Abstract
Introduction
The COVID-19 pandemic has been associated with a substantial rise in mental health challenges, prompting a need for accessible and effective therapeutic interventions. This review summarizes the evidence on remote Eye Movement Desensitization and Reprocessing (EMDR) therapy delivered in response to the increased need.
Methods
A systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Databases including PsychINFO, EMBASE, MEDLINE, and Web of Science were searched to identify studies assessing the efficacy of EMDR therapy administered online.
Results
Sixteen articles meeting the inclusion criteria were selected, involving 1,231 participants across various age groups. Studies covered remote individual and group EMDR sessions and self-administered computerized protocols. Findings indicate promising outcomes in reducing PTSD symptoms, anxiety, and depression.
Discussion
The analysis of the selected studies demonstrates the feasibility and potential efficacy of online EMDR as an accessible therapeutic option for addressing mental health difficulties, particularly during times of limited in-person interaction. However, the studies revealed limitations such as small sample sizes, absence of control groups, and reliance on self-reported measures.
Systematic review registration: The present review was registered on “The International Database to Register Your Systematic Reviews” (INPLASY) with the registration number 2023120018 and DOI number 10.37766/inplasy2023.2.0068.
Keywords: EMDR therapy, online therapy, mental health, online EMDR, remote EMDR, self-help
1. Introduction
The COVID-19 pandemic has been associated with a significant increase in mental health difficulties, including post-traumatic stress, anxiety, and depression (1). Studies have indicated that individuals reporting symptoms of anxiety or depression were more prone to severe COVID-19 outcomes (2). Further research has shown that individuals who contracted COVID-19 also experienced elevated levels of anxiety, depression, post-traumatic symptoms, and other difficulties (3, 4).
The pandemic affected mental health through different factors such as isolation, financial instability, grief, suicide, and substance use (5). Different psychological impacts persisted, leading to fatigue, cognitive impairments, and ongoing mental health difficulties even in many post-infection cases (6). Specific groups, including racial and ethnic minorities, displaced groups, individuals with financial insecurity, children, people with disabilities, and those with preexisting conditions, faced an even more heightened risk (7). Essential workers, for example, experienced worsened mental health due to the increased risk of contracting or becoming severely ill from COVID-19 (3).
The global increase in mental health difficulties during the pandemic was met with limited access to mental health services and resources due to restrictions such as lockdowns or the prioritization of other health services. The disruptions caused by COVID-19 led to a decrease in access to outpatient mental health care, reduced admissions, and earlier discharge from inpatient care (8). In European countries where rates of depression and anxiety among the general population are high, long waiting lists have been identified as a barrier to mental health services (9, 10).
In response to these challenges, there was a shift towards providing remote services and using technology in mental health care. Digital tools have supported mental health services for over two decades. However, the COVID-19 pandemic created a unique need for greater utilization of these digital technologies to offer effective and timely solutions that scale up and decentralize health care across a wide variety of platforms, including teletherapy, mHealth (mobile health) applications, and web-based interventions or self-help tools (11–13).
Eye Movement Desensitization and Reprocessing (EMDR) is a psychotherapy designed to alleviate distress associated with traumatic memories. It involves attention to three time periods: the past, present, and future, with a focus on past disturbing memories and related events (14). EMDR therapy is an eight-phase treatment that uses eye movements (or other bilateral stimulation) during one part of the session (15, 16). Research indicates that EMDR therapy can be an effective treatment for difficulties such as anxiety, depression, chronic pain, addictions, and other distressing life experiences (17–23).
With the emergence of the COVID-19 pandemic, like other forms of therapy, online EMDR therapy has gained widespread popularity. Following the widespread application, many EMDR organizations such as EMDR Europe, EMDR Association UK, and EMDR International Association (EMDRIA) have issued guidelines offering specific recommendations regarding security, therapeutic considerations, and client selection in this context (24). Qualitative studies have also shed light on the feasibility and accessibility of online EMDR therapy during the pandemic. For example, in a study conducted in the UK with therapists, most participants expressed high comfort in receiving EMDR therapy online (25). It suggested many therapists who were initially hesitant about doing EMDR therapy online decreased considerably within the first year of the pandemic. Moreover, four-fifths of therapists intended to continue offering online therapy even after pandemic restrictions were lifted. The number of therapists not delivering any EMDR therapy sessions online decreased significantly, and this trend continued to decline thereafter. In another study (26), some clinicians initially expressed questions about engaging in EMDR therapy, mainly due to the physicality involved, such as the bilateral stimulation. Despite their initial hesitation, clinicians recognized the value of integrating EMDR into their therapeutic toolkit and highlighted the significance of employing such approaches when working with clients under different circumstances.
The effectiveness of online Eye Movement Desensitization and Reprocessing (EMDR) is not well-established, with previous systematic reviews and meta-analyses concentrating on face-to-face applications. A notable gap exists in the literature regarding a systematic review summarizing the evidence for online EMDR. This review aims to fill this gap by focusing on remote EMDR interventions, contributing valuable insights to the existing literature (See Table 1).
Table 1.
Study characteristics.
| Authors | N in EMDR | Sample group | Study design | Comparison group | Type of protocol | Facilitator | Delivery format | Number of sessions | Longest follow up |
|---|---|---|---|---|---|---|---|---|---|
| Bates et al., 2022 | 13 | Adults Mean age not specified | RCT | Usual care | R-TEP | EMDR therapists | Individual live sessions | Up to 8 | 6 months |
| Farrell et al., 2023 | 95 | Frontline healthcare workers Mean age not specified | RCT | A delayed treatment | G-TEP | EMDR therapists | Group live sessions (6 participants) | 4 sessions | 6 months |
| Moench et al., 2021 | 34 | Healthcare workers Mean age not specified | RCT | A delayed treatment | STEP | NA | Self-administered computerized sessions | Single session | NA |
| Clarke, 2022 | 1 | Adults Mean age not specified | Single arm | Pre-post | R-TEP | EMDR therapists | Individual live sessions | 9 sessions | 4 months |
| Faretta et al., 2022 | 11 | Frontline healthcare workers 7 females 4 males Mean age not specified | Single arm | Pre-post | IGTP | EMDR therapists | Group live sessions | 3 sessions | 9 months |
| Farrell et al., 2022 | 24 | Frontline healthcare workers Mean age not specified | Single arm | Pre-post | Blind 2 Therapist | EMDR therapists | Individual live sessions | Single session | 6 months |
| Fernandez et al., 2022 | 587 | Frontline healthcare workers 433 females 154 males, Mean age 45.5 | Single arm | Pre-post | IGTP | EMDR therapists | Group live sessions (4–6 participants) | 3 sessions | NA |
| Goga et al., 2022 | 31 | Adults 14 males 17 females Mean age 26.2 | Single arm | Pre-post | Standard EMDR | NA | Self-administered computerized sessions | Single session | NA |
| Lazzaroni et al., 2021 | 50 | Adolescents and young adults Aged 13 to 24 years Mean age not specified | Single arm | Pre-post | R-TEP | EMDR therapists | Group live sessions (6 participants) | 3 sessions | NA |
| McGowan et al., 2021 | 93 | Adolescents and Adults 10 to 72 years Mean age 35.5 | Single arm | Pre-post | Standard EMDR | EMDR therapists with an average experience of 8.5 years | Individual live sessions | Unclear | NA |
| Mischler et al., 2021 | 76 | Adults 18 to 68 years Mean age 41 | Single arm | Pre-post | Standard EMDR | EMDR therapists with an average experience of 10.7 years | Individual live sessions | On average, patients had received 4.84 eEMDR sessions (SD = 5.28, range = 0–30) | NA |
| Morris et al., 2022 | 12 | Healthcare workers Mean age not specified | Single arm | Pre-post | R-TEP | EMDR therapists | Individual live sessions | ||
| Perri et al., 2021 | 19 | Adults males Mean age 48.3 | Single arm | Pre-post | R-TEP | EMDR therapists | Individual live sessions | 7 sessions | 1 month |
| Sagaltici et al., 2022 | 14 | Healthcare workers 3 males 11 females Mean age not specified | Single arm | Pre-post | R-TEP | EMDR therapists | Individual live sessions | 5 sessions | 1 month |
| Tarquinio et al., 2020 | 17 | Healthcare workers 17 females Mean age 33.2 | Single arm | Pre-post | URG-EMDR protocol | EMDR therapists | Individual live sessions | Single session | NA |
| Yurtsever et al., 2022 | 154 | Frontline workers Mean age not specified | Single arm | Pre-post | R-TEP | EMDR therapists | Individual live sessions | 5 sessions | 1 month |
2. Methods
2.1. Design
The protocol of the present systematic review was registered retrospectively on “The International Database to Register Your Systematic Reviews” (INPLASY) with the registration number 2023120018 and DOI number 10.37766/inplasy2023.12.0018. The study was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (27). The purpose of this review was to comprehensively summarize the effectiveness of EMDR therapy based on existing literature. The inclusion criteria encompassed studies that assessed the efficacy of any EMDR, provided that EMDR sessions were delivered online and the study employed at least one standardized outcome that measures mental health difficulties. Trials with or without a control group were both considered. The inclusion criteria were not restricted based on publication date, study design, setting, age, gender, or publication status, except for requiring the studies to be in English. However, studies that did not present primary quantitative findings on the effectiveness of EMDR in peer-reviewed publications, such as reviews, books, conference abstracts, or posters, were excluded. Additionally, studies that combined the EMDR with other therapies or interventions without providing appropriate statistical differentiation of EMDR effects were also excluded.
2.2. Search
A database search was conducted across multiple databases, including PsychINFO, EMBASE, MEDLINE, and Web of Science, between 1989 and September 2023. Additionally, the Francine Shapiro Library and the Journal of EMDR Practice and Research were hand-searched renowned for focusing on EMDR studies. To ensure inclusivity, ongoing studies were searched from the UK Clinical Trials Gateway and The ISRCTN Registry. The searches were repeated to guarantee the most current evidence for synthesis before finalizing the review. The search terms employed in all databases included combinations of terms Eye Movement Desensitization and Reprocessing (EMDR), along with remote, online, and web based. Furthermore, the reference lists of eligible studies as well as previous systematic reviews and meta-analyses pertaining to EMDR were searched for further studies. Two independent reviewers conducted the study selection process in two phases – initially focusing on titles and abstracts, followed by a comprehensive evaluation of full-text articles. Disagreements were solved through discussion or arbitration with a third reviewer. A data extraction sheet was developed, initially pilot-tested and subsequently refined. The data extraction covered various elements such as detailed sample and study design information. Additionally, specifics about the EMDR protocol were all extracted from each study.
2.3. Quality assessment
The risk of bias was evaluated across articles by using A Revised Tool to Assess the Risk of Bias in Randomised Trials (RoB-2) (28) and the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-1) (29).
2.4. Analysis
Given the significant heterogeneity in terms of study design, interventions, outcomes, follow-up periods, and sample characteristics, a meta-analysis was not feasible. Consequently, the study opted for a narrative synthesis approach to interpret and present the findings from the diverse studies included in this review. This method provided a descriptive and comprehensive account of the results, highlighting trends, patterns, and variations within the available evidence.
3. Findings
3.1. Study characteristics
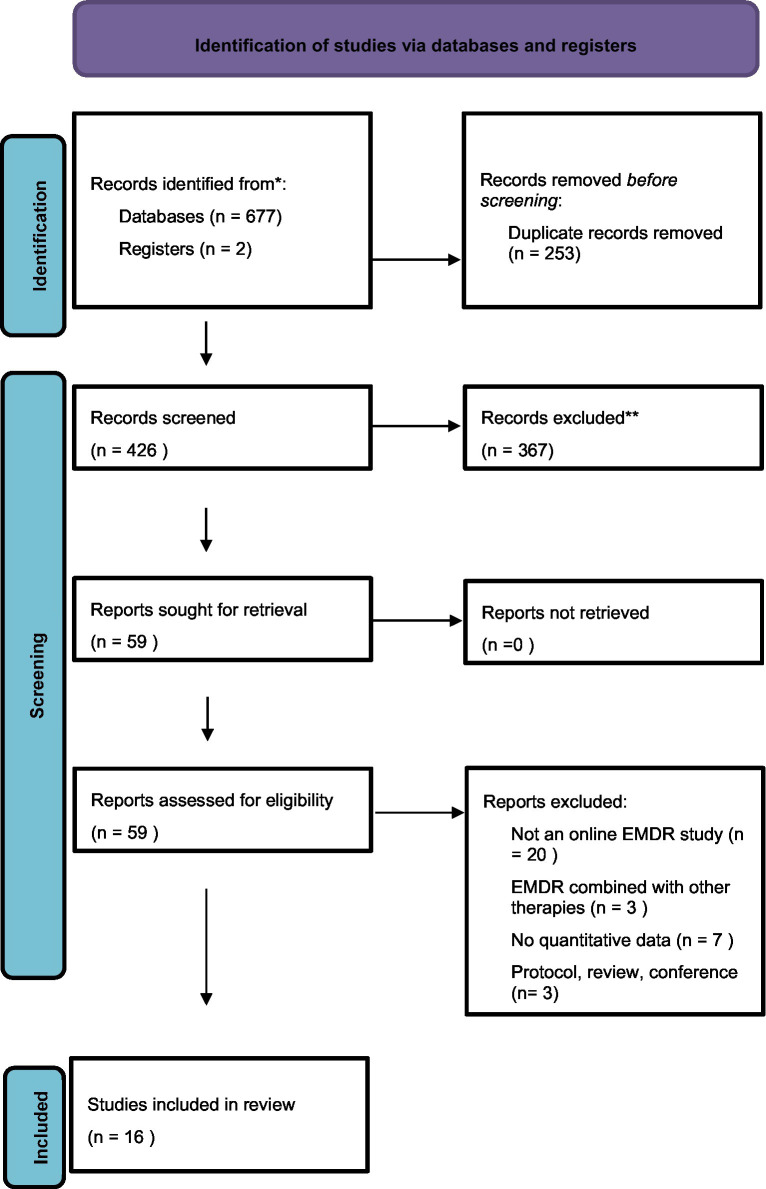
The flow of studies is displayed in Figure 1. Sixteen articles were included in the review.
Figure 1.
Flowchart of the systematic review process.
Participants: the total participant count across the 16 eligible studies was 1,231 individuals. The sample sizes showed considerable variation and encompassed both adolescents and adults. Among the studies, 14 recruited adult participants exclusively, while two had mixed groups comprising adolescents and adults. Notably, nine studies specifically focused on healthcare workers within their samples. Different studies utilize individual live sessions or group live sessions, showing flexibility in therapeutic delivery formats. Self-administered computerized sessions are also used in some cases.
Interventions: the treatment durations ranged from a single session to nine sessions, with each session ranging between 60 min and 134 min. The studies tested seven different protocols (R-TEP, G-TEP, IGTP, Standard EMDR protocol, STEP, Blind 2 Therapist, and URG-EMDR protocol), indicating the adaptability of EMDR to address various forms of trauma or distress. Notably, seven articles tested the efficacy of The Recent Traumatic Episode (R-TEP) protocol while 3 articles tested standard EMDR protocol.
Comparator/Design: studies incorporated randomised controlled trials and single-arm pre-post designs. Yet the majority of the studies used a one-arm design with pre- and post-treatment assessments. The follow-up durations ranged from 1 month to 9 months.
Outcomes: across all studies, the central focus was on the alteration of PTSD scores as the primary outcome. Secondary outcomes encompassed depression, anxiety, and Subjective Units of Disturbance (SUD), which is a patient-report scale that measures the distress the client feels about the particular memory that is being processed during the EMDR session. Studies used various tools such as PTSD CheckList – Civilian Version (PCL-C), PTSD Checklist for DSM-5 (PCL-5), Post-traumatic Stress Symptoms-14 (PTSS-14), The International Trauma Consortium (ITQ), Impact of Event Scale – Revised (IES-R), Depression, Stress and Anxiety Scale (DASS 21) and Hospital Anxiety and Depression Scale (HADS) to assess symptoms related to PTSD, stress, and trauma. Patient Health Questionnaire-9 (PHQ-9), Beck’s Depression Inventory (BDI-II), HADS, and DASS-21 were utilized across different studies to evaluate depressive symptoms. Generalised Anxiety Disorder Assessment (GAD-7), The State-Trait Anxiety Inventory (STAI), BDI-II, and HADS were used to measure symptoms of anxiety. Several studies evaluate SUD using different assessment tools. Additional measures, including burnout assessment tools like The Brief Resilience Scale (BRS), Maslach Burnout Inventory (MBI), and instruments for self-efficacy (General Self-Efficacy Scale [GSE]), post-traumatic growth (post traumatic growth inventory [PTGI]), and Mental Illness-Related Shame (MIES) were utilized in some studies. For outcomes, please refer to Table 2.
Table 2.
Outcomes.
| PTSD/Stress | Depression | Anxiety | SUD | Others | |
|---|---|---|---|---|---|
| Bates et al., 2022 | PCL-C+ | HADS | HADS | EQ-5D-5L BRS | |
| Farrell et al., 2023 | ITQ+ | PHQ-9+ | GAD-7+ | SUD+ | MIES |
| Moench et al., 2021 | DASS-21+ | DASS-21+ | GSE+ | ||
| Clarke, 2022 | PTSS-14+ | PHQ-9+ | GAD-7+ | EQ-5D-5L+ | |
| Faretta et al., 2022 | IES-R | THERMO+ | |||
| Farrell et al., 2022 | SUD+ | ||||
| Fernandez et al., 2022 | IES-R+ | THERMO+ | |||
| Goga et al., 2022 | IES-R+ | STAI+ | SUD+ | ||
| Lazzaroni et al., 2021 | IES-R+ | STAI+ | THERMO+ PTGI | ||
| McGowan et al., 2021 | IES(R)+ PCL-5+ | PHQ-9+ | GAD-7+ | ||
| Mischler et al., 2021 | SUD+ | ||||
| Morris et al., 2022 | PCL-5+ | SUD+ | |||
| Perri et al., 2021 | PCL-5+ | BDI-II+ | STAI+ | ||
| Sagaltici et al., 2022 | IES-R+ | BDI-II+ | BAI+ | MBI+ | |
| Tarquinio et al., 2020 | HAD+ | HAD+ | SUD+ | ||
| Yurtsever et al., 2022 | IES-R+ |
+Significant improvement at the final measurement point from the baseline or control group. PTGI, post-traumatic growth inventory; BRS, the brief resilience scale; MBI, Maslach burnout inventory; IES-R, the impact of event scale-revised; PCL-5, the PTSD checklist for DSM-5; HADS, the hospital anxiety and depression scale; BDI-II, the beck depression inventory-II; STAI, the state-trait anxiety inventory; SUD, subjective units of disturbance scale; PTGI, the post-traumatic growth inventory; PCL-C, the post-traumatic stress disorder checklist-Civilian; BAI, beck anxiety inventory; PTSS-14, the post-traumatic stress syndrome 14-questions inventory; The EQ-5D, EuroQol Group; SDS, the sheehan disability scale; DASS-21, depression and anxiety stress scale; GSE, the generalized self-efficacy scale; PCL-C, PTSD checklist; PSS-I, the PTSD symptom scale-interview; THERMO, the emotion thermometer; MIES, moral injury event scale; K10, the Kessler 10 item.
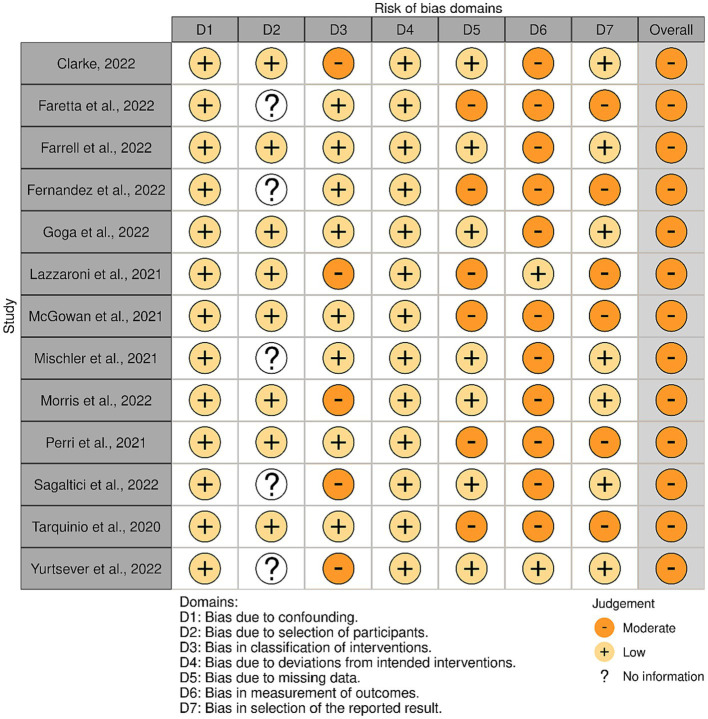
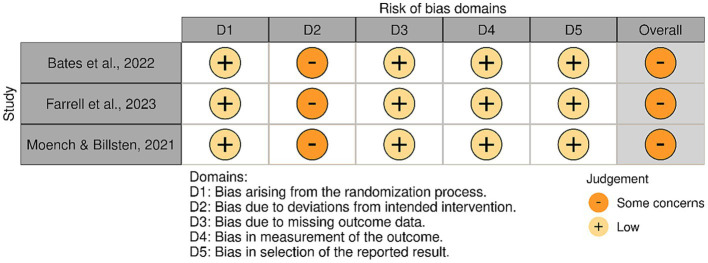
3.2. Quality assessment
The included articles varied regarding risk of bias. Figure 2 shows the assessment of the non-randomised studies. All studies received a moderate risk of bias. The most common shortcomings were the lack of blind assessors and the use of self-reported outcomes. Figure 3, shows the risk assessments of the randomised studies. Three randomised studies had some concerns of bias. This was due to allowing deviation from the intended intervention or the use of self-report measures only.
Figure 2.
Quality evaluation of non-randomised studies.
Figure 3.
Quality evaluation of randomised studies.
3.3. Findings
3.3.1. Therapist delivered live online sessions
3.3.1.1. Individual sessions
The Standard EMDR Protocol was assessed in two separate studies. The first study recruited EMDR therapists practicing in the UK and Ireland (30). A total of 33 therapists provided data on 93 different clients. The results demonstrated reductions in mean scores for the IES(R), GAD-7, PHQ-9, and PCL-5 checklists, indicating improvement in mental health difficulties. Yet, no significant correlation was found between the duration of EMDR training and clinical outcomes, nor was there a noteworthy difference in the connection between accreditation level and clinical outcome.
In a similar study conducted in Germany (31), data from 23 therapists who conducted 102 EMDR sessions with 76 patients were analyzed. The findings highlighted the potential efficacy and viability of online EMDR. The reduction in SUD was on the same level as that observed in face-to-face EMDR studies. Notably, the bilateral stimulation as eye movements led to greater reductions than tapping in sessions.
A separate study recruited a total of 24 participants for a single-session EMDR protocol known as the “Blind 2 Therapist” (VB2Tr), with measurements taken at pre-treatment, post-treatment, 1 month, and 6 month follow-ups (32). All 24 research participants completed the VB2Tr treatment session and subsequent measurements without any dropouts. The study demonstrated a substantial decrease in both SUD and emotional intensity.
The concluding study explored the effects of a single session of the Urgent EMDR (URG-EMDR) protocol on 17 healthcare professionals (33). The assessment focused on anxiety and depressive symptoms using the HAD scale, along with the level of perceived disturbance (SUD). The URG-EMDR protocol bears similarities to the standard EMDR protocol but aims to provide an intervention within 24 to 72 h following a critical incident. Seventeen female healthcare workers were involved in the study. The results indicated a significant difference between pre-test and post-test scores across all variables.
The R-TEP protocol was investigated across a total of six studies as an individual intervention, comprising 5 one-arm trials and one two-arm trial. The primary focus of these studies was to assess the impact of EMDR therapy on diverse mental health outcomes in participants, including health care professionals and patients.
Another study recruited healthcare workers diagnosed with post-traumatic stress disorder and utilized Beck Anxiety Inventory (BAI), Impact of Event Scale-Revised (EIS-R) and Maslach Burnout Inventory (MBI) (34). Each participant received five 90 min sessions. The study revealed significant decreases in mental health difficulties, with notable reductions in anxiety, depression, and emotional exhaustion symptoms that persisted at the 1 month follow-up.
In a separate study, out-of-home care staff who were regularly exposed to workplace-related trauma were recruited (35). Over a 3 years pilot study, both the Recent Traumatic Episode Protocol (R-TEP) and the Group Traumatic Episode Protocol (G-TEP) were administered. Due to the COVID-19 pandemic, individual EMDR (R-TEP) was provided online in 2020. The results indicated a substantial reduction in PCL-5 scores from baseline to follow-up, and participants who underwent R-TEP or G-TEP experienced symptom reductions. Both face-to-face and online deliveries exhibited significant reductions in PCL-5 scores, with no significant differences between the two modes of delivery.
Yurtsever and colleagues conducted another study employing online R-TEP with 154 individuals working alongside frontline professionals and COVID-19 patients (36). Participants underwent five sessions, and the analyses demonstrated the effectiveness of EMDR therapy in reducing PTSD levels across all groups. While PTSD levels in frontline professionals continued to decrease during the follow-up, they remained consistent in other groups.
In a different approach, Perri and colleagues recruited 38 patients diagnosed with acute stress disorder and randomly assigned them to receive either EMDR R-TEP or CBT treatment (37). Both groups underwent a 7-session therapy, resulting in significant reductions in anxiety, stress, and depression for both treatments.
Bates and colleagues conducted the sole RCT of R-TEP, enrolling 26 participants and randomizing them into online EMDR R-TEP or usual care groups (38). Participants were offered up to eight EMDR sessions until disturbance points were addressed. While an 83% intervention adherence rate was observed, and most participants completed all study procedures, no significant changes in anxiety or depression were noted. In a notable case study, Clarke explored the effects of nine sessions of online R-TEP on an intensive care survivor, indicating promising reductions in all outcome measures (39).
3.3.1.2. Group sessions
Four studies examined the feasibility of administering various EMDR protocols as group interventions through online delivery.
In an RCT (40), frontline mental health and emergency workers were recruited to evaluate the effectiveness of EMDR G-TEP for treating Post-Traumatic Stress Disorder (PTSD) and moral injury. Participants were randomised into either a treatment group or a delayed treatment group. All participants underwent four online sessions of G-TEP. Measurements encompassed the International Trauma Questionnaire (ITQ), Generalised Anxiety Disorder 7-item (GAD-7), Patient Health Questionnaire (PHQ-9), Moral Injury Events Scale (MIES), and the EuroQol (EQ-5D) for quality of life. The results demonstrated a significant treatment effect in both the active and control groups.
IGTP was assessed as an online treatment option in two separate studies involving healthcare workers during the COVID-19 pandemic in Italy, conducted by the same research team. In the first study, 11 healthcare workers from a nursing home were recruited (41). Participants engaged in three EMDR group therapy sessions. The outcomes revealed a noteworthy reduction in post-traumatic stress disorder (PTSD) symptoms measured by IES-R, and there was a substantial enhancement in the quality of emotional experience following the intervention. However, when the IES-R questionnaire was administered to participants again at the 9 months follow-up, it indicated an increase across all subscales. In the same team’s second study, 587 healthcare workers were recruited (42). The IGTP protocol was delivered online, utilizing the same outcome assessment tools. Groups consisted of 4–6 participants, and the treatment comprised three meetings of approximately 2 h each over a month, occurring approximately once a week. All variables showed significant improvement after EMDR therapy, underscoring a clear treatment effect.
Lazzaroni and colleagues conducted a study involving 50 adolescents and young adults aged 13 to 24 years (43). This study diverged from prior R-TEP research by delivering R-TEP through three group sessions, each lasting 1 h. Pre- and post-treatment evaluations incorporated the Impact of Event Scale-Revised (IES-R), State–Trait Anxiety Inventory (STAI) scales, and the Emotion Thermometer. Additionally, the Post-Traumatic Growth Inventory (PTGI) questionnaire was administered post-intervention. The outcomes exhibited substantial improvements in STAI, IES-R, and Emotion Thermometer scores, indicative of reduced post-traumatic symptoms. Furthermore, a significant positive change was observed in PTGI scores.
3.3.2. Self-administered computerised sessions
In addition to above studies, further attempts have already been made to extend the availability and accessibility of EMDR. Two studies have evaluated self-administered EMDR sessions of which one was a randomised controlled trial (44, 45).
In the first study standard EMDR protocol was again utilized using an artificial intelligence engine chatbot to fully replace clinicians (44). Moreover, the tool employed artificial intelligence (AI) to adjust the bilateral stimulation automatically based on the patient’s degree of responsiveness. A total of 31 participants participated in the single-session intervention, which incorporated various types of Bilateral Stimulation (BLS). The intervention consisted of four distinct phases. The initial three phases were formulated to diminish the intensity of emotions and beliefs linked to the traumatic event. The fourth phase was introduced to establish a positive belief concerning the same event. The IES-R and STAI instruments were administered as part of the pre-test assessment. Following this, four participants were excluded from the study based on their scores on the IES-R and STAI. These individuals were subsequently referred to a more specialized professional treatment. Following the single session intervention, participants showed the potential effectiveness of self-administered EMDR with the help of the AI tool in decreasing PTSD and anxiety.
In the second study on self-administered EMDR, Moench and Billsten conducted research during the COVID-19 pandemic involving healthcare workers and mental health clinicians (45). They implemented the EMDR-based protocol named Self-Care Traumatic Episode Protocol (STEP), which involved a single 90 mins session. This protocol, derived from the EMDR group treatment G-TEP, aimed to address trauma. The study encompassed a series of steps, starting with telephone assessment and screening. Following this, a 90 mins computerized session was conducted, where a recorded therapist guided the client through the protocol. Clients who managed to reduce their Subjective Units of Disturbance (SUD) level to 7 or lower after engaging in the 4 Elements activity were granted access to the intervention. The study included thirty-four participants who were randomly assigned to either the treatment group or a waitlist control. Assessments were conducted using the Generalised Self-Efficacy Scale (GSE) and the Depression and Anxiety Stress Scale (DASS-21). The results indicated a significant decrease in depression, anxiety, and stress levels, accompanied by an increase in general self-efficacy among the participants who underwent the STEP intervention.
4. Discussion
This systematic review aims to describe the current evidence regarding online/remote applications of EMDR therapy in patients with mental health difficulties. Overall, the results indicate that delivering EMDR therapy via online tools is feasible and potentially effective. This approach presents a promising alternative to in-person delivery of intensive trauma-focused therapy.
The studies in this review encompass a wide array of populations, including adults, adolescents, and healthcare workers, demonstrating the applicability of EMDR across various age groups and professional backgrounds. Some studies specifically target healthcare workers, emphasizing the need to address the mental health challenges within this occupational group. The delivery formats also vary, with studies utilizing individual live sessions, group live sessions, and self-administered computerized sessions.
4.1. Implications and recommendations
The application of online EMDR therapy seems to entail both advantages and disadvantages (32). On the advantageous side, this approach offers an alternative tool for reducing trauma symptoms, making it valuable in professional-limited environments. Furthermore, EMDR can be cost effective thanks to fewer sessions needed compared to CBT (46). Notably, in four studies in this review, the treatment was completed within a single session, suggesting that online EMDR could potentially serve as a time-efficient and cost-effective solution, especially in situations where there is a need for immediate intervention after incidents like work-related difficulties (34, 40, 44, 45).
Moreover, online EMDR can offer flexibility, adaptability, decrease in costs thanks to reduction in commute costs for both the clients and the therapists, and linguistic and cultural versatility, particularly for participants from already stigmatized groups (47) by conducing sessions from the privacy of one’s home which can help alleviate concerns about being seen entering or leaving a therapist’s office. By doing so, online EMDR might offer a more acceptable means of receiving therapy bypassing some cultural and social stigmas associated with seeking mental health help.
Furthermore, online EMDR’s capacity for intensive delivery and its integration into a comprehensive treatment package enhances accessibility. Although not included in this review, several articles are worth mentioning to showcase this. In these studies, EMDR has been successfully combined and integrated with other techniques (48–50). In the first study of its kind, EMDR therapy was administered utilizing a website (50) and combined with psychoeducation sessions. Fifteen adult patients diagnosed with PTSD were included and the findings revealed significant reductions in clinician-rated PTSD severity. However, there was no statistically significant decline in self-rated PTSD symptoms. In fact, three participants reported a worsening of self-rated PTSD symptoms after completing the treatment. In the second study, EMDR was offered as part of a comprehensive treatment program involving prolonged exposure, physical activities, and psychoeducation (48). This treatment was administered through telehealth over a 4 days period and the research involved six patients experiencing Complex PTSD. The findings revealed that four out of the six patients no longer met the diagnostic criteria for PTSD or Complex PTSD. In a subsequent study conducted by the same research team, EMDR therapy was once again combined with prolonged exposure, physical activities, and psychoeducation to treat 73 patients diagnosed with PTSD (50). The findings indicated that 60 patients (82.2%) no longer met the diagnostic criteria for PTSD, and the proportion of patients with Complex PTSD decreased from 47.1 to 10.1%.
On the other hand, this method relies heavily on technology and software access, which may not be universally available. Privacy and confidentiality issues may arise in the online context, and access to smart devices may become a prerequisite, limiting its applicability in certain areas for certain groups such as refugees and people with low finances. It may also not be well-suited for addressing severe mental health issues. Furthermore, concerns regarding potential risks accompany remote treatment, and the partial absence of non-verbal cues may also limit the therapeutic experience. Moreover, whether conducted in-person or online, the effectiveness of EMDR or any therapy depends on various factors, including the individual’s specific needs and the skills of the therapist. The low drop-out rates across studies indicate that participants generally tolerate online EMDR therapy well.
Processing experiences and memories within the context of EMDR treatments can sometimes lead to varying degrees of emotional distress and dysregulation (50). The capacity of clinicians to effectively address and manage these reactions might be constrained when conducting EMDR therapy online, potentially raising safety concerns that are challenging to navigate from a remote setting. The impact of EMDR therapists’ experience on treatment outcomes has been a subject of debate. Some studies indicate that EMDR therapy shows improved results with sessions lasting longer than 60 min (51) and when administered by more experienced therapists (18). However, this review did not find a direct connection between accreditation level and clinical outcomes (30). Additionally, the reduction in SUD was not linked to the age or gender of both therapists and patients (31).
As another challenge, the technological challenges can hinder the delivery of sessions and introduce distractions that may compromise the overall effectiveness of EMDR treatment (25, 26). A lack of focus, fatigue, or exhaustion stemming from online communication and difficulties related to the application of bilateral stimulation due to technical challenges can also be important difficulties during online EMDR sessions (52).
Future research should (a) evaluate the cost-effectiveness of online EMDR in comparison to other online interventions; (b) identify moderators and mediators that might influence treatment outcomes, such as the number of sessions, gender, age, facilitator characteristics, and the number and characteristics of traumas experienced and (c) incorporate qualitative techniques involving both participants and facilitators to understand the reasons for dropouts and withdrawals to develop strategies to improve recruitment. Finally, the majority of studies recruited adults, with some including adolescents. Although several systematic reviews indicated the effectiveness of EMDR for child and adolescent populations for a range of mental health conditions (20, 46, 53–58), the lack of studies targeting children in the context of online EMDR indicates a potential gap in the existing research. This suggests the need for more focused and comprehensive investigations into the efficacy and application of online EMDR specifically in children and adolescents.
4.2. Limitations
While this review presents promising findings, it is important to note that some studies within it exhibit significant limitations despite the importance of the quality of methodology in EMDR trials (59). These limitations include the lack of a control group, small sample sizes, absence of follow-up assessments, and reliance solely on self-report measures when evaluating the quality of evidence. Similarly, fidelity assessment was reported in only three out of the sixteen studies (32, 36, 40). In these studies, fidelity assessment was carried out through either recording of the sessions or group supervision.
Several systematic reviews indicate that, EMDR therapy has been mostly shown effective or promising for various other populations when offered face to face, including dementia patients with PTSD (60), incarcerated people with PTSD (61), and refugee and asylum seeker populations with PTSD (62, 63). Furthermore, other systematic reviews showed similar results for in person EMDR for various other conditions including but not limited to psychosis symptoms (64, 65), chronic pain (66, 67), functional neurological disorder (68), and bipolar affective disorder (69). However, even though this review included several populations (adults, adolescents, and healthcare professionals) for PTSD, depressive and anxiety symptoms, this review is unable to comment on the effectiveness of remote EMDR for above populations and conditions due to lack of research. Finally, the study’s protocol was registered retrospectively on INPLASY. A retrospective registration may be seen as a limitation; however, despite the lack of the initial registration, no substantial change was made on the protocol since its inception. Furthermore, to ensure transparency and good quality, multiple reviewers were involved in the screening and selection of the articles as detailed in the Methods section.
5. Conclusion
In summary, despite its limitations, the trials included in this review indicate that online EMDR shows promise as a valuable tool in alleviating PTSD symptoms and addressing other mental health difficulties. However, due to methodological challenges, there is a clear need for studies with more robust designs, larger sample sizes, validated assessment tools, and follow-up evaluations. Future comparative trials could shed light on how different delivery methods impact treatment outcomes, offering insights into the significance of group interaction in treatment effectiveness beyond just the treatment content itself.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SK: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. ZK: Methodology, Writing – review & editing, Conceptualization, Investigation, Writing – original draft. AA: Investigation, Conceptualization, Writing – review & editing, Writing – original draft, Methodology.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Bonati M, Campi R, Segre G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: a systematic review of the evidence. Epidemiol Psychiatr Sci (2022), 31,:e27, doi: 10.1017/S2045796022000051, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pedrosa AL, Bitencourt L, Fróes ACF, Cazumbá MLB, Campos RGB, de Brito SBCS, et al. Emotional, Behavioral, and psychological impact of the COVID-19 pandemic. Front Psychol. (2020) 11:566212. doi: 10.3389/fpsyg.2020.566212, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dragioti E, Tsartsalis D, Mentis M, Mantzoukas S, Gouva M. Impact of the COVID-19 pandemic on the mental health of hospital staff: an umbrella review of 44 meta-analyses. Int J Nurs Stud. (2022) 131:104272. doi: 10.1016/j.ijnurstu.2022.104272, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dragioti E, Li H, Tsitsas G, Lee KH, Choi J, Kim J. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J Med Virol. (2022) 94:1935–49. doi: 10.1002/jmv.27549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pietrabissa G, Simpson SG. Psychological consequences of social isolation during COVID-19 outbreak. Front Psychol. (2020) 11:2201. doi: 10.3389/fpsyg.2020.02201, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Penninx BWJH, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. (2022) 28:2027–37. doi: 10.1038/s41591-022-02028-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy L, Markey KO, Donnell C, Moloney M, Doody O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: a scoping review. Arch Psychiatr Nurs. (2021) 35:375–94. doi: 10.1016/j.apnu.2021.05.002, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Witteveen AB, Young S, Cuijpers P, Ayuso-Mateos JL, Barbui C, Bertolini F. Remote mental health care interventions during the COVID-19 pandemic: an umbrella review. Behav Res Ther. (2022) 159:104226. doi: 10.1016/j.brat.2022.104226, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duden GS, Gersdorf S, Stengler K. Global impact of the COVID-19 pandemic on mental health services: a systematic review. J Psychiatr Res. (2022) 154:354–77. doi: 10.1016/j.jpsychires.2022.08.013, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Punton G, Dodd AL, McNeill A. You’re on the waiting list: an interpretive phenomenological analysis of young adults’ experiences of waiting lists within mental health services in the UK. PLoS One. (2022) 17:e0265542. doi: 10.1371/journal.pone.0265542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li J. Digital technologies for mental health improvements in the COVID-19 pandemic: a scoping review. BMC Public Health. (2023) 23:413. doi: 10.1186/s12889-023-15302-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulvaney-Day N, Dean D, Miller K, Camacho-Cook J. Trends in use of telehealth for Behavioral health care during the COVID-19 pandemic: Considerations for payers and employers. Am J Health Promotion. (2022) 36:1237. doi: 10.1177/08901171221112488e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sriati A, Kurniawan K, Senjaya S, Khoirunnisa K, Muslim RNI, Putri AM. The effectiveness of digital-based psychotherapy in overcoming psychological problems in college students during the COVID-19 pandemic: a scoping review. J Holist Nurs. (2023):089801012311629. doi: 10.1177/08980101231162990, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapiro F, Laliotis D. EMDR and the adaptive information processing model: integrative treatment and case conceptualization. Clin Soc Work J. (2011) 39:191–200. doi: 10.1007/s10615-010-0300-7 [DOI] [Google Scholar]
- 15.Shapiro F. Adaptive information processing, and case conceptualization. J EMDR Pract Res. (2007) 1:68–87. doi: 10.1891/1933-3196.1.2.68 [DOI] [Google Scholar]
- 16.Shapiro F. EMDR 12 years after its introduction: past and future research. J Clin Psychol. (2002) 58:1–22. doi: 10.1002/jclp.1126 [DOI] [PubMed] [Google Scholar]
- 17.Carletto S, Ostacoli L, Colombi N, Calorio L, Oliva F, Fernandez I, et al. EMDR for depression: a systematic review of controlled studies. Clin Neuropsychiatry. (2017) 14:306–12. [Google Scholar]
- 18.Chen L, Zhang G, Hu M, Liang X. Eye movement desensitization and reprocessing versus cognitive-Behavioral therapy for adult post-traumatic stress disorder. J Nerv Ment Dis. (2015) 203:443–51. doi: 10.1097/NMD.0000000000000306, PMID: [DOI] [PubMed] [Google Scholar]
- 19.Kaptan SK, Dursun BO, Knowles M, Husain N, Varese F. Group eye movement desensitization and reprocessing interventions in adults and children: a systematic review of randomized and nonrandomized trials. Clin Psychol Psychother. (2021) 28:784–806. doi: 10.1002/cpp.2549, PMID: [DOI] [PubMed] [Google Scholar]
- 20.Rodenburg R, Benjamin A, de Roos C, Meijer AM, Stams GJ. Efficacy of EMDR in children: a meta-analysis. Clin Psychol Rev. (2009) 29:599–606. doi: 10.1016/j.cpr.2009.06.008, PMID: [DOI] [PubMed] [Google Scholar]
- 21.Yunitri N, Chu H, Kang XL, Wiratama BS, Lee T-Y, Chang L-F. Comparative effectiveness of psychotherapies in adults with post-traumatic stress disorder: a network meta-analysis of randomised controlled trials. Psychol Med. (2023) 53:6376–88. doi: 10.1017/S0033291722003737, PMID: [DOI] [PubMed] [Google Scholar]
- 22.Sepehry AA, Lam K, Sheppard M, Guirguis-Younger M, Maglio AS. EMDR for depression: a meta-analysis and systematic review. J EMDR Pract Res. (2021) 15:2–17. doi: 10.1891/EMDR-D-20-00038 [DOI] [Google Scholar]
- 23.Yunitri N, Kao CC, Chu H, Voss J, Chiu HL, Liu D. The effectiveness of eye movement desensitization and reprocessing toward anxiety disorder: a meta-analysis of randomized controlled trials. J Psychiatr Res. (2020) 123:102–13. doi: 10.1016/j.jpsychires.2020.01.005, PMID: [DOI] [PubMed] [Google Scholar]
- 24.Fisher N. Using EMDR therapy to treat clients remotely. J EMDR Pract Res. (2021) 15:73–84. doi: 10.1891/EMDR-D-20-00041 [DOI] [Google Scholar]
- 25.Bursnall M, Thomas BD, Berntsson H, Strong E, Brayne M, Hind D. Clinician and patient experience of internet-mediated eye movement desensitisation and reprocessing therapy. J Psychosoc Rehabil Ment Heal. (2022) 9:251–62. doi: 10.1007/s40737-022-00260-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unwin G, Stenfert-Kroese B, Rogers G, Swain S, Hiles S, Clifford C. Some observations on remote delivery of eye-movement desensitisation and reprocessing to people with intellectual disabilities. J Policy Pract Intellect Disabil. (2023) 20:205–15. doi: 10.1111/jppi.12452 [DOI] [Google Scholar]
- 27.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 29.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGowan IW, Fisher N, Havens J, Proudlock S. An evaluation of eye movement desensitization and reprocessing therapy delivered remotely during the COVID-19 pandemic. BMC Psychiatry. (2021) 21:560. doi: 10.1186/s12888-021-03571-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mischler C, Hofmann A, Behnke A, Matits L, Lehnung M, Varadarajan S, et al. Therapists’ experiences with the effectiveness and feasibility of videoconference-based eye movement desensitization and reprocessing. Front Psychol. (2021) 12:748712. doi: 10.3389/fpsyg.2021.748712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Farrell D, Moran J, Zat Z, Miller PW, Knibbs L, Papanikolopoulos P, et al. Group early intervention eye movement desensitization and reprocessing therapy as a video-conference psychotherapy with frontline/emergency workers in response to the COVID-19 pandemic in the treatment of post-traumatic stress disorder and moral injury. Front Psychol. (2023) 14:1129912. doi: 10.3389/fpsyg.2023.1129912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tarquinio C, Brennstuhl M-J, Rydberg JA, Bassan F, Peter L. EMDR in Telemental health Counseling for healthcare workers caring for COVID-19 patients: a pilot study. Issues Ment Health Nurs. (2021) 42:3–14. doi: 10.1080/01612840.2020.1818014, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Sağaltıcı E, Çetinkaya M, Şahin ŞK, Gülen B, Karaman Ş. Recent traumatic episode protocol EMDR applied online for COVID-19-related symptoms of Turkish health care workers diagnosed with COVID-19-related PTSD: a pilot study. Anadolu Psikiyatr Derg. (2022) 23:121–7. doi: 10.5152/alphapsychiatry.2022.21763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morris H, Hatzikiriakidis K, Dwyer J, Lewis C, Halfpenny N, Miller R. Early intervention for residential out-of-home care staff using eye movement desensitization and reprocessing (EMDR). Res Pract Policy. (2022) 15:S456–64. doi: 10.1037/tra0001418 [DOI] [PubMed] [Google Scholar]
- 36.Yurtsever A, Bakalim O, Karaman Ş, Kaya S, Konuk E. The effect of the online eye movement desensitization and reprocessing early intervention protocol (EMDR R-TEP) for the risk groups with post-traumatic stress symptoms during the COVID-19 pandemic. Front Psychol. (2022):1–9. doi: 10.3389/fpsyg.2022.935782/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perri RL, Castelli P, La Rosa C, Zucchi T, Onofri A. COVID-19, isolation, quarantine: on the efficacy of internet-based eye movement desensitization and reprocessing (EMDR) and cognitive-behavioral therapy (CBT) for ongoing trauma. Brain Sci. (2021) 11:579. doi: 10.3390/brainsci11050579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bates A, Golding H, Rushbrook S, Shapiro E, Pattison N, Baldwin DS, et al. A randomised pilot feasibility study of eye movement desensitisation and reprocessing recent traumatic episode protocol, to improve psychological recovery following intensive care admission for COVID-19. J Intensive Care Soc. (2022) 24:309. doi: 10.1177/17511437221136828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clarke R. The EMDR recent traumatic episode protocol with an intensive care survivor: a case study. J EMDR Pract Res. (2022) 16:50–60. doi: 10.1891/EMDR-2021-0028 [DOI] [Google Scholar]
- 40.Farrell D, Fadeeva A, Zat Z, Knibbs L, Miller P. A stage 1 pilot cohort exploring the use of EMDR therapy as a videoconference psychotherapy during COVID-19 with frontline mental health workers: a proof of concept study utilising a virtual blind 2 therapist protocol. Front Psychol. (2022) 13:1–14. doi: 10.3389/fpsyg.2022.901855/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Faretta E, Garau MI, Gallina E, Pagani M, Fernandez I. Supporting healthcare workers in times of COVID-19 with eye movement desensitization and reprocessing online: a pilot study. Front Psychol. (2022) 13:964407. doi: 10.3389/fpsyg.2022.964407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fernandez I, Pagani M, Gallina E. Post-traumatic stress disorder among healthcare workers during the COVID-19 pandemic in Italy: effectiveness of an eye movement desensitization and reprocessing intervention protocol. Front Psychol. (2022) 13:1–9. doi: 10.3389/fpsyg.2022.964334/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lazzaroni E, Invernizzi R, Fogliato E, Pagani M, Maslovaric G. Coronavirus disease 2019 emergency and remote eye movement desensitization and reprocessing group therapy with adolescents and Young adults: overcoming lockdown with the butterfly hug. Front Psychol. (2021) 12:1–9. doi: 10.3389/fpsyg.2021.701381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goga N, Boiangiu CA, Vasilateanu A, Popovici AF, Drăgoi MV, Popovici R, et al. An efficient system for eye movement desensitization and reprocessing (EMDR) therapy: a pilot study. Healthc. (2022) 10:133. doi: 10.3390/healthcare10010133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moench J, Billsten O. Randomized controlled trial: self-care traumatic episode protocol, computerized EMDR treatment of COVID-19-related stress. J EMDR Pract Res. (2021) 15:99–113. doi: 10.1891/EMDR-D-20-00047 [DOI] [Google Scholar]
- 46.Manzoni M, Fernandez I, Bertella S, Tizzoni F, Gazzola E. Eye movement desensitization and reprocessing: the state of the art of efficacy in children and adolescent with post traumatic stress disorder. J Affect Disord. (2021) 282:340–7. doi: 10.1016/j.jad.2020.12.088, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Kaptan SK, Varese F, Yilmaz B, Andriopoulou P, Husain N. Online delivery gave me privacy and distance from others: feasibility trial and qualitative evaluation of an online intervention for refugees and asylum seekers; LTP+EMDR G-TEP. Couns Psychother Res. (2022) 22:876–88. doi: 10.1002/capr.12580 [DOI] [Google Scholar]
- 48.Bongaerts H, Voorendonk EM, van Minnen A, de Jongh A. Safety and effectiveness of intensive treatment for complex PTSD delivered via home-based telehealth. Eur J Psychotraumatol. (2021) 12:346. doi: 10.1080/20008198.2020.1860346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bongaerts H, Voorendonk EM, Van Minnen A, Rozendaal L, Telkamp BSD, de Jongh A. Fully remote intensive trauma-focused treatment for PTSD and complex PTSD. Eur J Psychotraumatol. (2022) 13:3287. doi: 10.1080/20008066.2022.2103287, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spence J, Titov N, Johnston L, Dear BF, Wootton B, Terides M, et al. Internet-delivered eye movement desensitization and reprocessing (iEMDR): an open trial. F1000Research. (2013) 2:e79. doi: 10.12688/f1000research.2-79.v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Y-R, Hung K-W, Tsai J-C, Chu H, Chung M-H, Chen S-R, et al. Efficacy of eye-movement desensitization and reprocessing for patients with posttraumatic-stress disorder: a meta-analysis of randomized controlled trials. PLoS One. (2014) 9:e103676. doi: 10.1371/journal.pone.0103676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Papanikolopoulos P, Prattos T, Foundoulakis E. Pandemic times and the experience of online EMDR practice in Greece: a qualitative study on obstacles and perspectives. J EMDR Pract Res. (2022) 16:135–44. doi: 10.1891/EMDR-2021-0033 [DOI] [Google Scholar]
- 53.Retamal MI, Sepúlveda E, Cortés JP, Barraza F, Arancibia M. Desensibilización y reprocesamiento por movimientos oculares (EMDR) para trastornos ansiosos y depresivos en niños y adolescentes: revisión de la evidencia disponible. Rev Chil Neuropsiquiatr. (2022) 60:51–61. doi: 10.4067/s0717-92272022000100051 [DOI] [Google Scholar]
- 54.Civilotti C, Margola D, Zaccagnino M, Cussino M, Callerame C. Eye movement desensitization and reprocessing in child and adolescent psychology: a narrative review. Curr Treat Options Psychiatry. (2021) 8:95–109. doi: 10.1007/s40501-021-00244-0 [DOI] [Google Scholar]
- 55.Gillies D, Taylor F, Gray C, O’Brien L, D’Abrew N. Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents (review). Evidence-Based Child Heal A Cochrane Rev J. (2013) 8:1004–116. doi: 10.1002/ebch.1916 [DOI] [PubMed] [Google Scholar]
- 56.Dowd H, McGuire BE. Psychological treatment of PTSD in children: an evidence-based review. Irish J Psychol. (2011) 32:25–39. doi: 10.1080/03033910.2011.611612 [DOI] [Google Scholar]
- 57.Field A, Cottrell D. Eye movement desensitization and reprocessing as a therapeutic intervention for traumatized children and adolescents: a systematic review of the evidence for family therapists. J Fam Ther. (2011) 33:374–88. doi: 10.1111/j.1467-6427.2011.00548.x [DOI] [Google Scholar]
- 58.Adler-Nevo G, Manassis K. Psychosocial treatment of pediatric post-traumatic stress disorder: the neglected field of single-incident trauma. Depress Anxiety. (2005) 22:177–89. doi: 10.1002/da.20123, PMID: [DOI] [PubMed] [Google Scholar]
- 59.Maxfield L, Hyer L. The relationship between efficacy and methodology in studies investigating EMDR treatment of PTSD. J Clin Psychol. (2002) 58:23–41. doi: 10.1002/jclp.1127, PMID: [DOI] [PubMed] [Google Scholar]
- 60.Ruisch JE, Nederstigt AHM, van der Vorst A, Boersma SN, Vink MT, Hoeboer CM. Treatment of post-traumatic stress disorder in people with dementia: a structured literature review. Psychogeriatrics. (2023) 23:523–34. doi: 10.1111/psyg.12951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Malik N, Facer-Irwin E, Dickson H, Bird A, MacManus D. The effectiveness of trauma-focused interventions in prison settings: a systematic review and meta-analysis. Trauma Violence Abus. (2023) 24:844–57. doi: 10.1177/15248380211043890, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Dowllah IM, Melville C. Effectiveness of psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in low- and middle-income countries: a systematic review and meta-analysis. J Health Psychol. (2023) 11:254. doi: 10.1177/13591053231199254, PMID: [DOI] [PubMed] [Google Scholar]
- 63.Thompson CT, Vidgen A, Roberts NP. Psychological interventions for post-traumatic stress disorder in refugees and asylum seekers: a systematic review and meta-analysis. Clin Psychol Rev. (2018) 63:66–79. doi: 10.1016/j.cpr.2018.06.006, PMID: [DOI] [PubMed] [Google Scholar]
- 64.Adams R, Ohlsen S, Wood E. Eye movement desensitization and reprocessing (EMDR) for the treatment of psychosis: a systematic review. Eur J Psychotraumatol. (2020) 11:e1711349. doi: 10.1080/20008198.2019.1711349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sin J, Spain D. Psychological interventions for trauma in individuals who have psychosis: a systematic review and meta-analysis. Psychosis. (2017) 9:67–81. doi: 10.1080/17522439.2016.1167946 [DOI] [Google Scholar]
- 66.Tefft AJ, Jordan IO. Eye movement desensitization reprocessing as treatment for chronic pain syndromes. J Am Psychiatr Nurses Assoc. (2016) 22:192–214. doi: 10.1177/1078390316642519, PMID: [DOI] [PubMed] [Google Scholar]
- 67.Tesarz J, Leisner S, Gerhardt A, Janke S, Seidler GH. Effects of eye movement desensitization and reprocessing (EMDR) treatment in chronic pain patients: a systematic review. Pain Med (United States). (2014) 15:247–63. doi: 10.1111/pme.12303, PMID: [DOI] [PubMed] [Google Scholar]
- 68.Cope SR, Mountford L, Smith JG, Agrawal N. EMDR to treat functional neurological disorder: a review. J EMDR Pract Res. (2018) 12:118–32. doi: 10.1891/1933-3196.12.3.118 [DOI] [Google Scholar]
- 69.Bedeschi L. EMDR for bipolar disorder: a systematic review of the existing studies in literature. Clinical. Neuropsychiatry. (2018) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.