Abstract
Introduction
Tooth extraction due to dental caries is associated with socioeconomic deprivation and is a major reason for elective childhood hospital admissions in England. Consumption of sugar-sweetened beverages is a risk factor for dental caries. We examined whether the soft drinks industry levy (SDIL), announced in March 2016 and implemented in April 2018, was associated with changes in incidence rates of hospital admissions for carious tooth extraction in children, 22 months post-SDIL implementation.
Methods
Changes in incidence rates of monthly National Health Service hospital admissions for extraction of teeth due to a primary diagnosis of dental caries (International Classification of Diseases; ICD-10 code: K02) in England, between January 2012 and February 2020, were estimated using interrupted time series and compared with a counterfactual scenario where SDIL was not announced or implemented. Periodical changes in admissions, autocorrelation and population structure were accounted for. Estimates were calculated overall, by Index of Multiple Deprivation (IMD) fifths and by age group (0–4 years, 5–9 years, 10–14 years, 15–18 years).
Results
Compared with the counterfactual scenario, there was a relative reduction of 12.1% (95% CI 17.0% to 7.2%) in hospital admissions for carious tooth extractions in all children (0–18 years). Children aged 0–4 years and 5–9 years had relative reductions of 28.6% (95% CI 35.6% to 21.5%) and 5.5% (95% CI 10.5% to 0.5%), respectively; no change was observed for older children. Reductions were observed in children living in most IMD areas regardless of deprivation.
Conclusion
The UK SDIL was associated with reductions in incidence rates of childhood hospital admissions for carious tooth extractions, across most areas regardless of deprivation status and especially in younger children.
Trial registration number
ISRCTN18042742.
Keywords: biomarker, nutrition assessment, precision nutrition
WHAT IS ALREADY KNOWN ON THIS TOPIC
Dental extractions due to caries is the number one reason for children having an elective admission to hospital in England.
There is evidence for a strong relationship between consumption of sugar-sweetened beverages (SSBs) and the development of dental caries.
At present, there are no studies that have examined associations between SSB taxes and changes in childhood hospital admissions for carious tooth extractions, an indicator of severe dental decay.
WHAT THIS STUDY ADDS
Nearly 2 years after the soft drinks industry levy (SDIL) came into force, incident rates of hospital admissions for carious tooth extractions fell in children by 12% compared with the counterfactual scenario of no implementation of SDIL.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These findings add to the currently limited evidence base that SSB taxes can reduce hospital admissions for tooth extractions due to dental caries in children,
These effects were seen across the spectrum of deprivation suggesting widespread population benefits and particularly in preschool and primary school age children who have limited agency to make their own dietary decisions.
Introduction
Dental caries (tooth decay) is the most common non-communicable disease globally.1 In England, tooth extraction due to caries is the main reason for elective admission to hospital in children aged 5–9 years and nearly 90% of extractions in young children are due to decay.2 When left untreated, childhood dental caries is associated with pain, problems eating and socialising, and reduced school attendance. In England, approximately 60 000 school days are missed by children each year due to tooth extractions in hospital.2 The requirement for general anaesthesia, which itself is associated with distress, tiredness and bleeding,3 is the primary reason children attend hospital for tooth extractions and is most common in young children (<4 years) and when pain is widespread.4
Oral health among children has been improving for more than a decade, although large inequalities still exist, with children living in the most socioeconomically deprived areas having twice the number of decayed, missing (due to decay) and filled teeth (DMFT) as those from the least deprived.2 Population-level interventions that have the potential to improve oral health, particularly in early-life and in deprived communities, are an important component in addressing inequalities in oral health. A multitude of risk factors for dental caries have been identified including socioeconomic factors,5 less-than-twice daily toothbrushing,6 frequent exposure to free dietary sugars1 and (in infants) frequent bottle feeding especially at bedtime.7 While the UK government has concluded that water fluoridation is a safe and cost-effective way to reduce childhood tooth decay,5 it is not universally implemented. Furthermore, fluoridation schemes on their own are not sufficient to completely prevent tooth decay meaning additional interventions are necessary.1
WHO recommends added sugar should be limited to less than 10% of energy intake and that restricting sugars below 5% would provide further benefits to health, including dental health.1 In England, sugar-sweetened beverages (SSBs) are a major source of dietary added sugars in children, accounting for around 30% of added sugars in children 1–3 years and over 50% by late adolescence.8 WHO has recommended taxation of SSBs in order to reduce consumption of sugar9 and to date over 50 countries have implemented SSB taxes.10
In March 2016, the UK government announced a soft drinks industry levy (SDIL) with the aim of reducing sugar intake.11 The two-tier tax, which was implemented in April 2018, is designed to encourage manufacturers to reformulate their drinks rather than pass the tax on to the consumer. Manufacturers of soft drinks containing ≥8 g of sugar/100 mL are subject to a levy of £0.24 /L and those with ≥5 to <8 g of sugar/100 mL are taxed at £0.18 /L. Soft drinks containing <5 g/100 mL sugar are not liable for the levy and 100% fruit juices, powder to make drinks, milk and milk-based drinks and drinks with 1.2% alcohol by volume or more are exempt irrespective of sugar content. Through reformulation, the UK SDIL led to large reductions in the sugar levels in soft drinks12 and there was a reduction in sugar purchased from soft drinks.13 Furthermore, the SDIL was found to be associated with an 8% relative reduction in prevalence of obesity in girls aged 10/11 years who were in their last year of primary school education; however, this was not found in boys of the same age or in younger children who were in their first year of primary school.14
While the relationship between SSBs and dental caries is well established, there is limited evidence on the impacts of SSB taxes on oral health. One microsimulation study reported that an SSB tax alone was unlikely to have a significant impact on dental caries.15 However, other modelling studies have predicted that SSB taxes, based on a 20% tax16–18 or reformulation,19 would lead to reductions in dental caries and school absences attributable to dental health.20 These studies almost exclusively focus on age groups with permanent dentition, with some indicating the greatest benefits in children aged 15–19 years16 and 6–12 years,18 or in children16 and adults17 from lower income households.
We are aware of only one prior empirical study on a sugar tax and dental health. That study reported that taxes on unhealthy foods and drinks in Mexico were associated with a reduction in dental caries in adults. Associations in children aged 1–12 years were lower than in adults and no associations were observed in children aged 1–5 years.21 However, the study did not specifically examine tooth extractions due to dental caries—an indicator of more severe caries, especially in younger children.
We used hospital episode data from England to study changes in the incidence rates of hospital admission for carious tooth extraction in children in the 22 months following the implementation of the UK SDIL (1) overall, (2) by age and (3) by area-based deprivation.
Methods
This study is registered (ISRCTN18042742) and the protocol published.22 This study is reported as per the REporting of studies Conducted using Observational Routinely collected health Data Statement (S1 Checklist). Data were provided to us in an aggregated and anonymised state and ethical approval was not required for analysis of these data.
Data source
We used Hospital Episode Statistics (HES) on hospital admission for dental extraction of one or more deciduous or permanent teeth due to a primary diagnosis of dental caries (International Classification of Diseases; ICD-10 code: K02) in children aged 0–18 years in England attending a National Health Service (NHS) hospital. Data included in HES were grouped and summarised by (1) Index of Multiple Deprivation (IMD) quintile of the Lower Super Output Area (LSOA) of residence23 and (2) age groups 0–4, 5–9, 10–14, 15–18 years. In HES, patient age is calculated from patient date of birth and episode start date. LSOA of residence was determined from postcode of residence. HES used the 2010 version of the IMD to rank LSOAs from least to most deprived and to assign records into fifths. Where postcodes were not recorded or where a link could not be made, records were excluded from the analysis (0.06%). The study period ran for 98 months from January 2012 (study month 01) to February 2020 (study month 98) and included the periods of the SDIL announcement (March 2016; study month 51) and implementation (April 2018; study month 76).
Statistical analysis
Interrupted time series (ITS) analyses were performed to determine associations between the announcement and implementation of the SDIL and incidence rates of hospital admissions for carious tooth extractions (hereafter referred to as ‘hospital admissions’), in an overall model. Interaction terms revealed evidence of effect modification by age group and IMD quintile, thus further models were run for each age and deprivation category separately (online supplemental table S1). Modelling official statistics that reported numbers annually, we used polynomial regression to estimate groupwise (ie, age 0–4 years) population sizes in each study month.24 Incidence rates of hospital admissions were then calculated by dividing the groupwise number of admissions by the respective estimated population size, multiplied by 100 000 to give an incidence rate (per 100 000 population). Time series models were based on generalised least squares (GLS).
bmjnph-2023-000714supp001.pdf (164.8KB, pdf)
A data-driven approach, using calendar months, was used to determine periodic events associated with significant changes in hospital admissions. When calendar months were tested one-by-one, GLS models were finalised by including all the months that showed significant changes in hospital admissions. Thus, models were adjusted for the months of October, December and March where there were statistically significant changes in incidence rates of hospital admissions.
Autocorrelation was determined using Durbin-Watson statistical tests and graphically using autocorrelation and partial autocorrelation. For each model, an autocorrelation-moving average correlation structure was selected from a plurality of possible models, with main parameters including moving average (q) and order (p) adjusted to minimise the Akaike Information Criterion among the candidate models.
Preannouncement trends (study months 01–51) were used to estimate counterfactual scenarios. Absolute and relative differences in the incidence rates of hospital admissions were calculated by taking the difference between observed and counterfactual values at study month 98 (February 2020). Confidence intervals (CIs) of absolute and relative differences were estimated from standard errors that were calculated using the delta method.
The main analysis included a counterfactual based on a scenario in which there was no SDIL announcement or implementation. While SDIL implementation took place in April 2018, there is evidence that drinks reformulation was underway some months before.12 However, since implementation marked a precise time when legal enforcement of the SDIL came into effect for eligible soft drinks, we conducted secondary analysis where counterfactual scenarios were based on preimplementation trends (study months 01–76), rather than the preannouncement trends in the main analysis. Changes to the published protocol are available on the online supplemental material.22 Statistical analyses were conducted in R V.4.1.0.
Results
Over the 98-month study period, the mean incidence rate of hospital admissions fell from 31.0/100 000 population/month (p/m) in the preannouncement period (January 2014 – March 2016) to 28.5/100 000 p/m in the postannouncement period (April 2016–February 2020) (table 1). Admissions followed a strong social gradient with incidence rates being around five times higher in those living in the most (61.6/100 000 p/m in the preannouncement period) versus least deprived areas (12.7/100 000 p/m). In terms of age, the highest incidence rate was in the 5- to 9-year age group (66.2/100 000 p/m in the preannouncement period), which was approximately six times higher than in the 15- to 18-year age group (11.1/100 000 p/m).
Table 1.
Mean incidence (SD) of hospital admissions/100 000 population/ month for carious tooth extractions in the preannouncement* and postannouncement† periods of the UK SDIL, overall and by IMD quintiles and age group
| Preannouncement* | Postannouncement† | |
| Total population | 31.0 (2.5) | 28.5 (2.5) |
| Deprivation quintile | ||
| IMD1 (most deprived) | 61.6 (5.2) | 57.7 (4.7) |
| IMD2 | 38.1 (3.3) | 34.7 (3.7) |
| IMD3 | 24.3 (2.4) | 22.1 (2.2) |
| IMD4 | 16.7 (1.8) | 15.7 (1.6) |
| IMD5 (least deprived) | 12.7 (1.2) | 11.8 (1.3) |
| Age group (years) | ||
| 0–4 | 21.5 (2.1) | 18.3 (2.3) |
| 5–9 | 66.2 (5.5) | 60.7 (5.4) |
| 10–14 | 21.1 (2.0) | 18.8 (1.7) |
| 15–18 | 11.1 (1.2) | 9.4 (1.1) |
*Preannouncement period equates to the dates up to and including, January 2014–March 2016.
†Postannouncement period equates to the dates up to and including, April 2016–February 2020.
IMD, Index of Multiple Deprivation; SDIL, soft drinks industry levy.
Association between the UK SDIL and hospital admissions for carious tooth extractions
Unless indicated otherwise, all estimates of change in hospital admissions stated below are based on values in February 2020 at study month 98 in relation to the counterfactual scenario of no announcement or implementation of the UK SDIL.
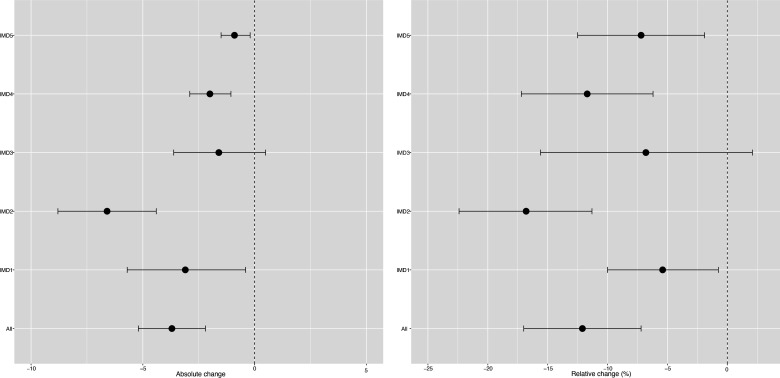
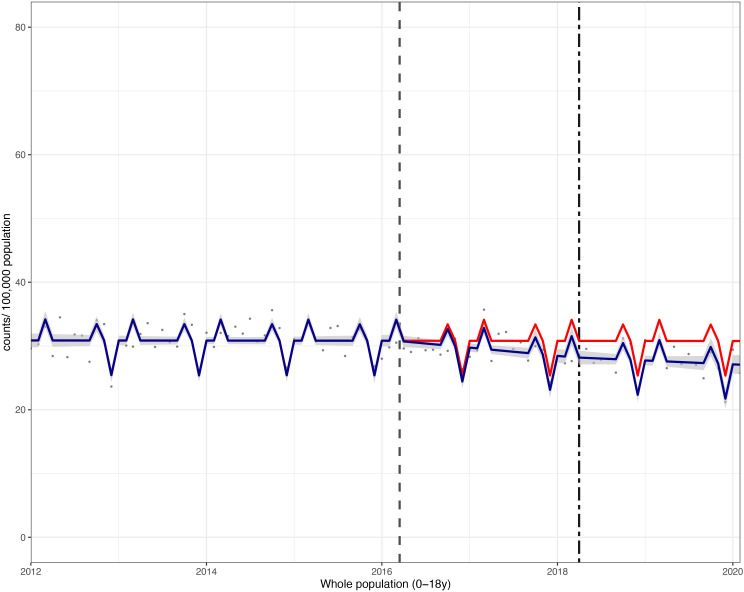
Overall, in children aged 0–18 years, there was an absolute reduction in hospital admissions of 3.7 (95% CI 5.2 to 2.2)/1 00 000 p/m or a relative reduction of 12.1% (95% CI 17.0% to 7.2%) compared with the counterfactual scenario (figures 1 and 2; online supplemental table S2).
Figure 1.
Changes in incidence/100 000 population/month of hospital admissions for carious tooth extractions (95% CIs), overall and by Index of Multiple Deprivation (IMD) fifth at 22 months postimplementation of the UK SDIL. SDIL, soft drinks industry levy.
Figure 2.
Incidence per 100 000 population per month of hospital admissions for carious tooth extractions, in children aged 0–18 years between January 2012 and February 2020. Observed and modelled incidence of hospital admissions for carious tooth extractions is shown. Dark blue points show observed data and dark blue lines (with grey shadows) show modelled data (and 95% CIs) of incidence. The red line indicates the counterfactual line based on the pre-SDIL announcement trend (based on the announcement and implementation having not occurred). The first and second dashed vertical lines indicate the time of the SDIL announcement and implementation, respectively. SDIL, soft drinks industry levy.
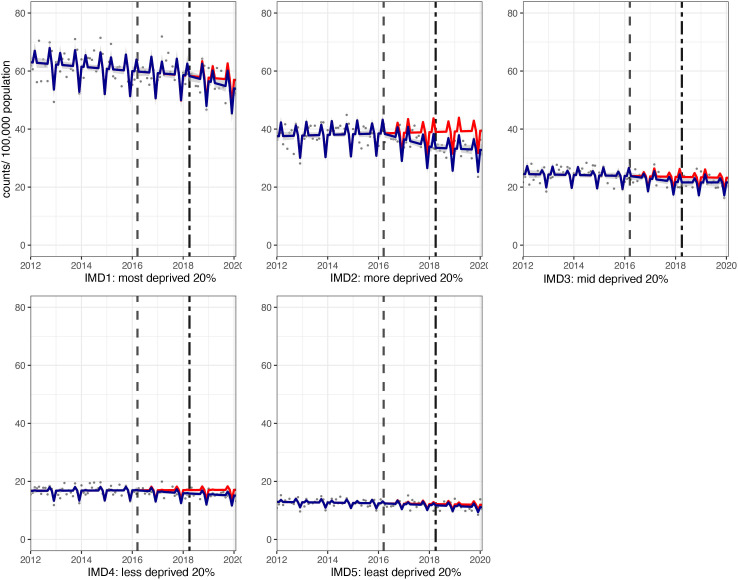
Significant reductions in hospital admissions were observed in children living in all areas regardless of deprivation, apart from the middle (IMD3) quintile (figures 1 and 3; online supplemental table S2). For example, children living, in the second most deprived areas (IMD2) had a relative reduction in hospital admissions of 16.8% (95% CI 22.4% to 11.3%). In visualisations, a steep divergence between counterfactual and observed models is observed in IMD2 soon after the SDIL announcement followed by notable flattening of the observed model following SDIL implementation (figure 3).
Figure 3.
Incidence per 100 000 population per month of hospital admissions for carious tooth extractions, in children aged 0–18 years between January 2012 and February 2020, by Index of Multiple Deprivation (IMD) fifth. Observed and modelled incidence of hospital admissions for carious tooth extractions is shown. Dark blue points show observed data and dark blue lines (with grey shadows) show modelled data (and 95% CIs) of incidence. The red line indicates the counterfactual line based on the pre-SDIL announcement trend (based on the announcement and implementation having not occurred). The first and second dashed vertical lines indicate the time of the SDIL announcement and implementation, respectively. SDIL, soft drinks industry levy.
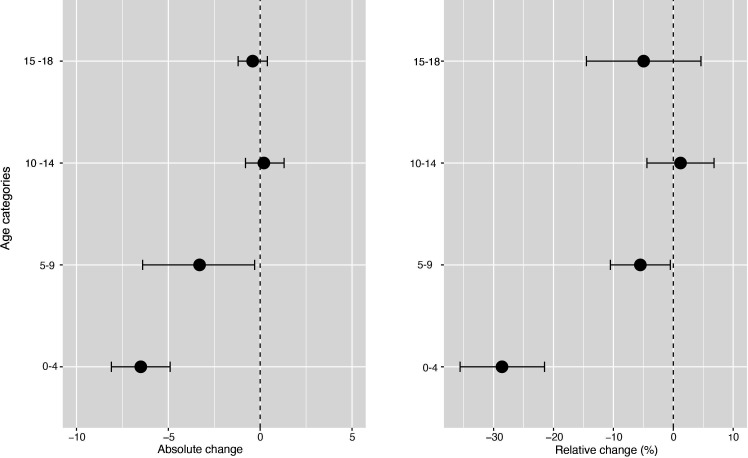
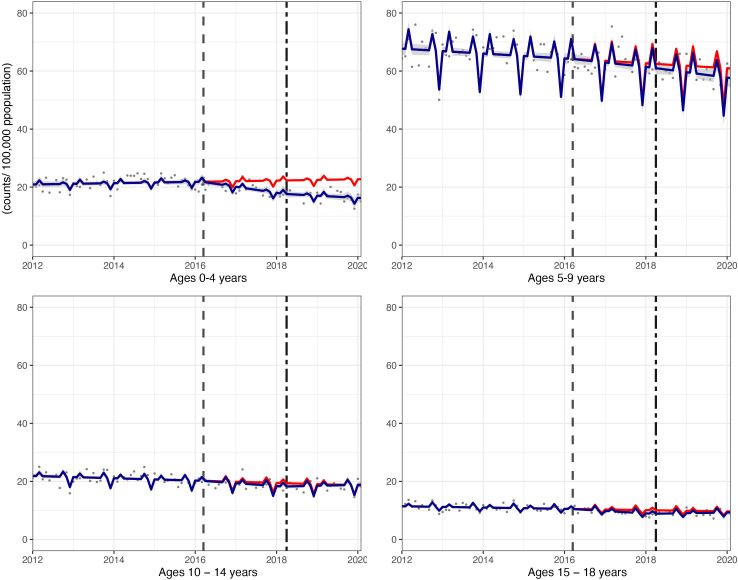
The youngest children had notable reductions in hospital admissions. For example, in children aged 0–4 years, a relative reduction of 28.6% (95% CI 35.6% to 21.5%) was observed (figures 4 and 5; online supplemental table S2). In this age group, rapid divergence between counterfactual and observed models was seen shortly after the SDIL announcement and continued with a slight flattening of the slope following implementation. A relative reduction of 5.5% (95% CI 10.5% to 0.5%) was observed for hospital admissions in children aged 5–9 years, the age group with the greatest number of extractions (table 1). No significant changes were observed in children in age groups 10–14 years and 15–18 years.
Figure 4.
Changes in incidence/100 000 population/month of hospital admissions for carious tooth extractions (95% CIs), by age group, at 22 months postimplementation of the UK SDIL. SDIL, soft drinks industry levy.
Figure 5.
Incidence per 100 000 population per month of hospital admissions for carious tooth extractions, in children aged 0–18 years between January 2012 and February 2020, by age group. Observed and modelled incidence of hospital admissions for carious tooth extractions is shown. Dark blue points show observed data and dark blue lines (with grey shadows) show modelled data (and 95% CIs) of incidence. The red line indicates the counterfactual line based on the pre-SDIL announcement trend (based on the announcement and implementation having not occurred). The first and second dashed vertical lines indicate the time of the SDIL announcement and implementation, respectively. SDIL, soft drinks industry levy.
Visualisations of the ITS models revealed notable troughs in hospital admissions in December and peaks in October and March. This may reflect periods with fewer elective surgeries due to public and school holidays, preceded or followed by catch-up periods.
In secondary analysis, we found that compared with the counterfactual scenario (of announcement but no implementation), there was no associated change in hospital admissions in children, overall (online supplemental table S3). Absolute reductions in hospital admissions of 3.3 (95% CI 0.7 to 6.0) were observed in children living in the most deprived areas, but there were increases relative to the counterfactual in children living in IMD2 and IMD3 and in all age groups except in children aged 5–9 years, where prevalence estimates were similar to the counterfactual.
Discussion
This is the first study we are aware of to use real-world data to examine the relationship between the UK SDIL and dental health. Compared with the counterfactual of no SDIL, we found a 12.1% (95% CI 17.0% to 7.2%) relative reduction in incidence rates of hospital admissions for carious tooth extractions in children 22 months following the UK SDIL implementation. Based on a population of 12 699 899 children aged 0–18 years in England in 2020, this reduction equates to an estimated 5638 averted cases of hospital admissions per annum.25 Reductions in the incidence rates of hospital admissions were observed in all deprivation groups except the middle quintile. Reductions in hospital admissions were greatest in younger children aged 0–4 years and 5–9 years, with absolute reductions of 6.5 and 3.3/100 000 p/m, respectively. This is an important finding given that children in the 5–9 age group are the most likely to be admitted to hospital for carious tooth extractions under general anaesthesia.26 Incidence rates remained unchanged in older age groups (10–14 years and 15–18 years).
Strengths and limitations
This study had several strengths. First, routinely collected HES data are not subject to response bias and instead capture all NHS attendances for carious tooth extraction. The requirement for critical care hospital support for dental extractions precludes similar activity in most private UK facilities meaning we are likely to have captured almost all relevant events (with only 0.6% of admissions excluded from analysis due to non-IMD linkage). Second, the availability of area-based sociodemographic data meant that hospital admissions could be examined by IMD group. Furthermore, changing population sizes across different sociodemographic groups were accounted for over time, making our effect estimates more precise. Third, availability of monthly HES data prior to the announcement of SDIL meant that we could base our counterfactual scenarios on 4 years of observed data. This meant we could both detect and statistically account for predictable cyclical variations in extractions across the calendar year. Such temporally sensitive analysis could not have been conducted with the other main source of data on children’s oral health, the Children’s Dental Health Survey that takes place only every second year.27
A comparable control group was not available, which limits our ability to fully attribute the observed changes in hospital admissions to the SDIL. It is therefore important to consider other factors that may have influenced the outcome. To our knowledge, the only other national intervention with the potential to impact substantially on dental public health was the sugar reduction programme (2015–2020).28 This aimed to achieve a 20% reduction in the sugar sold in food products, but only achieved a 3.5% reduction. Nevertheless, this programme, alongside the SDIL, may have raised public awareness of sugar consumption. Similarly, since December 2016 nutritional labelling has become compulsory on many prepackaged foods, including for example, adding the words ‘with sugar(s)’, which may have influenced consumer buying habits.29 Recent evidence suggests that colour-coded labels such as traffic light labelling system and Nutri-Score labelling performed well in promoting the purchasing of healthful products while nutrient-warning and health-warning labels discouraged unhealthful purchasing of food products.30 We are also not aware of notable changes in clinical practice during the study period. In fact, it was over a decade prior to the start point of our data (in 2000) when new regulations required that all dental general anaesthetics were carried out in hospital.31 Guidelines on improving preoperative paediatric care by involving specialists have been published.32 A study using retrospective records found that when assessment by a specialist does occur, the need for dental general anaesthetic (DGA), relative to referral request for DGA, may sometimes be avoided.33 However, children with severe decay is a main reason for DGA34 and with well-documented shortages of specialists in paediatric care, alternative pathways are not widely in place and DGA remains the most common reason children having an elective hospital admission in England.35 Additionally, there is evidence that not all NHS trusts will report activity using the HES system, for example, in 2019 ~25% of DGA providers did not appear on the HES dataset potentially leading to an underestimation in the levels of hospital admissions for tooth extractions;36 however, at present there is no longitudinal evidence suggesting variation in DGA providers in the HES dataset over the study period. A recent review on the variation in use of DGA in children found sociodemographic differences by age, deprivation, geographical location, ethnicity and service provision by health services.26 In this study, we were able to study hospital admissions for carious tooth extractions by child age group and level of area deprivation (recognised as the most important confounders for caries)37; however, we were unable to study by other potentially informative factors due to lack of available data.26 We were unable to account for presence or changes in water fluoridation levels in the analysis because geolocation (LSOA) data are not made available to researchers. We note the strong evidence that associates water fluoridation schemes with reductions in dental caries38 but also caution that the use of water fluoridation in the UK (which is devolved to local authorities) is both geographically limited and temporally inconsistent. For example, optimal fluoridation of potable water occurred in 10.9% of LSOAs in 2014, but just 6.3% in 2016.39 The results of this analysis are contingent on the modelled counterfactual based on 4 years of data prior to the intervention.
Comparison with other studies and interpretation of results
We are aware of only a few studies that have estimated the potential impacts of sugar taxes on dental caries in young children (<5 years) using either health impact modelling19 or empirical data.21 In contrast to our findings of greatest effects in younger groups, a modelling study predicted the SDIL would have greatest relative reductions in DMFT in English children aged 11–18 years as they had the highest baseline SSB consumption.19 That study, as well as using DMFT rather than incident hospital admissions for tooth extractions, assumed a uniform effect of sugar (and SSBs) on children’s teeth. Our contrasting findings may be explained by the intrinsic compositional differences between deciduous and permanent teeth.19 Deciduous teeth have a thinner enamel covering than permanent teeth which typically begin to erupt in children after 6 years of age. This means that the relationship between SSB consumption and caries may be stronger in younger than in older children. Thus, the timeline of permanent teeth eruption is an important factor to account for when comparing the impact of oral health interventions on children of different ages.40 Furthermore, a marked improvement in oral hygiene occurs as children age with a major turning point estimated to occur when children reach the age of approximately 11.41 This may increase protection from dental caries and may reduce the impact of any soft drink reformulation intervention, in older compared with younger children who may adopt a less effective brushing technique. As children age, they have increased autonomy for selecting their own food and drink. While it is possible that older children might be more likely to increase their consumption of sugar from other sources in order to compensate for lost sugar, through reformulation, previous studies have found no change in the level of sugar being purchased from food sources typically high in sugar such as confectionery, following the implementation of the SDIL.13
Age-related differences in feeding practices may also be an important reason, not factored into the previous modelling study, that could explain why younger children may appear to disproportionately benefit from SDIL-prompted reformulation.19 Expert opinion advises that use of infant bottles and sippy cups, especially those containing SSBs, should be avoided in the hour before bedtime because it increases the risk of dental caries due to a dramatic reduction in saliva production during sleep; ultimately leading to slow removal of dietary free sugars and in turn a low pH and a prolonged period of demineralisation of the teeth.42 One study found that approximately 50% of 4-year olds use a sippy cup and 11% continue to use an infant bottle.43 The use of these drinking vessels is likely to be rare in older children and thus in the context of SSBs and SDIL, infant bottles and sippy cups may therefore represent a unique risk factor in younger age groups that warrants further investigation.
In contrast to our findings, an empirical study examining taxes on unhealthy food and drink in Mexico reported reductions in dental caries in older children and adults but not children aged 1–5 years.21 Structural differences in the Mexican and UK taxes may explain these differences. In Mexico, the volume-based tax was fully passed on to the consumer in the form of increasing retail prices44 but there was no incentivisation for manufacturers to reformulate and reduce the sugar content of SSBs. In contrast, the UK SDIL was based on sugar density and was designed to encourage manufacturers to reformulate soft drinks, which they did.12 Furthermore, the Mexico study examined incident dental caries rather than the more severe carious dental extractions, precluding a direct comparison.
We observed reduced incidence rates of tooth extractions in children from all IMD fifths, except the middle group (IMD3). In contrast, a previous modelling study suggested SSB taxes would lead to greatest reductions in caries in the lowest income groups as they have the highest baseline SSB consumption.16 One potential reason why we did not find a clear trend in effect by IMD is that water fluoridation is more common in the most deprived areas in England. Nearly one-fifth (18.7%) of the population of England living in areas with fluoridated drinking water live in the most deprived tenth of areas.45 This additional protective factor was not considered in the modelling study.16
Our finding of an overall reduction in hospital admissions associated with the SDIL was not replicated in secondary analysis where the interruption point was moved to the date of SDIL implementation. This suggests that the biggest benefits to oral health occurred in the period between the SDIL announcement and implementation, when most reformulation took place.12
Conclusion
Using administrative data on hospital admissions, we found the announcement of the UK SDIL was associated with improvements in the incidence of hospital admissions for tooth extractions due to dental caries. These benefits were observed in children living in most areas regardless of deprivation and particularly in the youngest children (<9 years). This study provides evidence of possible benefits to children’s health from the UK SDIL beyond obesity which it was initially developed to address.
Footnotes
Twitter: @Nina_Tr_Rogers
Contributors: JA, MW, HR and OM conceptualised and acquired funding for the study. NTR and JA drafted the paper. NTR with help from JA and CHR was responsible for the methodology and carried out the formal data analysis. JA, MW and NTR had access to the data. NR accepts full responsibility for the work and had access to the data, and controlled the decision to publish. All authors were involved in data interpretation and critical reviewing of the manuscript. All authors accept responsibility for the decision to submit the publication.
Funding: NTR, OM, MW and JA were supported by the Medical Research Council (grant No MC_UU_00006/7). This project was funded by the NIHR Public Health Research programme (grant Nos 16/49/01 and 16/130/01) to MW. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health and Social Care, UK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: Noe declared.
Provenance and peer review: Not commissioned; externally peer reviewed by Dr Steven Kim, United Kingdom of Great Britain and Northern Ireland.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Data were acquired through a data sharing agreement with NHS digital for which conditions of use apply. Requests for data must be made directly to NHS digital and cannot be granted by the authors.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. World Health Organization . Guideline: sugars intake for adults and children. 2015. [PubMed]
- 2. GOV.UK . Child oral health: applying All Our Health, Available: https://www.gov.uk/government/publications/child-oral-health-applying-all-our-health/child-oral-health-applying-all-our-health
- 3. Bridgman CM, Ashby D, Holloway PJ. An investigation of the effects on children of tooth extraction under general anaesthesia in general dental practice. Br Dent J 1999;186:245–7. 10.1038/sj.bdj.4800076 [DOI] [PubMed] [Google Scholar]
- 4. Albadri SS, Lee S, Lee GT, et al. The use of general anaesthesia for the extraction of children’s teeth. results from two UK dental hospitals. Eur Arch Paediatr Dent 2006;7:110–5. [PubMed] [Google Scholar]
- 5. Public Health England . National dental epidemiology programme for England: oral health survey of 5-year-olds 2019 - A report on the variations in prevalence and severity of dental decay. 2020.
- 6. Boustedt K, Dahlgren J, Twetman S, et al. Tooth brushing habits and prevalence of early childhood Caries: a prospective cohort study. Eur Arch Paediatr Dent 2020;21:155–9. 10.1007/s40368-019-00463-3 [DOI] [PubMed] [Google Scholar]
- 7. Tinanoff N, Kanellis MJ, Vargas CM. Current understanding of the epidemiology mechanisms, and prevention of dental Caries in preschool children. Pediatr Dent 2002;24:543–51. [PubMed] [Google Scholar]
- 8. Griffith R, O’Connell M, Smith K, et al. What’s on the menu? policies to reduce young people’s sugar consumption. Fisc Stud 2020;41:165–97. 10.1111/1475-5890.12194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization . Together let’s beat NCDs. taxes on sugary drinks: Why do it? 2017.
- 10. Obesity Evidence Hub . Countries that have taxes on sugar-sweetened Beverages. 2021.
- 11. GOV.UK . Soft drinks industry levy comes into effect. 2018.
- 12. Scarborough P, Adhikari V, Harrington RA, et al. Impact of the announcement and implementation of the UK soft drinks industry levy on sugar content, price, product size and number of available soft drinks in the UK, 2015-19: A controlled interrupted time series analysis. PLOS Med 2020;17:e1003025. 10.1371/journal.pmed.1003025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rogers NT, Pell D, Mytton O, et al. n.d. Changes in soft drinks purchased by British households associated with the UK soft drinks industry levy: a controlled interrupted time series analysis. BMJ Open [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rogers NT, Cummins S, Forde H, et al. Associations between Trajectories of obesity prevalence in English primary school children and the UK soft drinks industry levy: an interrupted time series analysis of surveillance data. PLOS Med 2023;20:e1004160. 10.1371/journal.pmed.1004160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Urwannachotima N, Hanvoravongchai P, Ansah JP, et al. Impact of sugar-sweetened beverage tax on dental Caries: A simulation analysis. BMC Oral Health 2020;20:.:76. 10.1186/s12903-020-1061-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schwendicke F, Thomson WM, Broadbent JM, et al. Effects of taxing sugar-sweetened Beverages on Caries and treatment costs. J Dent Res 2016;95:1327–32. 10.1177/0022034516660278 Available: http://dx.doi.org/101177/0022034516660278 [DOI] [PubMed] [Google Scholar]
- 17. Sowa PM, Keller E, Stormon N, et al. The impact of a sugar-sweetened Beverages tax on oral health and costs of dental care in Australia. Eur J Public Health 2019;29:173–7. 10.1093/eurpub/cky087 [DOI] [PubMed] [Google Scholar]
- 18. Jevdjevic M, Trescher A-L, Rovers M, et al. The Caries-related cost and effects of a tax on sugar-sweetened Beverages. Public Health 2019;169:125–32. 10.1016/j.puhe.2019.02.010 [DOI] [PubMed] [Google Scholar]
- 19. Briggs ADM, Mytton OT, Kehlbacher A, et al. Health impact assessment of the UK soft drinks industry levy: a comparative risk assessment Modelling study. Lancet Public Health 2017;2:e15–22. 10.1016/S2468-2667(16)30037-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sowa PM, Birch S. The effects of a sugar-sweetened beverage tax: moving beyond dental health outcomes and service utilisation. Health Econ Policy Law 2023;18:139–53. 10.1017/S1744133122000147 [DOI] [PubMed] [Google Scholar]
- 21. Hernández-F M, Cantoral A, Colchero MA. Taxes to unhealthy food and Beverages and oral health in Mexico: an observational study. Caries Res 2021;55:183–92. 10.1159/000515223 [DOI] [PubMed] [Google Scholar]
- 22. White M, Scarborough P, Briggs A, et al. Evaluation of the health impacts of the UK Treasury Soft Drinks Industry Levy (SDIL). NIHR Public Health Research Programme, 2017. [Google Scholar]
- 23. Oxford Consultants for Social Inclusion . Why the indices of deprivation are still important in the open data era. 2011.
- 24. Office for National Statistics, National Records of Scotland, Northern Ireland Statistics and Research Agency – Population estimates, . 2020. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpop
- 25. Office for National Statistics . Population estimates for the UK, England and Wales. Scotland and Northern Ireland: mid-2020, 2021. [Google Scholar]
- 26. Broomhead T, Rodd HD, Baker SR, et al. A rapid review of variation in the use of dental general Anaesthetics in children. Br Dent J 2020;229:31–9. 10.1038/s41415-020-1846-6 [DOI] [PubMed] [Google Scholar]
- 27. NHS Digital . Children’s dental health survey. 2022.
- 28. Office for Health Improvement and Disparities . Sugar reduction – industry progress 2015 to 2020. final report for foods included in the programme and the latest data for drinks included in the soft drinks industry levy and juices and milk based drinks. 2022.
- 29. Department for Environment, Food & Rural Affairs and Food Standards Agency . Food labelling: giving food information to consumers. 2022.
- 30. Song J, Brown MK, Tan M, et al. Impact of color-coded and warning nutrition labelling schemes: A systematic review and network meta-analysis. PLoS Med 2021;18:e1003765. 10.1371/journal.pmed.1003765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Department of Health . A conscious decision. A review of the use of general anaesthesia and conscious sedation in primary dental care. Report by A group chaired by the Chief Medical Officer and the Chief Dental Officer. London: Department of Health, 2000. [Google Scholar]
- 32. Lawson J, Owen J, Deery C. How to minimize repeat dental general Anaesthetics. Dent Update 2017;44:387–95. 10.12968/denu.2017.44.5.387 [DOI] [PubMed] [Google Scholar]
- 33. Brown L, Kenny K, O’Sullivan E. Dental general anaesthetic pre-assessments completed by a specialist—does it change patient outcomes? A UK-based study. Int J Paediatr Dent 2018;29:162–8. 10.1111/ipd.12442 Available: https://onlinelibrary.wiley.com/toc/1365263x/29/2 [DOI] [PubMed] [Google Scholar]
- 34. Knapp R, Marshman Z, Rodd H. Treatment of dental Caries under general anaesthetic in children. BDJ Team 2017;4. 10.1038/bdjteam.2017.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Owen J. An impetus for change Br Dent J 2021;230:14–6. 10.1038/s41415-020-2507-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Alkhouri N, Sanders H, Waite C, et al. Variations in provision of dental general anaesthetic for children in England. Br Dent J 2022;1–6:1–6. 10.1038/s41415-022-4455-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kidd JB, McMahon AD, Sherriff A, et al. Evaluation of a national complex oral health improvement programme: A population data linkage cohort study in Scotland. BMJ Open 2020;10:e038116. 10.1136/bmjopen-2020-038116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Water fluoridation . Health monitoring report for England 2022. Office for Health Improvement & Disparities 2022. [Google Scholar]
- 39. Nyakutsikwa B, Walsh T, Pretty I, et al. Water fluoride concentrations in England, 2009-2020. Community Dent Health 2022;39:106–12. 10.1922/CDH_00267Nyakutsikwa07 [DOI] [PubMed] [Google Scholar]
- 40. Levine RS, Nugent ZJ, Rudolf MCJ, et al. Dietary patterns, Toothbrushing habits and Caries experience of schoolchildren in West Yorkshire, England. Community Dent Health 2007;24:82–7. [PubMed] [Google Scholar]
- 41. Krupińska-Nanys M, Zarzecka J. An assessment of oral hygiene in 7-14-year-old children undergoing orthodontic treatment. J Int Oral Heal JIOH 2015;7:6–11. [PMC free article] [PubMed] [Google Scholar]
- 42. Berkowitz RJ. Causes, treatment and prevention of early childhood Caries: a Microbiologic perspective. J Can Dent Assoc 2003;69:304–7. [PubMed] [Google Scholar]
- 43. Sealy PA, Farrell N, Hoogenboom A. Caregiver self-report of children’s use of the Sippy cup among children 1 to 4 years of age. J Pediatr Nurs 2011;26:200–5. 10.1016/j.pedn.2009.11.001 [DOI] [PubMed] [Google Scholar]
- 44. Colchero MA, Salgado JC, Unar-Munguía M, et al. Changes in prices after an excise tax to sweetened sugar Beverages was implemented in Mexico: evidence from urban areas. PLoS ONE 2015;10:e0144408. 10.1371/journal.pone.0144408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nyakutsikwa B, Allen T, Walsh T, et al. Who are the 10%? Characteristics of the populations and communities receiving fluoridated water in England. Community Dent Health, 2022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjnph-2023-000714supp001.pdf (164.8KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Data were acquired through a data sharing agreement with NHS digital for which conditions of use apply. Requests for data must be made directly to NHS digital and cannot be granted by the authors.