Abstract
Background and Objectives
Unprecedented social restrictions during the coronavirus disease 2019 (COVID-19) pandemic have provided a new lens for considering the interrelationship between social isolation and loneliness in later life. We present these interrelationships before and during the COVID-19 restrictions and investigate to what extent demographic, socioeconomic, and health factors associated with such experiences differed during the pandemic.
Research Design and Methods
We used data from four British longitudinal population-based studies (1946 NSHD, 1958 NCDS, 1970 BCS, and ELSA, N = 12,129). Rates, co-occurrences, and correlates of social isolation and loneliness are presented prior to and during the early stage of the COVID-19 pandemic and the interrelationships between these experiences are elucidated in both periods.
Results
Across the Four studies, prepandemic proportions reporting social isolation ranged from 15% to 54%, with higher rates in older ages (e.g., 32% of individuals aged 70–79 years and 54% of those more than 80). During the pandemic, the percentage of older people reporting both social isolation and loneliness and isolation only slightly increased. The interrelationship between social isolation and loneliness did not change. Associations between sociodemographic and health characteristics and social isolation and loneliness also remained consistent, with greater burden among those with higher economic precarity (females, nonhomeowners, unemployed, illness, and greater financial stress).
Discussion and Implications
There were already large inequalities in experiences of social isolation and loneliness and the pandemic had a small impact on worsening extent and inequalities in these. The concepts of loneliness and social isolation are not interchangeable, and clarity is needed in how they are conceptualized, operationalized, and interpreted. Given many older adults experience high levels of social isolation, there should be greater emphasis on reducing social isolation and the inequalities observed in who experiences greater isolation and loneliness.
Keywords: Conceptualization, Inequalities, Networks, Overlap
Translational Significance: There is a conflation of “loneliness” and “social isolation” in research and policy, and over-emphasis on loneliness in U.K. policy (e.g., loneliness ministers). Being female, economic precarity, and long-standing illness consistently correlated with isolation and loneliness; structural changes and policies designed to reduce these inequalities are needed. Given many older adults experience high levels of social isolation, there should be greater emphasis on reducing social isolation. The increases in social isolation observed in the pandemic highlight the need for efforts to support older people to (re)start hobbies, volunteer, and socialize to reduce isolation and its consequences for health and well-being.
Background and Objectives
Prior to the coronavirus disease 2019 (COVID-19) pandemic, loneliness was identified as a significant public health concern (Jeste et al., 2019): for example, in the U.K., a Minister for Loneliness was appointed in 2018 and the “Campaign to End Loneliness” was launched. Despite increased policy interest, there remains a need to better understand the conceptualization and measurement of social isolation and loneliness as they are often inconsistently applied and interchangeably referred to across research, policy, and practice (Wigfield et al., 2022). With the implementation of social distancing and quarantine measures due to the COVID-19 pandemic and several national lockdowns across Britain, social isolation—and its relationship with loneliness—were brought into even sharper focus. By carefully considering the operationalization of these complex concepts, this study has the dual aim to (1) explore the conceptual and empirical interrelationships between social isolation and loneliness, and (2) identify overlapping and independent correlates of social isolation and loneliness prior to and during the COVID-19 pandemic. Using data from four British longitudinal studies, we investigate associations between social isolation and loneliness under normal circumstances and during COVID-19 restrictions and examine whether the factors associated with such experiences differ due to the pandemic.
As an objective condition, social isolation can be quantified by a person’s network size, composition, and frequency of contact (Holt-Lunstad et al., 2015; Huisman & van Tilburg, 2021). On the other hand, the way in which an individual perceives and experiences their social circumstances includes qualitative assessments of the value, function, and meaning ascribed to relationships. Loneliness arises as a negative feeling associated with the perception of an inadequate quantity and/or quality of social relationships (Zavaleta et al., 2017). It can therefore be experienced in the absence of isolation and vice versa, that is, those who are socially isolated may not experience loneliness (de Jong Gierveld et al., 2006; Perlman & Peplau, 1984; Power et al., 2019).
Data from the European Social Survey collected before the pandemic indicated that 8.6% of the adult population had frequent feelings of loneliness, whereas 20.8% were socially isolated (d’Hombres et al., 2021). It is clear that one experience can exist without the other, with only a moderate association observed between social isolation and loneliness (Hughes et al., 2004). Both constructs have also been found to independently predict poorer health, well-being, cognitive capability, and mortality in older age through different mechanisms (Coyle & Dugan, 2012; Golden et al., 2009; Steptoe, Shankar, et al., 2013), providing empirical evidence for a conceptual distinction between these two constructs. However, the investigation of objective indicators of social isolation is often neglected, with few studies examining the interaction between isolation and loneliness (Holt-Lunstad & Steptoe, 2022).
The burden of these experiences is also not equally shared and, although overlapping, the sociodemographic factors associated with social isolation and loneliness are varied. Common risk factors include low economic position and poor health; however, older age is associated with increased social isolation but not loneliness (d’Hombres et al., 2021). Despite being more likely to live alone in later life, recent findings indicate that women are less lonely than men (Barreto et al., 2021; Esteve et al., 2020). Investigations of the interaction between age and other sociodemographic factors provide a more nuanced picture. For example, low education level, deprivation, and female gender were only associated with loneliness in adolescence and early adulthood in a large Danish population-based study (Lasgaard et al., 2016). In the U.K., lower levels of loneliness were associated with the number of social interactions in early adult life and relationship quality in midlife (Victor & Yang, 2012).
Although several cross-sectional studies have indicated high levels of social isolation and loneliness during the COVID-19 restrictions, it is difficult to infer causality in the absence of prepandemic scores (Killgore et al., 2020). The first large-scale, population-based study investigating the psychological impact of the pandemic was based on data collected in the first Understanding Society COVID-19 survey (Li & Wang, 2020). Over a third of the sample reported feeling lonely sometimes or often during the pandemic. Young people, women, and those with COVID-19 symptoms were more likely to report loneliness and mental health difficulties, whereas those in employment and with a cohabiting partner were found to report less loneliness. Low income, not being married or cohabiting, smaller household size (adults only), higher depressive symptoms, living in an urban area, and lower number of close friends and social support were also associated with loneliness (Bu et al., 2020; Groarke et al., 2020).
Limited to the unique experience of lockdown, few of these studies tell us much about the stability of demographic, socioeconomic, and health characteristics associated with social isolation and loneliness before and during the pandemic and the strength of these associations. Were the people at risk of social isolation and loneliness prior to COVID-19 more likely to have these experiences during lockdown? Or were new groups disproportionately affected by the drastic changes to their lifestyle? To answer these questions in relation to loneliness, Bu et al., (2020) conducted a cross-cohort study using data from the U.K. Household Longitudinal Study (Understanding Society; 2017–2019) and the COVID-19 Social Study. Different groups of individuals were identified, including those whose risk of loneliness remained the same during the pandemic (e.g., women, urban residents, and those living alone), those who experienced heightened risk (e.g., those with low income and young people), and those who emerged as high-risk groups during the pandemic (e.g., students). Due to the use of different cohorts, this study is unable to directly compare the experiences of individuals over time and therefore cannot make conclusions about changes due to the pandemic. The use of multiple successive birth cohorts in the current study, alongside a multigenerational aging cohort, provides a further opportunity to examine cross-generational differences in experiences during the pandemic and tease apart age or cohort effects from period effects related to the pandemic.
This article aims to overcome some of the existing methodological limitations in the field and has two main aims. First, we describe levels of social isolation and loneliness prior to and during the COVID-19 restrictions, testing associations between social isolation and loneliness under normal circumstances and during the early stage of COVID-19 restrictions. By following the same individuals before and during the pandemic, we also provide better evidence for the differential impacts of restrictions on social isolation, loneliness, and their intersection. Second, we compare the correlates of social isolation and loneliness, and the relationship between them, pre- and during the COVID-19 restrictions to answer the following research questions:
Research Questions
What were the levels of social isolation and loneliness, and what proportion of the sample was classified into different groups, for example, isolated, and/or lonely prior to and during the COVID-19 restrictions?
What were the interrelationships between social isolation and loneliness indicators prior to and during the COVID-19 restrictions?
To what extent were demographic, socioeconomic factors, and physical and mental health associated with social isolation and loneliness prior to and during the COVID-19 restrictions?
Research Design and Methods
Data Sources
Data collected at two time points prior to and during the COVID-19 pandemic were utilized from four U.K. population-based studies. Three are longitudinal birth cohort studies with samples born within a single week across England, Scotland, and Wales: the 1946 MRC National Survey of Health and Development (NSHD; Kuh et al., 2016; Wadsworth et al., 2006), the 1958 National Child Development Study (NCDS; Power & Elliott, 2006), and the 1970 British Cohort Study (BCS; Elliott & Shepherd, 2006; Sullivan et al., 2022). In contrast, the English Longitudinal Study of Ageing (ELSA) is a panel study following individuals aged ≥50 years biennially since 2002 (Steptoe, Breeze, et al., 2013).
Table 1 provides details of the studies including participants’ age and timing of data collection across surveys. It also provides details of the survey designs, sampling frames, response rates, and analytic sample sizes.
Table 1.
Details of the Cohort Studies Including Participants’ Age and Timing of Data Collection, Survey Designs, Sampling Frames, Response Rates, and Analytic Sample Sizes
| Study population | Design and sample frame | 2020 Age range in years | Most recent prepandemic survey | Details of wave 1 COVID-19 survey (response rate) | Analytic N |
|---|---|---|---|---|---|
| Age homogenous cohorts | |||||
| BCS70: British Cohort Study 1970 | Cohort of all children born in Great Britain (i.e., England, Wales, and Scotland) in one week in 1970, with regular follow-up surveys from birth. | 50 | 2016 | February–March (40%) | 3,075 |
| NCDS: National Child Development Study | Cohort of all children born in Great Britain (i.e., England, Wales, and Scotland) in one week in 1958, with regular follow-up surveys from birth. | 62 | 2008 | February–March (52%) | 3,851 |
| NSHD: National Survey of Health and Development | Cohort of all children born in Great Britain (i.e., England, Wales, and Scotland) in one week in 1946, with regular follow-up surveys from birth. | 74 | 2015 | February–March (90%) | 763 |
| Age heterogeneous studies | |||||
| ELSA: English Longitudinal Study of Aging | A nationally representative population study of individuals aged 50+ living in England, with biennial surveys and periodic refreshing of the sample to maintain representativeness. | 52–90+ | 2018–2019 | June–July (75%) | 4,440 |
Note: COVID-19 = coronavirus disease 2019.
Participants
The analytic sample for each cohort included those who were alive, living in Great Britain, who took part in the study at two time points prior to and one wave during the early stages of the pandemic, and who completed the prepandemic and wave 1 COVID-19 surveys including outcomes of interest (social isolation and loneliness). Across all cohorts, we further restricted the sample to those who directly participated in the surveys (i.e., we excluded proxy respondents). Age bands that mapped onto the age homogenous cohorts during the COVID-19 pandemic (e.g., 50–59, 60–69, 70–79, and 80+) were generated for ELSA participants to enable analysis to differentiate between age or cohort and period effects related to the pandemic. Participants’ demographic, socioeconomic, and health characteristics are summarized in Supplementary File S1.
Sampling Design Weights and Accounting for Nonresponse Bias
To account for sampling design and nonresponse biases, weights were applied to studies to improve representativeness of their target populations, that is, the general population of mid to older age adults in Great Britain/England. For NSHD, design weights were included in the generation of nonresponse weights for the wave 1 COVID-19 survey. Only survey nonresponse weights for the wave 1 COVID-19 timepoint were included for NCDS, BCS, and ELSA. Given that certain groups of individuals are more likely to discontinue participation in longitudinal surveys (e.g., males and those disadvantaged and less healthy), accounting for nonresponse in analyses ensures that data from these participants are given more weight, resulting in a more representative sample.
Measures
This section provides details of the measurement of social isolation and loneliness prior to and during the COVID-19 pandemic, and an overview of demographic, socioeconomic, and health characteristics being investigated in the current study. Full details of the original items, harmonization, and recoding are included in Supplementary File S2.
Social isolation
Self-reported indicators of social isolation were identified in the four studies prior to and during the COVID-19 restrictions. Relevant items were organized by their relational context (e.g., household and community) and by the domain of social isolation assessed (e.g., network size and frequency of contact). For example, items were generated for isolation within the household (i.e., living alone), family network (i.e., partnership and children), frequency of contact with friends and relatives, education and employment status, frequency of contact with people in the community (e.g., frequency of attending community groups/organizations), and volunteering. To compare study members who were isolated across contexts prior to and during the COVID-19 restrictions, items were reduced to those which could be harmonized across time points. An overall social isolation score was generated with a total index score (maximum value of six) indicating the number of contexts an individual was isolated across. This variable was also recoded as a binary variable, for estimating proportions and visualizing overlaps with loneliness, where a score greater than 3 (indicating isolation in at least three contexts) was used as a binary indicator of social isolation.
Loneliness
Prior to the COVID-19 pandemic, not all cohorts asked participants a full measure of loneliness such as the University of California, Los Angeles Loneliness scale. However, items included “I feel left out of things” and related to the extent to which cohort members had been feeling close to others, for example, “I’ve been feeling close to other people.” To make variables comparable across cohorts, items were recoded as binary, indicating those that were lonely and not lonely. Across all four cohorts, the UCLA Loneliness scale (3-item; Hughes et al., 2004) was included in the COVID-19 survey along with an overall item, “How often do you feel lonely?” The short version of the Revised UCLA Loneliness scale (R-UCLA; Russell et al., 1980) consists of three items relating to lacking companionship, feeling left out, and feeling isolated from others, with simplified response options (“hardly ever” = 1, “some of the time” = 2, or “often” = 3). For cohorts that did not include the UCLA Loneliness scale prior to the COVID-19 pandemic, the best-matched item was selected during COVID-19 to generate the loneliness indicator. For example, as can be seen in Supplementary File S2, in NCDS there was only 1 item relating to feeling left out collected prior to the COVID-19 pandemic; this was therefore matched with the UCLA item during COVID-19 relating to feeling left out to generate the most comparable loneliness indicators. Designed for large-scale social surveys, the three-item UCLA Loneliness scale provides a reliable assessment of loneliness. Only a modest relationship was found between this measure of loneliness and objective social isolation (Hughes et al., 2004) supporting the conceptual distinction in the current study.
Demographic, socioeconomic, and health characteristics
Demographic variables included sex as well as age and ethnicity (in ELSA only). Cohort members’ highest level of educational achievement (degree vs no degree) was also included. Socioeconomic indicators were self-reported financial difficulties, home ownership, and occupational social class. A binary variable was generated to indicate those with “poor/fair” health (vs good, very good, or excellent health). In addition, whether cohort members report a limiting longstanding illness or health problem was included as a binary variable. Continuous measures of psychological distress and life satisfaction were also included as indicators of mental health and well-being (see Supplementary File S2 for details).
Analysis Strategy
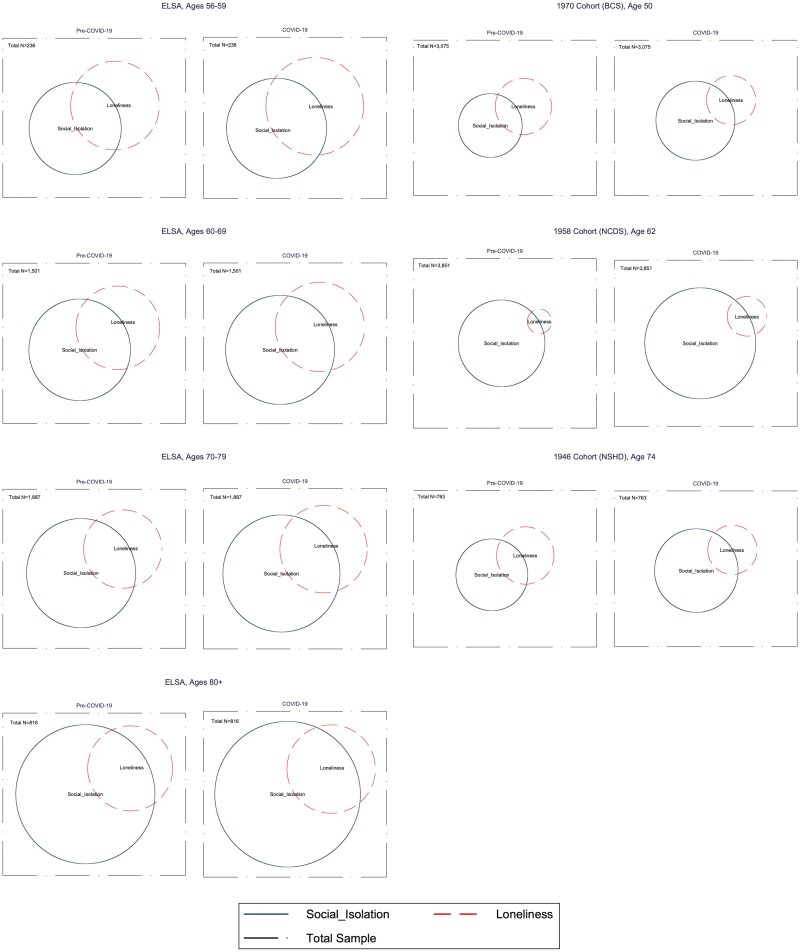
To answer the first research question and investigate the percentage of participants experiencing social isolation and loneliness prior to and during the first COVID-19 lockdown, binary variables were generated to identify those in each group. Using these indicator variables, the percentage of the sample reporting both, one, or neither was summarized prior to and during the COVID-19 restrictions. Analyses were stratified using age bands that mapped onto the other cohorts during the wave 1 COVID-19 timepoint for ELSA (50–59, 60–69, 70–79, 80+). We also presented Venn diagrams depicting the proportion of the cohort experiencing social isolation and loneliness prior to and during the pandemic and the extent of overlap between these experiences.
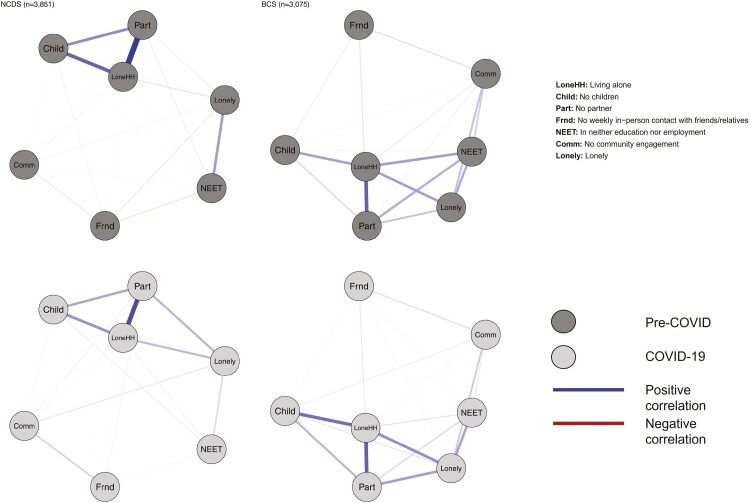
Our second research question was addressed by examining the associations between individual indicators of social isolation and loneliness prior to and during the first COVID-19 lockdown using tetrachoric correlations. Within each cohort, we estimated tetrachoric correlation matrices using data collected prior to the pandemic, and again during the COVID-19 restrictions. We then visualized these matrices as networks, using the “qgraph” package (Epskamp et al., 2018) in R. Our nodes were all the binary indicators of social isolation and loneliness that were available in each cohort, and the edges in the networks represented the strength of the tetrachoric correlations. We chose to present bivariate relationships in the networks rather than partial correlation coefficients to avoid introducing biased or spurious connections due to inappropriate statistical control (Wysocki et al., 2022).
The extent to which demographic, socioeconomic, and health characteristics were associated with social isolation and loneliness prior to and during the COVID-19 pandemic was examined using two modified Poisson regression models (Zou, 2004; Zou & Donner, 2013) for each outcome of interest and within each cohort study, that is, with social isolation and loneliness as dependent variables. For ELSA, models were stratified by age bands to ensure any age effects identified in the other cohort studies were not masked by ELSA’s age heterogenous sample.
Results
RQ1: Descriptives and Overlap of Social Isolation and Loneliness Prior to and During the COVID-19 Restrictions
Table 2 provides the count and weighted percentages of the sample reporting different indicators of social isolation and loneliness prior to and during the COVID-19 restrictions. Overall rates of social isolation and loneliness are also presented for each cohort and, for ELSA, presented by age band. In addition, Table 3 summarizes the count and weighted percentages of the sample reporting both social isolation and loneliness, social isolation only, loneliness only, or neither for the periods prior to and during the COVID-19 restrictions. By matching the appropriate ELSA age band with each of the other birth cohorts, Figure 1 also offers the opportunity to differentiate between age, cohort, and period effects related to the pandemic.
Table 2.
Count and Percentage of the Sample Reporting Social Isolation and Loneliness Prior to and During the COVID-19 Restrictions for Each Cohort
| Variable | NSHD | NCDS | BCS | ELSA | |||
|---|---|---|---|---|---|---|---|
| 70 | 50 | 46 | 50–59 | 60–69 | 70–79 | 80+ | |
| (n = 236) | (n = 1,501) | (n = 1,887) | (n = 816) | ||||
| Pre-COVID-19 | |||||||
| Social isolation % (N) | |||||||
| Living alone | 14.3 (109) | 9.8 (292) | 8.3 (160) | 16.6 (42) | 19.8 (282) | 22.8 (456) | 42.6 (340) |
| No children | 9.6 (73) | 16.2 (587) | 16.6 (489) | 18.9 (50) | 16.7 (259) | 10.7 (216) | 8.3 (74) |
| No partner | 16.0 (122) | 18.0 (581) | 15.9 (359) | 25.8 (59) | 27.9 (369) | 26.4 (510) | 50.2 (383) |
| No weekly in person contact with friends/relatives | 18.6 (142) | 57.7 (2,288) | 23.2 (766) | — | — | — | — |
| No weekly remote contact with friends/relatives | — | — | 5.1 (8) | 3.8 (56) | 4.3 (79) | 4.4 (35) | |
| In neither education nor employment | 78.8 (601) | 13.0 (372) | 13.2 (269) | 23.4 (53) | 53.6 (930) | 92.0 (18,740) | 99.2 (806) |
| No community engagement, that is, not a member of a club/organization or volunteer | 72.7 (555) | 77.2 (2,877) | 76.1 (2,174) | 90.0 (209) | 82.8 (1,196) | 77.6 (1,414) | 85.8 (672) |
| Social Isolation Indicator—high score (≥3) | 17.4 (133) | 22.8 (734) | 15.1 (346) | 22.8 (54) | 28.7 (415) | 31.6 (607) | 54.1 (418) |
| Loneliness % (N) | |||||||
| Feeling lack of companionship—often | 4.6 (35) | — | — | 8.4 (17) | 6.7 (93) | 5.1 (92) | 5.7 (41) |
| Feeling left out—often | 2.5 (19) | 2.2 (58) | — | 7.1 (12) | 3.5 (52) | 3.7 (62) | 4.3 (25) |
| Feeling isolated from others—often | 2.8 (21) | — | 11.9 (269) | 7.5 (16) | 4.7 (67) | 3.1 (53) | 3.9 (27) |
| Feeling lonely—often | — | — | — | 9.7 (21) | 7.2 (98) | 4.9 (86) | 5.0 (35) |
| UCLA total mean score (items 1–3) (3–9 range) | 3.74 | — | — | 4.28 | 4.13 | 3.98 | 4.20 |
| Loneliness Indicator—high score | 12.3 (94) | 2.2 (58) | 11.9 (269) | 22.8 (50) | 21.1 (281) | 17.3 (313) | 22.0 (156) |
| COVID-19 | |||||||
| Social isolation % (N) | |||||||
| Living alone | 24.4 (186) | 23.4 (834) | 13.8 (305) | 18.1 (43) | 22.2 (325) | 25.2 (495) | 45.7 (366) |
| No children | 5.5 (42) | 21.4 (765) | 18.9 (534) | 18.9 (50) | 16.7 (259) | 10.7 (216) | 8.3 (74) |
| No partner | 24.4 (186) | 16.7 (557) | 15.2 (345) | 28.0 (65) | 30.0 (414) | 30.6 (583) | 54.1 (422) |
| No weekly in person contact with friends/relatives | 0.5 (4) | 57.8 (2,217) | 59.5 (1,848) | — | — | — | — |
| No weekly remote contact with friends/relatives | 0.3 (2) | — | — | 3.0 (6) | 4.0 (54) | 4.2 (70) | 5.4 (38) |
| In neither education nor employment | 94.8 (723) | 66.9 (2,523) | 39.1 (1,034) | 43.5 (101) | 71.4 (1,171) | 96.7 (1,826) | 99.1 (806) |
| No community engagement, that is, not a member of a club/organization or volunteer | 36.4 (278) | 32.2 (1,139) | 26.3 (702) | 83.3 (193) | 79.6 (1,191) | 85.0 (1,586) | 88.1 (708) |
| Social Isolation Indicator—high score (≥3) | 22.2 (169) | 34.9 (1,226) | 22.6 (531) | 26.2 (63) | 32.5 (477) | 36.5 (693) | 57.2 (448) |
| Loneliness % (N) | |||||||
| Feeling lack of companionship—often | 4.5 (34) | — | — | 8.1 (20) | 7.1 (96) | 5.2 (100) | 8.5 (64) |
| Feeling left out—often | 2.2 (17) | 5.0 (156) | — | 6.2 (13) | 3.9 (57) | 3.4 (61) | 4.7 (32) |
| Feeling isolated from others—often | 9.0 (69) | — | 8.7 (205) | 8.3 (22) | 7.5 (102) | 6.2 (111) | 9.1 (64) |
| Feeling lonely—often | 3.7 (28) | — | — | 9.5 (20) | 5.8 (78) | 5.2 (90) | 4.9 (36) |
| UCLA total mean score (items 1–3) (3–9 range) | 3.98 | — | — | 4.42 | 4.2 | 4.14 | 4.25 |
| Loneliness Indicator—high score | 14.3 (109) | 5.0 (156) | 8.7 (205) | 25.6 (60) | 23.0 (320) | 20.4 (385) | 21.0 (165) |
Notes: BCS = 1970 British Cohort Study; COVID-19 = coronavirus disease 2019; ELSA = English Longitudinal Study of Ageing; NCDS = 1958 National Child Development Study; NSHD = 1946 MRC National Survey of Health and Development; UCLA = UCLA Loneliness scale. Weighted %. Social isolation indicator is calculated by giving a score of 1 for every type of social isolation and generating a score out of 6. Those with scores ≥3 indicate social isolation. Loneliness indicator is generated differently for NCDS and BCS, where the full UCLA Loneliness scale is not available. For these cohorts, loneliness = a response of “often” to the loneliness item available.
Table 3.
Count and % of the Sample Reporting Possible Combinations of Social Isolation and Loneliness Prior to and During the COVID-19 Restrictions for Each Cohort and for the Samples Combined
| Outcome variable | Pre-COVID-19 | COVID-19 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NSHD 70–79 |
NCDS 60–69 |
BCS 50–59 |
ELSA | NSHD 70–79 |
NCDS 60–69 |
BCS 50–59 |
ELSA | |||||||
| 50–59 | 60–69 | 70–79 | 80+ | 50–59 | 60–69 | 70–79 | 80+ | |||||||
| Both (socially isolated and lonely) | 3.3 (25) | 1.2 (26) | 4.8 (76) | 8.6 (20) | 10.7 (144) | 8.9 (165) | 15.7 (110) | 6.2 (47) | 2.9 (80) | 5.1 (81) | 11.3 (28) | 12.5 (170) | 11.4 (217) | 16.4 (126) |
| Only socially isolated | 14.2 (108) | 21.6 (708) | 17.8 (455) | 14.2 (34) | 18.1 (271) | 22.7 (442) | 38.4 (308) | 16.0 (122) | 32.0 (1,146) | 17.5 (450) | 14.9 (35) | 20.0 (307) | 25.1 (476) | 40.8 (322) |
| Only lonely | 9.0 (69) | 1.0 (32) | 7.2 (193) | 14.2 (30) | 10.4 (137) | 8.4 (148) | 6.2 (46) | 8.1 (62) | 2.1 (76) | 3.7 (124) | 14.3 (32) | 10.5 (150) | 9.0 (169) | 4.6 (39) |
| Neither | 73.5 (561) | 76.2 (3,085) | 70.3 (2,351) | 63.0 (152) | 60.9 (949) | 60.0 (1,132) | 39.7 (352) | 69.7 (532) | 63.0 (2,549) | 73.8 (2,420) | 59.5 (141) | 57.0 (874) | 54.5 (1,026) | 38.2 (329) |
Note: BCS = 1970 British Cohort Study; COVID-19 = coronavirus disease 2019; ELSA = English Longitudinal Study of Ageing; NCDS = 1958 National Child Development Study; NSHD = 1946 MRC National Survey of Health and Development; UCLA = UCLA Loneliness scale. Weighted percentages.
Figure 1.
Venn diagrams showing overlap in social isolation and loneliness across cohorts. BCS = 1970 British Cohort Study; COVID-19 = coronavirus disease 2019; ELSA = English Longitudinal Study of Ageing; NCDS = 1958 National Child Development Study; NSHD = 1946 MRC National Survey of Health and Development.
Table 3 shows that the percentages of respondents reporting social isolation and loneliness is generally higher in older ages in ELSA. We observe that 8.6%, 10.7%, 8.9%, and 15.7% of those aged respectively 50–59, 60–69, 70–79 and 80+ reported being both lonely and isolated in the pre-COVID-19 ELSA sample. Figures slightly increased in the COVID-19 wave with, respectively, 11.3%, 12.5%, 11.5%, and 16.4% of the sample. Looking at BCS, NCDS, and NSHD, percentages were 4.8, 1.2 and 3.3 in the pre-COVID-19 sweeps against 5.1, 2.9, and 6.2 during the pandemic.
The same trend is observed when looking at being socially isolated in ELSA: 14.2%, 18.1%, 22.7%, and 38.4% of those aged 50–59, 60–69, 70–79, and 80+ respectively reported being socially isolated in the prepandemic wave against 14.9, 20, 25.1, and 40.8 during the pandemic. Differences between prepandemic and pandemic times are of the same nature in BCS (17.8% and 17.5%) and NSHD (14.2% and 16%) but are slightly higher in NCDS (21.6% and 32%)
The percentages of those reporting being lonely but not socially isolated and neither socially isolated nor lonely decreased by age and did not change noticeably during the pandemic.
Finally, the percentages of those reporting being neither lonely nor socially isolated tend to be lower among older age groups. In ELSA, we can observe that 63% of those aged 50–59 reported neither social isolation nor loneliness against 59.5% during the pandemic. By contrast, figures for those aged 80+ were 39.7% before the pandemic and 38.2% during the pandemic. Percentages from BCS, NCDS, and NSHD are higher but show a similar pattern with respectively 70.3%, 76.3%, and 73.5% in prepandemic times and 73.8%, 63%, and 69.7% during the pandemic restrictions.
The Venn diagrams in Figure 1 illustrate the overlap between isolation and loneliness for each age-group and study as well as before and during pandemic restrictions. The left side of the figures shows the proportions for each age-band within ELSA, whereas their corresponding age-bands in BCS, NCDS, and NSHD are shown on the right side. Three main observations flow from these figures. First, the size of the circles representing social isolation and loneliness combined as well as their intersections tend to be bigger within ELSA than within the birth cohorts due to higher percentage of respondents reporting neither loneliness nor social isolation within the birth cohorts. Second, the size of the intersections (i.e., those reporting being lonely and isolated) has not noticeably changed during the pandemic restrictions. Finally, it can be observed that the share of the population aged 80+ reporting being only lonely (and not isolated) is small compared with other age-bands. For those aged 80 and older, social isolation seems to be associated with loneliness more than in the other age-groups.
RQ2: Interrelationships Between Social Isolation and Loneliness Indicators Prior to and During the COVID-19 Restrictions
Tetrachoric correlations between all indicators of social isolation and loneliness in the NCDS and BCS are presented as networks in Figure 2, and networks by age-bands in ELSA are presented in Supplementary File S3. Networks could not be estimated in NSHD due to a nonpositive definite correlation matrix, likely due to a tetrachoric correlation of 1 between living alone and partner status (i.e., all cohort members who lived alone also had no partner—likely a result of the advanced age of the cohort). As such, NSHD was excluded from this portion of the analyses. Within the NCDS and BCS cohorts, and also within ELSA age-bands, the networks were broadly similar pre- and during COVID, particularly for the strongest edges. In NCDS and BCS, loneliness was directly correlated with all measures of social isolation prior-to and during the pandemic. Prior to the pandemic, loneliness was most strongly associated with being out of work/education (NEET), living alone and having less than weekly contact with friends in the NCDS. During the pandemic, having no partner was most strongly associated with loneliness in this cohort, followed by living alone and NEET. For the BCS, the strongest prepandemic correlates of loneliness were living alone, NEET, and no community engagement. Living alone, having no partner, and NEET were the strongest correlates of loneliness in BCS during the pandemic.
Figure 2.
Tetrachoric correlation networks between indicators of social isolation and loneliness in National Child Development Study and British Cohort Study. BCS = 1970 British Cohort Study; COVID = coronavirus disease; COVID-19 = coronavirus disease 2019; NCDS = 1958 National Child Development Study.
In ELSA, the four indicators of self-reported loneliness/social isolation formed a strongly connected cluster of nodes. However, these clusters had many connections with the objective indicators of social isolation. Both prior to and during the pandemic, the strongest bridges between objective and subjective indicators of social isolation were between the “lives alone,” “has no partner,” “lacks companionship,” and “feels lonely” nodes. The tetrachoric correlation matrices used to create these networks are available in Supplementary File S4.
RQ3: Predictors of Social Isolation and Loneliness Prior to and During the COVID-19 Restrictions
Tables 4 and 5 present the results from the modified Poisson regression models for social isolation and loneliness prior to and during the COVID-19 pandemic. Demographic, socioeconomic, and health variables were added into the model in blocks.
Table 4.
Results from Modified Poisson Regression Models for Social Isolation Prior to and During the COVID-19 Pandemic Including Relative Risk (RR) and 95% Confidence Intervals (95% CI)
| Cohort | NSHD | NCDS | BCS | ELSA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time period | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | 50–59 | 60–69 | 70–79 | 80+ | ||||
| Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | |||||||
| Demographic | ||||||||||||||
| Gender (woman) | 1.64 0.92–2.91 |
1.25 0.61–2.56 |
1.02 0.86–1.20 |
1.05 0.94–1.18 |
0.65*** 0.48–0.88 |
0.83 0.67–1.04 |
1.21 0.70–2.06 |
1.22 0.75–1.98 |
1.11 0.89–1.36 |
1.18 0.97–1.43 |
1.30 1.12–1.51 |
1.29 1.13–1.48 |
1.76 1.48–2.09 |
1.63 0.38–1.90 |
| Black, Asian, and Minority Ethnic (if ethnic minority) | — | — | — | — | — | — | 0.44 0.13–1.50 |
0.75 0.26–2.19 |
1.02 0.54–1.87 |
1.03 0.59–1.80 |
0.98 0.55–1.72 |
1.20 0.77–1.87 |
1.09 0.79–1.50 |
1.03 0.74–1.44 |
| Education/socioeconomic | ||||||||||||||
| Degree (yes) | 1.40 0.81–2.41 |
0.96 0.38–2.44 |
0.94 0.71–1.25 |
0.91 0.74–1.12 |
1.15 0.80–1.67 |
1.01 0.77–1.33 |
0.69 0.35–1.35 |
0.98 0.56–1.71 |
1.09 0.83–1.42 |
0.92 0.73–1.15 |
0.94 0.77–1.15 |
0.82 0.69–0.98 |
0.86 0.67–1.11 |
0.91 0.72–1.15 |
| Self-reported financial difficulties (yes) | 1.28 0.54–3.04 |
1.25 0.48–3.25 |
1.41** 1.06–1.88 |
1.10 0.86–1.40 |
1.03 0.69–1.53 |
1.21 0.91–1.61 |
1.05 0.60–1.81 |
1.37 0.80–2.37 |
1.25 1.00–1.57 |
1.50 1.21–1.86 |
1.16 0.96–1.40 |
1.17 0.99–1.38 |
0.88 0.73–1.06 |
1.00 0.83–1.21 |
| Homeowner (yes) | 1.91 0.40–9.06 |
0.81 0.25–2.61 |
0.67*** 0.54–0.83 |
0.81** 0.68–0.97 |
0.41*** 0.31–0.54 |
0.57*** 0.45–0.73 |
0.47 0.27–0.83 |
0.60 0.33–1.07 |
0.46 0.37–0.57 |
0.52 0.42–0.63 |
0.52 0.44–0.63 |
0.51 0.44–0.59 |
0.67 0.57–0.79 |
0.72 0.61–0.83 |
| Occupational social classa | ||||||||||||||
| Intermediate (if yes) | 1.02 0.54–1.92 |
2.41 0.95–6.11 |
1.05 0.88–1.25 |
1.03 0.91–1.17 |
0.95 0.67–1.34 |
1.32 0.98–1.78 |
3.72 1.07–13.0 |
1.97 0.74–5.23 |
1.13 0.86–1.49 |
1.01 0.79–1.28 |
1.03 0.86–1.24 |
0.90 0.77–1.06 |
0.94 0.79–1.13 |
0.93 0.77–1.10 |
| Manual (if yes) | 0.65 0.22–1.91 |
2.72 0.67–10.93 |
0.85 0.63–1.15 |
0.91 0.09–0.76 |
0.78 0.54–1.14 |
1.47** 1.09–1.97 |
2.22 0.66–7.56 |
1.86 0.79–3.43 |
0.99 0.76–1.29 |
0.91 0.72–1.14 |
0.96 0.80–1.15 |
0.85 0.72–0.99 |
0.88 0.74–1.04 |
0.92 0.78–1.08 |
| Other (if yes) | 0.96 0.31–2.97 |
2.60 0.72–9.43 |
1.54*** 1.19–2.00 |
1.28** 1.02–1.62 |
2.56*** 1.79–3.65 |
2.81*** 2.08–3.79 |
2.81 0.99–7.98 |
1.79 0.85–3.79 |
1.08 0.76–1.53 |
1.06 0.77–1.44 |
0.49 0.11–2.14 |
0.37 0.08–1.73 |
1.00 0.71–1.42 |
1.07 0.77–1.48 |
| Managerial (ref.) | ||||||||||||||
| Physical and mental health | ||||||||||||||
| Self-reported health | 0.90 0.44–1.85 |
0.29 0.06–1.27 |
1.01 0.80–1.28 |
1.14 0.95–1.38 |
1.27 0.93–1.74 |
1.01 0.74–1.39 |
0.95 0.42–2.17 |
1.12 0.64–1.92 |
0.90 0.67–1.21 |
0.85 0.67–1.09 |
1.03 0.84–1.26 |
1.08 0.90–1.28 |
0.97 0.81–1.15 |
1.03 0.88–1.21 |
| Limiting long-standing illness or health problem (if yes) | 1.12 0.65–1.92 |
1.83 0.98–3.41 |
1.10 0.86–1.42 |
1.11 0.91–1.35 |
1.17 0.85–1.60 |
0.94 0.67–1.32 |
2.09 0.98–4.43 |
2.17 1.21–3.87 |
1.43 1.11–1.83 |
1.14 0.91–1.42 |
0.98 0.82–1.17 |
1.01 0.87–1.17 |
0.89 0.75–1.04 |
0.97 0.84–1.11 |
| Psychological distress | 1.29 0.81–2.04 |
0.96 0.55–1.66 |
1.01 0.94–1.09 |
0.96 0.89–1.02 |
1.02 0.91–1.15 |
1.05 0.95–1.17 |
0.98 0.77–1.24 |
1.13 0.90–1.41 |
1.06 0.96–1.17 |
1.00 0.92–1.08 |
1.05 0.97–1.14 |
0.99 0.89–1.06 |
1.08 1.01–1.15 |
1.06 1.00–1.13 |
| Life satisfaction | 0.74 0.66–0.84 |
0.70 0.60–0.81 |
0.91*** 0.87–0.95 |
0.93*** 0.89–0.96 |
0.92** 0.86–0.98 |
0.92*** 0.86–0.98 |
0.93 0.79–1.09 |
0.94 0.84–1.03 |
0.92 0.88–0.97 |
0.93 0.90–0.97 |
0.91 0.87–0.94 |
0.91 0.89–0.94 |
0.98 0.94–1.01 |
0.96 0.93–0.99 |
Notes: BCS = 1970 British Cohort Study; COVID-19 = coronavirus disease 2019; ELSA = English Longitudinal Study of Ageing; NCDS = 1958 National Child Development Study; NSHD = 1946 MRC National Survey of Health and Development; UCLA = UCLA Loneliness scale.
aOccupational Social Class refers to NS-SEC, the National Statistics Socio-Economic Classification, and is derived from the current or most recent (when the person is not working) job. Respondents who have never worked or for whom no NS-SEC information was collected are coded as “Other.”
**p < .05. ***p < .01.
Table 5.
Results From Modified Poisson Regression Models for Loneliness Prior to and During the COVID-19 Pandemic Including Relative Risk (RR) and 95% Confidence Intervals (95% CI)
| Cohort | NSHD | NCDS | BCS | ELSA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time period | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | 50–59 | 60–69 | 70–79 | 80+ | ||||
| Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | Pre-COVID-19 | COVID-19 | |||||||
| Gender (if woman) | 2.36 1.37–4.07 |
1.94 0.99–3.82 |
0.60 0.33–1.12 |
1.47** 0.96–2.25 |
0.54*** 0.39–0.75 |
1.04 0.65–1.67 |
1.08 0.62–1.86 |
1.79 1.05–3.06 |
1.39 1.07–1.81 |
1.75 1.35–2.27 |
1.32 1.05–1.65 |
1.69 1.37–2.10 |
1.39 0.99–1.95 |
1.62 1.14–2.30 |
| Black, Asian, and Minority Ethnic (if ethnic minority) | — | — | — | — | — | — | 2.47 1.22–5.00 |
2.28 1.12–4.64 |
2.21 1.46–3.35 |
1.52 0.94–2.46 |
0.96 0.39–2.13 |
0.54 0.17–2.10 |
0.92 0.28–3.02 |
1.32 0.54–3.26 |
| Education/Socioeconomic | ||||||||||||||
| Degree (if yes) | 1.38 0.84–2.27 |
1.01 0.51–1.99 |
0.46 0.11–1.91 |
0.70 0.32–1.51 |
0.98 0.64–1.49 |
0.86 0.52–1.41 |
0.73 0.37–1.40 |
0.61 0.32–1.14 |
0.47 0.32–0.70 |
1.04 0.79–1.37 |
0.63 0.45–0.89 |
0.99 0.78–1.27 |
0.79 0.47–1.32 |
0.91 0.58–1.43 |
| Self-reported financial difficulties (if yes) | 0.63 0.16–2.51 |
1.92 0.69–5.39 |
4.04*** 1.82–8.96 |
2.15** 1.14–4.05 |
2.19*** 1.40–3.43 |
2.05** 1.19–3.54 |
1.74 0.98–3.07 |
1.92 1.09–3.37 |
1.53 1.17–2.02 |
2.05 1.58–2.67 |
1.66 1.28–2.15 |
1.91 1.52–2.38 |
1.49 1.05–2.10 |
1.65 1.13–2.41 |
| Homeowner (if yes) | 0.90 0.30–2.71 |
0.74 0.28–1.94 |
1.58 0.62–4.02 |
0.57 0.31–1.05 |
0.77 0.55–1.09 |
0.42*** 0.29–0.62 |
0.70 0.40–1.21 |
0.95 0.51–1.76 |
0.80 0.58–1.09 |
0.70 0.52–0.93 |
0.72 0.52–1.00 |
0.74 0.55–1.00 |
0.70 0.47–1.04 |
1.00 0.62–1.63 |
| Occupational social classa | ||||||||||||||
| Intermediate (if yes) | 0.71 0.39–1.27 |
0.86 0.39–1.88 |
1.46 0.72–2.95 |
0.77 0.44–1.35 |
1.34 0.90–2.00 |
0.77 0.46–1.28 |
2.20 0.66–7.31 |
1.48 0.59–3.69 |
0.84 0.57–1.24 |
0.82 0.59–1.44 |
1.01 0.76–1.35 |
1.04 0.80–1.34 |
0.95 0.61–1.48 |
0.55 0.36–0.83 |
| Manual (if yes) | 0.57 0.22–1.53 |
1.28 0.42–3.96 |
2.26 0.69–7.39 |
0.87 0.49–1.54 |
1.93*** 1.33–2.80 |
1.29 0.81–2.04 |
1.64 0.60–4.47 |
1.08 0.51–2.27 |
1.32 0.95–1.83 |
0.99 0.73–1.34 |
0.97 0.74–1.28 |
1.11 0.87–1.41 |
0.91 0.63–1.32 |
0.78 0.55–1.11 |
| Other (if yes) | 0.45 0.15–1.34 |
0.49 0.15–1.61 |
5.76*** 2.61–12.70 |
1.98** 1.04–3.77 |
2.37*** 1.47–3.83 |
3.13*** 1.93–5.07 |
2.03 0.83–4.96 |
1.01 0.53–1.91 |
1.19 0.76–1.85 |
1.18 0.79–1.75 |
0.87 0.22–3.43 |
1.77 0.57–5.47 |
0.19 0.02–1.69 |
—b |
| Managerial (ref.) | ||||||||||||||
| Physical and mental health | ||||||||||||||
| Self-reported health | 0.97 0.55–1.69 |
1.64 0.93–2.90 |
1.04 0.58–1.85 |
0.77 0.41–1.45 |
1.52 0.99–2.34 |
0.91 0.58–1.41 |
1.00 0.46–2.17 |
1.27 0.74–2.16 |
0.76 0.54–1.06 |
0.76 0.54–1.04 |
0.62 0.46–0.82 |
0.89 0.69–1.13 |
1.28 0.88–1.86 |
0.75 0.51–1.11 |
| Limiting Long-standing illness or health problem (if yes) | 1.10 0.71–1.71 |
1.16 0.71–1.90 |
1.02 0.51–2.06 |
1.89** 1.10–3.25 |
0.90 0.59–1.38 |
1.07 0.71–1.61 |
1.57 0.76–3.26 |
1.59 0.86–2.97 |
1.22 0.90–1.65 |
0.87 0.66–1.17 |
0.76 0.58–0.97 |
1.09 0.87–1.36 |
1.36 0.95–1.96 |
0.88 0.61–1.26 |
| Psychological distress | 0.89 0.72–1.11 |
0.90 0.67–1.22 |
1.56*** 1.30–1.88 |
1.60*** 1.35–1.91 |
1.20*** 1.06–1.36 |
1.33*** 1.15–1.52 |
1.06 0.83–1.33 |
1.36 1.04–1.78 |
1.24 1.09–1.41 |
1.15 1.03–1.28 |
1.34 1.23–1.46 |
1.17 1.08–1.27 |
1.40 1.23–1.58 |
1.30 1.14–1.48 |
| Life satisfaction | 0.65 0.55–0.76 |
0.65 0.53–0.79 |
0.77*** 0.68–0.86 |
0.86*** 0.77–0.95 |
0.81*** 0.75–0.86 |
0.80*** 0.74–0.87 |
0.76 0.66–0.86 |
0.90 0.79–1.03 |
0.84 0.79–0.90 |
0.85 0.80–0.90 |
0.81 0.77–0.86 |
0.83 0.80–0.88 |
0.90 0.85–0.96 |
0.87 0.81–0.92 |
Notes: BCS = 1970 British Cohort Study; COVID-19 = coronavirus disease 2019; ELSA = English Longitudinal Study of Ageing; NCDS = 1958 National Child Development Study; NSHD = 1946 MRC National Survey of Health and Development; UCLA = UCLA Loneliness scale.
aOccupational Social Class refers to NS-SEC, the National Statistics Socio-Economic Classification, and is derived from the current or most recent (when the person is not working) job. Respondents who have never worked or for whom no NS-SEC information was collected are coded as “Other.”
bToo few cases.
**p < .05. ***p < .01.
Correlates of greater social isolation included female gender, manual occupational social class, self-reported financial difficulties, not being a homeowner, longstanding illness, and lower life satisfaction. There were no notable differences in the effect sizes of these associations in the prepandemic and lockdown periods.
Correlates of greater loneliness included female gender, not having degree-level education, manual occupational social class, self-reported financial difficulties, not being a homeowner, longstanding illness, greater psychological distress, and lower life satisfaction. There were no notable differences in the effect sizes of these associations in the prepandemic and lockdown periods.
Discussion and Implications
This study provides a conceptual and empirical contribution, presenting the interrelationship between social isolation and loneliness before and during the pandemic, with its unprecedented social restrictions. By using data from multiple successive birth cohorts, alongside several age-bands derived from a multigenerational aging cohort, we were also able to examine cross-cohort differences in experiences during the early stages of COVID-19 and distinguish age or cohort effects from period effects related to the pandemic. Furthermore, we present the demographic, socioeconomic, and health factors associated with experiences of social isolation and loneliness prior to and during the lockdown restrictions, adding to the literature that highlights the unequal burden of these experiences for females, those with greater economic precarity, including not owning a home, manual occupational social class, and greater financial stress.
We show support for these experiences as independent but related constructs (Hughes et al., 2004); however, our examination of demographic, socioeconomic, and health characteristics suggests mostly common correlates for these outcomes. Across all the data sets examined, and during both prepandemic and restricted periods of restrictions, more people reported being socially isolated than lonely based on our cutoff points. This maps onto findings from the European Social Survey collected before the pandemic, which indicated that 8.6% of the adult population had frequent feelings of loneliness, whereas 20.8% were socially isolated (d’Hombres et al., 2021). When examining age-based differences, we observe higher levels of isolation at older ages. However, levels of loneliness were more stable across later life. When comparing different age groups, we see that the overlap between social isolation and loneliness is fairly consistent pre- and during the COVID-19 restrictions.
Examining the associations at the indicator-level, we find that the interrelationships between indicators during the lockdown were less strongly connected compared to before the pandemic. This analysis suggests that there might have been an impact on how these concepts relate during restrictions, but these differences were not marked and are unlikely to indicate any fundamental differences in the conceptual links between loneliness and social isolation indicators during lockdown. The COVID-19 pandemic restrictions had specific effects on the prevalence of some of these indicators. For instance, remote contact increased and likely partially compensated for reductions in in-person contacts (Wels et al., 2023). There were also substantially fewer individuals in education and employment (Wels et al., 2022).
The study has several strengths, including the use of multiple data sources with slightly different designs and measures that permit the examination of consistency and replication of findings. However, there are limitations to note including the lack of availability of detailed measures of loneliness in the three birth cohorts before the pandemic, and data availability for relevant measures at certain timepoints (e.g., ELSA did not collect measures of face-to-face contact during the pandemic). We used data from participants who had responded before and during the pandemic surveys; this maintains a comparable sample, although those who dropped out might have been more isolated and in poorer health, potentially leading to some underestimation in the observed associations despite the use of sample and non-response weights in analyses.
By comparing data prior to and during enforced pandemic restrictions, we were able to provide insight into how these associations might vary in different contexts. In both these periods, we find similar associations between indicators of social isolation and loneliness, and with regard to other demographic, socioeconomic, and health correlates in both these periods. The number of study members reporting only isolation or loneliness, and the moderate overlap between older adults reporting both experiences indicate that these concepts are not interchangeable, and clarity in how they are conceptualized, operationalized, and interpreted in quantitative research is necessary. This, in turn, will contribute to a better understanding of the role and consequences of social isolation and loneliness in older age, and inform how interventions might support different aspects of these outcomes in older adults.
The increases in social isolation observed in the pandemic highlight the need for efforts to support older people to (re)start hobbies, volunteer, and schedule time to meet up with friends and neighbors, as these activities can also lead to health and other psychological benefits (Fancourt et al., 2022). The findings that being female, economic precarity, and long-standing illness are stable correlates of isolation and loneliness indicate a need for structural changes and policies designed to reduce these inequalities in experiences of isolation and loneliness.
We would also like to highlight the implications of our findings for the currently widespread conflation of the two terms “loneliness” and “social isolation” in policy, and the over emphasis on loneliness within the U.K. context (e.g., campaign to end loneliness, loneliness ministers). Given that many older adults experience high levels of social isolation, there should be greater emphasis on reducing social isolation through policy intervention rather than focusing on reducing individuals’ feelings of loneliness. Investigation of objective social isolation shifts the focus away from individuals and toward structural factors contributing to greater isolation and the inequities in these experiences and contributing factors (Umberson et al., 2022). This can help to identify areas that are modifiable through targeted policy and intervention.
Supplementary Material
Acknowledgments
The authors are grateful to all the cohort members who took part in the NSHD, NCDS, BCS, and ELSA cohorts analyzed in this article. We are also grateful to the survey and data management teams of the included longitudinal cohorts. The authors also acknowledge the input of the What Works Centre for Wellbeing, Campaign to End Loneliness, and our Stakeholder Advisory Group.
Contributor Information
Rosie Mansfield, Centre for Longitudinal Studies, University College London, London, UK.
Giorgio Di Gessa, Department of Epidemiology and Public Health, University College London, London, UK.
Kishan Patel, Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK.
Eoin McElroy, School of Psychology, Ulster University, Coleraine, Northern Ireland, UK.
Jacques Wels, Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK; Centre Metices, Université libre de Bruxelles, Brussels, Belgium.
Morag Henderson, Centre for Longitudinal Studies, University College London, London, UK.
Jane Maddock, Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK.
Jean Stafford, Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK.
Andrew Steptoe, Department of Behavioural Science and Health, University College London, London, UK.
Marcus Richards, Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK.
Praveetha Patalay, Centre for Longitudinal Studies, University College London, London, UK; Medical Research Council Unit for Lifelong Health and Ageing, University College London, London, UK.
Funding
This research was primarily supported by grants from the UK Economic and Social Council (ES/V012789/1 and ES/T007575/1). The authors also acknowledge the support of the Medical Research Council for the National Core Study in Longitudinal Health and Wellbeing (MC_PC_20059) and Medical Research Council Unit for Lifelong Health and Ageing (MC_UU_00019/1 and MC_UU_00019/3). In addition, J. Stafford, J. Maddock, and P. Patalay are supported by Alzheimer’s Society (Ref: 469). J. Wels is funded by the Belgian Fonds de la Recherche Scientifique (F.R.S.-FNRS) Research Associate-CQ research grant (40010931).
Conflict of Interest
None.
Data Availability
The data used for this project is available to all researchers from the U.K. Data Service: https://ukdataservice.ac.uk/ and NSHD: https://nshd.mrc.ac.uk/
References
- Barreto, M., Victor, C., Hammond, C., Eccles, A., Richins, M. T., & Qualter, P. (2021). Loneliness around the world: Age, gender, and cultural differences in loneliness. Personality and Individual Differences, 169, 110066. 10.1016/j.paid.2020.110066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu, F., Steptoe, A., & Fancourt, D. (2020). Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Social Science and Medicine, 265, 113521. 10.1016/j.socscimed.2020.113521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle, C. E., & Dugan, E. (2012). Social isolation, loneliness and health among older adults. Journal of Aging and Health, 24(8), 1346–1363. 10.1177/0898264312460275 [DOI] [PubMed] [Google Scholar]
- d’Hombres, B., Barjaková, M., & Schnepf, S. V. (2021). Loneliness and social isolation: An unequally shared burden in Europe (14245), 23.
- de Jong Gierveld, J., van Tilburg, T. G., & Dykstra, P. A. (2006). Loneliness and social isolation. In Perlman D. & Vangelisti A. (Eds.), The Cambridge handbook ofersonal relationships (pp. 485–500). Cambridge, UK: Cambridge University Press. [Google Scholar]
- Elliott, J., & Shepherd, P. (2006). Cohort profile: 1970 British Birth Cohort (BCS70). International Journal of Epidemiology, 35(4), 836–843. 10.1093/ije/dyl174 [DOI] [PubMed] [Google Scholar]
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteve, A., Reher, D. S., Treviño, R., Zueras, P., & Turu, A. (2020). Living alone over the life course: Cross-national variations on an emerging issue. Population and Development Review, 46(1), 169–189. 10.1111/padr.12311 [DOI] [Google Scholar]
- Fancourt, D., Mak, H. W., Noguchi, T., Bone, J., Wels, J., Gao, Q., Kondo, K., & Saito, T. (2022). Psychological benefits of hobby engagement in older age: A longitudinal cross-country analysis of 93,263 older adults in 16 countries. 10.21203/rs.3.rs-2349781/v1 [DOI] [Google Scholar]
- Golden, J., Conroy, R. M., Bruce, I., Denihan, A., Greene, E., Kirby, M., & Lawlor, B. A. (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry, 24(7), 694–700. 10.1002/gps.2181 [DOI] [PubMed] [Google Scholar]
- Groarke, J. M., Berry, E., Graham-Wisener, L., McKenna-Plumley, P. E., McGlinchey, E., & Armour, C. (2020). Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS One, 15(9), 1–18. 10.1371/journal.pone.0239698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad, J., & Steptoe, A. (2022). Social isolation: An underappreciated determinant of physical health. Current Opinion in Psychology, 43, 232–237. 10.1016/j.copsyc.2021.07.012 [DOI] [PubMed] [Google Scholar]
- Hughes, M. E., Waite, L. J., Hawkley, L. C., & Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huisman, M., & van Tilburg, T. G. (2021). Social exclusion and social isolation in later life. In Handbook of aging and the social sciences. Academic Press. 10.1016/b978-0-12-815970-5.00007-3 [DOI] [Google Scholar]
- Jeste, D. V., Lee, E. E., & Cacioppo, S. (2019). Battling the modern behavioral epidemic of loneliness: Suggestions for research and interventions. Physiology & Behavior, 176(3), 139–148. 10.1001/jamapsychiatry.2020.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore, W. D. S., Cloonan, S. A., Taylor, E. C., & Dailey, N. S. (2020). Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Research Journal, 290, 113117. 10.1016/j.psychres.2020.113117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh, D., Wong, A., Shah, I., Moore, A., Popham, M., Curran, P., Davis, D., Sharma, N., Richards, M., Stafford, M., Hardy, R., & Cooper, R. (2016). The MRC National Survey of Health and Development reaches age 70: Maintaining participation at older ages in a birth cohort study. European Journal of Epidemiology, 31(11), 1135–1147. 10.1007/s10654-016-0217-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasgaard, M., Friis, K., & Shevlin, M. (2016). “Where are all the lonely people?” Social Psychiatry and Psychiatric Epidemiology, 51(10), 1373–1384. 10.1007/s00127-016-1279-3 [DOI] [PubMed] [Google Scholar]
- Li, L. Z., & Wang, S. (2020). Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Research, 291(June), 113267. 10.1016/j.psychres.2020.113267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman, D., & Peplau Letitia Anne. (1984). Loneliness research: A survey of empirical findings. In Peplau L. A. & Goldston S. E. (Eds.), Preventing the harmful consequences of severe and persistent loneliness (pp. 13–46). National Institute of Mental Health. [Google Scholar]
- Power, C., & Elliott, J. (2006). Cohort profile: 1958 British birth cohort (National Child Development Study). International Journal of Epidemiology, 35(1), 34–41. 10.1093/ije/dyi183 [DOI] [PubMed] [Google Scholar]
- Power, J. E. M., Sjöberg, L., Kee, F., Kenny, R. A., & Lawlor, B. (2019). Comparisons of the discrepancy between loneliness and social isolation across Ireland and Sweden: Findings from TILDA and SNAC-K. Social Psychiatry and Psychiatric Epidemiology, 54(9), 1079–1088. 10.1007/s00127-019-01679-w [DOI] [PubMed] [Google Scholar]
- Russell, D., Peplau, L. A., & Cutrona, C. E. (1980). The revised UCLA Loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. 10.1037//0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Steptoe, A., Breeze, E., Banks, J., & Nazroo, J. (2013). Cohort profile: The English Longitudinal Study of Ageing. International Journal of Epidemiology, 42(6), 1640–1648. 10.1093/ije/dys168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe, A., Shankar, A., Demakakos, P., & Wardle, J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences of the United States of America, 110(15), 5797–5801. 10.1073/pnas.1219686110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan, A., Brown, M., Hamer, M., & Ploubidis, G. B. (2022). Cohort profile update: The 1970 British Cohort Study (BCS70). International Journal of Epidemiology, 52, e179–e186. 10.1093/ije/dyac148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Lin, Z., & Cha, H. (2022). Gender and social isolation across the life course. Journal of Health and Social Behavior, 63(3), 319–335. 10.1177/00221465221109634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor, C. R., & Yang, K. (2012). The prevalence of loneliness among adults: A case study of the United Kingdom. Journal of Psychology, 146(1–2), 85–104. 10.1080/00223980.2011.613875 [DOI] [PubMed] [Google Scholar]
- Wadsworth, M., Kuh, D., Richards, M., & Hardy, R. (2006). Cohort profile: The 1946 National Birth Cohort (MRC National Survey of Health and Development). International Journal of Epidemiology, 35(1), 49–54. 10.1093/ije/dyi201 [DOI] [PubMed] [Google Scholar]
- Wels, J., Booth, C., Wielgoszewska, B., Green, M. J., Di Gessa, G., Huggins, C. F., Griffith, G. J., Kwong, A. S. F., Bowyer, R. C. E., Maddock, J., Patalay, P., Silverwood, R. J., Fitzsimons, E., Shaw, R., Thompson, E. J., Steptoe, A., Hughes, A., Chaturvedi, N., Steves, C. J., & Ploubidis, G. B. (2022). Mental and social wellbeing and the UK coronavirus job retention scheme: Evidence from nine longitudinal studies. Social Science & Medicine, 308, 115226. 10.1016/j.socscimed.2022.115226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wels, J., Wielgoszewska, B., Moltrecht, B., Booth, C., Green, M. J., Hamilton, O. K., Demou, E., Di Gessa, G., Huggins, C., Zhu, J., Santorelli, G., Silverwood, R. J., Kopasker, D., Shaw, R. J., Hughes, A., Patalay, P., Steves, C., Chaturvedi, N., Porteous, D. J., … Ploubidis, G. B. (2023). Home working and social and mental wellbeing at different stages of the COVID-19 pandemic in the UK: Evidence from 7 longitudinal population surveys. PLoS Medicine, 20(4), e1004214. 10.1371/journal.pmed.1004214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigfield, A., Turner, R., Alden, S., Green, M., & Karania, V. (2022). Developing a new conceptual framework of meaningful interaction for understanding social isolation and loneliness. Social Policy and Society, 21(2), 172–193. 10.1017/S147474642000055X [DOI] [Google Scholar]
- Wysocki, A. C., Lawson, K. M., & Rhemtulla, M. (2022). Statistical control requires causal justification. Advances in Methods and Practices in Psychological Science, 5(2), 251524592210958. 10.1177/25152459221095823 [DOI] [Google Scholar]
- Zavaleta, D., Samuel, K., & Mills, C. T. (2017). Measures of social isolation. Social Indicators Research, 131(1), 367–391. 10.1007/s11205-016-1252-2 [DOI] [Google Scholar]
- Zou, G. (2004). A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology, 159(7), 702–706. 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- Zou, G., & Donner, A. (2013). Extension of the modified Poisson regression model to prospective studies with correlated binary data. Statistical Methods in Medical Research, 22(6), 661–670. 10.1177/0962280211427759 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used for this project is available to all researchers from the U.K. Data Service: https://ukdataservice.ac.uk/ and NSHD: https://nshd.mrc.ac.uk/