Abstract
Rheumatoid arthritis (RA) poses significant management challenges, especially in elderly patients living in rural areas with limited access to health care. This case report illustrates an integrative approach to managing RA, emphasizing the interplay of clinical, social, and environmental factors. A 72-year-old woman in a rural Japanese setting presented with progressive, widespread joint pain, initially self-managed with over-the-counter medications. Her condition, complicated by socioeconomic constraints and limited access to health care, necessitated a comprehensive management strategy. Clinical examination revealed bilateral joint tenderness, swelling, and high titers of rheumatoid factor and anti-citrullinated protein antibodies, confirming RA. Treatment included methotrexate and prednisolone, complemented by lifestyle modifications. Interdisciplinary collaboration among healthcare professionals, including nutritionists and physiotherapists, facilitated her management. The patient's care was guided by the chronic care model and the ecological model, addressing her clinical needs and socio-environmental context. This holistic approach resulted in improved clinical outcomes and enhanced quality of life. This case highlights the importance of a patient-centered, multidisciplinary approach in managing RA in rural settings. Integrating clinical management with an understanding of social determinants and patient empowerment is crucial for effective treatment. The case underscores the need for adaptable healthcare strategies that are sensitive to the unique challenges faced by elderly patients in rural communities.
Keywords: family medicine, systems approach, chronic care model, patient-centered care healthcare disparities, rural health services, geriatric medicine, rheumatoid arthritis
Introduction
Rheumatoid arthritis (RA) is a chronic and systemic inflammatory disorder, predominantly affecting joints and potentially involving multiple organ systems [1]. Its prevalence among older populations highlights an escalating public health issue. RA causes not only joint deformity and destruction but also markedly diminishes the quality of life through pain, decreased mobility, and related comorbidities [1].
Effectively managing RA is challenging due to the complex role of social determinants of health (SDH). These factors, including socioeconomic status, education, healthcare access, and environmental conditions, significantly affect health outcomes [2]. In rural areas, where resources and healthcare access are typically restricted, these SDHs create distinct challenges [3]. Research indicates that patients in these areas experience delayed diagnoses, fewer treatment options, and insufficient follow-up care, resulting in poorer health outcomes compared to those in urban areas [3,4]. Therefore, it is crucial to understand and contextualize this reality within rural settings. Given this reality, it is imperative to consider thorough assessments and interventions aimed at improving the quality of life for RA patients in rural areas.
This case report thus introduces one case study that delves into the relationship between SDH and RA, offering a comprehensive exploration of how these factors interplay to exacerbate the disease's impact in rural settings. This case study is not merely an examination of the clinical aspects of RA but a narrative that weaves in the principles of family medicine to address these broader social and environmental determinants. This case report underscores the importance of a comprehensive medical management plan that goes beyond pharmacological interventions to include preventative strategies and community-integrated care. This approach is characterized by its patient-centered nature, where patient agency and active participation in the management plan are paramount. The manuscript emphasizes that empowering patients in their care decisions leads to more personalized and effective management strategies integrating family medicine principles into managing chronic conditions like RA.
Case presentation
A 72-year-old woman reported six months of persistent, widespread joint pain, beginning in her wrists and progressively affecting multiple joints. Despite self-medication with acetaminophen 500 mg and a one-week trial of prednisone 10 mg daily by her primary care physician on suspicion of RA, her pain re-emerged and escalated during dose tapering. She, therefore, sought further management at our community hospital. Her medical history included hypertension and dyslipidemia, but no notable surgical procedures or allergies.
Clinical perspective
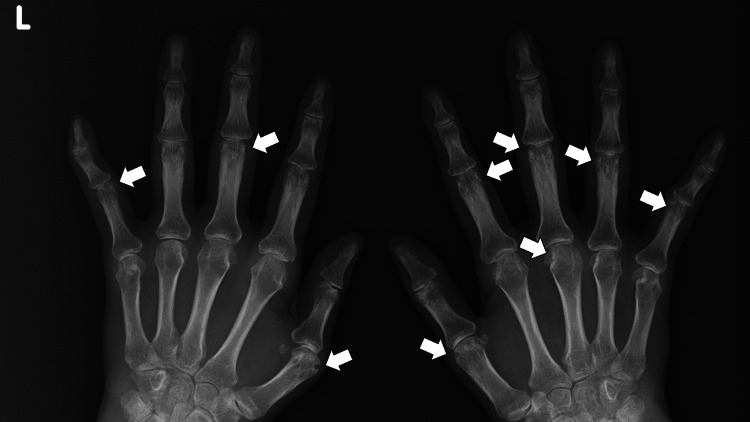
The vital signs at the visit were as follows: blood pressure of 156/97 mmHg, pulse rate of 69 beats/minute, body temperature of 37.1°C, respiratory rate of 16 breaths/minute, and oxygen saturation of 98 % on room air. Physical examination revealed bilateral tenderness, swelling, and warmth in the shoulders, wrists, and metacarpophalangeal joints, with absent systemic symptoms. High titers of rheumatoid factor (125 IU/mL; reference < 15) and anti-citrullinated protein antibodies (158 U/mL; reference < 4.5) without any positivity of antinuclear antibodies, coupled with high C-reactive protein (7.2 mg/dl; reference <0.3) and wrists X-ray findings of bone erosion, corroborated the RA diagnosis based on the American College of Rheumatology/European League Against Rheumatism 2010 score of 10 (Figure 1).
Figure 1. X-ray of bilateral hands showing multiple bone erosions.
Therapeutic prednisolone use prompted the calculation of her risk for secondary hypertension, diabetes, and osteoporosis.
Individual aspect
Despite living independently and engaging in backyard agriculture, the patient’s increasing joint pain, concern about RA progression, and loss of joint function witnessed by her peers became debilitating. Addressing her concerns about disability, the cost of medication, and lifestyle factors worsening her condition, such as a high-carbohydrate diet and sedentary lifestyle, required a comprehensive approach. Her expectations encompassed pain management and the resumption of daily activities without incurring prohibitively expensive treatments.
Contextual dimension
As a widow residing alone in a mountainous region, her non-driving status and limited public transport availability restricted her access to health care and support. While managing on a pension and minimal income from selling vegetables, her children did not support her financially. Furthermore, she found agricultural tasks increasingly difficult due to pain, rendering her income unreliable. These contextual factors significantly influenced her treatment and management strategy.
Treatment and response
The commencement of methotrexate (6 mg/week) and prednisolone (10 mg/day) was complicated by worsening hypertension (150/98 mmHg) and increased blood glucose levels (hemoglobin A1c: 8.6), likely due to prednisolone. The introduction of valsartan (40 mg/day) and metformin (750 mg/day), supplemented by dietary and exercise interventions devised by our multidisciplinary team, stabilized her secondary conditions. A revised higher dose of methotrexate enabled prednisolone discontinuation, further improving glycemic and blood pressure control. The potential complications of methotrexate were followed with monthly laboratory tests, and any abnormality was not observed.
Complications and multidisciplinary approach for rehabilitation and management of chronic diseases
Hyperglycemia and hypertension represented significant challenges to RA management, mandating attentive monitoring and action to mitigate additional risks [1]. Collaboration among internal medicine specialists, nutritionists, and physiotherapists was crucial in managing her complications and ensuring adherence to lifestyle changes. This reflects a scholarly approach to clinical care [2].
Ethical and professional care
Understanding our patient’s fears and financial constraints, our team facilitated access to affordable medication and enlisted community center assistance to ensure she benefitted from social and physical activities. This approach exemplified our dedication to delivering empathetic, ethical, and professionally outstanding care [3].
Discussion
Applying family medicine principles
Upholding a Patient-Centered Approach
Emphasizing a patient-centered approach in the principle of family medicine, the complexities of managing this elderly woman’s RA became navigable [4]. The five-star family physician framework guided our consideration of her socioeconomic status and family situation, consisting of five competencies such as care provider, decision maker, communicator, community leader, and manager [5]. Her reluctance to engage her children, who reside in distant locales, and her financial constraints shaped our care trajectory, such as focusing on conventional and cost-effective medicines. Recognizing her experiences both medically and personally was crucial for unbiased care provision based on her initial help-seeking behaviors and self-management with over-the-counter medication [5].
Embracing Family-Oriented and Community-Integrated Care
The principle of community-integrated family medicine took precedence, and the spatial and social environment was shared between healthcare providers and the patient [4]. In this case, a shared understanding of prevalent societal issues, such as isolation and challenges in caring for the elderly within a rural milieu, was facilitated. The partnership with the community center post-treatment supported her autonomy and integrated her recovery and ongoing health management with enhanced social connections and a safety net. Consequently, the patient was part of a network allowing her health and social well-being to be cohesively addressed, reflecting family medicine's collaborative and community-integrated ethos.
Comprehensive Management Viewed Through a Preventative Lens
The patient's management transcended the immediacy of RA treatment, venturing into a proactive domain where preventative and therapeutic strategies were interlaced. The sustained use of prednisolone prompted a vigilant approach focusing on early detection and management of complications like hypertension and diabetes [6]. Moreover, including the patient in community health initiatives paid homage to the principle of preventive care and health promotion integrated within the community's fabric and tailored to its peculiarities [4]. The healthcare provided was preventative and health-promotive, tailored to her daily life and circumstances.
Interdisciplinary Collaboration and Management
The merit of interdisciplinary collaboration was illuminated by crafting a symbiotic, patient-centered management path. In line with family medicine principles, family physicians acted as key resource managers, coordinating the involvement of dietitians, therapists, and specialists [4]. Respecting five-star family doctor approaches, this comprehensive, team-driven approach permeated beyond the hospital, assimilating resources from across the medical and community spectrum [5]. The patient's care transcended the domain of medical facilities to intertwine with societal structures. This was foundational in preserving her health and optimizing her quality of life and reflects the role of a manager and leader in holistic patient care [5].
Nurturing Patient Agency and Empowerment
Empowering the patient as an active co-creator in her care journey was paramount [5]. While the family physician’s expertise crafted the medical trajectory, her inputs, derived from her lived experiences, fears, and expectations, informed the management strategy, ensuring it was concurrently clinically sound and empathetically delivered. This approach established a synergy between clinical guidance and the patient’s personal experiences, jointly shaping the care pathway; this promoted adherence and ensured the care was compatible with her daily life rather than an extrinsic, enforced protocol.
Ethical and Professional Adherence
Throughout the course of caring for our patients, professional and ethical adherence was meticulously observed [7]. Her financial constraints and social isolation critically shaped clinical decisions, ensuring they were realistic and practical. The conscientious effort to align medical advice with affordability and accessibility demonstrated an unwavering commitment to equitable, empathetic, and holistic care [8]. Hence, each therapeutic choice and lifestyle recommendation was a testament to ethical, patient-centered medicine.
Social determinants affecting health in the patient and community
Self-Ageism and Its Infiltration Into Healthcare Perceptions
In Japan's elderly, self-ageism often leads to attributing symptoms to aging rather than potentially treatable conditions [9]. This mindset, intensified by Japan's cultural and societal narratives, may result in delays in seeking appropriate medical interventions. It necessitates consideration of symptom management in the context of the patient’s psycho-social dynamics, exploring how societal perspectives of age permeate individual health beliefs and behaviors [10].
Healthcare Accessibility and Literacy
In rural contexts like in some regions of Japan, limitations in healthcare resources and professional accessibility are amplified by gaps in health literacy among the elderly [11]. The barriers extend beyond the physical realm into the digital sphere; health information on the internet is frequently inaccessible to this demographic. Consequently, even with support structures, effective health-seeking behaviors among rural elders may be curtailed, manifesting in delays to or omission of crucial medical interventions for conditions like RA [12].
Social Isolation as a Multi-Faceted Challenge
Rural living, coupled with aging and further complexified by global crises like the COVID-19 pandemic, precipitates physical, emotional, and social isolation [13]. These factors confer an increased risk of poor mental health and physical health implications, such as increased stress and worsening chronic conditions like RA.
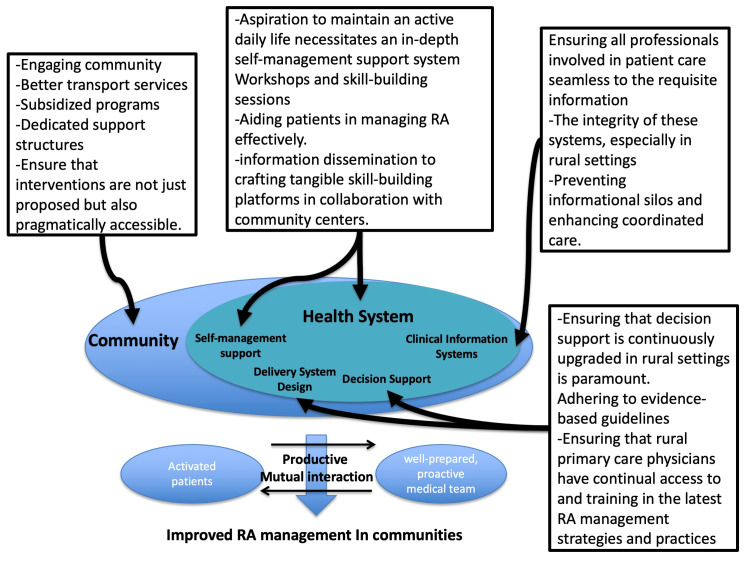
Chronic care model
The chronic care model (CCM) is a framework that enhances chronic disease management with an informed, proactive healthcare team and an engaged patient. The model comprises six essential elements: community health system self-management support, delivery system design, decision support, and clinical information systems [14]. This model can be applied to this case and health promotion in her community (Figure 2).
Figure 2. Chronic care model for effective rheumatoid arthritis management in rural contexts.
RA: rheumatoid arthritis.
Image credit: Ryuichi Ohta.
Self-Management Support
The patient’s aspiration to maintain an active daily life necessitates an in-depth self-management support system [14]. The CCM encourages practical steps, such as workshops and skill-building sessions, that could be integral in aiding patients in managing RA effectively [14]. This goes beyond information dissemination to crafting tangible skill-building platforms in collaboration with community centers.
Decision Support
Ensuring that decision support should be implemented and continuously upgraded in rural settings is paramount [14]. This entails adhering to evidence-based guidelines and ensuring that rural primary care physicians have continual access to training in the latest RA management strategies and practices.
Clinical Information Systems and Healthcare Organization
Ensuring that all professionals involved in patient care have seamless access to relevant information underpins effective management [14]. The integrity of these systems, especially in rural settings where healthcare professionals may operate in relative isolation, is crucial for preventing informational silos and enhancing coordinated care.
Community Resources and Policies
While engaging community resources is important, ensuring that these are not just available but also accessible and affordable, especially for elderly individuals in rural settings, is vital. Pragmatically, this may involve transport services, subsidized programs, and dedicated support structures.
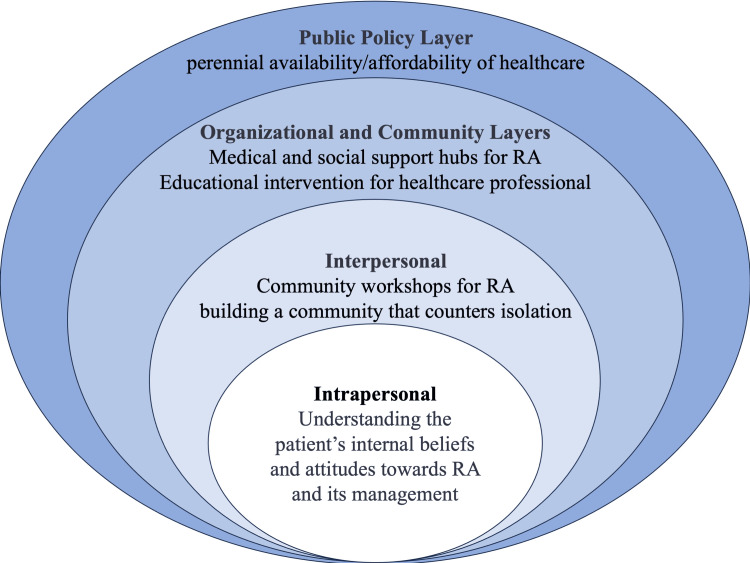
Ecological model
The ecological model emphasizes that interactions between individuals and their environment influence health and well-being. It is broken down into multiple layers: intrapersonal, interpersonal, organizational, community, and public policy [15]. This model can be applied to this case and the health promotion of her community (Figure 3).
Figure 3. Ecological model for rheumatoid arthritis management in communities.
RA: rheumatoid arthritis.
Image credit: Ryuichi Ohta.
Intrapersonal and Interpersonal Layers
Understanding the patient’s internal beliefs about and attitudes toward RA and its management is as crucial as ensuring a supportive social network [15]. Initiatives at this level encompass personal information provision through various information sources such as local newspapers and community workshops [16]. The latter increases understanding of RA management while building a community to counter isolation. Family physicians can collaborate to create articles for local newspapers and establish educational workshops.
Organizational and Community Layers
Local community centers can serve as medical and social support hubs, becoming a nexus for information, resources, and community-building [15]. This is especially pertinent in the social context of rural-dwelling elderly individuals. Family physicians can establish educational workshops for healthcare professionals in rural communities by collaborating with local governments and healthcare institutions [17].
Public Policy Layer
Ensuring that policies are formulated, implemented, and sustained to guarantee healthcare's persistent availability and affordability forms the linchpin on which the other interventions pivot [15]. Family physicians can continually discuss the management of RA in rural communities with policymakers [18].
Comparative insights: CCM vs. ecological model
While the CCM offers a structured approach to chronic disease management, leveraging healthcare team and patient involvement, it may risk overlooking broader social determinants. In contrast, the ecological model provides a multilayered view of the patient within their social and environmental context, suggesting intervention at various societal levels [14,15].
In the context of rural Japan, considerations of aging, social isolation, and healthcare accessibility become paramount [19]. The incorporation of both models offers a holistic approach. While CCM provides a systematic framework for managing RA at a healthcare level, the ecological model ensures that interventions also permeate to the community and policy levels, addressing root social determinants of health [14,15].
Integrating these approaches could curate a care methodology that is not only clinically robust but also socially and contextually sensitive, simultaneously addressing the immediate and root determinants of health [20]. This combined approach bridges immediate healthcare needs with long-term social change, fostering an environment that supports the holistic well-being of the elderly in rural areas.
Conclusions
Our case study of managing rheumatoid arthritis in an elderly, rural-dwelling woman underscores the need for an integrative approach combining the CCM and the ecological model. This strategy, which addresses both immediate clinical needs and broader socio-environmental factors, proved effective in navigating her complex healthcare and social challenges. The integration of clinical excellence with an understanding of her personal, economic, and community context led to improved health outcomes and quality of life. This case illustrates the importance of a holistic, adaptive approach in rural health care, emphasizing the need for strategies that are both medically robust and socially attuned.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Ryuichi Ohta, Chiaki Sano
Acquisition, analysis, or interpretation of data: Ryuichi Ohta, Chiaki Sano
Drafting of the manuscript: Ryuichi Ohta, Chiaki Sano
Critical review of the manuscript for important intellectual content: Ryuichi Ohta, Chiaki Sano
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Efficacy of pharmacological treatment in rheumatoid arthritis: a systematic literature research informing the 2019 update of the EULAR recommendations for management of rheumatoid arthritis. Kerschbaumer A, Sepriano A, Smolen JS, et al. Ann Rheum Dis. 2020;79:744–759. doi: 10.1136/annrheumdis-2019-216656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The effectiveness of family medicine-driven interprofessional collaboration on the readmission rate of older patients. Ohta R, Sano C. Healthcare (Basel) 2023;11:269. doi: 10.3390/healthcare11020269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perspectives about interprofessional collaboration and patient-centred care. Dahlke S, Hunter KF, Reshef Kalogirou M, Negrin K, Fox M, Wagg A. Can J Aging. 2020;39:443–455. doi: 10.1017/S0714980819000539. [DOI] [PubMed] [Google Scholar]
- 4.Core values of family medicine in Europe: current state and challenges. Arvidsson E, Švab I, Klemenc-Ketiš Z. Front Med (Lausanne) 2021;8:646353. doi: 10.3389/fmed.2021.646353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Five-star doctors for the 21st century: a BPKIHS endeavour for Nepal. Jha N, Premarajan KC, Nagesh S, Khanal S, Thapa LB. J Health Manag. 2005;7:237–247. [Google Scholar]
- 6.Rheumatoid arthritis. Smolen JS, Aletaha D, McInnes IB. Lancet. 2016;388:2023–2038. doi: 10.1016/S0140-6736(16)30173-8. [DOI] [PubMed] [Google Scholar]
- 7.Advancing the science of implementation in primary health care. Bazemore A, Neale AV, Lupo P, Seehusen D. J Am Board Fam Med. 2018;31:307–311. doi: 10.3122/jabfm.2018.03.180091. [DOI] [PubMed] [Google Scholar]
- 8.Family physicians as system-specific specialists in Japan’s aging society. Ohta R, Sano C. Cureus. 2022;14:0. doi: 10.7759/cureus.30811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Self-ageism among older rural people. Ohta R. Br J Gen Pract. 2023;73:110. doi: 10.3399/bjgp23X732129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clinical biopsychosocial reflection on coping with chronic illness and reliance upon nutrition support: an integrated healthcare approach. Price JS, Larsen SE, Miller LA, Smith HM, Apps JA, Weis JM. Nutr Clin Pract. 2019;34:220–225. doi: 10.1002/ncp.10263. [DOI] [PubMed] [Google Scholar]
- 11.Challenges in help-seeking behaviors among rural older people mitigated through family physician-driven outreach: a systematic review. Ohta R, Katsube T, Sano C. Int J Environ Res Public Health. 2022;19:17004. doi: 10.3390/ijerph192417004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Differentiating between seronegative elderly-onset rheumatoid arthritis and polymyalgia rheumatica: a qualitative synthesis of narrative reviews. Ohta R, Sano C. Int J Environ Res Public Health. 2023;20:1789. doi: 10.3390/ijerph20031789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solving social problems in aging rural Japanese communities: the development and sustainability of the Osekkai conference as a social prescribing during the COVID-19 pandemic. Naito Y, Ohta R, Sano C. Int J Environ Res Public Health. 2021;18:11849. doi: 10.3390/ijerph182211849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benefits and limitations of implementing Chronic Care Model (CCM) in primary care programs: a systematic review. Yeoh EK, Wong MC, Wong EL, et al. Int J Cardiol. 2018;258:279–288. doi: 10.1016/j.ijcard.2017.11.057. [DOI] [PubMed] [Google Scholar]
- 15.Using ecological models of health behavior to promote health care access and physical activity engagement for persons with disabilities. Kennedy W, Fruin R, Lue A, Logan SW. J Patient Exp. 2021;8 doi: 10.1177/23743735211034031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Educational intervention to improve citizen’s healthcare participation perception in rural Japanese communities: a pilot study. Ohta R, Ryu Y, Kitayuguchi J, Sano C, Könings KD. Int J Environ Res Public Health. 2021;18:1782. doi: 10.3390/ijerph18041782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rural health dialogue for the sustainability of help-seeking behaviors among older patients: grounded theory approach. Ohta R, Sano C. BMC Geriatr. 2023;23:674. doi: 10.1186/s12877-023-04401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Narratives in family medicine: a global perspective: the Besrour Papers: a series on the state of family medicine in the world. Gibson C, Woollard R, Kapoor V, Ponka D. https://www.cfp.ca/content/63/2/121.short. Can Fam Physician. 2017;63:121–127. [PMC free article] [PubMed] [Google Scholar]
- 19.Aging in rural Japan--limitations in the current social care policy. Tanaka K, Iwasawa M. J Aging Soc Policy. 2010;22:394–406. doi: 10.1080/08959420.2010.507651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Public health social work as a unifying framework for social work’s grand challenges. Cederbaum JA, Ross AM, Ruth BJ, Keefe RH. Soc Work. 2019;64:9–18. doi: 10.1093/sw/swy045. [DOI] [PubMed] [Google Scholar]