Abstract
Background:
Community participation has become a key outcome measure for people with disabilities. This has resulted in a shift in researchers focus from the individual to the environment. However, research has focused primarily on participation barriers in the community with limited research examining the role of the home environment. For people with mobility disabilities the home environment is the starting place for community participation and research is needed to understand the relationship between the home and participation outcomes.
Objective:
This study explores the effects of a consumer-driven home modification intervention on community participation for people with mobility disabilities.
Methods:
We conducted a randomized control trial (from June 2017–April 2019) of the effects of a consumer-directed home modification intervention on community participation. The intervention, the Home Usability Program, was implemented with consumers at two different Centers for Independent Living (N = 195) and included a self-assessment of their home environment and implementation of a home usability change.
Results:
The Home Usability program positively affected the community participation of people with mobility disabilities. Overall, intervention participants reported a 39.5% (p < .05) increase in social and recreational activities immediately following the intervention relative to the control group after controlling for health status and month when outcome data were collected. Six months after the intervention, this effect returned to baseline.
Conclusions:
Community-based, consumer-driven home modification programs show promise for improving community participation outcomes among people with disabilities, however, more research is needed to understand why results did not persist.
Keywords: Community participation, Mobility disability, Home usability, Home modification, Community based research
Background
Approximately 20.5 million adults in the United States report living with a mobility-related disability.1 However, many Americans with mobility disabilities remain isolated or dependent in their communities due to a lack of affordable and accessible housing.2,3 A report from the U.S. Department of Housing and Urban Development (HUD) Office of Policy Development and Research suggests 89.2% of people with mobility disabilities live in inaccessible housing.4 More specifically, over 50% of households with a person who has a mobility disabilities and who use wheeled mobility equipment live in homes with steps at their front entrance,5 directly impacting their ability to access their neighborhoods and communities. Living in unsuitable and inaccessible housing conditions creates a variety of adverse outcomes, including increased risk for fall-related injuries,6 activities of daily living (ADL) limitations,7 and institutionalization.8,9
The social model of disability recognizes that a person’s disability may be influenced by the supports, or lack thereof, afforded by their environment.10 For example, although a person with a mobility disability may not be able to bathe independently using a standard bathtub, they may be able to independently bathe by implementing an environmental change like a walk-in shower, bath bench, grab bars, and hand-held shower head. By modifying and tailoring the home environment to a person’s disability, these modifications contribute to maximizing the health and independence of people with disabilities. Stark et al.11 conducted a systematic review of the effects of home modification interventions on the participation of community-dwelling adults with health conditions and reported that home modifications have the potential to reduce fall risk, improve functional performance, and reduce demands on caregivers.
Although these health related outcomes are important, community participation has emerged as a new standard in outcome measurement for rehabilitation research.12 More recently, it has been used as a key success indicator to evaluate home- and community-based services and supports for people with disabilities.13 The emphasis on community participation as a desired outcome was largely driven by the World Health Organization (WHO). The WHO previously used “absence of disability” as a desired outcome, placing outcome measurement solely on individual f actors with limited emphasis on the role of the environment. However, in 2001 the WHO released the International Classification of Functioning, Disability and Health (ICF). The ICF provides a framework for understanding the social model of disability, unpacking the contextual relationship between disability, health and the environment.14 With the release of the ICF and the shift to participation as an outcome, researchers turned their focus to the environment. While most studies observing people with disabilities’ community participation are non-experimental, previous research has examined the effects of physical activity,15,16 transportation vouchers,17 entrance ramps,2 and personal assistance services (PAS) training18 on community participation.
Despite this shift, little research examines the effects of an environmental interventions within the home on community participation for people with disabilities. For example, a systematic review conducted by Stark et al.11 found no articles identified home modification intervention studies that included community participation as an outcome measure. Additionally, a scoping review of home modification interventions by Carnemolla and Bridge19 identified social participation as an emerging outcome of interest in home modification research, although no studies examined intervention effects on community participation.
Emerging research shows that people with unusable homes may exert additional energy completing activities of daily living, which may influence a person’s decision to participate in their community. For example, Greiman et al. (2018) show that people with mobility disabilities are more likely to report feeling more exerted than people without disabilities when cleaning, bathing, organizing, entering and exiting the home, preparing food, toileting, and using the bedroom. Additionally, results show that people with mobility disabilities who do not have grab bars but need grab bars report feeling more exerted while bathing than who have grab bars.20 If people with mobility disabilities have a limited amount of energy to expend throughout the day due to increased levels of pain and fatigue, these data suggest that completing certain activities, such as bathing, may have a “high cost” of energy expenditure, especially if a person’s home is not useable. These findings are supported by other research findings showing that people with mobility disabilities are more likely to engage in social activities if their home entrances 25 and bathrooms 26 are accessible.
The complexity and variation of individual home environments, physical abilities, assistive technology, personal assistance supports, and community-based service provision challenge conventional approaches to evaluation.21 Although researchers typically emphasize the importance of intervention standardization, it may not be possible to assume a prescriptive approach to home modification interventions given both ethical considerations and threats to external validity. Previous research has identified maintaining intervention standardization and implementation fidelity to be a challenge in community-based research.22 This can be particularly true when working in service settings and engaging services providers as researchers. Service providers may struggle to navigate the often blurred lines between service provision and research and evaluation,23 which can be additionally complicated by variation in practices and procedures from one organization to another. Maintaining strict intervention fidelity across multiple complex systems quickly becomes a fool’s errand. In fact, Hawe et al.24 argue for embracing this complexity in community-based interventions and shifting focus from form (i.e., following intervention steps precisely) to process (i.e., encouraging participant choice and control).
Engaging stakeholders in community-based rehabilitation research is recognized as a valuable strategy for informing rehabilitation practice.25 Additionally, Trickett et al.26 identified the importance of a shared cultural understanding when conducting research and implementing interventions in the communities. Ensuring that the research is “culturally situated”26 is particularly relevant when working with disability service and advocacy organizations like Centers for Independent Living (CILs). Centers for Independent Living are non-residential non-profit organizations that provide services and support to people with disabilities in the community through information and referral, advocacy, and training. CILs operate under a cultural mantra of “nothing about us without us,” recognizing that people with disabilities are the best experts in their own needs and necessitate choice and control over their lives. A shared cultural understanding is critical for engaging in community-based research with Centers for Independent Living.
The Home Usability Program (HUP) was developed with a team of five CIL staff (comprised of individuals both with and without disabilities) as an intervention aimed at empowering people with disabilities to identify their own home usability concerns and goals. During the development process the intervention’s core concept of home usability emerged as an alternative to home accessibility. Home usability represents a more holistic approach to addressing housing needs for people with disabilities, recognizing that the needs individuals have within their homes are personal and specific. The term accessibility evokes codes and requirements, and while accessibility standards are critical for promoting inclusion in public, people’s needs in their private home environments may be different (for example, an ADA accessible toilet may not be appropriate for someone of short stature). The home usability program stands in contrast to other home modification and repair programs as it is not prescriptive in the types of fundable home changes (i.e. ramps, grab bars or other pre-selected items). Rather, home usability asks the consumer what works for you, what are your needs, and what do you want, understanding that needs in the home vary from individual to individual and may not be an item or modification traditionally associated with accessibility (e.g., ramps, grab bars or widened doorways).
The goal of this study was to test the efficacy of the Home Usability Program by investigating the impacts of a consumer-directed home usability intervention on community participation among people with mobility disabilities. Our primary hypothesis is that a consumer-directed usability intervention will positively impact community participation.
Method
Participants
Participants (n = 232) for this project were people with mobility disabilities who were living in the community, over 18 years old, and consumers of services at Centers for Independent Living (CIL). Participants were recruited from two CILs across the United States, one in a small city in the Rocky Mountain West and the other in a large Midwestern metropolitan area. Study participants were recruited from June 2017 through April 2019 through the CILs via existing consumer mailing list serves, advertisements in organizational newsletters, and conversations with other CIL staff. Additionally, participants were recruited from partner organizations (e.g., home health care providers, disability-specific organizations and associations, and durable medical equipment providers). Participants recruited from outside organizations were registered as consumers with the CIL prior to engaging in the project. Participant demographics can be found in Table 1.
Table 1.
Participant demographic and housing characteristics.
| Demographic Characteristics | n = 195 | % |
|---|---|---|
| Sex | ||
| Female | 122 | 62.6% |
| Race and Ethnicity | ||
| American Indian/Alaskan Native | 15 | 7.7% |
| Asian | 1 | 0.5% |
| Black/African American | 33 | 16.9% |
| Native Hawaiian/Pacific Islander | 0 | 0.0% |
| White | 149 | 76.4% |
| Other | 6 | 3.1% |
| Hispanic/Latino | 6 | 3.1% |
| Disability | ||
| Hearing | 20 | 10.4% |
| Vision | 27 | 13.9% |
| Cognitive | 83 | 43.2% |
| Mobility | 162 | 85.3% |
| Self care | 92 | 48.2% |
| Independent Living | 107 | 56.6% |
| Highest educational level | ||
| Less than high school | 21 | 10.8% |
| High school graduate | 49 | 25.3% |
| Some college or technical training | 49 | 25.3% |
| Associate or technical degree | 23 | 11.9% |
| Bachelor’s degree | 32 | 16.5% |
| Master’s degree or higher | 20 | 10.3% |
| Household income | ||
| $10,000 or less | 79 | 41.8% |
| $10,001 to $20,000 | 50 | 26.5% |
| $20,001 to $30,000 | 15 | 7.9% |
| $30,001 to $40,000 | 15 | 7.9% |
| $40,001 to $50,000 | 11 | 5.8% |
| $50,001+ | 19 | 10.1% |
| Employment Status | ||
| Full time | 11 | 5.7% |
| Part time | 28 | 14.4% |
| Not employed | 155 | 79.9% |
Note: Average age for this sample was 53.9 (18–94).
We randomly assigned participants to either the intervention (HUP) or control condition. Participants in the intervention group completed the Home Usability Program and those in the control group received CIL services as usual. We randomly assigned 102 participants into the intervention and 88 into the control condition. Ultimately, 21 participants declined to participate in the intervention and were treated as controls, 37 withdrew from the study, and 5 participants died. See consort flow diagram for details about randomization and participation, Fig. 1.
Fig. 1.
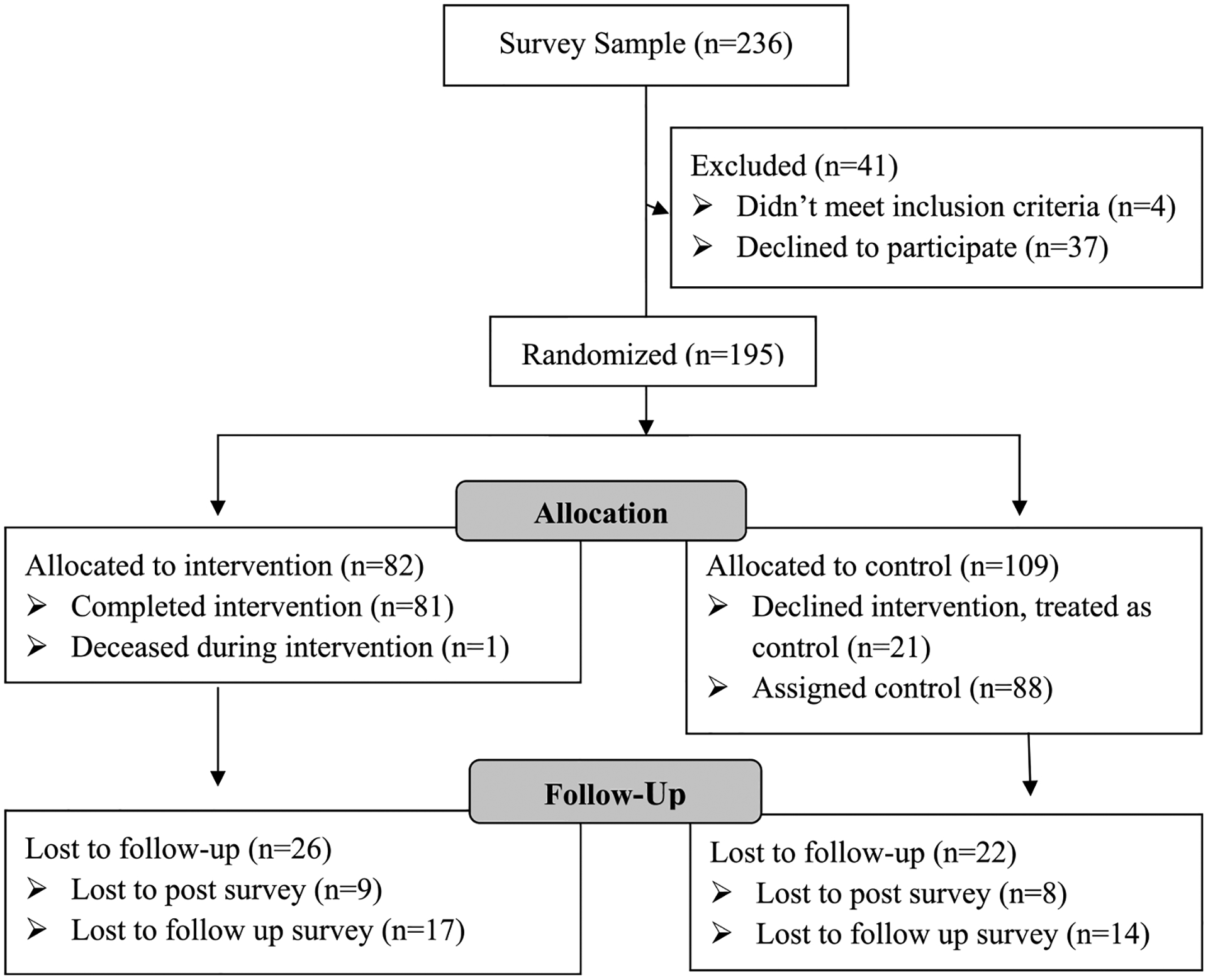
Consort flow diagram.
Intervention implementation
Participants assigned to the Home Usability Program (HUP) intervention worked with a CIL staff person to assess potential problems in the home and identify and implement solutions. The Home Usability Program was developed with a team of five CIL service providers who developed and vetted the intervention content and materials. While this intervention was relatively simple, its novel in that it was developed with a team of stakeholders and has very broad eligibility criteria and very few limitations on allowable home modifications. For example, many existing home modification programs place limitations on the types of modifications allowed or have strict income/tenure eligibility criteria. The intent of this research was to understand that when people are allowed to think more holistically about the usability of their home, does this have an impact on community participation.
The intervention content was available online via a website (www.useablehome.com) or through a printed manual depending on consumer preference. Participants started the program by meeting with CIL staff to discuss the usability of their home and taking a short “home satisfaction quiz” to identify possible problem areas. Participants engaged in a self-assessment of identified rooms (e.g., kitchen, bathroom, bedroom) using the American Association of Retired Persons (AARP) HomeFit Guide,27 which was oftentimes completed with the CIL staff during a scheduled in-person home visit. Next, the information on potential home usability problems was recorded and needs were prioritized. Once the home usability problem was identified, participants worked with the CIL staff person to identify personal and community resources to address the home usability concern, including consultation related to purchasing an item, installing equipment, or hiring a contractor for various types of home modifications (e.g., install grab bars). The intervention concluded when the participant indicated satisfaction with the home modification. Participants had access to $350 in grant funds to help supplement any costs of home modifications or purchases associated with their home usability goal. The cost of home usability projects identified varied by participant, and not all participates utilized the full $350 available. Costs ranged from $50 for items (e.g., bath chairs and shelving) to the full $350 (e.g., grab bar or ramp installation).
Procedures
Measures were collected using the “Home and Community Survey” that was administered prior to randomization. We collected post-test measures immediately after the consumer completed the intervention (or at 3 months for the control group) and 6 months post intervention. Participants randomized into the intervention were consented separately to participate in the home usability project. Those who declined to participate in the HUP were treated as controls. The intervention was considered complete when the consumer completed their home usability goal and the CIL reported this information to research staff. Participants had the option to complete the survey using paper and pencil forms, online (via Qualtrics survey software), over the phone, or in-person with the CIL staff. All study procedures were approved by the Institutional Review boards at both the [locations masked for blinded review]. All participating CIL staff were approved as research team members by their respective IRBs. Surveys took approximately 45 min to complete, and participants received either $10 or $25 as an incentive for completing each survey (i.e., we increased incentives to improve enrollment, participants in the latter half of the study received more per survey). After completing the pre-survey, participants were randomly assigned to the intervention or control groups.
Measures
In addition to basic demographics, we collected information about the housing characteristics of participants, such as the type of structure (e.g., single family home, apartment) ownership status (i.e., renter or homeowner), age of the home, and length of residence. Participant housing characteristics can be found in Table 2. The primary outcome of interest for this study was community participation. To measure community participation, we used the Brief Community Engagement Questionnaire,28 which asks about frequency of “trips” and “social and recreational activities” in the community. Respondents used a 7-point scale (from 1 to 7 or more) to indicate the number of times they physically visited a place (i.e., took a trip) or engaged in a social or recreational activity. This measure is based on a seven day recall (“thinking about the past seven days”) which does not delineate between weekdays and weekends. Trips are defined as activities such as going out to places in the community (i.e., the grocery stores, doctor’s offices, pharmacies and restaurants) to run errands, attend appointments and engage in other more obligatory activities. Social and recreational activities are more discretionary activities such as socializing with friends, visiting a park or recreation area, going to the movies, or attending community events.
Table 2.
Participant housing characteristics.
| Housing Characteristics | N = 195 | % |
|---|---|---|
| Housing status | ||
| Own | 51 | 26.6% |
| Rent | 129 | 67.2% |
| Other | 12 | 6.3% |
| Building type | ||
| Single family home/house | 81 | 42.2% |
| Town home, condominium, triplex | 18 | 9.4% |
| Apartment building with 4 or more units | 79 | 41.2% |
| Other (e.g. manufactured home) | 14 | 7.3% |
| Housing tenure duration | ||
| Less than 6 months | 18 | 9.3% |
| 6 months to 1 year | 17 | 8.8% |
| 1–5 years | 75 | 38.9% |
| More than 5 years | 83 | 43.0% |
| Building age | ||
| 1930 or earlier | 16 | 8.4% |
| 1931–1950 | 11 | 5.8% |
| 1951–1970 | 25 | 13.1% |
| 1971–1990 | 48 | 25.1% |
| 1991–2017 | 56 | 29.3% |
| Don’t know | 35 | 18.3% |
Note: Average household size for this sample was 1.79 (range 1–6).
A critical component of the intervention was consumer choice and control over the home usability problems and solutions identified. This resulted in a wide range of home usability intervention projects. In order to understand the effects of different types of home usability projects on participation, we collapsed and classified home usability projects by function (i.e., related to activities like bathing, grooming, cooking, and cleaning). Table 3 includes descriptive information about the projects implemented and the resulting classification.
Table 3.
Home usability program classifications.
| Classification | Examples | N = 81 | % |
|---|---|---|---|
| Bathing and grooming | Grab bars, shower chairs, non-slip mats | 21 | 25.9% |
| Cleaning | Robot vacuums, long handled dusters, storage | 15 | 18.5% |
| Mobility | Mobility devices such as walkers and canes | 15 | 18.5% |
| General safety | Fire extinguishers, medical alert device | 13 | 16.0% |
| Entrancing | Hand railings, video doorbells, threshold ramps | 10 | 12.3% |
| Cooking | Adaptive cooking equipment | 6 | 7.4% |
| Sleeping | New mattress | 5 | 6.2% |
| Moved | Moved to a more accessible space | 3 | 3.7% |
| Dressing | Assistive equipment | 3 | 3.7% |
| Furniture | Couch, desk | 2 | 2.5% |
| Assistive equipment | Reacher tool | 2 | 2.5% |
Research design and analytic method
Survey responses were entered into Excel, checked for accuracy, and imported into STATA 16.1 for analyses. We used linear regression analysis with a log link and Poisson distribution due to the inherent skew of participation data where many respondents simply do not participate in some activities. We compared within person change in outcome scores of participants in the treatment group to within person change among participants in the control group. This analysis assumes that change in the control group represents the change that would have been observed in the treatment group had they not participated in the intervention. More specifically, we regressed outcome variables on a treatment indicator, a post-test indicator, and the interaction of these two indicators. Our primary coefficient of interest is this interaction term. We included control variables for self-reported health status of the individuals and survey month, a proxy for the season when outcome variables were collected. This was important to account for the effects of winter and summer on participation.
Results
Overall, results support our primary hypothesis that consumer-directed home usability interventions in the home environment positively affect participation. Regarding the type of usability intervention participants selected, changes to the bathroom to facilitate bathing and grooming was chosen the most frequently (25.9%, n = 21). Other home changes included changes to facilitate cleaning (18.5%, n = 15), changes to improve mobility within the home (18.5%, n = 15), improvements in home safety (16%, n = 13), and improvements to the home entrance (12.3%, n = 10). We computed correlations between the type of change and personal/home characteristics such as demographics and home type (e.g., single family; not presented). While there were statistically significant coefficients, they were generally small with less than 5% of the variance in usability type accounted for by personal/home characteristics. The one exception was whether or not participants lived in a single family or multifamily housing unit. Living in a single family home accounted for 15% of the variation in selecting a safety change.
Table 4 includes the regression coefficients for the overall intervention effect on social and recreational activities and for the effect based on the type of change consumers chose to make. We are not presenting coefficients for our control variables as they are unlikely to contribute to a causal interpretation as indicated by Hunermund and Louw.29 Overall, intervention participants reported a 39.5% (p < .05) increase in social and recreational activities immediately following the intervention relative to the control group after controlling for health status and month when outcome data were collected. Six months after the intervention, this effect returned to baseline. Examination of specific intervention targets chosen by participants suggested the overall results were driven by changes in the bathroom (72% increase, p < .01), changes to make the home safer (80% increase, p < .05), and changes to improve sleeping (112% increase, p < .05). We did not observe any effects for the number of trips into the community that people reported.
Table 4.
Poisson regression of treatment effects on social and recreational activities immediate post intervention.
| Variable | Incident Rate Ratio | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention*Post | 0.395* (0.163) | |||||||
| Bathroom | 0.728** (0.198) | |||||||
| Cleaning | 0.214 (0.282) | |||||||
| Safety | 0.798* (0.352) | |||||||
| Mobility | 0.421 (0.345) | |||||||
| Entrancing | 0.614 (0.388) | |||||||
| Cooking | 0.160 (0.297) | |||||||
| Sleeping | 1.645** (0.287) |
Note: Health status and month of post-test collection were control variables in this analysis.
p < .05
p < .01.
Discussion
Overall, these results are consistent with other recent findings about the relationship between the home environment and community participation. For example, Ravesloot et al.30 recently reported that people with mobility impairments who must navigate stairs to enter/exit their homes report substantially less social and recreational activities than those without steps. Similarly, Santasier et al.20 reported that modifications to the bathroom, including adding bath benches, led to people reporting less time alone.
These results highlight differences between participation in obligatory and discretionary participation. Home usability changes did not have any effect on how much people went to places in the community often associated with obligatory activities like grocery shopping or picking up prescription drugs. Rather, effects were evident for discretionary activities like socializing with friends. This may be related to the amount of energy it takes to do daily home tasks like bathing. Research is beginning to link how much energy daily living consumes with the likelihood that people engage in discretionary activities.20 It may be that when consumers choose home usability changes, they tend toward making changes that help to conserve energy. Results for bathroom and entrancing changes on discretionary activities in this study are consistent with this interpretation. It is important to note that these results were observed immediately following the intervention, but not six months later. It may be that people adapted to the home usability changes such that their choices for discretionary activities were no longer affected by changes in their environment. Future research could examine the decision-making features that influence choices for engaging in discretionary activities, including energy expenditure and fatigue.
This research also supports that robust effects may be observed through the implementation of simple, low-cost interventions. CIL staff were oftentimes not able to identify sources of funding outside of the grant funds allocated for this research. Thus, the interventions implemented for this study cost $350 or less to implement. While future analysis could explore the impact modification cost has on community participation, these results suggest that even simple, low-cost interventions (e.g., grab bars, shower chairs, non-slip bathmats) can increase the participation of people with mobility disabilities. Further research comparing low-cost, consumer-directed usability goals to home modification interventions larger in magnitude may be warranted. For example, it is possible that interventions smaller in magnitude, such as a non-slip bathmat, may not affect participation to the extent of an intervention larger in magnitude, such as a full bathroom remodel. It is also possible that ongoing intervention services (continued home usability support) may lead to greater participation than “one-time” interventions larger in magnitude. Thus, additional research is needed to examine if continued, ongoing services to support consumer-directed home usability goals may be sufficient to maintain participation effects over time.
Finally, these results indicate that consumer-directed home usability changes can increase participation in social and recreational activities. These results are important because consumers chose the home usability interventions applied, rather than having these goals prescribed to them. Tailored approaches like these have proved effective in improving health and increasing community engagement via home- and community-based services.31
Limitations
This study has important limitations to the interpretation of results, which include common shortcomings associated with self-report data. Additionally, housing stock varies substantially by geographic location (e.g., age, design, costs) and, while this study was conducted in two locations, results may not generalize to other locations. We implemented a randomized study design to control for differences between the control and intervention groups. Participants who were randomized into the intervention were consented separately to participate in the home usability program, however, this led to substantial attrition in the intervention group with 21 participants choosing not to participate and subsequently treated as controls. It may be that these results only apply to people who consent to an in-home intervention that would not be observed had all participants consented to treatment. Additionally, there are a variety of challenges to implementing a randomized design in community-based settings including, but not limited to, threats to external validity, cross contamination of intervention components, and the ethics of consent.32 Finally, we did not include measures of consumer choice and control over the intervention process in the surveys and so were unable to understand the role that having that choice played in impacting participant’s community participation.
Conclusion
The home environment matters for community participation; a home environment that is useable and suitable can facilitate access to the community. Home usability modifications, such as those implemented via the Home Usability Program, can help conserve energy and prevent injury – paving the way for individuals to engage in social and recreational activities. While home and community environments are complex and difficult to measure, community-based research methods with more flexible, participant-centered designs are promising. As participation reflects the interaction between an individual and their environment, methods that focus on only the individual or their environment are limited. Instead, the best practice may be engaging with individuals to determine what they want and need from their home environment by asking: “What do you need?”
Funding Acknowledgment
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90RT5043). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
References
- 1.American Community Survey (ACS). Disability Characteristics. U.S. Census Bureau; 2019. [Google Scholar]
- 2.White GW, Paine-Andrews A, Mathews RM, Fawcett SB. Home access modifications: effects on community visits by people with physical disabilities. J Appl Behav Anal. 1995;28(4):457–463. 10.1901/jaba.1995.28-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White GW, Lloyd Simpson J, Gonda C, Ravesloot C, Coble Z. Moving from independence to interdependence: a conceptual model for better understanding community participation of Centers for independent living consumers. J Disabil Pol Stud. 2010;20(4):233–240. 10.1177/1044207309350561. [DOI] [Google Scholar]
- 4.Bo’sher L, Chan S, Ellen IG, Karfunkel B, Liao H. Accessibility of America’s Housing Stock: Analysis of the 2011 American Housing Survey (AHS). Social Science Research Network; 2015. 10.2139/ssrn.3055191. [DOI] [Google Scholar]
- 5.Greiman L, Ravesloot C. Housing characteristics of households with wheeled mobility device users from the American Housing Survey: do people live in homes that facilitate community participation? Community Dev. 2016;47(1): 63–74. 10.1080/15575330.2015.1108989. [DOI] [Google Scholar]
- 6.Berg K, Hines M, Allen S. Wheelchair users at home: few home modifications and many injurious falls. Am J Publ Health. 2002;92(1). 10.2105/AJPH.92.1.48, 48–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stineman MG, Ross RN, Maislin G, Gray D. Population-based study of home accessibility features and the activities of daily living: clinical and policy implications. Disabil Rehabil. 2007;29(15):1165–1175. [DOI] [PubMed] [Google Scholar]
- 8.Hwang E, Cummings L, Sixsmith A, Sixsmith J. Impacts of home modifications on aging-in-place. J Hous Elder. 2011;25(3):246–257. 10.1080/02763893.2011.595611. [DOI] [Google Scholar]
- 9.Stineman MG, Xie D, Streim JE, et al. Home accessibility, living circumstances, stage of activity limitation, and nursing home use. Arch Phys Med Rehabil. 2012;93(9):1609–1616. 10.1016/j.apmr.2012.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shakespeare T The social model of disability. In: The Disability Studies Reader. second ed. 2006:197–204. [Google Scholar]
- 11.Stark S, Keglovits M, Arbesman M, Lieberman D. Effect of home modification interventions on the participation of community-dwelling adults with health conditions: a systematic review. Am J Occup Ther. 2017;71(2). 10.5014/ajot.2017.018887, 7102290010p.1. [DOI] [PubMed] [Google Scholar]
- 12.Seekins T, Shunkamolah W, Bertsche M, et al. A systematic scoping review of measures of participation in disability and rehabilitation research: a preliminary report of findings. Disabil Health J. 2012;5(4):224–232. 10.1016/j.dhjo.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Cheng S-L, Prohn SM, Dinora P, Broda MD, Bogenschutz M. Measuring and tracking personal opportunity outcome measures over 3 Years to Guide policy and services that promote inclusive community living. Inclusion. 2020;8(4): 335–350. 10.1352/2326-6988-8.4.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Üstün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: a new tool for understanding disability and health. Disabil Rehabil. 2003;25(11–12):565–571. 10.1080/0963828031000137063. [DOI] [PubMed] [Google Scholar]
- 15.Crawford A, Hollingsworth HH, Morgan K, Gray DB. People with mobility impairments: physical activity and quality of participation. Disabil Health J. 2008;1(1):7–13. 10.1016/j.dhjo.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Dean CM, Rissel C, Sherrington C, et al. Exercise to enhance mobility and prevent falls after stroke: the community stroke club randomized trial. Neurorehabilitation Neural Repair. 2012;26(9):1046–1057. 10.1177/1545968312441711. [DOI] [PubMed] [Google Scholar]
- 17.Samuel PS, Lacey KK, Giertz C, Hobden KL, LeRoy BW. Benefits and quality of life outcomes from transportation voucher use by adults with disabilities. J Pol Pract Intellect Disabil. 2013;10(4):277–288. 10.1111/jppi.12054. [DOI] [Google Scholar]
- 18.Gray DB, Dashner JL, Morgan KA, et al. Influence of a consumer-directed personal assistance services program on the lives of persons with mobility impairments. Disabil Health J. 2009;2(4):188–195. 10.1016/j.dhjo.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Carnemolla P, Bridge C. A scoping review of home modification interventions – mapping the evidence base. Indoor Built Environ. 2020;29(3):299–310. 10.1177/1420326X18761112. [DOI] [Google Scholar]
- 20.Santasier AM, Myers A, Ward B, Bainbridge D, Ravesloot C. “I have more energy to do it”: how reducing the effort cost of bathing can promote community participation. Unplublished Manuscr Reserach Train Cent Disabil Rural Communties. Published online. 2020. [Google Scholar]
- 21.Fänge A, Iwarsson S. Changes in ADL dependence and aspects of usability following housing adaptation—a longitudinal perspective. Am J Occup Ther. 2005;59(3):296–304. 10.5014/ajot.59.3.296. [DOI] [PubMed] [Google Scholar]
- 22.Breitenstein SM, Gross D, Garvey CA, Hill C, Fogg L, Resnick B. Implementation fidelity in community-based interventions. Res Nurs Health. 2010;33(2): 164–173. 10.1002/nur.20373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adam SL, Morgan KA. Meaningful components of a community-based exercise program for individuals with disabilities: a qualitative study. Disabil Health J. 2018;11(2):301–305. 10.1016/j.dhjo.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Hawe P, Shiell A, Riley T. Complex interventions: how “out of control” can a randomised controlled trial be? BMJ. 2004;328(7455):1561–1563. 10.1136/bmj.328.7455.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Camden C, Shikako-Thomas K, Nguyen T, et al. Engaging stakeholders in rehabilitation research: a scoping review of strategies used in partnerships and evaluation of impacts. Disabil Rehabil. 2015;37(15):1390–1400. 10.3109/09638288.2014.963705. [DOI] [PubMed] [Google Scholar]
- 26.Trickett EJ, Beehler S, Deutsch C, et al. Advancing the science of community-level interventions. Am J Publ Health. 2011;101(8):1410–1419. 10.2105/AJPH.2010.300113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Free publication - AARP HomeFit Guide. AARP. Accessed http://www.aarp.org/livable-communities/housing/info-2020/homefit-guide.html. Accessed January 19, 2021. [Google Scholar]
- 28.Livingston NA, Hargrove T, Greiman L, Myers A, Ipsen C, Ravesloot C. An investigation into the temporal scaling of community participation measurement. Rehabil Psychol. 2015;60(4):367–375. 10.1037/rep0000062. [DOI] [PubMed] [Google Scholar]
- 29.Hünermund P, Louw B. On the nuisance of control variables in regression analysis. ArXiv200510314 Econ. Published online October 1, 2020. Accessed May 19, 2021. http://arxiv.org/abs/2005.10314.
- 30.Ravesloot C, Myers A, Greiman L, Ward B, Schinnick- Goddard K, Hall J. How much do home entrance steps affect participation of people with mobility impairments? Rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee M, Heo H-H, Oh S, Kim E, Yoon B. Patient-centered evaluation of home-based rehabilitation developed using community-based participatory research approach for people with disabilities: a case series. Disabil Rehabil. 2018;40(2):238–248. 10.1080/09638288.2016.1250121. [DOI] [PubMed] [Google Scholar]
- 32.Sanson-Fisher RW, Bonevski B, Green LW, D’Este C. Limitations of the randomized controlled trial in evaluating population-based health interventions. Am J Prev Med. 2007;33(2):155–161. 10.1016/j.amepre.2007.04.007. [DOI] [PubMed] [Google Scholar]


