Abstract
Background:
Impulsivity is viewed as key to attention-deficit/hyperactivity disorder (ADHD) and disruptive behavior disorders (DBD). Yet, to date, no work has provided an item-level analysis in longitudinal samples across the critical developmental period from childhood into adolescence, despite prior work suggesting items exhibit differential relevance with respect to various types of impairment. The current study conducted a novel longitudinal network analysis of ADHD and oppositional defiant disorder (ODD) symptoms between childhood and adolescence with important applied prediction of social skills in adolescence.
Methods:
Participants were 310 children over-recruited for clinical ADHD issues followed longitudinally for six years in total with gold standard diagnostic procedures and parent and teacher ratings of symptoms and social outcomes.
Results:
Findings from baseline, Year 3, and Year 6 suggested Difficulty waiting turn, Blurts, and Interrupts/intrudes were key bridge items across cross-sectional and longitudinal parent-reported DBD networks. Further, shortened symptom lists incorporating these symptoms were stronger predictors of teacher-rated social skills five years later compared to total DBD scores.
Conclusions:
Such findings are consistent with the trait impulsivity theory of DBD and ADHD and may inform useful screening tools and personalized intervention targets for children at risk for DBD during adolescence.
Keywords: ADHD, Oppositional Defiant Disorder, Longitudinal Studies, Impulsivity, Developmental Psychopathology
Attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) are commonly occurring disorders that are seen in approximately 5–10% of children and adolescents (Ghandour et al., 2019; Faraone et al., 2021). Comorbidity rates between these two disorders range from 40% to 60% (Biederman et al., 2007; Elia, Ambrosini, & Berrettini, 2008). ADHD is characterized by symptoms across two domains, inattentive and hyperactive/impulsive symptoms, while ODD is characterized by symptoms across three domains, argumentative/defiant behavior, angry/irritable mood, and a vindictive disposition (American Psychiatric Association, 2013). ADHD and ODD are each associated with a host of difficulties in virtually all areas of functioning including impaired interpersonal relationships, academic achievement, overall quality of life (Bauermeister et al., 2007; Staikova, Gomes, Tartter, McCabe, & Halperin, 2013; Wehmeier, Schact, & Barkley, 2010), and predict later psychological problems (e.g., antisocial behavior, mood problems; Stringaris & Goodman, 2009a, 2009b). There is a significant degree of heterogeneity in the presentation of ADHD and ODD, particularly at the symptom level (e.g., number and combination of symptoms; Luo, Weibman, Halperin, & Li, 2019). This heterogeneity complicates our understanding of how ADHD and ODD relate to one another and to negative life outcomes, particularly from childhood to adolescence. Using longitudinal symptom level analysis, the current study aims to identify the specific symptoms that explain the ADHD-ODD association and explore whether these specific symptoms contribute to relevant life outcomes. This could help identify aspects of these disorders that underlie their comorbidity, aid in transdiagnostic screening practices that predict the onset of ODD in children with ADHD (and vice versa), and specify potential assessment targets whose presence increases risk for clinically relevant outcomes.
ADHD and ODD are each associated with diverse negative outcomes, with social impairment being one particular area of dysfunction that characterizes both disorders. Prior research has suggested that both ADHD and ODD are uniquely associated with social functioning deficits (e.g., Frankel & Feinberg, 2002), and their combination leads to even greater social impairment (Antshel & Rerner, 2003). Other research has also highlighted the importance of understanding the precursors of social dysfunction, given that such issues had been found to predict current and future academic underachievement, elevated risk for comorbid psychopathology, delinquency, and criminal behavior (e.g., Lee, Lahey, Owens, & Hinshaw, 2008; Mrug et al., 2012). As such, the clarification of such precursors, including specific symptoms of childhood ADHD and ODD, represents a key aim for intervention efforts. Identifying the specific subset of these symptoms that uniquely predict future social impairments, in addition to comorbidity, could help tailor assessment and intervention approaches, in turn mitigating negative long-term outcomes for this population of youth.
Support for Impulsivity as a Bridge Between ADHD and ODD
One element of both ADHD and ODD that may play a key role in their comorbidity and relationship with social impairment is impulsivity, which has been found to play a key role in the etiology of both disorders (Beauchaine, Zisner, & Sauder, 2017) and social impairment (Barkley, 1997). These findings have been seen in cross-sectional studies that used samples ranging from preschool through young adulthood (Martel, Gremillion, Roberts, von Eye, & Nigg, 2010; Martel, Levinson, Langer, & Nigg, 2016; Martel, Levinson, Lee, & Smith, 2017) and in longitudinal work where hyperactive/impulsive ADHD symptoms, together, predict ODD behaviors (Ahmad & Hinshaw, 2017; Bell et al., 2022; Burns & Walsh, 2002). One neurobiological theory underlying such findings is that delays in cortical maturation that characterize ADHD and associated DBD (e.g., ODD) contribute to increased levels of impulsivity particularly in adolescence (Nigg & Casey, 2005; Shaw et al., 2007). This transdiagnsotic susceptibility to impulsive (or approach) behaviors, particularly in response to negative affect (e.g., anger), can lead adolescents to engage in risky peer interactions, which become increasingly prominent during adolescence, and a host of related risky behaviors (e.g., substance use, criminal behavior; Beauchaine et al., 2017).
The role of impulsivity in explaining the association between ADHD and ODD appears to have much support. However, to date, virtually all existing work has examined ADHD and ODD as composite scores, despite a growing body of evidence suggesting heterogeneity at the symptom level with respect to prediction of relevant outcomes (e.g., Goh, Martel, & Barkley, 2020; Goh et al., 2021; Martel et al., 2021). These latter studies also suggest that focusing on key symptoms allows for a more parsimonious assessment and could improve prediction, as weighted algorithms of core symptoms performed equally or better than those encompassing all symptoms in predicting relevant outcomes (e.g., functional impairment). Given these findings, along with the high prevalence of ADHD-ODD comorbidity, identifying core symptoms is crucial for understanding the association between ADHD and ODD, and the relationship between these disorders and specific areas of impairment.
Network Conceptualizations of Psychopathology and Comorbidity
One method that has shown to be especially useful in examining symptom level associations between constructs is network analysis. Over the past several years, network analysis has been used to model various childhood psychological disorders, including ADHD (Goh, Martel, et al., 2020; Goh et al., 2021; Martel et al., 2016, 2017) and ODD (Smith, Lee, & Martel, & Axelrad, 2017). The network theory posits that disorders are the product of causal relationships among symptoms, and how the associations between symptoms underlie the manifestation of various psychological disorders (Borsboom & Cramer, 2013). This analytic approach complements other statistical methods, such as latent variable models (for a full review on the similarities and differences between network and latent variable models, see Bringmann & Eronen, 2018).
Prior work has examined symptom level relations between ADHD and ODD, highlighting the pivotal role of impulsivity (e.g., Martel, Levinson, Lee, & Smith, 2017). Yet, there are limitations with the current network literature. Perhaps the most salient is the fact that most prior network findings are based upon cross-sectional data, which prevent inferences regarding causal relations between symptoms over time (i.e., Granger-causal relations). Dynamic modeling (i.e., longitudinal) approaches have been proposed to explore longitudinal, causal relations at the symptom level, which reflect the interactions between symptoms that evolve and change over time, a core notion of the network theory (Bringmann & Eronen, 2018). Examining symptom level relations between ADHD and ODD longitudinally is necessary for a few reasons. First, as aforementioned, ADHD and ODD present with significant heterogeneity, including at the symptom level (e.g., Lindhiem et al., 2015; Luo et al., 2019). Second, theoretical and empirical work demonstrate that ADHD precedes ODD (e.g., developmental precursor model; for review, see Harvey, Breaux, & Lugo-Candelas, 2016), necessitating a longitudinal design to test temporal relations between ADHD and ODD.
A second limitation is the fact that few, if any, network studies have examined whether specific symptoms of a construct are related relevant outcomes. For instance, Martel et al., (2021) found that a sum score comprised of four ADHD symptoms showed similar ability in predicting later mental health difficulties as compared to all 18 ADHD symptoms. These four symptoms may serve as screening items for ADHD and later mental health difficulties. Additional work is needed to determine whether specific subgroups of symptoms show predictive ability with relevant outcomes. Given the impact that ADHD and ODD have upon social functioning deficits, it is imperative to identify the subset of symptoms (known as “bridge symptoms”) that not only explain the ADHD-ODD relation, but also predict later social functioning. Identifying these bridge symptoms may translate to better designed interventions, where bridge symptoms are targeted and mitigate long-term negative outcomes, whereas attempting to treat broad syndromes may be contributing to limited treatment efficacy for certain disorders, such as ADHD (e.g., Chacko, Kofler, & Jarrett, 2014).
The Current Study
The current study used dynamic network modeling across a six-year period spanning from childhood to adolescence. The first goal of the study was to investigate the bridge symptoms that explained the comorbidity between ADHD and ODD. Based upon prior theoretical and empirical work emphasizing the role of impulsivity within the development of ADHD and ODD, it was hypothesized that impulsivity symptoms would serve as bridge symptoms and explain the association between ADHD and ODD within cross-sectional and longitudinal networks models. The second goal of the study was to determine whether these bridge symptoms would demonstrate unique ability in predicting later relevant outcomes as compared to a comprehensive group of symptoms. It was hypothesized that the bridge impulsivity symptoms, as identified in the network analyses, would show greater predictive utility relative to non-bridge symptoms in predicting longitudinal outcomes related to social skills rated by parents and teachers. Given the dearth of literature surrounding this goal, this hypothesis was considered preliminary.
Methods
Participants
Ethics approval was obtained from the Institutional Review Board at Oregon Health & Science University. Participants were drawn from the Oregon ADHD Cohort, a well-characterized child cohort over-recruited for attention and impulsivity-related behaviors reflective of ADHD. The community-based recruitment and enrollment procedures, along with the multi-informant diagnostic assessment procedures for ADHD, have been published in greater detail elsewhere (Goh, Martel, et al., 2020; Karalunas et al., 2017; Musser, Karalunas, Dieckmann, Peris, & Nigg, 2016). A parent/legal guardian provided written informed consent and children provided written assent. Data for the current study were drawn from more than 800 children who were followed annually across a six-year period spanning from middle childhood to adolescence (6–13 years in Year 1, 9–15 years in Year 3, and 11–18 years in Year 6). Ages across years overlapped to maximize statistical power. The current study examined data from a subset of 310 youth (M age = 8.96, SD = 1.42) who had complete data across Years 1, 3, and 6. This subset of youth were included in the current analyses because they all had complete teacher data at Year 1 and complete parent data at Year 6. Missing data can lead to biases in network results (Krause, Huisman, Steglich, & Snijders, 2018). Therefore, listwise deletion methods were used in the current study as they are one of the most common methods in dealing with missing data for network analysis (Kim, Kwon, Ha, Lim, & Kim, 2021).
Of the 310 youth, 199 (64.2%) were biological males and 247 (80%) identified as white and non-Hispanic. The average reported family income was approximately $75,000. Of the 310 youth, 168 (54.2%) met diagnostic criteria for ADHD, with an additional nine (2.9%) considered as subthreshold ADHD; the remainder of the sample did not meet ADHD diagnostic criteria. This sample captured the full range of ADHD symptoms and is consistent with prior research suggesting ADHD may be best described as falling on a continuum (Marcus & Barry, 2011). Similar diagnostic rates for ADHD were observed at the follow-up visits, with 141 (45.5%) and 120 (38.7%) participants meeting criteria at Years 3 and 6, respectively. Thirty-eight youth (12%) met diagnostic criteria for ODD at Year 1, with 22 (7.1%) and 18 (5.8%) meeting ODD criteria at Years 3 and 6, respectively. Additional diagnoses included 47 youth (15.2%) who met criteria for an anxiety disorder, nine (2.9%) who met criteria for a learning disorder, and three (1.0%) who met criteria for a mood disorder.
Few differences were seen between youth in the larger dataset who were versus were not included in the current study, although Hedge’s g effect sizes indicated generally small mean differences. Relative to youth who were included in analyses, youth who were excluded from analyses were older at Year 1 (p < .01, g = .50), showed higher rates of ADHD diagnoses (p < .01, g = .20), and had higher family income (p = .02, g = .17). However, no differences were observed on diagnostic status at the remaining follow-up points (i.e., ADHD at Years 3 and 6; ODD at Years 1, 3, 6; ps > .05; gs: −.09 to .15).
Sample Characterization
Recruitment
Volunteers were recruited via mass mailings, using commercial mailing lists, to all families with children in the target age range within the geographic radius of 50 miles from the University. The mailing made clear that we were looking for children with possible or definite ADHD, and for typically developing children with no history of learning or attention problems. In response to mailings to parents of all children in the target age range in our catchment area, we received 2,144 inquiries (a response rate of about 1% for participants without ADHD and about 30% for participants with ADHD).
First Screen
An initial screening phone call served to establish eligibility (below) and interest. Nearly half were ruled out at this stage due to medications, other illnesses (e.g., autism), or lack of interest. Those who were excluded at this stage did not differ reliably from the final sample on sex ratio (p = .11) or non-white race (p = .22) but were marginally lower on income (p = .06) and were marginally younger (p = .06).
Second Screen
Remaining participants (n = 1,449) underwent an in-person “diagnostic” visit. Parent(s) completed the Conners’ Rating Scales-3rd Edition short form, Strengths and Difficulties Questionnaire (SDQ) long form including the impairment module, the ADHD Rating Scale (ADHD-RS), and the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS; Puig-Antich & Ryan, 1986), a semi-structured clinical interview administered by a Master’s-level clinician. Children completed a brief unstructured clinical interview with the same clinician; then, with a psychometrician (BA-level staff or volunteer), children completed a three-subtest short form of the WISC-IV (i.e., Vocabulary, Block Design, and Information tasks), selected subtests on the WIAT-II (i.e., Word Reading and Numerical Operations) to estimate IQ and academic progress. Interviewers and testers wrote detailed observational notes. Teachers were contacted and completed the Conners’-3, SDQ, and ADHD-RS. All clinical interviewers were trained to reliability of κ > .80 with a master interviewer for all diagnoses seen at ≥ 5% base rate in this sample on the KSADS and had videotapes viewed by a supervisor and reviewed periodically to prevent procedural drift. Psychometric testers were trained to an accuracy standard prior to beginning work and had videotapes viewed periodically to prevent drift.
Exclusions
Children were excluded at baseline if (1) they were taking non-stimulant psychotropic medications or (2) had a parent reported history of: non-febrile seizure, head injury with loss of consciousness > 60 seconds, diagnosis of autism spectrum disorder or intellectual disability, or other major medical conditions. After the diagnostic team visit (Step 2), 103 (7.1%) children withdrew due to lack of further interest (e.g., only wanted the diagnostic screen), and 496 children were ruled out for the following reasons: excess teacher-parent rating discrepancy (situational problems; n = 173, 35%); subthreshold symptom count (not control or ADHD, n = 84, 17%); psychosis, mania, current severe depressive episode, Tourette’s syndrome, or head injury (n = 49, 10%); autism (n = 35, 7%); other health condition (n = 35, 7%); ineligible medication (n = 10, 2%); IQ < 80 (n = 1, .2%), or multiple rule outs (n = 387, 22.0%). Among the eligible children with ADHD, 35% (n = 59) were prescribed stimulant medications and needed to complete the washout, only slightly lower than rates in community surveys for pre-adolescent children.
“Gold Standard” Diagnostic Assignment Using a Best Estimate Procedure
All materials were scored and presented to a clinical diagnostic team composed of a board-certified child psychiatrist with over 25 years of experience and a licensed child neuropsychologist with over 10 years of experience. Masked to one another’s ratings and to the subsequent genetic or cognitive test scores, they formed a diagnostic opinion based on all available information. Their agreement rate for all diagnoses discussed in this paper was satisfactory (ADHD, κ = .88; ADHD subtype, κ > .80; ODD κ > .68; all other disorders with at least 5% base rate, κs > .68). Disagreements were conferenced and consensus reached. Cases where consensus was not readily achieved for ADHD diagnosis were excluded.
Using a best estimate procedure, DSM-IV diagnoses were made independently by each clinician using the “OR” algorithm (e.g., symptom is considered present if at least one rater endorses that symptom; Martel et al., 2021). Importantly, the “OR” algorithm was only used when the following conditions were satisfied: (1) t-scores ≥ 60 on an ADHD scale based upon both parent and teacher ratings and (2) both parents and teachers rated at least three symptoms as occurring “often” or “very often” on the ADHD-RS (parents could also have endorsed a symptom as present on the K-SADS). In situations where these conditions were not met by either informant (e.g., low t-scores, fewer than 3 symptoms endorsed), and clinicians determined that the low scores could not be explained by successful medication treatment during the school day, then the case was rejected as failing to meet the DSM-IV required criteria for ADHD (i.e., substantial symptoms present in more than one setting). In addition, it was required that all other DSM-IV criteria were met (i.e., impairment; onset of symptoms prior to age seven; sustained impairment > 1 year; symptoms not accounted for by other conditions/disorders). Both current and lifetime diagnoses were assigned; for the present report, all children in the ADHD group met current and lifetime diagnosis for ADHD, meaning that symptoms were always present and did not emerge at a particular developmental point (i.e., trait like).
Measures
DBD Symptoms
Parent-reported symptoms of ADHD (18 items) and ODD (8 items) were obtained from the KSADS (Puig-Antich & Ryan, 1986) where responses ranged from 1 (“no”) to 3 (“yes”) with 2 representing subthreshold. Teacher-reported symptoms were obtained from the ADHD-RS (DuPaul, Power, Anastopoulos, & Reid, 1998). Teachers responded to all 18 ADHD items and 8 ODD items on a 0 (“rarely or never”) to 3 (“always or very often”) scale. Items on the ADHD-RS are consistent with DSM-5 criteria. Reliability for ADHD and ODD for both parent- and teacher-report was high with alphas of .85 or above at all waves.
Social Skills
Parents and teachers reported on child social skills using the Social Skills Improvement System (SSIS) Rating Scale (Gresham & Elliot, 2008). The SSIS evaluated social skills, problematic behaviors, and academic competence on a four-point scale ranging from “not true” to “very true” across 84 items. For the current study, these 84 items were summed to create a total score, a method that allowed for the most parsimonious summary of social functioning as noted in in prior work (Gresham, Elliot, Vance, et al., 2011). Internal consistency for this total score at Year 6 was good across parent (α = .89) and teacher-report (α = .93).
Data Analytic Plan
Network Construction
The current analyses were not preregistered and should be considered exploratory. The R packages bootnet and qgraph were used to construct the Gaussian Graphical Models (GGM) which evaluated the relations amongst the ADHD and ODD symptom items (Epskamp, & Borsboom, 2018; Epskamp, Cramer, Waldorp, Schmittman, & Borsboom, 2012). Network estimation was done using the graphical least absolute shrinkage and selection operator (GLASSO; Friedman, Hastie, & Tibshirani, 2008) with extended Bayesian Information Criterion (EBIC; Foygel & Drton, 2010). These estimation procedures result in sparser network models, where only the strongest partial Spearman correlations are retained. A gamma (γ) hyperparameter of 0.5 was selected for the EBIC to maximize specificity of relations within networks (Epskamp & Fried, 2018). Visualization of network results were done using Multidimensional Scaling (MDS) techniques, which facilitate more interpretable visualizations of networks (i.e., more central nodes are placed more centrally) relative to the more commonly used Fruchterman-Reingold networks (Fruchterman & Reingold, 1991). The MDS networks were created using the R package networktools (Jones, 2018). Next, community detection analyses were done using the spinglass algorithm (Reichardt & Bornholdt, 2006) using igraph (Csardi & Nepusz, 2006). These analyses identified whether network items clustered together in a particular manner (e.g., if hyperactivity/impulsivity items clustered together). Items that shared the same output value were part of the same “community.” Several networks were created. First, three separate cross-sectional networks were created using parent-reported data at Years 1, 3, and 6. Then, a single network using teacher-reported data was constructed using only Year 1 data. This was done due to attrition seen in teacher-reported data at the longitudinal follow-up visits.
Bridge Symptoms
Bridge Expected Influence (BEI; i.e., sum of the partial correlations attached to an element from elements of different communities while accounting for the presence of negative correlations) identified bridge symptoms in each network (Jones, Ma, & McNally, 2019). In the current study, BEI assessed an element’s influence with its immediate neighbors in another community (Robinaugh, Millner, & McNally, 2016). Therefore, in the current study, BEI was used to examine the relations between ADHD and ODD symptom items. Like prior work (Goh et al., 2020), higher BEI values (i.e., BEI values ≥ 1) indicated that a given item exhibited stronger unique relations with symptoms in the remaining communities. These symptoms were identified through an adjacency matrix of partial correlations that are further penalized to prevent spurious findings (i.e., regularized correlations).
Network Comparison Tests
Network structure comparisons were conducted using the R package NetworkComparisonTest (van Borkulo et al., 2017). Two comparison indices were used (a) network structure invariance, which assesses the similarity in overall network structure between networks by evaluating whether the largest individual edge strength difference between two networks is significant and (b) global strength invariance, which determines the overall connectivity of edges (or, the sum of all absolute partial correlations) between networks (van Borkulo et al., 2017). Several comparison tests were conducted. First, tests were done to compare the network structure of the parent-reported networks across Years 1, 3, and 6. Then, an additional comparison test was done to compare the network structure of the Year 1 parent-reported network to the Year 1 teacher-reported network.
Longitudinal Network Analysis
A graphical vector-autoregression model was estimated from the Years 1, 3, and 6 ADHD and ODD panel data using the psychonetrics package (Version 0.9; Epskamp, 2021) with maximum likelihood estimation given the completeness of the data. In this multilevel model, between-person (Level-2) effects representing average differences between participants across all waves are disaggregated from within-person (Level-1) effects representing how deviations in each variable from each participants’ personal average predict subsequent changes in other variables, and random effects are estimated based on the variables’ mean structure. We focused on the longitudinal within-person model and used the networktools package to calculate BEI and out-expected influence. In longitudinal models, BEI is defined as the sum of the edges representing within-person deviations predicting subsequent changes extending both from a target symptom to symptoms of different communities and from symptoms of different communities to a target symptom. Out-expected influence, by contrast, is defined as only the sum of the edges representing within-person deviations in the target symptom predicting subsequent changes in symptoms from different communities. To facilitate comparisons among symptoms, all BEI and out-expected influence metrics were z-scored.
Applied Tests
Lastly, hierarchical linear regressions were used to evaluate whether the bridge symptoms, identified from the cross-sectional and longitudinal networks, measured at baseline demonstrated applied value in predicting future impairments in social skills. The top four parent-rated bridge symptoms from the cross-sectional networks and the top six parent-rated influential symptoms from the longitudinal network were summed. The remaining parent-rated ADHD and ODD symptoms were also summed together. These composite scores were obtained from the Year 1 network results and served as the model predictors. Social skills functioning at Year 6, as measured by the SSIS, was used as the longitudinal outcome variable. The combined use of use of parent and teacher data was done to reduce shared method variance.
Results
Parent-Reported ADHD and ODD Symptom Networks
Across the three resulting cross-sectional networks, the spinglass algorithm, in general, suggested three communities of symptoms that fell in line with ADHD-inattentive, ADHD-hyperactive/impulsive, and ODD symptom domains (see Supplemental Material for these cross-sectional network figures). Preliminary stability analyses suggested edges within each network were generally robust, with the strength of several edges being significantly different from zero (figures available upon request). Further, given the use of regularization techniques applied to the partial correlations, values in parentheses in the following sections represent partial correlations that are significantly different from zero (Epskamp & Fried, 2018).
Bridge Symptoms
Bridge centrality stability coefficients were above the recommended .25 cut-off value (Year 1 = .52, Year 3 = .36, Year 6 = .44; Epskamp et al., 2018). Across networks including parent-reported symptoms, assessment of BEI (Figure 1) revealed the ADHD symptom of Unable to engage in activities quietly (H4) as the primary bridge symptom that demonstrated robust relations with ODD symptoms at Year 1, specifically, Argues with adults (ODD2; .07) and Angry/resentful (ODD7; .06) and secondarily with Often loses temper (ODD1) and Disobeys rules (ODD3; both .03). Other important bridge items at Year 1 included Blurts and Difficulty Waiting Turn.
Figure 1.
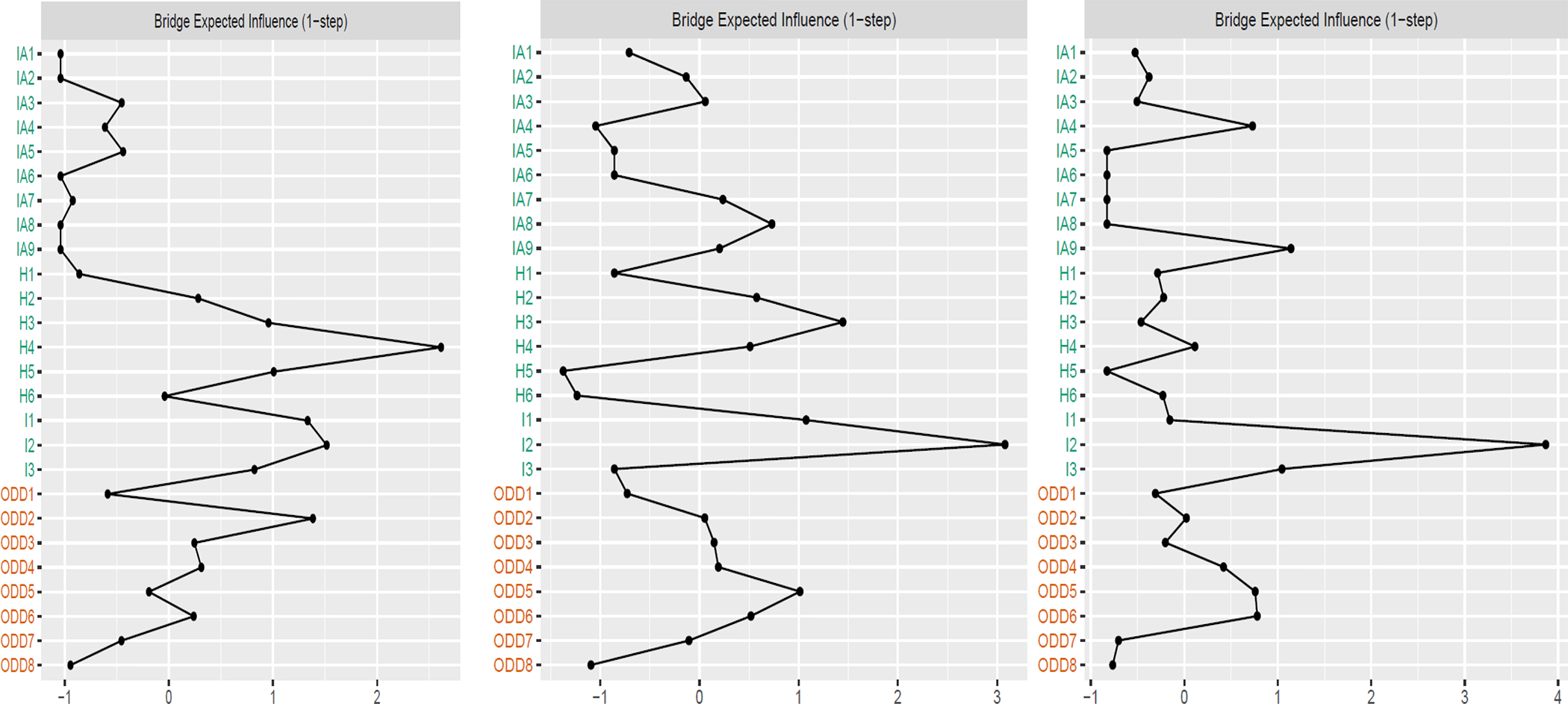
Bridge Expected Influence Results for ADHD and ODD Cross-Sectional, Parent-Reported Data for Year 1 (Left panel), Year 3 (Middle panel), and Year 6 (Right panel). IA1: careless mistakes; IA2: diff. sustaining attention; IA3: daydreams; IA4: diff. following instructions; IA5: diff. organizing; IA6: diff. sustaining mental effort; IA7: loses things; IA8: easily distracted; IA9: forgetful; H1: fidgets; H2: diff. remaining seated; H3: restless; H4: diff. playing quietly; H5: on the go; H6: talks excessively; I1: blurts; I2: diff. waiting turn; I3: interrupts; ODD1: loses temper; ODD2: argues; ODD3: disobeys rules; ODD4: deliberately annoys; ODD5: blames others; ODD6: easy to annoy; ODD7: angry/resentful; ODD8: spiteful/vindictive.
Conversely, the ADHD symptom Difficulty waiting turn (I2) emerged as the primary bridge symptom in Year 3 and Year 6 (Figure 1). At Year 3, the ADHD symptom Difficulty waiting turn (I2) was primarily associated with the following ODD symptoms: Angry/resentful (ODD7; .07), Easy to annoy (ODD6; .06), and Blames others (ODD5; .06); at Year 6, the ADHD symptom Difficulty waiting turn (I2) was primarily related to the ODD symptom Deliberately annoys others (ODD4; .17) and secondarily to Easy to annoy (ODD6; .12).
Longitudinal Stability and Change in Network Structure of Parent-Reported Symptoms
Assessment of correlations between corresponding edges in network pairs suggested generally robust similarities in edges within networks across years. Regarding network structure, omnibus tests suggested no change in network edges, overall, across years (ps ≥ .56). No significant differences emerged in global strength across any comparisons (ps ≥ .23). Overall, network comparison results suggested that the structure of ADHD and ODD symptom networks was generally robust.
Teacher-Reported ADHD and ODD Network at Year 1
The teacher-reported cross-sectional network can be found in online supplemental material. As seen in Figure 2, examination of bridge centrality stability suggested stability in BEI in Year 1 (.59). Assessment of BEI suggested the ADHD symptom items of Blurts (I1) and Interrupts/intrudes (I3) as bridge symptoms that demonstrated robust relations with symptoms of ODD.
Figure 2.
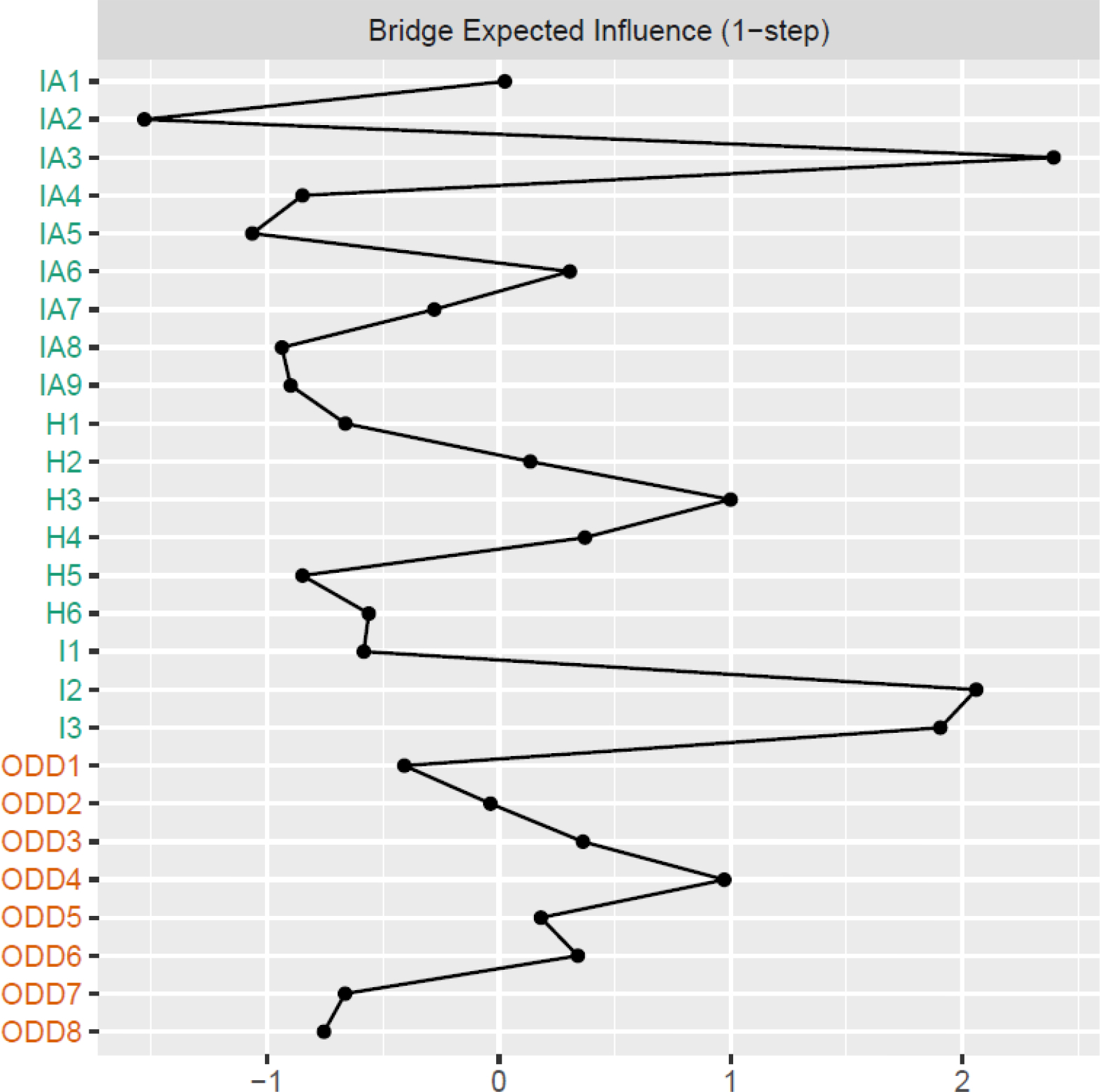
BEI Results for ADHD and ODD Network using Teacher-Reported Data for Year 1. IA1: careless mistakes; IA2: diff. sustaining attention; IA3: daydreams; IA4: diff. following instructions; IA5: diff. organizing; IA6: diff. sustaining mental effort; IA7: loses things; IA8: easily distracted; IA9: forgetful; H1: fidgets; H2: diff. remaining seated; H3: restless; H4: diff. playing quietly; H5: on the go; H6: talks excessively; I1: blurts; I2: diff. waiting turn; I3: interrupts; ODD1: loses temper; ODD2: argues; ODD3: disobeys rules; ODD4: deliberately annoys; ODD5: blames others; ODD6: easy to annoy; ODD7: angry/resentful; ODD8: spiteful/vindictive.
Network Comparison Tests
Network comparisons of teacher networks versus parent networks in Year 1 suggested significant differences in overall network structure (p = .04). Follow-up analyses comparing individual symptom-symptom relations suggested 26 relations that differed in strength across reporter-type. The pairs that significantly differed between ADHD and ODD symptoms included Forgetful and Loses temper (p = .02), Forgetful and Argues with adults (p = .02), Unable to engage in activities quietly and Argues with adults (p = .03), and On the go and Argues with adults (p = .01). Edge difference tests suggested that edge strength was greater in the parent-reported network relative to the teacher-reported network. Global strength in network pairs was significantly different (p < .001).
Longitudinal Network
The longitudinal graphical vector-autoregression model (Figure 3) demonstrated generally acceptable fit, χ2(1755) = 3773.34, p < .01; RMSEA = .061, 90% CI [.058, .064]; CFI = .88; TLI = .80. The items Angry/resentful (ODD7), Interrupts/intrudes (I9), Fidgets (H1), Difficulty sustaining attention (IA2), Difficulty waiting turn (I2), and Unable to play quietly (H4) demonstrated the highest out-expected influence (2.06, 1.33, 1.20, 1.14, 1,00, and .99, respectively; Figure 4). Similarly, these six items demonstrated the highest BEI, just in a slightly different order (Angry [ODD7]: 1.46, Interrupts/Intrudes [I9]: 1.18, Fidgets [H1]: .88, Difficulty waiting turn [I2]: .86, Unable to play quietly [H4]: .69, Difficulty sustaining attention [IA2]: .53; Figure 4).
Figure 3.
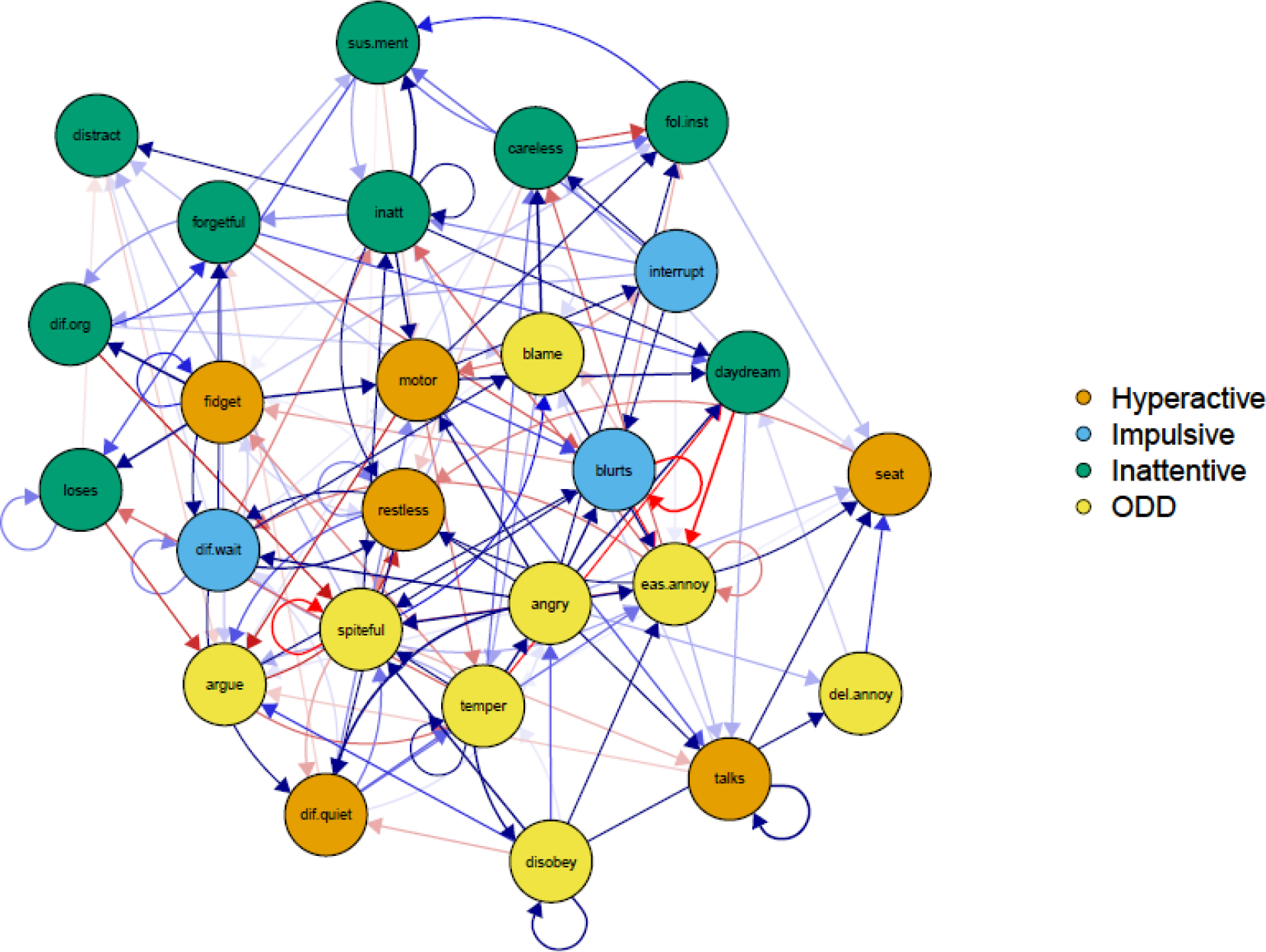
Longitudinal ADHD and ODD Network using Parent-Reported Data from Year 1 to Year 6. Only significant effects (ps < .05) are visualized.
Figure 4.
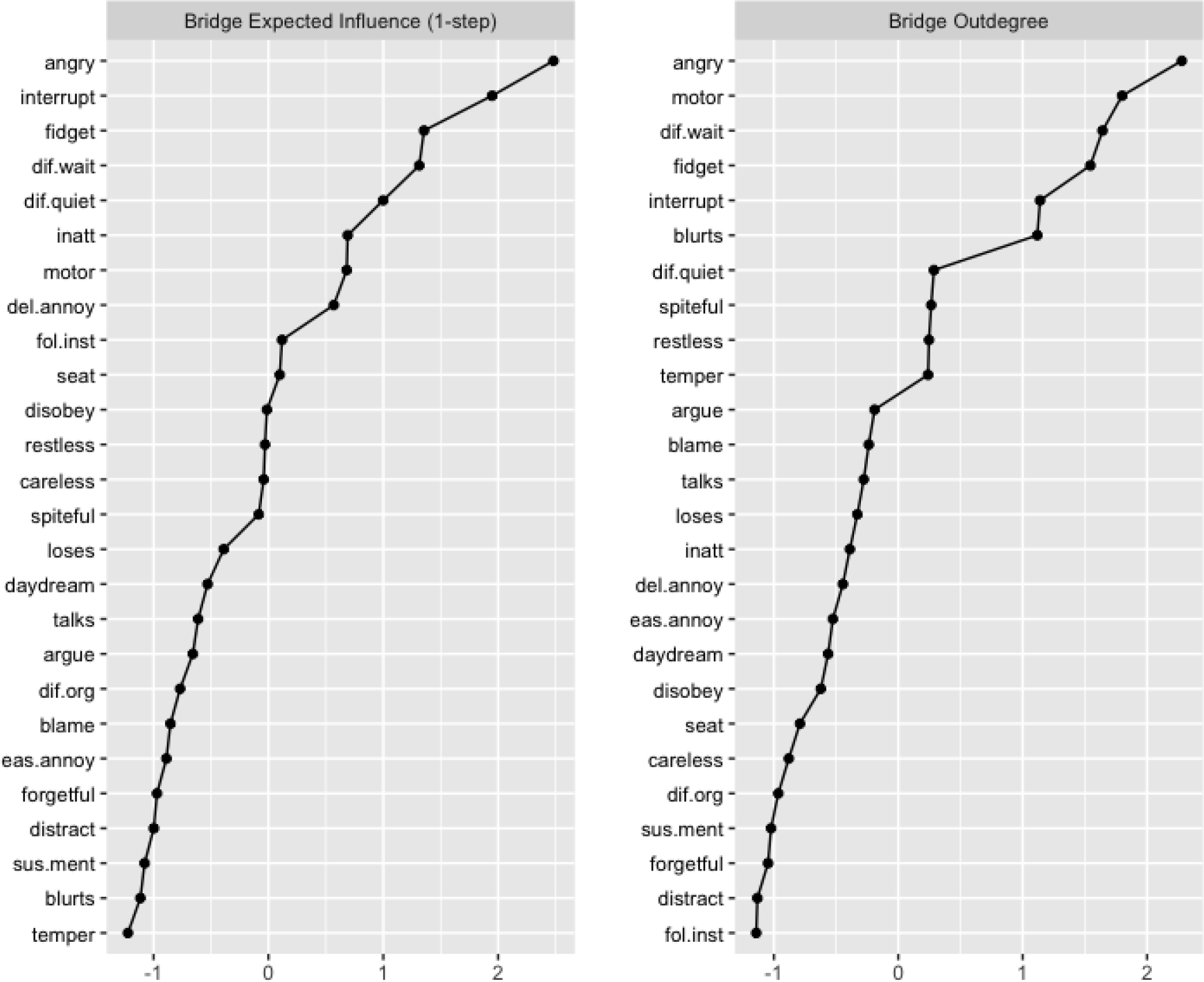
Bridge Expected Influence and Out-Expected Influence for Longitudinal Network.
Applied Tests
Lastly, hierarchical linear regressions examined the predictive ability of the bridge symptoms, relative to the non-bridge symptoms, in predicting teacher-rated social skill total scores at Year 6. The top four parent-rated bridge symptoms from cross-sectional networks (i.e., Unable to engage in activities quietly, Blurts, Difficulty waiting turn, and Argues with adults) were summed, and the top six parent-rated influential symptoms from the longitudinal network (i.e., Angry/resentful, Interrupts/intrudes, Fidgets, Difficulty sustaining attention, Difficulty waiting turn, and Can’t play quietly) were summed to form separate cross-sectional and longitudinal composites. In Model 1 (R2 = .08, F(2, 172) = 8.35, p < .001), the sum of the four top cross-sectional parent-rated bridge symptoms seemed to out-predicted (B = .27, SE = .11, p = .024) the remaining sum of Year 1 parent-rated DBD symptoms (B = .03, SE = .02, p = .78) in predicting the teacher-rated social skill total score at Year 6. In Model 2 (R2 = .09, F(2, 170) = 7.88, p = .001), the sum of the six most influential longitudinal symptoms appeared to out-predict (B = .36, SE = .10, p = .04) all remaining sum of Year 1 parent-rated DBD symptoms (B = −.07, SE = .03, p = .67) in predicting Year 6 teacher-rated social skill total score.
Discussion
The current study is the first to our knowledge to parse symptom level relations between ADHD and ODD using dynamic network modeling approaches across a six-year period from childhood through adolescence. This design allows for interpretation of longitudinal effects amongst symptoms, something that cross-sectional networks preclude. First, results found four bridge symptoms for the cross-sectional network and six bridge symptoms for the longitudinal network. Roughly half of the cross-sectional and longitudinal network bridge symptoms were from the impulsivity domain. These findings provide partial support for the hypothesis that impulsivity would play a central role as bridge symptoms across ADHD and ODD cross-sectionally and longitudinally. Next, these bridge symptoms at Year 1 appeared to out-predict non-bridge symptoms in explaining teacher-rated social skills five years later. These findings are further discussed below.
First, difficulty waiting turn was a key bridge symptom explaining the ADHD-ODD association that replicated across parent-rated cross-sectional and longitudinal networks. In addition, Interrupts/intrudes and Blurts were important across both parent and teacher networks. Impulsivity symptoms were core even during adolescence, a time when hyperactivity/impulsivity symptoms often decline while inattentive symptoms tend to persist and become more noticeable (Barkley, 1997). This may be a function of the impulsivity-enriched sample, which likely maintained a high level of impulsive behaviors well into adolescence. Other important items across networks included Unable to play quietly and perhaps Argues with adults and Angry/resentful. These symptoms are from other domains (e.g., hyperactivity, angry/irritable mood), but are in line with broader impulsivity phenotypes as included in the International Classification of Diseases-11th Revision (ICD-11; World Health Organization, 2018) which focuses more on verbal impulsivity and includes Talks a lot as an impulsivity item. This supports recent arguments to expand impulsivity items of ADHD (Nigg, 2017), given their potential to inform later negative outcomes (e.g., Goh, Martel, et al., 2020). Our work suggests that this might be particularly important for assessing broader risk for future negative outcomes, including risk of ODD and social deficits, during the transition from childhood to adolescence. Lastly, network comparison tests found that edges were stronger in parent networks relative to teacher networks. This may be due to true differences in how parents and teachers rate ADHD (e.g., Narad et al., 2015), or due to differences in the instrument used for each reporter. This is speculative and requires further investigation.
Next, preliminary exploration determined whether a subset of symptoms identified through dynamic modeling was associated with later negative outcomes. Linear regressions found that bridge symptoms, including a subset of impulsivity symptoms, predicted social dysfunction five years later during adolescence. Again, these results are at least partially consistent with our hypothesis and the overall theory of impulsivity of DBD (e.g., Barkley, 1997), where impulsivity is implicated in contributing to a host of negative impulsivity-related outcomes (e.g., substance use, reckless behavior). Social problems have been observed in up to 80% of children with ADHD (Staikova et al., 2013). Further, there is a considerable degree of social impairment during adolescence, and current results suggest that bridge symptoms, including specific impulsivity symptoms, contribute to elevated social dysfunction. Additional work is needed to determine whether bridge symptoms differentially impact certain social skills (e.g., conflict resolution, negotiation, and cooperation). These are all essential for competent social functioning across the lifespan and, if compromised, can lead to significantly impaired peer relations throughout childhood and adolescence (Bukowski, Laursen, & Rubin, 2018).
These findings continue informing our understanding of how ADHD and ODD symptoms interact with each other and with negative outcomes over time. Results could facilitate tailored and personalized assessment and intervention tools that account for heterogeneity in the relevance of such relations. For instance, the bridge symptoms, particularly Difficulty waiting turn, Interrupts/intrudes, and Blurts may be used to screen for concurrent and future impairment. Endorsement of and/or elevation on these symptoms would signal the need for more thorough assessment of ADHD and ODD, and treatment to mitigate negative social outcomes during this transition from childhood into adolescence. Further, identification of these bridge symptoms may lead to more effective treatments; rather than treating ADHD or ODD “as a whole,” the current findings highlight specific symptoms that may be more important to target in treatment to engender greater long-term change. More specifically, it may be more effective to tailor treatments that effectively target aspects such as impulse control specifically (e.g., Difficulty waiting turn, Interrupts/intrudes) to provide maximal benefit in reducing or even preventing social impairment. Further, alternate approaches have been used in identifying subsets of clinically relevant symptoms for ADHD such as machine learning (Goh, Martel et al., 2021) and item response theory (Li et al., 2016). ADHD symptom subsets somewhat differed based upon the analytic method, highlighting differences in the functions of these analytic approaches. Thus, future research should employ these methods within a single sample to determine which symptoms are most crucial in understanding DBD.
The current study had several strengths including a well-characterized longitudinal sample at heightened risk for impulsivity and use of symptom-level dynamic modeling methods. There were also several limitations. Characterization of impulsivity was limited to only three DSM-5 ADHD items (or four ICD-11 items) that are primarily based upon verbal impulsivity. There continues to be debate on whether inclusion of additional behavioral impulsivity items is necessary. Current results suggest that adolescent expression of ADHD may be better captured by additional impulsivity items. Next, teacher-rated social skills were used as an outcome given the available measures, but examination of other longitudinal outcomes would be an important future direction.
Longitudinal networks were constructed using slightly uneven time-points across the three waves (i.e., two years between waves 1 and 3, three years between 3 and 6). Longitudinal network analysis requires that time waves are equal across all assessment points, warranting future research to use data distributed evenly across a given timeframe. The use of uneven time-points may be a potential explanation for the longitudinal model fit which was generally acceptable, although certain indices were noticeably lower (e.g., TLI = .80), suggesting cautious interpretation of this model. Indeed, cross-sectional models were constructed using data from their respective years, perhaps leading to more stable networks. Age overlap was observed across the assessment waves (i.e., Year 1 ages 6–13, Year 3 ages 9–15, and Year 6 ages 11–18). While this was done to maximize statistical power, this overlap does not cleanly differentiate between youth measured in childhood versus adolescence. Future research should aim to recruit cohorts that are distinctly measured at the same developmental timepoints. The sample was part of a high-functioning, low-risk, affluent, and predominately White cohort where rates of comorbid disorders (e.g., ODD, conduct disorder) were lower than expected. Therefore, findings from this sample may not generalize to diverse, lower SES, and/or urban samples. Despite these limitations, this study is one of the few to conduct longitudinal network analysis and provides initial support for dynamic modeling approaches at the symptom level, which is a key area for future research (Bringmann & Eronen, 2018).
In sum, in an impulsivity enriched sample followed longitudinally from childhood to adolescence, results of the current study suggested that the impulsivity items of Difficulty waiting turn, Blurts, and Interrupts/intrudes were key in explaining the ADHD-ODD association. Further, the sum of six symptoms across ADHD and ODD, including two impulsivity symptoms (i.e., Interrupts/intrudes, Difficulty waiting turn) more strongly predicted teacher-rated social skills five years later than the remaining DBD symptoms. Such items might be useful for screening and personalized interventions targeting impulsivity in adolescents at risk for DBD and later social dysfunction.
Supplementary Material
Key points.
Youth with ADHD are at a substantially higher risk of developing other forms of psychopathology, particularly ODD, a specific type of DBD.
The comorbidity between ADHD and ODD appears to occur through mechanisms of impulsivity, yet little work has examined this association longitudinally at the item level.
Using dynamic symptom-level network analysis within a longitudinal design across three points spanning from childhood to adolescence, findings showed that a subset of symptoms, including two impulsivity symptoms (e.g., blurts, interrupts) explained the association between ADHD and ODD.
A composite score of these specific symptoms showed greater ability in predicting teacher-rated social skills five years later relative to a total DBD composite score.
Assessment and treatment protocols can be designed to better target specific symptoms, including impulsivity, to mitigate long-term negative outcomes.
Acknowledgements
The authors thank all participants for making this work possible. The efforts on this project by M.W.S., was partially supported by the National Institute of Mental Health under award number K23MH126211. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health. The remaining authors declare no conflict of interest. The datasets generated and analyzed for the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations:
- ADHD
Attention-Deficit/Hyperactivity Disorder
- ODD
Oppositional Defiant Disorder
- DBD
Disruptive Behavior Disorder
- SDQ
Strengths and Difficulties Questionnaire
- WISC-IV
Weschler Intelligence Scale for Children, 4th Edition
- BEI
Bridge Expected Influence
Footnotes
Conflict of interest statement: See Acknowledgements for full disclosures.
References
- Ahmad SI, & Hinshaw SP (2017). Attention-deficit/hyperactivity disorder, trait impulsivity, and externalizing behavior in a longitudinal sample. Journal of Abnormal Child Psychology, 45(6), 1077–1089. 10.1007/s10802-016-0226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. In DSM-5 (5th ed.). American Psychiatric Association. [Google Scholar]
- Antshel KM, & Remer R (2003). Social skills training in children with attention deficit hyperactivity disorder: A randomized-controlled clinical trial. Journal of Clinical Child and Adolescent Psychology, 32(1), 153–165. 10.1207/S15374424JCCP3201_14 [DOI] [PubMed] [Google Scholar]
- Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65. [DOI] [PubMed] [Google Scholar]
- Bauermeister JJ, Shrout PE, Ramírez R, Bravo M, Alegría M, Martínez-Taboas A, Chávez L, Rubio-Stipec M, García P, Ribera JC, & Canino G (2007). ADHD correlates, comorbidity, and impairment in community and treated samples of children and adolescents. Journal of Abnormal Child Psychology, 35(6), 883–898. 10.1007/s10802-007-9141-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Zisner AR, & Sauder CL (2017). Trait impulsivity and the externalizing spectrum. Annual Review of Clinical Psychology, 13(1), 343–368. 10.1146/annurev-clinpsy-021815-093253 [DOI] [PubMed] [Google Scholar]
- Bell ZE, Fristad MA, Youngstrom EA, Arnold LE, Beauchaine TP, Findling RL, ... & Horwitz SM. (2022). Attention-Deficit/Hyperactivity Disorder symptoms and externalizing progression in the LAMS Study: A test of trait impulsivity theory. Journal of the American Academy of Child & Adolescent Psychiatry, 61(2), 298–307. 10.1016/j.jaac.2021.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Spencer TJ, Newcorn JH, Gao H, Milton DR, Feldman PD, & Witte MM (2007). Effect of comorbid symptoms of oppositional defiant disorder on responses to atomoxetine in children with ADHD: a meta-analysis of controlled clinical trial data. Psychopharmacology, 190(1), 31–41. [DOI] [PubMed] [Google Scholar]
- Borsboom D, & Cramer AOJ (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Bringmann LF, & Eronen MI (2018). Don’t blame the model: Reconsidering the network approach to psychopathology. Psychological Review, 125(4), 606–615. 10.1037/rev0000108 [DOI] [PubMed] [Google Scholar]
- Bukowski WM, Laursen B, & Rubin KH (2018). Handbook of peer interactions, relationships, and groups (2nd ed.). Guilford. [Google Scholar]
- Burns GL, & Walsh JA (2002). The influence of ADHD–hyperactivity/impulsivity symptoms on the development of oppositional defiant disorder symptoms in a 2-year longitudinal study. Journal of Abnormal Child Psychology, 30, 245–256. 10.1023/A:1015102812958 [DOI] [PubMed] [Google Scholar]
- Casey BJ, Getz S, & Galvan A (2008). The adolescent brain. Developmental Review, 28(1), 62–77. 10.1016/j.dr.2007.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, & Somerville LH (2011). Braking and accelerating of the adolescent brain. Journal of Research on Adolescence, 21(1), 21–33. 10.1111/j.1532-7795.2010.00712.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chacko A, Kofler M, & Jarrett M (2014). Improving outcomes for youth with ADHD: A conceptual framework for combined neurocognitive and skill-based treatment approaches. Clinical Child and Family Psychology Review, 17(4), 368–384. 10.1007/s10567-014-0171-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csardi G, & Nepusz T (2006). The igraph software package for complex network research. International Journal of Complex Systems. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, & Reid R (1998). ADHD Rating Scale-IV (ADHD-RS). Guilford. [Google Scholar]
- Elia J, Ambrosini P, & Berrettini W (2008). ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child and Adolescent Psychiatry and Mental Health, 2(1), 1–9. 10.1186/1753-2000-2-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S (2021). psychonetrics: Structural equation modeling and confirmatory network analysis. https://cran.r-project.org/web/packages/psychonetrics/psychonetrics.pdf [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittman VD, & Borsboom D (2012). Qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48(4), 33–36. [Google Scholar]
- Epskamp S, & Fried EI (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23(4), 617–634. 10.1037/met0000167 [DOI] [PubMed] [Google Scholar]
- Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, Newcorn JH, Gignac M, Al Saud NM, Manor I, Rohde LA, Yang L, Cortese S, Almagor D, Stein MA, Albatti TH, Aljoudi HF, Alqahtani MMJ, Asherson P, … Wang Y (2021). The world federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews, 128, 789–818. 10.1016/j.neubiorev.2021.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foygel R, & Drton M (2010). Extended bayesian information criteria for gaussian graphical models. Advances in Neural Information Processing System, 23, 2020–2028. [Google Scholar]
- Frankel F, & Feinberg D (2002). Social problems associated with ADHD vs. ODD in children referred for friendship problems. Child Psychiatry and Human Development, 33(2), 125–146. [DOI] [PubMed] [Google Scholar]
- Friedman J, Hastie T, & Tibshirani R (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics, 9(3), 432–441. 10.1093/biostatistics/kxm045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruchterman TM, & Reingold EM (1991). Graph drawing by force-directed placement. Software: Practice and Experience, 21, 1129–1164. 10.1002/spe.4380211102 [DOI] [Google Scholar]
- Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, & Blumberg SJ (2019). Prevalence and treatment of depression, anxiety, and conduct problems in US children. The Journal of Pediatrics, 206, 256–267. 10.1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh PK, Martel MM, & Barkley RA (2020). Clarifying ADHD and sluggish cognitive tempo item relations with impairment: A network analysis. Journal of Abnormal Child Psychology. 10.1007/s10802-020-00655-2 [DOI] [PubMed] [Google Scholar]
- Goh PK, Martel MM, Jones PJ, Bansal PS, Eng AG, Elkins AR, & Barkley RA (2021). Clarifying relations between ADHD and functional impairment in adulthood: Utilization of network and machine learning approaches. Assessment. Advance online publication. 10.1177/10731911211050921 [DOI] [PubMed] [Google Scholar]
- Goh PK, Smith TE, Lee CA, Bansal PS, Eng AG, & Martel MM (2021). Etiological Networks of attention-deficit/hyperactivity disorder during childhood and adolescence. Journal of Clinical Child and Adolescent Psychology, 1–14. 10.1080/15374416.2021.1946820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham FM, & Elliot SN (2008). Social skills improvement system: Rating scales manual. NCS Pearson. [Google Scholar]
- Gresham FM, Elliott SN, Vance MJ, & Cook CR (2011). Comparability of the Social Skills Rating System to the Social Skills Improvement System: Content and psychometric comparisons across elementary and secondary age levels. School Psychology Quarterly, 26(1), 27. 10.1037/a0022662 [DOI] [Google Scholar]
- Harvey EA, Breaux RP, & Lugo-Candelas CI (2016). Early development of comorbidity between symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD). Journal of Abnormal Psychology, 125(2), 154–167. 10.1037/abn0000090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones PJ (2018). Network tools: Tools for identifying important nodes in networks. https://CRAN.R-project.org/package=networktools [Google Scholar]
- Jones PJ, Ma R, & McNally RJ (2019). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research, 1–15. 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- Karalunas SL, Gustafsson HC, Dieckmann NF, Tipsord J, Mitchell SH, & Nigg JT (2017). Heterogeneity in development of aspects of working memory predicts longitudinal attention deficit hyperactivity disorder symptom change. Journal of Abnormal Psychology, 126(6), 774–792. 10.1037/abn0000292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Kwon HJ, Ha M, Lim MH, & Kim KM (2021). Network analysis for the symptom of depression with children’s depression inventory in a large sample of school-aged children. Journal of Affective Disorders, 281, 256–263. 10.1016/j.jad.2020.12.002 [DOI] [PubMed] [Google Scholar]
- Krause RW, Huisman M, Steglich C, & Snijders TA (2018, August). Missing network data a comparison of different imputation methods. In 2018 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining (ASONAM) (pp. 159–163). IEEE. [Google Scholar]
- Li JJ, Reise SP, Chronis-Tuscano A, Mikami AY, & Lee SS (2016). Item response theory analysis of ADHD symptoms in children with and without ADHD. Assessment, 23(6), 655–671. 10.1177/1073191115591595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindhiem O, Bennett CB, Hipwell AE, & Pardini DA (2015). Beyond symptom counts for diagnosing oppositional defiant disorder and conduct disorder?. Journal of Abnormal Child Psychology, 43, 1379–1387. 10.1007/s10802-015-0007-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, & Hinshaw SP (2008). Few preschool boys and girls with ADHD are well-adjusted during adolescence. Journal of Abnormal Child Psychology, 36(3), 373–383. 10.1007/s10802-007-9184-6 [DOI] [PubMed] [Google Scholar]
- Luo Y, Weibman D, Halperin JM, & Li X (2019). A review of heterogeneity in attention deficit/hyperactivity disorder (ADHD). Frontiers in human neuroscience, 42. 10.3389/fnhum.2019.00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus DK, & Barry TD (2011). Does attention-deficit/hyperactivity disorder have a dimensional latent structure? A taxometric analysis. Journal of Abnormal Psychology, 120(2), 427. 10.1037/a0021405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Goh PK, Lee CA, Karalunas SL, & Nigg JT (2021). Longitudinal attention-deficit/hyperactivity disorder symptom networks in childhood and adolescence: Key symptoms, stability, and predictive validity. Journal of Abnormal Psychology, 130(5), 562–574. 10.1037/abn0000661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Gremillion M, Roberts B, von Eye A, & Nigg JT (2010). The structure of childhood disruptive behaviors. Psychological Assessment, 22(4), 816–826. 10.1037/a0020975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Levinson CA, Langer JK, & Nigg JT (2016). A network analysis of developmental change in ADHD symptom structure from preschool to adulthood. Clinical Psychological Science, 4(6), 988–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Levinson CA, Lee CA, & Smith TE (2017). Impulsivity symptoms as core to the developmental externalizing spectrum. Journal of Abnormal Child Psychology, 45(1), 83–90. 10.1007/s10802-016-0148-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, Molina BS, Hoza B, Gerdes AC, Hinshaw SP, Hechtman L, & Arnold LE (2012). Peer rejection and friendships in children with attention-deficit/hyperactivity disorder: Contributions to long-term outcomes. Journal of Abnormal Child Psychology, 40(6), 1013–1026. 10.1007/s10802-012-9610-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musser ED, Karalunas SL, Dieckmann N, Peris TS, & Nigg JT (2016). Attention-deficit/hyperactivity disorder developmental trajectories related to parental expressed emotion. Journal of Abnormal Psychology, 125(2), 182–195. 10.1037/abn0000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narad ME, Garner AA, Peugh JL, Tamm L, Antonini TN, Kingery KM, ... & Epstein JN. (2015). Parent–teacher agreement on ADHD symptoms across development. Psychological Assessment, 27(1), 239–248. 10.1037/a0037864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT (2017). Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58(4), 361–383. 10.1111/jcpp.12675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, & Casey BJ (2005). An integrative theory of attention-deficit/hyperactivity disorder based on the cognitive and affective neurosciences. Development and Psychopathology, 17(3), 785–806. 10.1017/S0954579405050376 [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, & Ryan N (1986). Kiddie schedule for affective disorders and schizophrenia. Western Psychiatric Institute. [Google Scholar]
- Reichardt J, & Bornholdt S (2006). Statistical mechanics of community detection. Physical Review E, 74(1), 016110. 10.1103/PhysRevE.74.016110 [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ, & McNally RJ (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757. 10.1037/abn0000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, Clasen L, Evans A, Giedd J, & Rapoport JL (2007). Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences, 104(49), 19649–19654. 10.1073/pnas.0707741104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TE, Lee CA, Martel MM, & Axelrad ME (2017). ODD symptom network during preschool. Journal of Abnormal Child Psychology, 45(4), 743–748. 10.1007/s10802-016-0196-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear L (2010). The behavioral neuroscience of adolescence. W. W. Norton & Company. [Google Scholar]
- Staikova E, Gomes H, Tartter V, McCabe A, & Halperin JM (2013). Pragmatic deficits and social impairment in children with ADHD. Journal of Child Psychology and Psychiatry, 54(12), 1275–1283. 10.1111/jcpp.12082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, & Goodman R (2009a). Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child and Adolescent Psychiatry, 48(4), 404–412. 10.1097/CHI.0b013e3181984f30 [DOI] [PubMed] [Google Scholar]
- Stringaris A, & Goodman R (2009b). Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry, 50(3), 216–223. 10.1111/j.1469-7610.2008.01989.x [DOI] [PubMed] [Google Scholar]
- van Borkulo CD, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, & Waldorp LJ (2017). Comparing network structures on three aspects: A permutation test. 10.13140/RG.2.2.29455.38569 [DOI] [PubMed] [Google Scholar]
- Wehmeier PM, Schacht A, & Barkley RA (2010). Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. Journal of Adolescent Health, 46(3), 209–217. 10.1016/j.jadohealth.2009.09.009 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018). International statistical classification of diseases and related health problems (11th Revision). World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


