Abstract
Background:
Person-centered maternity care is a crucial scheme for a positive childbirth experience. It enhances facility-based delivery, improves patient–provider communication, and increases women’s satisfaction. However, there is limited evidence on the magnitude of person-centered care and certain variables were missed in Ethiopia. Therefore, this study assessed the magnitude of person-centered maternity care during childbirth and associated factors at health institutions of Debre Markos town, Ethiopia.
Methods:
Institution-based cross-sectional study was conducted at public health institutions of Debre Markos town. Participants were enrolled using systematic random sampling technique. Data were collected through face-to-face exit interviews, cleaned, coded, and entered into Epi-Data version 3.1 then exported to SPSS version 25 for analysis. After generating simple linear regression analysis, variables with p-value ⩽ 0.25 were fitted into multivariable linear regression model and p-value < 0.05 was declared statistically significant with 95% CI for β. Finally, study findings were presented using texts, tables, and figures.
Results:
In this study, 380 women participated, with a response rate of 98.19%. The respondent’s mean person-centered maternity care score was 56.83 with 95% CI: (55.83, 57.83). Mean score for sub-scale was 15.08 for dignity and respect, 14.42 for communication and autonomy, and 27.33 for supportive care. Commencing antenatal care during third trimester (β = −4.86, 95% CI: −8.22, −1.49), caesarean delivery (β = −5.78, 95% CI: −7.68, −3.87), college and above educational level of women (β = 3.75, 95% CI: 1.11, 6.39), being multiparous (β = 3.69, 95% CI: 1.85, 5.55), and health center delivery (β = 6.59, 95% CI: 4.17, 9.02) were factors significantly associated with person-centered maternity care.
Conclusion:
This study showed person-centered maternity care was low compared with World Health Organization standards. This informs local policymakers, district health offices, institutional healthcare administrators, and healthcare professionals of the discrepancies in achieving international standards of quality care.
Keywords: Childbirth, Debre Markos, Ethiopia, person-centered maternity care
Background
Person-centered maternity care (PCMC) is depicted as offering a collective spectrum of maternity care that is respectful of and attentive to individual women’s choices, values, and requirements as well as ensuring women’s values guides all healthcare decisions prior to, during and after delivery.1–3 The World Health Organization (WHO) standards for improving quality of maternal and newborn care identified dignity and respect, communication and autonomy as well as supportive and responsive care as crucial domains of PCMC that should be rendered during childbirth.4–6 Among the eight WHO standards, standards 4, 5, and 6 highlighted the three dimensions of PCMC that women experience during childbirth. Standard 4 focused on the significance of communication and autonomy in that women should receive all information about her care and feel involved in all decisions regarding her treatment. The concern of standard 5 is to render total respect and to preserve the dignity of all women throughout their stay in the health facility. Standard 6 states that every woman should be provided with emotional support that is sensitive to their needs and strengthens the woman’s capability.
PCMC, which is accepted as a key aspect of quality maternity care, appreciates clients’ experience of care. 5 Besides, PCMC is an important strategy to diminish existing maternal and neonatal problems by enhancing clients’ satisfaction with services, timely provision of care, heightened patient–provider communications, increased facility-based delivery as well as ensuring execution of women’s reproductive health rights.1,7–10
Studies shown the provision of PCMC during childbirth in low- and middle-income countries (LMICs) remains inadequate.2,7,11,12 Previous studies from Turkey, Sri Lanka, three LMIC (India, Kenya, and Ghana), Nigeria, and Ethiopia highlighted that the magnitude of PCMC ranges from 39.96 to 62.2,9,11,13–15 Besides, PCMC during childbirth especially in the communication and autonomy as well as supportive and responsive care dimensions were lacking in those settings.2,7,11 Evidence from LMIC (India, Kenya, and Ghana) showed that healthcare providers never introduced themselves to 90% of women 7 and 64.5% of Ethiopian women reported that healthcare providers never introduced themselves. 11
Many women experienced poor PCMC as manifested by mistreatment, disrespect, and abuse during childbirth.16,17 The lack of PCMC during childbirth is responsible for a large percentage of maternal deaths globally,3,18 with nearly two-thirds (66%) occurring in Sub-Saharan Africa,19,20 where Ethiopia accounted for 412 per 100,000 live births. 21 Therefore, in order to meet the Sustainable Development Goal target of reducing the global maternal death to <70 per 100,000 live births by 2030, 22 PCMC plays a great role to achieve this goal.4,23
In addition, the lack of PCMC during childbirth predisposes to women’s deterrence of institutional delivery and contributes to adverse maternal and newborn outcomes7,8,15,16,18,24 which ultimately leads to adverse psychological influence on women’s overall health. 1 Studies have shown women avoid facility-based childbirth for their next delivery when they experience poor treatment from healthcare providers. 25 Furthermore, as women shared their feelings and negative experiences with communities, it resulted in a distorted community perception of quality of care which discourages other women from seeking institutional delivery.18,26,27
Factors found to be associated with PCMC during childbirth include; residence, socioeconomic status, educational level and occupation of women, marital status, husband’s educational level and occupation, timing of antenatal care (ANC) follow-up, parity, time of delivery, complication during childbirth, place of childbirth, fetal outcome, health facility length of stay, and sex of healthcare professionals attending the delivery.7,11,14,18,26,28–30
Ethiopia has been inculcated and implemented caring, compassionate and respectful care as one of the priority issues in the Health Sector Transformation Plan from 2015/16 to 2019/20. 31 Despite its implementation, the provisions of compassionate and respectful maternity care remain low in Ethiopia.32,33 Although limited studies were done on the level of PCMC in Ethiopia, they missed certain variables like husbands’ educational level, husbands’ occupation, and timing of ANC follow-up. A robust, valid, and comprehensive measurement tool which highlighted women’s real experience of care is currently launched as per the WHO’s standards for improving quality of maternal and newborn care.4,6 Accordingly, this study was designed to assess the magnitude of PCMC during childbirth and its associated factors among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia by using the newly validated comprehensive PCMC measurement tool.
Materials and methods
Study setting, period, and design
An institution-based cross-sectional study was conducted at public health institutions of Debre Markos town from 21 May to 21 June 2022. Debre Markos administrative town is found in East Gojjam zone, Amhara regional state, Northwest Ethiopia. The town is located 256 and 300 km away from Bahir Dar, the capital city of Amhara regional state, and Addis Ababa, the capital city of Ethiopia respectively. According to Debre Markos town administration health office report of 20 April 2022, the town has a total population of 146,153, of which 78,046 were females, with childbearing age group accounting for 34,463. 34 The administrative town has one public comprehensive specialized hospital and three public health centers. Debre Markos Comprehensive Specialized Hospital (DMCSH) provides health services for over 5 million populations with 104 health centers and 10 district hospitals under its catchment. Obstetrics and Gynecology department of the hospital has 42 maternity ward beds, 6 first stage of labor ward beds, 4 second stage of labor coaches, and 4 recovery beds. There are 46 midwives, 1 clinical midwifery specialist, 1 emergency surgeon, 11 general practitioners, and 7 obstetrics and gynecology specialists in the department. DMCSH serves as a teaching institution for Debre Markos University, where undergraduate medical interns, midwifery, and nursing students were available providing maternity services under supervision at the time of data collection. The three health centers (Debre Markos health center, Hedassie health center, and Wuseta health center) have 5 midwives each and provides an average of 50 deliveries per month. All four public health institutions provide maternity services in the administrative town.
Population and sample size determination
The source population was all mothers who gave birth at public health institutions of Debre Markos town and the study population was randomly selected mothers who gave birth at public health institutions of Debre Markos town during the data collection period. The study included mothers who gave birth at public health institutions of Debre Markos town during the data collection period.
The sample size for the first objective was determined by using a single population proportion formula with the assumption of a standard normal distribution (Z) at 95% confidence level, margin of error (d) 5%, and 64.5% magnitude of PCMC during childbirth in a study conducted at Dessie town, Northeastern Ethiopia. 11
By considering a 10% non-response rate, the final sample size for the first objective was 387.
The adequacy of sample size for the second objective was computed by using G*Power version 3.1.9.7 software, G*Power Team; Heinrich Heine University Düsseldor, Düsseldor, Germany for sample size determination and power analysis. 35
Given the following parameters
Test family—F-test; Statistical test—Linear multiple regression: fixed model, R2 deviation from zero; Analysis—a priori: compute required sample size—given α, power, and effect size. Evaluate whether a group of factors significantly predicts the outcome variable. The null hypothesis is that the proportion of variance in the outcome variable explained by a set of predictors equals zero. That is, Ho: R2 = 0. Do the predictor variables (socio-demographic, obstetrics, health care provider, and health facility factors) predict the outcome variable? Determine effect size (f2) by assuming multiple correlation coefficient (R) of 0.3 for this research, as it was not specified in previous similar studies. Then R square (R2) was determined by squaring the R, R2 = (0.3) 2 = 0.09. Then, f2 was calculated by entering R2 value into the G*Power software and transferred to the main window (f2 = 0.0989011). 35 Finally, entering f² = 0.0989011, α = 0.05, power = 0.8, and number of predictors = 21 in the software yielded a minimum sample size requirement of 233 to run a multiple linear regression analysis, and an actual power of 0.8006560 which indicated that there was an 80% chance that R² would significantly differ from zero among 233 study participants. Considering a 10% non-response rate, the final sample size required for the second objective was 256. The sample size calculated for the first objective (387) was greater than the sample size required for the second objective (256). Therefore, the final sample size for this study was 387.
Sampling procedures
All public health institutions in the administrative town were included. The sample size for all health care facilities was allocated proportionately based on the number of previous 1 month childbirth services prior to the data collection period (Figure 1). The number of deliveries in all health facilities on April, 2022 was 792. Finally, participants in all health facilities were selected through systematic random sampling technique. The sampling interval, K was determined by dividing the total number of childbirths in all health facilities to the total sample size and this interval was used in all health facilities to enroll study participants. K = N/n, K = 792/387 = 2.01~2. The first participant was selected by lottery method from the first two delivered mothers and then every second of mothers was interviewed at each health facility.
Figure 1.
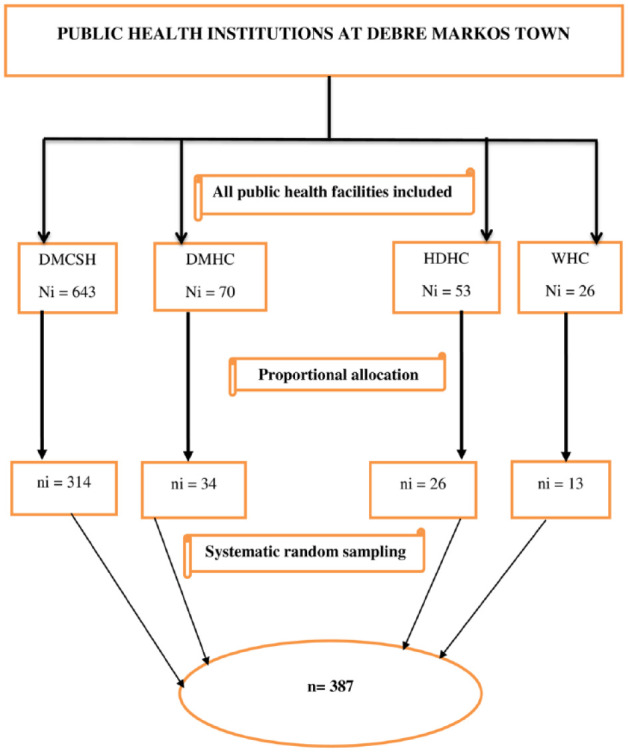
Schematic presentation of sampling procedures for person-centered maternity care at public health institutions of Debre Markos town, Northwest Ethiopia, 2022.
DMHC: Debre Markos Health Center; HDHC: Hedassie Health Center; WHC: Wuseta Health Center.
Study variables
The dependent variable was PCMC and independent variables were socio-demographic related factors (age of mothers, residence, educational level of women, occupation of women, marital status, educational level of husband, occupation of the husband, and average monthly income), obstetrics related factors (ANC follow-up, timing of ANC follow-up, frequency of ANC, place of ANC, parity, previous history of facility-based childbirths, mode of last delivery, time of delivery, complication during childbirth, and fetal outcome), health facility-related factors (type of health facility and length of stay at the facility), and healthcare provider-related factors (sex of delivery attendant) (Figure 2).
Figure 2.
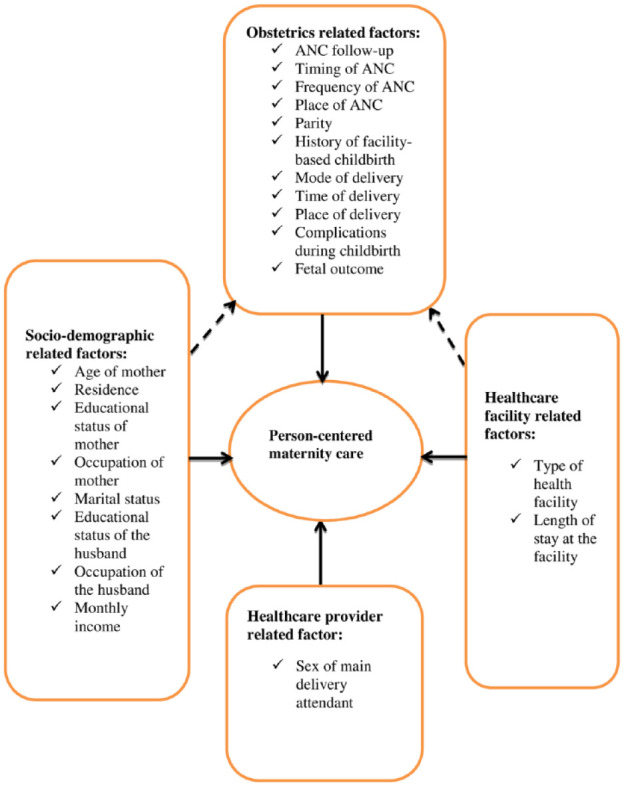
Conceptual framework showing factors associated with person-centered maternity care during childbirth among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia, 2022: adapted from related literatures.2,3,7,14,18,30
Operational definitions
Person-centered maternity care
PCMC was measured by using PCMC scale, which has three domains (sub-scales): dignity and respect (6 items), communication and autonomy (9 items), and supportive care (15 items), with a total of 30 items. Each item has a four-point frequency response scale, that is, 0 (“no, never”), 1 (“yes, a few times”), 2 (“yes, most of the time”) and 3 (“yes, all the time”). 3 Negatively phrased items such as physical abuse, verbal abuse, auditory privacy, and crowdedness of the room questions were reverse coded so that the highest score represents good care. The total PCMC score is generated as a summative score from the response to individual items, which ranges from a potential minimum score of 0 to a potential maximum score of 90. 3
Dignity and respect
Measured using six items, with each item having a four-point frequency response scale, the score ranges from 0 to 18. 3
Communication and autonomy
Measured using nine items, with each item having a four-point frequency response scale, the score ranges from 0 to 27. 3
Supportive care
Measured using 15 items, with each item having a four-point frequency response scale, the score ranges from 0 to 45. 3
The full PCMC scale and each sub-scale were sorted into “low, medium, and high” scores. Low was defined as scores in the approximate lower 25th percentile, whereas high was defined as scores in the upper 75th percentile.14,36 Finally, the mean PCMC score was compared with the 75th percentile and international standards to report as low or high PCMC.
Complication during childbirth
Having at least one complication during childbirth either on the mother or on the fetus such as severe vaginal bleeding, convulsion, labor lasting more than 12 h, foul-smelling vaginal discharge, high fever, retained placenta, and fetal distress.37,38
Data collection tools and procedures
Semi-structured interviewer-administered questionnaires including socio-demographic and obstetrics characteristics of participants, healthcare provider and health facility characteristics as well as the PCMC scale were employed to collect data from study participants. The PCMC measurement tool was validated in LMIC, initially in Kenya 3 and subsequently in India 2 and Turkey 13 to measure PCMC during childbirth, which was designed to be implemented on mothers who recently gave birth up to 9 weeks postpartum.2,3
The Cronbach’s alpha for the full PCMC scale was above 0.8, indicating that the scale had good internal consistency for reliability; and had high content, construct and criterion validity.2,3,13 Internal consistency reliability for this research was assessed using Cronbach’s alpha reliability coefficient for each sub-scale and the full PCMC scale, and it was 0.604 for dignity and respect, 0.736 for communication and autonomy, 0.737 for supportive care, and 0.82 for the full PCMC scale. The Cronbach’s alpha internal consistency reliability coefficient for this study of each sub-scale and the full PCMC scale was consistent with previous studies.2,3,11,13
A standardized, pre-tested, and semi-structured Amharic version questionnaire was used to collect data from mothers who gave birth at public health facilities of Debre Markos town. Data were collected through face-to-face exit interviews when postnatal mothers were discharged to home. The interview was made in a quiet and private room. Two MSc nurses and four BSc nurses were recruited for supervision and data collection respectively.
Data quality assurance
The questionnaire was first prepared in English and translated to Amharic, then translated back to English by language experts to ensure its consistency. Before the actual data collection, a pre-test was conducted on 5% (20 mothers) of the actual sample at Lumame Primary Hospital, and necessary modifications were made accordingly. One-day training was given for supervisors and data collectors regarding the purpose of the study, data collection procedures, the proper way of interacting with study participants, and data handling techniques. Data were checked daily for its completeness and consistencies by the principal investigator and supervisors.
Data processing and analysis
Data were checked for completeness, cleaned, coded and entered into EpiData statistical software version 3.1.2701.2008; EpiData Association, Odense, Denmark and exported to IBM® SPSS® ( Statistical Product and Service Solutions) version 25 for analysis. Descriptive statistics were generated, and the findings were presented using mean with standard deviation (SD) for normally distributed continuous variables and frequencies with percentages for categorical variables. Both simple and multivariable linear regression analyses were fitted to identify factors associated with the dependent variable.
Before fitting the linear regression model, the assumption of linearity was checked and satisfied by using a scatter plot. The normality of continuous data was tested and satisfied by plotting histograms and Q-Q plots. The result of histograms showed a bell-shaped, with only one peak, and is symmetric around the mean. The result of Q-Q plots also showed that all data sets lie closer to the diagonal line. The assumption of absence of outliers for continuous data was checked and satisfied by box plot chart, and hence no outliers were detected.
Multicollinearity was checked by variance inflation factor (VIF) (acceptable range <10, best if <5) and tolerance test (acceptable range >0.1, best if >0.2),39,40 bivariate correlation was checked by Pearson correlation coefficient (acceptable range <0.8). Therefore, for this data, the maximum VIF was 3.66, the minimum tolerance test was 0.27, and the maximum correlation coefficient was 0.61. The assumption of homoscedasticity was tested and satisfied by plotting two scatter plots of standardized residuals (ZRESID) against the standardized predicted values (ZPRED) and it was fairly distributed.
The assumption of independence of residual values (errors terms) was checked by the Durbin Watson statistic (acceptable range is 1.5 to 2.5). Hence, the value of Durbin Watson statistic for this data was 1.99. Therefore, this analysis satisfied the assumption of independence and no autocorrelations of residual values. The normality of residual values was tested and satisfied by plotting a P-P plot of standardized residuals. Therefore, the P-P plot showed the closeness of each dot to the diagonal line, indicating the normal distribution of residual values. The Cook’s distance values were all under 1 (minimum 0, maximum 0.032), which suggests individual cases were not unduly influencing the model.
Independent samples T-test and one-way analysis of variance (ANOVA) for mean comparison as well as Leven’s test for tests of homogeneity of variances. 39 across the various socio-demographic and obstetrics characteristics of study participants, as well as healthcare provider and facility characteristics were generated. Hypothesis testing was performed by p-value for the individual regression coefficient, and by F-statistic and coefficient of determination (R2) to the overall significance of the model.
The model fitness was checked by multiple correlation coefficient (R) and ANOVA test significance. Hence, the value of multiple correlation coefficient for this data was 0.61 and the p-value of the ANOVA test was <0.001. Simple and multivariable linear regression analyses were fitted after creating n−1 dummy variables. Those variables with a p-value ⩽ 0.25 in simple linear regression analysis were fitted into the multivariable linear regression model by enter method, and p-value < 0.05 was considered statistically significant with 95% CI for unstandardized adjusted β. Finally, the findings of the study were compiled and presented using texts, tables, and figures.
Results
Out of the total sample size, 380 women participated in this study with a response rate of 98.19%. Three questionnaires were found incomplete and excluded from the analysis. Four women were rushed to home as the decision to discharge was made after they told the data collectors they could not wait until the precedent women were interviewed.
Socio-demographic characteristics of respondents
From the total number of women who agreed to participate in this study, less than one-third, 154 (40.5%) participants were 25–29 years of age. The mean age of study participants was 27.99 with SD ±4.79 years. More than three-fourth, 313 (82.4%) participants were urban dwellers. Regarding the educational level of women, about 98 (25.8%) of participants had college and above level of education. Almost all, 366 (96.3%) of participants were married. Nearly one-third, 116 (31.7%) of participants’ husbands had college and above educational level. The respondents’ estimated mean monthly income was 6910 Ethiopian Birr (Table 1).
Table 1.
Socio-demographic characteristics of mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| Variable | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age of mothers (in years) | 16–24 | 91 | 23.9 |
| 25–29 | 154 | 40.5 | |
| ⩾30 | 135 | 35.5 | |
| Residence | Urban | 313 | 82.4 |
| Rural | 67 | 17.6 | |
| Educational level of women | No formal education | 47 | 12.7 |
| Primary school | 67 | 17.6 | |
| Secondary school | 168 | 44.2 | |
| College and above | 98 | 25.8 | |
| Occupation of women | House wife | 185 | 48.7 |
| Private employee | 16 | 4.2 | |
| Government employee | 102 | 26.8 | |
| Merchant | 63 | 26.6 | |
| Others a | 14 | 3.2 | |
| Marital status | Single | 14 | 3.7 |
| Married | 366 | 96.3 | |
| Educational status of husband (n = 366) | No formal education | 50 | 13.7 |
| Primary school | 69 | 18.9 | |
| Secondary school | 131 | 35.8 | |
| College and above | 116 | 31.7 | |
| Occupation of husband (n = 366) | Farmer | 38 | 10.4 |
| Private employee | 46 | 12.6 | |
| Government employee | 142 | 38.8 | |
| Merchant | 103 | 28.1 | |
| Others b | 37 | 10.1 |
Students, daily laborer.
Daily laborer, deriver, unemployed.
Obstetrics, provider and health facility characteristics of respondents
The findings of this research indicated that almost all, 373 (98.2%) of study participants had a history of ANC follow-up for their last delivery. Among these, more than one-third, 150 (40.2%) and about 48 (12.9%) of respondents commenced their ANC follow-up during the first and third trimester of pregnancy respectively. Nearly three-fourth, 274 (72.1%) of participants were multiparous. Less than half, 167 (43.9%) of women were delivered their last baby by caesarean section. Nearly two-thirds, 247 (65.0%) of mothers were delivered during nighttime and more than three-fourth, 308 (81.1%) of mothers were delivered at hospital. About 64 (16.8%) of women faced childbirth complications. Almost two-thirds, 250 (65.8%) of women stayed more than 24 h at the health institutions (Table 2).
Table 2.
Obstetrics, provider and facility characteristics among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| Variable | Category | Frequency | Percentage (%) |
|---|---|---|---|
| ANC follow-up | Yes | 373 | 98.2 |
| No | 7 | 1.8 | |
| Timing of first ANC follow-up (n = 373) | First trimester | 150 | 40.2 |
| Second trimester | 175 | 46.9 | |
| Third trimester | 48 | 12.9 | |
| Frequency of ANC follow-up (n = 373) | <4 | 139 | 36.6 |
| ⩾4 | 234 | 61.6 | |
| Place of ANC follow-up (n = 373) | Hospital | 125 | 33.5 |
| Health center | 212 | 56.8 | |
| Private clinic | 34 | 9.1 | |
| Health post | 2 | 0.5 | |
| Parity | Primiparous | 106 | 27.9 |
| Multiparous | 274 | 72.1 | |
| History of facility-based childbirth | Yes | 174 | 45.8 |
| No | 206 | 54.2 | |
| Mode of last delivery | Normal vaginal | 175 | 46.1 |
| Instrumental | 38 | 10.0 | |
| Caesarean section | 167 | 43.9 | |
| Sex of delivery attendant | Male | 194 | 51.1 |
| Female | 73 | 19.2 | |
| Both (male and female) | 113 | 29.7 | |
| Time of delivery | Day time | 133 | 35.0 |
| Night time | 247 | 65.0 | |
| Type of facility where the last delivery conducted | Hospital | 308 | 81.1 |
| Health center | 72 | 18.9 | |
| Complication during childbirth | Yes | 64 | 16.8 |
| No | 316 | 83.2 | |
| On whom complications occurred | Maternal | 29 | 45.3 |
| Neonatal | 22 | 34.4 | |
| Maternal and neonatal | 13 | 20.3 | |
| Fetal outcome | Alive | 370 | 97.4 |
| Dead | 10 | 2.6 | |
| Length of stay at health facilities | 24 h or less | 130 | 34.2 |
| More than 24 h | 250 | 65.8 |
PCMC scale and sub-scales
The respondents’ mean PCMC score was 56.83, 95% CI: (55.83, 57.83) with SD ± 9.94 from 90. The minimum and maximum score for PCMC was 31 and 84 respectively (out of 90).
Percentage standardization of the mean PCMC score was made by the following formula;
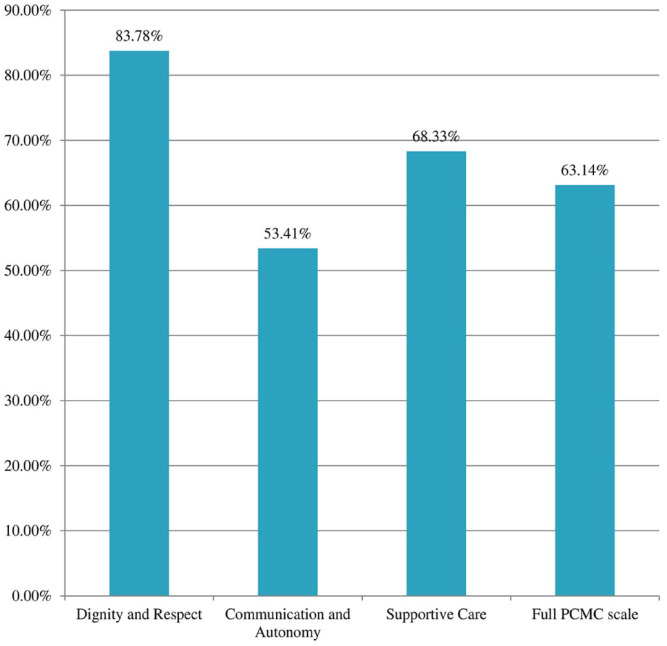
Therefore, the respondent’s percentage mean score for the full PCMC scale was 63.14% of the total expected score. Whereas the percentage mean sub-scale scores were 83.78% for dignity and respect, 53.41% for communication and autonomy, and 68.33% for supportive care (Figure 3).
Figure 3.
Distribution of percentage mean score for the full PCMC scale and sub-scales from the total expected score among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia, 2022.
Distribution of PCMC scale and sub-scales
All in all, as shown in (Table 3) Most women received a medium score on the full PCMC and on each sub-scale. Whereas as shown in (Table 4) lower than a quarter, 84 (22.1%) of women received a high PCMC whereas nearly over a quarter, 98 (25.8%) of women had a low PCMC. About 75 (19.7%) of women had a high score, while nearly over a quarter, 98 (25.8%) had a low score on the dignity and respect sub-scale. Nearly a quarter, 90 (23.7%) had a high score on the communication and autonomy sub-scale. About 86 (22.6%) of women had a high score on the supportive care sub-scale.
Table 3.
Descriptive statistics of person-centered maternity care at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| PCMC domain | Minimum | Maximum | Mean | SD | Percentiles | ||
|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | |||||
| Full PCMC score | 31 | 84 | 56.83 | 9.94 | 50 | 57 | 64 |
| Dignity and respect | 8 | 18 | 15.08 | 2.42 | 13 | 15 | 17 |
| Communication and autonomy | 4 | 27 | 14.42 | 4.85 | 11 | 14 | 17 |
| Supportive care | 12 | 40 | 27.33 | 5.55 | 24 | 27 | 32 |
Table 4.
Total and sub-scale score of person-centered maternity care at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| Outcome variable | Frequency | Percentage |
|---|---|---|
| Full PCMC scale | ||
| Low | 98 | 25.8 |
| Medium | 198 | 52.1 |
| High | 84 | 22.1 |
| Dignity and respect | ||
| Low | 98 | 25.8 |
| Medium | 207 | 54.5 |
| High | 75 | 19.7 |
| Communication and autonomy | ||
| Low | 118 | 31.0 |
| Medium | 172 | 45.3 |
| High | 90 | 23.7 |
| Supportive care | ||
| Low | 117 | 30.8 |
| Medium | 177 | 46.6 |
| High | 86 | 22.6 |
Dignity and respect
The mean score for dignity and respect of the study participants was 15.08 (SD ± 2.42) from 18. More than half, 211 (55.5%) of women were treated with respect all the time and 204 (53.7%) of women were treated in a friendly manner by healthcare providers. About 57 (15.0%) and 22 (5.8%) of women experienced verbal and physical abuse at least one time respectively. Regarding auditory privacy and confidentiality of health information, a quarter, 95 (25.0%) and about 76 (20.0%) of women reported their auditory privacy and health information was kept confidential a few times respectively (Table 5).
Table 5.
Distribution of dignity and respect at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| Items | No, never (%) | Yes, a few times (%) | Yes, most of the time (%) | Yes, all the time (%) |
|---|---|---|---|---|
| Treated with respect | 5 (1.3) | 37 (9.8) | 127 (33.4) | 211 (55.5) |
| Treated in a friendly manner | 7 (1.8) | 45 (11.9) | 124 (32.6) | 204 (53.7) |
| Providers shouted, scolded, insulted, talked to me rudely (RC) | 315 (82.9) | 57 (15.0) a | 8 (2.1) | 0 |
| Treated roughly like pushed, slapped, physically restrained (RC) | 356 (93.7) | 22 (5.8) | 2 (0.5) | 0 |
| People not involved in care hear the discussion with provider (RC) | 239 (62.9) | 95 (25.0) | 31 (8.2) | 15 (3.9) |
| Health information kept confidential | 27 (7.1) | 76 (20.0) | 124 (32.6) | 153 (40.3) |
RC: reverse coded.
Showed (yes, a few times) was changed to (yes, at least once).
Communication and autonomy
The mean score for communication and autonomy of the respondents was 14.42 (SD ± 4.85) out of 27. Nearly two-thirds, 245 (64.5%) of respondents reported that providers never introduced themselves during their stay at a health facility. Thirty-one (8.2%) of respondents reported healthcare providers never called them by their names. More than a quarter, 105 (27.6%) of women reported that they were involved in decisions about their care, while 33 (8.7%) reported they were never involved in decisions about their care by providers. More than half, 204 (53.7%) of women reported that healthcare providers never allowed their position of choice during delivery (Table 6).
Table 6.
Distribution of communication and autonomy at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| Items | No, never (%) | Yes, a few times (%) | Yes, most of the (%) | Yes, all the time (%) |
|---|---|---|---|---|
| Providers introduced themselves a | 245 (64.5) | 65 (17.1) | 47 (12.4) | 23 (6.0) |
| Providers called me by my name a | 31 (8.2) | 140 (36.8) | 136 (35.8) | 73 (19.2) |
| Feel involved in decisions about my care | 33 (8.7) | 80 (21.1) | 162 (42.6) | 105 (27.6) |
| Permission to examinations and procedures | 73 (19.2) | 60 (15.8) | 148 (38.9) | 99 (26.1) |
| Allowed position of choice | 204 (53.7%) | 71 (18.7) | 66 (17.4) | 39 (10.2) |
| Providers spoke in a language I can understand | 4 (1.1) | 13 (3.4) | 46 (12.1) | 317 (83.4) |
| Examinations and procedures explained | 86 (22.6) | 85 (22.4) | 123 (32.4) | 86 (22.6) |
| Purpose of medicine was explained b | 81 (21.4) | 103 (27.2) | 129 (34.1) | 65 (17.3) |
| I could ask any questions I had | 41 (10.8) | 75 (19.7) | 139 (36.6) | 125 (32.9) |
The choice of the item was changed into (no, none of them; yes, few of them; yes, most of them; and, yes, all of them).
Didn’t get any medicine 2 (0.5%).
Supportive care
The mean score for supportive care of the study participants was 27.33 (SD ± 5.55) from 40. The majority of women were not given continuous support during labor and delivery, while half, 190 (50.0%) of them were not allowed labor companion and most, 327 (86.1%) were delivered without delivery companion. Forty-seven (12.4%) of women reported providers never talked to them about their feeling, while nearly a quarter, 84 (22.1%) of women reported providers talked to them about their feeling all the time. Less than half, 157 (41.3%) of women trust health professionals with regards to their care. About 164 (43.2%) participants felt safe during their stay in the facility, and most 332 (87.4%) of women reported the facility was clean (Table 7).
Table 7.
Distribution of supportive care at public health institutions of Debre Markos town, Northwest Ethiopia, 2022 (n = 380).
| Items | No, never (%) | Yes, a few times (%) | Yes, most of the time (%) | Yes, all the time (%) |
|---|---|---|---|---|
| Allowed labor companion | 190 (50.0) | 119 (31.3) | 61 (16.1) | 10 (2.6) |
| Allowed delivery companion | 327 (86.1) | 35 (9.2) | 13 (3.4) | 5 (1.3) |
| Providers talk to me about my feeling | 47 (12.4) | 66 (17.4) | 183 (48.1) | 84(22.1) |
| Providers supported me when I had anxieties | 34 (8.9) | 69 (18.2) | 188 (49.5) | 89 (23.4) |
| Feel providers did their best to control my pain | 15 (3.9) | 48 (12.6) | 208 (54.8) | 109 (28.7) |
| Providers paid attention when I needed help | 19 (5.0) | 66 (17.4) | 154 (40.5) | 141 (37.1) |
| Providers took the best care of me | 4 (1.1) | 51 (13.4) | 162 (42.6) | 163 (42.9) |
| Trust providers with regards to care | 5 (1.3) | 53 (14.0) | 165 (43.4) | 157 (41.3) |
| There were enough providers to care for me | 7 (1.8) | 49 (12.9) | 118 (31.1) | 206 (54.2) |
| Feel the facility was crowded (RC) | 46 (12.1) | 95 (25.0) | 152 (40.0) | 87 (22.9) |
| There was water in the facility | 50 (13.1) | 66 (17.4) | 133 (35.0) | 131 (34.5) |
| There was electricity in the facility | 0 | 10 (2.6) | 90 (23.7) | 280 (73.7) |
| Feel safe in the facility | 20 (5.3) | 80 (21.0) | 116 (30.5) | 164 (43.2) |
| Feeling about waiting time | Very long (%) | Somewhat long (%) | Little long (%) | Very short (%) |
| 32 (8.4) | 168 (44.2) | 96 (25.3) | 84 (22.1) | |
| General environment of the facility | Very dirty (%) | Dirty (%) | Clean (%) | Very clean (%) |
| 2 (0.5) | 10 (2.6) | 332 (87.4) | 36 (9.5) |
RC: reverse coded.
Factors associated with PCMC
In simple linear regression analysis; residence, educational status of women, occupation of women, marital status, educational level of the husband, timing of ANC follow-up, frequency of ANC, parity, mode of last delivery, sex of main delivery attendant, place of last delivery, complication during childbirth, and fetal outcome were factors significantly associated with PCMC.
In multivariable linear regression analysis; by accounting for other factors, women’s level of education, timing of ANC follow-up, parity, mode of last delivery, and place of last delivery were factors significantly associated with PCMC.
Keeping all other variables constant, mothers with college and above level of education had an increased PCMC score by a factor of 3.75 times when compared to mothers who had no formal education (β = 3.75, 95% CI: 1.11, 6.39). With a net of other factors, women who commenced ANC follow-up during the third trimester had a decreased PCMC score by a factor of 4.86 times (β = −4.86, 95% CI: −8.22, −1.49) as compared to those who initiated during the first trimester of pregnancy. Multiparous women had an increased PCMC score by a factor of 3.69 times as compared to primiparous women (β = 3.69, 95% CI: 1.85, 5.55). Women who gave birth by caesarean section had a decreased PCMC care score by a factor of 5.78 time as compared to those who gave birth by normal vaginal delivery (β = −5.78, 95% CI: −7.68, −3.87). Women who gave birth at health centers had an increased PCMC score by a factor of 6.59 times when compared to those who gave birth at a government hospital (β = 6.59, 95% CI: 4.17, 9.02) (Table 8).
Table 8.
Multivariable linear regression analysis of factors affecting person-centered maternity care, Debre Markos town, Ethiopia, 2022 (n = 380).
| Variable | Category | Unstandardized adjusted β coefficients | 95% CI for β |
|---|---|---|---|
| Residence | Constant | 54.89 | (52.07, 57.70)*** |
| Urban | 1 | 1 | |
| Rural | −0.59 | (−3.13, 1.96) | |
| Women’s educational level | No formal education | 1 | 1 |
| Secondary school | 1.39 | (−0.64, 3.43) | |
| College and above | 3.75 | (1.11, 6.39)** | |
| Women’s occupation | House wife | 1 | 1 |
| Government employee | −0.11 | (−2.22, 2.00) | |
| Husbands’ education level | No formal education | 1 | 1 |
| College and above | 1.61 | (−0.34, 3.55) | |
| Timing of ANC follow-up | First trimester | 1 | 1 |
| Second trimester | −1.64 | (−3.47, 0.19) | |
| Third trimester | −4.86 | (−8.22, −1.49)** | |
| Frequency of ANC | <4 | 1.38 | (−0.67, 3.43) |
| ⩾4 | 1 | 1 | |
| Parity | Primiparous | 1 | 1 |
| Multiparous | 3.69 | (1.85, 5.55)*** | |
| Mode of last delivery | Normal vaginal | 1 | 1 |
| Instrumental | −2.14 | (−5.03, 0.76) | |
| Caesarean section | −5.78 | (−7.68, −3.87)*** | |
| Sex of main delivery attendant | Male | 1 | 1 |
| Both (male and female) | −1.54 | (−3.39, 0.32) | |
| Time of delivery | Daytime | 1 | 1 |
| Nighttime | −2.82 | (−4.27, −1.36) | |
| Place of last delivery | Hospital | 1 | 1 |
| Health center | 6.59 | (4.17, 9.02)*** | |
| Childbirth complication | Yes | −1.21 | (−2.28, 3.69) |
| No | 1 | 1 | |
| Fetal outcome | Alive | 1 | 1 |
| Dead | −1.62 | (−7.21, 3.98) |
1: reference; CI: confidence interval.
*Significant at p-value < 0.01, ***Significant at p-value < 0.001.
Discussion
This study attempted to investigate the magnitude of PCMC during childbirth and associated factors among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia. The findings of this study found that the mean score for PCMC was 56.83 with SD of ±9.94. The highest score was on the dignity and respect sub-scale whereas the least score was on the communication and autonomy sub-scale followed by the supportive care sub-scale. This showed that health care professionals at public health facilities of Debre Markos town established inadequate rapport with prospective mothers and rarely allowed a position of women’s choice as well as labor and delivery companion.
The finding of this research revealed that PCMC was low as compared to the 75th percentile of the validated measurement tool. The result of this study was also low when compared with studies done in Dessie Ethiopia, urban Kenya, Migori region Kenya, and Nairobi Kenya which showed the mean PCMC scores were 58, 60.2, 62, and 58.2 respectively.3,11,15,30 The possible justification might be due to the variation in study setting (where private and faith-based health facilities were not included in this study as compared to studies done in Ethiopia and Nairobi, Kenya), sample size (where the study conducted in urban Kenya had the largest sample size), population characteristics (where 53% of Kenyan women were employed as compared to 19% in this study), and the quality of maternity care and health professional training may be better in Kenya. Additionally, undergraduate medical interns, midwifery, and nursing students were engaged in maternity service provision in this study of hospital settings, which likely decreased the provision of PCMC.
However, the result of this study was higher than studies done in rural Ghana, Nigeria, Sri Lanka, India, and Turkey where the mean PCMC scores were 46.5, 49.07, 42.3, 50.3, and 39.96 respectively.2,7,9,13,14 The possible reason for this discrepancy could be due to variation in study period, sample size (small sample in Ghana and Turkey), measurement tool (where a 22, 27, and 21 item scale were used in Nigeria, India, and Turkey respectively when compared to a 30 item scale used in this study), socio-cultural difference, quality of maternity care, population characteristics (most women, 75% in rural Ghanaian had no formal education when compared to 15% in the current study), and study setting (only one higher level hospital in Sri Lanka, and rural health facilities were included in Ghana and India).
In this study, women had a highest score on the dignity and respect dimension was due to women having high experience on respectful care (55.5%), friendly care (53.7%), auditory privacy being maintained (62.9%), and no experience of verbal abuse (82.9%) and physical abuse (93.7%). This finding is equivalent to existing studies.2,7,11,14 The possible justification might be due to implementation of interventions to enhance respectful maternity care. Whereas, the lowest score on communication and autonomy dimension was due to the fact that providers never introduced themselves (64.5%), providers rarely called women by their names, less involvement of women in decisions regarding their care, limited permission to examinations and procedures, not allowed a position of women’s choice (53.7%), inadequate explanation of examinations and procedures (22.6%) as well as medicines (21.3%), which is in accordance with existing literatures.9,11,14 However, it is lower than other evidences2,7 which likely is due to the larger sample size in previous studies. A low score on the supportive care sub-scale was highlighted due to limited allowance of companions during labor (50.0%, never allowed) and delivery (86.1%, never allowed) and providers rarely talked to women about how they felt. This finding is in line with previous evidence.7,11,30
When compared with international standards (benchmarks) of maternal and newborn healthcare quality guidelines, the finding of this study is lower than the WHO standards for improving quality of maternal and newborn care in health facilities. 6 This emphasized how much work has to be done to ensure that healthcare facilities in Debre Markos town rendered quality care for expectant mothers and newborns in order to fulfill the WHO standards of quality of maternal and newborn care. Among the 8 standards, standards 4–6 highlighted the three dimensions of PCMC that women experienced during childbirth. Although standard 4 accounts for the value of effective communication and autonomy, less rapport of professionals to women, not allowed women’s position of choice, less involvement of women in decisions regarding their care, and inadequate explanation of examinations and procedures are commonplace in this study. Respect and preservation of women’s dignity is the focus of standard 5. When women asked whether they were treated with respect and in a friendly manner, they gave a more positive response; yet, auditory privacy and confidentiality of record keeping were not always maintained. Although it is far lower than standard 5, more than half of women were treated with respect in a friendly manner. Standard 6 deals with providing emotional support that is sensitive and responsive to women’s needs and enhances their capabilities. It was observed in this study that half of women and most women were not allowed labor and delivery companions respectively.
The result of this study showed college and above educated women had a higher PCMC score as compared to those women who had no formal education (β = 3.75, 95% CI: 1.11, 6.39). This finding is consistent with a study done in LMIC (Kenya and India) where college educated women had an increased PCMC score than women who had no formal education. 7 This result is also in agreement with a study conducted in peri-urban Kenya where education was replaced by literacy, which revealed that literate women had a higher PCMC score as compared to illiterate women. 30 The possible explanation could be due to the fact that more educated women are more likely to have good communication skills, so that they can easily communicate with healthcare providers and settle for an enhanced experience of care at healthcare institutions. 30 In addition, more educated women may have greater empowerment to ask questions regarding their rights and deal with providers to receive better care at health institutions. Furthermore, educated women are more likely to have a good health-seeking behavior through the capability to make better healthcare decisions, economic independence, and healthcare cognizance. 41
This study depicted that the later women commenced ANC, the more likely their PCMC score became decreased, indicating a more negative experience during labor and delivery. Women who commenced ANC follow-up during the third trimester had a decreased PCMC score by a factor of 4.86 times as compared to those women who initiated during the first trimester of pregnancy (β = −4.86, 95% CI: −8.22, −1.49). This result is in accordance with studies conducted in Kenya and Nigeria.14,30 The possible justification could be due to the fact that seeking early ANC follow-up is related to a positive childbirth experience, because women can get timely ANC services that can prevent, identify, and manage pregnancy and delivery complications.42,43 That is, failing to commence ANC in early pregnancy is associated with a possible risk of complications during pregnancy and childbirth. In addition, late initiation of ANC is related with less familiarity to the healthcare system14,44 so that women could not demonstrate a good relationship with their healthcare providers and could not get appropriate counseling which ultimately leads to a negative childbirth experience. 30
This study finding indicated that with an increase in parity, PCMC increases. Multiparous women had a higher PCMC score by a factor of 3.69 times as compared to primiparous women (β = 3.69, 95% CI: 1.85, 5.55). This is in agreement with studies conducted in Ethiopia and Palestine.29,45 This may be due to the fact that women with high parity may be accustomed to the healthcare system, healthcare providers, childbirth process, and the different and repeated procedures performed on them 29 so that they are capable to communicate appropriately with healthcare providers regarding their care. Furthermore, primiparous women may manifest anxiety and fears about the childbirth experience as they are exposed the first time to healthcare providers. 45
Concerning the mode of delivery, this study highlighted mothers who gave birth by caesarean section had a decreased PCMC score by a factor of 5.78 times as compared to those who gave birth by normal vaginal delivery (β = −5.78, 95% CI: −7.68, −3.87). This finding is in accordance with a study done in Bahir Dar, Ethiopia. 33 The possible justification could be due to those mothers who gave birth by caesarean section are more likely to suffer from pain after delivery, experience prolonged and more difficult postnatal recovery period, 46 and anesthetic complications as compared to those mothers who delivered by normal vaginal delivery.
Even though the quality of healthcare service provision is high in higher-level facilities than lower-level facilities, in this study women who gave birth at health centers experienced a higher PCMC score as compared to those who gave birth at a public hospital (β = 6.59, 95% CI: 4.17, 9.02). This finding is in line with studies conducted in western Kenya, rural and urban Kenya, Nigeria, and India.7,14,18 The possible reason might be due to healthcare providers having closer approach to mothers as health centers have lower patient load which likely decreases the strain of providers on their interaction with women. 18 Besides, medical and health science students were not engaged in maternity service provision at health centers of this study. This is supported by a study conducted in Ethiopia where students’ involvement in facility-based deliveries decreases the provision of PCMC. 45
Limitation and strength of the study
One of the limitations of this study was its dependency on self-reported data. Even though the PCMC measurement scale was constructed to decrease subjectivity by phrasing its questions and response options in a way that evokes factual information, it may bring out a certain degree of subjectivity. Another limitation of this study was that the cause-and-effect relationship cannot be established due to the nature of cross-sectional study design. As strength, all public health facilities were included and recall bias may be minimized because data were taken on exit interviews.
Conclusion and recommendation
The findings of this research showed that PCMC was low as compared with the 75th percentile of the validated measurement tool and when compared to WHO standards for quality maternity care. This finding renders evidence to local policy makers, district health offices, institutional healthcare administrators, and healthcare professionals about the discrepancies in achieving international standards for quality maternity care. This result showed how important it is to reinforce the provision of PCMC during childbirth, specifically in communication and autonomy as well as supportive care domains.
This study further points out that being multiparous and enhanced women’s education level are empowering factors for women to receive better PCMC. Whereas, women who underwent caesarean section delivery and women who initiated ANC follow-up in the late trimester reported poor PCMC during childbirth. Further research should be conducted with large-scale and mixed methods combined with observational studies so as to deliver more complete information that helps policy makers and program planners to develop guidelines and strategies to implement PCMC in maternity care services.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121231225352 for Person-centered maternity care during childbirth and associated factors among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia, 2022: A cross-sectional study by Yaregal Admasu Alelign, Misganaw Fikrie Melesse, Endihnew Beka, Addisu Alehegn Alemu, Neway Ejigu Meskele and Chernet Getnet Asres in SAGE Open Medicine
Acknowledgments
First and foremost, the authors would like to thank Debre Markos University, College of Health Sciences Department of Midwifery for letting us conduct this research. Next, our deepest gratitude extends to Debre Markos town administration health office and Debre Markos Comprehensive Specialized Hospital staff for their facilitation and collaboration. Finally, we cordially acknowledge all respected study participants, supervisors, and data collectors for their invaluable dedication throughout the entire data collection period.
Footnotes
Authors’ contributions: Conceptualization: YAA and NEM. Methodology: YAA, MFM, EB, AAA, and CGA. Software: YAA, NEM, AAA, and CGA. Data curation: YAA, EB, AAA, and NEM. Formal analysis: YAA, MFM, CGA, and NEM. Supervision: YAA, EB, AAA, MFM, CGA, and NEM. Validation: YAA, MFM, AAA, EB, CGA, and NEM. Visualization: YAA, MEM, EB, AAA, CGA, and NEM. Writing original draft: YAA, MFM, and EB. Writing of review and editing: YAA, MFM, AAA, EB, CGA, and NEM. The authors read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: Ethical approval was obtained from the Institutional Research Ethics Review Committee of Debre Markos University College of Health Sciences with a reference number HSC/R/C/Ser/PG/Co/157/11/14. Permission to conduct the study was also obtained from Debre Markos town administration health office and DMCSH medical director. Study participants were asked for their willingness to participate in the study after explaining the purpose of the study. They were informed that they are free to withdraw from the study at any time, and withdrawal from the study did not in any way affect the facility related activities of the participant or any relationship with the staff. Written informed consent was taken from volunteer study participants. For participants under 18 years old, written informed consent was obtained from parents or legally authorized representatives. For participants with no formal education, written informed consent was obtained by taking their fingerprints after the interviewers read the consent form to them and agreed to participate. The data for this research were collected in accordance with the Declaration of Helsinki. Confidentiality and anonymity were ascertained by using codes other than any personal identifiers throughout the process of the study.
Consent for publication: Not applicable.
Trial registration: Not applicable.
ORCID iDs: Yaregal Admasu Alelign  https://orcid.org/0009-0008-5627-8761
https://orcid.org/0009-0008-5627-8761
Misganaw Fikrie Melesse  https://orcid.org/0000-0002-6343-7651
https://orcid.org/0000-0002-6343-7651
Neway Ejigu Meskele  https://orcid.org/0000-0002-4139-5649
https://orcid.org/0000-0002-4139-5649
Availability of data and materials: The datasets used and analyzed in this study are not publicly available because we did not get consent for publication of raw data from study participants but are available and will be provided from the corresponding author upon reasonable request without undue reservation.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Sudhinaraset M, Afulani P, Diamond-Smith N, et al. Advancing a conceptual model to improve maternal health quality: the person-centered care framework for reproductive health equity. Gates Open Res 2017; 1: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Afulani PA, Diamond-Smith N, Phillips B, et al. Validation of the person-centered maternity care scale in India. Reprod Health 2018; 15(1): 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Afulani P, Diamond-Smith N, Golu G, et al. Development of a tool to measure person-centered care during labor and delivery in developing settings: validation in a rural and urban Kenyan population. Reprod Health 2017; 14: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tunçalp Ӧ, Were WM, MacLennan C, et al. Quality of care for pregnant women and newborns—the WHO vision. BJOG 2015; 122(8): 1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oladapo O, Tunçalp Ö, Bonet M, et al. WHO model of intrapartum care for a positive childbirth experience: transforming care of women and babies for improved health and wellbeing. BJOG 2018; 125(8): 918–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. Standards for improving quality of maternal and newborn care in health facilities. https://iris.who.int/handle/10665/249155 (2016, accessed 2 April 2022)
- 7. Afulani PA, Phillips B, Aborigo RA, et al. Person-centred maternity care in low-income and middle-income countries: analysis of data from Kenya, Ghana, and India. Lancet Glob Health 2019; 7(1): 96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fahy K. What is woman-centred care and why does it matter? Women Birth 2012; 25(4): 149–151. [DOI] [PubMed] [Google Scholar]
- 9. Rishard M, Fahmy FF, Senanayake H, et al. Correlation among experience of person-centered maternity care, provision of care and women’s satisfaction: cross sectional study in Colombo, Sri Lanka. PLoS One 2021; 16(4): e0249265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization. WHO recommendations on intrapartum care for a positive childbirth experience. Geneva: World Health Organization, 2018. [PubMed] [Google Scholar]
- 11. Dagnaw FT, Tiruneh SA, Azanaw MM, et al. Determinants of person-centered maternity care at the selected health facilities of Dessie town, Northeastern, Ethiopia: community-based cross-sectional study. BMC Pregnancy Childbirth 2020; 20(1): 524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sudhinaraset M, Giessler K, Golub G, et al. Providers and women’s perspectives on person-centered maternity care: a mixed methods study in Kenya. Int J Equity Health 2019; 18(1): 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Özşahin Z, Altiparmak S, Aksoy Derya Y, et al. Turkish validity and reliability study for the person-centered maternity care scale. J Obstetr Gynaecol Res 2021; 47(9): 3211–3222. [DOI] [PubMed] [Google Scholar]
- 14. Ogbuabor D, Nwankwor C. Perception of person-centred maternity care and its associated factors among post-partum women: evidence from a cross-sectional study in Enugu State, Nigeria. Int J Public Health 2021; 66: 612894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Odiase O, Akinyi B, Kinyua J, et al. Community perceptions of person-centered maternity care in Migori County, Kenya. Front Glob Womens Health 2021; 2: 668405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bohren MA, Hunter EC, Munthe-Kaas HM, et al. Facilitators and barriers to facility-based delivery in low-and middle-income countries: a qualitative evidence synthesis. Reprod Health 2014; 11(1): 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016; 388(10056): 2176–2192. [DOI] [PubMed] [Google Scholar]
- 18. Afulani PA, Sayi TS, Montagu D. Predictors of person-centered maternity care: the role of socioeconomic status, empowerment, and facility type. BMC Health Serv Res 2018; 18(1): 360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016; 387(10017): 462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. WHO, UNICEF, UNFPA, etal. Trends in maternal mortality: 1990–2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva, Switzerland: World Health Organization, 2015. [Google Scholar]
- 21. EPHI. Ethiopia mini demographic and health survey 2019: key indicators. Rockville, MD: EPHI and ICF, 2019. [Google Scholar]
- 22. WHO. Maternal mortality: levels and trends 2000 to 2017. Geneva, Switzerland: World Health Organization, 2019. [Google Scholar]
- 23. Kiti G, Prata N, Afulani PA. Continuous labor support and person-centered maternity care: a cross-sectional study with women in rural Kenya. Matern Child Health J 2022; 26(1): 205–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Montagu D, Giessler K, Nakphong MK, et al. Results of a person-centered maternal health quality improvement intervention in Uttar Pradesh, India. PLoS One 2020; 15(12): e0242909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Byford-Richardson L, Walker M, Muckle W, et al. Barriers to access of maternity care in Kenya: a social perspective. J Obstetr Gynaecol Canada 2013; 35(2): 125–130. [DOI] [PubMed] [Google Scholar]
- 26. Abuya T, Sripad P, Ritter J, et al. Measuring mistreatment of women throughout the birthing process: implications for quality of care assessments. Reprod Health Matters 2018; 26(53): 48–61. [DOI] [PubMed] [Google Scholar]
- 27. Bohren MA, Hofmeyr GJ, Sakala C, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev 2017; 2017(7): CD003766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Afulani PA, Aborigo RA, Nutor JJ, et al. Self-reported provision of person-centred maternity care among providers in Kenya and Ghana: scale validation and examination of associated factors. BMJ Glob Health 2021; 6(12): e007415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dwekat IMM, Ismail TAT, Ibrahim MI, et al. Mistreatment of women during childbirth and associated factors in northern West Bank, Palestine. Int J Environ Res Public Health 2022; 19(20): 13180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Oluoch-Aridi J, Afulani P, Makanga C, et al. Examining person-centered maternity care in a peri-urban setting in Embakasi, Nairobi, Kenya. PLoS One 2021; 16(10): e0257542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ministry of Health, Federal Democratic Republic of Ethiopia. Health Sector Transformation Plan: 2015/16–2019/20. Federal Ministry of Health Addis Ababa, Ethiopia. https://extranet.who.int/nutrition/gina/sites/default/filesstore/ETH%202016%20Health%20Sector%20Transformation%20Plan.pdf (2015, accessed 5 April 2022) [Google Scholar]
- 32. Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women’s perception of respectful maternity care in public health facilities. BMC Pregnancy Childbirth 2016; 16(1): 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wassihun B, Zeleke S. Compassionate and respectful maternity care during facility based child birth and women’s intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth 2018; 18(1): 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Office DMAH. Debre Markos town administration health office report (accessed 20 April, 2022). [Google Scholar]
- 35. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York, NY: Lawrence Erlbaum Associates, 2017. [Google Scholar]
- 36. Sudhinaraset M, Landrian A, Golub GM, et al. Person-centered maternity care and postnatal health: associations with maternal and newborn health outcomes. AJOG Glob Rep 2021; 1(1): 100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. World Health Organization UNPF and United Nations Children’s Fund (UNICEF). Managing complications in pregnancy and childbirth: a guide for midwives and doctors. 2nd ed. Geneva: World Health Organization, 2017. [Google Scholar]
- 38. Gausia K, Ryder D, Ali M, et al. Obstetric complications and psychological well-being: experiences of Bangladeshi women during pregnancy and childbirth. J Health Popul Nutr 2012; 30(2): 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Barton B, Peat J. Medical statistics: a guide to SPSS, data analysis and critical appraisal. Hoboken, NJ: John Wiley & Sons, 2014. [Google Scholar]
- 40. Pallant J. SPSS survival manual: a step by step guide to data analysis using IBM SPSS. New York, NY: McGraw-Hill Education, 2020. [Google Scholar]
- 41. Kifle D, Azale T, Gelaw YA, et al. Maternal health care service seeking behaviors and associated factors among women in rural Haramaya District, Eastern Ethiopia: a triangulated community-based cross-sectional study. Reprod Health 2017; 14(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. USAID. Focused antenatal care:providing integrated, individualized care during pregnancy.USAID, ACCESS, 2007. [Google Scholar]
- 43. Ochako R, Fotso J-C, Ikamari L, et al. Utilization of maternal health services among young women in Kenya: insights from the Kenya Demographic and Health Survey, 2003. BMC Pregnancy Childbirth 2011; 11(1): 1–9. 10.1186/1471-2393-11-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Afulani PA, Buback L, Essandoh F, et al. Quality of antenatal care and associated factors in a rural county in Kenya: an assessment of service provision and experience dimensions. BMC Health Serv Res 2019; 19(1): 684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Siraj A, Teka W, Hebo H. Prevalence of disrespect and abuse during facility based child birth and associated factors, Jimma University Medical Center, Southwest Ethiopia. BMC Pregnancy Childbirth 2019; 19(1): 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tonei V. Mother’s mental health after childbirth: does the delivery method matter? J Health Econ 2019; 63: 182–196. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121231225352 for Person-centered maternity care during childbirth and associated factors among mothers who gave birth at public health institutions of Debre Markos town, Northwest Ethiopia, 2022: A cross-sectional study by Yaregal Admasu Alelign, Misganaw Fikrie Melesse, Endihnew Beka, Addisu Alehegn Alemu, Neway Ejigu Meskele and Chernet Getnet Asres in SAGE Open Medicine