Abstract
Non-alcoholic fatty liver disease (NAFLD) has become an urgent public health issue with high global prevalence, but data on NAFLD are inconsistent. The association of total dietary vitamin A intake with the NAFLD risk was not well documented in previous studies. To explore the relationship between dietary vitamin A intake from different sources and NAFLD risk among American adults. Data were collected from the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2014. Logistic regression and restricted cubic spline models were used to estimate the relationship between total dietary vitamin A intake and NAFLD risk. 6,613 adult participants were included. After adjusting potential confounders, the odds ratios (ORs) with 95% confidence intervals (CIs) of NAFLD for the highest quartile intake of total vitamin A, preformed vitamin A, provitamin A carotenoids were respectively 0.86 (0.69–1.06), 0.97 (0.74–1.28), and 0.78 (0.61–0.99), compared to the lowest quartile. Stratifying gender and age, provitamin A carotenoids intake was inversely associated with NAFLD risk in females and participants aged < 45 years. Dose–response analysis indicated a linear negative relationship between provitamin A carotenoids intake and NAFLD risk. Provitamin A carotenoids intake was inversely associated with NAFLD, especially in women and those aged < 45 years among adult American.
Subject terms: Diseases, Health care, Medical research, Risk factors
Introduction
Non-alcoholic fatty liver disease (NAFLD) is characterized by lipid accumulation in the liver without excessive alcohol intake or any other liver diseases1. NAFLD encompasses a wide spectrum of liver damage, ranging from simple liver steatosis to non-alcoholic steatohepatitis (NASH), liver fibrosis, cirrhosis and hepatocellular carcinoma (HCC)2–5, which increases the risk of hypertension, diabetes, obesity, and cardiovascular diseases6–8. The prevalence of NAFLD is estimated to be approximately 30% among American adults9. To our knowledge, there is currently no pharmacological treatment approved for NAFLD10. Dietary modifications and antioxidants have been recommended to prevent the progression of NAFLD11.
Several modifiable lifestyles and dietary factors are associated with chronic diseases. Previous studies demonstrated that high intake of vegetables, fruits, and whole grains, as a dietary pattern was associated with reduced risk of hypertension, hyperuricemia, type 2 diabetes, and cardiovascular diseases12–16. In addition, several studies reported that consuming fried foods, refined grains, processed meat, and fructose-rich foods increased the risk of NAFLD17–19. In contrast, whole grains, legumes, probiotic dairy products, vegetables, and fruits reduced the risk of NAFLD19–22.
Vitamin A is a common dietary antioxidant23 with both antioxidant and antifibrotic properties24. The two major forms of dietary vitamin A are preformed vitamin A (such as retinol and retinyl esters) and provitamin A carotenoids (such as β-carotene). Animal products with preformed vitamin A provide ≥ 70% of daily vitamin A intake. Provitamin A carotenoids that are mainly found in fruits and vegetables provide ≤ 30% of daily vitamin A intake25, which can be cleaved and metabolized into retinol after absorption by the intestinal cells26. The basic mechanisms of preformed vitamin A and carotenoids absorption were first investigated 40 years ago using rat everted intestinal sacs27–29. The data obtained indicated that preformed vitamin A absorption occurred via (a) carrier-dependent proteins, while carotenoids were absorbed by a passive diffusion process 26. In addition, preformed vitamin A is absorbed by intestinal epithelial cells, stored in the liver, and metabolized into retinoic acid (RA) and retinyl esters (RE) in target cells30. In liver cells, RE are hydrolyzed by retinyl ester hydrolase to produce retinol, and RA can reduce the progression of NAFLD by increasing triglyceride hydrolysis and fat oxidation30. Carotenoids possess antioxidant properties and can physiologically scavenge free radical species in the liver, thereby ameliorating hepatic dysfunction31. Therefore, it is important to study the effects of dietary vitamin A on NAFLD patients. At present, the potential relationship between total dietary vitamin A intake and NAFLD risk remains elusive. An Iranian study indicated that higher vitamin A intake was associated with reduced risk of NAFLD32. Based on the results of the study of Vahid et al.33, dietary vitamin A was associated with a decreased the risk of NAFLD. Additionally, a Chinese cohort revealed an inverse relationship between vitamin A intake and NAFLD risk34. However, a Korean study showed that participants with NAFLD had higher vitamin A intake than healthy subjects35. Similarly, Federico et al. reported higher vitamin A intake in NASH subjects than those without NASH36.
Previous studies mainly focused on the association between total dietary vitamin A intake and NAFLD risk32–34. However, studies reporting the association between dietary vitamin A intake from different sources and NAFLD risk are scarce. Furthermore, the dose–response relationship between dietary vitamin A intake and NAFLD risk has not been previously investigated. The present cross-sectional study aimed to explore the relationship between dietary vitamin A intake from different sources and NAFLD risk. The results of our study may be useful for alleviating NAFLD in American adults.
Methods
Study population
The National Health and Nutrition Examination Survey (NHANES) was conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC) in the United States (US)37. The survey was a continuous program with 2-year cycles starting from 199938. The NHANES included demographic, socioeconomic, dietary, and health-related questions. The examinations consisted of medical, dental, and physiological measurements, as well as laboratory tests conducted by highly trained medical personnel, which were collected from a complex multistage stratified sample representative of the non-institutionalized civilian US population39. The study protocol was approved by the Research Ethics Review Board of National Center for Health Statistics. In addition to this, we confirmed that all research was performed in accordance with relevant guidelines/regulations, and included in our manuscript a statement confirming that informed consent was obtained from all participants and/or their legal guardians.
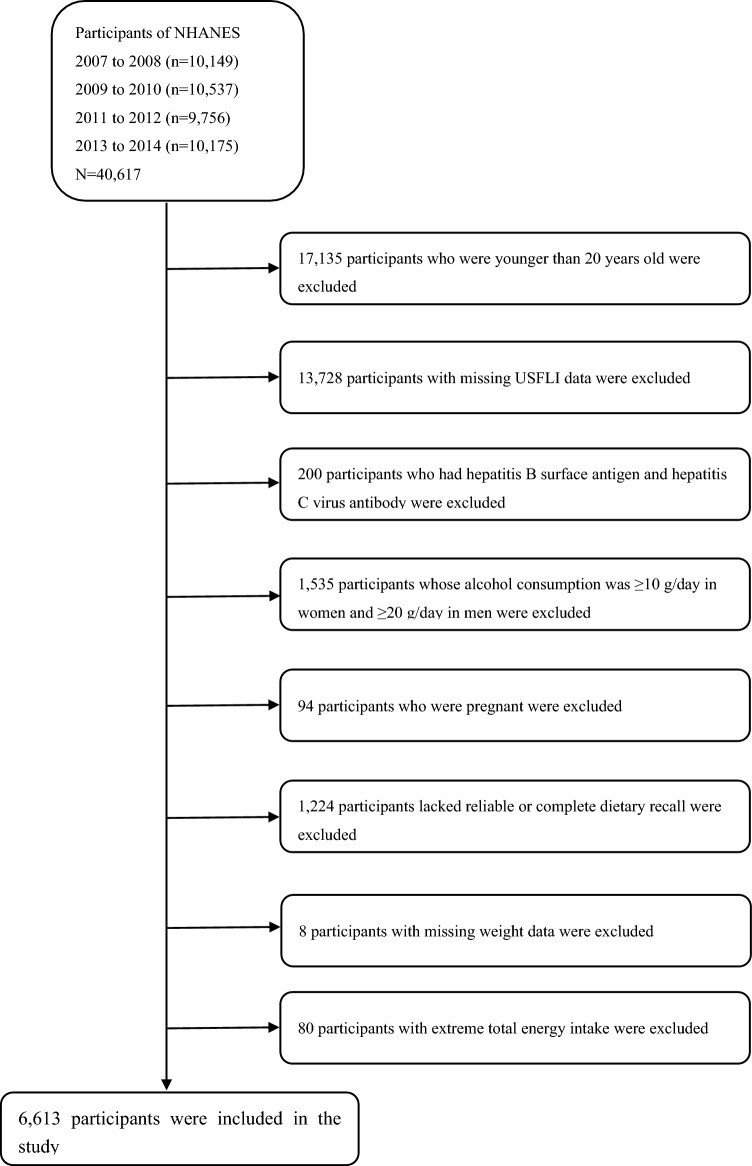
This study analyzed the continuous NHANES data between 2007 and 2014. The NHANES database included 40,617 participants (20,180 males and 20,437 females), and 23,482 subjects aged 20 years or older were included. Participants with missing information to calculate the United States fatty liver index (USFLI) were excluded (n = 13,728). Furthermore, 200 individuals who had hepatitis B surface antigen and hepatitis C virus antibodies were excluded. Subsequently, participants whose alcohol consumption was ≥ 10 g/day in women and ≥ 20 g/day in men (n = 1535) were also excluded. Finally, 6613 participants (3067 males and 3546 females) were included in our analyses, after excluding those who were pregnant (n = 94), lacking reliable or complete dietary recall (n = 1224), missing weight data (n = 8) and whose average energy intake was higher than mean + 3 standard deviations (SDs) or less than mean – 3 SDs (n = 80) (Fig. 1).
Figure 1.
Flow chart showing the eligible participants selection of the study. NHANES National Health and Nutrition Examination Survey.
NAFLD definition and measurement
According to a previous study40, NAFLD was defined based on USFLI, which was previously validated and excluded those with other causes of chronic liver disease and exposure to steatogenic medication. USFLI was calculated based on age, race, waist circumference, fasting glucose level, gamma glutamyl transferase level, and fasting insulin level41. A USFLI cut-off value of ≥ 30 indicated the presence of NAFLD41. As reported in previous articles, USFLI is a credible non-invasive measure of NAFLD and an independent predictor of liver-related and overall mortality42–44. The USFLI was calculated as follows:
The value for “non-Hispanic Black” and “Mexican American” is 1 if the person is of that ethnicity, and 0 if the person is not.
Dietary vitamin A intake
Dietary vitamin A intake was calculated by two 24-h dietary recall interviews in retinol activity equivalents (μg)45. The first dietary recall interview was performed in person at the mobile examination center, and the second interview was performed through telephone after 3–10 days. Nutrient intake was calculated according to the US Department of Agriculture’s Dietary Research Food and Nutrition Database for Dietary Studies15. Different sources of dietary vitamin A, such as preformed vitamin A (milk and milk products, meat, poultry, fish, eggs) and provitamin A carotenoids (legumes, nuts and seeds, grain products, fruits, vegetables) were identified using the food codes46. The dietary vitamin A intakes from the two 24-h recalls were averaged and adjusted to the energy intake for subsequent analysis. Dietary vitamin A intake (μg/1000 kcal/day) was divided into quartiles. It should be noted that dietary vitamin A intake from supplements was not included in total dietary vitamin A intake. As for preformed vitamin A, 1 μg retinol activity equivalents (RAEs) were equal to 1 μg all-trans retinol from animal foods. Provitamin A carotenoids was estimated by using the diet equation: 1 RAEs (μg) = 1/12 β-carotene (μg) + 1/24 other provitamin A (μg)45.
Covariates
Potential confounding factors were adjusted in multivariate models, including gender (male and female), age (20–44 years, 45–59 years, 60–74 years and ≥ 75 years), race (Mexican-Americans, other Hispanics, non-Hispanic Whites, non-Hispanic Blacks and other races), body mass index (BMI) (normal: < 25 kg/m2, overweight: 25 to < 30 kg/m2,obese: ≥ 30 kg/m2), education level (under high school, high school, and above high school), annual household income (< $20,000, $20,000–$44,999, $45,000–$74,999 and ≥ $75,000), smoking status (smoking at least 100 cigarettes in life or not), vigorous recreational activity (yes or no), diabetes (yes or no), hypertension (yes or no), total cholesterol (TC), and uric acid (UA). Diabetes was defined based on the following conditions: (1) fasting blood glucose level ≥ 7.0 mmol/L, (2) 2-h plasma glucose level ≥ 11.1 mmol/L, (3) use of antidiabetic pills or insulin, or (4) self-reported diabetes diagnosed by a physician47. Hypertension was defined as mean systolic blood pressure ≥ 130 mmHg or mean diastolic blood pressure ≥ 80 mmHg, and taking antihypertensive agents and self-reported physician diagnosis48.
Statistical analysis
All statistical analyses were performed using Stata 15.0. Appropriate sample weights and units and stratified information of the sample design were used in our analyses. In accordance with the NHANES guidelines49, new 8-year sample weights were computed by dividing the 2-year dietary weights by four. To compare the difference between groups, Chi-square test was used for categorical variables, while Student’s t-test or Mann–Whitney U test was used for continuous variables normal and non-normal distribution. Logistic regression models were used to evaluate the association between dietary retinol and NAFLD risk. For these analyses, the dietary vitamin A levels were divided into quartiles, and the first quartile (Q1) was set as a reference category. Two models were constructed: model 1 included gender and age; in model 2, we further adjusted for race, educational level, smoking status, recreational activities, annual household income, hypertension, diabetes, BMI, UA, and TC levels. After stratification by sex (male and female) and age (20–44 and ≥ 45 years), logistic regression analyses were conducted to analyze the relationship between total dietary vitamin A intake and NAFLD risk. Odds ratios (ORs) with 95% confidence intervals (CIs) were computed based on the results of logistic regression analyses. Furthermore, dose–response relationships between total dietary vitamin A intake and NAFLD risk were assessed using a restricted cubic spline regression and three knots were located at the 5th, 50th, and 95th percentiles. The non-linearity p-value was computed by examining the values of the quadratic zero spline coefficient, and a two-tailed p < 0.05 was considered statistically significant.
Ethics statement
The participants provided written informed consent for publishing any potentially identifiable images or data in this study.
Results
The mean age of participants was 50.75 years. The mean level of dietary vitamin A was 334 μg/1000 kcal/day (305 and 359 μg/1000 kcal/day in males and females, respectively). NAFLD was detected in 36.7% of participants (41.9% of males and 32.1% of females). Table 1 showed the comparison of baseline characteristics between the NAFLD and non-NAFLD groups (stratification by gender shown in Supplementary Table S1). Participants with NAFLD tended to be older, involved more Mexican-Americans, and had lower education level, annual household income, vigorous recreational activity, and provitamin A carotenoids intake compared to the control group. In addition, participants with NAFLD were more likely obese, smokers, hypertensive, diabetic, and hyperuricemic and had higher preformed vitamin A intake than those without NAFLD (all p < 0.01).
Table 1.
Baseline characteristics of the participants by NAFLD, U.S. adults aged ≥ 20 years, NHANES 2007–2014.
| Group | NAFLD (total) | p-value | |
|---|---|---|---|
| No | Yes | ||
| Age group (n, %) | < 0.001 | ||
| 20–44 years | 1890(45.12%) | 709(29.25%) | |
| 45–59 years | 988(23.59%) | 655(27.02%) | |
| 60–74 years | 862(20.58%) | 742(30.61%) | |
| ≥ 75 years | 449(10.72%) | 318(13.12%) | |
| Race/ethnicity (n, %) | < 0.001 | ||
| Mexican American | 488(11.65%) | 552(22.77%) | |
| Other Hispanic | 444(10.60%) | 294(12.13%) | |
| Non-Hispanic White | 1845(44.04%) | 1155(47.65%) | |
| Non-Hispanic Black | 931(22.22%) | 269(11.10%) | |
| Other/multiracial | 481(11.48%) | 154(6.35%) | |
| BMI (n, %) | < 0.001 | ||
| < 25 kg/m2 | 1716(41.02%) | 108(4.46%) | |
| 25 to < 30 kg/m2 | 1568(37.49%) | 637(26.32%) | |
| ≥ 30 kg/m2 | 899(21.49%) | 1675(69.21%) | |
| Educational level (n, %) | < 0.001 | ||
| < High school | 902(21.55%) | 802(33.14%) | |
| High school | 954(22.80%) | 543(22.44%) | |
| > High school | 2329(55.65%) | 1075(44.42%) | |
| Annual household income (n, %) | < 0.001 | ||
| < $20,000 | 780(19.45%) | 561(24.14%) | |
| $20,000–$44,999 | 1352(33.71%) | 931(40.06%) | |
| $45,000–$74,999 | 781(19.47%) | 409(17.60%) | |
| ≥ $75,000 | 1098(27.37%) | 423(18.20%) | |
| Smoking status (n, %) | < 0.001 | ||
| Yes | 1576(37.64%) | 1131(46.66%) | |
| No | 2611(62.36%) | 1293(53.34%) | |
| Vigorous recreational activity (n, %) | < 0.001 | ||
| Yes | 1031(24.61%) | 270(11.14%) | |
| No | 3158(75.39%) | 2154(88.86%) | |
| Hypertension (n, %) | < 0.001 | ||
| Yes | 1648(39.34%) | 1539(63.49%) | |
| No | 2541(60.66%) | 885(36.51%) | |
| Diabetes (n, %) | < 0.001 | ||
| Yes | 505(12.06%) | 910(37.54%) | |
| No | 3684(87.94%) | 1514(62.46%) | |
| Cholesterol (mg/dL) | 192.16 ± 41.19 | 194.23 ± 41.79 | 0.051 |
| Uric acid (mg/dL) | 5.14 ± 1.30 | 6.03 ± 1.43 | < 0.001 |
| Average energy intake (kcal/day) | 1903.27 ± 695.88 | 1912.03 ± 711.51 | 0.625 |
| Total dietary vitamin A intake (RAEs, μg/1000 kcal/day) | 338.66 ± 284.09 | 325.69 ± 279.77 | 0.072 |
| Preformed vitamin A intake (RAEs, μg/1000 kcal/day) | 122.70 ± 150.62 | 134.97 ± 205.69 | 0.005 |
| Provitamin A carotenoids intake (RAEs, μg/1000 kcal/day) | 198.80 ± 238.80 | 171.24 ± 181.11 | < 0.001 |
The associations of total dietary vitamin A, preformed vitamin A, and provitamin A carotenoids intake with NAFLD risk were shown in Table 2. In the univariate logistic regression model, the highest quartile of total dietary vitamin A intake (OR: 0.79, 95% CI: 0.67–0.92) and provitamin A carotenoids intake (OR: 0.64, 95% CI: 0.52–0.79) were inversely associated with NAFLD risk compared to the lowest quartile of intake. However, there was no significant association between preformed vitamin A intake and NAFLD risk. After adjusting age and gender, the association remained significant: 0.70 (95% CI: 0.58–0.84) and 0.59 (95% CI: 0.47–0.74) for total dietary vitamin A and provitamin A carotenoids intake, respectively. Furthermore, after adjusting race, educational level, smoking status, recreational activities, annual household income, hypertension, diabetes, BMI, UA and TC levels, the association remained significant for provitamin A carotenoids intake: 0.78 (95% CI: 0.61–0.99, p < 0.05). However, the protective effect of total dietary vitamin A intake on NAFLD was no longer significant after adjusting the above covariates (model 2).
Table 2.
Weighted ORs and 95% CIs for NAFLD according to the quartiles of dietary retinol intake (μg /1000 kcal/day).
| Crude, OR (95% CI) | p-trend | Model 1, OR (95% CI) | p-trend | Model 2, OR (95%CI) | p-trend | |
|---|---|---|---|---|---|---|
| Total dietary vitamin A intake (RAEs, μg/1000 kcal/day) | 0.004 | < 0.001 | 0.103 | |||
| < 191.63 | 1.00(ref.) | 1.00(ref.) | 1.00(ref.) | |||
| 191.63 to < 284.53 | 1.11(0.92–1.34) | 1.03(0.84–1.26) | 1.08(0.80–1.44) | |||
| 284.53 to < 418.94 | 1.06(0.91–1.23) | 0.96(0.81–1.15) | 1.01(0.79–1.29) | |||
| ≥ 418.94 | 0.79(0.67–0.92)** | 0.70(0.58–0.84)** | 0.86(0.69–1.06) | |||
| Preformed vitamin A intake (RAEs, μg/1000 kcal/day) | 0.217 | 0.773 | 0.655 | |||
| < 59.27 | 1.00(ref.) | 1.00(ref.) | 1.00(ref.) | |||
| 59.27 to < 104.86 | 1.10(0.92–1.31) | 1.02(0.86–1.22) | 1.12(0.88–1.42) | |||
| 104.86 to < 164.21 | 1.21(1.02–1.44)* | 1.13(0.95–1.34) | 1.12(0.88–1.43) | |||
| ≥ 164.21 | 1.11(0.92–1.32) | 1.02(0.83–1.24) | 0.97(0.74–1.28) | |||
| Provitamin A carotenoids intake (RAEs, μg/1000 kcal/day) | < 0.001 | < 0.001 | 0.011 | |||
| < 70.37 | 1.00(ref.) | 1.00(ref.) | 1.00(ref.) | |||
| 70.37 to < 138.53 | 0.95(0.78–1.15) | 0.94(0.77–1.16) | 1.08(0.84–1.38) | |||
| 138.53 to < 253.07 | 0.85(0.70–1.04) | 0.82(0.67–1.01) | 0.93(0.70–1.23) | |||
| ≥ 253.07 | 0.64(0.52–0.79)** | 0.59(0.47–0.74)** | 0.78(0.61–0.99)* |
OR odds ratio, CI confidence interval.
Model 1 adjusted for gender and age. Model 2 adjusted gender, age, race, education level, smoking status, physical activity, income level, hypertension, diabetes, BMI, UA and TC. The lowest quartile of dietary retinol intake was used as the reference group. Results are survey-weighted. *p < 0.05, **p < 0.01. Test for trend based on variable containing median value for each quartile.
Supplementary Tables S2 and S3 show the association between dietary vitamin A intake and NAFLD risk in the subgroup analyses stratified by gender and age, respectively. In multivariate-adjusted model 2, the highest quartile of provitamin A carotenoids intake (OR: 0.61, 95% CI: 0.43–0.89) was negatively associated with NAFLD risk only in females. In Supplementary Table S3 (model 2), provitamin A carotenoids intake had 40% lower odds of NAFLD risk (OR: 0.60, 95% CI: 0.42–0.87, the highest vs. lowest quartile of provitamin A carotenoids intake) among participants aged < 45 years. After adjusting potential confounding factors in model 2, there were no significant associations of total dietary vitamin A, preformed vitamin A, and provitamin A carotenoids intake with NAFLD risk among participants ≥ 45 years of age.
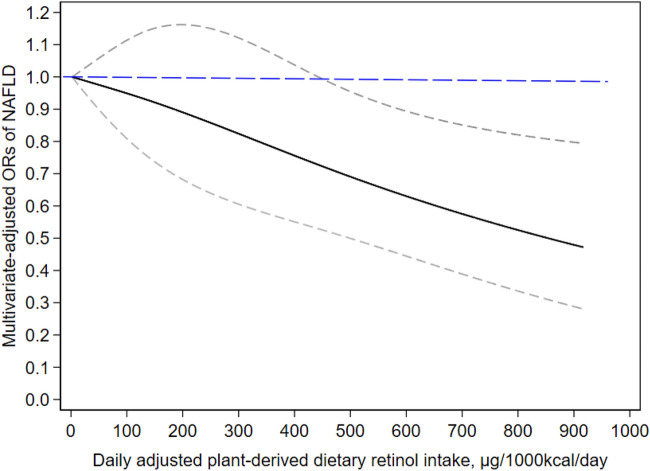
The dose–response relationship between provitamin A carotenoids intake and NAFLD risk is displayed in Fig. 2. A linear negative dose–response correlation was observed between provitamin A carotenoids intake and NAFLD risk (P for non-linearity = 0.734). When provitamin A carotenoids intake reached 449 μg/1000 kcal/day, it was inversely associated with NAFLD (OR: 0.72, 95% CI: 0.53–0.99).
Figure 2.
The dose–response pattern of plant-derived dietary retinol intake exposures and the NAFLD status was displayed in the restricted cubic splines model. The results were presented treating the lowest level of plant-derived dietary retinol intake (2 μg/1000 kcal/day) as a reference group. Potential confounding factors, such as gender, age, race, education level, smoking status, physical activity, income level, hypertension, diabetes, BMI, UA and TC were adjusted. The solid line and dashed line represent the estimated odds ratio (ORs) and the corresponding 95% confidence intervals (CIs), respectively.
Discussion
Total dietary vitamin A intake was not associated with NAFLD risk after adjusting potential confounders. However, there was a significant association between the dietary vitamin A intake from different sources and NAFLD risk, in which provitamin A carotenoids intake was inversely associated with the risk of NAFLD. After stratification by gender and age, the significant correlations remained in both females and participants aged less than 45 years. A linear negative dose–response relationship was also found between provitamin A carotenoids intake and NAFLD risk. To the best of our knowledge, this is the first study to demonstrate the relationship between dietary vitamin A intake from different sources and NAFLD risk.
Several studies reported contradictory results about the association between dietary vitamin A intake and NAFLD risk. A population-based study in Iran indicated that the consumption of dietary vitamin A could decrease the risk of NAFLD32. Vahid et al.33 reported that dietary vitamin A intake was negatively related to the risk of NAFLD. Moreover, a cohort study involving 241 Chinese rural adults also found a negative association between dietary vitamin A intake and NAFLD risk34. Conversely, a Korean study with 80 participants showed that the dietary intake of vitamin A was higher in NAFLD patients than in healthy subjects35. Another study in Italy also reported similar results36. These controversial findings might be attributed to the lack of adjustment for potential confounders as well as discrepancies in ethnic background, dietary patterns, and study design.
Provitamin A carotenoids are widely distributed in plant foods. In this study, provitamin A carotenoids (such as β-carotene) was assessed by calculating vitamin A mainly from plant foods such as legumes, beans, fruits, and vegetables. Previously, few studies had reported the association between dietary vitamin A intake from different sources with NAFLD risk. Our results found that provitamin A carotenoids intake was inversely associated with NAFLD. Although the mechanism underlying the association between provitamin A carotenoids intake and NAFLD risk remains unclear, some possible mechanisms have been proposed. Higher mobilization of β-carotene for conversion into retinol could be responsible for the lower intake of provitamin A carotenoids in NAFLD patients than in healthy subjects in the present study50. Another possible explanation might be that the bioavailability of carotenoids was greatly affected by food substrate51–54. Experimental studies showed that carotenoids could reverse steatosis, inflammation, and fibrosis progression in NASH, thereby preventing macrophage or Kupffer cell activation, attenuating insulin resistance, and ameliorating steatohepatitis55. Through their anti-inflammatory and antioxidant properties, carotenoids modulate intracellular signaling pathways involved in gene expression and protein translation56. A previous study indicated that the antioxidant properties of carotenoids could prevent liver damage and NAFLD by alleviating oxidative stress in hepatocytes57. Several studies reported that the levels of high-sensitivity C-reactive protein (hs-CRP) and inflammatory cytokines (e.g., IL-6 and TNF-α) were associated with NAFLD risk, which were considered as biomarkers of inflammation leading to endothelial cell damage58,59. Several studies demonstrated that carotenoids and their metabolites were likely to modulate adiponectin expression60,61. Adiponectin may alleviate inflammation by downregulating nuclear factor-kappa B (NFκB) and TNF-α, thereby reducing the risk of NAFLD62. Preformed vitamin A (such as retinol and retinyl esters) was not inversely associated with NAFLD was that with the increase of dietary retinol, the content of animal fat and cholesterol also increased, which was the risk factor for NAFLD. The exact mechanism for the association between total dietary vitamin A intake and NAFLD risk is still unclear. Additional studies were warranted to explore the underlying mechanisms.
Interestingly, some studies indicated that non-vitamin A intakes also have certain effect on NAFLD. A study showed that the increased incidence of NAFLD patients was closely related to the increased intake of cholesterol and saturated fat63. However, a Chinese study found a negative relationship between dietary vitamin C intake and NAFLD64. Another study revealed that dietary vitamin E intake was related to lower odds of NAFLD65. The study by Christensen reported that intake of α-carotene, β-carotene, β-cryptoxanthin, and lutein/zeaxanthin had a significant improvement in NAFLD57. In addition, Kaiyue et al.66 also reported that flavonoids can have beneficial effects on NAFLD by regulating the activity of CYP2E1.
The strength of our study is as follows. First, this study was a nationwide study conducted on American adults, which increased the statistical power and reliability of the study. Second, to explore the association between dietary vitamin A intake and NAFLD risk, the subgroup analyses stratified by gender and age were used. And provitamin A carotenoids intake was inversely associated with NAFLD, especially in women and those aged < 45 years among adult American in our study. Third, dose–response relationships between total dietary vitamin A intake and NAFLD risk were assessed using a restricted cubic spline regression.
Nevertheless, several limitations should be addressed. First, we did not determine the causal relationship between total dietary vitamin A intake and NAFLD risk because of the cross-sectional design of this study. Second, using data from two 24-h dietary recall interviews might lead to recall bias. In this study, dietary vitamin A intake from supplements was not included in total dietary vitamin A intake, so we did not evaluate the relationship between dietary vitamin A intake from supplements and NAFLD risk. Third, USFLI had superior sensitivity in identifying NAFLD patients9,41. However, USFLI cannot determine NAFLD stages, and the correlation between total dietary vitamin A intake and NAFLD risk is still unclear. Fourth, the possibility of residual confusion caused by other confounders cannot be excluded. Finally, NAFLD status was estimated based on a previously validated index rather than a clinical diagnosis.
Conclusions
Under the general trend of the increasing global prevalence rate of NAFLD, US has become one of the high-prevalence-rate countries. To reduce the prevalence of NAFLD, targeted measures have been implemented. Although therapeutic options for NAFLD are limited, the current findings shed light on the prevention and treatment of NAFLD by identifying modifiable lifestyle factors, especially the consumption of provitamin A carotenoids.
Supplementary Information
Acknowledgements
The authors thank all of the people who participated in this study.
Author contributions
C.L., J.L. and Y.H.F. designed the study. X.N.S., J.P. and H.Q.Y. collected the data. C.L. and J.L. analyzed the data and C.L. drafted the manuscript. J.L. and Y.H.F. critically revised the manuscript. Y.H.F. agreed to take responsibility for all aspects of the work. All authors read and approved the final manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (Project Approval No. 71804101).
Data availability
The dataset generated for this study is available in online repositories, and access is provided through the following link: https://www.cdc.gov/nchs/nhanes/index.htm.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-52077-5.
References
- 1.Angulo P. Nonalcoholic fatty liver disease. N. Engl. J. Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 2.Vadarlis A, Antza C, Bakaloudi DR, et al. Systematic review with meta-analysis: The effect of vitamin E supplementation in adult patients with non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2021;36:311–319. doi: 10.1111/jgh.15221. [DOI] [PubMed] [Google Scholar]
- 3.Afzali N, Ebadi SS, Afzali H, et al. Effect of Beta vulgaris extract on liver enzymes in patients with non-alcoholic fatty liver disease: A randomized clinical trial. Hepat. Mon. 2020;20:e102125. doi: 10.5812/hepatmon.102125. [DOI] [Google Scholar]
- 4.Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018;15:11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 5.Estes C, Razavi H, Loomba R, et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li H, Gu Y, Wu X, et al. Association between consumption of edible seaweeds and newly diagnosed non-alcohol fatty liver disease: The TCLSIH Cohort Study. Liver Int. 2021;41:311–320. doi: 10.1111/liv.14655. [DOI] [PubMed] [Google Scholar]
- 7.Younossi ZM, Henry L. The impact of obesity and type 2 diabetes on chronic liver disease. Am. J. Gastroenterol. 2019;114:1714–1715. doi: 10.14309/ajg.0000000000000433. [DOI] [PubMed] [Google Scholar]
- 8.Targher G, Byrne CD, Lonardo A, et al. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J. Hepatol. 2016;65:589–600. doi: 10.1016/j.jhep.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Le MH, Devaki P, Ha NB, et al. Prevalence of non-alcoholic fatty liver disease and risk factors for advanced fibrosis and mortality in the United States. PLoS One. 2017;12:e0173499. doi: 10.1371/journal.pone.0173499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rinella ME, Loomba R, Caldwell SH, et al. Controversies in the diagnosis and management of NAFLD and NASH. Gastroenterol. Hepatol. (N Y) 2014;10:219–227. [PMC free article] [PubMed] [Google Scholar]
- 11.Pietu F, Guillaud O, Walter T, et al. Ursodeoxycholic acid with vitamin E in patients with nonalcoholic steatohepatitis: Long-term results. Clin. Res. Hepatol. Gastroenterol. 2012;36:146–155. doi: 10.1016/j.clinre.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Sun Y, Sun J, Zhang P, et al. Association of dietary fiber intake with hyperuricemia in U.S. adults. Food Funct. 2019;10:4932–4940. doi: 10.1039/C8FO01917G. [DOI] [PubMed] [Google Scholar]
- 13.Buil-Cosiales P, Martinez-Gonzalez MA, Ruiz-Canela M, et al. Consumption of fruit or fiber-fruit decreases the risk of cardiovascular disease in a Mediterranean young cohort. Nutrients. 2017;9:295. doi: 10.3390/nu9030295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yao B, Fang H, Xu W, et al. Dietary fiber intake and risk of type 2 diabetes: A dose-response analysis of prospective studies. Eur. J. Epidemiol. 2014;29:79–88. doi: 10.1007/s10654-013-9876-x. [DOI] [PubMed] [Google Scholar]
- 15.Sun B, Shi X, Wang T, et al. Exploration of the association between dietary fiber intake and hypertension among U.S. adults using 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines: NHANES 2007–2014. Nutrients. 2018;10:1091. doi: 10.3390/nu10081091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kranz S, Dodd KW, Juan WY, et al. Whole grains contribute only a small proportion of dietary fiber to the U.S. diet. Nutrients. 2017;9:153. doi: 10.3390/nu9020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mollard RC, Sénéchal M, MacIntosh AC, et al. Dietary determinants of hepatic steatosis and visceral adiposity in overweight and obese youth at risk of type 2 diabetes. Am. J. Clin. Nutr. 2014;99:804–812. doi: 10.3945/ajcn.113.079277. [DOI] [PubMed] [Google Scholar]
- 18.Ouyang X, Cirillo P, Sautin Y, et al. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J. Hepatol. 2008;48:993–999. doi: 10.1016/j.jhep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shim P, Choi D, Park Y. Association of blood fatty acid composition and dietary pattern with the risk of non-alcoholic fatty liver disease in patients who underwent cholecystectomy. Ann. Nutr. Metab. 2017;70:303–311. doi: 10.1159/000475605. [DOI] [PubMed] [Google Scholar]
- 20.Dorosti M, Jafary Heidarloo A, Bakhshimoghaddam F, et al. Whole-grain consumption and its effects on hepatic steatosis and liver enzymes in patients with non-alcoholic fatty liver disease: A randomised controlled clinical trial. Br. J. Nutr. 2020;123:328–336. doi: 10.1017/S0007114519002769. [DOI] [PubMed] [Google Scholar]
- 21.Koutnikova H, Genser B, Monteiro-Sepulveda M, et al. Impact of bacterial probiotics on obesity, diabetes and non-alcoholic fatty liver disease related variables: A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2019;9:e017995. doi: 10.1136/bmjopen-2017-017995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maleki Z, Jazayeri S, Eslami O, et al. Effect of soy milk consumption on glycemic status, blood pressure, fibrinogen and malondialdehyde in patients with non-alcoholic fatty liver disease: A randomized controlled trial. Complement. Ther. Med. 2019;44:44–50. doi: 10.1016/j.ctim.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 23.Al-Busafi SA, Bhat M, Wong P, et al. Antioxidant therapy in nonalcoholic steatohepatitis. Hepat. Res. Treat. 2012;2012:947575. doi: 10.1155/2012/947575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pickett-Blakely O, Young K, Carr RM. Micronutrients in nonalcoholic fatty liver disease pathogenesis. Cell Mol. Gastroenterol. Hepatol. 2018;6:451–462. doi: 10.1016/j.jcmgh.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.USDA, ARS. What We Eat in America, NHANES 2009–2010. http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/0910/Table_1_NIN_GEN_09.pdf. Accessed 23 Feb 2011 (2011).
- 26.Reboul E. Absorption of vitamin A and carotenoids by the enterocyte: Focus on transport proteins. Nutrients. 2013;5:3563–3581. doi: 10.3390/nu5093563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hollander D, Muralidhara KS. Vitamin A1 intestinal absorption in vivo: Influence of luminal factors on transport. Am. J. Physiol. 1977;232:E471–477. doi: 10.1152/ajpendo.1977.232.5.E471. [DOI] [PubMed] [Google Scholar]
- 28.Hollander D, Ruble PE., Jr beta-carotene intestinal absorption: Bile, fatty acid, pH, and flow rate effects on transport. Am. J. Physiol. 1978;235:E686–691. doi: 10.1152/ajpendo.1978.235.6.E686. [DOI] [PubMed] [Google Scholar]
- 29.Hollander D. Intestinal absorption of vitamins A, E, D, and K. J. Lab. Clin. Med. 1981;97:449–462. [PubMed] [Google Scholar]
- 30.Bawa FNC, Zhang Y. Retinoic acid signaling in fatty liver disease. Liver Res. 2023;7:189–195. doi: 10.1016/j.livres.2023.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yilmaz B, Sahin K, Bilen H, et al. Carotenoids and non-alcoholic fatty liver disease. Hepatobiliary Surg. Nutr. 2015;4:161–171. doi: 10.3978/j.issn.2304-3881.2015.01.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lotfi A, Saneei P, Hekmatdost A, et al. The relationship between dietary antioxidant intake and physical activity rate with nonalcoholic fatty liver disease (NAFLD): A case–control study. Clin. Nutr. ESPEN. 2019;34:45–49. doi: 10.1016/j.clnesp.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 33.Vahid F, Rahmani D, Hekmatdoost A. The association between dietary antioxidant index (DAI) and nonalcoholic fatty liver disease (NAFLD) onset; new findings from an incident case–control study. Clin. Nutr. ESPEN. 2021;41:360–364. doi: 10.1016/j.clnesp.2020.10.020. [DOI] [PubMed] [Google Scholar]
- 34.Ma C, Liu Y, He S, et al. Negative association between antioxidant vitamin intake and non-alcoholic fatty liver disease in Chinese non-diabetic adults: Mediation models involving superoxide dismutase. Free Radic. Res. 2020;54:670–677. doi: 10.1080/10715762.2020.1825705. [DOI] [PubMed] [Google Scholar]
- 35.Lim HS, Choi J, Lee B, et al. Association between inflammatory biomarkers and nutritional status in fatty liver. Clin. Nutr. Res. 2020;9:182–194. doi: 10.7762/cnr.2020.9.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Federico A, Dallio M, Caprio GG, et al. Qualitative and quantitative evaluation of dietary intake in patients with non-alcoholic steatohepatitis. Nutrients. 2017;9:1074. doi: 10.3390/nu9101074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.NCHS. National Health and Nutrition Examination Survey (NHANES). http://www.cdcgov/nchs/nhaneshtm. Accessed 26 Aug 2022 (2022).
- 38.Zipf G, Chiappa M, Porter KS, et al. National health and nutrition examination survey: Plan and operations, 1999–2010. Vital Health Stat. 2013;1:1–37. [PubMed] [Google Scholar]
- 39.Choi WJ, Ford ES, Curhan G, et al. Independent association of serum retinol and beta-carotene levels with hyperuricemia: A national population study. Arthritis Care Res. (Hoboken) 2012;64:389–396. doi: 10.1002/acr.20692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhai T, Chen Q, Xu J, et al. Prevalence and trends in low bone density, osteopenia and osteoporosis in U.S. adults with non-alcoholic fatty liver disease, 2005–2014. Front. Endocrinol. (Lausanne) 2021;12:825448. doi: 10.3389/fendo.2021.825448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ruhl CE, Everhart JE. Fatty liver indices in the multiethnic United States National Health and Nutrition Examination Survey. Aliment Pharmacol. Ther. 2015;41:65–76. doi: 10.1111/apt.13012. [DOI] [PubMed] [Google Scholar]
- 42.Kim D, Kim W, Adejumo AC, et al. Race/ethnicity-based temporal changes in prevalence of NAFLD-related advanced fibrosis in the United States, 2005–2016. Hepatol. Int. 2019;13:205–213. doi: 10.1007/s12072-018-09926-z. [DOI] [PubMed] [Google Scholar]
- 43.Kim D, Yoo ER, Li AA, et al. Depression is associated with non-alcoholic fatty liver disease among adults in the United States. Aliment Pharmacol. Ther. 2019;50:590–598. doi: 10.1111/apt.15395. [DOI] [PubMed] [Google Scholar]
- 44.Meffert PJ, Baumeister SE, Lerch MM, et al. Development, external validation, and comparative assessment of a new diagnostic score for hepatic steatosis. Am. J. Gastroenterol. 2014;109:1404–1414. doi: 10.1038/ajg.2014.155. [DOI] [PubMed] [Google Scholar]
- 45.Zhang P, Sun J, Guo Y, et al. Association between retinol intake and hyperuricaemia in adults. Public Health Nutr. 2021;24:2205–2214. doi: 10.1017/S1368980020000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.U.S. Department of Agriculture, Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies 2011–2012. Food Surveys Research Group Home Page. http://www.ars.usda.gov/ba/bhnrc/fsrg (2014).
- 47.Menke A, Casagrande S, Geiss L, et al. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314:1021–1029. doi: 10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 48.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 49.Chen TC, Parker JD, Clark J, et al. National Health and Nutrition Examination Survey: Estimation procedures, 2011–2014. Vital Health Stat. 2018;2:1–26. [PubMed] [Google Scholar]
- 50.Mecocci P, Polidori MC, Troiano L, et al. Plasma antioxidants and longevity: A study on healthy centenarians. Free Radic. Biol. Med. 2000;28:1243–1248. doi: 10.1016/S0891-5849(00)00246-X. [DOI] [PubMed] [Google Scholar]
- 51.Edwards AJ, You CS, Swanson JE, et al. A novel extrinsic reference method for assessing the vitamin A value of plant foods. Am. J. Clin. Nutr. 2001;74:348–355. doi: 10.1093/ajcn/74.3.348. [DOI] [PubMed] [Google Scholar]
- 52.Edwards AJ, Nguyen CH, You CS, et al. Alpha- and beta-carotene from a commercial puree are more bioavailable to humans than from boiled-mashed carrots, as determined using an extrinsic stable isotope reference method. J. Nutr. 2002;132:159–167. doi: 10.1093/jn/132.2.159. [DOI] [PubMed] [Google Scholar]
- 53.Yeum KJ, Russell RM. Carotenoid bioavailability and bioconversion. Annu. Rev. Nutr. 2002;22:483–504. doi: 10.1146/annurev.nutr.22.010402.102834. [DOI] [PubMed] [Google Scholar]
- 54.Hickenbottom SJ, Follett JR, Lin Y, et al. Variability in conversion of beta-carotene to vitamin A in men as measured by using a double-tracer study design. Am. J. Clin. Nutr. 2002;75:900–907. doi: 10.1093/ajcn/75.5.900. [DOI] [PubMed] [Google Scholar]
- 55.Ni Y, Nagashimada M, Zhan L, et al. Prevention and reversal of lipotoxicity-induced hepatic insulin resistance and steatohepatitis in mice by an antioxidant carotenoid, β-cryptoxanthin. Endocrinology. 2015;156:987–999. doi: 10.1210/en.2014-1776. [DOI] [PubMed] [Google Scholar]
- 56.Elvira-Torales LI, García-Alonso J, Periago-Castón MJ. Nutritional importance of carotenoids and their effect on liver health: A review. Antioxidants (Basel) 2019;8:229. doi: 10.3390/antiox8070229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Christensen K, Lawler T, Mares J. Dietary carotenoids and non-alcoholic fatty liver disease among US adults, NHANES 2003(-)2014. Nutrients. 2019;11:1101. doi: 10.3390/nu11051101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yoneda M, Mawatari H, Fujita K, et al. High-sensitivity C-reactive protein is an independent clinical feature of nonalcoholic steatohepatitis (NASH) and also of the severity of fibrosis in NASH. J. Gastroenterol. 2007;42:573–582. doi: 10.1007/s00535-007-2060-x. [DOI] [PubMed] [Google Scholar]
- 59.Abe RAM, Masroor A, Khorochkov A, et al. The role of vitamins in non-alcoholic fatty liver disease: A systematic review. Cureus. 2021;13:e16855. doi: 10.7759/cureus.16855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shih PH, Shiue SJ, Chen CN, et al. Fucoidan and fucoxanthin attenuate hepatic steatosis and inflammation of NAFLD through modulation of leptin/adiponectin axis. Mar. Drugs. 2021;19:148. doi: 10.3390/md19030148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Iwaki M, Matsuda M, Maeda N, et al. Induction of adiponectin, a fat-derived antidiabetic and antiatherogenic factor, by nuclear receptors. Diabetes. 2003;52:1655–1663. doi: 10.2337/diabetes.52.7.1655. [DOI] [PubMed] [Google Scholar]
- 62.Cimini FA, Barchetta I, Carotti S, et al. Relationship between adipose tissue dysfunction, vitamin D deficiency and the pathogenesis of non-alcoholic fatty liver disease. World J. Gastroenterol. 2017;23:3407–3417. doi: 10.3748/wjg.v23.i19.3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mells JE, Fu PP, Kumar P, et al. Saturated fat and cholesterol are critical to inducing murine metabolic syndrome with robust nonalcoholic steatohepatitis. J. Nutr. Biochem. 2015;26:285–292. doi: 10.1016/j.jnutbio.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wei J, Lei GH, Fu L, et al. Association between dietary vitamin C intake and non-alcoholic fatty liver disease: A cross-sectional study among middle-aged and older adults. PLoS One. 2016;11:e0147985. doi: 10.1371/journal.pone.0147985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abdel-Maboud M, Menshawy A, Menshawy E, et al. The efficacy of vitamin E in reducing non-alcoholic fatty liver disease: A systematic review, meta-analysis, and meta-regression. Ther. Adv. Gastroenterol. 2020;13:1756284820974917. doi: 10.1177/1756284820974917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang K, Tan W, Liu X, et al. New insight and potential therapy for NAFLD: CYP2E1 and flavonoids. Biomed. Pharmacother. 2021;137:111326. doi: 10.1016/j.biopha.2021.111326. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset generated for this study is available in online repositories, and access is provided through the following link: https://www.cdc.gov/nchs/nhanes/index.htm.