Abstract
Background
Constipation is a common problem in late pregnancy. Circulating progesterone may be the cause of slower gastrointestinal movement in mid and late pregnancy.
Objectives
The objective of this review was to assess the effects of different methods for treating constipation in pregnancy.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group trials register, the Cochrane Controlled Trials Register and MEDLINE. Date of last search: January 2001.
Selection criteria
Randomised trials of any treatment for constipation in pregnancy.
Data collection and analysis
Trial quality assessments and data extraction were done independently by two reviewers.
Main results
Two suitable trials were identified. Fibre supplements increased the frequency of defecation (odds ratio 0.18, 95% confidence interval 0.05 to 0.67), and lead to softer stools. Stimulant laxatives are more effective than bulk‐forming laxatives (odds ratio 0.30, 95% confidence interval 0.14 to 0.61), but may cause more side effects.
Authors' conclusions
Dietary supplements of fibre in the form of bran or wheat fibre are likely to help women experiencing constipation in pregnancy. If the problem fails to resolve, stimulant laxatives are likely to prove more effective.
Keywords: Female, Humans, Pregnancy, Dietary Fiber, Dietary Supplements, Constipation, Constipation/therapy, Pregnancy Complications, Pregnancy Complications/therapy, Randomized Controlled Trials as Topic
Plain language summary
Interventions for treating constipation in pregnancy
Mild laxatives help relieve constipation in pregnancy.
Constipation is a common problem in late pregnancy. The time taken for food to get through the gut to the bowel is increased in the second and third trimester and may be caused by an increase in the hormone, progesterone. Adding more fibre to the diet increases the frequency of defecation (bowel movement) and leads to softer stools. The review of trials found that laxatives which stimulate the bowel are more effective than those that add bulk but may cause more adverse effects such as diarrhoea and abdominal pain. Fibre supplements are effective and appear to have no adverse effects.
Background
The prevalence of constipation in pregnancy is reported to be 11‐38%. It appears to be a problem of gastrointestinal motility, since there is an increase in gut transit time in the second and third trimester compared with both the first trimester and the postpartum period. As with heartburn of pregnancy, the likely cause is the rising level of circulating progesterone (West 1992).
Objectives
To assess the effectiveness of different methods for treating constipation in pregnancy.
Methods
Criteria for considering studies for this review
Types of studies
All acceptably controlled trials evaluating treatments for constipation in pregnancy.
Types of participants
Pregnant women complaining of constipation, however defined, either spontaneously or in response to specific questioning.
Types of interventions
Any interventions intended to increase the frequency or ease of defecation.
Types of outcome measures
Changes in the frequency or ease of defecation.
Search methods for identification of studies
Electronic searches
This review has drawn on the search strategy for the Pregnancy and Childbirth Group as a whole. See Review Group's details for more information. In addition, MEDLINE and the Cochrane Controlled Trials Register were searched using the terms 'constipat*' and 'pregnan*'. Date of last search: January 2001.
Data collection and analysis
Trials under consideration were evaluated for methodological quality and appropriateness for inclusion, without consideration of their results. Included trial data were processed as described in Clarke 2000.
All studies were read by both reviewers, who made independent assessments of quality of allocation concealment and who extracted data independently. Disagreements were resolved by discussion.
In the two included trials the numbers in each treatment group were small and there were no significant differences between different treatments of the same type (corn‐based biscuits compared with wheat bran in Anderson 1985; senna compared with dioctyl sodium succinate and sterculia alone compared with sterculia and frangula in Greenhalf 1973). For this reason the two groups in each case have been combined (fibre supplements in Anderson 1985; stimulant laxatives and bulk‐forming laxatives respectively in Greenhalf 1973).
Results
Description of studies
Two trials were found that met the inclusion criteria and provided data that could be used in a meta‐analysis. Two others have been excluded as their results were not usable. See tables of included and excluded studies.
Risk of bias in included studies
Anderson 1985 was a trial of fibre supplements in 40 ambulant women. The control group was not given any placebo preparation, but the authors note the difficulty of providing a suitable preparation in such trials. The other trial compared two different stimulant laxatives with two different bulk‐forming laxatives; there was no control group without laxatives (Greenhalf 1973). It is of moderate quality: details are not given of the method of randomisation although it is stated that researchers were blind to the type of intervention. There is also inadequate information about numbers, with the paper reporting recruitment of 175 women but data only given for 140.
Effects of interventions
There is clear evidence of the effectiveness of fibre supplements on the frequency of defecation (odds ratio (OR) 0.18, 95% confidence interval (CI) 0.05‐0.67). Participants also reported a change to softer faeces. The finding is supported by Gregersen 1985, which reported a statistically significant improvement of frequency of defecation in women in the treated group compared with those in the control group. Browne 1957 reported an increase in frequency in response to a single dose of 7.5 mg of senna (a small dose compared with current standard clinical practice), when compared with a placebo syrup. Greenhalf 1973 demonstrated that stimulant laxatives are more effective than bulk forming laxatives (OR 0.30, 95% CI 0.14 to 0.61). They are at the same time more likely to cause side effects of diarrhoea and abdominal pain. The acceptability is the same between the two groups, with effectiveness and side effects apparently balancing out in patients' reactions (Greenhalf 1973).
Discussion
The findings of these two small trials and the excluded trials are consistent with what is known about laxatives in non‐pregnant patients. Fibre supplements are effective, and raise no serious concerns about side effects to mother or fetus. Stimulant laxatives are more effective than bulk‐forming laxatives but are more likely to cause side‐effects that reduce their acceptability to patients.
Authors' conclusions
Implications for practice.
Women complaining of constipation in pregnancy can be treated effectively with daily dietary supplements of fibre in the form of bran or wheat fibre. If these are ineffective, stimulant laxatives may be effective.
Implications for research.
Besides the meagre data presented in this review about effectiveness, little is known about the long‐term acceptability of daily fibre supplements to women, or about the relative effectiveness and acceptability of other common treatments for constipation such as increased exercise. There may therefore be an argument for carrying out further research to identify the most acceptable, as well as the most effective treatment.
Feedback
Herxheimer, September 1998
Summary
Summary of analyses: Anderson 1985 was a three arm study, and the two groups given dietary fibre are combined within the review. Lumping in this way should be justified, and the groups reported separately as well as together.
Results: If there is any information about acceptability and patient preferences for any of the groups this should also be presented. Absolute numbers of defecations/day would also be useful information.
Reply
Summary of analyses: In Anderson 1985 the active ingredient for the two dietary fibre groups was the same, although the formulation was different. As formulation alone would be unlikely to influence the effect, lumping is justified. It also gives a more useful result. Data on similar laxatives from Greenhalf 1973 have also been lumped. Text in the results section and table of included references make this explicit.
Results: None of these papers report any data on numbers of defecations. Data on acceptability was reported in Greenhalf 1973 and has been included in the review.
Contributors
Summary of comments from Andrew Herxheimer, September 1998. Summary of response from David Jewell, January 2001.
What's new
| Date | Event | Description |
|---|---|---|
| 7 September 2015 | Amended | Text has been added to Published notes to explain that this review will not be updated and has been superseded by Rungsiprakarn 2015. |
History
Protocol first published: Issue 3, 1997 Review first published: Issue 3, 1998
| Date | Event | Description |
|---|---|---|
| 18 January 2012 | Amended | Contact details updated. |
| 11 September 2008 | Amended | Converted to new review format. |
| 26 February 2001 | New search has been performed | Search updated. |
| 26 February 2001 | New citation required but conclusions have not changed | An additional study (Greenhalf 1973) has been incorporated into this review and the text has been altered in response to a comment from Andrew Herxheimer. |
| 15 January 2001 | Feedback has been incorporated | Response to feedback added. |
Notes
This review will no longer be updated by the current review team and has been superseded by a new review on this topic, see Rungsiprakarn 2015.
Acknowledgements
None.
Data and analyses
Comparison 1. Effect of additional dietary fibre.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 No increased frequency of defecation | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.18 [0.05, 0.67] |
1.1. Analysis.
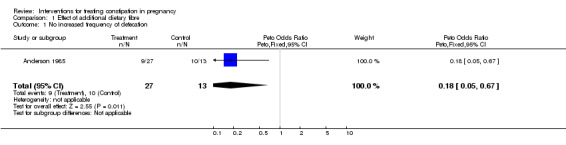
Comparison 1 Effect of additional dietary fibre, Outcome 1 No increased frequency of defecation.
Comparison 2. Comparison of stimulant laxatives with bulk‐forming laxatives.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Effect on constipation not resolved | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.14, 0.61] |
| 2 Treatment not acceptable to women | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.46, 1.73] |
| 3 Effect on side effects | 1 | 420 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.27, 3.41] |
| 3.1 Side effects: abdominal pain | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.91 [1.39, 6.11] |
| 3.2 Side effects: diarrhoea | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.90 [1.22, 6.91] |
| 3.3 Side effects: nausea | 1 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.13, 1.64] |
2.1. Analysis.
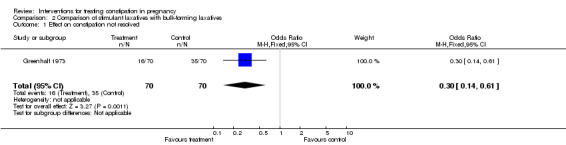
Comparison 2 Comparison of stimulant laxatives with bulk‐forming laxatives, Outcome 1 Effect on constipation not resolved.
2.2. Analysis.
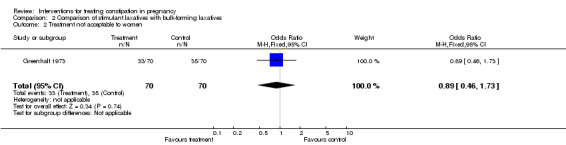
Comparison 2 Comparison of stimulant laxatives with bulk‐forming laxatives, Outcome 2 Treatment not acceptable to women.
2.3. Analysis.
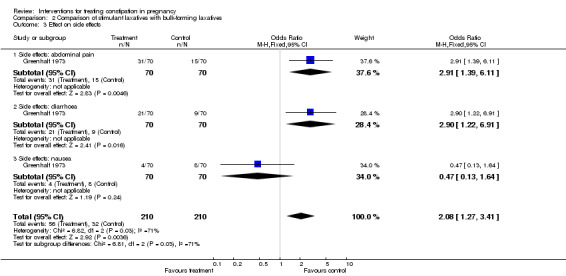
Comparison 2 Comparison of stimulant laxatives with bulk‐forming laxatives, Outcome 3 Effect on side effects.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anderson 1985.
| Methods | Women randomised into three groups, method of randomisation not stated. | |
| Participants | 40 women recruited from routine antenatal clinics in the third trimester of pregnancy. Women recruited in last trimester from antenatal clinics in Cambridge, UK. | |
| Interventions | Women in two intervention groups given 10gm dietary supplement per day, either in the form of corn‐based biscuits (proprietary product 'Fibermed') or as 23g wheat bran. Control group given nothing (ie not a placebo group), all for two weeks. | |
| Outcomes | Increase in stool frequency over two weeks of treatment. | |
| Notes | Energy and fibre intake were carefully monitored throughout the study. There were no differences in outcomes between the two treatment groups. This is unsurprising since the two treatments are different forms of fibre (ie the same type of laxative). For these reasons the two treatment groups have been combined in the meta‐analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Greenhalf 1973.
| Methods | Women randomised into four groups, method not stated. | |
| Participants | Women attending hospital antenatal clinic in UK. 175 women recorded as being entered, but data only available for 140 (35 in each group). | |
| Interventions | Groups given oral medication as follows: 1. Senna 14mg daily (Senokot). 2. Dioctyl sodium succinate 120mg and dihydroxyanthroquinone 100mg (Normax). 3. 10ml daily, containing 60% sterculia and 8% frangula (Normacol standard). 4. 10ml daily, containing 60% sterculia (Normacol special). | |
| Outcomes | Failure to correct constipation; poor acceptability of preparation; side effects. | |
| Notes | For the meta‐analysis groups 1 and 2 have been combined as stimulant laxatives and groups 3 and 4 as bulk‐forming laxatives. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Browne 1957 | Double‐blind randomised controlled trial, studying pregnant women admitted to hospital. Trial of different preparations and doses of senna. At higher doses (equivalent to 7.5 mg daily) increase in frequency of defecation noted within 24 hours of dose. However, results only presented as means for each treatment group. |
| Gregersen 1985 | Randomised double‐blind controlled study of constipation treated with fibre tablets (Dumovital) or placebo. The paper reported an increase in frequency of defecation in the fibre tablet group. Data only presented as means for the whole group, and therefore impossible to know how many patients recovered in each group. |
Contributions of authors
Both reviewers read the papers and agreed extraction and interpretation of data. David Jewell was responsible for all data entry and writing the review.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Anderson 1985 {published data only}
- Anderson AS, Whichelow MJ. Constipation during pregnancy: dietary fibre intake and the effect of fibre supplementation. Human Nutrition: Applied Nutrition 1985;39:202‐7. [PubMed] [Google Scholar]
Greenhalf 1973 {published data only}
- Greenhalf JO, Leonard HSD. Laxatives in the treatment of constipation in pregnant and breast‐feeding mothers. Practitioner 1973;210:259‐63. [PubMed] [Google Scholar]
References to studies excluded from this review
Browne 1957 {published data only}
- Browne JCM, Edmunds V, Fairbairn JW, Reid DD. Clinical and laboratory assessments of senna preparations. British Medical Journal 1957;23:436‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gregersen 1985 {published data only}
- Gregersen E. Constipation during pregnancy. Treatment with Dumovital fibre tablets [translation]. Ugeskrift for Laeger 1985;147:91‐3. [PubMed] [Google Scholar]
Additional references
Clarke 2000
- Clarke M, Oxman AD, editors. Cochrane Reviewers' Handbook 4.1 [updated June 2000]. In: Review Manager (RevMan) [Computer program]. Version 4.1 Oxford, England: The Cochrane Collaboration, 2000.
Rungsiprakarn 2015
- Rungsiprakarn P, Laopaiboon M, Sangkomkamhang US, Lumbiganon P, Pratt JJ. Interventions for treating constipation in pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 9. [DOI: 10.1002/14651858.CD011448.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
West 1992
- West L, Warren J, Cutts T. Diagnosis and management of irritable bowel syndrome, constipation, and diarrhoea in pregnancy. Gastroenterology Clinics of North America 1992;21(4):793‐802. [PubMed] [Google Scholar]
References to other published versions of this review
CDSR 2001
- Jewell DJ, Young G. Interventions for treating constipation in pregnancy (Cochrane Review). The Cochrane Library 2001, Issue 1. [DOI] [PubMed] [Google Scholar]
Jewell 1995
- Jewell MD. Treatments for constipation in pregnancy. [revised 30 April 1993] In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C (eds.) Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM]. The Cochrane Collaboration; Issue 2, Oxford: Update Software; 1995.


