Uterine inversion, or uterine intussusception, is a rare, potentially life-threatening entity characterized by inversion of the fundus into the uterine cavity, which often manifests as an acute complication of childbirth (1,2). Less commonly, uterine inversion is nonpuerperal, occurring as a result of an en dometrial or myometrial mass (2,3). Patients typically present with symptoms that include vaginal bleeding and pelvic pain.
At MRI, uterine inversion appears as a U-shaped uterus with loss of the normal convex fundal contour on sagittal images (Fig 1A, 1B) (2). A target configuration may be visualized on axial images, representing the concentric serosa, myometrium, and endometrium (Fig 1C, 1D) (2). MRI is also useful in assessing the cause in patients with nonpuerperal uterine inversion, including submucosal leiomyomas, uterine leio-myosarcomas, and endometrial malignancies. There are four grades of uterine inversion, which are characterized by the degree of inferior bowing of the fundus relative to the cervix and/or vaginal introitus (Fig 2).
Figure 1.
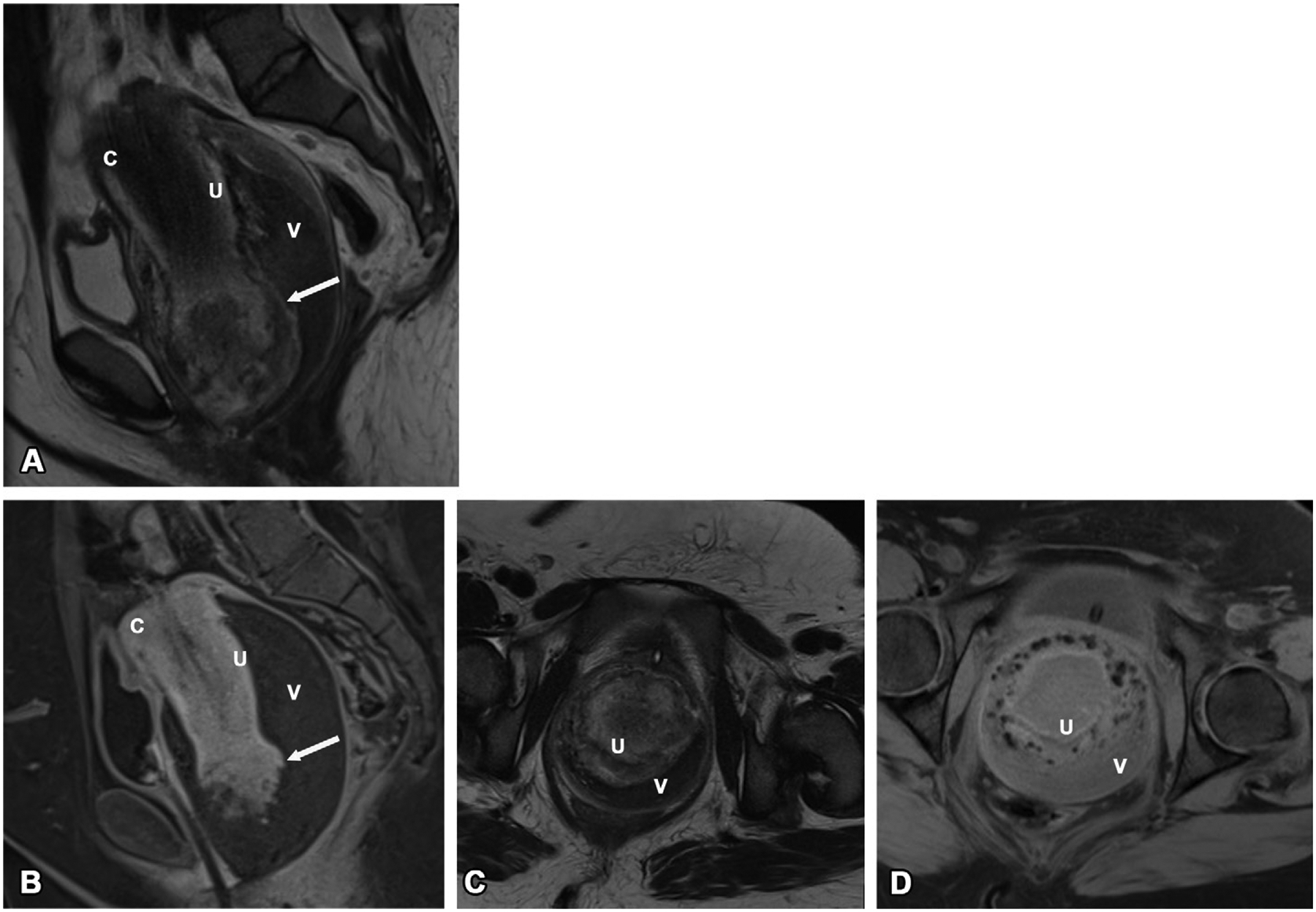
Uterine inversion in a previously healthy premenopausal female patient with acute onset of pelvic pain and vaginal bleeding. A bleeding vaginal or cervical mass was suspected on physical examination, and pelvic MRI was performed for further evaluation. Sagittal T2-weighted (A) and contrast-enhanced fat-suppressed T1-weighted (B) MR images of the pelvis demonstrate a U-shaped uterus (U) with loss of the normal fundal contour, with protrusion of the fundus into the distended vaginal canal (V), consistent with grade III uterine inversion. The cervix (C) is located superior to the inverted fundus. At the fundus, there is an ill-defined rounded lesion (arrow in A and B) with heterogeneous T1 signal intensity and enhancement with irregular margins, with adjacent heterogeneous T2 signal intensity and increased T1 signal intensity. The findings are most consistent with a hemorrhagic submucosal uterine leiomyoma. Axial T2-weighted (C) and contrast-enhanced fat-suppressed T1-weighted (D) MR images of the pelvis show concentric rings of signal intensity indicating the serosa, myometrium, endometrium, and vagina.
Figure 2.
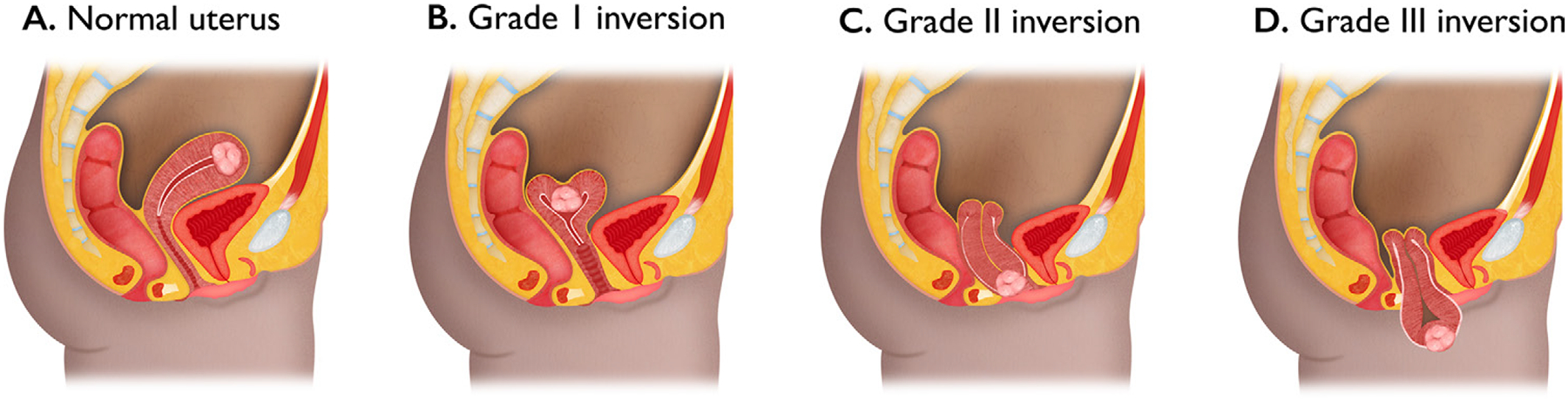
Illustration depicts the normal anatomic position of the uterus (A) and the various grades of inversion. Grade I uterine inversion (B) is characterized by inferior bowing of the fundus up to but not beyond the cervix. In grade II uterine inversion (C), the inverted fundus protrudes through the cervix and into the vagina. The uterus is fully inverted and protrudes out of the vagina in grade III uterine inversion (D).
Footnotes
Disclosures of conflicts of interest.—K.M.Z.M. Meeting attendance and travel reimbursement from Trinity Health Oakland Hospital. P.B. Editorial board member of RadioGraphics, Association of University Radiologists GE Radiology Research Academic Fellowship, meeting travel reimbursement from the American College of Radiology.
K.M.Z.M and P.B. have provided disclosures (see end of article); all other authors have disclosed no relevant relationships.
References
- 1.Wendel MP, Shnaekel KL, Magann EF. Uterine inversion: a review of a life-threatening obstetrical emergency. Obstet Gynecol Surv 2018;73(7):411–417. [DOI] [PubMed] [Google Scholar]
- 2.Foti PV, Tonolini M, Costanzo V, et al. Cross-sectional imaging of acute gynaecologic disorders: CT and MRI findings with differential diagnosis. Part II: uterine emergencies and pelvic inflammatory disease. Insights Imaging 2019;10(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dadgar S, Pourhosseini SA. Non Puerperal Uterine Inversion Due to Submucous Myoma: A Case Report. J Family Reprod Health 2018;12(3):169–172. [PMC free article] [PubMed] [Google Scholar]


