Abstract
Objective
The aim of this study was to evaluate the effect of perturbation-based treadmill training on gait quality in daily life, a predictor of fall risk that was used as the primary outcome. An additional aim was to evaluate the effects on secondary outcomes, including balance, gait performance, self-efficacy, daily life physical activity, and falls.
Methods
Seventy community-dwelling older adults (mean age = 74.73 [SD = 5.69] years; 46 women) at risk of falling were randomized and received 4 weeks of dual-task treadmill training, either with or without treadmill perturbations. Balance, gait performance, self-efficacy, and daily life trunk accelerometry at baseline, after intervention, and at a 6-month follow-up were assessed and compared within group over time and between groups for each time point, and their change rates between groups over time were also assessed.
Results
Both groups improved in their balance, gait performance, and self-efficacy; the experimental group showed a significantly larger decrease in concern of falling and an increase in physical performance than the controls. These training effects did not translate into significant improvements in daily life gait quality or physical activity. However, the number of daily life falls and the percentage of fallers decreased significantly more in the experimental group.
Conclusion
A 4-week perturbation-based dual-task treadmill training program can improve self-efficacy, balance, and gait performance in a controlled setting and reduce daily life falls, although not through changes in quantity or quality of daily life gait.
Impact
Perturbation-based treadmill training is a safe and efficient way to train older adults’ balance recovery and gait performance, increase self-efficacy, and prevent falls.
Keywords: Accidental Falls, Activities of Daily Living, Aging, Balance, Gait, Gait: Gait Training, Locomotion, Mobility, Posture, Virtual Reality
Introduction
Falls among older adults unfortunately are very common, with about one-third of older adults aged over 65 years experiencing at least 1 fall annually.1,2 The incidence rate increases with age, with half of the people aged over 80 years falling each year.2–4 A fall can have devastating consequences, such as fractures, head injuries, and even death. Preventing falls is therefore key for public health and quality of life among older adults.
As a large proportion of falls are caused by perturbations during walking, such as slips and trips,5 perturbation-based training may improve balance responses and reduce fall risk.6 On a treadmill, perturbations can be easily and safely applied by sudden belt accelerations or decelerations, provoking forward or backward balance loss. Recent studies have shown that perturbation training can be very effective with up to 50% reduction in daily life falls.7,8 Moreover, these type of interventions require less training sessions than conventional training.8–11 Perturbation-based treadmill training therefore seems to be an efficient and promising approach, in line with the concept of task specificity of training.12
Integrating cognitive dual tasking in a motor-learning intervention can facilitate learning, automatization of the motor task, and transfer to daily life situations by distracting participants from the primary motor task.13,14 Dual-task training has shown beneficial effects compared to single-task training. A systematic review concluded that dual-task training in older adults who were healthy had stronger effects on postural stability15 and, specifically, that walking under dual-task conditions improved more after training that combined treadmill walking with a cognitive dual task than with treadmill walking alone.14,16 The REACT is a treadmill module that was developed for the C-Mill (Motek Medical BV, Amsterdam, the Netherlands) and that allows perturbation training and dual-task exercises.
Although most studies on perturbation training have shown positive effects on stability and gait performance in clinical or laboratory settings,17,18 translation of these effects to daily life gait behavior remains unclear.18 To get a better insight into whether and how perturbation-based treadmill training affects gait quality and physical activity in daily life, ambulatory measurements of daily life gait are needed.
We aimed to evaluate the effect of the REACT perturbation-based treadmill training on gait quality in daily life, a predictor of fall risk that we used as our primary outcome. In addition, we aimed to evaluate effects on secondary outcomes: balance and gait performance and self-efficacy and daily life physical activity and falls. In this randomized controlled trial, we compared 4-week treadmill training programs under cognitive dual-task conditions with and without perturbations. We hypothesized that participants in the REACT group (with perturbations) would show larger effects than those in the control group (without perturbations) on all outcome measures. The results of this randomized controlled trial may support the application of perturbation-based treadmill training to enhance conventional fall prevention training in older adults.
Methods
Recruitment
In total, 70 participants were recruited, 30 through physical therapists on-site, 10 from a local hiking club, and the remaining through flyers distributed to general practitioners, leisure centers, local newspapers, and online. The participants were 65 years or older, generally healthy, and identified at being at risk of falling with a short questionnaire that asked for falls in the past 12 months and difficulties in moving, walking, and keeping balance.19 None of the participants had prior experience with perturbation training and all passed a cognition and memory test (>24 points on the Montreal Cognitive Assessment20). Any neurological, cardiovascular, or pulmonary morbidity (ie, stroke, heart attack, hypertension) led to exclusion, as did orthopedic complications (ie, lower extremity fractures, low bone density, joint replacements) within the past 6 months. A complete list of the inclusion and exclusion criteria is reported in our protocol article.21
For a more detailed description of the power analysis, we refer to Rieger et al.21 For our primary outcome, we used a 2-way repeated-measures analysis of variance with training (control group vs experimental group) as a between-subject factor and time point (before vs after training) as a within-subject factor. Based on a study on perturbation training and a meta-analysis on conventional training,8,22 a medium effect size (f = 0.25) for the interaction of group and time could be expected. However, since we used less strong perturbations, we assumed a slightly smaller effect size (f = 0.21). Setting alpha at .05 and power at 0.95 and assuming a 0.6 correlation between time points,23 G*Power,24 version 3.1.9.2, indicated a total sample size of 62 (31 per group). To account for dropouts, a total number of 70 participants was included. This study complied with the Declaration of Helsinki. Medical ethical approval was obtained (METC Brabant, project number P1856) and the trial was registered (trial NL7461 [NTR7703]). All participants provided written informed consent for this study.
Trial Setup
The setup was described in detail in our study protocol.21 Briefly, the participants walked on the C-Mill VR+ (Motek Medical BV), an instrumented treadmill with augmented and virtual reality to train balance, gait, and gait adaptability. The treadmill was equipped with the new REACT module that allowed sudden belt perturbations in the anterior and posterior directions, provoking forward or backward balance loss.21 A full-body harness connected to an overhead frame allowed the participants to move freely without body weight support but prevented them from hitting the treadmill in case of falling. At the same time, cognitive dual tasks were provided on the screen at the front of the treadmill; participants controlled these with a handheld controller (Switch Joy-Con; Nintendo Co Ltd, Kyoto, Japan). The dual-task exercises were designed to distract the participant from walking and facilitate implicit learning, automatization, and transfer to a daily life situation.
Study Design and Measurement Protocol
The procedure is described extensively in our study protocol.21 In short, participants trained twice per week for 30 minutes on the C-Mill for 4 weeks. They received a random computer-generated unique identification number at the baseline assessment. With this identification number, the therapist of the first training session allocated the participant to either the REACT group, receiving perturbation-based gait training under cognitive dual-task conditions, or the control group, receiving gait training under cognitive dual-task conditions without perturbation. This procedure kept the assessors blinded to treatment allocation.
Prior to the training and after the intervention, all participants wore an inertial measuring unit (Dynaport MoveMonitor; McRoberts BV, The Hague, the Netherlands) on their back with an elastic band around their waist for 7 consecutive days. Physical performance was assessed with the Short Physical Performance Battery (SPPB), Four Square Step Test, and Mini Balance Evaluation Systems Test (Mini-BESTest). Self-efficacy was assessed with the General Self-Efficacy Scale, Falls Efficacy Scale-International (FES-I), and modified Gait Efficacy Scale. These 3 questionnaires represent different aspects of confidence and quality of life in relation to falls and were administered because the experience of successful balance recovery during the training may affect confidence.
At baseline, participants were asked to report the number of falls experienced during the preceding 6 months. During the follow-up period of 6 months, the number of daily life falls was monitored with falls calendars. These calendars included questions for each fall on the activity preceding the fall (eg, walking, turning, standing up), the cause of falling (eg, trip, slip, dizziness), the fall direction (forward, backward, sideward), and whether the fall resulted in an injury. Participants received a phone call at the end of the follow-up period to discuss any issues in reporting falls and to remind them to return the calendar.
Training Progression
Over the 4-week training period, the therapist adjusted the training difficulty to match the participant’s improvements and to maintain a challenging training content. The therapist could adjust the walking speed and dual-task difficulty in both groups, and in the case of the REACT group, they could also modify the perturbation difficulty. The challenge experienced by the participant was judged by the therapist, because no objective criteria were available, and clinical evaluation was deemed appropriate in this context. Training progression was constrained by the following guidelines (in order of priority): increase walking speed every week, at least to reach preferred overground walking speed in week 4; increase the perturbation difficulty every week, by increasing the levels of acceleration/deceleration intensities and duration (resulting in a stronger perturbation with a greater displacement of the stance leg, independent of walking speed), without the participant’s needing to grab the handrail to recover; and increase the difficulty level of the dual task every week, by increasing the game speed and complexity. For a detailed description of the adjustable training parameters, please refer to our study protocol.21
Data Analysis
We processed accelerometer data with custom MATLAB scripts (version R2018a; The MathWorks, Inc, Natick, MA, USA). Daily life gait quality was calculated from all locomotion bouts, using algorithms that quantify gait speed, intensity, regularity, stability, symmetry, smoothness, and complexity, as described before.23,25,26 Briefly, a composite score of gait quality parameters was used. This score consists of the autocorrelation at the dominant frequency of vertical accelerations, describing gait variability; the SD of the signal in the mediolateral direction, describing the gait intensity; gait smoothness, as expressed with the index of harmonicity in the mediolateral direction; and gait variability, as expressed as the power at the dominant frequency in anterior–posterior acceleration. This score is reliable27 and predicts future falls.25 All locomotion bouts longer than 10 seconds were cut into 10-second epochs for which the composite score was determined.25 The composite score can be seen as a z score, where 0 is the average and the value of 1 is 1 SD better than average. To describe responders and nonresponder to the intervention, daily life gait quality composite scores were calculated for every walking episode and compared between time points on an individual level using paired-samples t-tests.
Gait speed, as estimated over each daily life gait epoch,28 was fitted with a Gaussian bimodal distribution divided by the pooled SD. The Ashman D was calculated using the difference in gait speed means in the distribution; an Ashman D of >2 indicates a bimodal distribution fit.29 To quantify the daily life gait speed at baseline and after the intervention, the second peak of the bimodal gait speed distribution was extracted. This peak is presumed to represent longer outdoor bouts of walking.30
On the basis of the inertial measuring unit data, the total wear time and activity classification per day (ie, standing, shuffling, locomotion, cycling, stair walking, lying, and sitting) were provided by the manufacturer’s algorithm.31 For days on which the accelerometer was worn more than 12 hours,32 we calculated the total duration of locomotion, sitting, standing, and lying, the number of strides, the average number of locomotion bouts, the median and maximum durations of walking bouts, and the number of transitions from sitting or lying. These numbers were averaged over all eligible days to quantify physical activity.
Statistics
Analyses were performed with SPSS version 25 (SPSS Inc, Chicago, IL, USA). First, we checked for normality of data using the Shapiro–Wilk test. Second, the interquartile range rule was used to detect potential outliers. As no extreme outliers (exceeding 3 times the interquartile range) were found, no data points were excluded from the analyses. The level of significance was set at alpha = .05.
To assess changes in gait quality, the effects of time point, group, and their interaction were analyzed using repeated-measures analysis of variance, with time as a within-subject factor and group as a between-subject factor. If analysis of variance revealed significant effects, then post hoc paired-samples t-tests were used to explore differences between groups or time points.
Nonparametric results are presented as the median difference between postintervention and baseline data and the minimum and maximum of the change. When data were not normally distributed, interactions between group and time points were identified with Mann–Whitney U tests on the delta scores between baseline and postintervention data. Wilcoxon signed rank tests were used to test for differences between measurement points within groups. This procedure was used for balance and gait performance tests, self-efficacy questionnaires, physical activity measures, and falls. For changes in the number of fallers, z tests were used.
Role of the Funding Source
The funder played no role in the design, conduct, or reporting of this study.
Results
Participant Characteristics
Figure 1 depicts the flow of participants through the progression of the study. Three participants discontinued the trial, either due to treatment allocation (control), knee pain (REACT), foot inflammation (REACT), or because the training was too intense (REACT). For 1 of these participants (REACT), data were available at both measurement time points, and these were included in the analysis. The other 3 also decided not to participate in the postintervention and follow-up assessments. Two other participants (REACT) had technical issues with the inertial measuring unit and were excluded from the analysis of the inertial measuring unit data (daily life gait quality and quantity) only. The Table presents participants’ characteristics. Only the Montreal Cognitive Assessment score showed a small but significant difference between the 2 groups.
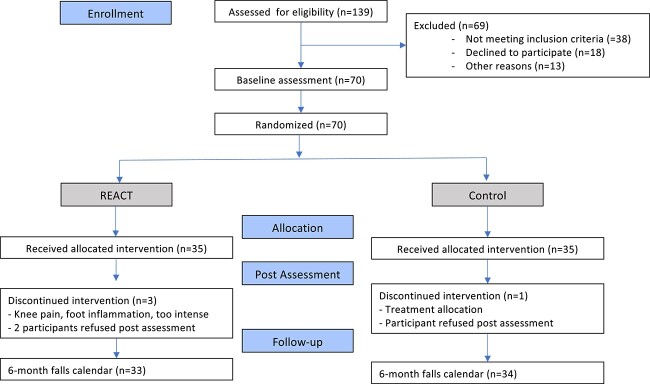
Figure 1.
Enrollment, allocation, and dropout of participants presented as a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. The number of participants in the group allocated to the REACT intervention is 33 because a participant without inertial measuring unit data still provided follow-up data.
Table.
Participant Characteristics
| Characteristic | REACT Group (n = 35) a | Control Group (n = 35) a | P b |
|---|---|---|---|
| Age, y | 75.5 (5.4) | 73.9 (5.9) | .25 |
| Sex assigned at birth, n (%) women | 25 (71) | 25 (71) | 1.00 |
| Height, m | 1.72 (0.09) | 1.69 (0.08) | .28 |
| Weight, kg | 76.2 (12.8) | 74.3 (13.1) | .55 |
| MoCA, points | 27.0 (1.7) | 27.9 (1.7) | .04 |
| No. of falls in 6 mo, median (minimum–maximum) | 0 (0–6) | 0 (0–4) | .21 |
| Fallers in 6 mo, n (%) | 14 (40) | 10 (29) | .16 |
| n with <2 falls | 5 | 7 | |
| n with ≥2 falls | 9 | 3 |
Data are presented as mean (SD) unless otherwise indicated. MoCA = Montreal Cognitive Assessment.
P indicates parametric or nonparametric group comparisons.
Daily Life Gait Quality
Gait quality composite scores were normally distributed. For the daily life gait quality, no significant time effects (F1,62 = 1.072 [P = .31]; group F1,62 < 0.001 [P = .99]) or time × group interaction effects (F1,62 = 2.384 [P = .13]) were found (Fig. 2). Additional analysis on an individual level revealed that 14 participants in the REACT group and 17 participants in the control group significantly improved their daily life gait quality, whereas 9 in the REACT group and 15 in the control group significantly decreased their daily life gait quality after the intervention. The results for the remaining 9 participants remained unchanged compared to those at baseline.
Figure 2.
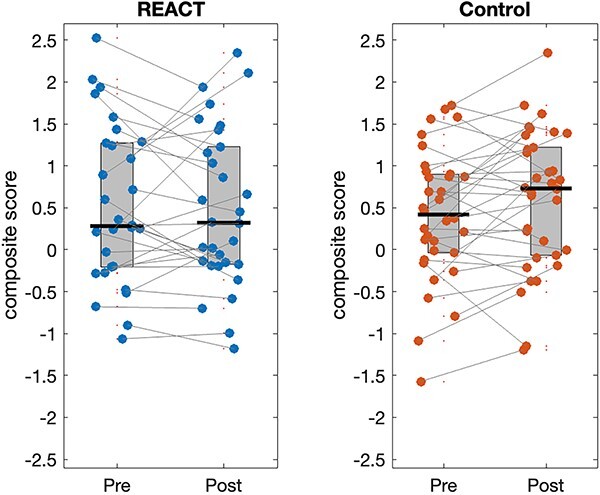
Daily life gait quality composite score calculated as the mean over the medians/d over the week. The dots indicate individual participants, with lines connecting their pre- and postintervention measurements. The horizontal black lines indicate the group means.
Physical Performance and Self-Efficacy
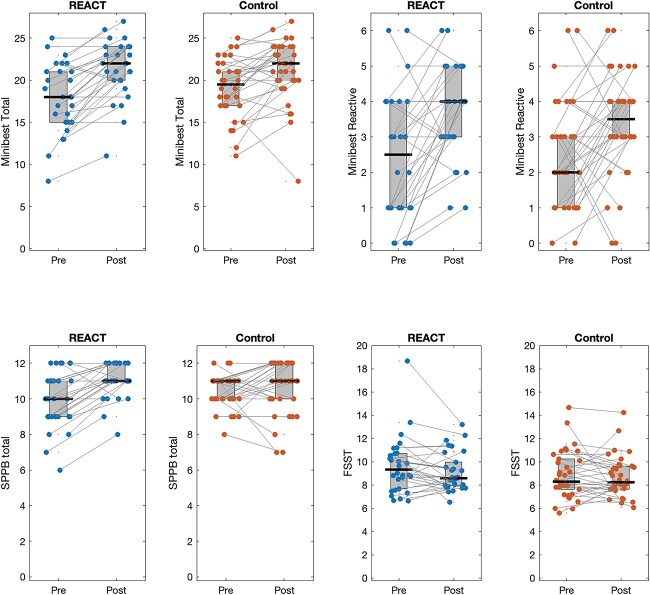
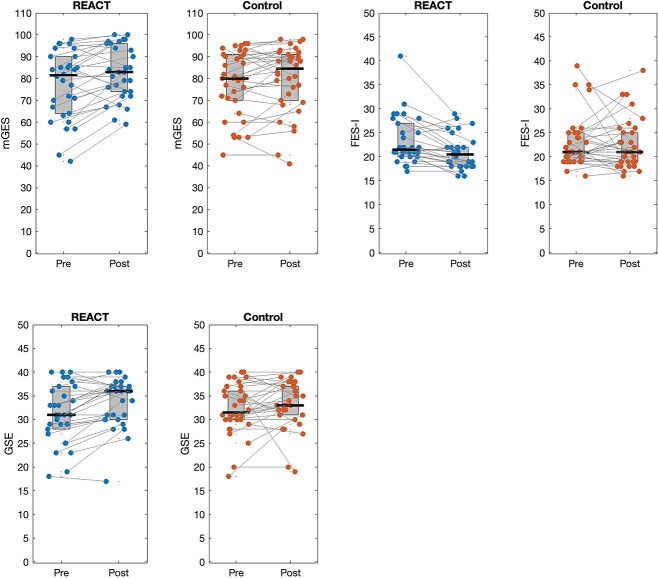
Clinical assessment scores were not normally distributed. We found no differences between groups at baseline for any of the physical performance and self-efficacy assessments. Comparison of delta values between groups yielded significantly larger improvements in the REACT group than in the control group for SPPB (P = .03) and FES-I (P = .01). The REACT group improved on the SPPB (the difference between base line and postintervention, Δ = 1 [−2, 3] point [P ≤ .001]), while the control group did not (Δ = 0 [−4, 3] point [P = .24]). Similarly, the REACT group improved on the FES-I (Δ = −2 [−12, 3] points [P < .001]), while the control group did not (Δ = 0 [−17, 12] point [P = .91]). Delta values did not significantly differ between groups, but significant improvements across both groups were found for the Mini-BESTest total scores (3 [−7, 10] [P < .001]) and Mini-BESTest reactive control scores (1 [−3, 4] [P < .001]) as well as for modified Gait Efficacy Scale (3.5 [−12, 23] [P < .001]) and General Self-Efficacy Scale (1.5 [−17, 10] [P < .001]). There were no significant changes in performance on the Four Square Step Test. Figures 3 and 4 illustrate the outcomes for all measures for both groups.
Figure 3.
Balance and gait performance. The dots indicate individual participants, with lines connecting their pre- and postintervention measurements. The horizontal black lines indicate the group medians. FSST = Four Square Step Test; Minibest Total = total score; Minibest Reactive = reactive subscore; SPPB = Short Physical Performance Battery.
Figure 4.
Self-efficacy outcomes. The dots indicate individual participants, with lines connecting their pre- and postintervention measurements. The horizontal black lines indicate the group medians. FES-I = Falls Efficacy Scale–International; GSE = General Self-Efficacy Scale; mGES = modified Gait Efficacy Scale.
Physical Activity
All participants had sufficient inertial sensor wear time (more than 12 h/d for a minimum of 4 days) to have reliable data over 7 consecutive days.27,33 Physical activity data were not normally distributed. There were no significant interactions (all Ps ≥ .21), effects of time (all Ps ≥ .23), or group differences (all Ps ≥ .31). An overview of physical activity outcomes is shown in the Supplementary Figure S1.
Daily Life Falls
The change in self-reported number of daily life falls from 6 months before the intervention to the 6-month follow-up was significantly different between the groups (P = .03). In the REACT group, the number of daily life falls decreased by 64% from 28 to 10 (0 [−6, 3] [P = .02]) (Fig. 5); however, it did not significantly change in the control group, in which falls decreased by 18.8% from 16 to 13 (0 [−3, 1] [P = .67]).
Figure 5.
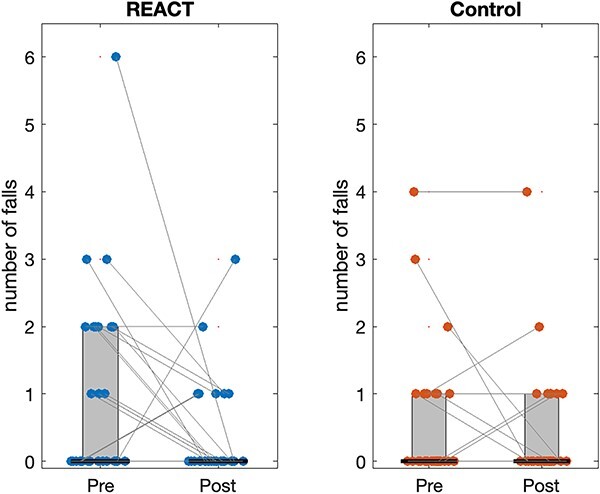
Total number of daily life falls. The dots indicate individual participants, with lines connecting their pre- and postintervention measurements. The horizontal black lines indicate the group medians.
The change in percentage of fallers was significantly different between groups (z = −2.82 [P = .01]). In the REACT group, the number of fallers decreased significantly by 46% from 13 to 7 fallers (z = −1.81 [P = .04]). In the control group, the number of participants who experienced a fall decreased nonsignificantly by 10% from 10 to 9 fallers (z = −0.27 [P = .39]).
Discussion
We compared the effects of dual-task perturbation-based treadmill training and dual-task treadmill training without perturbations on gait in daily life as our primary outcome, and physical performance, self-efficacy, physical activity, and falls in daily life as secondary outcomes. We observed no beneficial effects of perturbation-based training on daily life gait quality nor on the quantity of walking daily life, but did find beneficial effects on SPPB scores, concern of falling, number of falls, and percentage of fallers.
Training Effects on Daily Life Gait Quality and Quantity
No effects of training on daily life gait quality or quantity were found in spite of positive training effects on functional performance and concern of falling. Possibly longer training interventions are needed to achieve such behavioral changes. However, this remains speculative as, to our knowledge, no evidence of effects of longer training programs on daily life gait is available.
The composite score of daily life gait quality may not be sensitive enough to detect changes over time. We chose the composite score of daily life gait quality as our primary outcome, because it is a predictor for falls.24 However, it was recently shown not to be sensitive to change in relation to an exercise intervention or falling during follow-up.34
Variance in environmental conditions may confound ambulatory assessments; for example, more frequent walking in more challenging, complex environments may lead to less smooth, more variable, and less stable walking and hence result in lower gait quality.33 A relative increase in outdoor walking may have offset any changes in gait quality due to the higher challenges in outdoor situations. However, our participants did not take more steps, nor walked for a longer total duration or faster after the intervention. Therefore, it seems unlikely that participants exposed themselves more to challenging outdoor walking environments.
Due to task specificity, perturbation-based training may not influence steady-state gait but train perturbation responses to prevent falling.35 Daily life gait quality may not reflect an improvement in these responses, whereas our findings regarding falls suggest that they could be crucial for preventing falls when perturbed in daily life situations. Quantification of the number of near-falls and the quality of balance recovery responses from daily life accelerometry is still difficult,36 but may be a future way to understand the pathways for translation of perturbation-based treadmill training effects in reducing falls.
Training Effects on Clinical Assessments
The REACT group improved significantly more in physical performance (SPPB) and concern of falling (FES-I) than the control group. Although no significant interactions were found for balance performance (Mini-BESTest), general self-efficacy, and confidence in walking (modified Gait Efficacy Scale), implying that improvements were not significantly different between groups, the REACT group showed on average larger improvements in these outcomes. Compared with conventional fall-prevention interventions that mostly take longer than 1 month to achieve significant improvements in balance performance in older adults,22,37–39 the REACT program combining task-specific perturbation training with cognitive dual tasking appears to achieve similar results in balance and gait performance in a shorter period.
We found no indication for transfer to a lean-and-release task (Mini-BESTest reactive) and a voluntary stepping task (Four Square Step Test). Compared to other perturbation studies, we used smaller perturbations at a magnitude below threshold that induces falling, but with a large number of perturbations. A number of studies suggest that training with high-magnitude perturbations is more likely to trigger generalizable adaptations than low-magnitude ones.40–42 Previous work supports that not only an increased perturbation magnitude but also an increased number of perturbations may improve the transfer from treadmill-induced perturbations to overground perturbations.42,43
Previous literature reported that combined gait and cognitive task training can improve the balance as assessed with the Berg Balance Scale.14 This appears in contradiction with the lack of change on the SPPB in the control group and a lack of change on the Four Square Step Test in both groups in the present study. Obviously, these tests do not completely overlap in terms of constructs tested and hence may differ in sensitivity to change. In addition, differences in training intensity, frequency, and duration, as well as fitness of the populations tested may have contributed to such differences between study outcomes.
We assessed self-efficacy with the FES-I, modified Gait Efficacy Scale, and General Self-Efficacy Scale and showed that the REACT training led to significant improvements in all 3, and for FES-I larger improvements in the REACT group. Theoretically, performance accomplishments are needed to improve self-efficacy44 and these would be provided by successful balance responses during training in the REACT group. Regarding both groups, treadmill gait training with cognitive dual tasks or perturbations has been shown to increase gait stability in older adults at risk of falling.16,18 Improved gait stability may also be experienced as performance accomplishment and as a result increase self-efficacy. However, if present, such increased stability was not detected by the composite gait quality measure used.
Training Effects on Falls and Fallers
In the REACT group, we found a positive training effect on the number of falls and the number of fallers. These positive effects, which were not present in the control group and which did not coincide with improved gait quality, suggest that training may have had a task-specific effect, that is, achieved through improved balance recovery. Improved recovery responses after training with treadmill slips and trips and transfer to untrained overground slips and trips have been reported.9,45–51 These examples show that perturbation training can enhance recovery performance following untrained perturbations, similar to the trained task. Since slips and trips constitute the major causes of falls in daily life,52 such specific training effects may yield benefits in daily life as also found earlier.7,8
We aimed to improve transfer to daily life by adding cognitive dual tasking to the training to facilitate automatization of the motor task and transfer to daily life situations.13,15 Dual tasking during conventional treadmill gait training in older adults has been shown to improve balance, gait, and dual-task performance,14,53 presumably due to the fact that dual tasking is common in daily life gait as well.
Strengths and Limitations
The strength of our study was the comprehensive assessment and analysis of a range of outcome measures of perturbation-based treadmill training, from controlled assessment of physical performance to daily life behavior.
There are also some limitations to address. During the training sessions, level of challenge was judged by the therapist and adapted for the next training. No objective measure of a participant’s performance was used to adjust the training intensity. Although people were challenged, none of the participants fell in the harness during training. Possibly, even higher perturbation intensities, leading to more challenge and (near-) falls, would further improve reactive balance control and force participants to explore and adopt alternative recovery strategies.18 On the other hand, experiencing real falls, even in a safe environment, may also frighten participants and limit participation in the training. As it has been shown that even training with low-magnitude perturbations is effective to reduce fall risk,18,54 we chose for a challenging training without real falls, to achieve a continuous training without stopping the treadmill due to falls into the harness.
We assumed that participants had a regular week during our daily life inertial sensor measurements before and after the training, but obviously random and for example seasonal effects may have caused deviations in physical activity patterns between weeks. However, our block randomized design should be sufficient to account for such potential seasonal effects.
We used the McRoberts algorithm to classify episodes of walking, and only those of at least 10 seconds were used for our analyses. Annotation of separate walking episodes due to turns or sudden short stops may have limited the number of gait episodes of more than 10 seconds. Moreover, a shorter threshold may also increase to total amount of (short) gait episodes for analyses. Future research is needed to optimize gait classification and selection of relevant daily live gait episodes.
Reporting of falls was based on recall, and especially the baseline measurement may have been affected by this. However, we do not expect a differential effect of this in the 2 groups. For the follow-up, we provided clear instructions on how to fill in the falls calendar, which was supposed to be done as soon as a fall occurred during the follow-up period. In addition, we provided a 1-page instruction sheet and our contact details to allow posing any questions. With the use of a falls calendar in our population of people who were cognitively healthy, we expected biases to be minimal. We checked the total number of falls in a final call at the end of this follow-up period. On the final call, participants did not report to have experienced any issues in reporting falls. As falls incidence was not our primary outcome and the study was expected to be underpowered for this outcome, we had decided not to have monthly phone calls.
Finally, from March until May 2020, the COVID-19 pandemic led to a lockdown in the Netherlands for which people were advised to stay at home as much as possible. This may have influenced the 6-month follow-up on falls due to exposure of 9 participants from the REACT group and 10 from the control group. As the number of participants and the preintervention fall rate did not differ between groups, we kept these participants in the analyses.
Conclusion
REACT is a task-specific, safe, and effective stand-alone intervention that improves balance and gait performance and leads to a reduction in concern about falling. The training-specific improvements did not transfer to changes in participants’ daily life gait behavior, but did agree with a significant reduction of falls in the REACT group. Measures of balance recovery performance during training, as well as in daily life, are recommended to further improve our understanding of participants’ challenge during a training session, and of the mechanisms underlying transfer of training effects into reducing falls.
Supplementary Material
Contributor Information
Markus M Rieger, Department of Human Movement Sciences, Amsterdam Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands; Motek Medical B.V., Houten, Amsterdam, The Netherlands.
Selma Papegaaij, Motek Medical B.V., Houten, Amsterdam, The Netherlands.
Frans Steenbrink, Motek Medical B.V., Houten, Amsterdam, The Netherlands.
Jaap H van Dieën, Department of Human Movement Sciences, Amsterdam Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands.
Mirjam Pijnappels, Department of Human Movement Sciences, Amsterdam Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands.
Author Contributions
Markus M. Rieger (Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing—original draft), Selma Papegaaij (Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing—review & editing), Frans Steenbrink (Conceptualization, Funding acquisition, Resources, Supervision, Writing—review & editing), Jaap H. van Dieën (Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing—review & editing), and Mirjam Pijnappels (Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing—original draft, Writing–review & editing)
Funding
This study was funded by grants from the European Union’s Horizon 2020 Research and Innovation Program under the Marie Skłodowska-Curie grant agreement (721577) and by a Vidi grant (91714344) from the Dutch Organization for Scientific Research (NWO). Motek Medical B.V. did not fund this study, but a device from this company was used for this trial.
Ethics Approval
This study was approved by the Medisch Ethische Toetsingscommissie Brabant (Project No. P1856). Patients provided written informed consent.
Clinical Trial Registration
The study protocol is registered in the Dutch Trial Register (www.trialregister.nl identifier Trial NL7461 [PNTR7703]). Please find the full trial protocol at: https://pubmed.ncbi.nlm.nih.gov/32380950/.
Data Availability
Individual participant data presented in the figures are available upon request.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest. This article is adapted from a dissertation posted on the VU Research Portal, Vrije Universiteit Amsterdam’s repository (https://research.vu.nl/ws/files/121491546/400602.pdf). Three authors (M.M. Rieger, S. Papegaaij, and F. Steenbrink) are/were employed by Motek Medical B.V. and a device from this company was used for this trial.
References
- 1. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75:51–61. 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 2. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl 2:ii37–ii41. 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 3. Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–295. 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009;360:2390–2393. 10.1056/NEJMp0900963. [DOI] [PubMed] [Google Scholar]
- 5. Krasovsky T, Lamontagne A, Feldman AG, Levin MF. Effects of walking speed on gait stability and interlimb coordination in younger and older adults. Gait Posture. 2014;39:378–385. 10.1016/j.gaitpost.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 6. McCrum C. Fall Prevention in Community-Dwelling Older Adults. N Engl J Med. 2020;382:2579–2580. 10.1056/NEJMc2005662. [DOI] [PubMed] [Google Scholar]
- 7. Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: a prospective study. J Am Geriatr Soc. 2013;61:1629–1631. 10.1111/jgs.12428. [DOI] [PubMed] [Google Scholar]
- 8. Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults' annual fall risk: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69:1586–1594. 10.1093/gerona/glu087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pai YC, Yang F, Bhatt T, Wang E. Learning from laboratory-induced falling: long-term motor retention among older adults. Age (Dordr). 2014;36:9640. 10.1007/s11357-014-9640-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bhatt T, Espy D, Yang F, Pai YC. Dynamic gait stability, clinical correlates, and prognosis of falls among community-dwelling older adults. Arch Phys Med Rehabil. 2011;92:799–805. 10.1016/j.apmr.2010.12.032. [DOI] [PubMed] [Google Scholar]
- 11. Bhatt T, Yang F, Pai YC. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch Phys Med Rehabil. 2012;93:557–564. 10.1016/j.apmr.2011.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McCrum C, Essers JM, Jie LJ, Liu WY, Meijer K. Commentary: older adults can improve compensatory stepping with repeated postural perturbations. Front Aging Neurosci. 2016;8:111. 10.3389/fnagi.2016.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Studer M. Making balance automatic again: using dual tasking as an intervention in balance rehabilitation for older adults. SM Gerontol Geriatr Res. 2018;2:1–11. 10.36876/smggr.1015. [DOI] [Google Scholar]
- 14. Silsupadol P, Shumway-Cook A, Lugade V, et al. Effects of single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Arch Phys Med Rehabil. 2009;90:381–387. 10.1016/j.apmr.2008.09.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ghai S, Ghai I, Effenberg AO. Effects of dual tasks and dual-task training on postural stability: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:557–577. 10.2147/CIA.S125201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Silsupadol P, Lugade V, Shumway-Cook A, et al. Training-related changes in dual-task walking performance of elderly persons with balance impairment: a double-blind, randomized controlled trial. Gait Posture. 2009;29:634–639. 10.1016/j.gaitpost.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang Y, Wang S, Bolton R, Kaur T, Bhatt T. Effects of task-specific obstacle-induced trip-perturbation training: proactive and reactive adaptation to reduce fall-risk in community-dwelling older adults. Aging Clin Exp Res. 2020;32:893–905. 10.1007/s40520-019-01268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gerards MHG, McCrum C, Mansfield A, K. M.. Perturbation-based balance training for falls reduction among older adults: current evidence and implications for clinical practice. Geriatr Gerontol Int. 2017;17:2294–2303. 10.1111/ggi.13082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peeters GMEE, Deeg DJH, Elders PJM, Lips P. Snelle inschatting van de kans op herhaald vallen bij ouderen. Huisart Wet. 2011;54:186–191. 10.1007/s12445-011-0090-3. [DOI] [Google Scholar]
- 20. Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699. 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 21. Rieger MM, Papegaaij S, Steenbrink F, Dieën JH, Pijnappels M. Perturbation-based gait training to improve daily life gait stability in older adults at risk of falling: Protocol for the REACT randomized controlled trial. BMC Geriatr. 2020;20:167. 10.1186/s12877-020-01566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;2019:CD012424. 10.1002/14651858.CD012424.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schooten KS, Pijnappels M, Rispens SM, Elders P, Lips P, Dieen JH. Ambulatory fall-risk assessment: amount and quality of daily-life gait predict falls in older adults. J Gerontol A Biol Sci Med Sci. 2015;70:608–615. 10.1093/gerona/glu225. [DOI] [PubMed] [Google Scholar]
- 24. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 25. Schooten KS, Pijnappels M, Rispens SM, et al. Daily-life gait quality as predictor of falls in older people: a 1-year prospective cohort study. PLoS One. 2016;11:67. 10.1371/journal.pone.0158623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rispens SM, Schooten KS, Pijnappels M, Daffertshofer A, Beek PJ, Dieen JH. Do extreme values of daily-life gait characteristics provide more information about fall risk than median values? JMIR Res Protoc. 2015;4:e4. 10.2196/resprot.3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rispens SM, Schooten KS, Pijnappels M, Daffertshofer A, Beek PJ, Dieen JH. Identification of fall risk predictors in daily life measurements – gait characteristics’ reliability and association with self-reported fall history. Neurorehabil Neural Repair. 2015;29:54–61. 10.1177/1545968314532031. [DOI] [PubMed] [Google Scholar]
- 28. Van Ancum JM, Schooten KS, Jonkman NH, et al. Gait speed assessed by a 4-m walk test is not representative of daily-life gait speed in community-dwelling adults. Maturitas. 2019;121:28–34. 10.1016/j.maturitas.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 29. Ashman KM, Bird CM, Zepf SE. Detecting bimodality in astronomical datasets. Astron J. 1994;108:2348–2361. 10.1086/117248. [DOI] [Google Scholar]
- 30. Brodie MA, Coppens MJ, Ejupi A, et al. Comparison between clinical gait and daily-life gait assessments of fall risk in older people. Geriatr Gerontol Int. 2017;17:2274–2282. 10.1111/ggi.12979. [DOI] [PubMed] [Google Scholar]
- 31. Dijkstra B, Kamsma YP, Zijlstra W. Detection of gait and postures using a miniaturized triaxial accelerometer-based system: accuracy in patients with mild to moderate Parkinson's disease. Arch Phys Med Rehabil. 2010;91:1272–1277. 10.1016/j.apmr.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 32. Matthews CE, Ainsworth BE, Thompson RW, Bassett DR Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34:1376–1381. 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 33. Punt M, Bruijn SM, Port IG, Rooij IJM, Wittink H, Dieën JH. Does a perturbation based gait intervention enhance gait stability in fall prone stroke survivors? A pilot study. J Appl Biomech. 2019;35:173–181. 10.1123/jab.2017-0282. [DOI] [PubMed] [Google Scholar]
- 34. Schootemeijer S, Weijer RHA, Hoozemans MJM, Delbaere K, Pijnappels M, Schooten KS. Responsiveness of daily life gait quality characteristics over one year in older adults who experienced a fall or engaged in balance exercise. Sensors (Basel). 2022;23:101. 10.3390/s23010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Karamanidis K, Epro G, McCrum C, Konig M. Improving trip- and slip-resisting skills in older people: perturbation dose matters. Exerc Sport Sci Rev. 2020;48:40–47. 10.1249/JES.0000000000000210. [DOI] [PubMed] [Google Scholar]
- 36. Pang I, Okubo Y, Sturnieks D, Lord SR, Brodie MA. Detection of near falls using wearable devices: a systematic review. J Geriatr Phys Ther. 2019;42:48–56. 10.1519/JPT.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 37. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;15:CD007146. 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 38. Faber MJ, Bosscher RJ, Chin APMJ, Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87:885–896. 10.1016/j.apmr.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 39. Weerdesteyn V, Rijken H, Geurts AC, Smits-Engelsman BC, Mulder T, Duysens J. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology. 2006;52:131–141. 10.1159/000091822. [DOI] [PubMed] [Google Scholar]
- 40. Yang F, Wang TY, Pai YC. Reduced intensity in gait-slip training can still improve stability. J Biomech. 2014;47:2330–2338. 10.1016/j.jbiomech.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Liu X, Bhatt T, Pai YC. Intensity and generalization of treadmill slip training: high or low, progressive increase or decrease? J Biomech. 2016;49:135–140. 10.1016/j.jbiomech.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lee A, Bhatt T, Pai YC. Generalization of treadmill perturbation to overground slip during gait: effect of different perturbation distances on slip recovery. J Biomech. 2016;49:149–154. 10.1016/j.jbiomech.2015.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yang F, Cereceres P, Qiao M. Treadmill-based gait-slip training with reduced training volume could still prevent slip-related falls. Gait Posture. 2018;66:160–165. 10.1016/j.gaitpost.2018.08.029. [DOI] [PubMed] [Google Scholar]
- 44. Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37:122–147. 10.1037/0003-066X.37.2.122. [DOI] [Google Scholar]
- 45. Grabiner MD, Bareither ML, Gatts S, Marone J, Troy KL. Task-specific training reduces trip-related fall risk in women. Med Sci Sports Exerc. 2012;44:2410–2414. 10.1249/MSS.0b013e318268c89f. [DOI] [PubMed] [Google Scholar]
- 46. Wang Y, Bhatt T, Liu X, et al. Can treadmill-slip perturbation training reduce immediate risk of over-ground-slip induced fall among community-dwelling older adults? J Biomech. Feb 14 2019;84:58–66. 10.1016/j.jbiomech.2018.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bhatt T, Pai YC. Generalization of gait adaptation for fall prevention: from moveable platform to slippery floor. J Neurophysiol. 2009;101:948–957. 10.1152/jn.91004.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lee A, Bhatt T, Liu X, Wang Y, Pai YC. Can higher training practice dosage with treadmill slip-perturbation necessarily reduce risk of falls following overground slip? Gait Posture. 2018;61:387–392. 10.1016/j.gaitpost.2018.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Okubo Y, Sturnieks DL, Brodie MA, Duran L, Lord SR. Effect of reactive balance training involving repeated slips and trips on balance recovery among older adults: a blinded randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2019;74:1489–1496. 10.1093/gerona/glz021. [DOI] [PubMed] [Google Scholar]
- 50. Allin LJ, Brolinson PG, Beach BM, et al. Perturbation-based balance training targeting both slip- and trip-induced falls among older adults: a randomized controlled trial. BMC Geriatr. 2020;20:205. 10.1186/s12877-020-01605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McCrum C, Karamanidis K, Willems P, Zijlstra W, Meijer K. Retention, savings and interlimb transfer of reactive gait adaptations in humans following unexpected perturbations. Comm Biol. 2018;1:230. 10.1038/s42003-018-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26:261–268. 10.1093/ageing/26.4.261. [DOI] [PubMed] [Google Scholar]
- 53. Dorfman M, Herman T, Brozgol M, et al. Dual-task training on a treadmill to improve gait and cognitive function in elderly idiopathic fallers. J Neurol Phys Ther. 2014;38:246–253. 10.1097/NPT.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 54. Lurie JD, Zagaria AB, Pidgeon DM, Forman JL, Spratt KF. Pilot comparative effectiveness study of surface perturbation treadmill training to prevent falls in older adults. BMC Geriatr. 2013;13:49. 10.1186/1471-2318-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Individual participant data presented in the figures are available upon request.