diagnoses were selected because they were the conditions managed at the time by the transitional care navigation team that was part of this care model or initiative.
Admission: Patients who presented at the ED within 30 days of an index admission and met Medicare standardized readmission ratio criteria. The Standardized Readmission Ratio measures 30-day unplanned hospital readmission for patients discharged from a hospital in the U.S. 12
Exclusion criteria
Psychiatry Discharge: Patients discharged from psychiatric care were excluded to avoid confounding variables related to mental health treatment, which could affect readmission rates differently than general medical conditions.
Discharge Against Medical Advice: Patients discharged AMA were excluded as their non-adherence to medical advice could skew readmission rates, reflecting factors unrelated to the hospital’s discharge process or transitional care quality.
Other Criteria: Patients not meeting the age and insurance criteria or not having one of the specified diagnoses at discharge.
Intervention: Readmission reduction initiative process
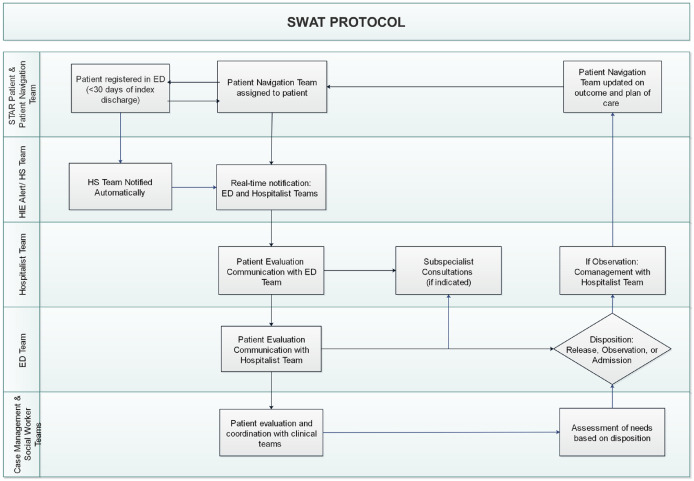
The readmission reduction initiative (RRI) was introduced at SIUH in November 2018. The program is a coordinated effort between the departments of medicine, emergency medicine, cardiology, case management, nursing, pharmacy, and Northwell Health Solutions. Figure 1 depicts the flow of an RRI patient.
Figure 1.
Readmission reduction initiative patient navigation.
Patients were identified during or after an index admission through the application and interface of a data collection logic that mimics CMS star diagnoses definitions. This process created a Northwell Health Solutions Care Management Platform case, which triggered the generation of a list for hospital staff. The inpatient team followed care pathways to ensure a safe transition to the outpatient setting. These care pathways included case management teams, home care services, disease process education, and a patient navigator as an outpatient for 30 days. The goals of these processes were accurately documenting diagnoses, goals of care conversations, transitioning safely with appropriate home care support or with medical follow-up as an outpatient, identifying barriers early, and educating or engaging the patients and their family members about the patient’s chronic illness.
Northwell Health Solutions is the Care Management arm of a large integrated healthcare system. The Health Solutions Transitional Care Management (TCM) team works with each hospital in the system, including SIUH, on readmission reduction efforts. TCM guides best practices for readmission reduction and provides data analytics to inform and advise each site on its performance. The TCM care navigation team comprises advanced care providers (ACP), nurses, and non-licensed care management coordinators. The navigators followed a model that, at minimum, included a 24-h phone call to review discharge instructions and medications, scheduling follow-up appointments, 72-h phone calls, and weekly touches until 30 days post-discharge. If a patient is deemed high risk or needs face-to-face clinical evaluation, a clinical escalation pathway exists for patients to receive home visits from the ACP. This clinical escalation can also be triggered by a disease-specific chatbot offered to all patients. A 24-h Health Solutions clinical call center staffed by nurses was available to each patient enrolled in the TCM program. If an enrolled patient presents to acute care and is available for communication with the ED and inpatient teams to add to the care disposition decision-making process, the navigation team received an automated email notification.
After hospital discharge, patients were enrolled in an electronic alert system. If an enrolled patient returned to any ED in the Northwell Health network, members of the RRI team who were familiar with the patient’s history received an electronic alert via Microsoft (MS) Teams (Microsoft, Redmond, Washington). In addition, a unique icon was placed next to the patient’s name on the EHR to notify the physician caring for the patient of the subject’s RRI status. Upon return, members of the RRI team and the physician caring for the patient were encouraged to work together to understand and implement the best care disposition for that patient. The designation was removed if the patient did not return to the ED within 30 days.
Outcomes
The primary outcomes of this study were rates and incidence per 100 patients of 30-day readmission following index discharge from the ED.
Statistical analysis
All data were analyzed using Stata, version 17.0 (College Station, TX, USA). Differences in patient strata were compared between patients who received transitional care before (control group) and after (intervention group) the multidisciplinary communication workflow for transitional care was implemented. Patient strata were compared using theχ2,t-tests, and two-sample tests of proportions when appropriate. Rates of readmission within 30 days of index discharge were compared between the control and intervention groups with χ2 and Fisher’s exact test for smaller samples. The adjusted incidence of readmission in the intervention group was compared to the control group using incident rate ratios from Poisson multivariate regression. Control variables included patient gender, age, race, ethnicity, discharge disposition, patient quality conditions, and LACE readmission risk scores. 13 The LACE index 14 uses four variables to predict the risk of death or nonelective 30-day readmission after hospital discharge among both medical and surgical patients: length of stay (L), acuity of the admission (A), comorbidity of the patient (C) and ED use in 6 months before admission (E). 15 Adjusted incidence of readmission was also compared across groups per 100 patients.
Results
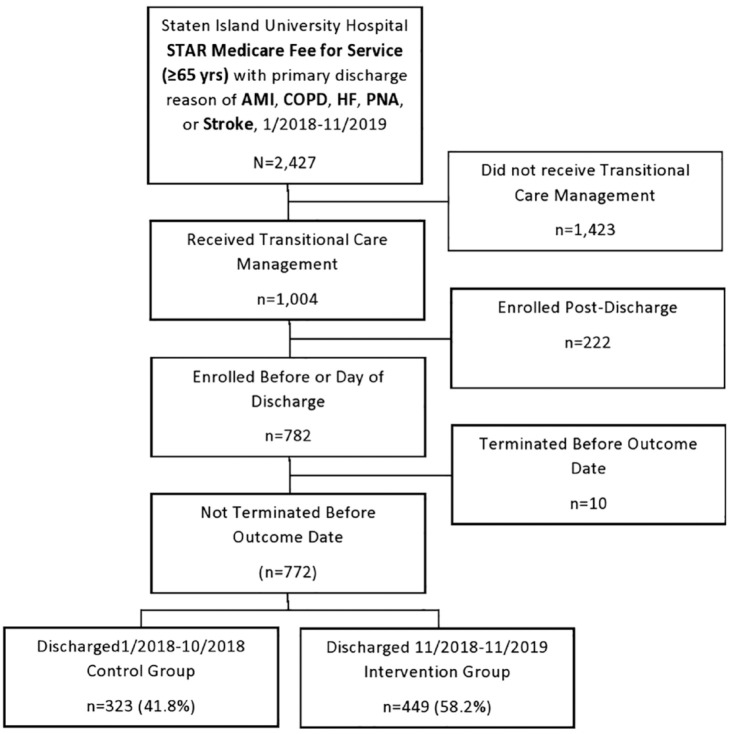
During the study period, 772 patients met the inclusion criteria and were included for analysis (see Figure 2).
Figure 2.
Study participant enrollment flow chart.
There were 323 patients (41.8%) in the control group and 449 patients (58.2%) in the intervention group. Most patients were female (54.3%), 75–84 years of age (37.8%), White (87.8%), and had heart failure (41.2%) (see Table 1).
Table 1.
Characteristics of participants, 1/2018–9/2021 (N = 772).
| Variable | N (%) | Control n (%) | Intervention n (%) | p a |
|---|---|---|---|---|
| % Total (N) | 772 (100) | 323 (41.8) | 449 (58.2) | 0.70 |
| Sex | ||||
| Male | 353 (45.7) | 150 (46.4) | 203 (45.2) | 0.74 |
| Female | 419 (54.3) | 173 (53.6) | 246 (54.8) | |
| Age | ||||
| M (SD) | 80.1 (8.3) | 80.6 (8.6) | 79.8 (8.1) | 0.21 |
| 65–74 | 230 (29.8) | 92 (28.5) | 138 (30.7) | 0.66 |
| 75–84 | 292 (37.8) | 121 (37.5) | 171 (38.1) | |
| ⩾85 | 250 (32.4) | 110 (34.1) | 449 (31.2) | |
| Race | ||||
| White | 678 (87.8) | 287 (88.9) | 391 (87.1) | 0.30 |
| African American/black | 37 (4.8) | 16 (5.0) | 20 (4.5) | |
| Multiracial | 35 (4.3) | 15 (4.6) | 20 (4.5) | |
| Asian or Pacific Islander | 14 (1.8) | 5 (1.6) | 9 (2.0) | |
| American Indian or Alaskan | 7 (0.9) | 0 (0.0) | 7 (1.6) | |
| Unknown | 1 (0.1) | 0 (0.0) | 1 (0.2) | |
| Ethnicity | ||||
| Not Hispanic or Latino | 735 (95.2) | 310 (96.0) | 425 (94.7) | 0.57 |
| Hispanic or Latino | 33 (4.3) | 11 (3.4) | 22 (4.9) | |
| Unknown | 4 (0.5) | 2 (0.6) | 2 (0.5) | |
| LACE readmission risk score | ||||
| M (SD) | 12.2 (3.2) | 10.1 (2.4) | 13.7 (2.7) | 0.00 |
| ⩽10 | 249 (32.3) | 193 (59.8) | 56 (12.5) | 0.00 |
| 11–15 | 385 (49.9) | 126 (39.0) | 259 (57.7) | |
| ⩾16 | 138 (17.9) | 4 (1.2) | 134 (29.8) | |
| Condition | ||||
| Heart failure | 318 (41.2) | 156 (48.3) | 162 (36.1) | 0.75 |
| Pneumonia | 228 (29.5) | 93 (28.8) | 135 (30.1) | 0.01 |
| COPD | 140 (18.1) | 68 (21.1) | 72 (16.0) | 0.74 |
| Stroke | 58 (7.5) | 4 (1.2) | 54 (12.0) | 0.00 |
| Acute myocardial infarction | 28 (3.6) | 2 (0.6) | 26 (5.8) | 0.00 |
| Discharge disposition | ||||
| Home | 230 (29.8) | 104 (32.2) | 126 (28.1) | 0.00 |
| Home care | 298 (38.6) | 124 (38.4) | 174 (38.8) | |
| Skilled nursing facility | 185 (24.0) | 71 (22.0) | 114 (25.4) | |
| Acute rehab | 30 (3.9) | 4 (1.2) | 26 (5.8) | |
| Hospice | 13 (1.7) | 11 (3.4) | 2 (0.5) | |
| Other | 16 (2.1) | 9 (2.8) | 7 (1.6) | |
Pearson Chi-square for group frequency differences, two-sample t-test for group mean differences, and two-sample tests of proportions for conditions.
After the implementation of the multidisciplinary communication workflow, there were fewer readmissions among African American/Black patients (0.0% vs 18.8%; p < 0.05) and patients with LACE readmission risk scores ⩽10 (5.4% vs 17.1%; p < 0.05) (see Table 2).
Table 2.
Unadjusted differences in 30-day readmission rates of Medicare star patients who received transitional care management (TCM) before and after implementing an enhanced communication workflow among admissions hospitalists a .
| Variable | Total | Control | Intervention | p b |
|---|---|---|---|---|
| Readmitted n (%) | Readmitted n (%) | Readmitted n (%) | ||
| Total | 122 (15.8) | 53 (16.4) | 69 (15.4) | 0.696 |
| Sex | ||||
| Male | 60 (17.0) | 26 (17.3) | 34 (16.8) | 0.885 |
| Female | 62 (14.8) | 27 (15.6) | 35 (14.2) | 0.695 |
| Age | ||||
| 65–74 | 28 (12.2) | 14 (15.2) | 14 (10.1) | 0.249 |
| 75–84 | 49 (16.8) | 18 (14.9) | 31 (18.1) | 0.464 |
| ⩾85 | 45 (18.0) | 21 (19.1) | 24 (17.1) | 0.691 |
| Race | ||||
| White | 114 (16.8) | 48 (16.7) | 66 (16.9) | 0.957 |
| African American/black | 3 (8.1) | 3 (18.8) | 0 (0.0) | 0.038 |
| Multiracial | 4 (11.4) | 2 (13.3) | 2 (10.0) | 0.759 |
| Asian or Pacific Islander | 1 (7.1) | 0 (0.0) | 1 (11.1) | 0.439 |
| American Indian or Alaskan | 0 (0.0) | 0 (0.0) | 0 (0.0) | — |
| Unknown | 0 (0.0) | 0 (0.0) | 0 (0.0) | — |
| Ethnicity | ||||
| Not Hispanic or Latino | 120 (16.3) | 52 (16.8) | 68 (16.0) | 0.779 |
| Hispanic or Latino | 2 (6.1) | 1 (9.1) | 1 (4.6) | 0.606 |
| Unknown | 0 (0.0) | 0 (0.0) | 0 (0.0) | — |
| LACE readmission risk score | ||||
| ⩽10 | 36 (14.5) | 33 (17.1) | 3 (5.4) | 0.028 |
| 11–15 | 50 (13.0) | 20 (15.9) | 30 (11.6) | 0.240 |
| ⩾16 | 36 (26.1) | 0 (0.0) | 36 (26.9) | 0.228 |
| Conditionb | ||||
| Heart failure | 52 (16.4) | 220 (14.1) | 30 (18.5) | 0.287 |
| Pneumonia | 36 (15.8) | 17 (18.3) | 19 (14.1) | 0.392 |
| COPD | 21 (15.0) | 13 (19.1) | 8 (11.1) | 0.185 |
| Stroke | 9 (15.5) | 1 (25.0) | 98 (14.8) | 0.587 |
| Acute myocardial infarction | 4 (14.3) | 0 (0.0) | 4 (15.4) | 0.730 |
| Discharge disposition | ||||
| Home | 20 (8.7) | 9 (8.7) | 11 (8.7) | 0.984 |
| Home care | 60 (20.1) | 29 (23.4) | 31 (17.8) | 0.237 |
| Skilled nursing facility | 31 (16.8) | 11 (15.5) | 20 (17.5) | 0.716 |
| Acute rehab | 7 (23.3) | 1 (25.0) | 6 (23.1) | 0.677 |
| Hospice | 0 (0.0) | 0 (0.0) | 0 (0.0) | — |
| Other | 4 (25.0) | 3 (33.3) | 1 (14.3) | 0.585 |
Control TCM patients were from 1/2018 to 10/2018. Intervention occurred between 11/2018 and 11/2019.
Pearson Chi-square tests of differences for all except Acute Myocardial Infarction, Acute Rehab, and Other (Fishers exact test for small samples).
Bolded values are statistically significant with p < 0.5.
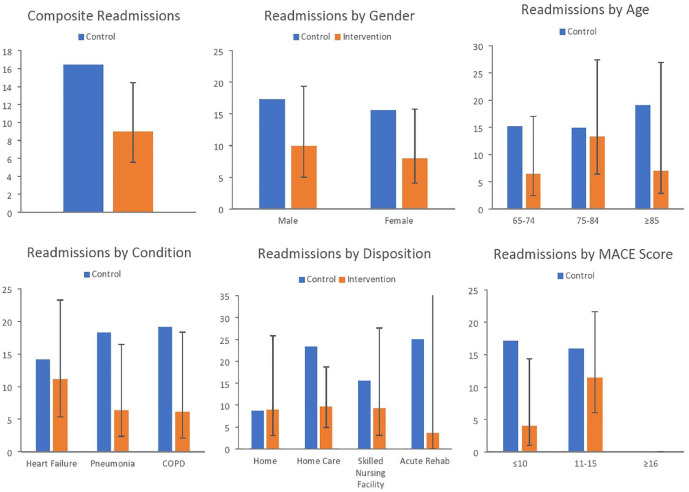
After adopting the workflow for multidisciplinary communication of transitional care, there was 45.2% less adjusted incidence of readmission, or approximately seven fewer overall readmissions per 100 patients (16.4% readmission vs 9.0% readmission; IRR, 0.55; 95% CI: 0.34–0.88) (see Table 3 and Figure 3).
Table 3.
Unadjusted and adjusted changes in 30-day readmission rates of Medicare star patients who received transitional care management (TCM) before and after implementing an enhanced communication workflow among admissions hospitalists a .
| Variable | Unadjusted % change | Adjusted % change b | 95% CI |
|---|---|---|---|
| Total | −6.1 | −45.2 | .34–.88 |
| Sex | |||
| Male | −2.9 | −57.3 | .29–1.12 |
| Female | −9.0 | −49.1 | .26–1.01 |
| Age | |||
| 65–74 | −33.6 | −57.8 | .16–1.12 |
| 75–84 | 21.5 | −11.0 | .43–1.84 |
| ⩾85 | −10.5 | −63.5 | .15–1.41 |
| Race | |||
| White | 1.2 | −41.6 | .36–.95 |
| African American/black | −100.0 | — | — |
| Multiracial | −24.8 | — | — |
| Asian or Pacific Islander | — | — | — |
| American Indian or Alaskan | — | — | — |
| Unknown | — | — | — |
| Ethnicity | |||
| Not Hispanic or Latino | −4.8 | −46.8 | .33–.86 |
| Hispanic or Latino | −49.5 | — | — |
| Unknown | — | — | — |
| LACE readmission risk score | |||
| ⩽10 | −68.4 | −76.6 | .06–.84 |
| 11–15 | −27.0 | −28.2 | .38–1.36 |
| ⩾16 | — | — | — |
| Condition b | |||
| Heart failure | 31.2 | −20.9 | .38–1.65 |
| Pneumonia | −23.0 | −65.5 | .13–.90 |
| COPD | −41.9 | −68.1 | .11–.96 |
| Stroke | −40.8 | — | — |
| Acute myocardial infarction | |||
| Discharge disposition | |||
| Home | 0.0 | 2.0 | .35–2.97 |
| Home care | −23.9 | −58.6 | .21–.80 |
| Skilled nursing facility | 12.9 | −39.8 | .20–1.78 |
| Acute rehab | −7.6 | −85.4 | .00–16.15 |
| Hospice | — | — | — |
| Other | −57.1 | — | — |
Control TCM patients were from 1/2018 to 10/2018. Intervention occurred between 11/2018 and 11/2019.
Separate Poisson fixed effects models adjusted for all other variables in table.
bolded values are significant findings.
Figure 3.
Readmissions per 100 subjects.
There were no statistical differences in readmission by gender or age before and after enhancing transitional care communication. Patients with PN or COPD readmitted respectively 65.5% and 68.1% less after improving transitional care communication, or 12 and 13 fewer times per 100 patients (18.3% readmission vs 6.3% readmission; IRR, 0.35; 95% CI: 0.13–0.90; and 19.1% vs 6.1%; IRR, 0.32; 95% CI: 0.11–0.96). Of index discharge dispositions, only patients discharged to Home Care readmitted less after enhanced transitional care communication (23.4% before vs 9.7% after; IRR, 0.41; 95% CI: 0.21–0.80) (Table 3).
Discussion
This study evaluated if an enhanced multidisciplinary communication workflow for transitional care reduced 30-day readmissions. We found that after the hospital adopted the enhanced communication workflow, there was 45% less adjusted incidence of readmission or approximately seven fewer overall readmissions per 100 patients.
In contrast, previous studies have shown that women and men may have different healthcare experiences and barriers to accessing and utilizing healthcare services. However, these differences may not necessarily translate to differences in readmission rates, as the causes and factors that contribute to them may be complex and multifactorial. One may also expect differences in readmission rates based on age. Age is a known risk factor for readmissions, 16 as older individuals may have more complex medical conditions and require more care and support than younger individuals. They may also have more difficulty transitioning from the hospital to home or a long-term care facility, which can lead to readmissions.
Additionally, older adults may be more likely to have functional or cognitive impairments that can make it challenging to follow discharge instructions and manage their care independently. Our study, however, did not find a significant difference in readmission rates based on age. This could imply that the enhanced communication strategies were equally effective across different age groups. A coordinated multidisciplinary approach that specifically addresses the needs of older adults and provides them with appropriate resources and support may be more effective in reducing readmissions among this population.
Overall, the results of this study suggest that enhanced communication measures effectively improve outcomes regardless of patients’ gender or age. There were no statistical differences in readmission by gender or age before and after strengthening transitional care communication. Previous research has highlighted gender-based disparities in healthcare experiences and access. 17 The lack of significant difference in readmission rates based on age may be due to the small sample size or because age is just one of many factors considered in the LACE Score, which is a predictor of 30-day mortality and readmission.
Patients with PN or COPD had significantly improved clinical outcomes regarding readmission rates after the study intervention. Specifically, the study found that patients with PN and COPD were readmitted 65% and 68% less, respectively, after enhancing transitional care communication. This finding also translates to 12 and 13 fewer times per 100 patients. Although our study showed a trend of reduced readmission rates for most diagnoses, this reduction only reached statistical significance in patients with PN and COPD. A study by Kripalani et al. 18 found similar reductions in readmission rates after a transitional care intervention. One likely explanation is that both are respiratory conditions that predominantly involve the pulmonary system and present mainly with shortness of breath, as opposed to patients with heart failure, which can have multiorgan manifestations and various clinical manifestations. Previous studies have shown decreased readmission rates for patients with CHF, 19 MI, 20 and select stroke patients. 21 The lack of reduced readmissions for patients with congestive heart failure (CHF), myocardial infarction (MI), and stroke in this study, compared to prior research, may stem from variations in patient characteristics, the types of the transitional care intervention, and the complex nature of these conditions. Factors such as variability in care practices and unmeasured variables could also contribute to the observed differences. Furthermore, the sample size of patients in our study with stroke or MI may have been insufficient to draw any clinical conclusions.
Overall, the study suggests the intervention was more effective in reducing readmission rates when patients discharged to home with home-care services were readmitted less after enhanced transitional care communication. There is evidence that patients who receive post-discharge care have better clinical outcomes when compared with patients discharged home without such services. 22 Our study showed improvement in the readmission rate for the intervention group released to a skilled nursing facility (SNF) and home with care services. The readmission reduction in the subgroup of patients discharged to home with care services reached statistical significance, likely reflecting the impact of improved communication and coordination between home care providers, patient navigation team, and inpatient providers. The need for improvement in readmission rates for patients discharged to skilled nursing facilities may be due to the relatively higher frailty and complexity of patients requiring institutionalized post-acute care and the difficulty for patient navigation teams to effectively communicate and coordinate care with usually large and complex third-party institutions. The authors suggest that further research is needed to understand why the intervention was not as effective in reducing readmission rates for patients discharged to other locations, such as skilled nursing facilities, and how to improve the efficacy of the intervention in these settings.
The intervention group had statistically fewer patients with a LACE score on admission <10 and more patients with a LACE score of 11–15 and >15. The same was true for readmitted patients. One possible explanation for this finding is that patients with more advanced morbidities and complexities, as indicated by a higher LACE score, may have benefited less from the intervention, and their inpatient needs (i.e., readmission) remained unchanged. However, the study found that the improvement in averting readmission reached statistical significance in patients with LACE<10 who received the intervention. The study suggests that the intervention effectively reduced readmission rates for patients with higher LACE scores. The effect might have been more pronounced if the two groups had similar LACE scores.
The results suggest there may have been a potential imbalance in the distribution of pre-existing conditions among the control and intervention groups. The higher percentage of heart failure and COPD in the control group and the higher percentage of AMI and CVA in the intervention group may have impacted the study results. However, since the absolute numbers of AMI and CVA were similar in both groups, these conditions are unlikely to influence the overall results significantly. It is essential to consider these imbalances in interpreting the study findings.
The results suggest that there may be a lack of representation of African American and Hispanic/Latino individuals in the intervention group, as no individuals from these groups were readmitted. This finding could be due to a selection bias, as the intervention group tended to be White. It is difficult to conclude the program’s potential benefits for these underrepresented groups due to the small number of individuals from these groups who were included in the study. It is essential to consider these demographic imbalances in interpreting the study findings and to investigate if there is something particularly beneficial to African Americans in the program or if something needs to be added to previous programs. According to the Centers for Medicare & Medicaid Services (CMS), in 2020, about 43% of Medicare beneficiaries were White, 10% were Black, 9% were Hispanic, 3% were Asian, and 35% identified as other or multiple races. This finding may help explain this study’s higher percentage of White patients.
Unlike most available literature on reducing readmissions, our study focused on the communication and close collaboration between Hospitalists and ED physicians when patients returned to the ED within 30 days after discharge. The effectiveness of such collaboration stems from weighing in the benefit of including the inpatient team to enhance the continuity of care provided during antecedent episodes of hospitalization and add another layer of expertise when caring for patients with multiple medical conditions. Our work further highlights the need to continue to explore the concept of ED and inpatient team collaboration and co-management of patients upon presentation in the ED.
Limitations
The study had several limitations that should be considered when interpreting findings. The study’s design as a retrospective study means that it is subject to bias, and the results may not be generalizable to other settings, institutions, or regions. Additionally, the study was conducted at a single institution in a specific region, which limits the ability to generalize the findings to other geographic areas. A multicenter study, including data from multiple institutions in different regions, would be needed to increase generalizability. Additionally, the processes described in the study are specific to the institution where the study was conducted and may only be partially applicable to other hospitals with different capabilities. Also, we chose a particular time frame with all eligible patients for the study. Therefore, no formal power analysis was used to determine a sample size. These limitations should be considered when interpreting the findings and planning future research.
This study focused only on Medicare recipients, who are known to be predominantly White and have little to no barriers to accessing care. The study’s results may not accurately reflect the experiences or outcomes of other patient populations, such as those underinsured or uninsured, or patients facing barriers to accessing care, such as healthcare providers, prescription medications, or home care services. Future research could consider including a more diverse range of subjects, including underinsured or uninsured patients or those who face barriers to accessing care. This method would provide a more comprehensive understanding of the experiences and outcomes of our intervention on different patient populations.
Patients who met the following criteria were “tagged” for electronic notification if they returned to the ED within 30 days of their previous visit: The criteria include age 65 or above, being enrolled in Medicare FFS, and having one of the following diagnoses at discharge: PN, MI, CHF, or CVA. However, the final discharge diagnoses submitted for billing may be changed based on a clinical documentation improvement (CDI) review of the documentation after the patient has been discharged. This method may have led to the under-reporting of some patients enrolled in the initiative and readmitted to the hospital. In other words, the electronic notification system may not accurately identify all patients who were readmitted within 30 days if the discharge diagnosis was changed after their discharge due to CDI review. This may result in some patients being missed or overlooked, impacting the accuracy of the initiative’s results. Therefore, one should consider this limitation when interpreting the results of the study and when planning future research. This limitation highlights the importance of ensuring that the discharge diagnoses submitted for billing are precise and complete to accurately identify patients at risk of readmission and to ensure that they receive appropriate follow-up care.
Finally, SNFs have independent teams who cannot access our hospital for post-acute care. They do not have access to the hospital’s electronic medical records. Additionally, coordination with Patient Navigation teams was not part of their specific care flow. The lack of coordination with Patient Navigation teams may limit the ability of the SNFs to address any barriers to care effectively or to ensure that patients receive the services and support they need. It is essential to consider these limitations when planning for post-acute care and address them to ensure that patients receive the best care. This may involve improving access to electronic medical records, increasing coordination with Patient Navigation teams, and making other changes to the care flow to ensure patients receive the care they need.
Conclusions
This study demonstrates the impact of a coordinated multidisciplinary approach on reducing 30-day readmissions. After implementing this approach, there was a 45% decrease in readmissions, with seven fewer readmissions per 100 patients. This reduction was particularly evident in patients with pneumonia and COPD. The study highlights the successful collaboration between the ED and Hospital Medicine teams, emphasizing the critical role of early involvement of inpatient teams in patient care. These findings underscore our intervention’s efficacy in enhancing patient outcomes and suggest a promising direction for similar healthcare strategies.
Acknowledgments
Not applicable.
Footnotes
Author contributions: The authors confirm their contribution to the paper as follows: study conception and design: BH, TB, WD, CC, HB, and AF; data collection: BH, WD, TB, and CC; analysis and interpretation of results: BH, WD, TB, and CC; draft manuscript preparation: BH, WD, TB, and CC. All authors reviewed the results and approved the final version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Barry Hahn  https://orcid.org/0000-0001-9035-5603
https://orcid.org/0000-0001-9035-5603
Ethics approval: Ethical approval for this study was obtained from Northwell Health IRB #: 21-0600.
Informed consent: Informed consent was not sought for the present study because the study was a retrospective chart review. The requirement for written informed consent was waived off by the Institutional Review Board (IRB).
Trial registration: This was not a randomized clinical trial and was not registered.
References
- 1. Cline DM, Silva S, Freiermuth CE, et al. Emergency department (ED), ED observation, day hospital, and hospital admissions for adults with sickle cell disease. West J Emerg Med 2018; 19(2): 311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wallins JS, Cajiao KM, McCarthy KJ, et al. Impact of an outpatient cardiology-managed urgent access and observation unit on hospital admissions. Crit Pathw Cardiol 2019; 18(3): 113–120. [DOI] [PubMed] [Google Scholar]
- 3. Fish-Trotter H, Collins SP, Danagoulian S, et al. Design and rationale of a randomized trial: using short stay units instead of routine admission to improve patient centered health outcomes for acute heart failure patients (SSU-AHF). Contemp Clin Trials 2018; 72: 137–145. [DOI] [PubMed] [Google Scholar]
- 4. Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 2011; 155: 520–528. [DOI] [PubMed] [Google Scholar]
- 5. Rennke S, Nguyen OK, Shoeb MH, et al. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158: 433–440. [DOI] [PubMed] [Google Scholar]
- 6. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007; 297: 831–841. [DOI] [PubMed] [Google Scholar]
- 7. Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Int Med 2019; 170: 673–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Goldman LE, Sarkar U, Kessell E, et al. Support from hospital to home for elders: a randomized trial. Ann Intern Med 2014; 161: 472–481. [DOI] [PubMed] [Google Scholar]
- 9. Hsuan C, Carr BG, Hsia RY, et al. Assessment of hospital readmissions from the emergency department after implementation of medicare’s hospital readmissions reduction program. JAMA Netw Open 2020; 3: e203857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prior MK, Bahret BA, Allen RI, et al. The efficacy of a senior outreach program in the reduction of hospital readmissions and emergency department visits among chronically ill seniors. Soc Work Health Care 2012; 51: 345–360. [DOI] [PubMed] [Google Scholar]
- 11. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015; 12: e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. He K, Kalbfleisch JD, Li Y, et al. Evaluating hospital readmission rates in dialysis facilities; adjusting for hospital effects. Lifetime Data Anal 2013; 19(4): 490–512. [DOI] [PubMed] [Google Scholar]
- 13. Staples JA, Wiksyk B, Liu G, et al. External validation of the modified LACE+, LACE+, and LACE scores to predict readmission or death after hospital discharge. J Eval Clin Pract 2021; 27: 1390–1397. [DOI] [PubMed] [Google Scholar]
- 14. Van Walraven C, Wong J, Forster AJ. LACE+ index: extension of a validated index to predict early death or urgent readmission after hospital discharge using administrative data. Open Med 2012; 6: e80–e90. [PMC free article] [PubMed] [Google Scholar]
- 15. Tarazi W, Welch WP, Nguyen N, et al. Medicare beneficiary enrollment trends and demographic characteristics. https://aspe.hhs.gov/sites/default/files/documents/f81aafbba0b331c71c6e8bc66512e25d/medicare-beneficiary-enrollment-ib.pdf (2022, accessed 1 February2023).
- 16. Cilla F, Sabione I, D’Amelio P. Risk factors for early hospital readmission in geriatric patients: a systematic review. Int J Environ Res Public Health 2023; 20: 1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Manuel JI. Racial/ethnic and gender disparities in health care use and access. Health Serv Res 2018; 53: 1407–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kripalani S, Chen G, Ciampa P, et al. A transition care coordinator model reduces hospital readmissions and costs. Contemp Clin Trials 2019; 81: 55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu S, Xiong XY, Chen H, et al. Transitional care in patients with heart failure: a concept analysis using Rogers’ evolutionary approach. Risk Manag Healthc Policy 2023; 16: 2063–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gupta S, Zengul FD, Davlyatov GK, et al. Reduction in hospitals’ readmission rates: role of hospital-based skilled nursing facilities. Inquiry 2019; 56: 46958018817994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jun-O’Connell AH, Grigoriciuc E, Gulati A, et al. Stroke nurse navigator utilization reduces unplanned 30-day readmission in stroke patients treated with thrombolysis. Front Neurol 2023; 14: 1205487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Werner RM, Coe NB, Qi M, et al. Patient outcomes after hospital discharge to home with home health care vs to a skilled nursing facility. JAMA Intern Med 2019; 179(5): 617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]