Summary:
The global market for hyaluronic acid (HA)-based dermal fillers has experienced substantial growth, providing patients with an effective nonsurgical cosmetic option. According to the global market report, the HA dermal fillers market size is expected to grow to $8.5 billion in 2027 at an annual growth rate (CAGR) of 8.9%. However, despite their popularity, HA injections are not free of complications. Vascular occlusion, particularly involving the central retinal artery, represents a significant risk. This case report presents a 60-year-old woman who presented with binocular vertical diplopia after HA filler injection in the right tear trough area. Upon evaluation, the patient exhibited right hypertropia, suggesting right inferior rectus paresis due to vascular injury of the infraorbital artery. Prompt management with hyaluronidase and oral steroids resulted in the resolution of double vision. This case highlights the importance of recognizing potential complications during HA filler injections and emphasizes the need for early intervention to minimize adverse effects.
A 60-year-old woman with a history of arthritis and hypertension was referred to the emergency department due to double vision during a cosmetic periocular injection. The patient was injected with 0.7 mL of 15 mg vycross hyaluronic acid (HA; Volbella Allergan AbbVie) with a 32-gauge needle in the right tear trough area by her dermatologist (Fig. 1). She reports that during this injection she immediately noticed discomfort, double vision, and nausea. No loss of vision was reported. Hyaluronidase was immediately injected with no relief of symptoms.
Fig. 1.
Red mark at right inferior periorbital area represents the area of injection of HA by dermatologist.
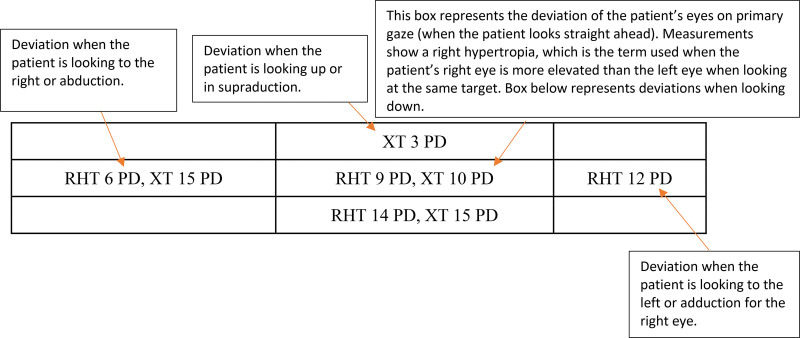
Upon arrival, the patient presented with stable vital signs and a visual acuity of 20 of 25 on both eyes and a normal intraocular pressure. No afferent pupillary defect was observed. Upon evaluation, there was a right hypertropia with small exotropia on primary gaze and livedo reticularis along the right infraorbital area. Extraocular movements were limited in right supraduction and infraduction with a negative forced duction test (Fig. 2). (See Video 1 [online], which displays the external motility exam on initial evaluation at our emergency department.) The patient was not able to fully look down with her right eye due to the right inferior rectus injury.
Fig. 2.
Motility examination. RHT, right hypertropia; XT, exotropia; PD, prism diopter.
Video 1. which displays the external motility exam on initial evaluation at our emergency department.
The rest of ocular examination was found normal, including no evidence of retinal ischemia. The patient was suspected to have a right inferior rectus paresis secondary to a vascular occlusion following HA filler injection.
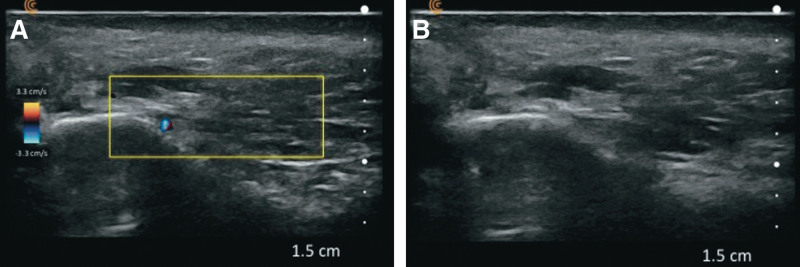
On follow-up examination, there was improvement in right infraduction but persistent diplopia. An ultrasound confirmed presence of hyaluronic material around the right inferior eyelid area (Fig. 3). The patient was started on dexamethasone 8 mg PO for 5 days and was referred to her dermatologist for further hyaluronidase treatment. The patient received a total of 1,500 IU of hyaluronidase around the right tear trough area. Three weeks after the filler injection, the patient was found with only a small deviation in downgaze but no complaints of diplopia.
Fig. 3.
Right tear trough skin ultrasound. A, B, Skin ultrasound showing hypoechoic areas corresponding to persistent HA material at the right tear trough area.
DISCUSSION
HA filler complications are classified based on severity. Mild complications can range from swelling or discomfort, whereas severe complications can result in necrosis and vascular occlusions.1 Mehta et al in January 2022 found 211 reported cases of vision loss after filler injections, but it is estimated that the actual number is significantly higher due to underreporting in the literature.2 However, based on our research,3 there are limited data describing isolated ophthalmoplegia after periocular HA filler injection.3,4 Our patient presented with persistent double vision with no other ocular complaints. We believe that our patient had vascular compromise to the right inferior rectus secondary to vascular injury of the infraorbital artery. Given the dual blood supply of the inferior rectus by the muscular branches of the ophthalmic artery and infraorbital artery, there can be mild weakness in the function of the muscle when one of its supplies becomes affected.5,6 Moreover, vascular injuries after filler injections are diverse, ranging from vascular compression to tissue necrosis.7 If dissemination of the HA occurs, it can lead to downstream vaso-occlusion and distal necrosis, which occurs as a retrograde emboli.2 Retrograde movement of the HA material is possible due to the complex facial vasculature and the Poiseuille law, which states that vessel branching and its reduced diameter increase resistance to anterograde flow.8
CONCLUSIONS
In conclusion, this report emphasizes the significance of the infraorbital artery as a secondary blood supply to the inferior rectus muscle and highlights its vulnerability during tear trough injections.9 Despite a positive outcome in our patient, the residual limitation in downgaze suggests vascular compromise and ischemia as the underlying etiology of the inferior rectus injury. These findings serve as a reminder of the diverse and potentially disabling presentations of injection-related complications. It is crucial for all physicians performing injections to possess a comprehensive understanding of periocular anatomy and be proficient in managing potential complications. Understanding the anatomy is paramount to ensure patient safety and optimal outcomes in aesthetic procedures involving periocular dermal fillers.10
DISCLOSURES
The authors have no financial interests to disclose in relation to this article.
PATIENT CONSENT
The patient provided written consent for the use of her image.
Footnotes
Published online 19 January 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Hönig JF, Brink U, Korabiowska M. Severe granulomatous allergic tissue reaction after hyaluronic acid injection in the treatment of facial lines and its surgical correction. J Craniofac Surg. 2003;14:197–200. [DOI] [PubMed] [Google Scholar]
- 2.Mehta P, Kaplan JB, Zhang-Nunes S. Ischemic complications of dermal fillers. Plast Aesthet Res. 2022;9:57. [Google Scholar]
- 3.Downie EM, Chen Y, Lucarelli MJ, et al. Isolated ophthalmoplegia following filler injections to the upper face. Ophthalmic Plast Reconstr Surg. 2020;36:e152–e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim A, Kim S-H, Kim H-J, et al. Ophthalmoplegia as a complication of cosmetic facial filler injection. Acta Ophthalmol. 2016;94:e377–e379. [DOI] [PubMed] [Google Scholar]
- 5.Shumway CL, Motlagh M, Wade M. Anatomy, head and neck, eye extraocular muscles [Updated 2022 Oct 13]. In: StatPearls. Treasure Island, Fla.: StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- 6.Chien HF, Wu CH, Wen CY, et al. Cadaveric study of blood supply to the lower intraorbital fat: etiologic relevance to the complication of anaerobic cellulitis in orbital floor fracture. J Formos Med Assoc. 2001;100:192–197. [PubMed] [Google Scholar]
- 7.Soares DJ. Bridging a century-old problem: the pathophysiology and molecular mechanisms of HA filler-induced vascular occlusion (FIVO)—implications for therapeutic interventions. Molecules. 2022;27:5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murthy R, Roos JCP, Goldberg RA. Periocular hyaluronic acid fillers: applications, implications, complications. Curr Opin Ophthalmol. 2019;30:395–400. [DOI] [PubMed] [Google Scholar]
- 9.De Silvia J. Facial danger zones: avoiding serious complications in non-surgical filler injections. Aesthetics. 2015;2:26–28. [Google Scholar]
- 10.Zein M, Tie-Shue R, Pirakitikulr N, et al. Complications after cosmetic periocular filler: prevention and management. Plast Aesthet Res. 2020;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]