SECTION 2 – ANSWER
CASE
A 47-year-old female dancer presented with right lateral heel edema and had pain with a numbness sensation. The range of motion of her right ankle was normal. She had not previously undergone any surgery on the affected ankle. Physical examination revealed a right lateral heel mass at the posterior talus–calcaneus junction. The mass was characterized by a mild numbness sensation on palpitation, which radiated to the lateral heel and foot. She underwent an ultrasound (US) examination [Figure 1]. Figure 1a was obtained by placing the transducer between the peroneus muscle and Achilles where the small saphenous vein and sural nerve are present. The subsequent US image revealed the long and short axis of a portion of the sural nerve [Figure 1b and c]. Magnetic resonance imaging (MRI) was performed for further evaluation and localization [Figure 2].
Figure 1.
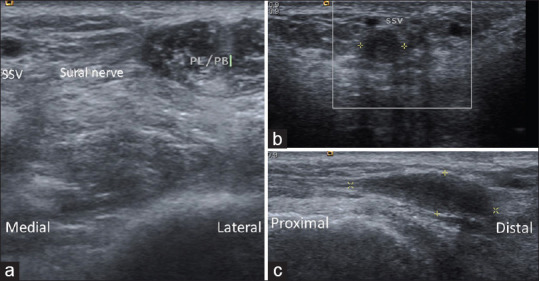
(a) Was obtained by placing the transducer between the peroneus muscle and the Achilles tendon where the small saphenous vein and sural nerve are just there. (b and c) Are ultrasound images of the long axis and short axis of part of the sural nerve. SSV: Small saphenous vein, PL: Peroneus longus muscle, PB: Peroneus brevis muscle
Figure 2.
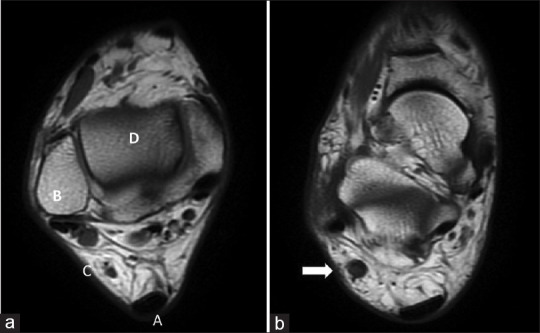
(a) A: Achilles tendon. B: Lateral malleolus of fibula bone. C: Sural nerve and small saphenous nerve. D: Tibial bone. (b) Magnetic resonance imaging long axis T1 FSE signal revealed an enlarged part of the sural nerve compared to Figure 1
INTERPRETATION
In the long-axis view [Figure 1], sonography revealed a hypoechoic mass in the sural nerve. The mass was 20 mm × 6 mm × 5 mm in size and located at the posterior to lateral malleolus level between the Achilles tendon and peroneus muscle. In addition, the power Doppler signal did not increase. The MRI image of the axis view at the level of the right lateral heel revealed an enlarged part of the sural nerve. The ultrasonographic and MRI diagnosis was a sural neuroma.
DISCUSSION
Dancers may experience some peripheral nerve disorders due to repetitive and extremely physiologically demanding movements.[1] Common nerve disorders in dancers are as follows: interdigital neuromas, tarsal tunnel syndrome, anterior tarsal tunnel syndrome, superficial and deep peroneal nerve entrapment, and sural nerve entrapment.
The sural nerve is a small sensory nerve that is located in the subcutaneous tissues of the calf.[2] It most frequently originates from the fusion of two proximal roots: the medial sural cutaneous nerve (a branch of the tibial nerve) and the lateral sural cutaneous nerve (a branch of the common fibular nerve). The nerve provides cutaneous innervation to the posterior calf, lateral ankle, lateral heel, and foot.
A sural neuroma is a peripheral nerve disorder that sometimes develops in dancers. Neuroma results from disorganized regeneration of following nerve injury and may be symptomatic, sometimes sural neuromas may arise from prior surgery or trauma to the lower extremity, but it may also be idiopathic. There are some surgical causes of sural neuroma: lateral ankle ligament repair, hindfoot arthrodesis, open reduction internal fixation, pes planovalgus correction, Achilles tendon repair, etc.[3]
US is a very useful tool that provides real-time evaluation, zero radiation, cost-effectiveness, portability, and ease of dynamic examination.[4] In addition, US offers some quantitative information for us.[5] In this case, the scanning protocol we adapt is from the previous literature by Chang, etc., that placing the transducer at the mid-calf level to visualize the sural nerve on top of the gastrocnemius muscle and then moving the transduce distally, we can see the sural nerve is descending with the small saphenous vein and courses between the Achilles tendon and peroneus muscles.[6]
The management of sural neuroma varies from conservative treatment to surgery. Sometimes, the sural neuroma is asymptomatic that is not necessarily to be treated. Symptomatic sural neuroma with presentation of pain or numbness should be treated start from conservative methods such as physical therapy, medication, or injection. If all the conservative treatment fails, surgery will be in consideration. Surgery may be divided into some techniques include resection alone, resection with subsequent nerve grafting or primary repair, transposition or relocation, relocation nerve grafting, targeted muscle reinnervation, etc., According to the previous literature, the surgical intervention resulted in either improvement or complete resolution of pain symptoms in 71% of the patients.[3]
Caused by extremely physiologically demanding movements, dancers may develop nerve disorders. Using US, clinicians can evaluate the presence of the pathologies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kennedy JG, Baxter DE. Nerve disorders in dancers. Clin Sports Med. 2008;27:329–34. doi: 10.1016/j.csm.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi S, Droz L, Lups Deplaine C, Dubois-Ferriere V, Delmi M. Ultrasonography of the sural nerve: Normal and pathologic appearances. J Ultrasound Med. 2018;37:1257–65. doi: 10.1002/jum.14444. [DOI] [PubMed] [Google Scholar]
- 3.Lans J, Gamo L, DiGiovanni CW, Chen NC, Eberlin KR. Etiology and treatment outcomes for sural neuroma. Foot Ankle Int. 2019;40:545–52. doi: 10.1177/1071100719828375. [DOI] [PubMed] [Google Scholar]
- 4.Chang PH, Chen YJ, Chang KV, Wu WT, Özçakar L. Ultrasound measurements of superficial and deep masticatory muscles in various postures: Reliability and influencers. Sci Rep. 2020;10:14357. doi: 10.1038/s41598-020-71378-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han DS, Wu WT, Hsu PC, Chang HC, Huang KC, Chang KV. Sarcopenia is associated with increased risks of rotator cuff tendon diseases among community-dwelling elders: A cross-sectional quantitative ultrasound study. Front Med (Lausanne) 2021;8:630009. doi: 10.3389/fmed.2021.630009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang KV, Mezian K, Naňka O, Wu WT, Lou YM, Wang JC, et al. Ultrasound imaging for the cutaneous nerves of the extremities and relevant entrapment syndromes: From anatomy to clinical implications. J Clin Med. 2018;7:457. doi: 10.3390/jcm7110457. [DOI] [PMC free article] [PubMed] [Google Scholar]


