Abstract
Black/African American (BAA) men have the lowest life expectancy among other major demographic groups in the United States, with BAA male mortality rates 40% higher than their White male counterparts. Despite known benefits of preventive health care utilization, BAA men are 43% more likely to use the emergency department for usual care. Many intersecting factors like medical mistrust and religion have been identified as common barriers BAA men face in health care utilization with few studies exploring factors that impact their current preventive health care utilization. In addition, BAA men’s perceptions of health and ability to identify or seek help have always been disproportionately lower than other racial groups despite higher rates of preventable diseases. Using the tenets of the Andersen Healthcare Utilization Model, this cross-sectional study of 176 BAA men explores BAA men’s current preventive health care practices while examining the intersection of predisposing, enabling, and need factors on BAA men’s preventive health care utilization. While it is well known that higher income levels and higher education positively influence health care utilization, the intersection of religious affiliation and higher levels of medical mistrust was associated with BAA men’s decreased engagement with health care as religion posed as a buffer to health care utilization. This study demonstrated that BAA men’s perception of health differed by sexual orientation, educational status, and income. However, across all groups the participants’ perspective of their health was not in alignment with their current health outcomes. Future studies should evaluate the impact of masculine norms as potential enabling factors on BAA men’s preventive health care utilization.
Keywords: Black, African American, preventive, health care utilization
Background
Black/African American Men’s Health and Preventive Health Care
Black/African American (BAA) men, a self-identification inclusive of all men of African descent, have the lowest life expectancy among all major demographic groups represented in the United States with mortality rates 40% higher than their White male counterparts (Bond & Herman, 2016). BAA men have disproportionately higher rates of illness being 60% more likely than White men to develop prostate cancer (Watson et al., 2019), 10% more likely to be hypertensive (Go et al., 2013), and 6 to 8 times more likely to contract a sexually transmitted disease, with a one in 22 chance of lifetime risk for HIV diagnosis (Centers for Disease Control and Prevention, 2022; Hess et al., 2017). Earlier detection and increased engagement with preventive health care have shown impact on morbidity and mortality rates among BAA men (Nies & McEwen, 2019; Watson et al., 2019).
Preventive health care is a proactive approach to health care utilization encompassing primary (health promotion and education), secondary (screenings and short-term treatment), and tertiary levels (long-term/ rehabilitation treatment) of prevention (Nies & McEwen, 2019). In 2021, 81.7% of BAA men aged 18 and over in the United States visited the doctor within the past 12 months (National Center for Health Statistics, 2022). Despite the known benefits of preventive health care utilization, BAA men are 43% more likely than other men to use the emergency room (ER) for their health care needs rather than to seek nonemergency care scenarios such as doctor’s offices or clinics (Arnett et al., 2016). By improving early detection and influencing better disease prognosis, preventive health care can address health disparities and increase the life expectancy of BAA men.
BAA Men’s Barriers to Health Care
Medical mistrust and alternative coping strategies such as religion and spirituality have been identified as barriers impeding BAA health care utilization (Arnett et al., 2016; Griffith et al., 2015; Powell et al., 2016). Medical mistrust is defined as distrust of the health care system in general and of its providers, institutions, and treatment plans specifically (Arnett et al., 2016; Williamson et al., 2019). Historically, race-based medical mistrust stems from the lack of culturally congruent providers, leading to less culturally competent care and to provider bias (Maina et al., 2018). In the face of the long history in the United States of medical discrimination and persistent systemic racism and mistreatment of BAA men, exemplified by the decades-long United States Public Health Service Study of Syphilis (USPHSS), longer delays between prostate cancer diagnosis and treatment, and continued COVID-19-treatment-related medical mistrust, such resistance to health care is well founded (Arnett et al., 2016; Bazargan et al., 2021; Czeisler et al., 2020; Lillard et al., 2022; Meyers-Pantele et al., 2022). Discrimination and mistreatment lead to inequitable care. As a result, engagement with preventive health care among BAA men, including practices of routine medical visits, new interventions, screenings, and the like, is avoided and viewed as potentially harmful due to lack of trust in the health care system (Dale et al., 2016; Meyers-Pantele et al., 2022; Rogers et al., 2022). In the absence of medical trust, BAA men turn to religion and spirituality, or belief in something beyond self, as alternative avenues to express health-seeking behaviors and as protective factors against discrimination and medical mistrust (Mushonga & Henneberger, 2020; Robinson et al., 2018). Religion and spirituality are intertwined concepts within the BAA experience transcending medical advice serving as a sense of hope and a means of coping (Haidar et al., 2023). As such, BAA men are less likely than their White counterparts to seek psychological or psychiatric therapy or counseling, for example, outside their religious institutions (Hankerson et al., 2015; Robinson et al., 2018).
Understanding the barriers that impede BAA men’s outlook on health care, influence their ability to participate in health care, or increase their need to utilize health care is crucial to clarifying BAAs’ engagement with health care measures. This study explores the impact of such barriers on BAA men’s current preventive health care utilization.
Conceptual Framework
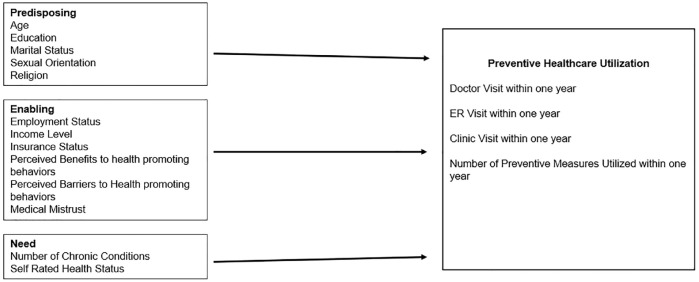
According to the Andersen Healthcare Utilization Model (AHM), the use of preventive health care services is a function of a person’s predisposition to health-seeking behaviors (predisposing factors), factors that facilitate or impede seeking health care (enabling factors), and the need for health care (need factors) (Andersen, 1995; Bradley et al., 2002). Predisposing factors include sociodemographic variables such as age, marital status, sexual orientation, and education. Enabling factors include an individual’s employment status, degree of medical mistrust, perceived benefits to health-promoting behaviors, perceived barriers to health-promoting behaviors, health insurance status, and income level. Needs factors include immediate or critical factors such as preexisting conditions and self-rated health status. Using this model, researchers have clarified how predisposing, enabling, and need factors affect health care engagement within the BAA community regarding the use of health care resources, use of preexposure prophylaxis, and keeping of physician appointments, among other topics (Burns et al., 2021; Parker et al., 2017).
The purpose of this study is to explore predisposing factors, enabling factors, and need factors as predictors of preventive health care utilization in BAA men (see conceptual framework in Figure 1). The hypothesis is that predisposing factors and enabling factors will have the most impact on preventive health care utilization among BAA men based on previous studies using the AHM and cultural congruence with the desired sample (Assari & Caldwell, 2017; Parker et al., 2017; Tabaac et al., 2020).
Figure 1.
Conceptual Framework for AHM Factors in BAA Men
Note. AHM = Andersen Healthcare Utilization Model; BAA = Black/African American; ER = emergency room.
Method
Study Design
A nonexperimental, correlational cross-sectional design was used to examine predisposing factors, enabling factors, and need factors of the AHM as predictors of preventive health care utilization in BAA men. The study sample includes BAA men predominantly from the Upper Midwest metropolitan area surveyed in a single online session. Based on power analysis using Soper’s model for multiple regression with 13 predictors, a desired sample size of 131 BAA men with an effect size of 0.15, power of 0.80, and alpha of .05 was determined (Soper, 2022).
The sample inclusion criteria were the following: (a) identify as male, (b) identify as BAA, and (c) are between the ages of 26 and 75. While BAA men are not a monolith across the African, African American, Afro-Caribbean and Afro-Latino diaspora, for the purpose of this study, BAA represents any participant who self-identified as Black or African American. The minimum age of 26 years old was selected because it is the age at which young adults are no longer eligible to be covered under their parent’s health insurance (U.S. Department of Health and Human Services, 2022). An upper age limit of 75 was selected because many preventive health screens stop at age 75, like the colorectal cancer screening (Grossman et al., 2018). This study was approved by the institutional review board (IRB) as a cross-sectional study. Convenience sampling was selected as the method of recruitment and took place through the use of social networks of the researcher. Once eligibility was confirmed, participants were emailed a link to the survey. A waiver of consent documentation was used. The survey consisted of 95 items, and validated scales were employed. The average time for completion was about 10 to 20 min. Participants were compensated with a US$20 gift card for their time.
Study Measures
Outcome
Preventive health measures can be primary, secondary, or tertiary with primary prevention focusing on health promotion and education, secondary prevention focusing on screenings and short-term treatment, and tertiary prevention focusing on long-term treatment (Nies & McEwen, 2019). To operationalize the concept of preventive health care utilization, the Older Men’s Health Program and Screening Inventory (OMHPSI) was used as a tool to ascertain men’s current health practices and beliefs with findings that support reliability with a Cronbach’s alpha of .78 (Loeb, 2003). Although categorized for older men, identified in the measure as any man older than 55, this comprehensive tool has been used in varying studies to assess all levels of prevention and assesses participants’ current perceptions of their health and engagement with or barriers to health care programming and resources (Loeb, 2003; Loeb et al., 2008). As older men often need to utilize health care more frequently, the OMHPSI includes questions on the utilization of preventive health measures such as preparing healthy foods, exercising, and getting immunized (primary-level prevention); health screenings such as blood pressure, colonoscopy, and physical exam (secondary level of prevention); and taking medication and engaging in memory improvement efforts (tertiary level of prevention) giving a wider range of preventive health care options than other tools. The OMHPSI was also found to be especially relevant for this study amid the 2020 COVID-19 pandemic. While assessing men’s current health practices, the tool also assesses current immunizations or vaccinations within the past year.
The National Health Interview Survey (NHIS) was also adapted into this study as it has been used to monitor national health since 1957 and includes measurement of participants’ preventive health care utilization (National Center for Health Statistics—Division of Health Interview Statistics, 2020). The NHIS was used to measure participants’ time since the last doctor visit, time since the last ER visit, and time since the last clinic visit with scoring in an ordinal fashion with time ranging from less than 12 months ago (0) to within the last 10 years (5). Doctor visits were defined as seeing a doctor or health professional for a wellness visit, physical, or general-purpose check-up. Clinic visits were defined as being synonymous with urgent care visits for one’s health that could include preventive measures (receiving vaccinations, check-ups, lab diagnostics, follow-ups, etc.) or more urgent matters. ER visits, while not preventive, were included for comparison purposes as many BAA men utilize ERs for their health care needs (Arnett et al., 2016; Powell et al., 2019). For purposes of this study, these variables were measured dichotomously, viewing answer choices as yes or no to indicate whether the participant had engaged in the visit within the past year.
Independent Variables
Predisposing factors of the AHM were assessed using demographic questions of age (ranging from 26 to 75 years), education level (less than bachelor’s degree, bachelor’s degree, advanced degree), marital status (not married or married), sexual orientation (heterosexual or not heterosexual), and religion (yes or no).
As enabling factors are considered factors that facilitate or impede seeking health care (Andersen, 1995), participants were asked additional demographic questions such as annual income (less than US$10,000 to greater than US$110,000), employment status (unemployed, student worker, worker only, or retired), and known insurance status (yes or no). Variables of perceived benefits to health-promoting behaviors and perceived barriers to health-promoting behaviors were examined with the use of questioning from the OMHPSI. Research shows BAA men have lower self-efficacy in preventive health care utilization practices due to conformity to gender norms, mistrust of the health care system, and distrust of physicians (Powell et al., 2016, 2019). As medical mistrust has been identified as a common barrier to health care among BAA men, this variable was added using the Medical Mistrust Index (MMI). The MMI is a 17-item measure established to ascertain the degree to which an individual mistrusts health care organizations with studies supporting the association with underutilization of health services (Laveist et al., 2009). All 17 items were scored on a 4-point Likert-type scale from strongly disagree (0) to strongly agree (3). This measure has been used in numerous studies supporting reliability with a test–retest of the overall scale resulting in 0.70 and a Cronbach’s alpha of .83 for this study.
Within our model, needs factors were assessed using the following variables: number of chronic conditions and self-rated health status (poor, fair, good, excellent). Participants were presented with a list of potential health conditions identified by the Older Men’s Health Program and Screening Inventory. Participants were asked to report the health conditions that currently coincide with their health history and to list any other condition(s) not listed. This variable was used as the total number of conditions. Self-rated health status was evaluated on a continuous level (1 = poor, 2 = fair, 3 = good, 4 = excellent) to determine participants’ current perceptions of their health status.
Data Analysis
Data analysis was conducted using Stata 15 with descriptive statistics for all variables summarized in Table 1. Relating to the distribution of the outcome variables, utilization of a doctor, ER, and clinic visit in the past year were dichotomized and logistic regression models were used to examine the predictive effects of predisposing factors, enabling factors, and need factors on these outcomes. Poisson regression, a regression used when dependent variables are count variables (UCLA: Statistical Consulting Group, 2022), was used to analyze the number of preventive measures BAA men used within the past year. The effects of predisposing, enabling, and need factor models were analyzed independently in reduced models with results depicted in Tables 3 to 5, respectively, to analyze the predictive effects of each factor independent of each other. Based on results from the reduced models, the independent variables of self-rated health and sexual orientation never had a p ≤ .2 and, therefore, were removed from the full model depicted in Table 2 to improve parameter estimates.
Table 1.
Participant Statistics (N = 176)
| Characteristics | N | % |
|---|---|---|
| Predisposing factors | ||
| Age (26–74) | (M = 38.5, SD = 12.95) | |
| Marital status | ||
| Not married | 76 | 43.18 |
| Married | 100 | 56.5 |
| Religion | ||
| No religion | 23 | 13.07 |
| Religion | 153 | 86.93 |
| Education | ||
| Less than bachelor’s degree | 46 | 26.14 |
| Bachelor’s degree | 89 | 50.57 |
| Advanced degree | 41 | 23.30 |
| Sexual orientation | ||
| Heterosexual | 139 | 78.98 |
| Not heterosexual | 37 | 21.02 |
| Enabling factors | ||
| Known insurance | ||
| Yes | 152 | 86.36 |
| No | 24 | 13.64 |
| Employment | ||
| Unemployed | 12 | 6.82 |
| Student worker | 30 | 17.05 |
| Worker only | 120 | 68.18 |
| Retired | 14 | 7.95 |
| Income level | (M = US$73,209.83, SD = US$30,370.28) | |
| Medical Mistrust Index (0–51) | (M = 26.99, SD = 6.82) | |
| No. of perceived barriers | (M = 1.79, SD = 1.75) | |
| No. of perceived benefits | (M = 4.50, SD = 2.40) | |
| Need factors | ||
| Self-rated health status | ||
| Less than good | 34 | 19.32 |
| Good | 101 | 57.39 |
| Excellent | 41 | 23.30 |
| No. of health conditions (0–15) | (M = 1.18, SD = 1.31) | |
| Outcome variables | ||
| Dr visit within the past 1 year | 144 | 81.82 |
| ER visit within the past 1 year | 56 | 31.82 |
| Clinic visit within the past 1 year | 87 | 49.43 |
| No. of preventive measures in the past 1 year | (M = 4.10, SD = 2.45) | |
Note. ER = emergency room.
Table 3.
Predisposing Factors to Predict Outcomes
| Characteristics | Dr visit within 1 year* | ER visit within 1 year | Clinic visit within 1 year | No. of preventive measures within 1 year* | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | Coef. | 95% CI | |
| Age (26–74) | 1.07* | [1.02,1.13]* | 1.00 | [0.97, 1.03] | 1.00 | [0.98, 1.03] | 0.00 | [−0.01, 0.01] |
| Marital status | ||||||||
| Not Married (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Married | 0.54 | [0.22, 1.31] | 1.00 | [0.50, 2.00] | 0.71 | [0.37, 1.36] | −0.29* | [−0.44, 0.13]* |
| Religion | ||||||||
| No religion (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Religion | 0.82 | [0.23, 2.93] | 1.54 | [0.55, 4.31] | 2.61 | [0.97, 6.99] | −0.06 | [−0.28, 0.17] |
| Education | ||||||||
| Less than bachelor (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Bachelor’s degree | 0.67 | [0.21, 2.15] | 0.77 | [0.34, 1.77] | 0.87 | [0.39, 1.94] | 0.24* | [0.04, 0.44]* |
| Advanced degree | 1.52 | [0.35, 6.58] | 0.50 | [0.18, 1.38] | 1.19 | [0.46, 3.05] | 0.32* | [0.08, 0.55]* |
| Sexual orientation | ||||||||
| Heterosexual (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Not heterosexual | 0.66 | [0.25, 1.74] | 0.87 | [0.38, 1.98] | 1.37 | [0.63, 2.97] | −0.07 | [−0.25, 0.12] |
Note. ER = emergency room; OR = odds ratio; CI = confidence interval.
p < .05.
Table 5.
Need Factors to Predict Outcomes
| Characteristics | Dr visit within 1 year | ER visit within 1 year | Clinic visit within 1 year | No. of preventive measures within 1 year | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | Coef | 95% CI | |
| No. of health conditions | 1.65* | [1.04, 2.61]* | 1.06 | [0.82, 1.37] | 1.23 | [0.95, 1.60] | 0.00 | [−0.06, 0.06] |
| Self-rated health status | 1.27 | [0.66, 2.44] | 0.85 | [0.51, 1.44] | 1.26 | [0.77, 2.06] | 0.06 | [−0.06, 0.18] |
Note. ER = emergency room; OR = odds ratio; CI = confidence interval.
p < .05.
Table 2.
AHM Full Model in Black/African American Men
| Characteristics | Dr visit within 1 year | ER visit within 1 year | Clinic visit within 1 year* | No. of preventive measures within 1 year* | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | Coef. | 95% CI | |
| Age (26–74) | 1.06 | [1.00,1.13]* | 1.01 | [0.97, 1.05] | 1.01 | [0.97, 1.05] | 0.00 | [−0.01, 0.01] |
| Marital status | ||||||||
| Not married (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Married | 0.55 | [0.22, 1.41] | 1.17 | [0.55, 2.50] | 0.75 | [0.37, 1.55] | −0.27* | [−0.43, −0.11]* |
| Religion | ||||||||
| No religion (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Religion | 0.77 | [0.20, 3.96] | 1.81 | [0.60, 5.48] | 3.63 | [1.28, 10.49]* | 0.08 | [−0.31, 0.15] |
| Education | ||||||||
| No degree (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Bachelor’s degree | 0.73 | [0.20, 2.65] | 0.98 | [0.37, 2.58] | 1.35 | [0.53, 3.46] | 0.20 | [−0.02, 0.42] |
| Advanced degree | 1.39 | [0.27, 7.27] | 0.49 | [0.14, 1.68] | 2.52 | [0.79, 8.03] | 0.17 | [−0.10, 0.44] |
| Known insurance | ||||||||
| No (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 1.12 | [0.35, 3.56] | 0.23* | [0.09, 0.85]* | 0.74 | [0.27, 2.01] | −0.04 | [−0.23, 0.22] |
| Employment | ||||||||
| Unemployed (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Student worker | 4.19 | [0.81, 21.77] | 2.47 | [0.47, 12.92] | 0.60 | [0.13, 2.86] | −0.02 | [−0.36, 0.32] |
| Worker only | 3.36 | [0.80, 14.05] | 2.19 | [0.50, 9.69] | 0.51 | [0.13, 2.00] | −0.11 | [−0.41, 0.19] |
| Retired | 2.05 | [0.11, 37.87] | 0.33 | [0.03, 3.43] | 0.34 | [0.05, 2.38] | −0.03 | [−0.56, 0.36] |
| Income level | 1.00 | [0.73, 1.38] | 0.94 | [0.71, 1.23] | 0.82 | [0.63, 1.06] | 0.06* | [0.00, 0.12]* |
| Medical Mistrust Index | 1.01 | [0.94, 1.08] | 1.03 | [0.97, 1.08] | 1.10* | [1.04, 1.16]* | −0.01 | [−0.02, 0.00] |
| No. of perceived barriers | 0.91 | [0.69, 1.20] | 0.83 | [0.65, 1.05] | 1.01 | [0.81, 1.26] | −0.01 | [−0.06, 0.04] |
| No. of perceived benefits | 1.00 | [0.83, 1.21] | 1.01 | [0.87, 1.17] | 1.00 | [0.87, 1.15] | 0.05* | [0.01, 0.08]* |
| No. of health conditions | 1.41 | [0.84, 2.35] | 1.22 | [0.86, 1.72] | 1.10 | [0.80, 1.50] | 0.04 | [−0.03, 0.11] |
Note. ER = emergency room; OR = odds ratio; CI = confidence interval.
p < .05.
Table 4.
Enabling Factors to Predict Outcomes
| Characteristics | Dr visit within 1 year | ER visit within 1 year | Clinic visit within 1 year | No. of preventive measures within 1 year* | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | Coef. | 95% CI | |
| Known Insurance | ||||||||
| No (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 1.24 | [0.41, 3.73] | 0.32* | [0.12, 0.82]* | 0.81 | [0.32, 2.06] | −0.04 | [−0.26, 0.19] |
| Employment | ||||||||
| Unemployed (ref) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Student worker | 3.11 | [0.66, 14.69] | 1.86 | [0.36, 9.52] | 0.75 | [0.17, 3.25] | 0.01 | [−0.34, 0.31] |
| Worker only | 3.26 | [0.89, 12.01] | 2.20 | [0.50, 9.45] | 0.69 | [0.19, 2.57] | −0.14 | [−0.44, 0.15] |
| Retired | 8.48 | [0.75, 95.46] | 0.66 | [0.08, 5.16] | 0.51 | [0.09, 2.80] | −0.13 | [−0.54, 0.27] |
| Income level | 0.93 | [0.72, 1.21] | 0.88 | [0.71,1.09] | 0.90 | [0.74, 1.10] | 0.05* | [0.00−0.10]* |
| Medical Mistrust Index | 1.00 | [0.94, 1.07] | 1.03 | [0.98, 1.08] | 1.08* | [1.03, 1.13]* | −0.01 | [0.02, 0.00] |
| No. of perceived barriers | 0.89 | [0.86, 1.20] | 0.86 | [0.70, 1.06] | 1.03 | [0.86, 1.25] | 0.01 | [−0.04, 0.05] |
| No. of perceived benefits | 1.01 | [0.16, 17.03] | 0.99 | [0.86, 1.14] | 1.01 | [0.89, 1.15] | 0.05* | [0.02, 0.08]* |
Note. ER = emergency room; OR = odds ratio; CI = confidence interval.
p < .05.
Results
The convenience sample recruitment method using social networks resulted in exceeding the powered sample size of 131 participants and resulted in 176 participants. Five were excluded from participating for either not meeting the age requirement or not identifying as male. Table 1 depicts the descriptive statistics for predisposing, enabling, and need factors of the 176 participants in the study. For enabling factors, the BAA men scored an average of 27 on the MMI with the lowest score being 5 and the highest being 45. BAA men on average identified 1.80 perceived barriers to health care ranging from 0 to 8 with the most common barriers being perceived cost (34%) and not having time (32.4%). Yet, BAA men also identified 4.49 perceived benefits to health care ranging from 0 to 9 with the most prevalent being the feeling of being healthy (76%) and feeling better with more energy (57%). Finally, 80% of BAA men rated their current health status as good or excellent regarding need factors. The average participant also identified at least one health condition, the most prominent being hypertension (19%).
For the outcome variables, the study sample had a comparable engagement with visiting a doctor within the past year with 81.8% among the BAA men compared with 81.7% of BAA men nationally (National Center for Health Statistics, 2022). Nearly half the study sample (49.43%) reported visiting a clinic within the past year, which is considerably higher than the national average of 14% for BAA men. Moreover, a third (31.82%) reported utilizing the ER within the past year, higher than the national average of 23%. For the number of preventive measures used within the past year, findings support reliability of the OMHPSI within this population resulting in a Cronbach’s alpha of .71. Participants reported an average of four preventive measures used within the past year, ranging from 0 to 11. In this sample, the top two preventive measures utilized within the past year were exercise (60% of the BAA men) and annual physicals (53% of the BAA men). Each outcome variable was regressed independently on the predisposing factors, enabling factors, and need factors as shown in Tables 3 to 5. In this independent analysis, older BAA men with more education and religious affiliation engaged in higher levels of preventive health care utilization for predisposing factors. Married BAA men reported engaging in fewer preventive measures in the past year. For enabling factors, BAA men with higher income levels, more perceived benefits to health promoting behaviors, having health insurance, and having higher levels of medical mistrust were associated with higher preventive health care utilization. Finally, for need factors, BAA men reporting more health conditions had higher preventive health care utilization.
Table 2 depicts the results of the full models including predisposing factors, enabling factors, and need factors together as predictors of four outcomes: doctor visit within the past year, ER visit within the past year, clinic visit within the past year, and the number of preventive measures utilized within the past year. Models predicting BAA men’s clinic visits within the past year and the number of preventive measures used within the past year were significant with p < .03. BAA men with religious affiliations were 3.66 times more likely than those who did not report visiting a clinic within the past year (odds ratio [OR] = 3.66, 95% confidence interval [CI] = [1.28, 10.49], p < .02). BAA men with higher medical mistrust had higher likelihood of visiting a clinic within the past year (OR = 1.10, 95% CI = [1.04, 1.16], p < .05). Married BAA men report fewer preventive health measures utilized within the past year (coefficient = −0.28, 95% CI = [−0.45, −0.12], p < .001). Higher income levels (coefficient = 0.07, 95% CI = [0.01, 0.12], p < .03) and higher number of perceived benefits (coefficient = 0.04, 95% CI = [0.01, 0.07], p < .02) were associated with engaging in more preventive health measures within the past year. The models to predict doctor and ER visits within the past year were not significant.
Discussion
This cross-sectional study explores preventive health care utilization among BAA men using the AHM. This study addresses a paucity of data on BAA men’s health by examining predisposing, enabling, and need factors as predictors of preventive health care utilization among BAA men. We found that by grounding our analysis within the AHM, predisposing factors (religious affiliation) and enabling factors (medical mistrust, being married, higher income levels, and a higher number of perceived benefits) significantly predicted BAA men’s preventive health care utilization. Such findings align with the literature as BAA men’s level of medical mistrust, religious affiliation, marital status, and income status have been identified as facilitators or inhibitors of health care utilization (Guner et al., 2018; Khumalo et al., 2021; Luo et al., 2022; Robinson et al., 2018).
The emergence of BAA men’s religious affiliation and higher levels of medical mistrust significantly affect BAA men’s engagement with health care (Arnett et al., 2016; Bazargan et al., 2021; Powell et al., 2019; Williamson et al., 2019). Medical mistrust has been identified as a historical barrier to health care among the BAA community, whereas religion is posited to be a buffer (Bazargan et al., 2021; Bowen-Reid & Harrell, 2002; Mushonga & Henneberger, 2020). Such findings support the understanding that BAA men utilize religion and spirituality as a preferred coping mechanism for health conditions in comparison with seeking traditional health care visits (Namageyo-Funa et al., 2015; Robinson et al., 2018). Research has also shown that religion affected health care utilization, medical mistrust, and the overall health care experience of BAA men (Hankerson et al., 2018; Smith et al., 2022). The lack of a trusting relationship with providers often linked to historical medical mistreatment, discrimination, and unconscious or implicit bias feeds BAA men’s mistrust and positions them to seek other means to cope (Assari, 2018; Marcelin et al., 2019). In addition, research suggests that religion, spirituality, and the quality of the patient–provider relationship influence BAA men’s perception of the health care system (Bukavina et al., 2017; Wallace et al., 2016). Studies have shown that the quality of care received during a regular doctor visit can shape BAA men’s perception of health care and thus influence their likelihood of engaging in health care visits (Chinegwundoh, 2021; Harawa et al., 2013). This suggests that exploring patient–provider interaction may be an important avenue of research in BAA men. Being a provider of health care is no longer limited to having a medical degree but now includes advanced practice practitioners such as physician assistants and nurse practitioners. Their presence in the medical field has shown improved patient education and improved engagement with preventive health care (Park et al., 2020). Positive patient–provider interaction may foster trust in the medical system and improve preventive health care utilization among BAA men.
BAA men’s perceptions of their health and ability to identify or seek help have always been disproportionately lower than that of other racial groups, despite their having higher rates of preventable diseases (Bukavina et al., 2017; Khumalo et al., 2021; Wallace et al., 2016). Historically, BAA men’s self-perception in America is rooted in systemic racism and systemic inequalities found within numerous organizations, including health care institutions (Bazargan et al., 2021; Ferguson, 2000; Greer et al., 2014; Phelan & Link, 2015). As a result, BAA men have an overall perception of their lives and their health through an optimistic or aspirational lens that has roots in religious affiliation (Hankerson et al., 2018; Robinson et al., 2018; Wallace et al., 2016) which were highlighted in this study. One participant reported vision issues, diabetes, urinary complications, and hypertension, yet he still rated his health as “good.” Another participant was currently on dialysis and needed a kidney, yet also rated his health as “good.” A third participant had recently battled with stomach cancer, but stated that because of his faith in God, he rated his health as “excellent.” Regardless of the number of health conditions, 80% of the BAA men in this study rated their health as good or excellent. This lack of variability suggests that self-rated health is not helpful among BAA men; it also speaks to a disconnect between what BAA men perceive as their current health status versus how the health care system defines their condition(s). BAA men and White men have comparable rates of visiting a doctor within the past year, 81.8% and 83.1% respectively, yet BAA men continue to suffer from poorer health outcomes (Bond & Herman, 2016; National Center for Health Statistics, 2022). Although annual doctor visits are the first step, the quality of health education provided during the visit is essential to affect health outcomes (Leitch et al., 2021; Nies & McEwen, 2019). Medical mistrust experienced during the patient–provider interaction is the likely culprit of the noticeable disconnect. Therefore, providers and health care professionals who engage with BAA men in preventive health care utilization can build on the asset-centered nature of how BAA men rate and, therefore, understand their health.
Research shows that cultural congruence with the provider leads to improved patient–provider interaction coupled with improved health care engagement and health outcomes in BAA men (Hannon & Vereen, 2016; Harawa et al., 2013; Watson et al., 2019). Cultural congruence, or shared beliefs and ways of living, allows for a patient’s improved interest and engagement with health resources (Abitz, 2016). Such components enhance the provision of culturally competent care. Trusting in the person giving health information coupled with the level of care being congruent with a person’s cultural needs is key to the administration of culturally competent care (Chinegwundoh, 2021; Nies & McEwen, 2019). Cultural congruence with the researcher may have been an important factor that allowed swift data collection in this study, with the proposed sample size achieved in 2 weeks. There is a need to understand how a lack of adequate assessment and explanation of findings from health providers influences BAA men’s understanding of their health status. More work is needed to explore ways to change BAA men’s health perceptions, and this is likely linked to more cultural congruence with the researcher and practitioners administering health care.
While much of the data from our study aligned with existing literature, one critical area emerged that differed from historical findings related to marriage. It is well known that income and education are two key social determinants of health affecting health care utilization (Nies & McEwen, 2019; Thorpe et al., 2015). BAA men with higher income and education engaged in more preventive measures utilized within the past year following trends within previous studies (Assari et al., 2018; Guzman, 2022; Luo et al., 2022). Research confirms the influence that higher education and income have on BAA men’s understanding of the positive impact of health practices, positioning BAA men for improved access to quality health care related to affordability and health literacy (Bradley et al., 2002; Nies & McEwen, 2019; Suntai et al., 2022). Finally, being married was associated with fewer preventive health measures utilized within the past year. While many studies support the notion that marriage positively influences health-seeking behaviors, studies are beginning to show that marriage is also associated with a decline in physical and mental health practices (Bukavina et al., 2017). COVID-19 is an external factor that potentially influenced the number of preventive measures used among married BAA men as well. While not measured precisely, it is possible that this may have led to less preventive health care utilization as studies have shown delayed, avoided, or limited access to non-COVID health services during the pandemic (Czeisler et al., 2020; Tuczyńska et al., 2021). Future research should focus on a larger representative sample of BAA men to understand the role of marriage in influencing preventive health care utilization.
While this study highlighted some key findings among BAA men that can inform future interventions, there are some fundamental limitations to consider. First, while we quickly achieved our desired sample size, our study sample may have needed to be larger than expected due to the need to dichotomize the outcome variables and use logistic regression when we powered analysis for multiple regression. Therefore, some effects may have yet to be detected. Second, the sample was not representative of BAA men. Men in this study had a higher education and higher income levels while utilizing health care more frequently than the national average. The online nature of the survey attracted people who were more technologically inclined or had more of a social media presence. Future studies can compare cohorts like this with those collected in a more community-centric approach. Like all research recruitment using online sources, there is always the limitation of self-determined alignment with inclusion and exclusion criteria. Efforts were made to ensure eligibility for the study before receipt of the survey; however, the online nature of the survey allowed anyone who identified as a BAA male to participate. Finally, as the study was cross-sectional, we cannot determine the direction of the effects. Despite study limitations, this study unveiled critical information about BAA men’s current preventive health care utilization while identifying the predictive impact of predisposing, enabling, and need factors of the AHM.
Conclusion
This study was one of few to test the tenets of the AHM in a BAA male sample. Findings showed that when all factors of the AHM are used, predisposing, and enabling factors impact the preventive health care utilization of BAA men. Many studies to date pinpoint lack of access or insurance as reasons to explain BAAs’ lack of engagement with health care. This study shows that while the educated predominantly heterosexual high-income sample of BAA men utilized preventive health care within the past year, participant’s perceptions of their health were not in alignment with their current health outcomes. Such findings support the need for improved patient–provider experiences with implications for more culturally congruent care. Research also supports the significance of physician assistants and nurse practitioners and the role they can play in improving health care utilization among BAA men. With providers at the forefront of patient education, they play a vital role in shifting narratives around health care affecting BAA men’s trust in the health care system. Improved trust leads to better communication that can have a significant impact on BAA men’s perceptions of their current health status.
Future studies should evaluate the impact of masculine norms as a potential enabling factor of BAA men’s preventive health care utilization. Aspects of masculinity may prove to be better predictors of preventive health care utilization as studies have shown that conformity to certain masculine norms impact health/help-seeking behaviors (Brown, 2020; Iwamoto et al., 2018; Salgado et al., 2019). BAA men are dying at a faster rate from preventable diseases and conditions with their livelihood depending on identification of appropriate measures to improve their utilization of health care. Findings of this study identify current preventive health care utilization among BAA men based on factors explicating by the AHM. Better understanding of factors that promote or impede BAA men’s preventive health care utilization is a necessity for increased engagement with preventive resources and improved health outcomes.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. This study received ethical approval by the University of Illinois Chicago IRB (Approval # 2022-0187) as a cross sectional study on April 6, 2022. The ethics committee waived the need for ethics approval and the need to obtain consent for the collection, analysis, and publication of this anonymized data for this non-interventional study.
ORCID iDs: Harrell Jordan  https://orcid.org/0009-0008-7237-8826
https://orcid.org/0009-0008-7237-8826
Rohan Jeremiah  https://orcid.org/0000-0003-3774-8816
https://orcid.org/0000-0003-3774-8816
Alicia K. Matthews  https://orcid.org/0000-0002-0074-681X
https://orcid.org/0000-0002-0074-681X
References
- Abitz T. L. (2016). Cultural congruence and infusion nursing practice. Journal of Infusion Nursing, 39(2), 75–79. 10.1097/NAN.0000000000000157 [DOI] [PubMed] [Google Scholar]
- Andersen R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10. [PubMed] [Google Scholar]
- Arnett M. J., Thorpe R. J., Gaskin D. J., Bowie J. V., LaVeist T. A. (2016). Race, medical mistrust, and segregation in primary care as usual source of care: Findings from the exploring health disparities in integrated communities study. Journal of Urban Health, 93(3), 456–467. 10.1007/s11524-016-0054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S. (2018). Interaction between race and gender and effect on implicit racial bias against Blacks. International Journal of Epidemiologic Research, 5(2), 43–49. 10.15171/ijer.2018.10 [DOI] [Google Scholar]
- Assari S., Caldwell C. H. (2017). Mental health service utilization among Black youth; psychosocial determinants in a national sample. Children, 4(5), 1–13. 10.3390/children4050040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S., Lapeyrouse L. M., Neighbors H. W. (2018). Income and self-rated mental health: Diminished returns for high income Black Americans. Behavioral Sciences, 8(5), 1–14. 10.3390/bs8050050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazargan M., Cobb S., Assari S. (2021). Discrimination and medical mistrust in a racially and ethnically diverse sample of California adults. Annals of Family Medicine, 19(1), 4–15. 10.1370/afm.2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond M. J., Herman A. A. (2016). Lagging life expectancy for Black men: A public health imperative. American Journal of Public Health, 106(7), 1167–1169. 10.2105/AJPH.2016.303251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen-Reid T. L., Harrell J. P. (2002). Racist experiences and health outcomes: An examination of spirituality as a buffer. The Journal of Black Psychology, 28(1), 18–36. [Google Scholar]
- Bradley E. H., Mcgraw S. A., Curry L., Buckser A., King K. L., Kasl S. V., Andersen R. (2002). Expanding the Andersen Model: The role of psychosocial factors in long-term care use. HSR: Health Services Research, 37(5), 1221–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown L. E. C. (2020). Eat to live, don’t live to eat: Black men, masculinity, faith and food. International Journal of Environmental Research and Public Health, 17(12), 1–13. 10.3390/ijerph17124264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukavina L., Zaramo C. E. B., Tarabonata L., Modlin C. S. (2017). Perceptions of health-related quality of life: A minority men’s perspective. American Journal of Men’s Health, 11(4), 990–998. 10.1177/1557988315580131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns P. A., Hall C. D. X., Poteat T., Mena L. A., Wong F. Y. (2021). Living while Black, gay and poor: The association of race, neighborhood structural disadvantage, and PreP utilization among a sample of Black men who have sex with men in the Deep South. AIDS Education and Prevention, 33(5), 395–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022). HIV and Black/African American people in the U.S. https://www.cdc.gov/nchhstp/newsroom/fact-sheets/hiv/black-african-american-factsheet.html
- Chinegwundoh F. I. (2021). The relationship between Black men with prostate cancer and their health-care providers. Nature Reviews Urology, 18(12), 701–702. 10.1038/s41585-021-00525-6 [DOI] [PubMed] [Google Scholar]
- Czeisler M. É., Marynak K., Clarke K. E. N., Salah Z., Shakya I., Thierry J. M., Ali N., Mcmillan H., Wiley J. F., Weaver M. D., Czeisler C. A., Rajaratnam S., Howard M. E. (2020). Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. Morbidity and Mortality Weekly Report, 69(36), 1250–1257. 10.1101/2020.04.22.20076141v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale S. K., Bogart L. M., Wagner G. J., Galvan F. H., Klein D. J. (2016). Medical mistrust is related to lower longitudinal medication adherence among African-American males with HIV. Journal of Health Psychology, 21(7), 1311–1321. 10.1177/1359105314551950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson A. A. (2000). Bad boys: Public schools in the making of black masculinity. University of Michigan Press. [Google Scholar]
- Go A. S., Mozaffarian D., Roger V. L., Benjamin E. J., Berry J. D., Borden W. B., Bravata D. M., Dai S., Ford E. S., Fox C. S., Franco S., Fullerton H. J., Gillespie C., Hailpern S. M., Heit J. A., Howard V. J., Huffman M. D., Kissela B. M., Kittner S. J., . . .Turner M. B. (2013). Heart disease and stroke statistics-2013 update: A Report from the American Heart Association. Circulation, 127(1), e6–e245. 10.1161/CIR.0b013e31828124ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer T. M., Brondolo E., Brown P. (2014). Systemic racism moderates effects of provider racial biases on adherence to hypertension treatment for African Americans. Health Psychology, 33(1), 35–42. 10.1037/a0032777 [DOI] [PubMed] [Google Scholar]
- Griffith D. M., Brinkley-Rubinstein L., Bruce M. A., Thorpe R. J., Metzl J. M. (2015). The interdependence of African American men’s definitions of manhood and health. Family and Community Health, 38(4), 284–296. 10.1097/FCH.0000000000000079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman D. C., Curry S. J., Owens D. K., Bibbins-Domingo K., Caughey A. B., Davidson K. W., Doubeni C. A., Ebell M., Epling J. W., Kemper A. R., Krist A. H., Kubik M., Seth Landefeld C., Mangione C. M., Silverstein M., Simon M. A., Siu A. L., Tseng C. W. (2018). Screening for prostate cancer: US preventive services task force recommendation statement. Journal of the American Medical Association, 319(18), 1901–1913. 10.1001/jama.2018.3710 [DOI] [PubMed] [Google Scholar]
- Guner N., Kulikova Y., Llull J. (2018). Marriage and health: Selection, protection, and assortative mating. European Economic Review, 104, 138–166. 10.1016/j.euroecorev.2018.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzman G. (2022). Household income: 2021. www.census.gov/
- Haidar A., Nwosisi E., Burnett-Zeigler I. (2023). The role of religion and spirituality in adapting mindfulness-based interventions for Black American communities: A scoping review. Mindfulness, 14(8), 1852–1867. 10.1007/s12671-023-02194-5 [DOI] [Google Scholar]
- Hankerson S. H., Lee Y. A., Brawley D. K., Braswell K., Wickramaratne P. J., Weissman M. M. (2015). Screening for depression in African-American churches. American Journal of Preventive Medicine, 49(4), 526–533. 10.1016/j.amepre.2015.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankerson S. H., Svob C., Jones M. K. (2018). Partnering with black churches to increase access to care. Psychiatric Services, 69(2), 125. 10.1176/appi.ps.69201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannon M. D., Vereen L. G. (2016). Irreducibility of Black male clients: Considerations for culturally competent counseling. Journal of Humanistic Counseling, 55(3), 234–245. 10.1002/johc.12036 [DOI] [Google Scholar]
- Harawa N. T., Williams J. K., McCuller W. J., Ramamurthi H. C., Lee M., Shapiro M. F., Norris K. C., Cunningham W. E. (2013). Efficacy of a culturally congruent HIV risk-reduction intervention for behaviorally bisexual Black men: Results of a randomized trial. AIDS, 27(12), 1979–1988. 10.1097/QAD.0b013e3283617500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess K. L., Hu X., Lansky A., Mermin J., Hall H. I. (2017). Lifetime risk of a diagnosis of HIV infection in the United States. Annals of Epidemiology, 27(4), 238–243. 10.1016/j.annepidem.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto D. K., Brady J., Kaya A., Park A. (2018). Masculinity and depression: A longitudinal investigation of multidimensional masculine norms among college men. American Journal of Men’s Health, 12(6), 1873–1881. 10.1177/1557988318785549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khumalo S., Mabaso M., Makusha T., Taylor M. (2021). Narratives of young Black men on barriers to health care and poor health care seeking behaviours at a university setting: A qualitative study. BMC Health Services Research, 21(1), Article 445. 10.1186/s12913-021-06470-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laveist T. A., Isaac L. A., Williams K. P. (2009). Mistrust of health care organizations is associated with underutilization of health services. Health Services Research, 44(6), 2093–2105. 10.1111/j.1475-6773.2009.01017.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitch S., Corbin J., Boston-Fisher N., Ayele C., Delobelle P., Gwanzura Ottemöller F., Matenga T., Mweemba O., Pederson A., Wicker J. (2021). Black lives matter in health promotion: Moving from unspoken to outspoken. Health Promotion International, 36(4), 1160–1169. 10.1093/heapro/daaa121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillard J. W., Moses K. A., Mahal B. A., George D. J. (2022). Racial disparities in Black men with prostate cancer: A literature review. Cancer, 128(21), 3787–3795. 10.1002/cncr.34433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb S. J. (2003). The Older Men’s Health Program and Screening Inventory: A tool for assessing health practices and beliefs. Geriatric Nursing, 24(5), 278–285. [DOI] [PubMed] [Google Scholar]
- Loeb S. J., Steffensmeier D., Lawrence F. (2008). Comparing incarcerated and community-dwelling older men’s health. Western Journal of Nursing Research, 30(2), 234–249. 10.1177/0193945907302981 [DOI] [PubMed] [Google Scholar]
- Luo J., Hendryx M., Wang F. (2022). Mortality disparities between Black and White Americans mediated by income and health behaviors. SSM—Population Health, 17, 101019. 10.1016/j.ssmph.2021.101019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maina I. W., Belton T. D., Ginzberg S., Singh A., Johnson T. J. (2018). A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science and Medicine, 199, 219–229. 10.1016/j.socscimed.2017.05.009 [DOI] [PubMed] [Google Scholar]
- Marcelin J. R., Siraj D. S., Victor R., Kotadia S., Maldonado Y. A. (2019). The impact of unconscious bias in healthcare: How to recognize and mitigate it. Journal of Infectious Diseases, 220, S62–S73. 10.1093/infdis/jiz214 [DOI] [PubMed] [Google Scholar]
- Meyers-Pantele S. A., Sullivan P., Mansergh G., Hirshfield S., Stephenson R., Horvath K. J. (2022). Race-based medical mistrust, HIV-related stigma, and ART adherence in a diverse sample of men who have sex with men with HIV. AIDS and Behavior, 26(5), 1456–1466. 10.1007/s10461-021-03500-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mushonga D. R., Henneberger A. K. (2020). Protective factors associated with positive mental health in traditional and nontraditional Black students. American Journal of Orthopsychiatry, 90(1), 147–160. 10.1037/ort0000409 [DOI] [PubMed] [Google Scholar]
- Namageyo-Funa A., Muilenburg J., Wilson M. (2015). The role of religion and spirituality in coping with type 2 diabetes: A qualitative study among Black men. Journal of Religion and Health, 54(1), 242–252. 10.1007/s10943-013-9812-0 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2022). Percentage of having a doctor visit for any reason in the past 12 months for adults aged 18 and over, United States, 2021. Centers for Disease Control and Prevention. https://wwwn.cdc.gov/NHISDataQueryTool/SHS_adult/index.html [Google Scholar]
- National Center for Health Statistics—Division of Health Interview Statistics. (2020). 2020 National Health Interview Survey (NHIS) questionnaire contents. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2020/EnglishQuest-508.pdf
- Nies M. A., McEwen M. (2019). Community/public health nursing: Promoting the health of populations (7th ed.). Elsevier. [Google Scholar]
- Park J., Han X., Pittman P. (2020). Does expanded state scope of practice for nurse practitioners and physician assistants increase primary care utilization in community health centers? Journal of the American Association of Nurse Practitioners, 32(6), 447–458. 10.1097/JXX.0000000000000263 [DOI] [PubMed] [Google Scholar]
- Parker L. J., Hunte H., Ohmit A., Thorpe R. J. (2017). Factors associated with Black men’s preference for health information. Health Promotion Practice, 18(1), 119–126. 10.1177/1524839916664488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan J. C., Link B. G. (2015). Is racism a fundamental cause of inequalities in health? Annual Review of Sociology, 41, 311–330. 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- Powell W., Adams L. B., Cole-Lewis Y., Agyemang A., Upton R. D. (2016). Masculinity and race-related factors as barriers to health help-seeking among African American men. Behavioral Medicine, 42(3), 150–163. 10.1080/08964289.2016.1165174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell W., Richmond J., Mohottige D., Yen I., Joslyn A., Corbie-Smith G. (2019). Medical mistrust, racism, and delays in preventive health screening among African-American men. Behavioral Medicine, 45(2), 102–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M. A., Jones-Eversley S., Moore S. E., Ravenell J., Adedoyin A. C. (2018). Black male mental health and the Black church: Advancing a collaborative partnership and research agenda. Journal of Religion and Health, 57(3), 1095–1107. 10.1007/s10943-018-0570-x [DOI] [PubMed] [Google Scholar]
- Rogers C. R., Rogers T. N., Matthews P., Le Duc N., Zickmund S., Powell W., Thorpe R. J., McKoy A., Davis F. A., Okuyemi K., Paskett E. D., Griffith D. M. (2022). Psychosocial determinants of colorectal cancer screening uptake among African-American men: Understanding the role of masculine role norms, medical mistrust, and normative support. Ethnicity & Health, 27, 1103–1122. 10.1080/13557858.2020.1849569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado D. M., Knowlton A. L., Johnson B. L. (2019). Men’s health-risk and protective behaviors: The effects of masculinity and masculine norms. Psychology of Men and Masculinity, 20(2), 266–275. 10.1037/men0000211 [DOI] [Google Scholar]
- Smith M. L., Bergeron C. D., Sherman L. D., Goidel K., Merianos A. L. (2022). Contextualizing the chronic care model among non-Hispanic Black and Hispanic Men with chronic conditions. International Journal of Environmental Research and Public Health, 19(6), 3655. 10.3390/ijerph19063655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soper D. S. (2022). A-priori sample size calculator for multiple regression [Software]. https://www.danielsoper.com/statcalc
- Suntai Z., Noh H., Won C. R. (2022). Examining racial differences in the informal discussion of advance care planning among older adults: Application of the Andersen Model of Health Care Utilization. Journal of Applied Gerontology, 41(2), 371–379. 10.1177/0733464821993610 [DOI] [PubMed] [Google Scholar]
- Tabaac A. R., Solazzo A. L., Gordon A. R., Austin S. B., Guss C., Charlton B. M. (2020). Sexual orientation-related disparities in healthcare access in three cohorts of U.S. adults. Preventive Medicine, 132, 105999. 10.1016/j.ypmed.2020.105999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe R. J., Kennedy-Hendricks A., Griffith D. M., Bruce M. A., Coa K., Bell C. N., Young J., Bowie J. V., LaVeist T. A. (2015). Race, social and environmental conditions, and health behaviors in men. Family and Community Health, 38(4), 297–306. 10.1097/FCH.0000000000000078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuczyńska M., Matthews-Kozanecka M., Baum E. (2021). Accessibility to non-COVID health services in the world during the COVID-19 pandemic: Review. Frontiers in Public Health, 9, 1–7. 10.3389/fpubh.2021.760795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UCLA: Statistical Consulting Group. (2022). Poisson regression: Stata data analysis examples. https://stats.oarc.ucla.edu/stata/dae/poisson-regression/
- U.S. Department of Health and Human Services. (2022, March 17). About the ACA: Young adult coverage. https://www.hhs.gov/healthcare/about-the-aca/young-adult-coverage/index.html
- Wallace S. A., Sloan Strike K., Yonnette Marcia Glasgow M., Kailyn Lynch Robert Fullilove M. E., Marcia Glasgow Y. (2016). “Other than that, I’m good”: Formerly incarcerated young Black men’s self-perceptions of health status. Journal of Health Care for the Poor and Underserved, 27, 163–180. [DOI] [PubMed] [Google Scholar]
- Watson K. S., Henderson V., Murray M., Murphy A. B., Levi J., Ben McDowell T., Holloway-Beth A., Gogana P., Dixon M. A., Moore L., Hall I., Kimbrough A., Molina Y., Winn R. A. (2019). Engaging African American men as citizen scientists to validate a prostate cancer biomarker: Work-in-progress. Progress in Community Health Partnerships: Research, Education, and Action, 13, 103–112. 10.1353/cpr.2019.0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson L. D., Smith M. A., Bigman C. A. (2019). Does discrimination breed mistrust? Examining the role of mediated and non-mediated discrimination experiences in medical mistrust. Journal of Health Communication, 24(10), 791–799. 10.1080/10810730.2019.1669742 [DOI] [PubMed] [Google Scholar]