Abstract
Introduction and importance
Outflow tract disorders are uncommon causes of primary amenorrhea. Transverse vaginal septum (TVS) is a rare cause of outflow tract obstruction.
Case presentation
A 15-year-old female presented to us with severe abdominal pain. Abdominal examination revealed a boggy mass in the suprapubic region. The diagnosis was made following a history of primary amenorrhea, lower abdominal pain, and pelvic examination which revealed a vaginal septum. She had surgical resection of the vaginal septum and a mold was left in situ to keep the vagina patent during the healing process. The procedure was uneventful and she was able to achieve menstrual flow following surgery, septoplasty being performed after three months.
Discussion
Transverse vaginal septum is an unusual cause of primary amenorrhea. These lesions, albeit rare, usually have a typical presentation and are amenable to surgical management.
Conclusion
Although transverse vaginal septum is a rare diagnosis in our practice, it is important to establish early diagnosis and carry out proper management so as to preserve normal physiology and fertility as well as to prevent complications.
Keywords: Outflow tract disorder, Primary amenorrhea, TVS, Case report
Highlights
-
•
TVS are rare outflow tract anomalies that can cause primary amenorrhea.
-
•
Presentation varies with age and diagnosis is in totality of clinical and radiologic findings.
-
•
While septoplasty is definitive, psychosocial support is an important aspect in management.
1. Introduction
Primary amenorrhea is defined by the absence of menstruation by the age of 15 years in the presence of normal growth and secondary sexual characteristics and/or the absence of menses by 13 years of age if there is a complete absence of secondary sexual characteristics [1]. Outflow tract disorders constitute about 20 % of cases of primary amenorrhea [2]. Transverse vaginal septum (TVS) is rare outflow tract disorders that may sometimes cause primary amenorrhea. These congenital abnormalities of the vagina have reported incidence ranging from 1 in 30,000 to 1 in 80,000 females [3]. The septa are usually less than a centimeter thick and are variably located in the vagina.
Herein, we illustrate a case of a 15-year-old female presenting to our facility with primary amenorrhea secondary to high TVS and its surgical management. Our work has been reported in line with the SCARE Guidelines 2020 criteria [4].
2. Case presentation
A 15-year-old, unmarried, sexually inactive female, yet to attend her menarche, presented to the emergency department of our hospital with the chief complaint of severe lower abdominal pain for 2 h. The pain was acute, severe (8 out of 10 on the pain scale), throbbing type, in the suprapubic and periumbilical region, and non-radiating. Her past medical and surgical history were non-revealing.
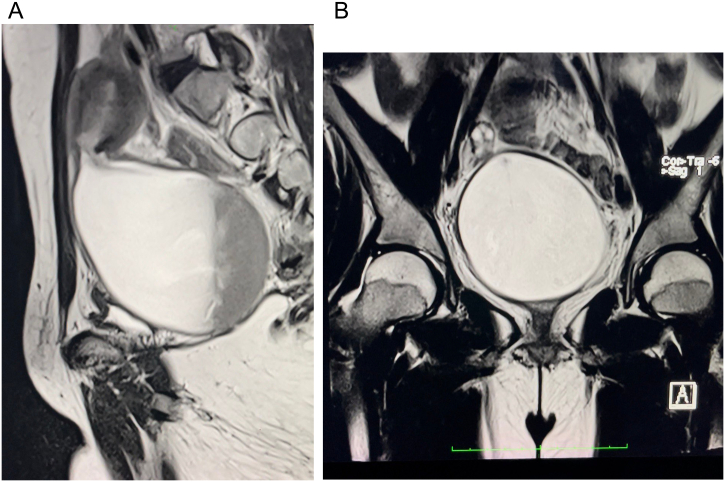
On examination, our patient had a blood pressure of 100/70 mm Hg, pulse rate of 88 beats per minute, respiratory rate of 22 breaths per minute, oxygen saturation of 96 %, and temperature of 101 F. Her height and weight were 152 cm and 45 kg respectively (Body Mass Index BMI 19.5 kg/m2). The secondary sexual characteristics were well-developed. Abdominal examination revealed a boggy mass (approximately 14 weeks in size) in the suprapubic region extending to the left iliac fossa which was firm, non-mobile and mildly tender. Per speculum examination and per vaginal examination were planned for during Evaluation Under Anesthesia (EUA). Baseline laboratory investigations were within normal limits. Ultrasonography showed a large echogenic fluid collection (approx 500 cc) in the cervicouterine cavity suggestive of hematocolpometra. Magnetic Resonance Imaging, MRI (Fig. 1) showed a loculated fluid collection with dependent layering, grossly distending the endocervical canal and vagina, and displacing the uterus superiorly. Due to suspected infection, antibiotics were started.
Fig. 1.
MRI findings a) saggital, b) coronal showing loculated fluid collection with dependent layering, grossly distending the endocervical canal and vagina and displacing the uterus superiorly.
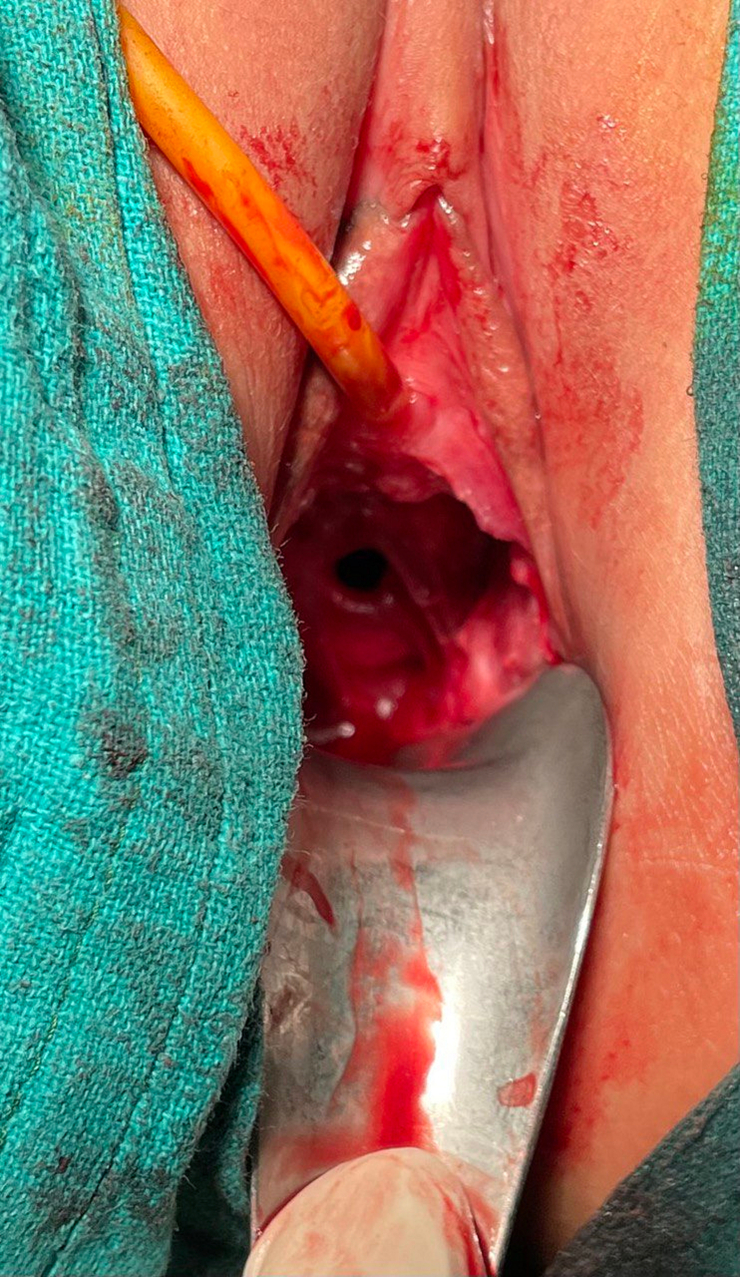
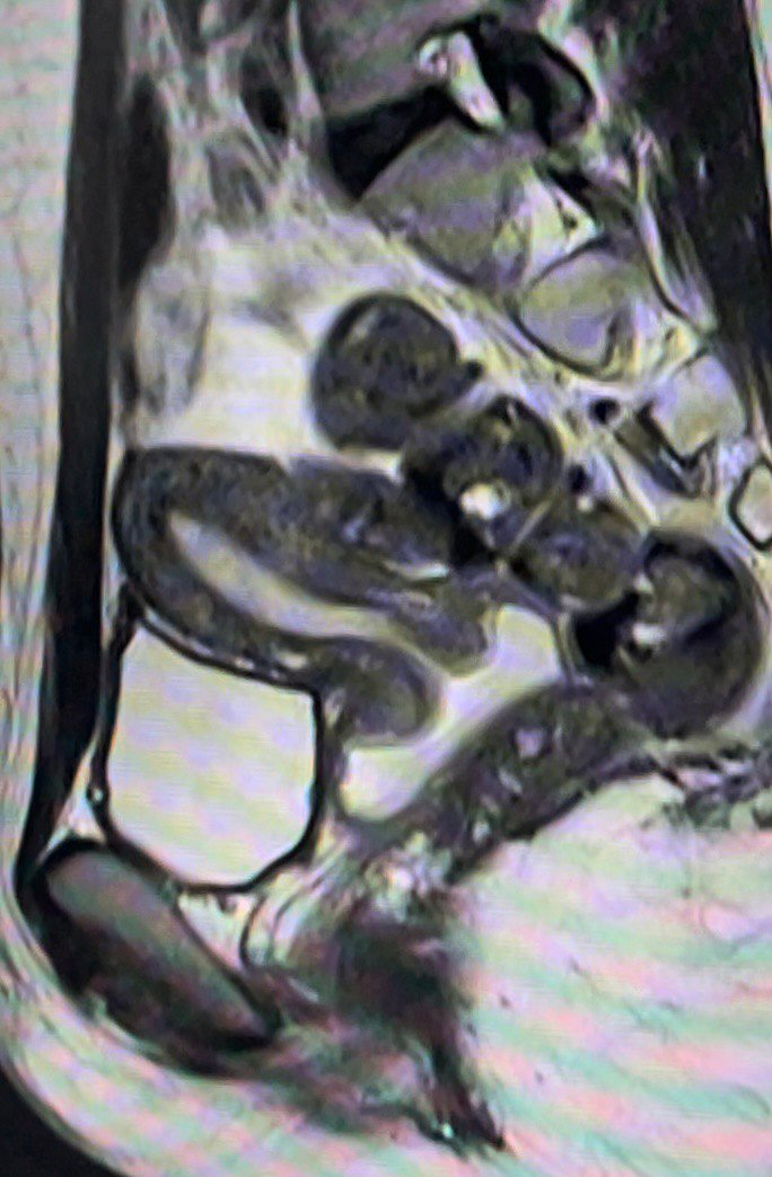
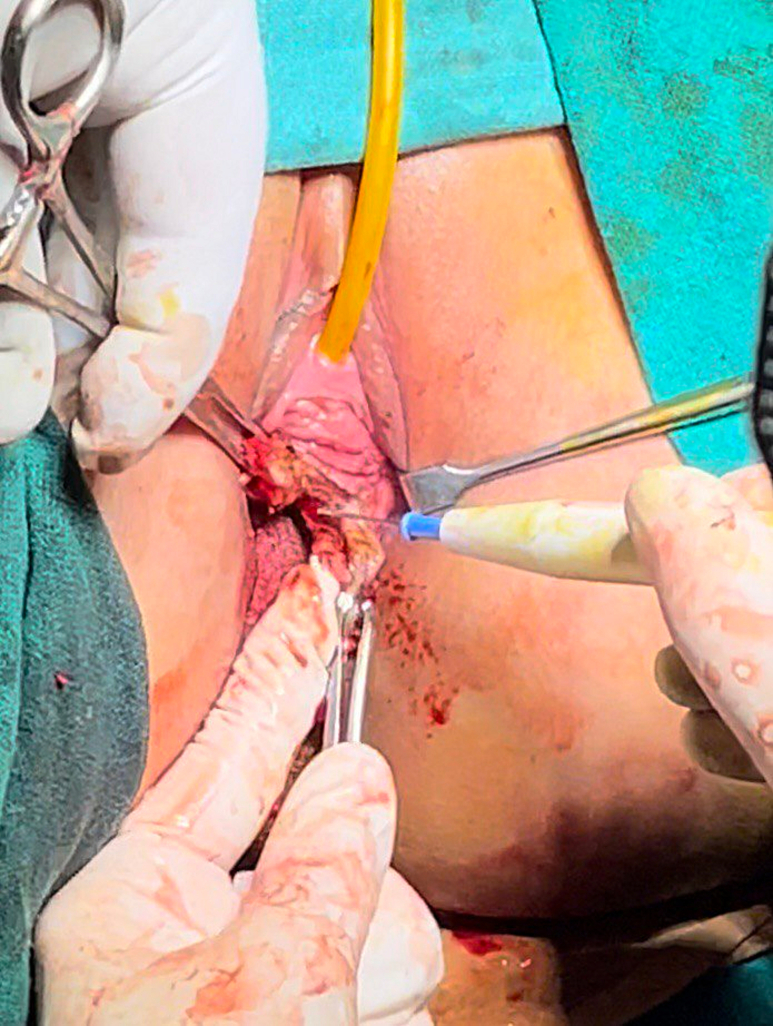
EUA (Fig. 2) showed a blind-ending lower two-thirds of the vagina, and cervix was not visualized. A boggy mass was felt anteriorly on rectal examination and the cervix was not felt. Nick incision was given on the junction of the upper one-third and lower two-thirds of TVS (identified retrospectively) after which the vaginal epithelium opened. A bluish, bulging mass was seen and a 2 cm transverse incision was given on the most dependent part. Approximately 800 ml of blood and foul-smelling mucopus were drained. A mold was made of a 3 ml syringe plunger wrapped with condom and was left in the created opening to maintain patency. Postoperatively, full course of antibiotics were continued. On examination during the second postoperative day, the cervix was not visualized but could be felt through that opening. A thick fold of soft tissue was covering the cervix which was then identified as TVS (Fig. 3). Her postoperative period was uneventful. Psychosocial support and counseling were provided throughout. She was subsequently discharged home and was instructed on how to use a dilator for maintaining vaginal patency. This was done satisfactorily. At one-month follow-up, the outflow tract was patent, and menstruation was achieved. MRI (Fig. 4) showed mild collection in the uterine cavity. Septoplasty was done after 3 months (Fig. 5). At six months and one-year follow-up, menses were regular and the outflow tract was patent.
Fig. 2.
Examination under anesthesia revealed a blindly ending vagina.
Fig. 3.
Reveal of TVS after nick incision.
Fig. 4.
MRI at one month post-procedure showing mild collection in the cervico-uterine cavity.
Fig. 5.
Intraoperative image showing resection of the septum.
3. Discussion
A vaginal septum is an uncommon outflow tract disorder that occurs due to a fusion defect resulting in a fibrous band of variable thickness within the vaginal canal. The septum may be transverse or longitudinal in orientation and can be complete (with obstruction) or incomplete (with fenestrations) [5]. Transverse vaginal septum is a rare Mullerian anomaly that results from failure of fusion and/or canalization of the urogenital sinus with the Mullerian ducts. TVS are commonly classified on the basis of their location: low (14 %), mid (40 %), and high TVS (46 %). These are also classified on the basis of thickness, most being less than a cm thick [6]. Children usually present with mucocolpos. Adolescents may present with muco/hematocolpos or pyohematocolpos (if secondarily infected). In our case, the septum was unusually thick and our patient had pyohematocolpos with fever which led to difficulty in establishing the diagnosis as it mimicked a synechiae.
The diagnosis of TVS is usually established in totality of clinical and radiological findings. An obstructive genital anomaly should be considered in all young women who present with the typical symptoms mentioned and have primary amenorrhea. Imperforate hymen and TVS are the main differential diagnoses, and these can be distinguished by physical examination. A bluish bulge is often seen between the labia in the case of an imperforate hymen which undergoes visible distention on application of suprapubic pressure, this being absent in the case of TVS [7].
Ultrasonography (USG) is cheap and easily accessible modality to investigate a case of suspected TVS or any congenital outflow tract abnormality. USG helps to define the location as well as thickness of the septum. It also helps in estimating the distance from introitus as well as in looking out for any other abnormalities that may be present [8].
MRI is the best modality for evaluating a case of TVS as it gives information about the orientation, site, distance from introitus, septal thickness and any concomitant genitourinary abnormalities that may be present as well as ruling out cervical agenesis. The classic MRI sign associated with TVS is an abrupt cutoff of vaginal caliber with or without hydro or hematocolpos [9].
The management of TVS is primarily surgical, which is aimed at removal of the septum without significantly shortening the vaginal canal. Various techniques are described in the literature, the most popular being resection and anastomosis. Recommendations are that in cases of complete TVS with hematocolpos, initial incision and drainage and delayed reconstruction (6–8 weeks) result in better outcomes, as was the management strategy adopted in our case [7]. Our patient could not undergo the procedure due to her educational commitments within eight weeks and thus we did the procedure at three months.
The exact surgical technique used to anastomose the vagina depends on the thickness of the TVS. A thin septum can be repaired relatively easily with an end-to-end anastomosis especially if located low in the vagina [7]. Thicker septa may require undermining the vaginal mucosa to allow the lower vagina to reach the upper vagina. This may lead to postoperative scar constriction and vaginal stenosis, requiring further surgery or dilatation [10]. To decrease the risk of post-operative stenosis, a Z-plasty may be performed, thereby allowing scarring to occur longitudinally instead of transversely [7]. In cases of very thick TVS and lack of perioperative dilation, a skin graft may be required for anastomosis. The risk of vaginal stenosis can be decreased after surgery by the use of a vaginal mold or dilator and preoperative use to thin the TVS is also suggested [11]. In recent times, vaginoscopic hysteroscopy has emerged as an effective modality for septal resection. The added advantage with this approach is that it helps with hymen preservation in young women as well as in societies with socio-cultural barriers [7].
The difficulty in this scenario was obtaining vaginal dilators because they weren't easily accessible, requiring us to use a makeshift dilator. Young teenagers and families who are not emotionally ready to use such equipment may find the idea of mold or dilators quite traumatic, especially in low-income countries where this may be considered socially or religiously unacceptable. Patient counseling is important in this regard.
4. Conclusion
Patients with primary amenorrhea should be actively evaluated for underlying causes. Although vaginal abnormalities such as TVS are rare in our practice, it is important to establish early diagnosis and proper management of these surgically amenable lesions to preserve normal physiology and fertility and prevent complications. Psychosocial support is an important aspect of management, especially for adolescents.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
No ethical approval necessary.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Chapagain S, Khadka B, Lama CS, Shrestha S and Karn M designed the report, reviewed the literature, edited the images and wrote the paper; Devkota S and Pandit C revised the paper. All the authors have read and approved the final manuscript.
Guarantor
Chandika Pandit.
Research registration
None.
Disclaimer
No patient or author details are included in the figures.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors report no conflicts of interest.
References
- 1.Williams C.E., Nakhal R.S., Hall-Craggs M.A., Wood D., Cutner A., Pattison S.H., Creighton S.M. Transverse vaginal septae: management and long-term outcomes. BJOG. 2014;121:1653–1658. doi: 10.1111/1471-0528.12899. [DOI] [PubMed] [Google Scholar]
- 2.Acién P., Acién M. Diagnostic imaging and cataloguing of female genital malformations. Insights Imaging. 2016;7:713. doi: 10.1007/S13244-016-0515-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rock J.A., Azziz R. Genital anomalies in childhood. Clin. Obstet. Gynecol. 1987;30:682–696. doi: 10.1097/00003081-198709000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. Dec. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Paudel R., Dangal G., Karki A., Pradhan H., Shrestha R., Bhattachan K., Bajracharya N. Primary amenorrhoea with transverse vaginal septum presented with infected pyometra of 24 weeks size, Nepal. J. Obstet. Gynaecol. 2017;12:66–68. doi: 10.3126/njog.v12i1.18986. [DOI] [Google Scholar]
- 6.Joki-Erkkilä M.M., Heinonen P.K. Presenting and long-term clinical implications and fecundity in females with obstructing vaginal malformations. J. Pediatr. Adolesc. Gynecol. 2003;16:307–312. doi: 10.1016/S1083-3188(03)00157-8. [DOI] [PubMed] [Google Scholar]
- 7.Scutiero G., Greco P., Iannone P., Bernardi G., Greco F., Nappi L. Management of transverse vaginal septum by vaginoscopic resection: hymen conservative technique. RBGO Gynecol. Obstet. 2018;40:642. doi: 10.1055/S-0038-1670714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puscheck E.E., Cohen L. Congenital malformations of the uterus: the role of ultrasound. Semin. Reprod. Med. 2008;26:223–231. doi: 10.1055/S-2008-1076141. [DOI] [PubMed] [Google Scholar]
- 9.Zulfiqar M., Shetty A., Yano M., McGettigan M., Itani M., Naeem M., Ratts V.S., Siegel C.L. Imaging of the vagina: spectrum of disease with emphasis on MRI appearance. Radiographics. 2021;41:1549–1568. doi: 10.1148/RG.2021210018. [DOI] [PubMed] [Google Scholar]
- 10.Lacy J., Correll G.R., Walmer D.K., Price T.M. Simple vaginal mold for use in the postoperative care of patients with a transverse vaginal septum. Fertil. Steril. 2007;87:1225–1226. doi: 10.1016/J.FERTNSTERT.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Hurst B.S., Rock J.A. Preoperative dilatation to facilitate repair of the high transverse vaginal septum. Fertil. Steril. 1992;57:1351–1353. doi: 10.1016/S0015-0282(16)55102-4. [DOI] [PubMed] [Google Scholar]