Abstract
Introduction.
The SARS-CoV-2 virus that causes the COVID-19 disease, reports hundreds of infections daily, the alterations and sequelae of this new pathogen have been reported globally, due to the seriousness of being an older adult and evolving seriously.
Methodology.
The present work has a qualitative ap-proach, with exploratory and descriptive intentions of the alterations at a cognitive, neuropsychological, neuropsy-chiatric and neurological level.
Results.
In the analysis, 16 articles were included that express alterations in areas of functioning that compro-mise the quality of life in patients over 18 years of age, the scientific evidence is strong on the alterations caused by the new SARS-CoV-2 virus, from the deterioration of cognition, visuospatial abilities and constant headaches among other symptoms, which are of attention from a multidisciplinary perspective.
Conclusions.
The transmission of the virus in the adult population poses a risk to health, this study shows alterations at the cognitive, motor and neurological lev-el, age being a factor that predisposes the appearance of sequelae.
Keywords: COVID-19, Adults, neuropsychological disorders, cognitive impairment, neuropsychiatric sequelae, disease
ALTERACIONES COGNITIVAS, NEUROLÓGICAS, NEUROPSICOLÓGICAS Y NEUROPSIQUIÁTRICAS EN PACIENTES POST-COVID-19. UNA REVISIÓN SISTEMÁTICA
Introducción.
El virus SARS CoV-2 causante de la en-fermedad COVID-19, reporta cientos de contagios diaria-mente, las alteraciones y secuelas de este nuevo patógeno han sido reportadas a nivel global, por la gravedad que implica ser adulto mayor y evolucionar de manera grave.
Metodología.
El presente trabajo tiene un enfoque cualitativo, con intenciones exploratorias y descriptivas de las alteraciones a nivel cognitivo, neuropsicológico, neuropsiquiátrico y neurológico.
Resultados.
En el análisis fueron incluidos 16 artícu-los que expresan alteraciones en áreas de funcionamiento que comprometen la calidad de vida en pacientes mayores de 18 años, la evidencia científica es fuerte sobre las al-teraciones que provoca el nuevo virus SARS Cov-2, desde el deterioro de la cognición, habilidades visuoespaciales y cefaleas constantes entre otros síntomas, que son de atención desde una perspectiva multidisciplinar.
Conclusiones.
La transmisión del virus en la población adulta supone un riesgo a la salud, este estudio eviden-cia las alteraciones a nivel cognitivo, motor y neurológico siendo la edad un factor que predispone la aparición de secuelas.
INTRODUCTION
At the end of 2019 in Wuhan, China, a case of atyp-ical pneumonia with abnormal characteristics was re-ported that quickly began to spread, and in January 2020, health authorities recognized a new pathogen called SARS-CoV-2, which shares a strong connection with severe acute respiratory syndrome (SARS), and Middle East respiratory syndrome (MERS); This new virus is the cause of the disease COVID-19 (Wu et al., 2020), which in March 2020 was declared a global pandem-ic by the World Health Organization (WHO) due to its high level of contagion and mortality. (León et al., 2020; Mayo Clinic, 2021).
Among the most common symptoms are fever, cough, tiredness, loss of taste or smell, sore throat, headache, aches or pains in the body, although it can also cause di-arrhea, rash or discoloration of the fingers. hands or feet, red or irritated eyes, difficulty breathing or dyspnea, loss of mobility or speech, feeling confused and chest pain (Médica Sur, 2020; WHO, 2020).
However, brain imaging of patients who have required hospitalization have revealed Central Nervous System abnormalities as an important feature of COVID-19 that compromises the patient's health; these records sug-gest that the virus can penetrate the blood-brain barri-er and enter the central nervous system (neuroinvasion). This statement is evidenced by the following premises (Carod-Artal, 2020):
Involvement of the central nervous system by other respiratory viruses.
Neurological damage from coronavirus in other spe-cies.
Animal models of infection of the central nervous sys-tem by human coronaviruses.
Evidence of neurological complications from other coronaviruses.
Patients with COVID-19 who have presented neuro-logical manifestations.
This implies that the SARS-CoV-2 virus can cause neurological sequelae, with anosmia and ageusia being found more frequently, present in up to 88% of young female patients, while headaches appear in up to 34% of males. cases (Bernardo, 2021). However, other conditions can become as serious as brain parenchymal abnormal-ities, subcortical microhemorrhages and macrohemor-rhages, cortical subcortical swelling, and nonspecific deep changes in the white matter, triggering various pathologies: stroke, anosmia, cortical blindness, deliri-um, encephalitis., encephalopathy, hemiparesis, dizzi-ness, meningitis, flaccid paralysis, psychosis, memory problems, among others (Abenza-Abildúa et al., 2020; Carod-Artal, 2020; Da Silva, 2020; García et al., 2020; Quiroz and Amarales, 2020).
For this reason, it is suggested that the COVID-19 dis-ease causes a neurological, neuropsychological, neuro-psychiatric compromise, which can be caused through a direct lesion (viral replication in the nervous system) or an indirect lesion (activation of the inflammatory cascade, toxic alterations). -metabolic, immune dysregulation and immune-mediated mechanisms), which will entail 3 types of manifestations: of the central nervous system, of the peripheral nervous system and of the muscles (Aguilar and López, 2021). For the purposes of this research, the article will focus exclusively on the clinical manifesta-tions and alterations in perspective with the central ner-vous system.
In this regard, it is expected that COVID-19 will result in significant cognitive impairment (Riordan et al., 2020) that will affect a large part of the infected people, even if they were asymptomatic (Da Silva, 2020); In addition, the pandemic viral infection has reached about 362,549,889 infections around the world (Ritchie et al., 2022) and at least 70% of the survivors are expected to present some type of neurological, psychiatric or cognitive impairment after hospital discharge. (He et al., 2021; Sasannejad et al., 2019).
For this reason, the present work carried out a sys-tematic review of the neurological, neuropsychological, neuropsychiatric and neurocognitive consequences of in-fection by SARS-CoV-2, with the aim of classifying the neurological sequelae of COVID-19 in the adult popula-tion.
METHOD
The present work was carried out from a qualitative approach with exploratory and descriptive purposes. Spe-cifically, a systematic review was carried out that ana-lyzed the neurological, neuropsychological, neuropsychi-atric and neurocognitive effects of the COVID-19 disease in patients aged 18 years and older.
Sample
This was made up of articles available in the Clari- vate, EBSCO Medic Latina, JStor and Scopus databases, which have been published during the years 2020 and 2022 and are in open access.
Process
The search for scientific literature was carried out in the Clarivate, EBSCO Medic Latina, JStor and Scopus da-tabases using the terms "COVID-19", "neuropsychology", "neurocognitive" and "neuropsychiatric". With these, two search strings were created by adding the boolean oper-ator "AND":
1) "COVID AND neuropsychology".
2) "COVID AND neuropsychiatric".
3) "COVID AND neurocognitive"
Filter was applied by year. The review was carried out during the months of October-November 2021, Janu- ary-February and October-November 2022 with access to the databases from the BUAP Libraries electronic resourc-es repository. For data analysis, a database was created using the Google spreadsheet.
INCLUSION AND EXCLUSION CRITERIA
For the object of study, the included articles had to: 1) be scientific articles: 2) empirical: 3) open access; 4) available in Spanish or English; 5) address the neuropsy- chological/neuropsychiatric/neurocognitive sequelae of COVID-19 in adults older than 18 years; 6) these adults must not have had any type of medical problem prior to being infected with SARS-CoV-2; 7) all symptoms must have been reported at least 10 days after infection; 8) the data obtained should be shown by age ranges.
On the other hand, all those investigations that: 1) were of closed access were excluded; 2) were gray litera-ture; 3) were published in any language other than Span-ish or English; 4) had children or adolescents as a sample; 5) adults over 18 years of age with a medical problem prior to being infected with SARS-CoV-2; 6) had caregiv-ers as a sample; 7) had deceased people as a sample; 8) sampled pregnant women; 9) had medical personnel as a sample; 9) the information was obtained through self-re-ports; 10) the information would have been obtained by telephone and 11) the information would have been ob-tained online.
Selection process
Clarivate yielded 483 results, EBSCO Medic Latina 36, JStor 203 results, and Scopus provided 2,197. In to-tal, 2,506 entries were obtained, of which 349 articles were selected whose title alluded to "COVID-19," "neu- ro," "cognitive", "psychiatric", "psychology" and "SARS- CoV-2", and with them the systematic review began fol-lowing the phases proposed by the PRISMA flowchart, whose flowchart is visible in Figure 1.
Figura 1.
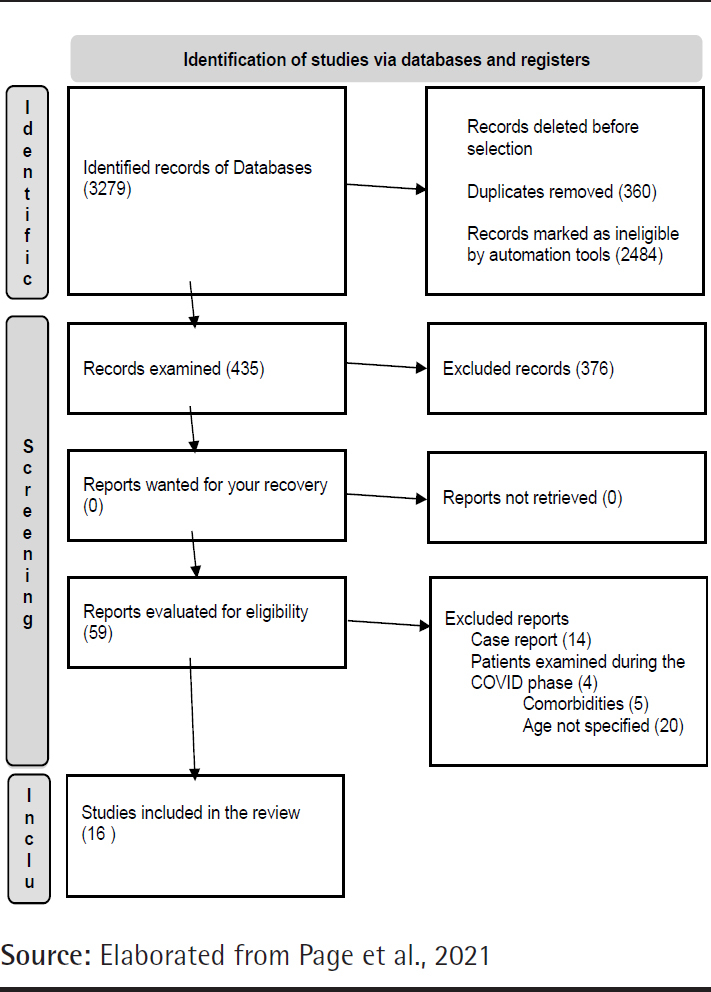
PRISMA 2020 Flow Diagram
RESULTS
16 articles were analyzed. In this regard, the predomi-nant language was English and the keywords found most frequently were "COVID-19" and "SARS-CoV-2". Most of the investigations used a qualitative approach with a descriptive and cross-sectional design.
The selection of the sample was non-probabilistic in all the articles, and it comprised from 4 to more than 100 participants. On the other hand, the age range was from 18 years onwards and the patients were predominantly male.
Regarding post-COVID cognitive manifestations, the lit-erature reported cognitive impairment, memory problems, and executive dysfunction. This is detailed in Table 1.
Table 1.
Neurological sequelae in post-COVID patients
|
Neurological sequelae | |||
|---|---|---|---|
| Author | Year | Sample | Post-COVID manifestations |
| Besteher et al. | 2022 | 17 women and 13 men with an average age of 47 years |
Cognitive deficits |
| Checa et al. | 2022 | 29 men and 21 women aged 51 and 65 | 82.35% (n=14) presented cognitive impairment |
| Calabria et al. |
2022 | 49 men and 87 women from 20 to 88 years of age |
Executive dysfunction increased steadily after infection. |
| García-Sánchez et al. | 2022 | 22 men and 41 women from 22 to 78 years old |
The most commonly affected domain was attention (61.9% of the sample). |
| Hellgren et al. |
2021 | 28 men and 7 women from 51 to 66 years old |
Sixteen of 35 patients (46%) showed cognitive impairment; 6 of these (17%) had mild/moderate cognitive impairment. |
| Ortelli et al. | 2021 | 10 men and 1 woman from 56 to 80 years old |
Cognitive fatigue and executive dysfunction. |
| Pinna et al. | 2021 | 29 men and 21 women with an average age of 60 years |
Short-term memory impairment. |
| Pistarini et al. | 2021 | 13 men and 7 women over 50 years of age |
Impairment of executive functions, short and long term memory, visuospatial abilities, abstraction and orientation. |
Regarding post-COVID neurological manifestations, cerebrovascular events, seizures and neuromuscular fatigue were found. This is visible in Table 2.
Table 2.
Neurological sequelae in post-COVID patients
| Neurological sequelae | |||
| Author | Year | Sample | Post-COVID manifestations |
|---|---|---|---|
| Avula et al. | 2020 | Three women aged 83, 80 and 88 and a 73-year-old man |
Presence of cerebrovascular event. |
| Besteher et al. |
2022 | 17 women and 13 men with an average age of 47 years |
Increased gray matter in patients with prolonged COVID. |
| Birberg et al. | 2022 | 82 men and 54 women with an average age of 57 years |
Significantly lower scores on late and immediate memory tests. Attention deficits, psychomotor speed, verbal fluency. |
| Dressing et al. | 2022 | 17 women and 13 men with an average age of 53 years |
Microembolic subacute cortical infarction in the left occipital lobe in 1 patient (65-year-old man) and mild microangiopathic changes were present in a 61-year-old patient. |
| Krishnan et al. | 2022 | 36 women and 4 men with an average age of 44 years. |
Impairment of cognitive domains. |
| Langavant et al. |
2021 | 19 men and 7 women with a mean age of 58 years |
Presence of neurological disorders, encephalitis, encephalopathy, cerebrovascular events and Guillain-Barré syndrome. |
| Ortelli et al. | 2021 | 10 men and 1 woman from 56 to 80 years old |
Neuromuscular fatigue. Flaccid tetraparesis, muscle atrophy, areflexia, anosmia, sensory disturbances. |
| Pinna et al. | 2021 | 29 men and 21 women with an average age of 60 years |
Presence of seizures, hypoxic ischemic brain injury. |
Lastly, Table 3 contains the neuropsychological and neu-ropsychiatric manifestations, among which fatigue, depres-sion and anxiety were found.
Table 3.
Neuropsychological and neuropsychiatric sequelae in post-COVID patients
| Neuropsychological and neuropsychiatric sequelae | |||
|---|---|---|---|
| Author | Year | Sample | Post-COVID Post-COVID manifestations |
| Ahmed et al. | 2021 | 84 men and 98 women with an average age of 46 years |
Poor sleep quality, probable PTSD, somatization, anxiety, anger-hostility, phobia-anxiety, obsession-compulsion |
| Besteher et al. | 2022 | 17 women and 13 men with an average age of 47 years |
Fatigue and depression. |
| Calabria et al. | 2022 | 49 men and 87 women from 20 to 88 years of age |
82.3% of people reported clinically significant levels of fatigue. Depressive and anxiety symptoms were less prevalent with 23.5% and 35.3% of patients reaching significant levels, respectively. Apathy increased steadily after infection. |
| Cattarinussi et al. | 2022 | 33 men and 46 women with an average age of 42 years. |
The most reported symptoms were fatigue (71.2%), anxiety and depression |
| Dressing et al. | 2022 | 17 women and 13 men with an average age of 53 years |
All the patients complained of difficulties with attention, memory, and multitasking skills. Additionally, 24 of 31 (77%) complained of fatigue. |
| Hellgren et al. | 2021 | 28 men and 7 women from 51 to 66 years old |
Clinically significant fatigue was reported by 25 patients (74%). Depression, anxiety. |
| Krishnan et al. | 2022 | 36 women and 4 men with an average age of 44 years. |
Anxiety, depression and recurrent fatigue. |
| Author | Year | Sample | Post-COVID sequelae |
| Lamontagne et al. | 2021 | 29 women and 21 men aged 18 to 49 years |
Persistent brain fog, depression, anxiety, and anhedonia. |
| Ortelli et al. | 2021 | 10 men and 1 woman from 56 to 80 years old |
Apathy. |
| Pinna et al. | 2021 | 29 men and 21 women with an average age of 60 years |
Altered mental status, headaches. |
DISCUSSION
The SARS-CoV-2 virus (responsible for the current pan-demic) is generating multiple effects at the neurological level, which has aroused great interest due to uncertainty about the scope and impact of this pathogen on the central nervous system. Therefore, the objective of this study was to classify the neurological sequelae of COVID-19 in the adult population:
Neurocognitive sequelae
Cognitive dysfunction is one of the most frequent-ly reported mental health problems and can affect more than half of post-COVID patients even six months after hospital discharge (Estrada et al., 2021). In this regard, it was found that the patients presented executive dys-function, memory problems and cognitive deficit, which is consistent with the findings made by Altuna et al (2022) and Crivelli et al (2021). It should be noted that more and more studies are reporting a type of dysfunction at the level of processing and difficulties in recalling informa-tion, which has a functional impact on the activities of daily living of patients recovered from COVID 19. What is responsible for this effect is called "mental fog", this being one of the main neurocognitive sequelae that has been described as slow thinking, difficulty concentrating and the presence of episodes of confusion Pattnaik et al (2021).
It is worth mentioning that these alterations can arise thanks to 3 fundamental variables (Mata, 2021):
1) How strong was the COVID-19 disease.
2) Previous health conditions of each particular patient.
3) Areas of opportunity for care and clinical follow-up.
Therefore, it is still too early to describe the full scope that this infection can have, since almost three years after the start of the COVID 19 pandemic, the scope is evident from a neurocognitive and clinical perspective.
Neurological sequelae
According to Zambrano et al. (2022) neurological se-quelae are one of the main complications present in post- COVID-19 patients and includes a wide variety of symp-toms, although these could be due to the accumulation of molecular and cellular damage typical of the aging process (WHO, 2021). as well as different conditions of social vul-nerability that the population faces, such as lack of person-al or economic resources and lack of access to protection policies (Guerrero and Yépez, 2015).
However, in the present review, it was possible to find encephalitis, encephalopathy, sensory alterations, anosmia, Guillain-Barré syndrome, cerebrovascular events, among others. This is consistent with Da Silva (2020), Rahman et al. (2020), Sinanovic (2021) and Yadav et al. (2020), who reported post-COVID-19 patients with headaches, dizzi-ness, encephalopathy, delirium, seizures, hypoxia, loss of consciousness, coma, paralysis, and/or stroke.
Neuropsychological and neuropsychiatrie sequelae
Manríquez et al (2021) have pointed out that there is no single and clear pattern in the neuropsychological func-tioning of patients, which is why it is common to find a wide variety of symptoms. In the selected samples, anxiety problems, delusions, hallucinations, depression and mental fog were observed; however, these could also be due to ex-posure to other factors during the pandemic, such as lock-down and economic or social problems (Ziyad et al., 2022).
Regarding the limitations of this study, it is worth noting that no comparison was made between pre and post COVID-19 patients. Similarly, although neurological and psychiatric manifestations affect both symptomatic and asymptomatic people (Da Silva, 2020). Possible dif-ferences between the two groups were not considered due to the lack of scientific evidence, in addition, other vari-ables such as vaccination, time of confinement, severity of COVID-19, variants of SARS-CoV-2, etc. were not tak-en into account. Therefore, for future research, it will be necessary to present a global vision of COVID-19 in the field of neuroinfection contemplating the human being as a social and integral being in all aspects of psychologi-cal and anthropological functioning, since for Carod-Artal (2020) in specific tropical regions, co-circulation can oc-cur of SARS-CoV-2 with the dengue, chikungunya, Zika or Japanese encephalitis viruses, which could generate some confusion in symptoms and reach vulnerable populations or add other complementary symptoms compared to those already reported for SARS-CoV-2.
CONCLUSION
Severe cases of COVID-19 have a high risk of develop-ing sequelae and alterations in different areas of the patient's overall functioning (cognitive, emotional, physical and motor), which frame difficulties in recovery or even the appearance of new pathologies. The sequelae reported by the patients classified as psychiatric symptoms are: depression, anxiety, and even paranoid disorder; Neurological symptoms such as recurrent headaches and loss of cognitive abilities (memory, attention and perception of the world) have also been found, and in some cases patients describe a type of mental fog that makes it impossible for them to carry out their daily lives, within their recovery with some global deficits.
In addition to this, the pandemic has greatly affected the elderly population, who are the most vulnerable due to underlying diseases, or due to the wear and tear of the organic and/or immune system; In addition, individual and socioeconomic differences mark a huge gap in medical and hospital care, where respiratory and bodily complications can be treated at different times, given that the sanitary collapse in health-providing institutions has been evident within the waves of infections.
The challenges that neuropsychology faces involve pa-tient care and rehabilitation strategies. From a global per-spective, it is essential to implement strategies that promote the mental health and quality of life of the person in recov-ery and of the families who directly or indirectly They have been harmed with a contagion.
Studies included in this review.
REFERENCIAS
Studies included in this review.
- 1.Akinci M., Sánchez-Benavides G., Brugulat-Serrat A., Peña C., Palpatzis, Shekari M., Deulofeu C., Fuentes S., Salvadó G., Gonzalez J., Suarez M., Miguillon C., Fauria K., Molinuevo J., Domingo j., & Arenaza E. Subjective cognitive decline and anxious/de- pressive symptoms during the COVID-19 pandemic: what is the role of stress perception, stress resilience, and β-amyloid? Alzheimer's Research & Therapy. https://doi.org/10.1186/s13195-022-01068-7. 2022;1(4):1–26. doi: 10.1186/s13195-022-01068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avula A., Nalleballe K., Narula N., Sapozhnikov S., Dandu V., Toom S., Glaser A., & Elsayegh D. COVID-19 presenting as stroke. https://doi.org/10.1016/j.bbi.2020.04.077. Brain, Behavior, and Immunity. 2020;87(3):115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Besteher B. M., Machnik M., Troll A., Toepffer A., Zere- kidze T., Rocktaschel C., Heller Z., Kikinis S., Brodoehl K., Finke P., Reuken N., Opel A., Stallmach C., Gaser M., y Walter M. Larger gray matter volumes in neuropsychiatric long-COVID síndrome. https://doi.org/10.1016/j.psy-chres.2022.114836. Psychia-try Research. 2022;317:1–8. doi: 10.1016/j.psychres.2022.114836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Besteher B., Machinik M., Troll M., Toepffer A., Zere- kidze A., Roctaschel T., Heller C., Kikinis Z., Brodoehl S., Finke K., Reunken P., Opel N., Stallmach A., Gas-er C., & Walter M. Larger gray matter volumes in neuropsychiatric long-COVID syndrome. https://doi.org/10.1016/j.psy-chres.2022.114836. Psychiatry Research. 2022;3(16):134–151. doi: 10.1016/j.psychres.2022.114836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birberg U., Andersson A., Lindh M., Hellgren L., Di- vanoglou A., & Levi R. Neurocognitive defi-cits in COVID-19 patients five months after discharge from hospital. Neuropsychological Rehabilitation. 2022 doi: 10.1080/09602011.2022.2125020. DOI: 10.1080/09602011.2022.2125020. [DOI] [PubMed] [Google Scholar]
- 6.Calabria M., García-Sánchez C., Grunden N., Pons C., Arroyo J., Arroyo B., Estévez C., Belvís R., Morollón N., Vera J., Mur I., Pomar V., y Domingo P. https://doi.org/10.1007/s00415-022-11141-8. Journal of Neurology. 2022;269:3990–3999. doi: 10.1007/s00415-022-11141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cattarinussi G., Miola S., Trevisan N., Valeggia S., Tra- marin E., Mucignat C., Morra F., Minerva M., Librizzi C., Bordin A., Causin F., Ottaviano G., Antonini A., Sambataro F., y Manara R. Altered brain region-al homogeneity is associated with depressive symptoms in COVID-19. https://doi.org/10.1016/j.jad.2022.06.061. Journal of Affective Disorders. 2022;313:36–42. doi: 10.1016/j.jad.2022.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Checa A., Navas E., Valencia V., y Alcívar J. Cognitive impairment in people with COVID-19 with mild-moderate symptoms in Ecuador. https://doi.org/10.24875/rmn.21000060 Revista Mex-icana de Neurociencia. 2022;23(4):125–129. [Google Scholar]
- 9.Conway S., Healy B., Zurawski J., Severson C., Kaplan T., Stazzone L., Galetta K., Chitnis T., & Houtchens M. COVID-19 severity is associated with worsened neurological outcomes in multiple sclerosis and relat-ed disorders. Multiple Sclreosis. 2022;63(56):1039–1051. doi: 10.1016/j.msard.2022.103946. DOI:https://doi.org/10.1016/j.msard.2022.103946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dressing A., Bormann T., Blazhenets G., Schroeter N., Walter L., Thurow J., August D., Hilger H., Stete K., Gerstacker K., Arndt S., Rau A., Urbach H., Rieg S., Wagner D., Weiller C., Meyer P., Hosp J. Neu-ropsychologic Profiles and Cerebral Glucose Metabolism in Neurocognitive Long COVID Syndrome. https://doi.org/10.2967/jnumed.121.262677. The Journal of Nuclear Medicine. 2022;63(7):1058–1063. doi: 10.2967/jnumed.121.262677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernández L., Garcia C., Martins M., Figueredo I., Diaz M., Facucho J., Carreno J., Vieira C., Oliveira C., Luis A., & Maia T. Prevalence of the Most Frequent Neuropsychiatric Diagnoses in Hospitalized SARS-CoV-2 Patients Evaluated by Liaison Psychiatry: Cross-Section-al Study. Acta medica portuguesa. 2022;35(38):1143–1159. doi: 10.20344/amp.16410. DOI: https://doi.org/10.20344/amp.16410 . [DOI] [PubMed] [Google Scholar]
- 12.García-Sánchez C., Calabria M., Grunden N., Pons, C. Arroyo J., Gómez-Anson B., Lleó A., Alcolea D., Belvís R., Morollón N., Mur I., Pomar V., y Domingo P. Neuropsychological deficits in patients with cognitive complaints after COVID-19. https://doi.org/10.1002/e2508. Brain and Behavior. 2021;12(3):1–11. doi: 10.1002/brb3.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hellgren L., Thornberg U., Samuelsson K., Levi R., Di-vanoglou A., y Blystad I. Brain MRI and neu-ropsychological findings at long-term follow-up after COVID-19 hospitalisation: an observational cohort study. https://doi:10.1136/bmjop-en-2021-055164. BMJ Open. 2021;11:1–9. doi: 10.1136/bmjopen-2021-055164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iqbal Y., Alabdulla M., Kumar R., Latoo J., Albrahim S., Wadoo O., & Haddad O. Characteristics of 100 consecutive patients with COVID-19 referred to consul-tation-liaison psychiatry services in Qatar: A compari-son of patients with delirium versus other psychiatric diagnoses. Qatar medicine journal. 2022;3(28):358–367. doi: 10.5339/qmj.2022.28. DOI: 10.5339/qmj.2022.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krishnan K. Miller A., Reiter K., Bonner A.. Neurocognitive Profiles in Patients With Persisting Cog-nitive Symptoms Associated With COVID-19. https://doi.org/10.1093/arclin/acac004. Archives of Clinical Neuropsychology. 2022;37(45):729–737. doi: 10.1093/arclin/acac004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lamontagne S., Winters M., Pizzagalli D., & Olmstead M. Post-acute sequelae of COVID-19: Evidence of mood & cognitive impairment. https://doi.org/10.1016/j.bbih.2021.100347. Brain, Behavior, & Immunity - Health. 2021;1(7):4–23. doi: 10.1016/j.bbih.2021.100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langavant L., Petit A., Nguyen T., Gendre J., Abdelhedi A., Djellaoui L., Seddik L., Lim F., Faugeras H., Salhi A., Wahab L., Fechtenbaum A., Dormeuil H., Hosseini, K., Youssov G., Fénelon B., Bapst P., Brugières T., Tuil-ier E., Kalsoum M., Matignon J., Oniszczuk S., Gallien W., Vindrios G., Melica A., Scain R., Esser L., Rostain C., Guillaud G., Dubos-Lascu N., Saada H., Guillet M., Khellaf B., Bardel S., Ayache J., Lefaucheur J., Paw- lotsky S., Fourati A., Bachoud-Lévi A. Clinical description of the broad range of neurological presen-tations of COVID-19: A retrospective case series. https://doi.org/10.1016/j.neurol.2021.01.004. Revue Neurologique. 2021;3(17):275–282. doi: 10.1016/j.neurol.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ortelli P., Ferrazzoli D., Sebastianelli L., Engl M., Ro- manello R., Nardone R., Bonini I., Koch G., Saltuari, L., Quartarone A., Oliviero A., Kofler M.y, Versace V. Neuropsychological and neurophysiological cor-relates of fatigue in post-acute patients with neurolog-ical manifestations of COVID-19: Insights into a chal-lenging symptom. https://doi.org/m1016/jjns.2020.117271. Journal of the Neurological Sciences. 2021;420:1–9. doi: 10.1016/j.jns.2020.117271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinna P., Grewal P., Hall J., Tavarez T., Dafer R., Garg N., Pellack D., Asthana A., Fegan K., Patel V., Conners J., John S., & Da Silva I. Neurological mani-festations and COVID-19: Experiences from a tertiary care center at the Frontline. https://doi.org/10.1016/j.jns.2020.116969. Journal of the neurologi-cal sciences. 2021;15(41):116–139. doi: 10.1016/j.jns.2020.116969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pistarini C., Fiabane, E.,Houdayer E., Vassallo C., Mane-ra M. y, Alemanno F. Cognitive and Emotional Disturbances Due to COVID-19: An Exploratory Study in the Rehabilitation Setting. https://doi.org/10.3389/fneur.2021.643646. Frontiers in Neurology. 2021;12:1–8. doi: 10.3389/fneur.2021.643646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santos C., Nuradin N., Joplin C., Leigh A., Burke R., Rome R., McCall J., & Raines M. Risk factors for delirium among SARS-CoV-2 positive veterans. https://doi.or-g/10.1016/j.psychres.2021.114375. Psychiatry Research. 2022;23(34):1114–1136. doi: 10.1016/j.psychres.2021.114375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Serrano P., Garzón F., Casado I., Ollero A., Minguez A., Iglesias M., Baena P., Sanchez V., Sanchez R., Calle-jon J., Esteves C., Galeano B., Romero J., Sobrino B., Arrabal C., Oliver B., Muñoz L., Requena N., Gonzalez, M., Estivill G., Suarez J., Lundahl N., Pons G., Reyes J., & Rodriguez F. The cognitive and psychiatric subacute impairment in severe COVID-19. https://doi.org/10.1038/s41598-022-07559-9. Scientific Reports. 2022;3(2):35–63. doi: 10.1038/s41598-022-07559-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soriano M., Anschau F., Kopittke L., Frizzo M., Delfi-no P., & Teixeira A. Frequency and burden of neurological manifestations upon hospital presentation in COVID-19 patients: Findings from a large Brazilian cohort. https://doi.org/10.1016/j.jns.2022.120485. Neurological Sciences. 2022;3(5):134–156. doi: 10.1016/j.jns.2022.120485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Abenza-Abidúa M., Ramírez Prieto M., Moreno-Za- baleta R., Arenas-Valls L., Salvador-Maya M., Alga-ra-Lucas C., Moreno-Arrones B., Sánchez-Cordon B., Ojeda-Ruiz de Luna J., Jimeno-Montero C., Navacerra- da-Barrero F., Borrue-Fernández C., Malmierca-Corral E., Ruiz-Seco P., González-Ruano P., Palmí-Cortes I., Fernández-Travieso J., Mata-Álvarez de Santillana M., Almarcha-Menargues M., Pérez-López C. Neurological complications in critical patients with COVID-19. https://doi.or-g/10.1016/j.nrleng.2020.07.012. Neurología. 2020;35(9):621–627. doi: 10.1016/j.nrleng.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Aguilar F. y, López A. COVID-19: manifestacio-nes neurológicas más frecuentes y poco diagnosticadas. https://dx.doi.org/10.35366/103087 Plasticidad y Restauración Neurológica. 2021;8(2):89–95. [Google Scholar]
- •.Altuna M., Sánchez M. y, Lleó A. Cognitive symptoms after COVID-19. https://doi.org/10.1016/j.neurop.2021.10.005. Neurology Perspectives. 2022;1:16–24. doi: 10.1016/j.neurop.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Bernardo L. Consecuencias neurológicas de la COVID-19 y la importancia de la neurorrehabilitación: revisión bibliográfica [Tesis de fin de grado, Universi-dad Complutense de Madrid] https://eprints.ucm.es/id/eprint/69491/1/MARTIN-BERNARDOMOYALTFG.pdf 2021 [Google Scholar]
- •.Carod-Artal F. Complicaciones neurológicas por coronavirus y COVID-19. Neurología. https://doi.org/10.33588/rn.7009.2020179. 2020;70(9):311–322. doi: 10.33588/rn.7009.2020179. [DOI] [PubMed] [Google Scholar]
- •.Crivelli L., Calandri I., Corvalán N., Carello M., Keller G., Martínez C., Arruabarrena M. y, Allegri R. Cognitive consequences of COVID-19: results of a co-hort study from South America. https://doi.org/10.1590/0004-282X-ANP-2021-0320. Arquivos de Neuro-Psi-quiatria. 2021;80(3):240–247. doi: 10.1590/0004-282X-ANP-2021-0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Da Silva C. Neurological and neurocognitive al-terations by COVID-19 Interaction. https://doi.org/10.24016/2020 2020;6(3):e181. [Google Scholar]
- •.Desforges M., Coupanec A., Dubeau P., Bourgouin A., Lajoie L., Dubé M., Talbot P. Human Corona- viruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System Viruses. https://doi.org/10.3390/v12010014. National center for biotechnology information. 2019;12(1):14–21. doi: 10.3390/v12010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Estrada H., Cervantes G. y, Rodriguez M. Capí-tulo 5: Deterioro cognitivo. En Halabe, J., Robledo Z. y Fajado, G. (Coords.), Síndrome post-COVID'-19. Editorial Médica Panamericana 2021 [Google Scholar]
- •.García J., Pérez M. y, Bender J. COVID-19. neu-rological manifestations. https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=95663 Sancti Spiritus Medical Ga-zette. 2020;22(1):1–6. [Google Scholar]
- •.Guerrero N. y, Yépez M. Factores asociados a la vulnerabilidad del adulto mayor con alteraciones de salud. http://www.scielo.org.co/pdf/reus/v17n1/v17n1a11.pdf Universidad y Salud. 2015;17(1):121–131. [Google Scholar]
- •.Han Y., Yuan K., Wang Z., Liu W., Lu Z., Liu L., Shi L., Yan W., Yuan J., Li J., Shi J., Liu Z., Wang G., Kosten T., Bao Y. y, Lu L. Neuropsychiatric manifestations of COVID-19-19, potential neurotropic mechanisms, and therapeutic interventions. https://doi.org/10.1038/s41398-021-01629-8. Translational Psychiatry. 2021;11:1–20. doi: 10.1038/s41398-021-01629-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.He Y., Yu R. y, Ren J. The correlation between psychiatric disorders and COVID-19: a narrative re-view. https://doi.org/10.24869/psyd.2021.76. Psychiatria Danubina. 2021;33(1):76–85. doi: 10.24869/psyd.2021.76. [DOI] [PubMed] [Google Scholar]
- •.Hu J., Jolkkonen J., Zhao C. Neurotropism of SARS-CoV-2 and its neuropathological alterations: Similarities with other coronaviruses. https://doi.org/10.1016/j.neubiorev.2020.10.012. Neuroscience & Biobehavioral Reviews. 2020;119(2):184–193. doi: 10.1016/j.neubiorev.2020.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Kumar S., Veldhuis A. y, Malhotra T. Neuropsy-chiatric and Cognitive Sequelae of COVID-19. https://doi.org/10.3389/fpsyg.2021.577529. Fron-tiers in Psychology. 2021;12:1–6. doi: 10.3389/fpsyg.2021.577529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.León R., Bender del Busto J. y, Velázquez L. Afec-tación del sistema nervioso por la COVID-19. http://www.revistaccuba.cu/index.php/revacc/article/view/760/796 Anales de la Academia de Ciencias de Cuba. 2020;10(2):1–4. [Google Scholar]
- •.Manriquez L., Saldaña C., Gómez R., Enríquez K., Aran-da S., García R. y, Martinez F. Cuadernos de Neuropsicología. https://www.researchga-te.net/publication/358281492 2021;15(3):37–53. [Google Scholar]
- •.Mata M. Afectación de las funciones cognitivas, una de las molestias post-COVID. http://www.gaceta.udg.mx/afectacion-de-las-funciones-cog- nitivas-una-de-las-molestias-post-COVID/ Gaceta UdeG. 2021 [Google Scholar]
- •.Mattioli F., Stampatori C., Righetti F., Sala E., Toma-si C. y, De Palma G. Neurological and cognitive sequelae of COVID-19-19: a four month follow-up. https://doi.org/10.1007/s00415-021-10579-6. Journal of Neurology. 2021;268:4422–4428. doi: 10.1007/s00415-021-10579-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Mayo Clinic. Enfermedad del coronavirus 2019 (COVID-19) https://www.mayoclinic.org/es-es/dis-eases-conditions/coronavirus/symptoms-causes/syc-20479963?page=0&citems=10&p=1 2021 [Google Scholar]
- •.Médica Sur. ¿Cuáles son los síntomas del COVID 19? https://medicasur.com.mx/en_mx/ms/Cuales_son_los_sintomas_de_COVID-19 2020 [Google Scholar]
- •.Merino J., Macho-González A., Benedi J. y, González M. Neurological manifestations of COVID-19-19 in patients: from pathophysiology to therapy. https://doi.org/10.1007/s10072-021-05505-7. Neurolo-gical Sciences. 2021;42:4867–4879. doi: 10.1007/s10072-021-05505-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Organización Mundial de la Salud, corp-author. Coronavirus. https://www.who.int/es/health-topics/coronavirus#ta-b=tab_3 2020 [Google Scholar]
- •.Organización Mundial de la Salud, corp-author. Envejecimien-to y Salud. https://www.who.int/es/news-room/fact-sheets/detail/ageing-and-health 2021 [Google Scholar]
- •.Page M., McKenzie J., Bossuyt P., Boutron I., Hoffman T., Mulrow C., Shamseer L., Tetzlaff J., Akl E., Brennan S., Chou R., Glanville J., Grimshaw J., Hróbjartsson A., Lalu M., Li T., Loder E., Mayo E., McDonald S., McGuin- ness L., Moher D. Declaración PRISMA 2020: una guía actualizada para la publicación de revisiones sistemáticas. https://doi.org/10.1016/j.rcesp.2021.06.016. Revista Española de Cardiología. 2021;79(4):790–799. doi: 10.1016/j.rec.2021.07.010. [DOI] [PubMed] [Google Scholar]
- •.Quiroz V. y, Amarales C. Compromiso neurológi- co en infección por COVID-19 en pacientes pediátricos. https://dx.doi.org/10.32641/rchped.v91i4.2526. Revista Chilena de Pediatría. 2020;91(4):614–619. doi: 10.32641/rchped.vi91i4.2526. [DOI] [PubMed] [Google Scholar]
- •.Rahman A., Niloofa R., De Zoysa I., Cooray A., Ka-riyawasam J. y, Seneviratne S. Neurolog-ical manifestations in COVID-19: A narrative re-view. https://doi.org/10.1177/2050312120957925. Sage Open Medicine. 2020;8:1–10. doi: 10.1177/2050312120957925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Riordan P., Stika M., Goldberg J. y, Drzewiecki M. COVID-19 and clinical neuropsychology: A re-view of neuropsychological literature on acute and chronic pulmonary disease. https://doi.org/10.1080/13854046.2020.1810325. The Clinical Neuropsychol-ogist. 2020;34(7):1480–1497. doi: 10.1080/13854046.2020.1810325. [DOI] [PubMed] [Google Scholar]
- •.Ritchie H., Mathieu E., Rodés-Guirao L., Appel C., Giattino C., Ortiz-Ospina E., Hasell J., Macdonald B., Beltekian D., & Roser M. Coronavirus Pandemic (COVID-19) https://ourworldindata.org/coronavirus 2022 [Google Scholar]
- •.Sasannejad C., Ely E., y Lahiri S. Long-term cognitive impairment after acute respiratory distress syndrome: a review of clinical impact and pathophys-iological mechanisms. https://doi.org/10.1186/s13054-019-2626-z. Crit Care. 2019;23:352. doi: 10.1186/s13054-019-2626-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Sinanović O. Long-term neuropsychiatric con-sequences of Sars-Cov infections. https://www.researchgate.net/publica-tion/351732940_Long-Term_neuropsychiatric_conse-quences_of_sars-cov_infections. Psychiatria Danubina. 2021;33(3):74–82. [PubMed] [Google Scholar]
- •.Wu C., Chen X., Cai Y., Xia J., Zhou, Xing, Xu S., Huang H., Zhang L., Zhou X., Xia J., Zhang Y., Song J., Wang S., Chao Y., Yang Z., Xu J., Zhou X., Chen D., Xiong W., Xu L., Zhou F., Jiang J., Bai C., Zheng J., Song Y. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Corona-virus Disease 2019 Pneumonia in Wuhan, China. JAMA International Medical. 2020;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Yadav R., Kumar D., Kumar P. y, Kumar R. Neu-rological involvement in COVID-19 patients: A narrative review. https://doi.org/10.1055/s-0040-1716423. Journal of Neurosciences in Rural Practice. 2020;11(4):526–529. doi: 10.1055/s-0040-1716423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Zambrano D., Farfan L., Briones C. COVID-19 a largo plazo, consecuencias musculares, neurológicas y respiratorias. https://doi.org/10.37811/cl_rcm.v6i1.1800p4311Vindegaar Ciencia Latina Revista Científica Mul-tidisciplinar. 2022;6(1):4298–4311. [Google Scholar]
- •.Ziyad A. Mental health in people with COVID-19. http://dx.doi.org/10.1136/bmj.o415. BMJ. 2022;376:1. doi: 10.1136/bmj.o415. [DOI] [PubMed] [Google Scholar]
- •.Ziyad A., Yan X. y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. https://doi.org/10.1038/s41586-021-03553-9. Nature. 2021;596:259–283. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]


