Abstract
Transvenous lead extraction has been increasingly recognized as a safe and effective method of lead extraction, but there are only few references for extracting leads migrating outside the heart. We present a successful extraction of a fractured pacemaker lead from the spermatic vein using several approaches and multiple tools.
Key Words: abandoned lead, ablation catheter, device infection, Needle’s Eye Snare, steerable introducer
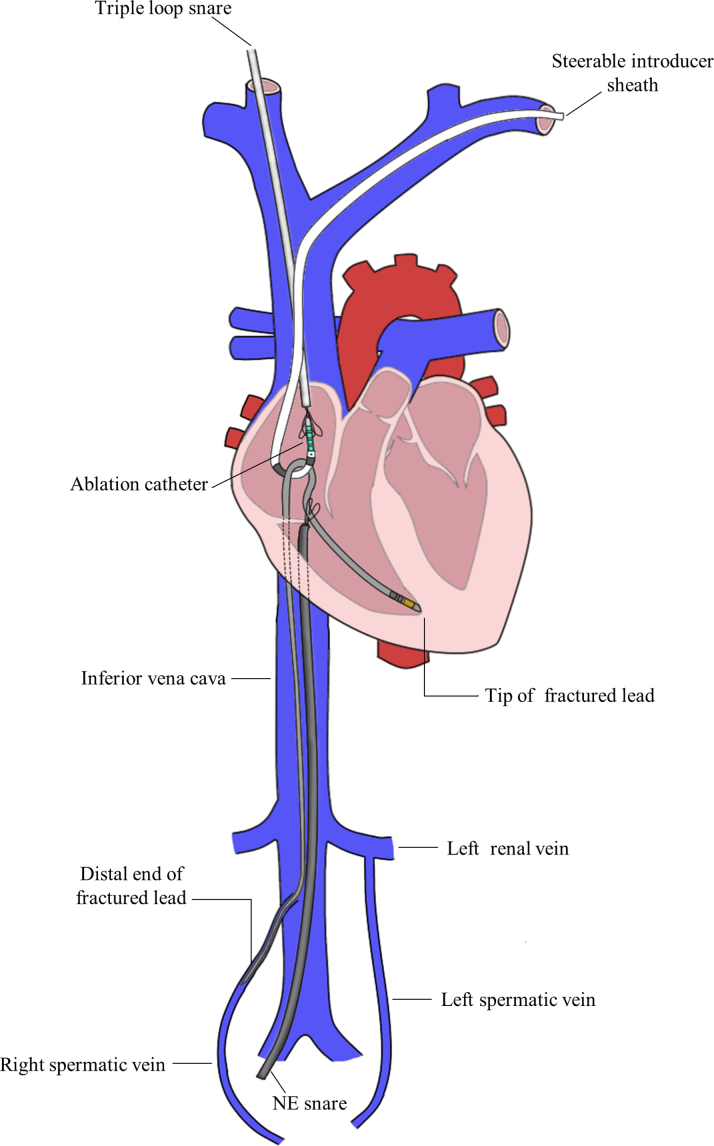
Graphical abstract
History of Presentation
An 80-year-old man with a history of sick sinus syndrome underwent a dual-chamber pacemaker implantation in 1994. A new ventricular lead was inserted because of lead failure in 2013 (Figures 1A and 1B), and in 2020, he was referred to our institution for pocket infection (Figure 2). Blood cultures showed no bacterial growth, and transesophageal echocardiography revealed no vegetations.
Learning Objectives
-
•
Using a CT scan is useful to confirm the location of the fractured lead when migration of a fracture lead is suspected, and early removal is recommended to prevent adhesion of the dislocated lead.
-
•
To combine several approaches and tools, such as ablation catheters and multiple snares for lead extraction, is a novel method of lead extraction when the fractured lead has migrated into the IVC.
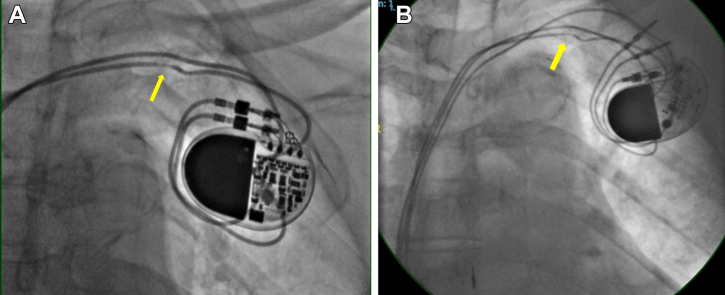
Figure 1.
Lead Fracture
(A) A chest radiograph taken in 2013 showing the ventricular lead fractured by subclavian crush (yellow arrows). (B) A chest radiograph taken after the new ventricular lead insertion.
Figure 2.
The Device Pocket
Redness and swelling observed at the device pocket.
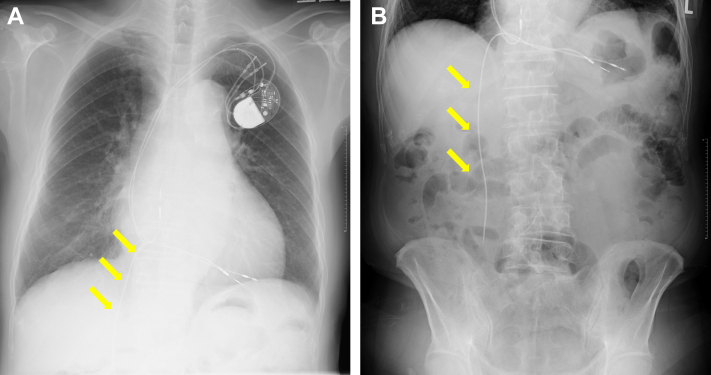
Chest radiography showed the abandoned ventricular lead fractured near the generator pocket and the distal segment of the broken lead migrating past the subclavian vein into the inferior vena cava (IVC) (Figures 3A and 3B). Past chest radiography revealed this dislocation had occurred in 2019; however, he was followed up on an outpatient basis with no signs of infection or abdominal pain. Further investigation using computed tomography (CT) showed that the lead had migrated further down the IVC into the right spermatic vein (Figure 4, Video 1).
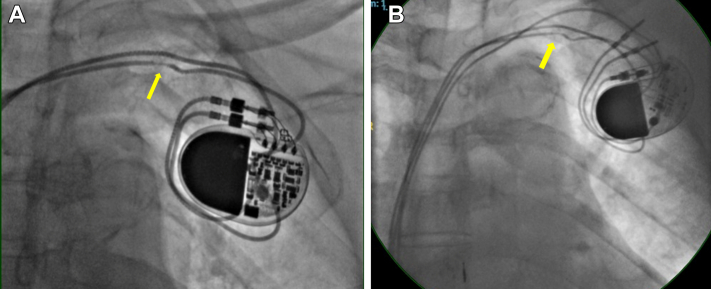
Figure 3.
Fluoroscopy
(A and B) Chest and abdominal fluoroscopy show the distal end of the fractured lead migrating toward the inferior vena cava (yellow arrows).
Figure 4.
Computed Tomography
A volume-rendered computed tomography image shows the distal end of the fractured lead (visualized in green) migrating down the inferior vena cava into the right spermatic vein (visualized in blue).
Past Medical History
The patient was diagnosed with persistent atrial fibrillation in 2010. He was switched from a dual-chamber to a single-chamber pacemaker at the time of the additional ventricular lead insertion in 2013 because of atrial fibrillation.
Differential Diagnosis
The question of whether the fractured abandoned ventricular lead had adhered to the vascular wall of the spermatic vein was raised.
Investigations
We first began by removing the functional ventricular lead and the nonfunctional atrial lead, which were both easily extracted using a laser sheath. Next, we switched the laser sheath to a 9.0-F introducer and inserted a deflectable ablation catheter from the left subclavian vein to remove the fractured abandoned ventricular lead. We tried looping the ablation catheter around the fractured lead, but the tip of the ablation catheter was too soft to maintain its bend position against the tension created when pulling at the lead. We then created a pulley by grasping the catheter tip with a triple-loop snare inserted from the right jugular vein to support the ablation catheter and to add more traction (Video 2). However, even with the added force, we were unable to free the lead, leading us to believe that the lead had strongly adhered to the vascular wall.
Management
We exchanged the 9.0-F introducer sheath with a steerable introducer, but this also failed to release the lead. After a few more attempts, we decided to change the direction of the force being applied because the current method was adding excessive tension to the tip of the lead embedded at the ventricle as well. An 18-F sheath was inserted through the right femoral vein for a femoral approach using a Needle’s Eye Snare. The Needle’s Eye Snare (Cook Medical LLC) was positioned to grasp the lead between the pulley and the tip of the lead at the ventricle. The pulley was pulled upward while keeping the Needle’s Eye Snare grasp fixed to prevent extra force being added to tip of the lead (Figure 5, Video 3). Because the lead adhering to the spermatic vein gradually started to release, we used the Needle’s Eye Snare to slowly pull the lead in toward the right atrium while simultaneously continuing to pull the pulley upward. As a result, we successfully removed the distal end of the fractured lead from the spermatic vein and migrated it into the right atrium (Video 4).
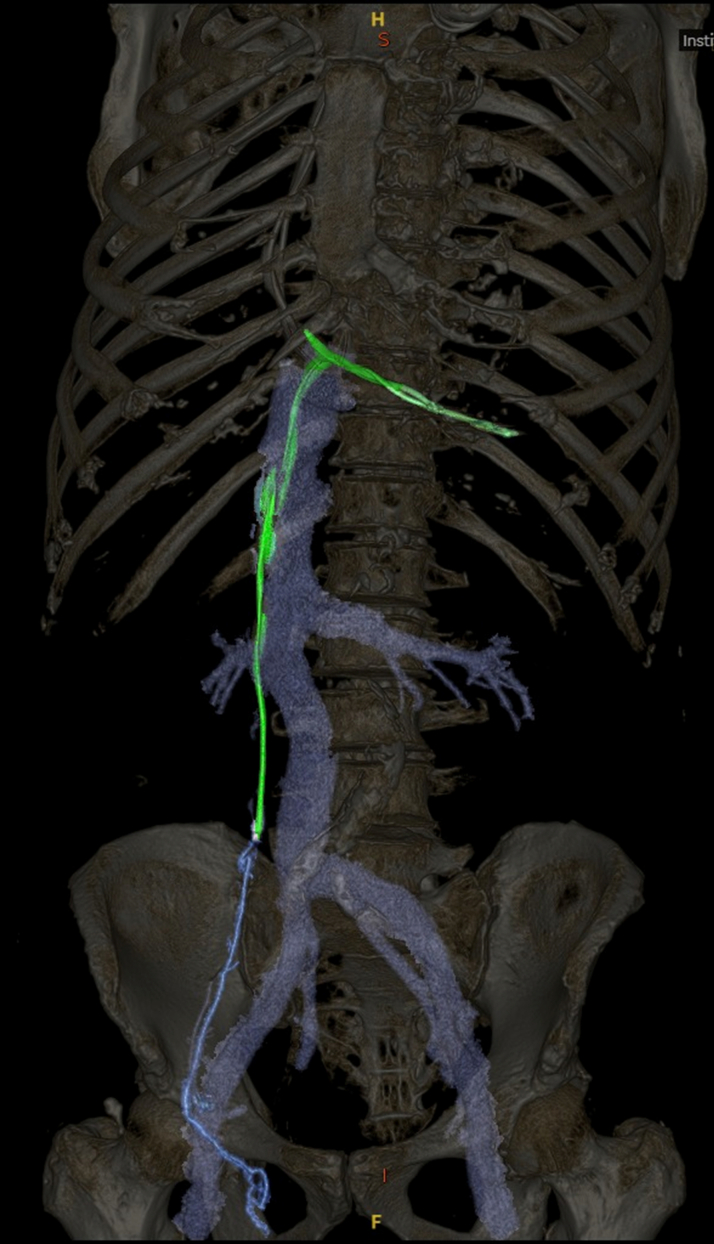
Figure 5.
Illustrative Figure
The illustration shows each of the subclavian, femoral, and jugular approaches as well as the anatomy of the right and left spermatic veins. Although the left spermatic vein connects to the left renal vein, the right spermatic vein connects to the inferior vena cava, which may be why the fractured lead migrated into the right spermatic vein.
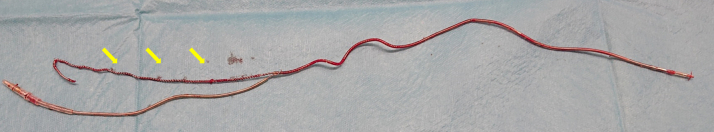
Although transvenous lead extraction (TLE) via the jugular vein is a very useful method, in our case, the end of the fractured lead was pointing downward and was overstretched, making it difficult to grasp the lead from a jugular approach. Therefore, to prepare for lead extraction from the femoral vein, the Needle’s Eye Snare was exchanged with a triple-loop snare to grasp the distal end of the lead. A laser sheath was then inserted along the lead but did not reach the tip of the lead at the ventricle. Therefore, a steerable introducer was inserted along the lead into the laser sheath, and the tip of the lead was successfully removed using countertraction (Video 5). The extracted lead had partially damaged silicone coating, and the inner coil was overstretched (Figure 6).
Figure 6.
The Extracted Lead
The outer silicone coating was partially peeled off, and the inner coil was overstretched (yellow arrows).
Discussion
Despite higher comorbidity rates, TLE in elderly patients has been reported as a safe and effective method of lead extraction.1 On the other hand, elderly patients have been reported to be 1 of the predictors of higher long-term mortality rates in patients undergoing TLE.2 Additionally, the ELECTRa (The European Lead Extraction ConTRolled) registry has associated a previously abandoned lead at the time of TLE with increased procedural failure and major complications.3 Hussein et al4 have also reported that TLE in patients with abandoned leads was more likely to require specialized extraction tools and an adjunctive rescue femoral approach. Both reports have shown increased failure and mortality rates in patients with abandoned leads undergoing TLE.
Although TLE is a technically complex procedure, a combined superior and femoral approach has been associated with a high complete success rate and a low complication rate.5 However, the reported cases involving the removal of fractured leads that have migrated outside of the heart are limited. Bontempi et al6 reported the removal of a fractured ventricular lead that had migrated into the IVC after 2 years of follow-up. Fortunately, in their case, they were able to successfully remove the lead using a single-loop snare and a laser sheath inserted from the femoral vein.
In our case, the attempt to remove the lead by simple upward traction using an ablation catheter failed. Further traction would have added an excessive load to the tip of the lead, so by inserting a Needle’s Eye Snare via the femoral approach, we were able to apply direct vertical force to the fractured lead and successfully detach the lead from the spermatic vein. We believe that changing the traction direction using a different approach is a useful technique for extracting a fractured lead that has migrated outside of the heart and has adhered to vessel walls. Furthermore, if migration of a fractured lead is suspected, early removal is recommended to minimize the effects of adhesion.
Follow-Up
After 2 weeks of adequate antibiotic therapy, a leadless pacemaker was implanted. The patient was discharged with no complications.
Conclusions
There is no established technique for the removal of fractured leads that have migrated out of the heart, especially when the lead has adhered to the vascular wall. We believe that changing the direction of traction force by using several approaches and tools—from the subclavian vein, internal jugular vein, or femoral vein with multiple snares and/or an ablation catheter—can be useful in removing fractured leads adhering to the vascular wall outside of the heart.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Coronal View CT Scan Showing the Fractured Lead Migrating From the IVC to the Right Spermatic Vein
The Fractured Lead Was Pulled Upward Using a Pulley Created by an Ablation Catheter Inserted From the Left Subclavian Vein and a Triple-Loop Snare Inserted From the Right Jugular Vein, But the Extraction Was Unsuccessful
To Change the Direction of Force, a Needle’s Eye Snare Was Inserted From the Right Femoral Vein
The Needle’s Eye Snare grasped the portion of the lead between the ablation catheter and the tip of the lead at the ventricle. We repeatedly pulled the pulley upward while keeping the Needle’s Eye Snare grasp fixed.
Successful Removal of the Fractured Lead From a Spermatic Vein
The dislodged portion of the fractured lead migrated into the right atrium.
Using the Femoral Approach, a Steerable Introducer Was Inserted Along the Lead Into the Laser Sheath, and the Tip of the Lead Was Successfully Extracted Using Countertraction
References
- 1.Pelargonio G., Narducci M.L., Russo E., et al. Safety and effectiveness of transvenous lead extraction in octogenarians. J Cardiovasc Electrophysiol. 2012;23:1103–1108. doi: 10.1111/j.1540-8167.2012.02372.x. [DOI] [PubMed] [Google Scholar]
- 2.Narducci M.L., Ruscio E., Nurchis M.C., et al. Mortality after transvenous lead extraction: a risk prediction model for sustainable care delivery. Eur J Clin Invest. 2023;53 doi: 10.1111/eci.13969. [DOI] [PubMed] [Google Scholar]
- 3.Segreti L., Rinaldi C.A., Claridge S., et al. Procedural outcomes associated with transvenous lead extraction in patients with abandoned leads: an ESC-EHRA ELECTRa (European Lead Extraction ConTRolled) Registry Sub-Analysis. Europace. 2019;21:645–654. doi: 10.1093/europace/euy307. [DOI] [PubMed] [Google Scholar]
- 4.Hussein A.A., Tarakji K.G., Martin D.O., et al. Cardiac implantable electronic device infections: added complexity and suboptimal outcomes with previously abandoned leads. J Am Coll Cardiol EP. 2017;3:1–9. doi: 10.1016/j.jacep.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Yap S.C., Bhagwandien R.E., Theuns D., et al. Efficacy and safety of transvenous lead extraction using a liberal combined superior and femoral approach. J Interv Card Electrophysiol. 2021;62:239–248. doi: 10.1007/s10840-020-00889-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bontempi L., Aboelhassan M., Cerini M., et al. Abandoned and fractured ICD lead with complete superior veins occlusion: is transvenous lead extraction still possible? J Cardiovasc Electrophysiol. 2020;31:3042–3044. doi: 10.1111/jce.14752. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronal View CT Scan Showing the Fractured Lead Migrating From the IVC to the Right Spermatic Vein
The Fractured Lead Was Pulled Upward Using a Pulley Created by an Ablation Catheter Inserted From the Left Subclavian Vein and a Triple-Loop Snare Inserted From the Right Jugular Vein, But the Extraction Was Unsuccessful
To Change the Direction of Force, a Needle’s Eye Snare Was Inserted From the Right Femoral Vein
The Needle’s Eye Snare grasped the portion of the lead between the ablation catheter and the tip of the lead at the ventricle. We repeatedly pulled the pulley upward while keeping the Needle’s Eye Snare grasp fixed.
Successful Removal of the Fractured Lead From a Spermatic Vein
The dislodged portion of the fractured lead migrated into the right atrium.
Using the Femoral Approach, a Steerable Introducer Was Inserted Along the Lead Into the Laser Sheath, and the Tip of the Lead Was Successfully Extracted Using Countertraction