Abstract
The Coronavirus disease (COVID-19) pandemic has revealed the fragility of pre-crisis African health systems, in which too little was invested over the past decades. Yet, development assistance for health (DAH) more than doubled between 2000 and 2020, raising questions about the role and effectiveness of DAH in triggering and sustaining health systems investments. This paper analyses the inter-regional variations and trends of DAH in Africa in relation to some key indicators of health system financing and service delivery performance, examining (1) the trends of DAH in the five regional economic communities of Africa since 2000; (2) the relationship between DAH spending and health system performance indicators and (3) the quantitative and qualitative dimensions of aid substitution for domestic financing, policy-making and accountability. Africa is diverse and the health financing picture has evolved differently in its subregions. DAH represents 10% of total spending in Africa in 2020, but DAH benefitted Southern Africa significantly more than other regions over the past two decades. Results in terms of progress towards universal health coverage (UHC) are slightly associated with DAH. Overall, DAH may also have substituted for public domestic funding and undermined the formation of sustainable UHC financing models. As the COVID-19 crisis hit, DAH did not increase at the country level. We conclude that the current architecture of official development assistance (ODA) is no longer fit for purpose. It requires urgent transformation to place countries at the centre of its use. Domestic financing of public health institutions should be at the core of African social contracts. We call for a deliberate reassessment of ODA modalities, repurposing DAH on what it could sustainably finance. Finally, we call for a new transparent framework to monitor DAH that captures its contribution to building institutions and systems.
Keywords: Health financing, development assistance, UHC, Africa
Key messages.
Development assistance for health (DAH) reaching African countries is lower than what is frequently recorded. Africa is diverse and the health financing picture has evolved differently in its subregions.
Overall, DAH may have undermined the formation of sustainable universal health coverage financing models in Central, Western and Eastern Africa.
The current architecture of official development assistance is no longer fit for purpose. Domestic financing of public health institutions and a package of basic services, mostly for maternal and child health, should be at the core of African social contracts.
The world needs a new transparent framework to monitor aid funds that captures their contribution to building institutions and systems.
Introduction
The COVID-19 pandemic has revealed the fragility of African health systems, in which too little was invested over the past decades. Investments in public health institutions, pre-service training, infrastructure and domestic supply chains have been particularly low. Development assistance for health (DAH) increased >5-fold between 2000 and 2020, with low-income countries (LICs), predominantly in Africa, being especially dependent on such assistance compared with other regions of the world (World Health Organization, 2021a). DAH has funded basic services’ commodities, such as routine childhood vaccines, insecticide-treated bed nets (ITNs) and medicines for child and maternal health services, all of which contributed to improvements in outcomes such as child mortality. However, there is no empirical evidence that DAH has resulted in a marked and durable improvement in health policy capacity, health system capacity (particularly in terms of human resources for health) and institutional functions of recipient LICs and lower-middle-income countries (LMICs) of Africa. By contrast, the literature shows that DAH partially substitutes for domestic government health spending (Farag et al., 2009; Dieleman and Hanlon, 2014).
In addition to the direct consequences of the pandemic, related macroeconomic pressures on fiscal space (World Bank Group, 2022) now increase uncertainties about the scale, predictability and geopolitics or conditions that come with DAH by financiers, be they bilateral, multilateral (largely mediated via institutional agents dominated by high income countries, (HICs)) or independent foundations. Globally in 2019, external health spending of US$17 billion accounted for just 0.21% of all health spending in the world (World Health Organization, 2021a). The proportion is, however, larger in LICs and LMICs, particularly regarding expenditures on basic health services and technologies like routine childhood vaccines, ITNs, diagnostics and medicines for child and maternal health services.
DAH has both quantitative and qualitative dimensions. The premise of contemporary DAH architecture seems coherent at first glance. Economic rationale calls for identifying key ‘health commons’ or ‘common goods for health’ to be funded through collective (i.e. ‘public’) funding of health interventions as market forces fail to ensure adequate funding (Soucat, 2019; Financing the Global Commons for Pandemic Preparedness and Response, 2022).
Common goods for health are population-based functions or interventions that require collective financing, either from governments or donors based on the following conditions:
Contribute to health and economic progress.
There is a clear economic rationale for intervention based on market failures, with a focus on (1) public goods (non-rival and non-exclusionary) or (2) large social externalities (Yazbeck and Soucat, 2019).
Global burden of disease estimates provide broad parameters to identify these unmet needs for technology-based interventions and policy measures, such as taxes, to curb the consumption of harmful products with negative externalities, a prime example of which is tobacco (Gaudin et al., 2019). Cost-effectiveness estimates inform selections of ‘best buy’ interventions for collective financing to achieve value for money, where value is defined as the avoided loss of life-years (Jamison et al., 2013). Finally, the equity dimension has been increasingly built into the rationale for public financing and DAH, highlighting the need for public collective financing to support the needs and rights of poor people to access health care. This rationale has been expanded to poorer countries to access more health funding, using a welfare economics- or rights-based approach, although evidence tends to show public financing and DAH benefit richer groups more (Yazbeck, 2009; Wagstaff, 2012).
To the extent that DAH contributed to the dissemination of technologies whose delivery drove improvements in indicators such as those for child mortality, DAH in its current form has some health benefits (Adeyi, 2023a). These benefits should, however, be considered in relation to other drivers of improvements in health such as female education, access to clean water and income growth (Abbuy, 2018). The analysis of cross-country spending on health consistently shows economic growth and poverty reduction as the single largest driver of improvements in health service use (World Health Organization, 2018).
The current logic of DAH has major risks. First, global compacts, such as political declarations of intent to achieve universal health coverage (UHC) (United Nations, 2019), implicitly promise the impossible: unlimited quantities of DAH for indefinite periods. Second, by centring on global compacts, powerful institutions and influential philanthropists, it sidelines the messy but vital country policy processes and sovereign decisions. Third, the effects of associated health system strengthening investments are unclear, particularly considering the global crisis of human resources for health (World Health Organization, 2016). Finally, the current construct of DAH has negative unintended consequences of major proportions. Those consequences include a qualitative displacement of domestic LMIC policy processes by externally decided priorities and varying degrees of displacement of LMIC domestic health funding by DAH (Adeyi, 2022, 2023a); reported abdication of responsibility by some LMIC governments (US Mission Liberia, 2023); and mismatches between the realities of LMICs on the one hand and the behaviours of major global health institutions on the other hand (Adeyi, 2023b).
No comprehensive assessment of the impact of health aid on health systems has been conducted so far. Typical assessments are either disease-specific or outcome-based. The global community still lacks an assessment framework to measure the reach of DAH, its effectiveness and its impact on health systems. This paper is a first step in addressing this issue by highlighting specific areas in which DAH has underperformed in terms of health systems strengthening in Africa, particularly in the areas of health financing and service delivery.
The paper focuses on two specific areas: spending on health and coverage with basic health services, with the aim of generating hypotheses for further analysis and research. Specifically, it analyses the evolution of DAH in Africa between 2000 and 2020 in relation to some key indicators of finance and health system performance, examining: (1) the evolution of DAH in the five regional economic communities of Africa between 2000 and 2020; (2) the relationship between DAH spending and health system performance indicators; (3) the hypothesis that increased fragmentation of DAH, with crowding out of domestic funding, contributed to weak health system responses to COVID-19 in African countries and (4) the quantitative and qualitative dimensions of aid substitution for domestic financing, policy-making and accountability.
Methods
Scope and time frame
The study aims to assess the impact of DAH spending on key health system performance indicators. It analyses DAH over the past two decades (2000–20) for all countries of Africa as the main variable of interest in relation to key economic, health spending and service delivery indicators.
The paper aims to generate initial responses and hypotheses to the following key research questions:
Do recipient country income and subregional location affect the level of DAH in Africa?
Are DAH trends different according to country income, regional location and public/private spending patterns?
Has DAH affected the performance of health service delivery in Africa over the past decade?
Did the COVID-19 crisis lead to a change in the DAH pattern in Africa?
The paper focuses on an analysis of trends of DAH in the 55 Member States of the African Union (AU) over 21 years in relation to country income, regional location, levels of public and private domestic spending on health, performance on coverage of health services and the COVID crisis in Africa. The study includes four key steps:
An analysis of DAH to the countries of the AU in relation to regional location, country income and levels of public and private financing for health.
An analysis of variations in DAH regional trends, as a share of overall spending as well as per capita spending.
An analysis of the relationship between DAH spending and health systems’ performance in terms of service delivery measured through the UHC index and sub-indexes, using the UHC health system sub-index to assess health system capacity.
A pre–post analysis of the impact of the COVID-19 crisis on health spending in African countries.
Data sources
The health spending and health service coverage data were extracted from the World Health Organization’s Global Health Expenditure Database (GHED), the Organisation for Economic Co-operation and Development (OECD) Development Assistance Committee (DAC) database, Global Health Observatory data repository, the World Bank DataBank and the ProPublica Nonprofit Explorer.
The GHED provides National Health Accounts expenditure data for WHO member states. These indicators encompassed measures of health spending, government expenditures on health (GGHE-D), private-sector contributions (PVT-D), external aid (EXT) and total aid to developing countries [official development assistance (ODA)]. Finally, the UHC service index, infectious disease and health system sub-indices were extracted from the Global Health Observatory data repository. The World Bank DataBank provides gross domestic product (GDP) per capita. The DAC website provides data on aid flow from OECD countries to developing countries.
Data analysis
Annual data on the indicators identified in Table 1 were extracted from the various sources for 2000–20. Comparative analyses of the evolution of DAH were undertaken for all countries. DAH funding was analysed as total, percentage of total spending and per capita and compared across the five geographical African regions (Western, Eastern, Central, Northern and Southern Africa) and over time. The trends of DAH spending per capita, as a total, as a share of overall spending and on a per capita basis compared between regions, between different country income groups and overtime between 2000 and 2020.
Table 1.
Study indicators
| Indicator category | Indicator | Source |
|---|---|---|
| Health financing | Current health expenditure (CHE) | World Health Organization Global Health Expenditure Databasea |
| Domestic general government health expenditure (GGHE-D) as a percentage of CHE | ||
| Domestic private health expenditure (PVT-D) as a percentage of CHE | ||
| External health expenditure (EXT) as a percentage of CHE | ||
| GGHE-D per capita in US$ | ||
| PVT-D per capita in US$ | ||
| EXT per capita in US$ | ||
| Global Fund income and disbursement data | ProPublica websiteb | |
| Total net ODA to developing countries | OECD DAC ODA resource flow databasec | |
| UHC index of service coverage GDP per capita |
Global Health Observatory data repositoryd The World Bank DataBanke |
Note: see the list of countries in the Supplementary Appendix.
World Health Organization. GHED. https://apps.who.int/nha/database/Select/Indicators/en, accessed 18 February 2023.
Propublica Nonprofit Explorer. https://projects.propublica.org/nonprofits/organizations/980380092, accessed 18 February 2023.
OECD ODA database. https://stats.oecd.org/viewhtml.aspx?datasetcode=TABLE2A&lang=en#, accessed 18 February 2023.
Global Health Observatory data repository. https://apps.who.int/gho/data/view.main.INDEXOFESSENTIALSERVICECOVERAGEv?lang=en, accessed 23 February 2023.
The World Bank DataBank. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=A9, accessed 23 February 2023.
Finally, multivariate panel data regression analyses were conducted to investigate the relationship between three dependent variables identified as proxies of health system performance (the UHC service index, UHC infectious disease sub-index and the UHC health system index) and DAH per capita. In this study, we used an aggregate production of the UHC coverage modelling framework. This model is given as follows:
UHC index = f(DAH per capita, GDP per capita, Domestic spending on health per capita, Country, Year), where the UHC index is the universal health coverage index that represents health system performance; DAH per capita is the development assistance per capita, signifying the external financial support for health-related initiatives; GDP per capita is the real GDP per capita, indicative of economic growth and development; and domestic spending on health per capita is the per capita expenditure on health services within the country.
This model examines the relationship between DAH and coverage of health services. It also incorporates measures for public domestic spending and country income to circumvent the possibility of omitted variable bias.
We also run a multivariate analysis looking at the relationship between the increase in the UHC index and cumulative DAH.
Finally, patterns of health spending in Africa were analysed between 2019 and 2020 looking at the evolution of DAH in relation to other health spending indicators before and during the COVID-19 pandemic.
Results
In 2020, spending on health in Africa (defined as AU states) represented US$118.7 billion or US$118 per capita (in 2020 US dollars), amounting to ∼5% of Africa’s total GDP. Most of this spending (48%) was private, while public spending was 42%. Donor spending amounted to US$11 billion or about US$12 per capita and 10% of total health spending in AU countries (Table 2). The picture of this funding varies between the regions in Africa. Private spending is the highest in Western Africa (63% of health spending) driving a high level of spending on health per capita. Spending in Northern and Southern Africa tends to be more public, while Eastern, Western and Central Africa are more aid dependent. DAH constituted higher percentages of total health spending in Eastern Africa (27%) and Central Africa (22%) than in Western Africa (12%). It was lower still in Southern Africa (6%) and Northern Africa (1%) (Table 3).
Table 2.
Total health spending by financing source, 2020
| Indicator | 2020 | % | Per capita | %GDP |
|---|---|---|---|---|
| (US$ million) | US$ | |||
| Domestic general government health expenditure | 50 261 | 42 | 38 | 2.1 |
| Domestic private health expenditure | 57 144 | 48 | 43 | 2.4 |
| External health expenditure | 11 307 | 10 | 8 | 0.5 |
| Current health expenditure | 118 712 | 100 | 89 | 5 |
Table 3.
Spending on health in the regions of Africa, 2020
| Region | Private | % | Public | % | Donor | % | Total spending | Per capita | %GDP |
|---|---|---|---|---|---|---|---|---|---|
| (US$ million) | (US$) | ||||||||
| Western Africa | 16 365 | 63 | 6429 | 25 | 3212 | 12 | 26 007 | 64 | 3.8 |
| Eastern Africa | 5536 | 36 | 5677 | 37 | 4091 | 27 | 15 304 | 40 | 4.0 |
| Central Africa | 3239 | 55 | 1356 | 23 | 1305 | 22 | 5901 | 36 | 4.2 |
| Northern Africa | 19 185 | 55 | 15 596 | 44 | 344 | 1 | 35 125 | 170 | 5.1 |
| Southern Africa | 12 819 | 35 | 21 202 | 58 | 2355 | 6 | 36 376 | 196 | 7.4 |
| Africa (all) | 57 144 | 48 | 50 261 | 42 | 11 307 | 10 | 118 712 | 118 | 4.9 |
Health spending represents 4% of GDP overall in Central, Eastern and Western Africa while reaching ∼6% in Northern Africa and 7% in Southern Africa. Private spending represents significant amounts, equivalent to or exceeding public spending (Table 4).
Table 4.
Per capita spending on health by source for Africa and each of the five regions, 2020
| Per capita spending on health by the source of funding (US$) | GDP per capita (US$) | Health spending as a percentage of GDP | Total public spending as a percentage of GDP (2020) | |||
|---|---|---|---|---|---|---|
| Region | Private | Public | Donor | |||
| Western Africa | 40 | 16 | 8 | 1292 | 5 | 24 |
| Eastern Africa | 15 | 15 | 11 | 2488 | 5 | 25 |
| Central Africa | 20 | 8 | 8 | 2262 | 5 | 20 |
| Northern Africa | 93 | 76 | 2 | 3269 | 6 | 55 |
| Southern Africa | 69 | 114 | 13 | 2534 | 7 | 33 |
| Africa (all) | 46 | 60 | 12 | 2171 | 5 | 26 |
Between 2000 and 2020, spending on health increased in Africa from US$53 per capita to US$118 per capita (in real 2022 USD) representing 4% of growth per year. Public spending increased 2.5-fold from US$24 to US$60, while private spending increased 1.8-fold from US$25 to US$46. Donor spending also increased 2.4-fold from US$5 to US$12. The growth of health spending has been slower than economic growth, which has been 5% on average over the period. Spending on health increased slowly and steadily in all regions until 2010 and then declined or stabilized. The pattern is, however, quite different between regions. The overall increase was, however, slower and more limited in Eastern and Central Africa (Figure 1).
Figure 1.

Evolution of total spending on health in the five regions of Africa. Spending on health in Africa increased fast and then declined and stabilized
When it comes to public spending, both Northern and Southern Africa experienced a rapid increase in public spending until 2011 and then a decrease and stabilization after 2015. Public spending has increased much more slowly in Central, Eastern and Western Africa and has remained flat since 2010. Western and Central Africa remain the regions with the lowest levels of public spending (Figure 2). Private spending follows a similar pattern as public spending in Northern and Southern Africa, both driven by economic or lack of economic growth. Western Africa is the region with the highest and most rapidly growing private spending pulled by the growth of private spending in Nigeria (Figure 3). DAH increased in all regions except Northern Africa before 2010. DAH then stabilized and even declined slightly after in all regions. Between 2003 and 2013, Southern Africa (and South Africa in particular) benefitted the most from DAH. DAH per capita in Southern Africa has been three to five times as high as it was in Western and Central Africa over this period. Overall, DAH decreased after 2013 with the sharp decline of DAH in South Africa but has remained stable afterwards(Figure 4).
Figure 2.
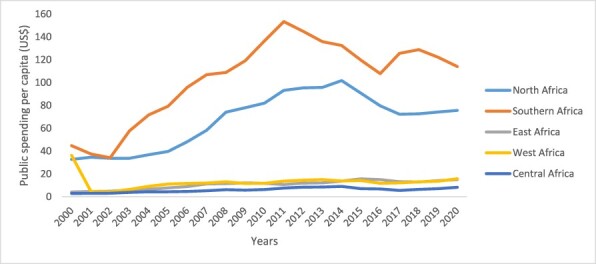
Evolution of public spending on health in the five regions of Africa 2000–20. Public spending has increased slowly in Central, Eastern and Western Africa between 2019 and 2020
Figure 3.
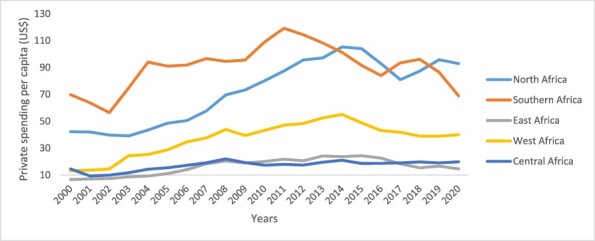
Evolution of private spending on health in the five regions of Africa 2019–20. Public spending has increased fast in Western and Northern Africa, while remaining more stable in Eastern and Central Africa
Figure 4.
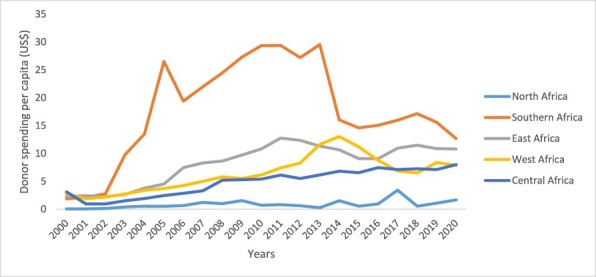
Evolution of donor spending on health in the five regions of Africa 2019–20. Donor spending in Southern Africa (to fight HIV) has been very high between 2003 and 2013
Overall, DAH is not allocated according to the economic needs of the recipient country. There is no relationship between GDP per capita and the amount of DAH received per capita (Figure 5). DAH to Africa represents US$11 billion overall, with a slightly higher share going to middle-income countries (MICs) (53%). Historically, DAH has benefitted richer countries of Southern Africa more than other regions. In 2020, significant amounts of DAH (5%) are still channelled to upper-middle-income countries (UMICs), particularly in Southern Africa. The 20 countries receiving the most DAH per capita are mostly MICs, including South Africa, an UMIC, 11 LMICs (Cameroon, Côte d’Ivoire, Democratic Republic of the Congo, Egypt, Ghana, Kenya, Nigeria, Senegal, Zambia, Zimbabwe and Tanzania) and only 8 LICs (Burkina Faso, Ethiopia, Malawi, Mali, Mozambique, Rwanda, South Sudan and Uganda) (Figure 6).
Figure 5.
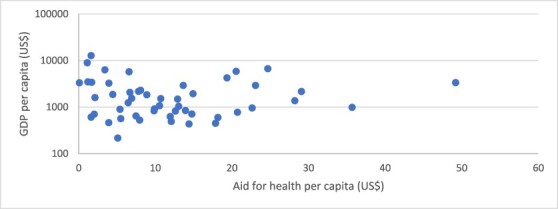
GDP per capita vs DAH per capita (all African countries). DAH is not related to country income
Figure 6.
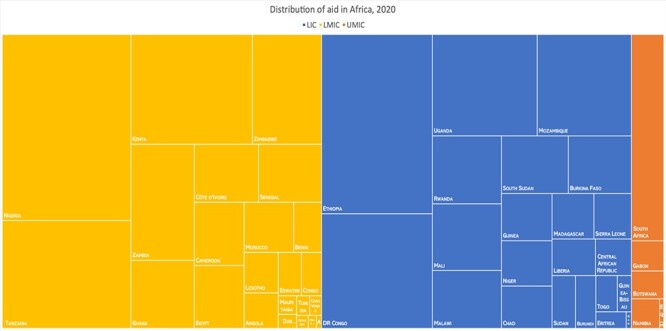
More DAH goes to MICs than LICs
Yet using another metric—the share of total spending covered by DAH—it appears that the poorest countries in Africa are still strongly dependent on DAH to fund their health. Most of these countries have a large share of their health spending funded by households when public spending is low. Among the 20 countries with the highest proportion of health spending funded by DAH, only two (Lesotho and Zimbabwe) are MICs (Figure 7). In these countries, DAH and private spending together constitute most of the spending with public spending representing the lowest share. In LICs, the share of public spending allocated to health also tends to decrease when DAH increases as aid tends to substitute for public spending on health. We find this effect to be particularly important in Western Africa (Figure 8).
Figure 7.
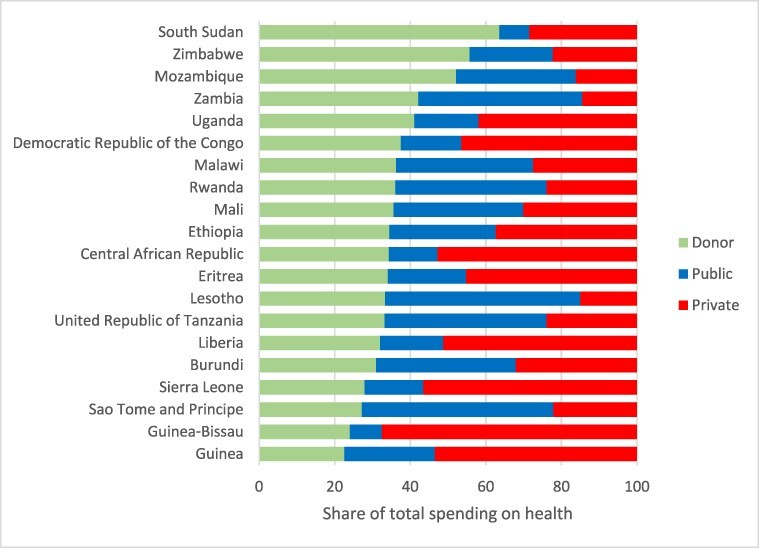
Share of health spending in 20 countries receiving most DAH in Africa. Health services in the poorest countries of Africa are mostly funded by households and DAH
Figure 8.
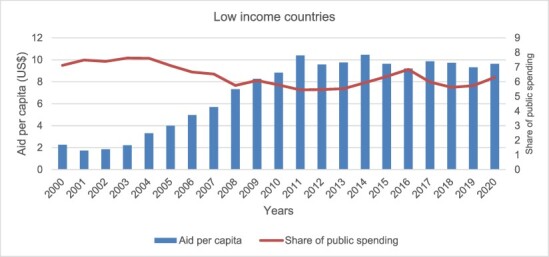
LICs’ evolution of the share of public spending on health and the amount of DAH per capita. Aid tends to crowd out public spending on health in LICs
The performance of DAH is also not clearly established when it comes to driving indicators of service coverage. There is no clear relationship between DAH per capita and the UHC Service Delivery Index. DAH per capita is also not related to the infectious disease component of the UHC index, although most DAH is typically targeted at these services (Figures 9 and 10).
Figure 9.
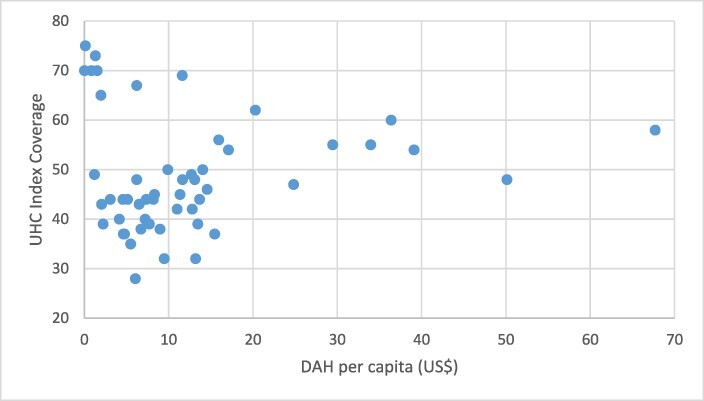
Aid per capita in Africa vs full UHC index coverage, 2019. There is little evidence of a relationship between public spending on health or aid spending on health and the UHC index
Figure 10.
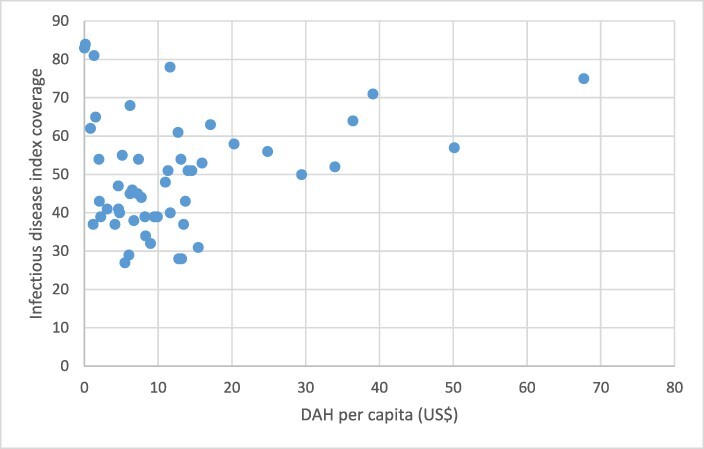
Infectious disease and DAH per capita in Africa, 2019. DAH per capita also shows little relationship with the infectious disease index coverage
The multivariate panel data analysis was done to investigate the relationship between the dependent variable (UHC index) and DAH per capita for all African countries from 2000 to 2019. The analysis shows mixed results. Domestic financing was found to significantly affect the level of the overall UHC index but DAH per capita was not. The analysis also found no significant country effect but a time effect. Aggregate DAH per capita between 2000 and 2020 was slightly significant in affecting the UHC infectious diseases and Health Systems Strengtehning sub-indexes, but the magnitude of the effect was small, hence a weak association with UHC. No effect of DAH was found on the increase of the UHC index between 2000 and 2019 (Supplementary Appendix).
Between 2019 and 2020, as the world was hit by the COVID-19 crisis, spending on health in Africa declined overall. But regions differed in the way they handled the crisis. Public spending on health declined in Eastern (−1%), Central (−9%) and Southern Africa (−6%), while it increased in Northern (+9%) and Western Africa (+4%). DAH increased in Central and Western Africa and in Northern Africa, most likely driven by the COVID response. But somewhat surprisingly, DAH per capita declined in Southern Africa (−28%) and Eastern Africa (−4%) (Figure 11). During the pandemic, government spending on health increased in LICs but not in MICs. Most of the response to the COVID pandemic in 2020 in LICs and LMICs was domestic with DAH declining among LMICs. Meanwhile, during the 2020 crisis, DAH increased mostly in UMICs, and mostly in Northern Africa (Figure 12).
Figure 11.
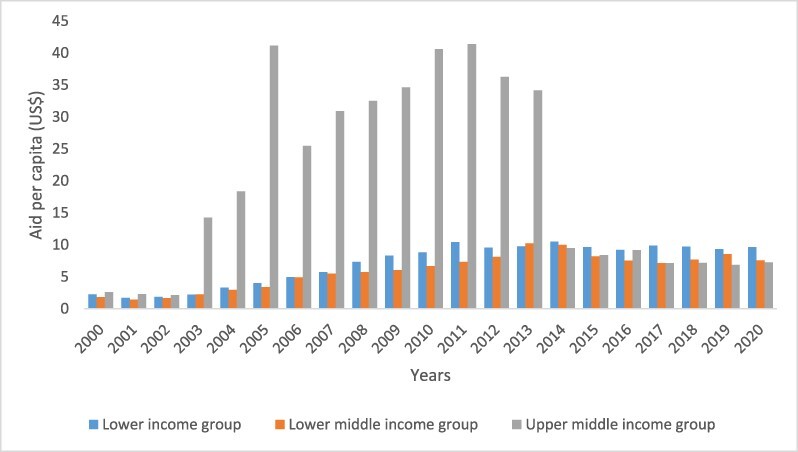
DAH per capita 2000–20 per country income group. DAH has been mostly driven by HIV funding and did not increase during the COVID-19 pandemic
Figure 12.
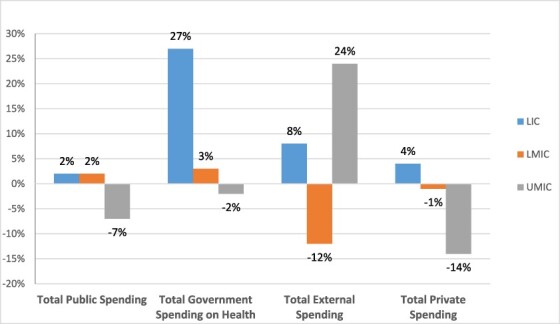
The percent change in expenditures between 2019 and 2020, per country income group. Spending during the COVID-19 crisis shows a mixed picture, with a major increase in domestic spending on health in LICs and an increase of DAH in UMICs
DISCUSSION
This study relies on data produced by countries over the past 20 years and as such is highly dependent on the quality of the process of country data production. The reliability and validity of DAH spending has been an issue for many years. However, this paper uses the GHED, a methodologically stable source of data managed by the WHO, which is produced and validated at the country, regional and global levels through a transparent process and uses a consistent methodology throughout 21 years of observation. The data reflect DAH spending at the country level and are produced using both national data and data reported to the OECD DAC. Those data show slightly lower health spending levels than DAC-reported disbursements as they reflect spending at the country level and do not account for disbursements to international health institutions that may have used these funds for global activities. These data also exclude overhead costs of donor organizations. The data are consistent with thorough work conducted by the WHO, which estimates DAH at the country level to be about US$16 billion in 2020 (World Health Organization, 2022a). The data are also consistent with those of Schäferhoff et al. (2019), using the Creditor Reporting System and G-FINDER databases, which estimated DAH to be about US$7 billion for global common goods in 2017 in addition to spending at the country level and overheads, bringing overall DAH spending to about US$29 billion. The data are, however, clearly lower than amounts based on expenditure modelling quoted in some reports, which estimate DAH to be much higher at about US$41 billion in 2020. We find no evidence to support the latter high number, which might reflect double counting, use of commitment figures rather than actual disbursements and misallocation of sovereign lending amounts as DAH (Institute of Health Metrics and Evaluation (IHME), 2022). We, therefore, think that the sources of data we used in this study are the best estimates currently available.
This study also shows the sensitivity to any analysis of DAH to the metrics used. Conclusions differ whether we use total DAH spending, share of DAH as part of total spending or DAH per capita spending. Our analysis shows that health spending in Africa remains low overall, both on a per capita basis and as a share of GDP, particularly in Central, Eastern and Western Africa. DAH constituted 10% of health spending in Africa in 2020 and overall amounts were concentrated in Eastern and Western Africa. But as a share of health spending overall, DAH represents a significant share of spending (>20% of total spending) only in Eastern and Central Africa, and mostly in LICs.
On a per capita basis, however, Southern Africa and Eastern Africa benefit significantly more, most probably because DAH has been driven by earmarked spending to address the human immunodeficiency virus (HIV) epidemic, and the largest number of people living with HIV in Africa are in these regions.
The analysis also confirms that health spending more than doubled in Africa between 2000 and 2020, yet health remained a low priority of government spending throughout the continent during the same period. On a per capita basis, it increased from US$53 to US$118 in real terms. Health spending increased from each source—government, private and external (DAH). Both public spending and DAH more than doubled during this period, while private spending increased the least among the three sources. The increase in overall spending was, however, slower than economic growth, showing an overall lack of prioritization of health, in household spending but also particularly in public budgets. Domestic public spending increased particularly slowly in Central, Eastern and Western Africa. These regions’ health financing framework is dominated by private spending and DAH, and only a handful of countries have initiated their health financing transition involving more pooled and more domestic public financing.
Africa is diverse and should not solely be looked at as one block. Overall findings mask inter-regional variations. Northern Africa and most of Southern Africa display a more mature health financing framework in terms of the absolute value and percentages of health spending derived from domestic public sources. At the same time, per capita, private spending on health is higher in Southern Africa (where Botswana and the Republic of South Africa have a very pluralistic public and private service delivery system). Northern Africa has also witnessed a rapid increase in private spending on health, faster than elsewhere on the continent. Donor financing is logically low in those two regions, which are richer than the other three. Yet, for 10 years, Southern Africa, mostly South Africa, has received extraordinarily high levels of DAH, in response to the HIV crisis in this region, and while these numbers have now declined, the rationale for DAH allocation has not yet been redefined. HIV/acquired immune deficiency syndrome programmes still dominate in DAH’s allocation, with little attention to the income rationale and the need to build country systems including building health infrastructure and tackling the human resources global shortage.
The other regions also display sharp differences. Strikingly, Western and Central Africa lag behind other regions both in terms of low amounts spent on health and because of their low levels of public domestic financing and high levels of private financing. Private financing in Western Africa is dominant largely due to the outsized reliance on out of pocket payments (OOPs) in Nigeria.
On a per capita basis, the MICs of Southern Africa were major beneficiaries of DAH during the 10-year period that started in 2003. Large amounts of DAH (more than half) also continue to be allocated to MICs (both UMICs and LMICs). This is particularly so for Nigeria, where DAH was 7% of the country’s current health expenditure in 2020. However, inherently regressive OOPs accounted for 75% of Nigeria’s current health expenditure during that year. Clearly, public financing remains a quantitatively minor factor in Nigeria’s health spending (World Health Organization, 2022c). Nigeria receiving significant amounts of aid has not slowed the growth of private spending, challenging the use of DAH to achieve UHC.
DAH accounted for >20% of total health spending in 24 countries in 2020, a measure of aid dependency. By that metric, the 10 most DAH-dependent AU countries in that year were South Sudan, Zimbabwe, Mozambique, Zambia, Uganda, Democratic Republic of the Congo, Malawi, Rwanda, Mali and Ethiopia, which are among the poorest countries in Africa. Furthermore, DAH exceeded domestic government spending in 10 countries in 2020. These countries were South Sudan, Zimbabwe, Mozambique, Uganda, the Democratic Republic of the Congo, Mali, Ethiopia, the Central African Republic, Eritrea and Liberia. These findings complement those reported elsewhere, including sub-Saharan Africa’s status as the most dependent on DAH compared with other regions, and the reliance of LICs on DAH and private spending to finance health (World Health Organization, 2022a).
The UHC index increased for every country between 2000 and 2019, with inter-country variations in the rate of change. In prior literature, the highest UHC index values were in the Southern and Northern African subregions (75 and 53, respectively), while the most rapid progress between 2000 and 2019 was observed in the Eastern African subregion (24 index points), followed by the Western and Southern African subregions (23 index points) (World Health Organization, 2022b). Almost all the measured progress is attributable to success in increasing the uptake of HIV interventions, ITNs and, to a lesser extent, improvements in maternal and child health. But there has been no improvement in the UHC health system index over time in Africa.
There is also a weak relationship between the per capita DAH and UHC index, particularly for the infectious diseases and health system components of the index. The effect is, however, of very small magnitude. While we do not underestimate the benefits of some aid programmes, there is, however, little evidence that those were instrumental in driving the progress in health coverage, once the effect of economic growth is accounted for. This finding is consistent with the analysis of the 2019 WHO Global Spending Report (World Health Organization, 2019).
Finally, the overall health financing framework has been tested by the COVID-19 pandemic. Total health spending in Africa increased from $112 billion in 2016 to $120 billion in 2019 and then declined to $118.7 billion in 2020, the first year of the COVID-19 pandemic. In 2020, as the pandemic hit hardest, overall spending on health decreased in Africa. Admittedly, there are plausible reasons for any decrease in health spending during the COVID-19 crisis, such as an expected net reduction in private spending on health, due to disruptions in mobility and/or provision of essential health services. But spending during the COVID-19 crisis shows a mixed picture in percentage terms, with a major increase in domestic spending on health in LICs, an increase of DAH in UMICs and a sharp decrease in DAH in LMICs. But this observation highlights the limitation of aid as a crisis response mechanism for LMICs.
Despite decades of statements of commitment to strengthening health systems in Africa, including by the WHO (World Health Organization, 2007) and global financiers (Global Fund to Fight AIDS, Tuberculosis, and Malaria, 2007; Kenney and Glassman, 2019; Waithaka et al., 2022), there were widespread fears and acknowledgements that African countries did not have health system capacities to effectively respond to the COVID-19 pandemic (Tessema et al., 2021). This suggests that the pre-COVID-19 aid architecture was ineffective in enabling African countries to develop robust health systems.
The combination of relatively high reliance on DAH compared with other regions, high OOPs and persistence of DAH for basic health services poses challenges for AU countries. Their exit from reliance on DAH for basic health services to funding those services exclusively from domestic resources, in what is often referred to as the economic transition of health, is fraught with risks of failure (Ly et al., 2017; OECD, 2021). While Northern and Southern Africa have initiated this transition, public spending has stalled after the 2008 crisis, with Northern Africa even witnessing an increase in private spending. Western and Central Africa still lag, with heavy reliance on private spending.
In combination with the above, two additional prior findings inform our subsequent perspectives and conclusions in this paper. First, in LICs, health spending from external aid increased from 0.7% of GDP in 2000 to 1.8% in 2020. Second, spending on inpatient care, outpatient care and medical goods accounted for >60% of total health spending in 2019 in all income groups globally, across the 109 countries with data; most government spending and DAH and donor spending on primary health care in the 18 LICs with available data went to preventive care (World Health Organization, 2022a). This is consistent with a dominant worldview that, within the overall health spending, DAH should be spent on the best buys of highly cost-effective services in preventive and clinical services in primary care settings.
The combination of this technocratic logic, when pitched as charitably saving the lives of people in LICs and LMICs, together with the tying of DAH to the procurement of goods and services from donor countries, is a political winner for leaders of HICs. But our findings lead us to challenge the practice of using DAH to finance cost-effective ‘best buys’ and now argue that governments of LICs and LMICs, not DAH, should pay for universal coverage with locally determined packages of the most cost-effective interventions and essential health commodities, determined through context-relevant priority setting. Doing so would have multiple ramifications. First, it would free each country to make executive policy choices that are truly owned by country leaders and citizens, not beholden to globally determined compacts or external preferences of DAH financiers. Such compacts and preferences constitute qualitative substitutions for stakeholder engagement in setting (Tomlinson et al., 2011) country policy priorities that derive from domestic transactions and bargaining among interest groups of policymakers, elected officials, technocrats, health service professionals and civil society—the foundation of durable social compacts. Second, it would free up, indeed compel, the reallocation of DAH funds from such basic health services at the country level to public goods and commons at the regional and global levels (Soucat and Kickbusch, 2020; Adeyi, 2023a). This combination of African self-reliance for basic services and commodities, with the repurposing of DAH on public goods and commons, would better serve the continent during normal times and crisis periods.
Policymaking is a complex and non-linear process. Governance, accountability and corruption issues plague health systems in many countries. Africa is no exception. The lack of progress on reaching the Abuja commitment of 15% of public spending allocated to health cannot be blamed on external aid only. But merely tinkering with the status quo, such as the proposal to refocus health aid at the margin of essential services (Drake et al., 2023), will not suffice. Instead, it could compound the problem by keeping aid agencies as de facto overseers of sovereign national priority setting. That strategy has not served LICs and LMICs well overall (Adeyi, 2022); it unwittingly provides an incentive for LIC and MIC governments to minimize their domestic public spending on basic services, based on expectations that DAH would cover all other basic services, and substitutes a narrow emphasis on health technology assessment for a robust priority setting exercise that includes not only technical considerations but also socio-political transactions and bargaining among domestic interest groups (Baltussen et al., 2023). Some advocates for DAH might argue that fiscal constraints and debt service obligations in LMICs justify continued or even greater DAH in its current form. Such advocacy unwittingly strengthens a charity-based narrative that ignores the intricacies of the international financial system and wrongly casts LMIC governments as passive victims who lack the agency to allocate more of their own resources to health. Many countries that benefitted from debt relief under the Heavily Indebted Poor Countries, or HIPC, Initiative have since accumulated high levels of debt and continued to be dependent on DAH (Adeyi, 2021). Although HICs have larger fiscal capacity and generally spend more on health per capita, there are large variations in health spending within each income group and prioritizing health is largely a choice at each income level (WHO, 2021b).
Finally, the global health enterprises that produce metrics of disease burden and cost-effectiveness are not accountable to governments of LICs and MICs (Shiffman and Shawar, 2020). We, therefore, call for a new transparent framework to monitor aid, which would include their contribution to building institutions and systems. With heightened priority to address deeper structural public health deficiencies at the national, regional and global levels, the AU through the Africa Centres for Disease Control and Prevention launched a framework for action, ‘A New Public Health Order for Africa’ in 2021 with five strategic pillars: (1) strengthened public health institutions, (2) strengthened public health workforce, (3) expanded manufacturing of vaccines, diagnostics and therapeutics, (4) increased domestic resources for health security and (5) respectful and action-oriented partnerships. Implementation of this framework is a political response to the experience of the past decades. Integral to the New Public Health Order is that African leaders take responsibility for formulating and financing health policies and programmes on the continent and that external actors and DAH play secondary roles, not the other way round. We do not argue for an abrupt end to DAH; instead, we propose an explicit transition from the status quo, including a shift of DAH from the current focus (country-specific basic health commodities and services) to the one where it has greater added value (regional and global commons), and an end to externally determined priorities for health in Africa, with emphasis on the accountability of African leaders to their citizens.
Conclusions
The external financing architecture was unable to mobilize additional funds for the health response to the worst health and development crisis in a generation. This counter-intuitive finding is from a continent with almost half of its countries relying on DAH for at least 20% of total health spending. There is an indication of a positive relationship between per capita DAH and the UHC index, particularly for the infectious disease component of the index (perhaps given the history of significant DAH going to infectious diseases), but this relationship is tempered by the overarching effect of domestic funding. We conclude that the pre-COVID-19 finance architecture lulled African governments into an ultimately unmet trust that additional DAH would be forthcoming during an extraordinary crisis. We suggest that it is time to decisively break from the status quo. Doing so is an essential and practical step from the legacy of externally driven disease control to an increasingly self-financed public health order.
Supplementary Material
Acknowledgements
The authors would like to thank Anas Ismail and Lorena Guerrero-Torres from the Alliance for Health Policy and Systems Research, WHO for their help with proofreading the paper.
Contributor Information
Justice Nonvignon, Africa Centre for Disease Control and Prevention, Addis Ababa, Ethiopia; School of Public Health, University of Ghana, Accra, Ghana.
Agnès Soucat, Agence Francaise de Developpement, Paris, France; Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States.
Paulina Ofori-Adu, Policy Planning Monitoring and Evaluation Division, Ghana Health Service, Ghana.
Olusoji Adeyi, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; Resilient Health Systems, Washington, DC, United States.
Supplementary data
Supplementary data is available at Health Policy and Planning online.
Data availability
The datasets were derived from sources in the public domain: WHO Global Health Expenditure Database available at https://apps.who.int/nha/database/ViewData/Indicators/en, ProPublica available at https://projects.propublica.org/nonprofits/organizations/980380092, OECD ODA database available at https://stats.oecd.org/viewhtml.aspx?datasetcode=TABLE2A&lang=en#, Global Health Observatory data repository available https://apps.who.int/gho/data/view.main.INDEXOFESSENTIALSERVICECOVERAGEv?lang=en, The World Bank DataBank. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=A9.
Author contributions
J.N. conceived and designed the paper, defined the hypotheses and conclusions, supervised data analytics, wrote the methodology section and revised the write-up of all sections. A.S. oversaw the design and interpretation of the data analysis, wrote the first draft of the results and discussion sections and contributed to the write-up of all sections. P.A.O.A. conducted the data analysis under the supervision of the other authors. O.A. wrote the first draft of the background section and contributed to the final write-up of all sections through critical revision.
Reflexivity statement
The authors include two women and two men, two policymakers and two researchers. The authors’ nationalities are from Ghana, Nigeria and France. Each of the four authors lived and worked for >10 years in Africa. Three authors are economists. Two authors are Medical Doctors.
Ethical approval
The study relies on publicly available secondary economic data. The study did not include interactions with human subjects and did not require ethical approval for Human Subject Research as per the World Medical Association (WMA) Helsinki declaration.
Conflict of interest statement
None declared.
References
- Abbuy E. 2018. Macroeconomic determinants of infant mortality in WAEMU countries: evidence from panel data analysis. Applied Economics and Finance 5: 52–56. [Google Scholar]
- Adeyi O. 2021. Opinion: global health, narcissistic charity, and neo-dependency. Development Today.https://www.development-today.com/archive/dt-2021/dt-9—2021/global-health-narcissistic-charity-and-neo-dependency, accessed 17 February 2023.
- Adeyi O. 2022. Global Health in Practice: Investing Amidst Pandemics, Denial of Evidence, and Neo-Dependency. Singapore: World Scientific, 221–54. [Google Scholar]
- Adeyi O. 2023a. In focus: transitioning out of aid dependency in health. Development co-operation report 2023: debating the aid system. Paris: OECD, 87–96. [Google Scholar]
- Adeyi O. 2023b. Misguided charity: the bane of global health. BMJ Global Health 8: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltussen R, Mwalim O, Blanchet K et al. 2023. Decision-making processes for essential packages of health services: experience from six countries. BMJ Global Health 8: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieleman JL, Hanlon M. 2014. Measuring the displacement and replacement of government health expenditure. Health Economics 23: 129–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake T, Regan L, Baker P. 2023. Reimagining global health financing: how refocusing health aid at the margin could strengthen health systems and futureproof aid financial flows. Policy Paper. Center for Global Development. https://www.cgdev.org/publication/reimagining-global-health-financing-how-refocusing-health-aid-margin-could-strengthen, accessed 28 February 2023.
- Farag M, Nandakumar AK, Wallack SS, Gaumer G, Hodgkin D. 2009. Does funding from donors displace government spending for health in developing countries? Health Affairs 28: 1045–55. [DOI] [PubMed] [Google Scholar]
- Financing the Global Commons for Pandemic Preparedness and Response . 2022. Financing the Global Commons for Pandemic Preparedness and Response. Retrieved from Financing the Global Commons for Pandemic Preparedness and Response. https://pandemic-financing.org/about-us/, accessed 23 February 2023.
- Gaudin S, Smith PC, Soucat A, Yazbeck AS. 2019. Common goods for health: economic rationale and tools for prioritization. Health Systems & Reform 5: 280–92. [DOI] [PubMed] [Google Scholar]
- Global Fund to Fight AIDS, Tuberculosis, and Malaria . 2007. Global Fund Strategic Approach to Health-Systems Strengthening. Board Decisions. GF/B15/DP06. https://www.theglobalfund.org/kb/board-decisions/b15/b15-dp06/, accessed 27 February 2023.
- Institute of Health Metrics and Evaluation (IHME) . 2022. Global Expected Health Spending 2019-2050, GHDx. https://ghdx.healthdata.org/record/ihme-data/global-expected-health-spending-2019-2050, accessed 27 February 2023.
- Jamison DT, Summers LH, Alleyne G et al. 2013. Global health 2035: a world converging within a generation. The Lancet 382: 1898–955. [DOI] [PubMed] [Google Scholar]
- Kenney C, Glassman A. 2019. Gavi’s Approach to Health Systems Strengthening: Reforms for Enhanced Effectiveness and Relevance in the 2021–2025 Strategy. https://www.cgdev.org/sites/default/files/gavis-approach-health-systems-strengthening-reforms-revised-june-2019.pdf, accessed 27 February 2023.
- Ly C, Eozenou P, Nandakumar A et al. 2017. The economic transition of health in Africa: a call for progressive pragmatism to shape the future of health financing. Health Systems & Reform 3: 290–300. [DOI] [PubMed] [Google Scholar]
- OECD . 2021. Financing transition in the health sector: what can development assistance committee members do? OECD Development Policy Paper No. 37, Paris: OECD. [Google Scholar]
- Schäferhoff M, Chodavadia P, Martinez S et al. 2019. International funding for global common goods for health: an analysis using the creditor reporting system and G-Finder databases. Health Systems & Reform 5: 350–65. [DOI] [PubMed] [Google Scholar]
- Shiffman J, Shawar Y. 2020. Strengthening accountability of the global health metrics enterprise. The Lancet 395: 1452–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soucat A. 2019. Financing common goods for health: fundamental for health, the foundation for UHC. Health Systems & Reform 5: 263–7. [DOI] [PubMed] [Google Scholar]
- Soucat A, Kickbusch I. 2020. Global common goods for health: towards a new framework for global financing. Global Policy 11: 628–35. [Google Scholar]
- Tessema GA, Kinfu Y, Dachew BA et al. 2021. The COVID-19 pandemic and healthcare systems in Africa: a scoping review of preparedness, impact, and response. BMJ Global Health 6: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson M, Chopra M, Hoosain N et al. 2011. A review of selected research priority setting processes at national level in low and middle income countries: towards fair and legitimate priority setting. Health Research Policy and Systems 9: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . 2019. Political Declaration of the High-Level Meeting on Universal Health Coverage. https://www.uhc2030.org/news-and-stories/news/political-declaration-for-the-un-high-level-meeting-meeting-on-uhc-555296/#:∼:text=in%20New%20York-,The%20Political%20Declaration%20for%20the%20UN%20High%2DLevel%20Meeting%20on,2019%20in%20New%20York%2C%20USA.&text=The%20Declaration%20follows%20months%20of,movement%20including%20these%20Key%20Asks, accessed 17 February 2023.
- US Mission Liberia . 2023. A Press Statement by U.S. Ambassador to Liberia Michael A. Mccarthy. https://lr.usembassy.gov/a-press-statement-by-u-s-ambassador-to-liberia-michael-a-mccarthy/, accessed 17 February 2023.
- Wagstaff A. 2012. Benefit-incidence analysis: are government health expenditures more pro-rich than we think? Health Economics 21: 351–66. [DOI] [PubMed] [Google Scholar]
- Waithaka D, Cashin C, Barasa E. 2022. Is performance-based financing a pathway to strategic purchasing in sub-Saharan Africa? A synthesis of the evidence. Health Systems & Reform 8: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank Group . 2022. Fiscal Implications of the Deteriorating Global Economic Environment for EMDEs. Washington, DC: The World Bank Group. [Google Scholar]
- World Health Organization . 2007. Everybody’s Business—Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action. https://apps.who.int/iris/handle/10665/43918, accessed 23 February 2023.
- World Health Organization . 2016. High-Level Commission on Health Employment and Economic Growth: Report of the Expert Group. World Health Organization. https://apps.who.int/iris/handle/10665/250040.
- World Health Organization . 2018. Public spending on health: a closer look at global trends. No. WHO/HIS/HGF/HFWorkingPaper/18.3. World Health Organization. License: CC BY-NC-SA 3.0 IGO.
- World Health Organization . 2019. Global spending on health: a world in transition. No. WHO/HIS/HGF/HFWorkingPaper/19.4. World Health Organization. License: CC BY-NC-SA 3.0 IGO.
- World Health Organization . 2021a. . Global Expenditure on Health: Public Spending on the Rise? World Health Organization. https://apps.who.int/iris/handle/10665/350560.
- World Health Organization . 2021b. External Health Expenditure (EXT) as Percentage of Current Health Expenditure (CHE) (%). The Global Health Observatory. Geneva: World Health Organization. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/external-health-, accessed 17 February 2023. [Google Scholar]
- World Health Organization . 2022a. Global Spending on Health: Rising to the Pandemic’s Challenges. World Health Organization. https://www.who.int/publications/i/item/9789240064911, accessed 17 February 2023.
- World Health Organization . 2022b. Tracking Universal Health Coverage in the WHO African Region, 2022. https://www.afro.who.int/publications/tracking-universal-health-coverage-who-african-region-2022, accessed 16 February 2023.
- World Health Organization. 2022c. Global Health Expenditure Database. https://apps.who.int/nha/database/ViewData/Indicators/en, accessed 10 February 2023.
- Yazbeck A. 2009. Attacking Inequality in the Health Sector: A Synthesis of Evidence and Tools. Washington, DC: The World Bank. [Google Scholar]
- Yazbeck AS, Soucat A. 2019. When both markets and governments fail health. Health Systems & Reform 5: 268–79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets were derived from sources in the public domain: WHO Global Health Expenditure Database available at https://apps.who.int/nha/database/ViewData/Indicators/en, ProPublica available at https://projects.propublica.org/nonprofits/organizations/980380092, OECD ODA database available at https://stats.oecd.org/viewhtml.aspx?datasetcode=TABLE2A&lang=en#, Global Health Observatory data repository available https://apps.who.int/gho/data/view.main.INDEXOFESSENTIALSERVICECOVERAGEv?lang=en, The World Bank DataBank. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=A9.


