Abstract
Background:
Traditionally, the use of a pneumatic arterial tourniquet was requisite for safe and effective surgery of the hand. The use of arterial tourniquets necessitates the use of regional or general anaesthesia. Wide-awake local anaesthetic no tourniquet (WALANT) has emerged as a novel technique to overcome the limitations of tourniquet use in conjunction with regional/general anaesthesia. This review aimed to examine the safety and effectiveness of WALANT and provide guidance for surgeons with limited WALANT experience.
Methods:
A literature review of MEDLINE was performed up to March 2021 to identify all articles related to the use of WALANT in hand surgery. Any article reporting original data related to the use of WALANT was eligible for inclusion.
Results:
A total of 101 articles were identified through database searching. Of these, 79 met full inclusion criteria and described the use of WALANT in 19 elective and trauma procedures. Current data suggest that WALANT is safe and effective for use in a range of procedures.
Conclusions:
WALANT surgery is increasing in popularity as evidenced by the variety of surgical indications reported in the literature. There is limited comparative data on the cost-effectiveness of WALANT compared to conventional methods. Current data suggest that WALANT is safe, better tolerated by patients and associated with direct and indirect cost savings.
Takeaways
Question: What should a hand and wrist surgeon incorporating wide awake local anesthetic no tourniquet (WALANT) into their practice for the first time know?
Findings: Literature review consistently shows that use of adrenaline in the hand and digits is safe. WALANT is a well-tolerated method of anesthesia and can produce surgical conditions comparable to tourniquet use. WALANT is effective for the gamut of elective and traumatic, bony and soft tissue pathologies. Adoption can lead to considerable cost savings and provide an opportunity to redesign patient pathways to be more time efficient and environmentally friendly.
Meaning: WALANT is a safe, effective, efficient, versatile, and environmentally friendly way to operate on the hand and digit.
INTRODUCTION
Traditional hand surgery requires pneumatic arterial tourniquets (AT) to maintain a bloodless field and improve visibility. However, extended tourniquet usage can lead to severe pain, requiring mitigation with either general or regional anesthetic. The wide awake local anesthetic no tourniquet (WALANT) technique can negate this issue by infiltrating an adrenaline-containing local anesthetic (ACLA) into the operative field. Historically, infiltration of adrenaline into an extremity has been discouraged1 due to the risk of ischemic necrosis in areas perfused by end arteries. Now, there is strong evidence to suggest WALANT is a safe technique and a favorable method of anesthesia for hand surgery. However, the uptake of WALANT remains slow.1 The aim of this review is to explore the indications for WALANT in hand surgery and outline the benefits of this technique. The barriers to WALANT uptake will be discussed along with practical guidance on how to overcome these.
METHODOLOGY
A search of the PubMed database for all publications in the English language up to March 1, 2021 was performed with the Medical Subject Heading “WALANT.” In addition, all eligible studies’ reference lists were reviewed to include articles that add to the understanding of WALANT. Full-text review was performed for all selected articles.
Inclusion Criteria
All studies assessing the use of WALANT in hand surgery were included. In particular, literature on the WALANT indications, the financial benefits of the procedure including direct cost, efficiency, and resource savings, patient benefits, and the disadvantages of the technique were analyzed.
Exclusion Criteria
Abstracts and presentations without full text, reviews not adding new data or insight, papers not published in English language, anatomical locations outside the hand or wrist, and responses to full articles that did not add materially to the literature were excluded.
RESULTS
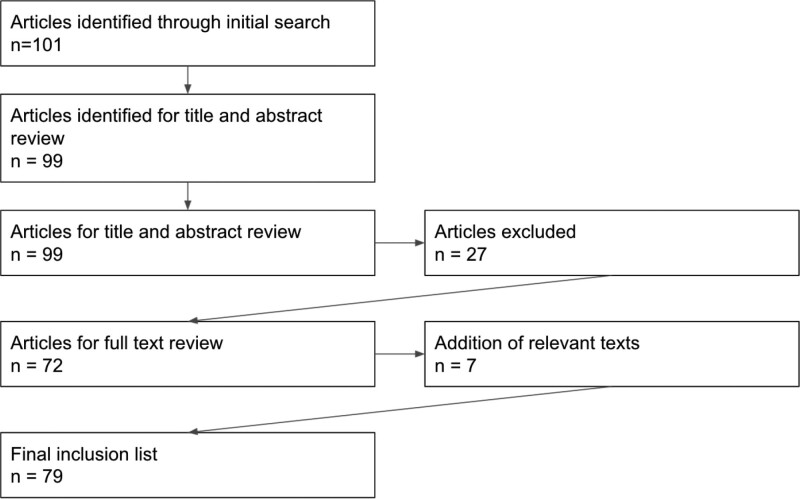
The literature search identified 101 articles, of which 99 were available for title and abstract review. In total, 27 articles were excluded as per the above criteria. Following a full-text review of the remaining articles and addition of suitable references, 79 articles were finally included (Fig. 1).
Fig. 1.
Study selection and inclusion flowchart.
The Need for WALANT: AT Complications
Tourniquet pain is the limiting factor in AT use, patients will tolerate discomfort for 18 minutes and 25 minutes on the arm and forearm, respectively.2 This window of time is often insufficient for complex cases, dealing with unexpected intraoperative findings and for delivering training.3
Infrequently, prolonged tourniquet pressure can lead to nerve injury, ranging from paraesthesia to complete paralysis.4 Other complications include reperfusion injury, friction, and chemical burns.5–7
Adrenaline Safety in the Hand
The occurrence of ischemic necrosis from infiltrating adrenaline around end arteries has consistently been shown to be vanishingly rare.8 In 2001, Denkler9 found sporadic reports of finger necrosis. However, all of these occurred before 1948, when commercial lidocaine-adrenaline mixes were unavailable. Only 48 cases were reported between 1880 and 2000, with the majority occurring before 1950 and only 21 of which involved injection of adrenaline.10 Krunic11 later in 2004 also concluded that there were no reports of digital ischemia associated with the use of commercially available lidocaine-adrenaline mixes. Later, in 2007, Thompson12 reported that cases of digital ischemia in the early 20th century were likely due to cocaine and procaine, commonly used at the time. These agents are now known to degenerate overtime and when improperly stored, can cause severe tissue acidosis.13 This was likely the cause of digital necrosis rather than adrenaline-mediated vasoconstriction. More recently, it has been shown that injections of 1:200,000 adrenaline into the fingers of 17 patients did not cause critical hypoperfusion to the fingertip.14
Fitzcharles-Bowe identified 57 patients who underwent 1:1000 adrenaline injections into the hand. No patient had irreversible ischemic necrosis; however, 13 required treatment with phentolamine15 (reversal agent for adrenaline-mediated vasoconstriction16), which takes approximately 85 min to restore bloodflow.17 It is widely accepted that all surgeons using WALANT should possess working knowledge of phentolamine,18 a view our team agrees with. Systemic complications associated with WALANT are rare. Although some cite the theoretical risk of cardiac complications, a study of 51 patients undergoing WALANT found no statistical difference in incidence of arrhythmia between those in the WALANT group and those in the local anesthetic/tourniquet (LA/TQ) group.19
Composition of WALANT: ACLA Solutions
A range of ACLA solutions have been described, most containing lidocaine with a low-dose adrenaline.20 Lalonde originally described a mix of 1% lidocaine with 1:100,000 adrenaline, with a maximum dose of 7 mg per kg of lidocaine.21 Others add 8.4% sodium bicarbonate to alleviate some of the discomfort associated with acidity of local anesthetics.22 Some have modified the concentration of lidocaine for more practical reasons: for example, surgeons in Preston use 1.8% lidocaine mixture, which can be easier to reconstitute with the available solutions in the UK.23 Some have described diluting their mixtures with saline to achieve an adrenaline concentration of 1:400,000, especially in cases requiring larger volumes of infiltrate.24 Lalonde now recommends a solution of 0.5% bupivacaine with 1:200,000 adrenaline for procedures lasting longer than 2 hours, reducing the need for intraoperative ACLA injections.18
Concerns with WALANT: Is It Effective in Creating a Bloodless Field?
Some question WALANT’s vasoconstrictive ability and its impact on surgical efficiency and safety, partly explaining its slow uptake amongst surgeons. The absence of a completely bloodless operative field, otherwise afforded by a tourniquet, is generally accepted with WALANT.25 Gunasagaran has shown no significant difference in estimated blood loss or operative time between WALANT and LA/TQ-based anesthetics.26 Others have found that WALANT provided a better surgical field than a tourniquet for trigger finger release (TFR) amongst 86 patients.27
Efficient surgery under WALANT requires adequate time for adrenaline to produce vasoconstriction. Some quote 26 minutes from injection to optimal visibility.28 In contrast, others suggest there is no difference in waiting 7 minutes versus 30 minutes after injection,29 whereas others still found “good enough” visibility was achieved in between 5 and 15 minutes.30 A balance between surgical efficiency and waiting for optimum vasoconstriction is required, requiring each surgeon to personalize their practice. Novice surgeons or those with limited experience of WALANT may require a period of familiarization—anatomy may be distorted, and the operative field may be wet with ACLA and/or blood. The current literature indicates that for those experienced with WALANT, there is minimal or no difference in operating time, safety, and outcomes in comparison with traditional methods.
INDICATIONS FOR WALANT
Many hand and wrist procedures can be performed under WALANT (Table 1).
Table 1.
Published Indications for WALANT SURGERY
| Location | Indication | Author(s) |
|---|---|---|
| Digit | Phalangeal fracture | Tang,30 Khor31 |
| Flexor tendon repair/transfer | Gueffier,32 Mohammed,33 Woo,34 Tang,30 Khor31 | |
| Extensor tendon repair/transfer | Miyashima,35 Abdullah,24 Mohammed,33 Woo,34 Tang,30 Khor31 | |
| Digital nerve | Sawhney,36 Tang,30 Khor31 | |
| Trigger finger | Mohd,27 Maliha,37 Gunasagaran,26 Hernandez,29 Codding,38 Ki Lee,39 Shulman,3 Rhee,40 Tang,30 Burn41 | |
| Digital revascularization | Wong,42 Khor31 | |
| Digital replantation | Wong,42 Khor31 | |
| Skin flap | Xu43 | |
| Palm | Metacarpal fracture | Feldman,44 Tang30 |
| Ganglion excision | Gunasagaran26 | |
| Wrist | Carpal tunnel release | Tulipan,45 Sraj,46 Kang,47 Via,48 Chapman,49 Kazmers,50 Gunasagaran,26 Hernandez,29 Ki Lee,39 Shulman,3 Rhee,51 Mckee |
| First dorsal compartment release | Ki Lee,39 Shulman,3 Rhee40 | |
| Wrist arthroscopy | Liu52 | |
| Trapiezectomy/carpal prosthesis | Müller53 | |
| Distal radius fracture | Huang,54 Ahmad,55 Tahir56 | |
| Miscellaneous | Mass excision | Shulman3 |
| Local debridement | Tang30 | |
| Foreign body removal | Tang30 |
Hand Trauma Surgery
A unique benefit of WALANT is the ability to conduct intraoperative assessments of repairs.24,35 Currently, intraoperative assessment of flexor tendon repair is limited to subjective means, highly dependent on operator skill and experience.35 With a patient unable to perform active movements under regional or general anesthesia, it is difficult to accurately assess tendon gapping, bunching and glide, and their effect on the need for venting of pulleys, which may affect overall function.57 Excessive pulley venting may lead to tendon bowstringing, whereas under-venting may result in reduced glide. Higgins reported a flexor tendon rupture rate of 3.3% through intraoperative assessments to identify and correct gapping or bunching.34 Woo identified this as a significant advantage of WALANT, allowing the operator to confidently achieve optimal glide and tension before closure.43
Revascularization and replantation of amputated digits have also successfully been undertaken using WALANT. A study encompassing five digital revascularizations and eight finger replantations demonstrated good functional outcomes under this technique.32 However, a temporary digital tourniquet was initially required in three cases to safely identify anatomical structures.32
No specific literature on the outcomes of nerve repair under WALANT was found. However, our group has previously published on the high rate of patient satisfaction with WALANT in the context of hand trauma, including those undergoing digital neurosynthesis.36 The senior author would, however, caution against undertaking surgery for nerve injury proximal to the wrist, as it is often poorly tolerated by patients.
Fixation of bony injuries under WALANT is well documented.30,44 In a study of 25 patients undergoing metacarpal fracture fixation, positive outcomes (including no loss of reduction, inadequate fixation, malrotation, screw migration, or infection) were achieved.20 Dynamic intraoperative assessment allows for identification of impingement or improper tendon glide over metalwork, as well as assessment of range of motion, and provides the opportunity for patient education about postoperative care.54 Distal radius fracture fixation can also be performed under WALANT with good outcomes.54,55 WALANT expedites surgery by avoiding extensive preoperative workup in older and/or co-morbid patients presenting with distal radius fracture.56
Elective Hand Surgery
Elective hand procedures such as carpal tunnel release (CTR)30,50 and TFR30 (Table 1) can be performed under WALANT. Ki Lee reported significantly reduced postoperative pain within 24 hours after de Quervain’s tenosynovitis (DQT) release and achieved high patient satisfaction.39 Mohammed reported a series of tendon transfers for leprosy patients under WALANT, providing treatment at significantly reduced cost to a disadvantaged population in India.33 Trapeziometacarpal joint arthroplasties (TMJA) performed under WALANT have been associated with higher patient satisfaction rates compared to general anesthetic/tourniquet.53,58 Liu reported the use of ACLA in wide awake wrist arthroscopy, citing the key advantage of intraoperative “grip and release” kinetic testing, particularly beneficial in the dynamic assessment of carpal instability.52
Although there is a paucity of high-quality randomized controlled evidence to demonstrate an improvement in functional outcome in elective WALANT-based surgery, there is no evidence to suggest inferiority. A meta-analysis of published data sought to compare outcomes of hand surgeries using WALANT versus intravenous, regional or local anesthesia with tourniquet and found no statistical difference in complication rates.59 Several other studies have found no difference in operative time between WALANT and LA/TQ groups in CTR, TFR, and DQT release or TMJA.39,58 One study did find that WALANT resulted in a significant reduction in postoperative pain.59 Tulipan compared outcomes of CTR under WALANT versus LA/TQ with sedation and found no difference between the groups in postoperative disability, intraoperative pain scores, time to return to work or satisfaction with their method of anesthesia.45 Sraj reported outcomes of CTR using plain lidocaine versus WALANT and noted an increase in mean operative time of 36% in the plain lidocaine group, thereby highlighting the importance of the vasoconstrictive effect of adrenaline.46
NONOPERATIVE BENEFITS OF WALANT
Cost Savings
WALANT minimizes the need for anesthetic staff and associated cost of machinery, along with the requirement for operating theaters. Many hand procedures can be performed safely in minor procedure rooms.37 Rhee reported an average saving of approximately 85% per procedure, and Kazmers, an 11-fold saving by performing CTRs in a clinic setting under WALANT.40,50 Van-Demark combined WALANT with minor field sterility to decrease surgical wastage and reduce costs. Amongst 1099 cases, $12,350.32 was saved and 2.8 tonnes of waste reduced.60 Burns modified their TFR surgery pathway by switching from IV sedation to WALANT administered in the preoperative holding room rather than the operating theater. They found an 18% reduction in cost and an overall reduction in treatment time of 41 minutes per patient.41 Despite clear reductions in cost, the complex nature of clinician reimbursement, particularly in the US, may reduce the monetary benefit for providers.
In the UK, WALANT has enabled a “one stop wide awake” pathway for a variety hand procedures, resulting in a saving of approximately 25%–50% of the national tariff price and a total saving of £750,000 per 1000 cases,61 in addition to a reduction of between 30%–45% of theater time. Codding ran a cost analysis showing patients undergoing WALANT spent less time in operating theaters, had shorter operating times, and had speedier postoperative recovery, resulting in financial and other resource savings.38,62 Wheelcock suggests that direct savings accrue to patients too.63 Costs and inconvenience shouldered by patients traveling from rural areas to regional centers are not insignificant; they often need to purchase accommodation or stay overnight following general anesthetic.63 Specialist hand surgery services are often centralized to regional university teaching hospitals, known as the hub and spoke model of healthcare. We hypothesize that WALANT, coupled with the concept of limited field sterility, could allow the surgeon to overcome this issue by delivering treatment directly in the community.60,61,64
Remote working through video conferencing is now possible as a result of the COVID-19 pandemic. In this way, pre- and post-surgical care can be easily delivered to patients. As such, an outreach program can be developed in which patient care is expanded further, local resources utilized, and the financial burden reduced for patients and the healthcare system.
Resource Efficiency
An advantage of WALANT is its utilization in under-resourced environments. During the COVID-19 pandemic, healthcare systems struggled to balance the demand for anesthetists, surgical staff, ventilators and recovery beds with the need to provide elective procedures.65 This has resulted in increased WALANT surgery uptake through efficiently re-designed treatment pathways. Assessment and operative intervention can occur simultaneously, with minimal staff and equipment requirements66 and no increase in complications.64 The British Society for Surgery of the Hand (BSSH) and British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS) provided guidance that all hand injuries be operated on under WALANT to limit patient footfall within hospitals related to general anesthesia requirements.67 WALANT facilitated “one-stop” clinics are likely to become the new normal31 with educators calling for its incorporation into the plastic surgery training curriculum.68
Rhee highlighted the invaluable utility of WALANT in conflict zones. Austere environments have limited access to anesthetic personnel or equipment. Procedures such as phalangeal and metacarpal fracture fixation, tendon repairs, digital revascularisation and replantation can be performed under WALANT, conserving finite military resources.32,51 WALANT reduces the need for unnecessary preoperative investigations, which can be costly, lengthy and delay time to operation. One study comparing WALANT to LA/TQ with sedation found that those in the WALANT group spent around 50% less time in postoperative recovery.69 In addition, 48% of those given LA/TQ + sedation required preoperative investigations including ECGs, blood tests and chest imaging, while only 3% of the WALANT group did.
WALANT surgery minimizes the need for recovery bed, unnecessary perioperative investigations and systemic anesthetic care requirements.51,69 Lastly, WALANT provides a safe method of operating on complex patients whose co-morbidities would otherwise be a contraindication to general anesthetic.54,70 The risks of serious postoperative complications associated with general anesthetic such as respiratory failure, infection, and venous thromboembolism are significantly reduced.71
Patient Experience
Electively, WALANT has been shown to be comfortable method of anesthesia that is welcomed by patients. A study involving 100 patients undergoing elective hand procedures under ACLA were asked to rate their postoperative levels of anxiety and pain on a visual analogue scale. The authors found that 91% of their respondents rated their intraoperative pain and anxiety as 2 of 10 or less, and 3 of 10 or less, respectively. Additionally, 86% stated they would undergo WALANT surgery again.72 Similarly, Van-Demark reported high satisfaction ratings amongst his cohort of 111 patients, with 95% relating their experience dentist visit or better, 99% willing to repeat their experience under WALANT again, and 99% willing to recommend it to others.64 Gunasagaran compared the effect of WALANT with the traditional LA/TQ method on patient comfort during ganglion excision, CTR, and TFR surgery.26 They reported patients found WALANT more comfortable and preferable with mean visual analogue scale scores of 2.33 and 4.72 (P < 0.05), respectively.26 Nikkhah also found that their patients experienced less pain during CTR with WALANT.73 However, other researchers have shown no significant difference between the two techniques.48 In the context of trauma, our team has shown WALANT to be effective, with patient reported comfort similar to the elective setting.36 WALANT can also improve comfort during the perioperative period. There is no requirement for preoperative fasting or postoperative carer support after general anesthetic.74 Equally, postoperative nausea and vomiting, which can affect around 30% of patients can also be avoided.75 Lastly the analgesic effects of WALANT can prevent the need for postoperative opioid analgesics, reducing possible dependency on these narcotic agents.47,49,76
CONSIDERATIONS FOR NEW WALANT PRACTITIONERS
Contraindications
ACLAs should not be injected into patients with a documented allergy or into the hands of those with a previous arterial injury or a known vascular insufficiency.77 Local anesthetic is also known to be less effective in tissues with active infection. Injecting ACLA can be challenging in pediatric, anxious or non-compliant patients. For patients with cardiac disease, the adrenaline concentration can be diluted down to 1:400,000.77 Operating time under WALANT is limited by duration of anesthesia, vasoconstriction, and patient comfort. The former two factors can be extended by intraoperative “top-up” injections of ACLA. To address patient comfort, case selection is key; the authors limit WALANT to a maximum of 2 hours of expected operating time and do not offer this to patients who indicate high levels of anxiety about awake surgery.78 In addition, there is a theoretical risk of inducing sickling in patients with sickle cell disease; however, no data are available to guide the practitioner in such cases.79 Lastly, the operator should be prepared for the unlikely event of failure of anesthesia, which may require abandonment of procedure or conversion to traditional anesthetic techniques; there is, however, no literature on incidence of such events.
Misconceptions around WALANT Use
The most notable barrier to uptake of WALANT is the perception that injecting adrenaline into the extremity will cause ischemic necrosis. However, there is now ample literature, including those with large patient cohorts8,80 much of which has been discussed in earlier sections of this paper, to show these concerns are without merit. Digital necrosis has now largely been attributed to the historic use of procaine rather than the effects of adrenaline.12,13 Appropriate surgeon education can help overcome this taboo. With the rising popularity of WALANT, it is vital that its safety profile is discussed more amongst colleagues.
A second barrier is the efficacy of adrenaline in achieving a safe and bloodless operating field, especially in procedures with minimal working space such as CTR or TFR. As has been highlighted in this review, sufficient data exists to show that WALANT affords a satisfactory operating field, with no significant effect on operating time, blood loss or complications. The caveat to this is that the surgeon must allow sufficient time for the ACLA to “cook,” or produce its hemostatic effect. This requires the surgeon to adapt their management of operating lists and operating theater efficiency. We would advise that the surgeon, or a competent assistant, inject the ACLA in a holding room before or during the preceding case to help manage patient flow in the operating room.
A third barrier is operator unfamiliarity with the wide spectrum of hand procedures that can be performed safely under WALANT in both the trauma and elective settings (Table 1). Historical dogma and relatively recent adoption of ACLA in the hand may hinder its routine uptake over traditional methods; however, this review provides strong evidence for its safety, efficacy, versatility, cost effectiveness and patient satisfaction to overcome this. These advantages should be communicated through further research, conference presentations, and colleague discussions. Ultimately, this benefits all stakeholders including patients, surgeons, and healthcare systems.
CONCLUSIONS
WALANT is increasing in popularity following the acceptance of the safety of adrenaline in the extremity. Our review clearly outlines the benefits of this technique with regard to expedited and safe patient care, cost saving, resource allocation, and intraoperative assessment compared with conventional techniques. In the current international climate of spiraling healthcare costs and finite resources, WALANT provides an excellent opportunity to redesign and optimize surgical pathways toward providing safe and efficient surgery in the hand and wrist. We believe our review provides clear precedence for utilizing WALANT and hope it will inform surgeons beginning their practice with it.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 22 January 2024.
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Deutsch CJ, Jones K, Dassayanake S, et al. Concern about ischaemia drives a persistent and generation-spanning aversion to adrenaline in digital anaesthesia. JPRAS Open. 2021;28:61–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maury AC, Roy WS. A prospective, randomized, controlled trial of forearm versus upper arm tourniquet tolerance. J Hand Surg. 2002;27:359–360. [DOI] [PubMed] [Google Scholar]
- 3.Shulman BS, Rettig M, Yang SS, et al. Tourniquet use for short hand surgery procedures done under local anesthesia without epinephrine. J Hand Surg. 2020;45:554.e1–554.e6. [DOI] [PubMed] [Google Scholar]
- 4.Noordin S, McEwen JA, Kragh JF, et al. Surgical tourniquets in orthopaedics. J Bone Joint Surg. 2009;91:2958–2967. [DOI] [PubMed] [Google Scholar]
- 5.Oragui E, Parsons A, White T, et al. Tourniquet use in upper limb surgery. Hand. 2011;6:165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choudhary S, Koshy C, Ahmed J, et al. Friction burns to thigh caused by tourniquet. Br J Plast Surg. 1998;51:142–143. [DOI] [PubMed] [Google Scholar]
- 7.Dickinson JC, Bailey BN. Chemical burns beneath tourniquets. BMJ. 1988;297:1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lalonde D, Bell M, Benoit P, et al. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie project clinical phase. J Hand Surg. 2005;30:1061–1067. [DOI] [PubMed] [Google Scholar]
- 9.Denkler K. A comprehensive review of epinephrine in the finger: to do or not to do. Plast Reconstr Surg. 2001;108:114–124. [DOI] [PubMed] [Google Scholar]
- 10.Lalonde DH. Conceptual origins, current practice, and views of wide awake hand surgery. J Hand Surg. 2017;42:886–895. [DOI] [PubMed] [Google Scholar]
- 11.Krunic AL, Wang LC, Soltani K, et al. Digital anesthesia with epinephrine: an old myth revisited. J Am Acad Dermatol. 2004;51:755–759. [DOI] [PubMed] [Google Scholar]
- 12.Thomson CJ, Lalonde DH, Denkler KA, et al. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119:260–266. [DOI] [PubMed] [Google Scholar]
- 13.Pires Neto PJ, Moreira LA, Las Casas PP. Is it safe to use local anesthesia with adrenaline in hand surgery? WALANT technique. Revista Brasileira de Ortopedia. 2017;52:383–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moog P, Dozan M, Betzl J, et al. WALANT–epinephrine injection may lead to short term, reversible episodes of critical oxygen saturation in the fingertips. Arch Orthop Trauma Surg. 2021;141:527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fitzcharles-Bowe C, Denkler K, Lalonde D. Finger injection with high-dose (1:1,000) epinephrine: does it cause finger necrosis and should it be treated? Hand. 2007;2:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walsh K, Baker BG, Iyer S. Adrenaline Auto-injector injuries to digits; a systematic review and recommendations for emergency management. Surgeon. 2020;18 :305–310. [DOI] [PubMed] [Google Scholar]
- 17.Nodwell T, Lalonde D. How long does it take phentolamine to reverse adrenaline-induced vasoconstriction in the finger and hand? A prospective, randomized, blinded study: the dalhousie project experimental phase. Canadian J Plastic Surg. 2003;11:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lalonde D. Minimally invasive anesthesia in wide awake hand surgery. Hand Clin. 2014;30:1–6. [DOI] [PubMed] [Google Scholar]
- 19.Farkash U, Herman A, Kalimian T, et al. Keeping the finger on the pulse: cardiac arrhythmias in hand surgery using local anesthesia with adrenaline. Plast Reconstr Surg. 2020;146:54e–60e. [DOI] [PubMed] [Google Scholar]
- 20.Poggetti A, Nucci A, Giesen T, et al. Percutaneous intramedullary headless screw fixation and wide-awake anesthesia to treat metacarpal fractures: early results in 25 patients. J Hand Microsurg. 2018;10:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lalonde D, Martin A. Epinephrine in local anesthesia in finger and hand surgery: The case for wide-awake anesthesia. J Am Acad Orthopaedic Surgeons. 2013;21:443–447. [DOI] [PubMed] [Google Scholar]
- 22.Cepeda MS, Tzortzopoulou A, Thackrey M, et al. Adjusting the pH of lidocaine for reducing pain on injection. In: Cochrane Database of Systematic Reviews. 02010:CD006581. [DOI] [PubMed] [Google Scholar]
- 23.Amin KR, Al-Hamdi A, Chen JHC, et al. An alternative solution in wide-awake surgery: The Preston WALANT mixture. J Hand Microsurg. 2021;13:119–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abdullah S, Ahmad AA, Lalonde D. Wide awake local anesthesia no tourniquet forearm triple tendon transfer in radial nerve palsy. Plast Reconstr Surg Glob Open. 2020;8:e3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castro Magtoto IJ, Alagar DL. Wide awake local anesthesia no tourniquet: a pilot Study for carpal tunnel release in the Philippine Orthopedic Center. J Hand Surg. 2019;24:389–391. [DOI] [PubMed] [Google Scholar]
- 26.Gunasagaran J, Sean ES, Shivdas S, et al. Perceived comfort during minor hand surgeries with wide awake local anaesthesia no tourniquet (WALANT) versus local anaesthesia (LA)/tourniquet. J Orthopaedic Surg. 2017;25:2309499017739499. [DOI] [PubMed] [Google Scholar]
- 27.Rashid MZM, Sapuan J, Abdullah S. A randomized controlled trial of trigger finger release under digital anesthesia with (WALANT) and without adrenaline. J Orthopaedic Surg. 2019;27:2309499019833002. [DOI] [PubMed] [Google Scholar]
- 28.Mckee DE, Lalonde DH, Thoma A, et al. Achieving the optimal epinephrine effect in wide awake hand surgery using local anesthesia without a tourniquet. Hand. 2015;10:613–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hernandez A, Rosario M, Mendoza-Torres R, et al. Evaluating clinical outcomes for determining the optimal delay to skin incision under WALANT: a prospective series of 34 patients from a low-resource tertiary setting. Adv Orthop. 2020;2020:9351354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tang JB, Gong KT, Xing SG, et al. Wide-awake hand surgery in two centers in china: experience in nantong and tianjin with 12,000 patients. Hand Clin. 2019;35:7–12. [DOI] [PubMed] [Google Scholar]
- 31.Khor WS, Lazenby DJ, Campbell T, et al. Reorganisation to a local anaesthetic trauma service improves time to treatment during the COVID-19 pandemic—experience from a UK tertiary plastic surgery centre. J Plast, Reconstr Aesthet Surg. 2021;74:890–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gueffier X, Lalonde D, Ahmad AA. Flexor pollicis longus zone 2 tendon repair under WALANT with ultrasound assistance. Trauma Case Rep. 2021;32:100446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohammed AK, Lalonde DH. Wide awake tendon transfers in leprosy patients in India. Hand Clin. 2019;35:67–84. [DOI] [PubMed] [Google Scholar]
- 34.Woo SH, Yoo MJ, Ahn HC. Lessons learned in the authors’ first years of wide-awake hand surgery at the W Hospital in Korea. Hand Clin. 2019;35:59–66. [DOI] [PubMed] [Google Scholar]
- 35.Miyashima Y, Uemura T, Yokoi T, et al. Traumatic index extensor tendon attenuation mimicking closed tendon rupture: two case reports. BMC Musculoskelet Disord. 2020;21:672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sawhney A, Thacoor A, Akhavani M. Wide awake local anaesthetic no tourniquet (WALANT) technique in hand trauma surgery: a prospective study of efficacy and peri-operative patient experience. J Plastic, Reconstr Aesthet Surg. 2021;74:2392–2442. [DOI] [PubMed] [Google Scholar]
- 37.Maliha SG, Cohen O, Jacoby A, et al. A Cost and efficiency analysis of the walant technique for the management of trigger finger in a procedure room of a major city hospital. Plast Reconstr Surg Glob Open. 2019;7:e2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Codding JL, Bhat SB, Ilyas AM. An economic analysis of MAC versus WALANT: a trigger finger release surgery case study. Hand. 2017;12:348–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ki Lee S, Gul Kim S, Sik Choy W. A randomized controlled trial of minor hand surgeries comparing wide awake local anesthesia no tourniquet and local anesthesia with tourniquet. Orthopaedics Traumatol Surg Research. 2020;106:1645–1651. [DOI] [PubMed] [Google Scholar]
- 40.Rhee PC, Fischer MM, Rhee LS, et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg. 2017;42:e139–e147. [DOI] [PubMed] [Google Scholar]
- 41.Burn MB, Shapiro LM, Eppler SL, et al. Clinical care redesign to improve value for trigger finger release: a before-and-after quality improvement study. Hand. 2019;16:624–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wong JKF, Lin CH, Chang NJ, et al. Digital revascularization and replantation using the wide-awake hand surgery technique. J Hand Surg. 2017;42:621–625. [DOI] [PubMed] [Google Scholar]
- 43.Xu J, Yin L, Cao S, et al. Application of WALANT technique for repairing finger skin defect with a random skin flap. J Orthop Surg Res. 2021;16:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feldman G, Orbach H, Rinat B, et al. Internal fixation of metacarpal fractures using wide awake local anesthesia and no tourniquet. Hand Surg Rehabil. 2020;39:214–217. [DOI] [PubMed] [Google Scholar]
- 45.Tulipan J, Kim N, Abboudi J, et al. Open carpal tunnel release outcomes: performed wide awake versus with sedation. J Hand Microsurg. 2017;09:074–079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sraj S. Carpal tunnel release with wide awake local anesthesia and no tourniquet: with versus without epinephrine. Hand. 2021;16:592–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kang SW, Park HM, Park JK, et al. Open cubital and carpal tunnel release using wideawake technique: reduction of postoperative pain. J Pain Res. 2019;12:2725–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Via GG, Esterle AR, Awan HM, et al. Comparison of local-only anesthesia versus sedation in patients undergoing staged bilateral carpal tunnel release: a randomized trial. Hand. 2020;15:785–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chapman T, Kim N, Maltenfort M, et al. Prospective evaluation of opioid consumption following carpal tunnel release surgery. Hand. 2017;12:39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kazmers NH, Presson A, Xu Y, et al. Cost implications of varying the surgical technique, surgical setting, and anesthesia type for carpal tunnel release surgery HHS public access. J Hand Surg Am. 2018;43:971–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rhee PC. The current and possible future role of wide-awake local anesthesia no tourniquet hand surgery in military health care delivery. Hand Clin. 2019;35:13–19. [DOI] [PubMed] [Google Scholar]
- 52.Liu B, Ng CY, Arshad MS, et al. Wide-awake wrist and small joints arthroscopy of the hand. Hand Clin. 2019;35:85–92. [DOI] [PubMed] [Google Scholar]
- 53.Müller CT, Christen T, Heidekruger PI, et al. Wide-awake anesthesia no tourniquet trapeziometacarpal joint prosthesis implantation. Plast Reconstr Surg Glob Open. 2018;6:e1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang YC, Hsu C-J, Renn J-H, et al. WALANT for distal radius fracture: open reduction with plating fixation via wide-awake local anesthesia with no tourniquet. J Orthop Surg Res. 2018;13:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ahmad AA, Yi LM, Ahmad AR. Plating of distal radius fracture using the wide-awake anesthesia technique. J Hand Surg. 2018;43:1045.e1–1045.e5. [DOI] [PubMed] [Google Scholar]
- 56.Tahir M, Chaudhry EA, Zaffar Z, et al. Fixation of distal radius fractures using wide-awake local anaesthesia with no tourniquet (WALANT) technique: A randomized control trial of a cost-effective and resource-friendly procedure. Bone Joint Res. 2020;9:429. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 57.Higgins A, Lalonde DH, Bell M, et al. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. 2010;126:941–945. [DOI] [PubMed] [Google Scholar]
- 58.Larsen LP, Hansen TB. Total trapeziometacarpal joint arthroplasty using wide awake local anaesthetic no tourniquet. J Hand Surg. Eur. 2020;46:125–130. [DOI] [PubMed] [Google Scholar]
- 59.Evangelista TMP, Pua JHC, Evangelista-Huber MTP. Wide-awake local anesthesia no tourniquet (WALANT) versus local or intravenous regional anesthesia with tourniquet in atraumatic hand cases in orthopedics: a systematic review and meta-analysis. J Hand Surg Asian Pac. 2019;24:469–476. [DOI] [PubMed] [Google Scholar]
- 60.Van Demark RE, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg. 2018;43:179–181. [DOI] [PubMed] [Google Scholar]
- 61.Bismil M, Bismil Q, Harding D, et al. Transition to total one-stop wide-awake hand surgery service-audit: a retrospective review. JRSM Short Reports. 2012;3:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kamal RN, Behal R. Clinical care redesign to improve value in carpal tunnel syndrome: a before-and-after implementation study. J Hand Surg. 2019;44:1–8. [DOI] [PubMed] [Google Scholar]
- 63.Wheelock M, Petropolis C, Lalonde DH. The Canadian model for instituting wide-awake hand surgery in our hospitals. Hand Clin. 2019;35:21–27. [DOI] [PubMed] [Google Scholar]
- 64.Van Demark RE, Becker HA, Anderson MC, et al. Wide-awake anesthesia in the in-office procedure room: lessons learned. Hand. 2018;13:481–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Turcotte JJ, Petre BM, Jones CM, et al. Maintaining access to orthopaedic surgery during periods of operating room resource constraint: expanded use of wide-awake surgery during the COVID-19 pandemic. J Am Acad Orthop Surg Glob Res Rev. 2020;4:e20.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hobday D, Welman T, O’Neill N, et al. A protocol for wide awake local anaesthetic no tourniquet (WALANT) hand surgery in the context of the coronavirus disease 2019 (COVID-19) pandemic. Surgeon. 2020;18:e67–e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.British Orthopaedic Association, British Association of Plastic Reconstructive and Aesthetic Surgeons & The British Society for Surgery of the Hand. Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at https://www.boa.ac.uk/latest-news/specialty-and-subspecialty-guidance-and-resources.html. Published January 2021. Accessed November 29, 2023.
- 68.Thakkar M, Bednarz B. Should WALANT surgery be included in the training curriculum? J Plastic, Reconstr Aesthet Surg. 2020;73:1575–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Davison PG, Cobb T, Lalonde DH. The patient’s perspective on carpal tunnel surgery related to the type of anesthesia: A prospective cohort study. Hand. 2013;8:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abd Hamid MH, Abdullah S, Ahmad AA, et al. A randomized controlled trial comparing wide-awake local anesthesia with no tourniquet (WALANT) to general anesthesia in plating of distal radius fractures with pain and anxiety level perception. Cureus. 2021;13:e12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hustedt JW, Chung A, Bohl DD, et al. Comparison of postoperative complications associated with anesthetic choice for surgery of the hand. J Hand Surg. 2017;42:1–8.e5. [DOI] [PubMed] [Google Scholar]
- 72.Teo I, Lam W, Muthayya P, et al. Patients’ perspective of wide-awake hand surgery—100 consecutive cases. J Hand Surg. 2013;38:992–999. [DOI] [PubMed] [Google Scholar]
- 73.Nikkhah D, Ruston J, Pearl R, et al. WALANT carpal tunnel release: technical considerations and pain outcomes. J Plastic Reconstr Aesthet Surg. 2019;72:1576–1606. [DOI] [PubMed] [Google Scholar]
- 74.Thompson Orfield NJ, Badger AE, Tegge AN, et al. Modeled wide-awake, local-anesthetic, no-tourniquet surgical procedures do not impair driving fitness: an experimental on-road noninferiority study. J Bone Joint Surg. 2020;102:1616–1622. [DOI] [PubMed] [Google Scholar]
- 75.Gan TJ. Postoperative nausea and vomiting—can it be eliminated? JAMA. 2002;287:1233–1236. [DOI] [PubMed] [Google Scholar]
- 76.Lalchandani GR, Halvorson RT, Rahgozar P, et al. Wide-awake local anesthesia for minor hand surgery associated with lower opioid prescriptions, morbidity, and costs: a nationwide database study. J Hand Surg Global Online. 2020;2:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brown M, Bainbridge C, Wong J, et al. Wide Awake Hand Surgery Handbook. Available at https://www.bssh.ac.uk/_userfiles/pages/files/COVID/Wide%20Awake%20Hand%20Surgery%20Handbook%20v2.pdf. Published March 2020. Accessed November 29, 2023. [Google Scholar]
- 78.Lalonde DH. Wide Awake Hand Surgery. Boca Raton, FL: CRC Press; 2016. [Google Scholar]
- 79.Thakkar M, Bednarz B. WALANT and sickle cell disease: a cautionary tale. J Plastic, Reconstr Aesthet Surg. 2021;74:1633–1701. [DOI] [PubMed] [Google Scholar]
- 80.Chowdhry S, Seidenstricker L, Cooney DS, et al. Do not use epinephrine in digital blocks: myth or truth? Part II. A retrospective review of 1111 cases. Plast Reconstr Surg. 2010;126:2031–2034. [DOI] [PubMed] [Google Scholar]