Abstract
Background:
The US health care system is the second largest contributor of trash. Approximately 20% to 70% of waste is produced by operating rooms, and very few of this waste is recycled. The purpose of this study is to quantify the opened but unused disposable supplies and generate strategies to reduce disposable waste.
Methods:
A single-center prospective study to evaluate the cost of opened but unused single-use operating room supplies was completed by counting the number of wasted disposable products at the end of hand surgery cases. We used χ2 test, t test, Wilcoxon rank-sum test, and simple linear regression to assess the associations between patient and case variables and the total cost of wasted items. Environmentally Extended Input Output Life Cycle Assessment methods were used to convert the dollar spent to kilograms of carbon dioxide equivalent (CO2-e), a measure of greenhouse gas emissions.
Results:
Surgical and dressing items that were disposed of and not used during each case were recorded. We included 85 consecutive cases in the analysis from a single surgeon’s practice. Higher cost from wasted items was associated with shorter operative time (P = .010). On average, 11.5 items were wasted per case (SD: 3.6 items), with a total of 981 items wasted over the 85 cases in the study period. Surgical sponges and blades were 2 of the most unused items. Wasted items amounted to a total of $2193.5 and 441 kg of CO2-e during the study period.
Conclusions:
This study highlights the excessive waste of unused disposable products during hand surgery cases and identifies ways of improvement.
Keywords: surgical waste, carbon footprint, unused surgical supplies, greenhouse gas emissions, hand surgery
Introduction
The US health care system generates 10% of total US greenhouse gas (GHG) emissions, and hospitals are the second largest contributor to landfills and the second largest consumer of energy after the food industry.1,2 Most of this waste is produced by operating rooms (ORs), generating between 20% and 70% of total waste produced in hospitals—approximately 2.8 to 4 billion pounds of waste, mostly due to the lack of recycling owing to the inappropriate disposal of waste as biohazard waste.3-5 In 2009, the World Health Organization emphasized that hospitals have responsibilities in making health care more sustainable.6,7
The waste produced in our ORs and hospitals is one of the reasons for growing health care costs. As of 2016, health care spending was estimated to be $3.35 trillion dollars, that is, per capita spending of $10 345, double that of any other first world country. Waste disposal accounts for 20% of a hospital’s annual environmental budget, and therefore reduction can lead not only to ecologic benefits but also to reduction in health care costs. 8
Operating rooms in the United States produce between 2000 and 7000 tons of waste per day. Approximately 70% to 90% of OR waste is designated as biohazard when disposed, but the Centers for Disease Control and Prevention has reported that only 1% to 2% of this waste needs to be disposed as infectious waste. This is extremely costly for hospitals, who can pay up to 10 times more for biohazard waste disposal. This waste treatment pathway also results in higher environmental emissions due to more treatment steps. 9
Unfortunately, some of the waste generated in ORs are unused disposable supplies. Supplies are brought into ORs based on physician preference cards, which describe all of the supplies, pharmaceuticals, and equipment a particular surgeon needs to perform a surgery. Most hospitals also develop a disposable supply “custom pack” that contains a set of basic single-use supplies needed per surgical procedure. Additional supplies, or “pick items,” are brought into each surgery as needed. Custom packs can lead to unnecessary waste as some items may not be used by certain physicians performing the procedure but must be thrown away due to hospital standards.10,11 Physician preference cards can also lead to unnecessary surgical waste if not properly used and maintained.12-14
Studies have begun to analyze the impact of excessive resource use in ORs. A study of neurosurgery cases found that an average of $968 (17%) of supply spending per case went toward unused and wasted supplies. Unused products quantified were single-use items, and the most common were sponges, gloves, blue towels, and sutures and the most expensive being bone sealant products, drills bits, and screws, among other neurosurgery-specific items. 15 Each one had to be manufactured, packaged, sterilized, and transported to the OR, resulting in unnecessary environmental emissions. Given the heightened concern for health care cost and environmental sustainability, we seek to identify opportunities to reduce waste, improve health care’s impact on the environment, and generate cost savings. Here, we analyze the quantity, cost, and GHG emissions of opened and unused disposable surgical supplies, with the goals of identifying sources of unnecessary waste and increasing value of care by decreasing cost.
Materials and Methods
In this prospective study, we evaluate the cost and GHG emissions from production of opened but unused single-use OR supplies for hand surgery. The study site is a single ambulatory surgical center, affiliated with a large academic practice. Institutional Review Board approval from our institution was obtained, and informed consent was obtained from all individual participants included in the study. Eighty-five consecutive cases from February 2018 to July 2018 were included in the study. Wasted items were defined as opened disposables, with no direct contact with the patient or patient-related fluids. The items were quantified immediately after each case by the surgeon, written down with the patient identifying information, and secured. Costs of each item were obtained from Medline list prices for a standard hand pack provided by Medline’s administration and are not specific to our case study location. Descriptive analysis included the type of surgery, age of the patient, length of surgery, tourniquet time, which items were disposed, patient demographics, comorbidities, and smoking status. Cases were grouped into 4 categories by identification of Current Procedural Terminology codes, and 32 codes were used for analysis: endoscopic carpal tunnel releases (29848), tendon and soft tissue–related procedures (ie, 25118, 26442, 26020,26115, 26210,26480), open fracture fixation and associated procedures (ie, 25607, 25609,25645, 26110), and other procedures including percutaneous fracture fixation (26727) and application of a splint (29125).
Statistics
We summarized categorical variables using proportions and continuous variables using means and standard deviations (SDs) or medians and interquartile ranges (IQRs), as appropriate, according to data distribution. We used χ2 test, t test, Wilcoxon rank-sum test, and simple linear regression to assess the associations between patient and case variables and the total cost of wasted items. We defined P < .05 as statistically significant.
Carbon Footprinting
The GHG emissions or a “carbon footprint” of the supply item’s production and delivery was estimated using the hospital’s purchasing data and an environmentally extended input output (EEIO) life cycle assessment (LCA) model. The EEIO-LCAs have been used to estimate the environmental footprint of other medical services, including hysterectomy16,17 cataract surgery,18-20 and national health care emissions.4,21 This study uses the US EEIO model, maintained by the US Environmental Protection Agency, which combines the economic transactions between 389 industrial sectors (2008 data) with environmental data for these sectors (2013 data). 22 Of the economic sectors available in the model, we use the sector “Surgical and medical instruments; at manufacturer” (North American Industry Classification System code 339112) to estimate GHG emissions from production of our unused hand surgery supplies. Financial data of our study were deflated from the year of the supply purchase (2018) to the year of the EEIO-LCA model (2013) using Producer Price Index Tables for this sector maintained by the US Bureau of Economic Analysis. The US EEIO model was analyzed using “OpenLCA” software 23 with the Centre for Environmental Studies (CML) 2001 Base Life Cycle Impact Assessment method, a global impact assessment method developed by the Center of Environmental Science of Leiden University. 24 Here, GHG emissions are reported in kilograms of carbon dioxide equivalents (kg CO2-e).
Results
Of the 85 cases studied, 64.7% (55) of patients were women, and the mean age was 56.4 years (SD: 16 years). Thirty-four patients had hypertension (40%), 30 had hyperlipidemia (35%), 21 were smokers (24%), and 13 had diabetes (15%). Procedures consisted of 45 endoscopic carpal tunnel releases (53%), 30 tendon transfers, tenolysis, and tendon sheath incisions (35%), and 7 open reductions of distal radius and internal fixations, and carpal bone and phalangeal fractures (7%). The median operative time was 22 minutes (IQR: 14-44 minutes). The median tourniquet time (which was only applicable to 73 cases) was 10 minutes (IQR: 6-20 minutes).
The mean number of unused and wasted surgical items was 11.5 items per case (SD: 3.6 items, out of 51 items per custom pack) or a total of 981 items over the 85 cases included in the study. Most of the unused, wasted items came from the custom pack, with an average of 22.6% of items in the pack wasted during the study period. The hand custom pack is opened in all hand cases regardless of whether the approach is open or endoscopic. The surgical item in the custom pack that was wasted most often was surgical sponges (RayTec Johnson and Johnson, New Brunswick, New Jersey) with an average of 3.3 sponges wasted per case and a total of 280 wasted sponges. Of the 85 cases in our study period, only 18 cases (21%) had no wasted sponges. Similarly, surgical blades from the custom pack were wasted 198 times (2.3 per case) and had only 10 cases (12%) with no wasted blades. Stockinettes from the custom pack were wasted 62 times (0.73 per case), and only 28% of cases had no wasted stockinettes. Drapes, clings, and gowns were also often wasted; listed in Table 1 are wasted surgical items and the percentage of cases with no waste for that item in the study period.
Table 1.
Surgical Items Wasted Over 85 Consecutive Cases.
| Item | No. of items unused and wasted | Cases with no unused waste (%, n = 85) | Total cost ($) |
|---|---|---|---|
| Plaster | 0 | 100 | 0.0 |
| Spec. cups | 2 | 99 | 1.8 |
| Matisol adhesive | 1 | 99 | 1.7 |
| 4 × 4 gauze | 5 | 99 | 1.3 |
| Soft roll | 2 | 98 | 32.7 |
| Coban bandage | 2 | 98 | 4.4 |
| Steri-strips | 2 | 98 | 1.6 |
| Needles | 3 | 98 | 0.5 |
| Bins | 5 | 98 | - |
| Webril | 3 | 96 | 2.9 |
| Irrigation bulbs | 3 | 96 | 1.5 |
| Esmarch | 4 | 95 | 13.8 |
| Sutures | 7 | 94 | 49.0 |
| Marker | 5 | 94 | 2.8 |
| Bucket | 5 | 94 | - |
| Syringes | 9 | 92 | 2.8 |
| Gloves | 14 | 91 | 15.5 |
| Ace bandage | 8 | 91 | 7.4 |
| Bipolar forceps | 16 | 82 | 586.6 |
| Table cover | 29 | 79 | 53.1 |
| Xeroform | 19 | 79 | 9.9 |
| Basins | 50 | 64 | 330.5 |
| Blue towels | 64 | 64 | 43.5 |
| Drape | 69 | 47 | 329.8 |
| Cling | 55 | 36 | 30.8 |
| Gown | 57 | 34 | 215.5 |
| Stockinette | 62 | 28 | 300.1 |
| Surgical sponges (Raytecs) | 280 | 21 | 154.0 |
| Surgical blades | 198 | 12 | 99 |
The item that accounted for most of the wasted cost and carbon footprint was bipolar forceps ($586.6 and 118 kg CO2-e), followed by basins ($330.5, 67 kg CO2-e), drapes ($329.8, 66 kg CO2-e), and stockinettes ($300.1 60 kg CO2-e). Wasted items amounted to a total of $2,193.5 and 441 kg of CO2-e during the study period. These GHG emissions are equivalent to the emissions from a standard US passenger vehicle driving 1080 miles (1818 km) or to the GHG emissions from charging 56 360 smart phones. 25 This wasted additional cost was distributed unevenly across cases, wherein the top 18 cases (18%) with most waste accounted for 44% of the cost and emissions ($970 and 195 kg CO2-e).
When analyzing procedure factors with cost, we found that higher costs from unused, wasted items were associated with shorter operative time (P = .010), suggesting that cases that are expected to be shorter might benefit from a more consolidated custom pack. Figure 1 shows a scatter plot between operative time and unused, wasted cost. Likely related to this previous finding, shorter tourniquet time was also associated with higher costs from unused, wasted items (P = .011). There was suggestive evidence for an association between higher cost from unused, wasted items and a history of hypertension (P = .058) or diabetes (P = .083). Table 2 shows results from univariate analysis comparing case and patient variables with total unused, wasted cost.
Figure 1.
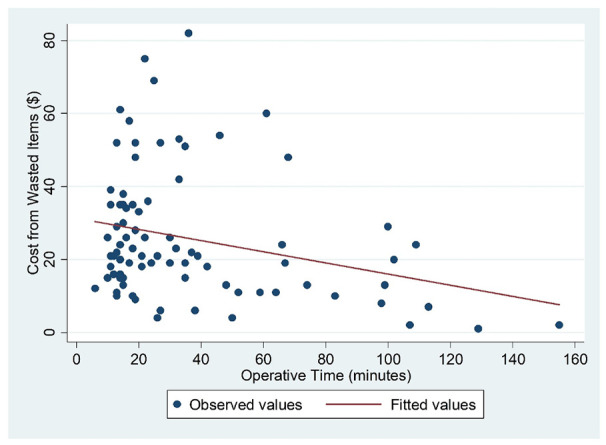
Scatter plot demonstrating an association between operative time and cost of wasted items.
Table 2.
Univariate Associations Between Case and Patient Characteristics With Cost of Wasted Items.
| Variable | Categories | Cost of unused, wasted items | P value |
|---|---|---|---|
| Sex, median (IQR) | Men | 25 (12-44) | .410 |
| Women | 21 (13-29) | ||
| Age, cost per additional year (95% CI) | 0.05 (–0.19 to 0.29) | .669 | |
| Procedure | Carpal tunnel release | 22 (16-30) | .901 |
| Tendon transfer, tenolysis, tendon sheath incision | 21 (11-49) | ||
| Open reduction of fractures | 16 (2-31) | ||
| Other | 26 (8-62) | ||
| Operative time, cost per additional min (95% CI) | –0.15 (−0.27 to −0.04) | .010 | |
| Tourniquet time, cost per additional min (95% CI) | –0.21 (−0.37 to −0.05) | .011 | |
| Hypertension, median (IQR) | No | 20 (11-30) | .058 |
| Yes | 26 (16-35) | ||
| Hyperlipidemia, median (IQR) | No | 21 (13-35) | .511 |
| Yes | 24 (15-35) | ||
| Diabetes, median (IQR) | No | 21 (13-29) | .084 |
| Yes | 35 (17-39) | ||
| Previous surgeries, median (IQR) | No | 21 (14-36) | .353 |
| Yes | 20 (13-28) | ||
| Smoking, median (IQR) | No | 21 (13-32) | .160 |
| Yes | 22 (12-36) | ||
Note. IQR = interquartile range; CI = confidence interval.
Discussion
There is an obvious environmental and cost savings benefit to waste reduction in the OR. We have currently outlined several methods previously published and will highlight a few here. 26 In their article on decreasing waste in health care, Kagoma et al lay out 5 basic principles (the 5 Rs): (1) Reducing waste; (2) Reusing materials; (3) Recycling; (4) Rethinking the way of disposing of waste; and (5) Research. Our article uses research to help identify strategies to reduce unused supply wastage. Table 1 highlights several commonly wasted items in the OR; identifying these products is the first step in waste reduction (Table 1). Here, we discuss implementing basic principles of Kagoma et al 6 to increase the value of surgical care.
Reduce
This study demonstrates that shorter cases, specifically carpal tunnel releases and soft tissue procedures, or those approximately less than 20 minutes in length had the most unused, wasted items and would benefit from a custom consolidated hand pack (Figure 1). This hand pack could be modeled after the “lean and green initiative” with “green packs” discussed by Van Demark et al and Thiel et al.8,27,28 Both have demonstrated that with limited field sterility and a consolidated or “green pack,” waste can be reduced significantly without compromising patient safety.
Robert Van Demark et al implemented the use of “green packs” for their Wide-Awake Local Anesthesia No Tourniquet (WALANT) cases and estimated savings of $10.64 and 2.3 kg per case solely by using the suggested consolidated “green packs.” After 1099 hand cases, the institution saved $13 250.42, and waste was decreased by 2.8 tons. The author estimates that if approximately 2000 hand surgeons in the country were to do 100 “green” cases a year, there would be a nationwide savings of $2.13 million and a decrease of 506 tons of waste.
In addition to refining the custom packs, physicians should regularly update their preference cards to remove (or shift to “as needed”) supplies that are not routinely used during surgery. 28 Establishing good communication with surgical teams about necessary supplies and location of potential pick items can also help reduce erroneously opened supplies and reduce opening standardized surgical packs. In one study of laparoscopic hysterectomy’s carbon footprint, Thiel et al 17 determined that reducing supplies brought in to the OR could reduce the carbon footprint over 45%.
Reuse
Where possible, surgical teams should strive to use reusable instruments, as this is generally shown to reduce emissions and waste generation. If reusable instruments are not an option, surgical teams should explore opportunities for single-use device (SUD) reprocessing. Single-use device reprocessing is currently carried out by a third-party vendor through a Food and Drug Administration–approved process. Hospitals send used SUDs to the third-party reprocessor who safely dismantles, cleans, reassembles, sterilizes, and resells the reprocessed SUDs, often at a lower cost than original manufacturing.29-31 Although few studies show the carbon footprint of SUD reprocessing, it is shown to reduce waste generation.
Rethink
Rethinking the surgical process is one of the most important steps. Rethinking can be done at a local level, by individual surgeons or surgical teams. Surgeons or teams should identify what is needed in each case, communicate this in effective preoperative briefings, reduce handoffs to consistently work with the same surgical team, and store supplies in appropriate and strategic places.
Rethinking at the specialty level can also reduce waste and costs. Adopting WALANT protocols in hand surgery cuts not only on labor costs of the anesthesiologists and recovery room staff, but preoperative testing is no longer required, thus reducing patient travel and waste from testing itself. 15 Lalonde and Martin published a study analyzing the cost benefit of completing WALANT surgeries in the OR versus in the office or clinic with limited field sterility. 32 The authors demonstrated that OR procedures were more costly given the amount of materials used for full sterility in the OR versus field sterility in the clinic or ambulatory setting. LeBlanc et al 33 demonstrated that limited field sterility for carpal tunnel releases was safe, determined by the low risk of superficial infection in their study (0.4%) and deep infection (0%), and was cost-effective. Another study combined WALANT surgeries with a minimal custom pack, reducing waste generation in hand surgeries by 13% and saving $125 (or 55%) on surgical supply items. 27
Waste reduction is imperative in all processes. While contemplating how to decrease OR waste, we must consider all visits, procedures, labs, and studies the patient must complete to obtain medical clearance. Beyond WALANT, other techniques to reduce the need for in-person preoperative and postoperative visits, such as telemedicine, should also be considered. 28
Recycle
Albert et al conducted a similar study identifying commonly wasted items in hand surgery, and by reducing waste and recycling they estimated a total cost savings of $41 844 per year. They also identified that the blue wrap used for tray sterility accounted for 19% of OR waste and 5% of all hospital waste. 34 This blue wrap is made of #5 plastic and is not biodegradable, but there is a resale market for the material to other companies who can repurpose the #5 plastic. After instituting a blue wrap recycling vendor, 1.2 tons of waste was diverted at this site over the course of 10 months.
Study Limitations
There are several limitations to this study. First, the results are limited to a single surgeon’s practice, in an ambulatory setting, mainly doing short hand cases, limiting generalizability. Second, as the project continued, staff awareness to disposable waste grew, and this may have influenced individual behavior. Third, EEIO-LCA modeling has some inherent limitations. The EEIO-LCA modeling is built around costs of supplies, which can be notoriously difficult to quantify for US medical facilities. As such, this study uses catalog prices which may or may not reflect actual spending on supplies at this particular location. The carbon footprint of individual items in this study all fall within the same economic sector (surgical and medical instruments) and therefore cannot be compared with each other, limiting the accuracy of the EEIO-LCA model. In other words, even if a syringe is manufactured in exactly the same way, if one costs more than the other, it would appear to have greater carbon emissions. The EEIO-LCA modeling is intended to give a rough estimate of carbon emissions, but it typically represents order-of-magnitude accuracy.
Finally, because of our focus solely on unused items, it is likely that we underestimated the true effect a lean and green approach could have in our department. For example, partially used pharmaceuticals were found to be a large source of unnecessary waste in cataract surgeries, but we did not assess supply items that had come into contact with the patient or patient fluids. 19 As we continue to gather data in the hand surgery and orthopedic surgery departments, more specific insight on the impact of potential implementation of lean and green initiatives at our institution will be revealed.
Conclusion
All items brought into the OR must be carefully considered, as unnecessary materials reduce the value of medical care by needlessly increasing costs and impacts on the environment and public health. The first step toward reducing unnecessary waste in surgery can be achieved by first creating awareness. Once staff are aware of and interested in this issue, problems such as excess materials during short procedures can be identified, and potential solutions can be proposed and tested. Several methods of reducing unnecessary waste in hand surgery include reducing the supplies we bring into the OR from the onset, properly sorting all items for disposal, choosing the correct setting for our cases, recycling eligible items, and continued research on supply optimization and green initiatives in the OR.
Acknowledgments
The authors acknowledge Kimberly Orozco, BS, for her contributions to this article.
Footnotes
Ethical Approval: IRB approval from our institution was obtained.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of informed Consent: Informed consent was obtained from all individual participants included in the study
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: N.P. and C.T. are paid consultants for Stryker corporation, E.M. is a paid consultant for NewClip and Axogen. D.B., R.B., and A.M. have no conflict of interests.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dalibel Bravo  https://orcid.org/0000-0002-6350-7787
https://orcid.org/0000-0002-6350-7787
References
- 1. Wormer B, Augenstein VA, Carpenter CL, et al. The green operating room: simple changes to reduce cost and our carbon footprint. Am Surg. 2013;79(7):666-671. [PubMed] [Google Scholar]
- 2. Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PLoS One. 2016;11(6)e:0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cotton R, Cohen AP. Eco-conservation and healthcare ethics: a call to action. Laryngoscope. 2010;120:4-8. [DOI] [PubMed] [Google Scholar]
- 4. Lee R, Mears SC. Greening of orthopedic surgery. Orthopedics. 2012;35:e940-944. [DOI] [PubMed] [Google Scholar]
- 5. Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131-136. [DOI] [PubMed] [Google Scholar]
- 6. Kagoma Y, Stall N, Rubinstein E, et al. People, planet and profits: the case for greening operating rooms. CMAJ. 2012;184:1905-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sherman JD, MacNeill A, Thiel C. Reducing pollution from the health care industry. JAMA. 2019;322(11):1043-1044. [DOI] [PubMed] [Google Scholar]
- 8. Van Demark RE, Jr, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg Am. 2018;43(2):179-181. [DOI] [PubMed] [Google Scholar]
- 9. H2E: Regulated medical waste reduction. Ten steps to implementing a regulated medical waste reduction plan. Hosp a Healthy Environment. http://hospital2020.org/documents/h2e10steprmw20103.pdf (accessed 3 November 2022).
- 10. Campion N, Thiel CL, DeBlois J, et al. Life cycle assessment perspectives on delivering an infant in the US. Sci Total Environ. 2012;425:191-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Campion NTC, Woods NC, Swanzy L, et al. Sustainable healthcare and environmental life-cycle impacts of disposable supplies: a focus on disposable custom packs. J Cleaner Prod. 2015;94:46-55. [Google Scholar]
- 12. Guzman MJ, Gitelis ME, Linn JG, et al. A Model of cost reduction and standardization: improved cost savings while maintaining the quality of care. Dis Colon Rectum. 2015;58(11):1104-1107. [DOI] [PubMed] [Google Scholar]
- 13. Skarda DE, Rollins M, Andrews S, et al. One hospital, one appendectomy: the cost effectiveness of a standardized doctor’s preference card. J Pediatr Surg. 2015;50(6):919-922. [DOI] [PubMed] [Google Scholar]
- 14. Urbach DR, Baxter NN. Reducing variation in surgical care. BMJ (International Edition). 2005;330(7505):1401-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zygourakis C, Yoon S, Valencia V, et al. Operating room waste: disposable supply utilization in neurosurgical procedures. J Neurosurg. 2016;6:1-6. [DOI] [PubMed] [Google Scholar]
- 16. Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Tech. 2014;49(3):1779-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thiel CL, Woods NC, Bilec MM. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am J Public Health. 2018;108(S2):S158-S164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thiel CL, Schehlein E, Ravilla T, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43(11):1391-1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tauber J, Chinwuba I, Kleyn D, et al. Quantification of the cost and potential environmental effects of unused pharmaceutical products in cataract surgery. JAMA Ophthalmol. 2019;137:1156-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Venkatesh R, van Landingham SW, Khodifad AM, et al. Carbon footprint and cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2016;27(1):82-88. [DOI] [PubMed] [Google Scholar]
- 21. Eckelman MJ, Sherman JD. Estimated global disease burden from US health care sector greenhouse gas emissions. Am J Public Health. 2018(suppl):S120-S122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang Y, Ingwersen WW, Hawkins TR, et al. USEEIO: a new and transparent United States environmentally-extended input-output model. J Clean Prod. 2017;158:308-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ciroth A. ICT for environment in life cycle applications openLCA—A new open source software for life cycle assessment. Int J Life Cycle Ass. 2007;12(4):209. [Google Scholar]
- 24. Guinée JB. Handbook on life cycle assessment operational guide to the ISO standards. The Int J Life Cycle Ass. 2002;7(5):311. [Google Scholar]
- 25. US EPA. Greenhouse Gas Equivalencies Calculator. United States Environmental Protection Agency. Updated May 2016. https://www.epa.gov/energy/greenhouse-gas-equivalencies-calculator (accessed 2 January 2017).
- 26. Dalibel B, Glenn GR, Eitan M. Environmentally responsible hand surgery: past, present, and future. J Hand Surg. 2020;45(5). doi: 10.1016/j.jhsa.2019.10.031. [DOI] [PubMed] [Google Scholar]
- 27. Thiel CLCR, Fiorin Carvalho R, Hess L, et al. Minimal custom pack design and wide-awake hand surgery: reducing waste and spending in the orthopedic operating room. Hand (N Y). 2019;14(2):271-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Van Demark RE, Jr, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg. 2018;43(2):179-181. [DOI] [PubMed] [Google Scholar]
- 29. (FDA) UFaDA. Reprocessing and Reuse of Single-Use Devices. Guidance for Industry and FDA Reviewers. Updated 2003. https://www.fda.gov/media/71124/download (accessed 3 November 2022). [Google Scholar]
- 30. Unger S, Landis A. Assessing the environmental, human health, and economic impacts of reprocessed medical devices in a phoenix hospital’s supply chain. J Cleaner Prod. 2016;112(3):1995-2003. [Google Scholar]
- 31. Potera C. Strategies for greener hospital operating rooms. Environ Health Perspect. 2012;120(8):a306-a307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: improved results, cost effectiveness, and wide- awake patient satisfaction. Arch Plast Surg. 2014;41(4):312-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. LeBlanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? a multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y). 2011;6(1):60-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Albert M, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg (Oakv). 2015;23(4):235-238. [DOI] [PMC free article] [PubMed] [Google Scholar]


