Abstract
Background
Self-paced internet interventions for gambling problems offer cost-effective, accessible, and private alternatives to traditional psychotherapy for a population that rarely seeks help. However, these interventions have been relatively slow to develop, evaluate, and deploy at scale relative to those for other addictive behaviors. Moreover, user engagement remains low despite the high interest. Motivational interviews have improved the effectiveness gambling bibliotherapy but have not been augmented with an analogous web-based self-guided program.
Objectives
This trial aimed to replicate and extend prior work by translating a paperback workbook to the internet and pairing it with a single motivational interview. It was hypothesized that the motivational interview would enhance program engagement and gambling outcomes.
Methods
A two-arm randomised controlled trial was conducted. Treatment-seeking Canadian adults recruited solely via social media received one year of access to a web-based self-guided program, either alone (N = 158) or in combination with a virtual motivational interview completed upon enrolment (N = 155). The program was based on principles of cognitive-behavioral therapy and motivational interviewing. Gambling severity, expenditures, frequency, and duration were assessed via online questionnaires at baseline and 3-, 6-, and 12-months post-baseline, along with secondary outcomes (i.e., depression, anxiety, nonspecific psychological distress, alcohol consumption).
Results
Baseline characteristics were indicative of severe gambling problems and concurrent mental health problems but not problematic alcohol consumption in this sample. Both treatment groups demonstrated roughly equal improvements across all gambling outcomes and most secondary outcomes over time, except alcohol consumption, which did not meaningfully change. Changes were most prominent by 3 months, followed by more gradual change by 6 and 12 months. Only 57 % of gamblers who were assigned to receive a motivational interview completed that interview. About 40 % of users did not complete any program modules and 11 % completed all four. No group differences in program engagement were observed, although the number of modules completed was associated with greater reductions in gambling behaviors in both groups.
Discussion
The problem of user engagement with web-based self-help programs remains. There is a dose-response relationship between engagement and outcomes when engagement is measured in terms of therapeutic content completed.
Conclusions
The addition of a motivational interview to a web-based self-help program for gambling problems was unsuccessful in improving engagement or outcomes. Future work should aim to make self-guided programs more engaging rather than solely making users more engaged.
Trial registration
Registered on 7 July 2020 (ISRCTN13009468).
Keywords: Self-help, Gambling disorder, Internet intervention, Randomised controlled trial, Motivational interviewing, User engagement
Highlights
-
•
Web-based self-help interventions for gambling problems are few but in high demand.
-
•
User engagement with these interventions remains low.
-
•
There is a dose-response relationship between engagement and outcomes.
-
•
Motivational interviewing was unable to enhance outcomes in this context.
-
•
Motivational interviewing itself may be subject to the engagement problem.
1. Introduction
1.1. Background
In Canada, past-year estimates of problem gambling and at-risk gambling approximate 0.6 % and 2.7 %, respectively (Williams et al., 2020). However, >85 % of individuals with gambling problems do not obtain formal or informal treatment (Hodgins et al., 2022; Petry et al., 2017). Indeed, only one in 25 at-risk gamblers and one in five problem gamblers seek professional help (Bijker et al., 2022), while as many as 90 % who make a change attempt do so independently (Hodgins et al., 2022). Several low-intensity interventions have thus been developed to reduce the threshold for treatment access, limit demands on users, and address the treatment preferences of people with gambling problems, such as privacy and self-pacing (Andersson, 2016; Andersson and Titov, 2014). Such interventions, particularly when delivered online, offer a cost-effective and flexible alternative to traditional treatments (e.g., weekly face-to-face psychotherapy).
A number of self-guided gambling interventions have been developed and implemented (Boumparis et al., 2022; Brazeau and Hodgins, 2021). One workbook was developed by (Hodgins and Makarchuk, 2002) and composed of four modules based on cognitive-behavioral principles. The original paperback version has been evaluated in multiple trials (Abbott et al., 2012; Hodgins et al., 2001; Hodgins et al., 2004; Hodgins et al., 2009), and more recently, the online version has too (Cunningham et al., 2019a; Hodgins et al., 2019). The results of these trials suggest that workbook effectiveness held without therapist contact, although brief contact appears to enhance uptake and outcomes. Indeed, differential improvements in gambling severity and frequency were still detected at 24 months when the paperback version was supplemented with a single motivational interview (MI) upon study enrollment (Hodgins et al., 2004). Of note, additional MI booster sessions have not appeared to offer incremental benefit over an initial session in this context (Hodgins et al., 2009).
Internet-based interventions have shown promise when used to improve a variety of health behaviors, such as diet, physical activity, and other substance-related and behavioral addictions (Boumparis et al., 2022; Afshin et al., 2016; Boumparis and Schaub, 2022). However, internet interventions for gambling problems have been relatively slower in their development, evaluation, and scaled deployment. Moreover, despite the success of these interventions, user engagement remains a significant barrier to the treatment of people with addictions (Borghouts et al., 2021; Newman et al., 2011; Ramos et al., 2021). In two comparable gambling trials, only 24 % (Wall et al., 2021) and 31 % (Hodgins et al., 2019) of gamblers accessed all of the therapeutic material within their online program. As many as 40 % do not return to their program after the initial visit (Hodgins et al., 2019; Brazeau, 2021). A balance must be struck such that users are supported enough to maintain their engagement, without that support being so involved that users are deterred from engaging in the first place given the premium they place on privacy and independence. Given the need to strike this balance, as well as the effectiveness of MI in small doses, MI represents a strong candidate to augment online self-help programs. MI is hypothesized to enhance intrinsic motivation and commitment to behavior change (Miller and Rollnick, 2023). Along those lines, it would be expected that MI could increase the motivation of gamblers to engage in self-help. In theory, MI is useful because it encourages recipients to generate their own reasons for change and strengthen their perceived ability to implement changes (Miller and Rollnick, 2023). Interactive therapeutic contact, including that of MI, also allows providers to respond to participants in the moment and gently correct or redirect them as needed. For instance, MI makes use of directive open-ended questions that specifically elicit participants' reasons for wanting to make changes.
To date, there has been mixed evidence for the inclusion of brief therapeutic contact in order to enhance outcomes of internet interventions for gambling problems (Hodgins et al., 2009; Carlbring and Smit, 2008; LaBrie et al., 2012; Luquiens et al., 2016). Our own line of research has suggested that a single MI session can serve this purpose effectively when paired with a self-paced paperback workbook (Hodgins et al., 2001; Hodgins et al., 2004). The current trial aimed to replicate and extend this finding by translating the workbook to an online program and pairing it with one MI session upon enrollment.
1.2. Objectives
The purpose of this study was to explore whether an online self-guided program for gambling problems could have a more pronounced benefit when paired with minimal clinician contact in the form of a single MI delivered virtually. The specific objectives were twofold: 1) replicate, in the context of virtual care, the finding that supplemental motivational enhancement improves self-directed gambling treatment outcomes; and 2) test the hypothesis that supplemental motivational enhancement increases online self-help treatment engagement of individuals seeking treatment for gambling problems.
1.3. Hypotheses
This trial randomly assigned participants to one of two conditions: internet program only (IO) or internet program plus motivational interview (IMI). The five hypotheses and one research question were:
Hypothesis 1
(H1): Those in both the IO and IMI groups will experience a reduction in gambling severity over the course of treatment. However, this reduction is expected to be more pronounced for those in the IMI condition.
Hypothesis 2
(H2): Those in both the IO and IMI groups will experience a reduction in monthly gambling expenditures over the course of treatment. However, this reduction is expected to be more pronounced for those in the IMI condition.
Hypothesis 3
(H3): Those in both the IO and IMI groups will experience a reduction in gambling frequency and duration over the course of treatment. However, this reduction is expected to be more pronounced for those in the IMI condition.
Hypothesis 4
(H4): Reductions in gambling problems for both the IO and IMI groups will be positively correlated with intervention engagement (i.e., number of logins, duration of time spent on the program, and number of program modules completed).
Hypothesis 5
(H5): The IMI group will demonstrate greater adherence (i.e., more modules completed) compared to the IO group.
Question 1
(Q1): Will there be a difference in online program ratings between IO and IMI groups?
2. Methods
2.1. Ethics approval
Complete details of this trial protocol were published elsewhere (Brazeau et al., 2021). Since that publication, one amendment (i.e., increase target sample size) was agreed upon by the researchers and ethically approved prior to implementation. Results for the 3-month outcomes and program usage data on the first 123 participants were also reported in a master's thesis (Brazeau, 2021). Ethics approval for this trial was obtained in May 2020 from the Conjoint Faculties Research Ethics Board at the University of Calgary. Participants were compensated with e-gift cards valued at CAD$10 for completing the baseline assessment and, if applicable, the MI session. They were also compensated with CAD$30 e-gift cards for each follow-up assessment completed (3-, 6-, and 12-months), for a total possible CAD$100 per participant. Data collection for 24-month outcomes is ongoing, and thus participants can earn an additional CAD$30 in e-gift cards. Once those data have been collected, the trial will be terminated.
2.2. Recruitment and randomisation
Participants were recruited across Canada with targeted advertisements posted to internet media sites (i.e., Facebook, Instagram, Kijiji, Google, Twitter, and Reddit). Some were also recruited via direct contact from the researchers using a contact list of past participants from prior studies in our lab. Inclusion criteria were: a) residence in Canada; b) 18 years of age or older; c) gambled at least once in the past month; d) score of 5 or greater on the Problem Gambling Severity Index (PGSI) (Currie et al., 2013; Ferris and Wynne, 2001); and e) not involved in other psychosocial gambling treatment at the time of enrollment. Exclusion criteria were: a) unable or unwilling to provide a phone number and email address; and b) unable or unwilling to access the online program and create an account. After registering for the program, participants were randomised with MINIM (Evans et al., 2017) in a 1:1 ratio to either the IO or IMI group. Randomisation was stratified by sex, PGSI gambling severity, and whether they had ever received prior gambling treatment. Eligibility screening, as well as baseline and follow-up assessments, were completed within Qualtrics.
2.3. Interventions
2.3.1. Internet Only (IO)
The IO group was provided with one year of unrestricted access to an online program (eHub Health Pty Ltd, 2023) based on the paperback workbook discussed earlier (Hodgins and Makarchuk, 2002). It consists of four self-paced, repeatable modules that cover self-assessment, goal setting, goal implementation, and goal maintenance. Modules were informed by the principles of cognitive-behavioral therapy and motivational interviewing (Hodgins et al., 2001). Users were informed of their yearlong unrestricted access and instructed via email to complete the workbook activities in any order, at any pace, and as many times as they would like. In terms of self-assessment, users can complete a PGSI to view their risk category, identify reasons for and consequences of gambling, and calculate how much money they spent gambling in the past month. The second module helps users make a recovery decision (i.e., abstinence or moderation) with a decisional balance exercise to weigh benefits and costs of gambling. In the third module, users can engage with several cognitive, behavioral, and practical strategies for coping with urges (e.g., completing thought records, identifying social supports, limiting access to money). Finally, the fourth module helps users identify triggers and other life stressors and facilitates proactive strategies for dealing with those triggers. Activities within each module were most often formatted as fillable tables (e.g., thought record, decisional balance) or surveys (e.g., identifying triggers, selecting coping strategies). Program use in the IO group was unguided in order to prevent confounding MI with general human contact or support; this has been recommended by past research which has not separated self-help from community support or general therapist contact (Carlbring and Smit, 2008).
2.3.2. Internet plus motivational interview (IMI)
The IMI group was provided with the same program access as those in the IO group, plus one brief MI session delivered via Microsoft Teams within the first two weeks of study enrollment. Motivational interviewing involves the assessment of a client's readiness for change, followed by the facilitation of behavioral change by exploring ambivalence, building commitment, and eliciting reasons for change (Miller and Rollnick, 2023). Clinical psychology graduate students were trained to conduct the motivational interviews. Within each MI session, facilitators first elicited participants' gambling concerns and reasons for seeking treatment by using several MI strategies (e.g., directional open-ended questions). Participants were then given personalized PGSI feedback and prompted to reflect on their risk category. Past attempts to quit or moderate gambling or other addictions were also discussed with an emphasis on current applicability. Participants were asked to commit to their gambling goal, whether abstinence or moderation. Consistent with the spirit of MI, empathetic affirmations and reflections were delivered throughout every session. Finally, facilitators used MI strategies to inquire about the workbook (e.g., asking whether participants accessed it yet and how they believe it will help them).
2.4. Measures
2.4.1. Primary outcomes
Gambling problem severity and diagnostic status were measured with the NODS-GD (Brazeau and Hodgins, 2022), which is a 16-item revision of the original NODS (Gerstein et al., 1999) based on DSM-5 diagnostic criteria for gambling disorder (α = 0.82 in this sample). Gambling duration (hours) and expenditures (dollars lost), per month and per session, were probed with retrospective open-ended self-report questions adapted from the Gambling Participation Instrument (GPI) (Williams et al., 2017). Past month gambling frequency was queried with an ordinal scale, also adapted from the GPI. All primary outcomes were assessed at baseline and each follow-up time point.
2.4.2. Secondary outcomes
Depression symptoms were measured with the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001) (α = 0.71 in this sample). Anxiety symptoms were identified with the Generalized Anxiety Scale-7 (GAD-7) (Spitzer et al., 2006) (α = 0.75 in this sample). Nonspecific psychological distress was assessed with the Kessler Psychological Distress Scale-10 (K−10) (Kessler et al., 2002) (α = 0.92 in this sample). Alcohol consumption was measured with the Alcohol Use Disorder Identification Test – Consumption (AUDIT-C) (Bradley et al., 1998) (α = 0.78 in this sample). All secondary outcomes were assessed at baseline and each follow-up time point. The inclusion of secondary outcomes in addition to gambling is consistent with best practices in gambling intervention research (Walker et al., 2006).
2.4.3. Program evaluation and engagement
Participants' experiences and perceptions of the online program were assessed at all follow-up time points with the Internet Evaluation and Utility Questionnaire (IEUQ) (Ritterband et al., 2008) (α = 0.90 in this sample). Questions were related to ease of use, convenience, subjective engagement, mode of delivery, and likelihood of returning. In addition to the IEUQ, objective user engagement data was collected monthly from the program website. These data included number of logins, duration of time spent on each module, and which modules were in progress or completed.
2.4.4. Sample size estimation
The sample size was computed using G*Power (Erdfelder et al., 1996) based on a repeated-measures between-factors analysis of variance, a simpler derivative of the generalized linear model that the primary analyses were based on (Hodgins et al., 2013; Liang and Zeger, 1986). Accounting for 30 % attrition over 12 months, the targeted sample size (N = 310) was designed to detect small to medium effect sizes that correspond to approximately two days less gambling per month and a 1-point decrease in NODS scores at each follow-up time point (Hodgins et al., 2013), which are sufficiently large to have clinical relevance.
2.4.5. Data analysis
All data analyses were conducted using R and RStudio (R Core Team, 2020) using the packages mice (Buuren and Groothuis-Oudshoorn, 2011), gee (Carey and Ripley, 2022), and emmeans (Lenth, 2023). <5 % of the primary outcome data were missing (MCAR). Given that missing data were few and MCAR, multiple imputation would not add information but would increase standard error estimates (Jakobsen et al., 2017). Therefore, analyses were only executed on complete cases for each outcome variable. Outcome data were all non-normally distributed; thus, logarithmic transformations were applied to approximate normality and identify outliers. Implausible values were removed (e.g., if participants reported spending more money per session than per month or gambling >24 h per day). Plausible outliers were retained; however, log hours and expenditures that exceeded the interquartile range (IQR) upper limit were recoded to the next highest value plus 1 for the main analyses. For all analyses, participants were first grouped according to the intent-to-treat approach (i.e., based on initial randomisation), then analyzed by the per-protocol approach (i.e., based on whether they actually completed an MI session). In other words, participants randomised to the IMI group who did not complete their MI session were reassigned to the IO group for per-protocol analyses, but kept in the IMI group for intent-to-treat analyses. Ultimately, results did not differ when data were analyzed according to intent-to-treat versus per-protocol, so we report only the results of the intent-to-treat analyses.
Generalized estimating equations (GEE) were used to test H1–H3, with intervention group as the between-subjects factor (IO, IMI) and time as the within-subjects factor (baseline, 3 months, 6 months, 12 months). The first-order autoregressive correlation structure was used. Primary gambling outcomes were diagnostic severity (NODS-GD score), total monthly expenditures (dollars), total monthly duration (hours), and past-month frequency. H4 was analyzed with bivariate Pearson correlations between user engagement and gambling outcomes. H5 and Q1 were analyzed with unpaired t-tests that compared program engagement and IEUQ ratings between the IO and IMI groups.
3. Results
3.1. Participants
Canadian adults seeking treatment for gambling problems were recruited over 22 months from August 18, 2020, to May 24, 2022, via internet advertisements and direct email contact from researchers (62 % Facebook, 14 % Kijiji, 10 % direct contact, 4 % Instagram, 4 % Google, 6 % other). The final sample (N = 313) had a mean age of 39.0 years (SD = 11.9, range = 18–70) and comprised 57 % females. Most participants (66 %) were White and 11 % were Indigenous. The majority met diagnostic criteria for gambling disorder (GD) upon enrollment (87 %), and only 4 % had received previous treatment for gambling problems. A sizable minority of participants (20 %) were unemployed at the time of recruitment, but most (62 %) reported full-time or part-time work. Baseline scores on the PHQ-9, GAD-7, K-10, and AUDIT-C were indicative of concurrent mental health symptoms but not alcohol use problems in this sample. No significant differences were observed between intervention groups on any baseline characteristics (Table 1).
Table 1.
Sample baseline characteristics.
| Baseline characteristic |
Descriptive statistics |
||||
|---|---|---|---|---|---|
| IO group (n = 158) |
IMI group (n = 155) |
Total (N = 313) |
t/ | p | |
| Age in years, mean (SD) | 39.9 (11.9) | 38.0 (11.9) | 39.0 (11.9) | 1.09 | .276 |
| Female sex, n (%) | 89 (56) | 90 (58) | 179 (57) | 0.36 | .836 |
| Married or common-law, n (%) | 49 (31) | 56 (36) | 105 (34) | 0.92 | .338 |
| Any post-secondary education, n (%) | 113 (72) | 106 (68) | 219 (70) | 0.37 | .546 |
| White ethnicity, n (%) | 109 (69) | 98 (63) | 207 (66) | 1.16 | .282 |
| Employed full- or part-time, n (%) | 93 (59) | 102 (66) | 195 (62) | 1.61 | .205 |
| Household income ≥ $30,000, n (%) | 110 (70) | 110 (71) | 220 (70) | 0.07 | .794 |
| PGSI score, mean (SD) | 16.6 (5.3) | 16.5 (5.5) | 16.6 (5.4) | 0.14 | .888 |
| Met criteria for GD diagnosis, n (%) | 144 (91) | 128 (83) | 272 (87) | 3.77 | .052 |
| NODS-GD score, mean (SD) | 7.3 (1.8) | 7.0 (2.0) | 7.1 (1.9) | 1.13 | .261 |
| Expenditures per month, mean (SD) | 1663 (2660) | 1577 (2945) | 1620 (2801) | 0.61 | .544 |
| Expenditures per session, mean (SD) | 241 (393) | 280 (645) | 260 (530) | 0.56 | .575 |
| Hours per month, mean (SD) | 45.9 (46.9) | 42.0 (51.3) | 44.0 (49.1) | 0.75 | .454 |
| Hours per session, mean (SD) | 3.5 (2.5) | 3.2 (2.4) | 3.4 (2.5) | 0.96 | .339 |
| Gambled once/week or more, n (%) | 145 (92) | 143 (92) | 288 (92) | 0.03 | .874 |
| Had previous treatment, n (%) | 4 (3) | 7 (5) | 11 (4) | 0.39 | .533 |
| Abstinence treatment goal, n (%) | 79 (50) | 82 (53) | 161 (51) | 0.08 | .780 |
| K-10 score, mean (SD) | 19.5 (7.6) | 20.8 (7.7) | 20.1 (7.6) | 1.38 | .170 |
| PHQ-9 score, mean (SD) | 12.1 (5.7) | 12.7 (5.8) | 12.4 (5.8) | 0.64 | .524 |
| GAD-7 score, mean (SD) | 9.6 (4.7) | 10.5 (4.9) | 10.1 (4.8) | 1.43 | .153 |
| AUDIT-C score, mean (SD) | 3.6 (2.8) | 3.6 (2.9) | 3.6 (2.9) | 0.10 | .917 |
| Recruited from Facebook, n (%) | 100 (63) | 93 (60) | 193 (62) | 0.36 | .549 |
At baseline, participants estimated gambling a mean of 44.0 h per month (Mdn = 28, SD = 49.1, range = 0–300) and 3.4 h per gambling episode (Mdn = 3, SD = 2.5, range = 0–12). They also reported a mean net loss of $1620 per month (Mdn = $700, SD = $2801, range = $15–$27,000) and $260 per gambling episode (Mdn = $100, SD = $530, range = $0–$6000) over the three months prior to their enrollment. The most endorsed types of gambling were instant or scratch tickets (73 %), lottery-type games (62 %), casinos (60 %), slot machines (57 %), and video lottery terminals (32 %). Sports betting of any kind was not popular in this sample relative to other gambling methods; the types queried included Sports Select (14 %), sports pools (13 %), sports betting with a bookie (12 %), informal sports betting (8 %), and horse/dog racing (7 %). Nearly all participants (92 %) reported gambling at least once per week, exceeding the Canadian Low-Risk Gambling Guidelines (Young et al., 2021). About one third (38 %) reported gambling four or more times per week. About half (51 %) indicated abstinence rather than moderation as their treatment goal.
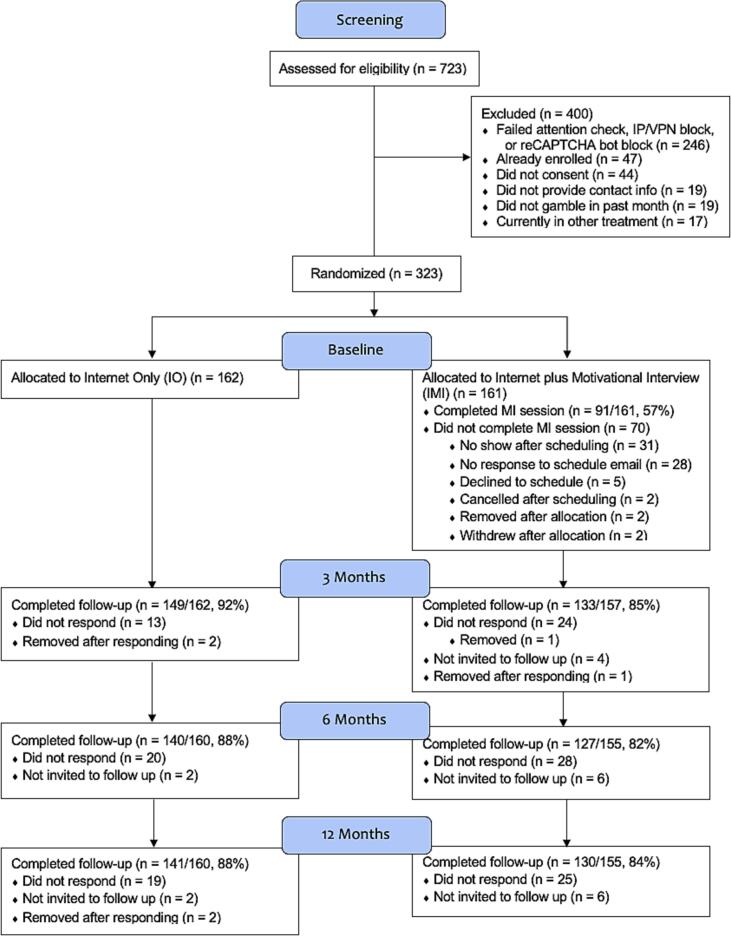
The overall follow-up rates are presented below (Fig. 1). Loss to follow-up (i.e., non-response to invitation) was significantly greater for the IMI group at 3 months, (1) = 4.10, p = .043, but no group differences were observed at 6 months, (1) = 1.89, p = .169, or 12 months, (1) = 1.19, p = .276. Completers and non-completers of the 3-month follow-up did not demonstrate significant differences in any baseline characteristics. Results did not differ when analyses were conducted per protocol or with logarithmically transformed data. Thus, we report results of the intent-to-treat analyses with untransformed data.
Fig. 1.
CONSORT chart.
3.2. Gambling problems
Fig. 2, Fig. 3, Fig. 4 illustrate the primary continuous gambling outcomes by group and time. Significant time effects were observed at all follow-ups for gambling severity and expenditures, with the greatest improvements observed at 3 months. Time effects for duration were significant at 6 and 12 but not 3 months. No group differences or interactions were significant at any time point in the full GEE models. However, because the trajectory of change visually appeared greater for the IMI group versus the IO group from baseline to 3 months for all variables (see Fig. 2, Fig. 3, Fig. 4), an exploratory piecewise analysis was conducted. This analysis showed that gamblers in the IMI group achieved greater reductions in expenditures per session compared to those in the IO group by 3 months, Estimate = −141.53, SE = 67.47, Wald(1) = 4.40, p = .036. Results for the other outcome variables were non-significant. The GEE model summaries and estimated marginal means for primary continuous gambling outcomes are presented in Table 2, Table 3, respectively. Dichotomous gambling outcomes by group and time are presented in Table 4.
Fig. 2.
Gambling severity.
Fig. 3.
Gambling expenditures per month.
Fig. 4.
Gambling expenditures per session.
Table 2.
GEE for continuous gambling outcomes.
| Effect | Estimate | SE | Wald | p | 95 % CI |
|
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Severity (NODS-GD) | ||||||
| Intercept | 7.29 | 0.14 | 2769.26 | <.001 | 7.01 | 7.56 |
| Group: IMI | −0.24 | 0.21 | 1.28 | .260 | −0.66 | 0.18 |
| Time: 3 months | −2.25 | 0.26 | 73.95 | <.001 | −2.76 | −1.73 |
| Time: 6 months | −2.94 | 0.29 | 106.74 | <.001 | −3.50 | −2.38 |
| Time: 12 months | −3.40 | 0.28 | 153.11 | <.001 | −3.94 | −2.86 |
| Group × Time: 3 months | −0.12 | 0.39 | 0.10 | .760 | −0.88 | 0.64 |
| Group × Time: 6 months | 0.18 | 0.40 | 0.21 | .650 | −0.61 | 0.98 |
| Group × Time: 12 months | 0.05 | 0.40 | 0.02 | .900 | −0.74 | 0.85 |
| Expenditures (dollars per month) | ||||||
| Intercept | 1755 | 219 | 64.20 | <.001 | 1325 | 2185 |
| Group: IMI | −267 | 286 | 0.87 | .350 | −828 | 294 |
| Time: 3 months | −747 | 280 | 7.14 | .008 | −1296 | −198 |
| Time: 6 months | −848 | 258 | 10.83 | .001 | −1353 | −342 |
| Time: 12 months | −993 | 248 | 16.00 | <.001 | −1480 | −506 |
| Group × Time: 3 months | −133 | 373 | 0.13 | .722 | −864 | 599 |
| Group × Time: 6 months | −49 | 329 | 0.02 | .882 | −695 | 597 |
| Group × Time: 12 months | 235 | 331 | 0.50 | .478 | −414 | 883 |
| Duration (hours per month) | ||||||
| Intercept | 45.40 | 3.67 | 153.08 | <.001 | 38.2 | 52.60 |
| Group: IMI | −4.12 | 5.48 | 0.56 | .452 | −14.9 | 6.64 |
| Time: 3 months | −9.56 | 5.50 | 3.02 | .082 | −20.4 | 1.24 |
| Time: 6 months | −19.15 | 4.97 | 14.84 | <.001 | −28.9 | −9.39 |
| Time: 12 months | −19.03 | 5.19 | 13.41 | <.001 | −29.2 | −8.83 |
| Group × Time: 3 months | −2.81 | 7.99 | 0.12 | .726 | −18.5 | 12.88 |
| Group × Time: 6 months | 3.70 | 7.97 | 0.22 | .642 | −11.9 | 19.35 |
| Group × Time: 12 months | −0.31 | 7.54 | 0.00 | .968 | −15.1 | 14.49 |
Table 3.
Estimated marginal means of primary gambling outcomes by group and time.
| Outcome | IO group |
IMI group |
Total |
|||
|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | |
| Severity (NODS-GD) | ||||||
| Baseline | 7.29 | 0.14 | 7.04 | 0.16 | 7.16 | 0.11 |
| 3 months | 5.04 | 0.22 | 4.68 | 0.23 | 4.86 | 0.16 |
| 6 months | 4.34 | 0.25 | 4.29 | 0.24 | 4.31 | 0.17 |
| 12 months | 3.89 | 0.24 | 3.70 | 0.25 | 3.79 | 0.17 |
| Expenditures (dollars per month) | ||||||
| Baseline | 1755 | 219 | 1488 | 183 | 1621 | 143 |
| 3 months | 1008 | 174 | 608 | 165 | 808 | 120 |
| 6 months | 907 | 135 | 591 | 92 | 749 | 82 |
| 12 months | 762 | 117 | 730 | 118 | 746 | 83 |
| Duration (hours per month) | ||||||
| Baseline | 45.4 | 3.7 | 41.3 | 4.1 | 43.3 | 2.7 |
| 3 months | 35.8 | 4.1 | 28.9 | 4.1 | 32.4 | 2.9 |
| 6 months | 26.3 | 3.4 | 25.8 | 4.7 | 26.0 | 2.9 |
| 12 months | 26.4 | 3.7 | 22.0 | 3.6 | 24.2 | 2.6 |
Table 4.
Dichotomous gambling outcomes by group and time.
| Outcome | IO group |
IMI group |
Total |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Diagnosis: Met criteria | ||||||
| Baseline | 144/158 | 91.1 | 128/155 | 82.3 | 272/313 | 86.9 |
| 3 months | 86/146 | 58.9 | 68/132 | 51.5 | 154/278 | 55.4 |
| 6 months | 62/138 | 44.9 | 60/127 | 47.2 | 122/265 | 46.0 |
| 12 months | 53/139 | 38.1 | 42/130 | 32.3 | 95/269 | 35.3 |
| Goal: Attained | ||||||
| 3 months | 38/146 | 26.0 | 35/132 | 26.5 | 73/278 | 26.3 |
| 6 months | 38/138 | 27.5 | 40/127 | 31.5 | 78/265 | 29.4 |
| 12 months | 42/139 | 30.2 | 41/130 | 31.5 | 83/269 | 30.9 |
| Frequency: Weekly or more | ||||||
| Baseline | 145/158 | 91.8 | 143/155 | 92.2 | 288/313 | 92.0 |
| 3 months | 114/146 | 78.1 | 89/132 | 67.4 | 203/278 | 73.0 |
| 6 months | 99/138 | 71.2 | 81/127 | 63.8 | 180/265 | 67.9 |
| 12 months | 85/139 | 61.2 | 75/130 | 57.7 | 160/269 | 59.5 |
3.3. Concurrent mental health problems
Similar to the primary outcomes in most regards, participants regardless of group experienced reductions in mental health outcomes over time. The time effects were significant at all follow-ups for depression, anxiety, and general distress. However, when analyzed in an exploratory piecewise manner, gamblers in the IMI group achieved greater reductions in nonspecific distress compared to those in the IO group by 3 months, Estimate = −2.52, SE = 1.27, Wald(1) = 3.95, p = .047. These differences were no longer apparent at 6 and 12 months. No meaningful differences in alcohol consumption were observed for either group at any time point. The GEE estimated marginal means for secondary outcomes are presented in Table 5.
Table 5.
Estimated marginal means for secondary outcomes by group and time.
| Outcome | IO group |
IMI group |
Total |
|||
|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | |
| Depression (PHQ-9) | ||||||
| Baseline | 12.20 | 0.46 | 12.61 | 0.45 | 12.40 | 0.32 |
| 3 months | 10.14 | 0.49 | 9.47 | 0.50 | 9.81 | 0.35 |
| 6 months | 10.22 | 0.57 | 9.83 | 0.51 | 10.03 | 0.38 |
| 12 months | 9.56 | 0.55 | 9.59 | 0.55 | 9.58 | 0.39 |
| Anxiety (GAD-7) | ||||||
| Baseline | 9.71 | 0.37 | 10.47 | 0.38 | 10.09 | 0.27 |
| 3 months | 8.27 | 0.43 | 8.25 | 0.42 | 8.26 | 0.30 |
| 6 months | 8.24 | 0.47 | 8.31 | 0.47 | 8.28 | 0.33 |
| 12 months | 7.71 | 0.44 | 8.06 | 0.50 | 7.89 | 0.33 |
| Psychological distress (K-10) | ||||||
| Baseline | 19.6 | 0.60 | 20.8 | 0.59 | 20.2 | 0.42 |
| 3 months | 17.0 | 0.64 | 15.8 | 0.68 | 16.4 | 0.47 |
| 6 months | 16.1 | 0.76 | 16.4 | 0.71 | 16.3 | 0.52 |
| 12 months | 14.7 | 0.66 | 15.9 | 0.77 | 15.3 | 0.51 |
| Alcohol use (AUDIT-C) | ||||||
| Baseline | 3.67 | 0.22 | 3.63 | 0.23 | 3.65 | 0.16 |
| 3 months | 3.45 | 0.23 | 2.90 | 0.23 | 3.18 | 0.16 |
| 6 months | 3.35 | 0.24 | 3.06 | 0.24 | 3.20 | 0.17 |
| 12 months | 3.37 | 0.24 | 2.95 | 0.25 | 3.16 | 0.17 |
3.4. Motivational interviews
In total, 91 participants in the IMI group (57 %) completed their MI session. Sessions averaged 46.3 min (Mdn = 43, SD = 18.8, range = 15.7–130.0). Most of those who attended the MI session (90 %, N = 82) completed the subsequent 3-month follow-up assessment, while only 70 % (N = 49) of those that did not attend the MI session completed it, (1) = 10.55, p = .001. At baseline, MI completers reported gambling fewer hours per episode (M = 2.8, Mdn = 2, SD = 1.9) compared to MI non-completers (M = 3.8, Mdn = 3, SD = 2.8), t(159) = −2.53, p = .013, d = 0.43. Otherwise, no baseline differences between MI completers and non-completers within the IMI group were observed.
Thirty percent of the MI sessions (N = 27) were randomly selected, assessed, and rated for treatment fidelity by two independent raters using a treatment adherence checklist adapted the Motivational Interviewing Treatment Integrity Code (Moyers et al., 2016). Our checklist covered MI and study protocol elements that were essential to include (e.g., offer PGSI feedback) and not include (e.g., provide unsolicited advice). Overall, interrater percent agreement was 80 %. Facilitators' mean adherence score was 30.6 out of 34 (SD = 1.8). Scores did not significantly differ between IMI participants who did versus did not complete the 3-month follow-up assessment, p > .05.
3.5. Program engagement
Program data was unavailable for 16 participants (5 %) because they registered for the program without inputting their assigned token. The remaining 95 % created an account with their token and were thus included in the following analyses. Participants completed a mean of 1.2 out of 4 modules (Mdn = 1, SD = 1.5). About 11 % of participants completed all four modules and 41 % did not complete any. About 73 % accessed at least one module (i.e., at least one but not all activities in a module) and 48 % completed at least one module in its entirety. Gamblers spent a mean of 27.2 min (Mdn = 14, SD = 35.8, range = 0–248.8) with the program and logged in approximately 2.0 times (Mdn = 1, SD = 1.9, range = 1–14), inclusive of the initial login to create an account. >90 % of logins, module completions, and minutes spent online occurred prior to the 3-month follow-up regardless of treatment group. Contrary to expectations, there were no significant group differences in any user data variables, all p > .05. Within the IMI group, however, those who completed their MI session spent nearly twice as many minutes with the online program (M = 28.9, Mdn = 16, SD = 38.0) compared to those who did not complete their MI session (M = 15.1, Mdn = 7, SD = 25.3), t(131) = 2.06, p = .042, d = 0.44. MI completers in the IMI group also completed more program modules (M = 1.3, Mdn = 1, SD = 1.6) compared to MI non-completers (M = 0.7, Mdn = 0, SD = 1.2), t(131) = 2.44, p = .017, d = 0.43. There was no significant difference in the number of logins for MI completers versus non-completers, p > .05.
In terms of program engagement and gambling outcomes, we found that the number of completed modules was positively associated with reductions in gambling expenditures, r = 0.14, t(251) = −2.0, p = .030, as well as reductions in NODS-GD scores by 3 months, r = 0.18, t(252) = −3.0, p = .004. Number of logins and minutes on the program were not significantly correlated with reductions in any primary gambling outcomes.
Overall, participants rated the online program favourably on the IEUQ (M = 34.2, Mdn = 37, SD = 13.1). No differences in mean ratings were observed between treatment groups, p > .05. The proportion of users that rated IEUQ items as “mostly true” or “very true” ranged from 44 % (“the program kept my interest and attention”) to 75 % (“the information in the program was easy to understand”).
4. Discussion
4.1. Principal results
All outcomes except alcohol use meaningfully improved over time, particularly within the first 3 months. About 27 % reported achievement of their gambling treatment goal by 3 months, but no significant changes in perceived goal attainment occurred thereafter. This estimate is somewhat lower than in other trials but may be a result of providing a binary rather than graded response option. Gambling outcomes continued to improve in the subsequent months, albeit at a reduced pace. The same pattern was observed regarding anxiety, depression, and nonspecific distress, although improvements were less extreme relative to gambling. In contrast to our hypotheses, most primary and secondary outcomes did not demonstrate a differential change by group over time. Two minor exceptions to this finding were observed when data were analyzed in an exploratory piecewise manner. First, the IMI group reduced their mean expenditures per gambling episode much quicker than the IO group, which experienced a more linear and gradual reduction before achieving the same outcome as the IMI group by 12 months. Second, that same pattern was observed regarding nonspecific distress, albeit to a lesser degree. Given that few participants received the full dose of the online program, it is unlikely that our study was sufficiently powered to detect differential improvements. While it is possible that improvements could be attributed to natural recovery or regression to the mean, past research suggests that similar gambling self-help interventions yield greater improvements relative to waitlist controls when unguided (Hodgins et al., 2001) or guided (Carlbring and Smit, 2008).
Regarding the online program, nearly half of users did not return after the initial login, and only one in ten received the full treatment dose (i.e., completed all four modules). Still, nearly three quarters of participants demonstrated some level of engagement with the program. This partial implementation, which is reflective of real-world uptake, is important given that we observed a positive dose-response relationship between module completion and reductions in gambling severity and expenditures. Notably, IMI participants did not demonstrate greater engagement on any metric. However, within the IMI group, those who attended their MI session completed twice as many modules and spent twice as many minutes with the program as those who did not. Taken together, these results suggest that engagement is important for recovery, but MI may not be an optimal adjunct to facilitate engagement. Alternatively, given the differences within the IMI group, MI may improve program engagement and outcomes yet be subject to the engagement problem itself. Indeed, face-to-face gambling treatment is not immune to this dilemma (Pfund et al., 2021). It is also possible that the benefits of MI are subject to sleeper effects (Hodgins et al., 2004), unrelated to program engagement, or concealed due to the low rate of MI session completion. To add a caveat, more engagement may not be a universal positive, as research on smoking cessation and alcohol treatment has indicated that users experience varying engagement trajectories and benefits, such as productive disengagement (e.g., disengaging from the intervention following perceived benefits) (Chung et al., 2023; Smith et al., 2017). Given the pandemic context, it is also possible that participants or therapists had experienced “Zoom fatigue” and were thus less effectively engaged during the virtual MI sessions (Barker and Barker, 2022). While our sample was based on recruitment of passive rather than active treatment seekers, it is possible that participants were nonetheless already motivated to engage in treatment and thus MI offered no incremental increase in motivation. A different explanation might be that the baseline assessments served as an intervention in and of themselves by encouraging the self-reflection that MI is purported to encourage; for instance, one study found no differences in alcohol outcomes for groups that received complete MI, spirit-only MI, or assessment feedback (Morgenstern et al., 2017).
Other technology-related barriers may also be the culprit. For instance, emerging evidence suggests that empathy and presence are significantly decreased in virtual compared to face-to-face psychotherapy (Grondin et al., 2023). Moreover, while fidelity ratings for our MI facilitators were high, they are independent of participant reactions or perceptions. Given that genuinely expressed empathy is a core principle of MI and one that distinguishes it from motivational strategies per se (e.g., self-guided decisional balance exercises in our online program), it is possible that our virtual MI delivery obscured participants' experience of facilitator empathy. One potential solution to the engagement problem is to focus on making programs more engaging rather than making users more engaged (e.g., via MI). Indeed, fewer than half of users found the program subjectively engaging. In accordance with their suggestions, similar programs would likely benefit from the addition of reminders or prompts to engage, greater interactivity and personalization of activities (e.g., personalized graphs plotting user gambling over time, vignettes to describe strategy implementation), and enhanced aesthetic appeal (e.g., greater use of audiovisual rather than written content) (Brazeau, 2021). Many users, however, rated the information and activities per se as very useful and trustworthy.
4.2. Comparison with prior work
The sample recruited for this trial was comparable in most regards to that of similar trials and the general population of Canadian treatment-seeking adult gamblers. However, our sample was particularly treatment naïve in that only 4 % had received prior gambling treatment (cf. Hodgins et al., 2019, which reported a 37 % rate of prior treatment). Thus, meaningful behavioral changes may have occurred at a different rate relative to previous trials, although the effect of treatment naivete on outcomes in this context is inconclusive (Haller et al., 2023). Moreover, much of our recruitment and intervention occurred in the context of the pandemic, which may explain the higher rates of unemployment than would otherwise be expected. Finally, participants were recruited solely from internet media sites, which yielded an appropriate sample for the intervention (i.e., those with internet access) but may have introduced a sampling bias. Specifically, passive social recruitment has been shown to engage more females than males and participants with less severe problems relative to more active online recruitment methods, such as Google searches (Lindner et al., 2015).
It is atypical that our sample was composed of more females than males. Males tend to have higher rates of gambling problems and tend to engage in different forms of gambling, so it is possible that our results were colored by the gender composition of our sample. It is likely that we recruited more females because our recruitment occurred almost exclusively on social media, with which females tend to engage more frequently and actively than males (Krasnova et al., 2017). However, gambling severity of our sample was comparable to prior trials, and differences in gambling types are at least partly attributable to the pandemic (e.g., reduced access to brick-and-mortar casinos). It is unlikely that the gender composition of our sample ultimately impacted results; no prior comparable studies have found gender differences in treatment outcomes to our knowledge.
While our attrition rates were much lower than many related trials, we were still met with challenges engaging participants. Only 57 % of IMI participants completed their MI session, which may be due to our not requiring it as a condition of enrollment as has been done in the past (cf., Hodgins et al., 2001). Alternatively, the reduced privacy afforded to the IMI group may have deterred some from engaging, which could explain the differences in program engagement for MI completers and non-completers within the IMI group. It may also explain the higher attrition rates for the IMI group initially observed, given that the IO group was not subject to any verbal contact with the research team, whether related to assessment or treatment, which is typically not the case. In other words, our results may be confounded given that one group was necessarily subjected to a prominent treatment barrier (i.e., reduced privacy) and the other was not.
Our results are unique in that MI did not differentially improve gambling outcomes. In a comparable trial, Jonsson and colleagues found that a very brief motivational contact (i.e., approximately six minutes), including personal risk feedback, was more effective than similar information delivered in written format (Jonsson et al., 2020). However, their sample differed from ours in that it had a greater proportion of males, higher mean age, and much higher engagement with riskier forms of gambling such as VLTs. Participants were also selected based on their high gambling expenditures rather than general social media advertisements. Moreover, they did not have access to a self-help program, so the only intervention was the brief contact in verbal or written form.
4.3. Strengths and limitations
This trial has several strengths, including the upcoming two-year follow-up, remarkably low attrition rate, collection of quantitative and qualitative user feedback, comparison group unconfounded by general therapist contact (e.g., guidance or support (Carlbring and Smit, 2008)), and use of cost-effective and high-demand technology to deliver the intervention. In terms of limitations, one is the use of a simplified MI adherence checklist. While best practices recommend more thorough evaluations of treatment integrity, the briefer checklist permitted for efficient coding of whole sessions. Since the more comprehensive protocols are designed to code partial interviews, and therapist adherence can fluctuate throughout a single MI session (Jelsma et al., 2015; Kramer Schmidt et al., 2019), our checklist also permitted more representative coding than extensive protocols might feasibly allow. Another limitation is that we did not include a true control group, although this is a relatively lesser concern given that our primary question was whether MI could enhance the benefit of a workbook for which the standalone efficacy has already been demonstrated (Abbott et al., 2012; Hodgins et al., 2001; Hodgins et al., 2004; Hodgins et al., 2009; Cunningham et al., 2019a; Hodgins et al., 2019; Cunningham et al., 2019b). However, the efficacy has not been established with a true control group for the internet program specifically, so there is still a possibility that improvements were due to natural recovery or regression to the mean. Finally, future gambling intervention trials would benefit from the inclusion of questions that directly correspond to the Canadian Low-Risk Gambling Guidelines (Young et al., 2021) or their equivalent in other jurisdictions.
A final consideration relates to the analytic method we employed, GEE, which is a common and useful method for modelling nonparametric longitudinal data. However, its basis in generalized linear models renders it less than ideal for identifying nonlinear, emergent, complex patterns on smaller time scales. This limitation is important given that much of the behavioral changes in the current study, like in many others, occurred prior to the first follow-up. Nearly all participants had terminated program use by that time as well, whether by completing all modules, deciding not to return, or forgetting to log in. Similar findings have been observed with other mental health and addiction interventions (Bricker et al., 2023), whereby differential trajectories of treatment engagement and behavioral change are most prominent in the early days and weeks of treatment. New technologies that permit much higher sampling frequencies with convenience and ease (e.g., smartphone apps with daily diaries) will be extremely useful to zoom in on recovery dynamics at previously inaccessible time scales. Complexity science can inform the field in terms of more sophisticated theories and analytic methods to discover how people change and how that can be facilitated (Hayes and Andrews, 2020; Hayes et al., 2022; Heino et al., 2022; Hofmann et al., 2020; Olthof et al., 2020).
5. Conclusions
The addition of a motivational interview to an online self-help program for gambling problems was generally unsuccessful in improving program engagement or treatment outcomes. It is possible that group differences were obscured by the low rate of MI session completion or IMI group exposure to a common treatment barrier (i.e., lack of privacy). Future work should aim to make self-guided programs more engaging rather than solely making users more engaged. Analytic methods that measure change at smaller time scales may shed light on dynamics that traditional randomised controlled trials are unable to capture.
Abbreviations
- AUDIT-C
Alcohol Use Disorder Identification Test-Consumption
- CONSORT
Consolidated Standards of Reporting Trials
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- CAD
Canadian dollars
- GAD-7
Generalized Anxiety Disorder Scale-7
- GD
gambling disorder
- GEE
generalized estimating equations
- GPI
Gambling Participation Instrument
- IEUQ
Internet Evaluation and Utility Questionnaire
- IMI
internet plus motivational interview
- IO
internet only
- K-10
Kessler Psychological Distress Scale-10
- MI
motivational interviewing
- NODS-GD
National Opinion Research Center Diagnostic Screen for Gambling Disorder
- PGSI
Problem Gambling Severity Index
- PHQ-9
Patient Health Questionnaire-9
Funding
This work was supported by Alberta Gambling Research Institute (grant #95).
CRediT authorship contribution statement
All authors intellectually contributed to this study. BWB: Conceptualization, methodology, software, validation, formal analysis, investigation, data curation, writing – original draft, writing – review and editing, visualization, funding acquisition. JAC: Methodology, writing – review and editing, funding acquisition. DCH: Conceptualization, methodology, validation, investigation, resources, writing – review and editing, supervision, project administration, funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2023.100707.
Appendix A. Supplementary data
The following are the supplementary data related to this article.
CONSORT-EHEALTH checklist (Eysenbach and CONSORT-EHEALTH Group, 2011) for the current trial.
Additional methods.
Data availability
Cleaned anonymized data will be made available to others by the authors upon request via email. R code for statistical analyses will similarly be made available upon request. Data and code can be requested from the corresponding author (brad.brazeau@ucalgary.ca) beginning 3 months after publication. Data and/or code will be supplied to anyone who provides a sound proposal and specific purpose.
References
- Abbott M.W., Bellringer M., Vandal A., Hodgins D.C., Du Preez Palmer, K, Landon J, Sullivan S, Feigin V. Gambling & Addictions Research Centre; Wellington, NZ: 2012. Effectiveness of Problem Gambling Brief Telephone Interventions: A Randomised Controlled Trial. [DOI] [PubMed] [Google Scholar]
- Afshin A., Babalola D., Mclean M., Yu Z., Ma W., Chen C.Y., Arabi M., Mozaffarian D. Information technology and lifestyle: a systematic evaluation of internet and mobile interventions for improving diet, physical activity, obesity, tobacco, and alcohol use. J. Am. Heart Assoc. 2016;5(9) doi: 10.1161/JAHA.115.003058. (PMID:27581172) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G. Internet-delivered psychological treatments. Annu. Rev. Clin. Psychol. 2016;12:157–179. doi: 10.1146/annurev-clinpsy-021815-093006. (PMID:26652054) [DOI] [PubMed] [Google Scholar]
- Andersson G., Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatry. 2014;13(1):4–11. doi: 10.1002/wps.20083. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker G.G., Barker E.E. Online therapy: lessons learned from the COVID-19 health crisis. Br. J. Guid. Couns. 2022;50(1):66–81. doi: 10.1080/03069885.2021.1889462. Jan 2. [DOI] [Google Scholar]
- Bijker R., Booth N., Merkouris S.S., Dowling N.A., Rodda S.N. Global prevalence of help-seeking for problem gambling: a systematic review and meta-analysis. Addiction. 2022;117(12):2972–2985. doi: 10.1111/add.15952. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borghouts J., Eikey E., Mark G., De Leon C., Schueller S.M., Schneider M., Stadnick N., Zheng K., Mukamel D., Sorkin D.H. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J. Med. Internet Res. 2021;23(3) doi: 10.2196/24387. e24387. Mar 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boumparis N., Schaub M.P. Recent advances in digital health interventions for substance use disorders. Curr. Opin. Psychiatry. 2022;35(4):246–251. doi: 10.1097/YCO.0000000000000798. Jul. [DOI] [PubMed] [Google Scholar]
- Boumparis N., Haug S., Abend S., Billieux J., Riper H., Schaub M.P. Internet-based interventions for behavioral addictions: a systematic review. J. Behav. Addict. 2022;11(3):620–642. doi: 10.1556/2006.2022.00054. Sep 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley K.A., McDonell M.B., Bush K., Kivlahan D.R., Diehr P., Fihn S.D. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Alcohol. Clin. Exp. Res. 1998;22(8):1842. doi: 10.1097/00000374-199811000-00034. [DOI] [PubMed] [Google Scholar]
- Brazeau B.W. University of Calgary; Calgary, AB: 2021. Augmenting an Online Self-directed Intervention for Gambling Disorder with a Single Motivational Interview: A Randomized Controlled Trial 3-Month Follow-Up. [Master’s thesis]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazeau B.W., Hodgins D.C. In: Gambl Disord Clin Guide Treat. 2nd ed. Grant J.E., Potenza M.N., editors. American Psychiatric Publishing, Inc.; New York, NY: 2021. Psychosocial treatments; pp. 233–255. [Google Scholar]
- Brazeau B.W., Hodgins D.C. Psychometric evaluation of the NORC diagnostic screen for gambling problems (NODS) for the assessment of DSM-5 gambling disorder. Addict. Behav. 2022;130 doi: 10.1016/j.addbeh.2022.107310. 107310. Jul. [DOI] [PubMed] [Google Scholar]
- Brazeau B.W., Hodgins D.C., Cunningham J.A., Bennett K., Bennett A. Augmenting an online self-directed intervention for gambling disorder with a single motivational interview: study protocol for a randomized controlled trial. Trials. 2021;22(1):947. doi: 10.1186/s13063-021-05912-3. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricker J., Miao Z., Mull K., Santiago-Torres M., Vock D.M. Can a single variable predict early dropout from digital health interventions? Comparison of predictive models from two large randomized trials. J. Med. Internet Res. 2023;20(25) doi: 10.2196/43629. e43629. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buuren S.V., Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011;45(3) doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Carey V.J., Ripley B. gee: Generalized Estimation Equation Solver. 2022. https://cran.r-project.org/web/packages/gee/index.html Available from:
- Carlbring P., Smit F. Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. J. Consult. Clin. Psychol. 2008;76(6):1090–1094. doi: 10.1037/a0013603. [DOI] [PubMed] [Google Scholar]
- Chung T., Ahn C., Suffoletto B.P. Trajectory classes of engagement with an alcohol text message intervention and predictors of intervention engagement. Addict. Behav. 2023;144 doi: 10.1016/j.addbeh.2023.107729. 107729. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham J.A., Hodgins D.C., Mackenzie C.S., Godinho A., Schell C., Kushnir V., Hendershot C.S. Randomized controlled trial of an internet intervention for problem gambling provided with or without access to an internet intervention for co-occurring mental health distress. Internet Interv Elsevier. 2019;17(March) doi: 10.1016/j.invent.2019.100239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Godinho A, Hodgins DC. Pilot randomized controlled trial of an online intervention for problem gamblers. Addict Behav Rep Elsevier; 2019b;9(March):100175. doi: 10.1016/j.abrep.2019.100175. [DOI] [PMC free article] [PubMed]
- Currie S.R., Hodgins D.C., Casey D.M. Validity of the problem gambling severity index interpretive categories. J. Gambl. Stud. 2013;29(2):311–327. doi: 10.1007/s10899-012-9300-6. [DOI] [PubMed] [Google Scholar]
- eHub Health Pty Ltd Gambling Self-help. 2023. www.gamblingselfhelp.com Available from:
- Erdfelder E., Faul F., Buchner A. GPOWER: a general power analysis program. Behav. Res. Methods Instrum. Comput. 1996;28(1):1–11. doi: 10.3758/BF03203630. [DOI] [Google Scholar]
- Evans S., Royston P., Day S. University of York; 2017. MINIM: Allocation by Minimisation in Clinical Trials.https://www-users.york.ac.uk/~mb55/guide/minim.htm Available from: [accessed May 7, 2020] [Google Scholar]
- Eysenbach G., CONSORT-EHEALTH Group CONSORT-EHEALTH: improving and standardizing evaluation reports of web-based and mobile health interventions. J. Med. Internet Res. 2011;13(4):e126. doi: 10.2196/jmir.1923. Dec 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris J., Wynne H. 2001. The Canadian Problem Gambling Index: Final Report. Ottawa Canadian Centre on Substance Abuse. Available from: http://www.cclat.ca/2003 and earlier CCSA Documents/ccsa-008805-2001.pdf{%}5Cnpapers3://publication/uuid/C97148A6-7463-49C3-A03B-509DF4119119. [Google Scholar]
- Gerstein D., Hoffmann J., Larison C., Engelman L., Murphy S., Palmer A. National Opinion Research Center; Chicago: 1999. Gambling impact and behavior study: Report of thenational gambling impact study commission. [Google Scholar]
- Grondin F., Lomanowska A.M., Belleville G., Yampolsky M.A., Tremblay M.-P.B., Jackson P.L. Therapist and client perceptions of empathy in simulated teletherapy sessions. Behav. Inform. Technol. 2023:1–16. doi: 10.1080/0144929X.2023.2214636. May 26. [DOI] [Google Scholar]
- Haller K., Becker P., Niemeyer H., Boettcher J. Who benefits from guided internet-based interventions? A systematic review of predictors and moderators of treatment outcome. Internet Interv. 2023;33 doi: 10.1016/j.invent.2023.100635. 100635. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.M., Andrews L.A. A complex systems approach to the study of change in psychotherapy. BMC Med. 2020;18(1):197. doi: 10.1186/s12916-020-01662-2. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S.C., Ciarrochi J., Hofmann S.G., Chin F., Sahdra B. Evolving an idionomic approach to processes of change: towards a unified personalized science of human improvement. Behav. Res. Ther. 2022;156 doi: 10.1016/j.brat.2022.104155. 104155. Sep. [DOI] [PubMed] [Google Scholar]
- Heino M.T.J., Proverbio D., Marchand G., Resnicow K., Hankonen N. Attractor landscapes: a unifying conceptual model for understanding behaviour change across scales of observation. Health Psychol. Rev. 2022;13:1–18. doi: 10.1080/17437199.2022.2146598. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgins D.C., Makarchuk K. Addictive Behaviours Laboratory, University of Calgary; Calgary, AB: 2002. Becoming a Winner: Defeating Problem Gambling: A Self-help Manual for Problem Gamblers. [Google Scholar]
- Hodgins D.C., Currie S.R., El-Guebaly N. Motivational enhancement and self-help treatments for problem gambling. J. Consult. Clin. Psychol. 2001;69(1):50–57. doi: 10.1037/0022-006X.69.1.50. [DOI] [PubMed] [Google Scholar]
- Hodgins D.C., Currie S., El-Guebaly N., Peden N. Brief motivational treatment for problem gambling: a 24-month follow-up. Psychol. Addict. Behav. 2004;18(3):293–296. doi: 10.1037/0893-164X.18.3.293. [DOI] [PubMed] [Google Scholar]
- Hodgins D.C., Currie S.R., Currie G., Fick G.H. Randomized trial of brief motivational treatments for pathological gamblers: more is not necessarily better. J. Consult. Clin. Psychol. 2009;77(5):950–960. doi: 10.1037/a0016318. [DOI] [PubMed] [Google Scholar]
- Hodgins D.C., Fick G.H., Murray R., Cunningham J.A. Internet-based interventions for disordered gamblers: study protocol for a randomized controlled trial of online self-directed cognitive-behavioural motivational therapy. BMC Public Health. 2013;13(1) doi: 10.1186/1471-2458-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgins D.C., Cunningham J.A., Murray R., Hagopian S. Online self-directed interventions for gambling disorder: randomized controlled trial. J. Gambl. Stud. Springer US. 2019;35(2):635–651. doi: 10.1007/s10899-019-09830-7. [DOI] [PubMed] [Google Scholar]
- Hodgins D.C., Williams R.J., Belanger Y.D., Christensen D.R., El-Guebaly N., McGrath D.S., Nicoll F., Shaw C.A., Stevens R.M.G. Making change: attempts to reduce or stop gambling in a general population sample of people who gamble. Front. Psychol. 2022;17(13) doi: 10.3389/fpsyt.2022.892238. 892238. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann S.G., Curtiss J.E., Hayes S.C. Beyond linear mediation: toward a dynamic network approach to study treatment processes. Clin. Psychol. Rev. 2020;76 doi: 10.1016/j.cpr.2020.101824. 101824. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakobsen J.C., Gluud C., Wetterslev J., Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Med. Res. Methodol. 2017;17(1):162. doi: 10.1186/s12874-017-0442-1. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelsma J.G.M., Mertens V.-C., Forsberg L., Forsberg L. How to measure motivational interviewing fidelity in randomized controlled trials: practical recommendations. Contemp. Clin. Trials. 2015;7 doi: 10.1016/j.cct.2015.05.001. [DOI] [PubMed] [Google Scholar]
- Jonsson J., Hodgins D.C., Munck I., Carlbring P. Reaching out to big losers leads to sustained reductions in gambling over 1 year: a randomized controlled trial of brief motivational contact. Addiction. 2020 doi: 10.1111/add.14982. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L., Walters E.E., Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. (PMID:12214795) [DOI] [PubMed] [Google Scholar]
- Kramer Schmidt L., Andersen K., Nielsen A.S., Moyers T.B. Lessons learned from measuring fidelity with the motivational interviewing treatment integrity code (MITI 4) J. Subst. Abus. Treat. 2019;97:59–67. doi: 10.1016/j.jsat.2018.11.004. Feb. [DOI] [PubMed] [Google Scholar]
- Krasnova H., Veltri N.F., Eling N., Buxmann P. Why men and women continue to use social networking sites: the role of gender differences. J. Strateg. Inf. Syst. 2017;26(4):261–284. doi: 10.1016/j.jsis.2017.01.004. Dec. [DOI] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(02):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie R.A., Peller A.J., LaPlante D.A., Bernhard B., Harper A., Schrier T., Shaffer H.J. A brief self-help toolkit intervention for gambling problems: a randomized multisite trial. Am. J. Orthop. 2012;82(2):278–289. doi: 10.1111/j.1939-0025.2012.01157.x. [DOI] [PubMed] [Google Scholar]
- Lenth R.V. emmeans: Estimated Marginal Means, Aka Least-squares Means. 2023. https://cran.r-project.org/web/packages/emmeans/index.html Available from:
- Liang K.Y., Zeger S.L. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- Lindner P., Nyström M.B.T., Hassmén P., Andersson G., Carlbring P. Who seeks ICBT for depression and how do they get there? Effects of recruitment source on patient demographics and clinical characteristics. Internet Interv. 2015;2(2):221–225. doi: 10.1016/j.invent.2015.04.002. May. [DOI] [Google Scholar]
- Luquiens A., Tanguy M.-L., Lagadec M., Benyamina A., Aubin H.-J., Reynaud M. The efficacy of three modalities of internet-based psychotherapy for non–treatment-seeking online problem gamblers: a randomized controlled trial. J. Med. Internet Res. 2016;18(2) doi: 10.2196/jmir.4752. e36. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W., Rollnick S. 4th ed. Guilford Press; New York, NY: 2023. Motivational Interviewing: Helping People Change and Grow. [Google Scholar]
- Morgenstern J., Kuerbis A., Houser J., Levak S., Amrhein P., Shao S., McKay J.R. Dismantling motivational interviewing: effects on initiation of behavior change among problem drinkers seeking treatment. Psychol. Addict. Behav. 2017;31(7):751–762. doi: 10.1037/adb0000317. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers T.B., Rowell L.N., Manuel J.K., Ernst D., Houck J.M. The motivational interviewing treatment integrity code (MITI 4): rationale, preliminary reliability and validity. J. Subst. Abuse Treat. Elsevier Inc. 2016;65:36–42. doi: 10.1016/j.jsat.2016.01.001. 26874558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman M.G., Szkodny L.E., Llera S.J., Przeworski A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: is human contact necessary for therapeutic efficacy? Clin. Psychol. Rev. 2011;31(1):178–186. doi: 10.1016/j.cpr.2010.10.002. Feb. [DOI] [PubMed] [Google Scholar]
- Olthof M., Hasselman F., Lichtwarck-Aschoff A. Complexity in psychological self-ratings: implications for research and practice. BMC Med. 2020;18(1):317. doi: 10.1186/s12916-020-01727-2. Oct 8. (PMID:33028317) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry N.M., Ginley M.K., Rash C.J. A systematic review of treatments for problem gambling. Psychol. Addict. Behav. 2017;31(8):951–961. doi: 10.1037/adb0000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfund R.A., Peter S.C., McAfee N.W., Ginley M.K., Whelan J.P., Meyers A.W. Dropout from face-to-face, multi-session psychological treatments for problem and disordered gambling: a systematic review and meta-analysis. Psychol. Addict. Behav. 2021;35(8):901–913. doi: 10.1037/adb0000710. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Staistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing.http://www.R-project.org Available from: [Google Scholar]
- Ramos L.A., Blankers M., Van Wingen G., De Bruijn T., Pauws S.C., Goudriaan A.E. Predicting success of a digital self-help intervention for alcohol and substance use with machine learning. Front. Psychol. 2021;3(12) doi: 10.3389/fpsyg.2021.734633. 734633. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritterband L.M., Ardalan K., Thorndike F.P., Magee J.C., Saylor D.K., Cox D.J., Sutphen J.L., Borowitz S.M. Real world use of an internet intervention for pediatric encopresis. J. Med. Internet Res. 2008;10(2):1–12. doi: 10.2196/jmir.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith W., Ploderer B., Wadley G., Webber S., Borland R. Proc 2017 CHI Conf Hum Factors Comput Syst. ACM; Denver Colorado USA: 2017. Trajectories of engagement and disengagement with a story-based smoking cessation app; pp. 3045–3056. [DOI] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. (PMID:16717171) [DOI] [PubMed] [Google Scholar]
- Walker M., Toneatto T., Potenza M.N., Petry N., Ladouceur R., Hodgins D.C., el-Guebaly N., Echeburua E., Blaszczynski A. A framework for reporting outcomes in problem gambling treatment research: the banff, Alberta consensus. Addiction. 2006 Apr;101(4):504–511. doi: 10.1111/j.1360-0443.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- Wall H., Magnusson K., Berman A.H., Bewick B.M., Hellner C., Jayaram-Lindström N., Rosendahl I. Evaluation of a brief online self-help program for concerned gamblers. J. Gambl. Stud. 2021;37(4):1277–1290. doi: 10.1007/s10899-021-10005-6. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams R.J., Volberg R.A., Stevens R.M.G., Williams L.A., Arthur J.N. The definition, dimensionalization, and assessment of gambling participation. Rep. Prep. Can. Consort. Gambl. Res. 2017:1–157. [Google Scholar]
- Williams R.J., Leonard C.A., Belanger Y.D., Christensen D.R., el-Guebaly N., Hodgins D.C., DS McGrath, Nicoll F., RMG Stevens. Gambling and problem gambling in canada in 2018: prevalence and changes since 2002: le jeu et le jeu problématique au canada en 2018 : prévalence et changements depuis 2002. Can. J. Psychiatr. 2020 doi: 10.1177/0706743720980080. Dec 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young M., Currie S., Dufour M., Nadeau L., Hodgins D.C., Brunelle N., Flores-Pajot M.-C., Paradis C. Canadian Centre on Substance Use and Addiction; Ottawa, ON: 2021. Developing Lower-risk Gambling Guidelines; p. 32. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT-EHEALTH checklist (Eysenbach and CONSORT-EHEALTH Group, 2011) for the current trial.
Additional methods.
Data Availability Statement
Cleaned anonymized data will be made available to others by the authors upon request via email. R code for statistical analyses will similarly be made available upon request. Data and code can be requested from the corresponding author (brad.brazeau@ucalgary.ca) beginning 3 months after publication. Data and/or code will be supplied to anyone who provides a sound proposal and specific purpose.