Abstract
Objectives:
To estimate the indirect economic impact of tibial fractures and their associated adverse events (AEs) in Tanzania.
Design:
A secondary analysis of the pilot Gentamicin Open (pGO)-Tibia randomized control trial estimating the indirect economic impact of suffering an AE, defined as a fracture-related infection (FRI) and/or nonunion, after an open tibial fracture in Tanzania.
Setting:
The pGO-Tibia trial was conducted from November 2019 to August 2021 at the Muhimbili Orthopaedic Institute in Dar es Salaam, Tanzania.
Patients/Participants:
One hundred adults with open tibial shaft fractures participated in this study.
Intervention:
Work hours were compared between AE groups. Cost data were analyzed using a weighted-average hourly wage and converted into purchasing power parity–adjusted USD.
Main Outcome Measurements:
Indirect economic impact was analyzed from the perspective of return to work (RTW), lost productivity, and other indirect economic and household costs. RTW was analyzed using a survival analysis.
Results:
Half of patients returned to work at 1-year follow-up, with those experiencing an AE having a significantly lower rate of RTW. Lost productivity was nearly double for those experiencing an AE. There was a significant difference in the mean outside health care costs between groups. The total mean indirect cost was $2385 with an AE, representing 92% of mean annual income and an increase of $1195 compared with no AE. There were significantly more patients with an AE who endorsed difficulty affording household expenses postinjury and who borrowed money to pay for their medical expenses.
Conclusions:
This study identified serious economic burden after tibial fractures, with significant differences in total indirect cost between those with and without an AE.
Level of Evidence:
II.
Keywords: open tibial fractures, indirect cost, economic impact, adverse events, orthopaedics
1. Introduction
Fracture-related disability is a significant public health and economic burden worldwide.1 Since the 1990s, the global incidence of fractures has increased by 33%, and the years lived with disability from fractures has increased by 65%.1 Tibial fractures are the most common type of long-bone fracture and most likely to be open.2 Open fractures are at higher risk of both developing fracture-related infections (FRIs) and progressing to nonunion.3,4 Both FRIs and nonunion contribute increased morbidity, loss of productivity, and other significant economic costs.1,3,5,6
The economic burden of open tibial fractures, FRI, and nonunion have been studied extensively in high-income countries (HICs).5–10 For example, one Belgian study found that total health care costs of open tibial fractures were double that of closed fractures and that one of the major cost drivers was infection.10 Another study found that FRI was associated with 8 times higher direct hospital costs than non-FRI patients.8 FRI has also been associated with higher median indirect costs and absenteeism when compared with patients without FRI.8 Similarly, a US-based study found that median total care costs for patients with nonunion was double than that of patients without.6
Although the economic costs of FRI and nonunion have been outlined in HICs, very little existing literature is written about the costs of these complications in LMICs. A Ugandan study outlined the themes of the economic burden of surgical care, including fracture care.11 Commonly cited themes included missed education, inability to work, loss of income/savings, and negative impact on business ventures.11 However, indirect costs are not explicitly reported in the literature. This is particularly relevant because most social safety nets, such as disability insurance, are not available in low-income settings. This study aims to measure the effect of FRI and nonunion on return-to-work (RTW) and indirect cost using data from a pilot randomized control trial on open tibial fractures in Tanzania.
2. Methods
2.1. The pilot Gentamicin Open-Tibia Trial
This study reports on the economic impact of suffering an adverse event (AE), defined as an FRI or nonunion, measured by RTW and indirect economic costs collected during the pilot Locally-applied Gentamicin versus Saline in Open Tibia Fractures (pGO-Tibia) trial conducted in Dar es Salaam, Tanzania.12 The pilot trial assessed the feasibility of a randomized control trial comparing the efficacy of local gentamicin with placebo for FRIs in open tibial shaft fractures.12 The single-center trial was a collaborative effort between the Muhimbili Orthopaedic Institute (MOI) in Dar es Salaam, Tanzania, and the Institute for Global Orthopaedics and Traumatology (IGOT) at the University of California, San Francisco (UCSF).12 The trial enrolled 100 Tanzanian patients and randomized them to either receive local gentamicin or saline placebo for their open tibial shaft fracture. Patients were enrolled from November 2019 to August 2020 and were followed for 1 year. The planned primary end point was the occurrence of FRI. Secondary end points included nonunion, reoperation, health-related quality of life, radiographic healing, clinical healing, suggestive FRI, lost productivity, and direct medical costs.12 Ethical approval was obtained by the National Institute of Medical Research, Tanzania (Ref#:NIMR/HQ/R.8a/Vol. IX/2958) and the UCSF Human Subjects Research Internal Review Board (IRB# 17-23950).
2.2. Measuring Indirect Economic Impact
Indirect economic cost data were collected at each visit, which included lost productivity, follow-up appointment costs, outside health care costs, loans, and items sold to cover costs. Lost productivity included paid and unpaid work and was measured using time from injury to RTW and mean work hours at each follow-up. Economic costs were compared between those with and without an AE by 1-year follow-up. In addition, lost productivity was compared at each follow-up between groups and with baseline. All cost data were converted from 2020 Tanzanian shillings (TSh) to 2020 US dollars (USD) using the World Bank purchasing power parity (PPP)-adjusted exchange rate (888.37 TSh/USD).13 A PPP-adjusted rate was used to better contextualize the costs faced by patients in Tanzania.
To better represent the economic impact of both paid and unpaid work, lost productivity costs were estimated using the mean hourly wage and preinjury and postinjury combined paid and unpaid work hours. Hourly wage was estimated by stratifying participants by their employment sector to calculate a weighted-average hourly wage using published minimum wages in Tanzania for each employment sector represented.14 Mean weekly wages were calculated at each follow-up and stratified between those with and without an AE. Mean weekly wages at follow-up for each group were plotted and trendlines integrated over time from the start of RTW. Preinjury work hours were also integrated over the time period to calculate lost productivity by subtracting postinjury work hours from preinjury work hours over time.
2.3. Statistical Analysis
Descriptive and inferential statistics were performed using Stata 17.15 Demographics and injury characteristics were compared to adjust for potential confounding. The 2-sample t test and Fisher exact test were used to compare continuous and categorical variables between those with and without an AE, respectively.
To address right censoring, a survival analysis was conducted to compare the rate of RTW between those with and without an AE using a Kaplan-Meier function. The risk of AE on the rate of RTW was further analyzed using both univariate and multivariate Cox regression models. Initially all variables with P-values ≤0.2 and putative risk factors for AE were included in the multivariate model. Established statistical methods were used to identify the optimal model fit.16
3. Results
3.1. Demographics
There was 80% follow-up at 1 year. Of the 100 participants in the pGO-Tibia trial, there were 22 who suffered an adverse event (AE), defined as having an FRI and/or nonunion. Demographic data can be seen in Table 1. The mean age was 34 years, with 80% being male. Most had either a primary (44%) or secondary (43%) education level. Road traffic injury was the most common mechanism of injury (85%). The most common injury was a Gustilo-Anderson Type IIIA tibial fracture (75%), fixed with either an intramedullary nail (53%) or external fixator (46%).
TABLE 1.
Patient Demographics
| Factor | Total | No AE | AE | P |
| N | 100 | 78 | 22 | |
| Age, mean (SD) | 34 (±12) | 33 (±13) | 35 (±12) | 0.51 |
| Sex (%) | 0.14 | |||
| Male | 80 (80%) | 65 (83%) | 15 (68%) | |
| Female | 20 (20%) | 13 (17%) | 7 (32%) | |
| BMI, mean (SD) | 25 (±4) | 25 (±3) | 26 (±5) | 0.24 |
| Smoking status (%) | 0.19 | |||
| Current smoker | 17 (17%) | 16 (21%) | 1 (5%) | |
| Former smoker | 5 (5%) | 4 (5%) | 1 (5%) | |
| Nonsmoker | 78 (78%) | 58 (74%) | 20 (91%) | |
| Alcohol use (%) | 0.81 | |||
| Yes | 58 (59%) | 32 (42%) | 8 (38%) | |
| No | 40 (41%) | 45 (58%) | 13 (62%) | |
| Diabetes (%) | 0.64 | |||
| Yes | 1 (1%) | 1 (1%) | 0 (0%) | |
| No | 96 (96%) | 75 (96%) | 21 (96%) | |
| Unknown | 3 (3%) | 2 (3%) | 1 (5%) | |
| HIV/AIDS status (%) | 0.41 | |||
| No | 91 (91%) | 72 (92%) | 19 (86%) | |
| Unknown | 9 (9%) | 6 (8%) | 3 (14%) | |
| Education completed (%) | 0.96 | |||
| None | 3 (3%) | 2 (3%) | 1 (5%) | |
| Primary | 44 (44%) | 34 (44%) | 10 (46%) | |
| Secondary ordinary | 42 (42%) | 33 (42%) | 9 (41%) | |
| Secondary advanced | 1 (1%) | 1 (1%) | 0 (0%) | |
| College/university | 10 (10%) | 8 (10%) | 2 (9%) | |
| Preinjury work (%)* | 0.78 | |||
| Yes | 79 (79%) | 62 (80%) | 17 (77%) | |
| No | 21 (21%) | 16 (21%) | 5 (23%) | |
| Mechanism of injury (%) | 0.41 | |||
| Road traffic injury | 84 (85%) | 67 (87%) | 17 (77%) | |
| Fall | 5 (5%) | 3 (4%) | 2 (9%) | |
| Crush injury | 5 (5%) | 3 (4%) | 2 (9%) | |
| Gunshot | 2 (2%) | 2 (3%) | 0 (0%) | |
| Other | 3 (3%) | 2 (3%) | 1 (5%) | |
| Injury to debridement, mean days (SD) | 0.88 (0.3) | 0.88 (±0.3) | 0.89 (±0.4) | 0.83 |
| Gustilo-Anderson classification (%) | 0.46 | |||
| Type I | 3 (3%) | 3 (4%) | 0 (0%) | |
| Type II | 22 (22%) | 19 (24%) | 3 (14%) | |
| Type IIIA | 75 (75%) | 56 (72%) | 19 (86%) | |
| Fixation type (%) | <0.001† | |||
| Intramedullary nail | 53 (53%) | 49 (63%) | 4 (18%) | |
| External fixation | 46 (46%) | 28 (36%) | 18 (82%) | |
| Cast | 1 (1%) | 1 (1%) | 0 (0%) | |
| Randomization (%) | 0.34 | |||
| Gentamicin | 55 (55%) | 33 (42%) | 12 (55%) | |
| Saline | 45 (45%) | 45 (58%) | 10 (46%) | |
| Injury to hospital, mean km (SD) | 22 (±24) | 20 (±14) | 32 (±41) | 0.030† |
Includes paid and unpaid work.
Statistically significant.
Demographic data were compared between those with or without an AE. There was no difference in socioeconomic factors between groups. There was a significant difference between groups based on fixation type (P < 0.001) and distance from injury to the hospital (P = 0.03), with external fixation and longer distance from hospital associated with increased risk of an AE.
3.2. Return to Work
There were 79 participants who worked preinjury, with the majority working in trade/business (54%) or transportation (22%), as shown in Table 2. Only half of the participants returned to work by the end of follow-up, as shown in Table 3. Significantly less participants returned to work who suffered a complication (27%, P = 0.028) compared with no complication (73%). Of those who did RTW by the end of follow-up (50%), the mean time from injury to RTW was 27 weeks, with none returning to work before 6-week follow-up.
TABLE 2.
Participant Employment Categories and Wages
| Employment Category* | N | Mean Wage (2020 PPP-Adjusted USD/Hour) |
| Agriculture | 3 | $0.58 |
| Domestic worker/laborer | 5 | $0.46 |
| Education | 1 | $0.81 |
| Energy | 1 | $0.87 |
| Financial institutions | 2 | $2.31 |
| Fishing | 1 | $1.16 |
| Health care | 1 | $0.76 |
| Media | 1 | $0.87 |
| Restaurant/bar | 3 | $0.75 |
| Security | 1 | $0.87 |
| Trade, industry, and commerce | 43 | $0.66 |
| Transportation (inland) | 17 | $1.16 |
| Total | 79 | $0.82† |
Based on data from africapay.org.
Weighted average.
TABLE 3.
Indirect Cost Data
| Factor | Total | No AE | AE | P |
| Preinjury weekly work hours, mean (SD) | 61 (±23) | 61 (±23) | 61 (±24) | 0.981 |
| RTW by the end of follow-up? (%) | 0.028* | |||
| Yes | 50 (50%) | 44 (56%) | 6 (27%) | |
| No | 50 (50%) | 34 (44%) | 16 (73%) | |
| Weekly work hours postinjury, mean (SD)† | 44 (±35) | 50 (±34) | 24 (±33) | 0.006* |
| 2 weeks | 0 | 0 | 0 | |
| 6 weeks | 0 | 0 | 0 | |
| 3 months | 11 (±23) | 13 (±25) | 3 (±12) | 0.190 |
| 6 months | 27 (±35) | 33 (±36) | 5 (±19) | 0.012* |
| 9 months | 44 (±36) | 52 (±34) | 13 (±27) | 0.002* |
| 1 year | 56 (±35) | 64 (±30) | 25 (±37) | <0.001* |
| Travel to follow-up appointment, mean hours (SD) | 1.6 (±1.8) | 1.6 (±1.6) | 1.6 (±2.5) | 0.91 |
| Travel to follow-up appointment, mean cost (SD)‡ | $37.67 ± 38.60 | $35.37 ± 39.60 | $45.82 ± 34.44 | 0.26 |
| Outside health care costs postinjury? (%) | <0.001* | |||
| Yes | 49 (49%) | 32 (41%) | 19 (86%) | |
| No | 51 (51%) | 46 (59%) | 3 (14%) | |
| Amount of outside health care costs, mean (SD)‡ | $41.85 ± 85.98 | $18.76 ± 37.50 | $123.72 ± 143.84 | <0.001* |
Statistically significant.
Includes paid and unpaid work.
2020 PPP-adjusted USD
To account for right censoring as a result of missing follow-up, RTW was analyzed using a Kaplan-Meier function, as seen in Figure 1. The failure function was analyzed by AE using a univariate cox regression model, which demonstrated the rate of RTW as being 77% lower in patients with an AE (Hazard ratio = 0.33, 95% CI = [0.14,0.76], P = 0.010). The multivariate model, which adjusted for age, sex, smoking status, injury severity, and distance from hospital, demonstrated similar results to the univariate model (Hazard ratio = 0.33, 95% CI = [0.14, 0.82], P = 0.017).
Figure 1.
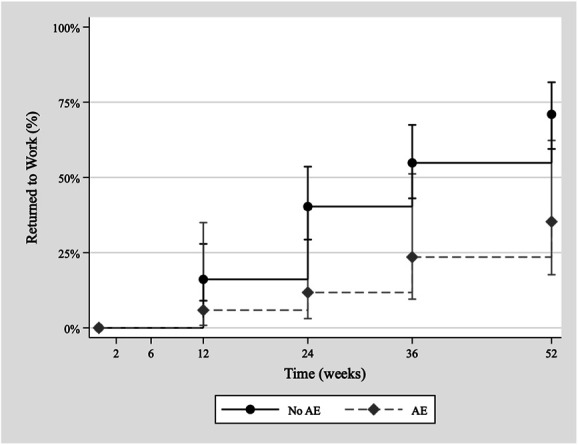
Kaplan-Meier RTW function (95% CI). RTW, return-to-work.
3.3. Indirect Costs
Among those employed preinjury (79%), the average participant worked 61 hours of work per week, including paid and unpaid work. Compared with preinjury work hours, patients employed preinjury worked significantly less at each follow-up until 1-year follow-up, as shown in Figure 2 (P ≤ 0.001). At 1-year follow-up, patients who had experienced an AE were working significantly less compared with preinjury (P = 0.019) while those without an AE were not (P = 0.971). In addition, there was a significant difference in work hours between AE groups after 6-month follow-up (P ≤ 0.012).
Figure 2.
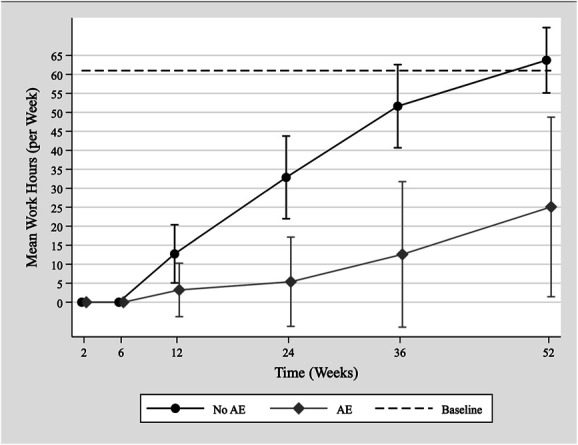
Mean follow-up work hours over time (95% CI).
Lost productivity was estimated using mean preinjury and postinjury work hours and the weighted-average hourly wage, which was estimated to be $0.82/h (724.33TSh/hour) or an annual income of $2569 (2,297,575 TSh). Mean postinjury work hours were plotted over time and stratified by the AE group (Fig. 2). Both curves were fitted to second-order polynomial functions (R2 > 0.99) and integrated over time from the start of RTW (Fig. 3). By 1-year follow-up, the mean work hours lost were estimated to be 1390 hours (44% of yearly mean) without AE and 2727 hours (86%) with AE. By 1-year follow-up, the mean lost productivity was estimated to be $1133 (1,006,819 TSh) without AE and $2224 (1,975,248 TSh) with AE. Between AE groups at 1 year, the lost productivity of having an AE was nearly double, with the difference being 1323 hours costing $1079 (958,289 TSh).
Figure 3.
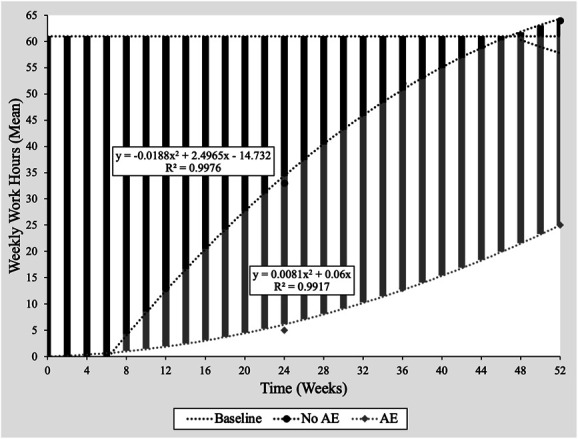
Polynomial trendlines for calculating lost productivity.
Other indirect costs measured included follow-up travel time and outside health care costs. The mean total follow-up travel time was 1.6 hours costing $38 (33,467 TSh), representing 1.5% of estimated yearly income. Forty-nine percent of participants endorsed outside health care costs postinjury, mostly surgical wound dressings, with significantly more endorsing these costs in the AE group (P < 0.001). In addition, there was a significant difference in the mean total outside health care costs between groups ($124 [109,909 TSh] AE vs. $19 [16,667 TSh] no AE, P < 0.001), representing 4.8% and 0.7% of estimated yearly income, respectively.
Overall, the total mean indirect cost as measured in this study was estimated to be $1190 (1,056,953 TSh) without AE and $2385 (2,118,624 TSh) with AE, representing 46% and 92% of mean annual income, respectively. In addition, there was a $1195 (1,061,671 TSh) increase in total mean indirect cost in the setting of an AE compared with no AE.
3.4. Other Household Economic Costs
Household economic costs were analyzed between groups, as shown in Table 4. Twenty-three percent of participants endorsed difficulty affording household expenses after surgery, with significantly more participants endorsing these difficulties who suffered an AE (P = 0.009). To pay for expenses postsurgery, 60% borrowed money with a mean value of $102 (90,350 TSh), representing 3.9% of estimated yearly income, and 82% sold assets for money with a mean value of $204 (180,800 TSh), representing 7.9% of estimated yearly income. There was a significant difference in borrowing between groups (P = 0.05).
TABLE 4.
Household Economic Costs
| Factor | Total | No AE | AE | P |
| Can you afford household expenses postinjury? (%) | 0.009* | |||
| Yes | 77 (77%) | 13 (17%) | 10 (45%) | |
| No | 23 (23%) | 65 (83%) | 12 (55%) | |
| Did you borrow money postinjury? (%) | 0.050* | |||
| Yes | 60 (60%) | 27 (35%) | 13 (59%) | |
| No | 40 (40%) | 51 (65%) | 9 (41%) | |
| Amount borrowed, mean (SD)† | $101.70 ± 199.02 | $83.05 ± 168.62 | $167.82 ± 276.75 | 0.078 |
| Have to sell assets for money postinjury? (%) | 0.22 | |||
| Yes | 82 (82%) | 12 (15%) | 6 (27%) | |
| No | 18 (18%) | 66 (85%) | 16 (73%) | |
| Amount sold, mean (SD)† | $203.52 ± 740.53 | $157.74 ± 656.62 | $365.83 ± 984.34 | 0.25 |
Statistically significant.
2020 PPP-adjusted USD
4. Discussion
This study was a secondary analysis of the pGo-Tibia trial estimating the indirect economic impact of suffering an adverse event, defined as an FRI or nonunion, after an open tibial fracture in Tanzania. Indirect economic impact was analyzed from the perspective of RTW, lost productivity, and other indirect economic costs. Only 50% of patients returned to work at 1-year follow-up, with those experiencing an AE having a significantly lower rate of RTW. Lost productivity was nearly double for those experiencing an AE, with those patients losing 86% of 1-year productivity. In addition, there were significantly more patients with an AE who endorsed difficulty affording household expenses postinjury and who borrowed money to pay for their medical expenses.
The economic impact of tibial fractures is significant and is greatly compounded by suffering an AE. This study determined that suffering an AE nearly doubled economic costs. However, one recent study in Belgium reported indirect costs as nearly 4 times higher in patients with FRI.8 This may be because costs are greater in high-resource countries and that patients in HICs are more likely to undergo reoperation. In Tanzania, many patients do not undergo reoperation for AEs because of the high cost of reoperation. For example, in this cohort, only 3 of 22 patients with an AE underwent reoperation. Although this may lessen the short-term economic costs, this likely results in substantially more clinical and quality-of-life impact in the long term because of the persistent pain and functional limitation from chronic osteomyelitis and/or nonunion.17 No other studies reporting the indirect costs of AEs after open tibial fractures in a low-resource country could be identified for comparison.
This study suggests that lost productivity is the main driver of economic impact from complicated tibial fractures in Tanzania. This is consistent with findings from other studies. A recent meta-analysis looking at the rate of RTW among patients with musculoskeletal injuries after road traffic accidents across 28 identified studies reported a pooled rate of RTW of 83% at 1 year, with 36% having taken some sick leave.18 However, most of these studies were conducted in high-income countries, and AEs were not considered. In addition, many LMICs do not have social safety nets such as disability insurance or sick leave, which results in increased individual economic burdens.19 Few RTW studies have been conducted in low-resource settings, and none could be identified that stratified patients by suffering from a complication. One study looking at patients with isolated tibial or femoral fractures in Uganda found that only 63% of patients returned to work within 2 years, with only 34% having returned to their previous income level.20 One study conducted in Belgium looked at the effect of FRI on absenteeism and identified a significant difference between those with and without FRI at 1 year (340 vs. 86 days, respectively). Although this study reported high rates of absenteeism, the actual economic impact may be less than in LMICs because of access to safety net programs.
The economic burden of fracture-related indirect costs is of concern. In this study, 23% of patients reported difficulty paying for hospital expenses, with a majority selling assets (82%) and more than half (60%) borrowing money to pay for these costs. Perceived difficulty paying for hospital expenses was comparable with data reported in the United States.21 One study in Uganda reported that only half of participants were willing to borrow money after orthopaedic trauma, with those who borrowed requesting principal loans of nearly the median annual income.22 Although patients borrowed significantly less in this study than those in Uganda, the percent borrowing money is comparable, and the amount borrowed in this study is consistent with other studies in low-resource settings.23 By contrast, one study in the United States looking at trauma patients reported that only 23% of patients had to take out loans for medical expenditures while 54% used savings to pay for medical care.21
This study had various limitations. The biggest limitation was missing data because of the lack of follow-up, ranging from 61% to 80% at each time point, with 80% follow-up at 1 year. In addition, this study did not factor presenteeism into the indirect cost. Furthermore, direct costs were not able to be collected using the same survey instruments used to capture indirect costs from patients. Direct costing requires direct observation of the procedures and care provided. The research team did not have the capacity to do this resource-intensive cost measurement for the follow-up care or reoperations that occurred during this study. Finally, although results were unchanged in the multivariate analysis, additional confounding from confounders that were not recorded in the study database remains a possibility.
In conclusion, this study found a high economic burden after open tibial fractures, which was significantly worse in cases complicated by infection and nonunion. Investments in strategies to prevent and more effectively treat open tibial fractures and their sequelae are needed to avoid catastrophic economic consequences.
Footnotes
The pilot Gentamicin Open-Tibia trial received funding from the Orthopaedic Trauma Association International Grant, the Hellman Fellows Fund as part of the UCSF Hellman Fellowship Program, and the UCSF Department of Orthopaedic Surgery.
This work was previously presented as an abstract at 2022 OTA meeting.
The authors report no conflict of interest.
This work was performed at the University of California, San Francisco, in partnership with the Muhimbili Orthopaedic Institute.
Authorship has been granted only to those individuals who have contributed substantially to the research or manuscript
Contributor Information
Michael J. Flores, Email: michael.flores@ucsf.edu.
Kelsey E. Brown, Email: kelsey_brown@brown.edu.
Billy Haonga, Email: bhaonga@gmail.com.
Saam Morshed, Email: saam.morshed@ucsf.edu.
David W. Shearer, Email: david.shearer@ucsf.edu.
References
- 1.Wu AM, Bisignano C, James SL, et al. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021;2:e580–e592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson JH, Koutsogiannis P, Jahangir A. Tibia fractures overview. In: StatPearls. StatPearls Publishing; 2021. Available at: http://www.ncbi.nlm.nih.gov/books/NBK513267/. Accessed November 18, 2021. [PubMed] [Google Scholar]
- 3.Metsemakers WJ, Kuehl R, Moriarty TF, et al. Infection after fracture fixation: current surgical and microbiological concepts. Injury. 2018;49:511–522. [DOI] [PubMed] [Google Scholar]
- 4.Tian R, Zheng F, Zhao W, et al. Prevalence and influencing factors of nonunion in patients with tibial fracture: systematic review and meta-analysis. J Orthop Surg Res. 2020;15:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tay WH, de Steiger R, Richardson M, et al. Health outcomes of delayed union and nonunion of femoral and tibial shaft fractures. Injury. 2014;45:1653–1658. [DOI] [PubMed] [Google Scholar]
- 6.Antonova E, Le TK, Burge R, et al. Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord. 2013;14:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olesen UK, Pedersen NJ, Eckardt H, et al. The cost of infection in severe open tibial fractures treated with a free flap. Int Orthop. 2017;41:1049–1055. [DOI] [PubMed] [Google Scholar]
- 8.Iliaens J, Onsea J, Hoekstra H, et al. Fracture-related infection in long bone fractures: a comprehensive analysis of the economic impact and influence on quality of life. Injury. 2021;52:3344–3349. [DOI] [PubMed] [Google Scholar]
- 9.Metsemakers WJ, Smeets B, Nijs S, et al. Infection after fracture fixation of the tibia: analysis of healthcare utilization and related costs. Injury. 2017;48:1204–1210. [DOI] [PubMed] [Google Scholar]
- 10.Hoekstra H, Smeets B, Metsemakers WJ, et al. Economics of open tibial fractures: the pivotal role of length-of-stay and infection. Health Econ Rev. 2017;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nwanna–Nzewunwa O, Oke R, Agwang E, et al. The societal cost and economic impact of surgical care on patients' households in rural Uganda; a mixed method study. BMC Health Serv Res. 2021;21:568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Kaeppler EP, Donnelley C, Ali SH, et al. A study protocol for a pilot masked, randomized controlled trial evaluating locally-applied gentamicin versus saline in open tibia fractures (pGO-Tibia) in Dar es Salaam, Tanzania. Pilot Feasibility Stud. 2021;7:47–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.PPP conversion factor, GDP (LCU per international $)—Tanzania|Data. Available at: https://data.worldbank.org/indicator/PA.NUS.PPP?locations=TZ. Accessed April 6, 2022. [Google Scholar]
- 14.Minimum wages. WageIndicator subsite collection. Available at: https://africapay.org/tanzania/salary/minimum-wages. Accessed April 6, 2022. [Google Scholar]
- 15.StataCorp. Stata statistical software: release 17. College Station, TX: StataCorp LLC, 2021. [Google Scholar]
- 16.Survival analysis with stata. Available at: https://stats.oarc.ucla.edu/stata/seminars/stata-survival/. Accessed September 1, 2022. [Google Scholar]
- 17.Cortez A, Urva M, Haonga B, et al. Outcomes of intramedullary nailing and external fixation of open tibial fractures: three to five-year follow-up of a randomized clinical trial. J Bone Joint Surg Am. 2022:104:1877–1885. [DOI] [PubMed] [Google Scholar]
- 18.Gane EM, Plinsinga ML, Brakenridge CL, et al. The impact of musculoskeletal injuries sustained in road traffic crashes on work-related outcomes: a systematic review. Int J Environ Res Public Health. 2021;18:11504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinda EM, Rajkumar AP, Attermann J, et al. Health, social, and economic variables associated with depression among older people in low and middle income countries: World Health Organization Study on Global AGEing and Adult Health. Am J Geriatric Psychiatry. 2016;24:1196–1208. [DOI] [PubMed] [Google Scholar]
- 20.O'Hara NN, Mugarura R, Potter J, et al. The socioeconomic implications of isolated tibial and femoral fractures from road traffic injuries in Uganda. J Bone Joint Surg Am. 2018;100:e43. [DOI] [PubMed] [Google Scholar]
- 21.Bhashyam AR, McGovern MM, Mueller T, et al. The personal financial burden associated with musculoskeletal trauma. J Bone Joint Surg Am. 2019;101:1245–1252. [DOI] [PubMed] [Google Scholar]
- 22.O'Hara NN, Odull E, Potter J, et al. The willingness of orthopaedic trauma patients in Uganda to accept financial loans following injury. OTA Int. 2019;2:e028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ir P, Jacobs B, Asante AD, et al. Exploring the determinants of distress health financing in Cambodia. Health Policy Plan. 2019;34(suppl 1):i26–i37. [DOI] [PMC free article] [PubMed] [Google Scholar]


