Abstract
Background
Video analysis (VA) is commonly used in the assessment of sports injuries and has received considerable research interest. Until now, no tool has been available for the assessment of study quality. Therefore, the objective of this study was to develop and evaluate a valid instrument that reliably assesses the methodological quality of VA studies.
Methods
The Quality Appraisal for Sports Injury Video Analysis Studies (QA-SIVAS) scale was developed using a modified Delphi approach including expert consensus and pilot testing. Reliability was examined through intraclass correlation coefficient (ICC3,1) and free-marginal kappa statistics by three independent raters. Construct validity was investigated by comparing QA-SIVAS with expert ratings by using Kendall’s tau analysis. Rating time was studied by applying the scale to 21 studies and computing the mean time for rating per study article.
Results
The QA-SIVAS scale consists of an 18-item checklist addressing the study design, data source, conduct, report, and discussion of VA studies in sports injury research. Inter- and intra-rater reliability were excellent with ICCs > 0.97. Expert ratings revealed a high construct validity (0.71; p < 0.001). Mean rating time was 10 ± 2 min per article.
Conclusion
QA-SIVAS is a reliable and valid instrument that can be easily applied to sports injury research. Future studies in the field of VA should adhere to standardized methodological criteria and strict quality guidelines.
Key Points
| Multiple rounds of consensus and pilot testing led to key domains and criteria for the development of the QA-SIVAS scale as a new instrument in the quality assessment of video analysis studies. |
| Testing of QA-SIVAS revealed the scale to be a reliable and valid instrument that can easily be adapted into sports research. |
| Although designed as an assessment tool, QA-SIVAS can also act as a guide for researchers when designing and conducting studies. |
Introduction
A healthy lifestyle including physical fitness has many benefits, and participation in sports activities is increasing [9]. However, injuries are frequent among athletes of all performance levels [16, 25], and the number one cause of injury-related emergency department visits in young populations is attributed to sports participation [47]. Compared with overuse injuries [24, 35], traumatic sports injuries are less predictable and the current lack of knowledge in preventing these conditions may substantially affect long-term health [17].
Detailed analyses of how injuries happen contribute to a more comprehensive understanding of the underlying factors [3]. A holistic approach is essential and requires the assessment of both the injury situation and biomechanical patterns [3, 13, 21]. Knowledge of the cause of injury has major implications for injury prevention but is also of clinical relevance for early on-field diagnosis.
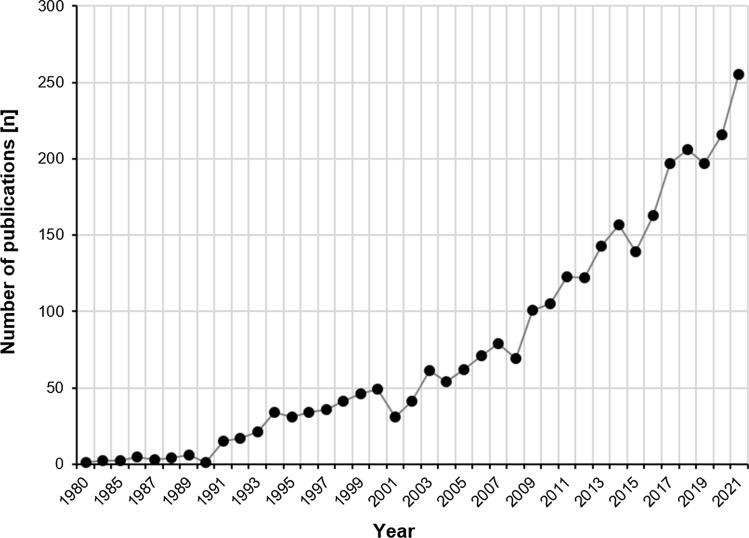
Video analysis (VA) has been an increasingly used tool to investigate sports injuries over the last 40 years (Fig. 1). It has gained high popularity in recent years, and there is widespread agreement regarding its scientific and clinical value to the sports medicine community [13, 21]. Among others, reports have been published describing situations, mechanisms and biomechanics of injury to the anterior cruciate ligament [13], Achilles tendon [14, 26], adductor longus muscle [43], and hamstring muscles [21]. However, to date, a lack of standardized methods is seen as a major limitation of VA studies [1]. Quality assessment tools, methodological gold standards, and consensus on terminology may increase consistency and allow a better comparison between studies. Most likely, with growing interest in the methodological framework of VA, systematic reviews will become available. A systematic appraisal of the literature provides the highest level of evidence, but can only be as good as the studies included [23]. Consequently, quality and risk of bias assessments of studies become necessary [23]. However, to date, no instruments exist for assessing study quality in video-based sports injury analysis. Thus, the objective was to develop and evaluate a tool that helps to assess the methodological quality of VA studies for the purpose of enhanced sports injury investigation.
Fig. 1.
Yearly number of studies for the search term “video analysis AND injury” since 1980 (Medline, accessed via PubMed on 21 November 2022)
Materials and Methods
The present study took place between January and December 2022 in three phases: (a) development of the QA-SIVAS (Quality Appraisal for Sports Injury Video Analysis Studies) scale; (b) evaluation of its reliability and within-item agreement, and (c) assessment of its construct validity and feasibility. Ethical approval was not required as this study did not involve any patient data. All expert panelists provided written consent to participate.
Scale Development
The QA-SIVAS scale was developed using a modified Delphi approach including expert consensus and pilot testing [47].
At first, experts in the field of sports science and sports medicine (TG, TH, LR, KH, DF, SW, PM, JW, and TK) independently listed criteria they considered important when assessing sports injuries by using VA. One reviewer (TG) summarized the group’s responses according to frequency and topic. The categorized criteria were then sent back to the experts. After comparing their submissions with those of the other reviewers, each reviewer was allowed to comment on other statements and to revise their own submissions. Subsequently, the criteria were again categorized by the same reviewer (TG). A face-to-face panel discussion with all contributing experts involved was then held, and this led to the development of the first version of QA-SIVAS. Five raters (TG, TH, LR, DF, SW) compared the scale against five randomly selected VA studies out of a pool of 21 included VA studies of anterior cruciate ligament (ACL) injuries from a recent systematic review project (PROSPERO registration: CRD42022337340). The preliminary testing was used to further adjust the rating criteria and instructions.
Reliability
To estimate inter- and intra-rater reliability, three reviewers (TG, LR, TH) independently assessed the risk of bias of all 21 VA studies from the aforementioned recent systematic review project (PROSPERO registration: CRD42022337340) by applying the QA-SIVAS scale. The rating was repeated after 3 weeks. The reliability of the main outcome, the total QA-SIVAS score [%], was estimated by using the Intraclass Correlation Coefficient (ICC3,1). Results were interpreted as ‘poor’ (ICC < 0.4), ‘fair to good’ (0.4–0.75), and ‘excellent’ (> 0.75). Agreement of each QA-SIVAS item was estimated using free-marginal kappa statistics by Brennan and Prediger [39], which minimizes prevalence-related biases. Interpretation of the results was carried out based on Landis and Koch (1977): k < 0 (‘poor’); k = 0.01–0.20 (‘slight’); k = 0.21–0.40 (‘fair’); k = 0.41–0.60 (‘moderate’); k = 0.61–0.80 (‘substantial’); k = 0.81–1.00 (‘almost perfect’).
Construct Validity
To evaluate construct validity, an approach similar to Jadad et al. [27] and Wilke et al. [47] was used. All 21 studies were assigned to two field-related experts, an orthopedist and sports physician (DD) and an exercise scientist and physiotherapist (IK). They independently rated each study’s quality with 1–4 points (1: poor; 2: poor to moderate; 3: moderate to good; 4: excellent). The mean ratings were correlated to the scores obtained with the QA-SIVAS scale (TG, LR, TH) using Kendall’s tau analysis.
Rating Time
Rating time was evaluated as the required mean time for the rating of one study. All three reviewers involved in the reliability study (TG, LR, TH) recorded the time (min:sec per study article) needed to evaluate the study quality for each article. Means were calculated for all three reviewers.
Statistical calculations were performed using SPSS version 27.0 (SPSS, Chicago, IL, USA). p-values < 0.05 were considered significant.
Results
The final QA-SIVAS scale consists of an 18-item checklist addressing the study design, data source, conduction, reporting, and discussion of VA studies in sports injury assessment. Each item is to be answered with either 0 (no/not stated) or 1 (yes/present) point. The maximum score is 18. The quality rating is expressed as a percentage value (reached score/maximum score [%]). Detailed information about the components and scoring guidelines is displayed in Table 1.
Table 1.
Items and scoring criteria of the QA-SIVAS scale
| No. | Item | When to score ‘yes ‘ | Purpose |
|---|---|---|---|
| 1 | Objective stated | The study’s aims OR hypotheses are clearly stated | To indicate the overarching purpose of the study |
| 2 | A representative sample was chosen |
The study considers a homogenous group of athletes with systematic registration of injuries; the number of injuries investigated and video recordings accessible is stated Example: Professional female football players (homogenous group of athletes) with 20 anterior cruciate ligament ruptures (systematic registration of injuries, number of injuries investigated), ten out of which were recorded on video (number of video recordings accessible) |
To ensure reliable data acquisition |
| 3 | Information about sample is included | Characteristics of the study population are included (at least age, sex, sport, performance level, and sample size are stated) | To support interpretation and differentiation of the results |
| 4 | Information about video source and quality of the footage are included | Source (e.g., television or private recording, video platform) AND quality of video footage are described (all of the following are described: sampling frequency, quality of resolution and number and type of camera views); if mixed datasets are used, minimum and maximum values of the features are reported | To enhance objectivity of the observations |
| 5 | Applied methods are described comprehensively | A clearly structured, detailed outline of the study protocol AND the process of video analysis is stated | To provide a basis for comparisons with similar studies |
| 6 | A systematic approach to video analysis was chosen | A systematic approach to video analysis is used (e.g., checklist, observation form) AND clearly defined observation criteria are used (e.g., definition of injury mechanism and/or pattern) | To enhance objectivity of the observations |
| 7 | Medical report information is included | Study included medical report information (e.g., confirmation of diagnosis, injury location, type, diagnosis) either directly (extraction from medical reports) or through communication with medical professionals | To support interpretation and differentiation of the results |
| 8 | Background/expertise of rater(s) is stated | Relevant occupation (e.g., physician, sports scientist, physiotherapist) AND experience (or training in video rating) of the video rater(s) in the specific domain are reported | To evaluate the expertise of the rater |
| 9 | Findings are observed by more than one researcher | It is clearly stated that two or more raters independently made the observations | To enhance reliability of the observations |
| 10 | A control group is included | A control group with similar situations and/or biomechanics not resulting in injury is included (e.g., landing with a straight leg) | To enable the derivation of causal relationships and to avoid misinterpretation of findings |
| 11 | A quantitative biomechanical analysis was conducted using validated methods | Quantitative descriptions of biomechanics are included (e.g., joint angles and/or kinematics) AND have been created using validated methods (validity and reliability of the methods is reported in the methods section) | To enhance understanding of the findings |
| 12 | The main results of the study are clearly described | Results are described with a clear structure AND figures or tables are included | To avoid misleading interpretation of results |
| 13 | Absolute numbers or proportions of injury cases (for each/the main outcome) are reported | Absolute numbers OR proportions (percentage) of injury cases are included, mechanisms (e.g., non-contact vs contact) and/or pattern (e.g., knee valgus pattern vs hyperextension pattern) are reported | To allow interpretations about the frequency of a finding |
| 14 | Details about the injury context are included | Information about the injury context/situation (e.g., player action, match or training injuries, time in game, hours of exposure during game/training) are included | To enhance understanding of the findings |
| 15 | Example screenshots/video frames are included | Example screenshots/video frames of the observed injury-specific outcomes of interest are included (e.g., injury mechanisms and/or pattern) | To overcome communication barriers and to communicate research with a broad readership |
| 16 | Findings are discussed within the context of the current evidence | Other relevant trials relating to the field of study are stated and discussed | To point out the studies' contribution to what was already known |
| 17 | Clinical/practical implications of the results are discussed | Information on how to use study findings in clinical/sports practice are discussed | To help the transfer of findings into practice |
| 18 | Limitations of the study are addressed | Weaknesses OR methodological shortcomings are reported | To avoid misinterpretation of findings and to identify the need for future studies |
Reliability
The analysis of raters’ agreement with regard to the total score (%) revealed an ICC of 0.98, interpreted as ‘excellent’ (95% confidence interval [CI] 0.96–0.99; p < 0.001). Repeated scoring showed excellent intra-rater reliability for all three raters: ICC rater 1 = 0.99 (95% CI 0.99–0.99; p < 0.001); ICC rater 2 = 0.99 (95% CI 0.98–0.99; p < 0.001), and ICC rater 3 = 0.99 (95% CI 0.98–0.99; p < 0.001).
Free marginal kappa values of the individual items ranged between 0.68 and 1.00 (substantial to almost perfect) with an exact agreement of 84–100% (Table 2).
Table 2.
Reliability and percent agreement of individual QA-SIVAS items
| No. | QA-SIVAS scale item | Base rate | Free-marginal kappa | Kappa (95% CI) | Percent exact agreement |
|---|---|---|---|---|---|
| 1 | Objective stated | 100 | 1.00 | 1.00–1.00 | 100 |
| 2 | A representative sample was chosen | 40 | 0.68 | 0.42–0.93 | 84 |
| 3 | Information about sample is included | 0 | 1.00 | 1.00–1.00 | 100 |
| 4 | Information about video source and quality of the footage are included | 13 | 0.68 | 0.43–0.93 | 84 |
| 5 | Applied methods are described comprehensively | 95 | 1.00 | 1.00–1.00 | 100 |
| 6 | A systematic approach to video analysis was chosen | 94 | 0.94 | 0.81–1.00 | 96 |
| 7 | Medical report information is included | 29 | 1.00 | 1.00–1.00 | 100 |
| 8 | Background/expertise of rater(s) is stated | 49 | 0.81 | 0.61–1.00 | 90 |
| 9 | Findings are observed by more than one researcher | 70 | 0.94 | 0.81–1.00 | 96 |
| 10 | A control group is included | 14 | 1.00 | 1.00–1.00 | 100 |
| 11 | A quantitative biomechanical analysis was conducted using validated methods | 13 | 0.86 | 0.67–1.00 | 92 |
| 12 | The main results of the study are clearly described | 95 | 0.87 | 0.70–1.00 | 93 |
| 13 | Absolute numbers or proportions of injury cases (for each/the main outcome) are reported | 95 | 0.87 | 0.70–1.00 | 93 |
| 14 | Details about the injury context are included | 92 | 0.94 | 0.81–1.00 | 96 |
| 15 | Example screenshots/video frames are included | 76 | 1.00 | 1.00–1.00 | 100 |
| 16 | Findings are discussed within the context of the current evidence | 100 | 1.00 | 1.00–1.00 | 100 |
| 17 | Clinical/practical implications of the results are discussed | 90 | 0.81 | 0.61–1.00 | 90 |
| 18 | Limitations of the study are addressed | 100 | 1.00 | 1.00–1.00 | 100 |
Base rate refers to the percentage of ratings that were answered with yes/present out of 63 ratings per scale item (21 studies, 3 reviewers)
Construct Validity
The analysis of construct validity with two experts in the field revealed a strong association of the results obtained by means of the QA-SIVAS scale and the expert ratings (Kendall’s tau B = 0.71, p < 0.001; see Table 3).
Table 3.
Ratings for the validity analysis made by two experts in the field (point scale: 1–4) and the corresponding QA-SIVAS scores (point scale: 0–18) for the included 21 studies
| Study | Expert 1 | Expert 2 | Mean | QA-SIVAS score (%) |
|---|---|---|---|---|
| Belcher et al. (2022) [4] | 3 | 3 | 3 | 12 (67) |
| Boden et al. (2000) [5] | 1 | 1 | 1 | 6 (33) |
| Boden et al. (2009) [6] | 2 | 2 | 2 | 9 (50) |
| Brophy et al. (2015) [7] | 2 | 2 | 2 | 11 (61) |
| Cochrane et al. (2007) [10] | 3 | 3 | 3 | 11 (61) |
| De Carli et al. (2022) [12] | 1 | 3 | 2 | 10 (56) |
| Della Villa et al. (2020) [13] | 4 | 4 | 4 | 14 (78) |
| Della Villa et al. (2021) [15] | 4 | 4 | 4 | 14 (78) |
| Grassi et al. (2017) [19] | 3 | 3 | 3 | 11 (61) |
| Grassi et al. (2020) [20] | 3 | 3 | 3 | 11 (61) |
| Johnston et al. (2018) [28] | 3 | 3 | 3 | 12 (67) |
| Koga et al. (2010) [30] | 3 | 4 | 3.5 | 12 (67) |
| Koga et al. (2017) [29] | 4 | 4 | 4 | 11 (61) |
| Krosshaug et al. (2007) [31] | 3 | 3 | 3 | 13 (72) |
| Lucarno et al. (2021) [32] | 4 | 4 | 4 | 14 (78) |
| Montgomery et al. (2018) [36] | 4 | 4 | 4 | 14 (78) |
| Olsen et al. (2004) [38] | 4 | 4 | 4 | 13 (72) |
| Rolley et al. (2023) [40] | 3 | 3 | 3 | 10 (56) |
| Sheehan et al. (2012) [44] | 2 | 3 | 2.5 | 10 (56) |
| Stuelcken et al. (2016) [45] | 3 | 3 | 3 | 13 (72) |
| Waldén et al. (2015) [46] | 4 | 4 | 4 | 15 (83) |
Rating Time
The mean rating time among all three reviewers was 10:07 ± 02:27 min:sec per article.
Discussion
A state-of-the-art method was applied to develop the QA-SIVAS scale. The tool covers 18 distinct items. Scores of each item can be used cumulatively for an overall judgment of a study’s quality. Inter- and intra-rater reliability, construct validity and user rating time were excellent. Consequently, the QA-SIVAS scale can be used by researchers for judging the quality of studies using video analysis of injuries in sports.
To our knowledge, QA-SIVAS is the first scale that addresses the quality of studies using video-based assessment of sports injuries. As no assessment instrument has been available hitherto, the scale was developed based on the consensus of an interdisciplinary multi-center reviewer team with field-specific knowledge. The final version was implemented in a systematic review covering 21 studies that have investigated ACL injuries in sports (PROSPERO registration: CRD42022337340).
The intra- and inter-rater reliability were excellent, indicating that the QA-SIVAS scale can be reliably used. This finding is comparable to the risk of bias scales from other medical fields. For instance, the inter-rater reliability of the PEDro scale, a commonly used tool in the assessment of clinical trials, ranges between 0.56 and 0.91 [18, 34]. The excellent inter-rater agreement of the QA-SIVAS scale is particularly notable given the multidisciplinary reviewer team of medical doctors, biomechanists, and sports scientists. Potentially, a background in sports injury research may be necessary, as this was a given prerequisite for all reviewers involved in the development of QA-SIVAS. However, the involvement of coaches and players in the research team has clear benefits, and is recommended [42]. Construct validity of the scale can be interpreted as high based on the correlation analysis revealing a Kendall’s tau B-value of 0.71. All assessments were done in a reasonable amount of time (average duration of around 10 min per article). This is comparable to other quality appraisal instruments and supports its feasibility [37, 47]. The rating time may be even less than 10 min if the raters know the studies beforehand (e.g., from performing a systematic literature search).
Our results from the evaluation process give some guidance on how to interpret QA-SIVAS. Most studies included through the systematic search on ACL injuries scored between 60 and 80%. No study achieved maximal scoring. Only a few studies scored < 60%. One study scored > 80%. However, there was only one item (item 3; Characteristics of the study population are included) that was not met by any of the included studies. Although no study has met the criteria of this item (by not reporting the age of the study population in the majority of studies), item 3 was still considered indispensable due to its clinical implication for injury prevention. It may thus be proposed to use the following interpretation when judging study quality: < 60%: low quality; 60–70%: moderate quality; 71–80%: good quality, 81–100%: high quality. Accordingly, five studies were of low quality, eight studies of moderate quality, seven studies of good quality, and one study of high quality.
For studies already completed, the QA-SIVAS scale may help to highlight methodological concerns. The QA-SIVAS scale can thus be used for assessing multiple studies that are included in a systematic review. High-quality systematic reviews are of great importance [41], and can support clinical decision making in sports [2]. However, shortcomings in the quality of included studies are of major concern. Quality assessment of studies is a challenging but indispensable task in order to draw valid conclusions based on the available evidence on a given topic [48]. QA-SIVAS can be used when conducting systematic reviews, and may also help researchers assess the quality of individual studies.
Although designed as an assessment tool, QA-SIVAS can also be a guidance for researchers. To date, only few recommendations on how to standardize VA have been published. These recommendations were specific to sports or injuries such as concussion, rugby or netball [11, 22, 33]. For example, in future VA research, QA-SIVAS may improve study design when used as a checklist in the planning of new studies [48]. By developing the QA-SIVAS scale, it was the firm intention of our group to extend the principles of evidence-based medicine into the field of video-based sports injury assessment. Future studies in the field should adhere to the QA-SIVAS criteria. In the planning of future studies, items 2 and 11 should be given special attention to allow for a homogenous and standardized methodological approach. When reporting study results, particular attention may be given to items 3, 4, and 8 of the QA-SIVAS scale. These data can easily be included when reporting study results. However, only a minority of the studies assessed fulfilled these items.
Strength and Limitations
To the best of our knowledge, the QA-SIVAS scale is the first specific tool to assess the quality of studies using VA of injuries in sports. It was developed and refined based on multiple rounds of consensus. However, reliability and validity testing was applied to anterior cruciate ligament ruptures without considering other injury mechanisms. Further, the independence of reviewers is not granted as some of the authors have previously worked together on research projects [8]. For this reason, it was a strategic goal to include multidisciplinary reviewers from multiple centers. Nevertheless, the practical implementation of QA-SIVAS is pending. As with other tools, the significance of QA-SIVAS will depend on feedback from the research community and updates may be required in future years.
Conclusion
We identified key domains and criteria for the evaluation and development of studies in the field of video-based assessment of sports injuries. By using multiple rounds of consensus and pilot testing, the QA-SIVAS scale was developed as a new instrument in the quality assessment of studies in this field. We have provided evidence that QA-SIVAS is reliable, valid, and can be easily adapted into sports research. Future studies in the field of video-based analysis of sports injuries should adhere to standardized methodological criteria and strict quality guidelines.
Declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no other funding related to this project.
Competing Interests
Authors declare that they have no conflict of interest relevant to the content of this article.
Availability of Data and Material
All data generated or analysed during this study are included in the published article.
Authors’ Contributions
TH, JW and TG: concept, planning, design. TG, TH, LR, KH, DF, SW, PM, JW, and TK: development of QA-SIVAS and interpretation of data. TG, LR and TH: reliability and rating time assessment. DD and IK: construct validity assessment. TH and TG: writing the first draft of the manuscript. TG, TH, LR, KH, DF, SW, PM, JW, DD, IK and TK: revision of the manuscript. All authors read and approved the final version of the manuscript.
References
- 1.Aiello F, Impellizzeri FM, Brown SJ, Serner A, McCall A. Injury-inciting activities in male and female football players: a systematic review. Sports Med. 2022 doi: 10.1007/s40279-022-01753-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ardern CL, Büttner F, Andrade R, Weir A, Ashe MC, Holden S, et al. Implementing the 27 PRISMA 2020 Statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: the PERSiST (implementing Prisma in Exercise, Rehabilitation, Sport medicine and SporTs science) guidance. Br J Sports Med. 2022;56:175–195. doi: 10.1136/bjsports-2021-103987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39:324–329. doi: 10.1136/bjsm.2005.018341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belcher S, Whatman C, Brughelli M. A systematic video analysis of 21 anterior cruciate ligament injuries in elite netball players during games. Sports Biomech. 2022 doi: 10.1080/14763141.2022.20349281-18. [DOI] [PubMed] [Google Scholar]
- 5.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Torg JS, Knowles SB, Hewett TE. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37:252–259. doi: 10.1177/0363546508328107. [DOI] [PubMed] [Google Scholar]
- 7.Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending puts the anterior cruciate ligament at risk during soccer: a gender-based analysis. Sports Health. 2015;7:244–249. doi: 10.1177/1941738114535184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buehn S, Mathes T, Prengel P, Wegewitz U, Ostermann T, Robens S, et al. The risk of bias in systematic reviews tool showed fair reliability and good construct validity. J Clin Epidemiol. 2017;91:121–128. doi: 10.1016/j.jclinepi.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cochrane JL, Lloyd DG, Buttfield A, Seward H, McGivern J. Characteristics of anterior cruciate ligament injuries in Australian football. J Sci Med Sport. 2007;10:96–104. doi: 10.1016/j.jsams.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Davis GA, Makdissi M, Bloomfield P, Clifton P, Echemendia RJ, Falvey ÉC, et al. International consensus definitions of video signs of concussion in professional sports. Br J Sports Med. 2019;53:1264–1267. doi: 10.1136/bjsports-2019-100628. [DOI] [PubMed] [Google Scholar]
- 12.De Carli A, Koverech G, Gaj E, Marzilli F, Fantoni F, Liberati Petrucci G, et al. Anterior cruciate ligament injury in elite football players: video analysis of 128 cases. J Sports Med Phys Fitness. 2022;62:222–228. doi: 10.23736/S0022-4707.21.11230-7. [DOI] [PubMed] [Google Scholar]
- 13.Della Villa F, Buckthorpe M, Grassi A, Nabiuzzi A, Tosarelli F, Zaffagnini S, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med. 2020;54:1423–1432. doi: 10.1136/bjsports-2019-101247. [DOI] [PubMed] [Google Scholar]
- 14.Della Villa F, Buckthorpe M, Tosarelli F, Zago M, Zaffagnini S, Grassi A. Video analysis of Achilles tendon rupture in male professional football (soccer) players: injury mechanisms, patterns and biomechanics. BMJ Open Sport Exerc Med. 2022;8:e001419. doi: 10.1136/bmjsem-2022-001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Della Villa F, Tosarelli F, Ferrari R, Grassi A, Ciampone L, Nanni G, et al. Systematic video analysis of anterior cruciate ligament injuries in professional male rugby players: pattern, injury mechanism, and biomechanics in 57 consecutive cases. Orthop J Sports Med. 2021;9:23259671211048182. doi: 10.1177/23259671211048182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Engebretsen L, Soligard T, Steffen K, Alonso J, Aubry M, Budgett R, et al. Sport injuries and illnesses during the London Summer Olympic Games 2012. Br J Sports Med. 2013;47:407–414. doi: 10.1136/bjsports-2013-092380. [DOI] [PubMed] [Google Scholar]
- 17.Filbay SR, Skou ST, Bullock GS, Le CY, Räisänen AM, Toomey C, et al. Long-term quality of life, work limitation, physical activity, economic cost and disease burden following ACL and meniscal injury: a systematic review and meta-analysis for the OPTIKNEE consensus. Br J Sports Med. 2022 doi: 10.1136/bjsports-2022-105626. [DOI] [PubMed] [Google Scholar]
- 18.Foley NC, Bhogal SK, Teasell RW, Bureau Y, Speechley MR. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther. 2006;86:817–824. doi: 10.1093/ptj/86.6.817. [DOI] [PubMed] [Google Scholar]
- 19.Grassi A, Smiley SP, Roberti di Sarsina T, Signorelli C, Marcheggiani Muccioli GM, Bondi A, et al. Mechanisms and situations of anterior cruciate ligament injuries in professional male soccer players: a YouTube-based video analysis. Eur J Orthop Surg Traumatol. 2017;27:967–981. doi: 10.1007/s00590-017-1905-0. [DOI] [PubMed] [Google Scholar]
- 20.Grassi A, Tosarelli F, Agostinone P, Macchiarola L, Zaffagnini S, Della Villa F. Rapid posterior tibial reduction after noncontact anterior cruciate ligament rupture: mechanism description from a video analysis. Sports Health. 2020;12:462–469. doi: 10.1177/1941738120936673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gronwald T, Klein C, Hoenig T, Pietzonka M, Bloch H, Edouard P, et al. Hamstring injury patterns in professional male football (soccer): a systematic video analysis of 52 cases. Br J Sports Med. 2022;56:165–171. doi: 10.1136/bjsports-2021-104769. [DOI] [PubMed] [Google Scholar]
- 22.Hendricks S, Till K, den Hollander S, Savage TN, Roberts SP, Tierney G, et al. Consensus on a video analysis framework of descriptors and definitions by the Rugby Union Video Analysis Consensus group. Br J Sports Med. 2020;54:566–572. doi: 10.1136/bjsports-2019-101293. [DOI] [PubMed] [Google Scholar]
- 23.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoenig T, Ackerman KE, Beck BR, Bouxsein ML, Burr DB, Hollander K, et al. Bone stress injuries. Nat Rev Dis Primers. 2022;8:26. doi: 10.1038/s41572-022-00352-y. [DOI] [PubMed] [Google Scholar]
- 25.Hoenig T, Edouard P, Krause M, Malhan D, Relógio A, Junge A, et al. Analysis of more than 20,000 injuries in European professional football by using a citizen science-based approach: an opportunity for epidemiological research? J Sci Med Sport. 2022;25:300–305. doi: 10.1016/j.jsams.2021.11.038. [DOI] [PubMed] [Google Scholar]
- 26.Hoenig T, Gronwald T, Hollander K, Klein C, Frosch K-H, Ueblacker P, et al. Situational and biomechanical patterns of Achilles tendon ruptures in professional male football: a systematic video analysis of 80 cases. Knee Surg Sports Traumatol Arthrosc. 2023;31:2236–2245. doi: 10.1007/s00167-023-07384-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 28.Johnston JT, Mandelbaum BR, Schub D, Rodeo SA, Matava MJ, Silvers-Granelli HJ, et al. Video analysis of anterior cruciate ligament tears in professional American football athletes. Am J Sports Med. 2018;46:862–868. doi: 10.1177/0363546518756328. [DOI] [PubMed] [Google Scholar]
- 29.Koga H, Nakamae A, Shima Y, Bahr R, Krosshaug T. Hip and ankle kinematics in noncontact anterior cruciate ligament injury situations: video analysis using model-based image matching. Am J Sports Med. 2018;46:333–340. doi: 10.1177/0363546517732750. [DOI] [PubMed] [Google Scholar]
- 30.Koga H, Nakamae A, Shima Y, Iwasa J, Myklebust G, Engebretsen L, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38:2218–2225. doi: 10.1177/0363546510373570. [DOI] [PubMed] [Google Scholar]
- 31.Krosshaug T, Nakamae A, Boden BP, Engebretsen L, Smith G, Slauterbeck JR, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359–367. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 32.Lucarno S, Zago M, Buckthorpe M, Grassi A, Tosarelli F, Smith R, et al. Systematic video analysis of anterior cruciate ligament injuries in professional female soccer players. Am J Sports Med. 2021;49:1794–1802. doi: 10.1177/03635465211008169. [DOI] [PubMed] [Google Scholar]
- 33.Mackay L, Jones B, Janse van Rensburg DCC, Hall F, Alexander L, Atkinson K, et al. Consensus on a netball video analysis framework of descriptors and definitions by the netball video analysis consensus group. Br J Sports Med. 2023;57:441–449. doi: 10.1136/bjsports-2022-106187. [DOI] [PubMed] [Google Scholar]
- 34.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. doi: 10.1093/ptj/83.8.713. [DOI] [PubMed] [Google Scholar]
- 35.Millar NL, Silbernagel KG, Thorborg K, Kirwan PD, Galatz LM, Abrams GD, et al. Tendinopathy Nat Rev Dis Primers. 2021;7:1–21. doi: 10.1038/s41572-020-00234-1. [DOI] [PubMed] [Google Scholar]
- 36.Montgomery C, Blackburn J, Withers D, Tierney G, Moran C, Simms C. Mechanisms of ACL injury in professional rugby union: a systematic video analysis of 36 cases. Br J Sports Med. 2018;52:994–1001. doi: 10.1136/bjsports-2016-096425. [DOI] [PubMed] [Google Scholar]
- 37.Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ. Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther. 2008;88:156–175. doi: 10.2522/ptj.20070147. [DOI] [PubMed] [Google Scholar]
- 38.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 39.Randolph JJ. Free-marginal multirater kappa: an alternative to Fleiss’ fixed marginal multirater kappa. Joensuu Learning and Instruction Symposium, Joensuu, Finland; 2005.
- 40.Rolley TL, Saunders N, Bonacci J, Keast M, Fox AS. Video analysis of anterior cruciate ligament injury situations in the women's Australian football league. Sci Med Footb. 2023;7:106–123. doi: 10.1080/24733938.2022.2076897. [DOI] [PubMed] [Google Scholar]
- 41.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sacristán JA, Aguarón A, Avendaño-Solá C, Garrido P, Carrión J, Gutiérrez A, et al. Patient involvement in clinical research: why, when, and how. Patient Prefer Adherence. 2016;10:631. doi: 10.2147/PPA.S104259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Serner A, Mosler AB, Tol JL, Bahr R, Weir A. Mechanisms of acute adductor longus injuries in male football players: a systematic visual video analysis. Br J Sports Med. 2019;53:158–164. doi: 10.1136/bjsports-2018-099246. [DOI] [PubMed] [Google Scholar]
- 44.Sheehan FT, Sipprell WH, 3rd, Boden BP. Dynamic sagittal plane trunk control during anterior cruciate ligament injury. Am J Sports Med. 2012;40:1068–1074. doi: 10.1177/0363546512437850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stuelcken MC, Mellifont DB, Gorman AD, Sayers MG. Mechanisms of anterior cruciate ligament injuries in elite women's netball: a systematic video analysis. J Sports Sci. 2016;34:1516–1522. doi: 10.1080/02640414.2015.1121285. [DOI] [PubMed] [Google Scholar]
- 46.Waldén M, Krosshaug T, Bjørneboe J, Andersen TE, Faul O, Hägglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Br J Sports Med. 2015;49:1452–1460. doi: 10.1136/bjsports-2014-094573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilke J, Krause F, Niederer D, Engeroff T, Nürnberger F, Vogt L, et al. Appraising the methodological quality of cadaveric studies: validation of the QUACS scale. J Anat. 2015;226:440–446. doi: 10.1111/joa.12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8:2–10. doi: 10.1111/jebm.12141. [DOI] [PubMed] [Google Scholar]