Abstract
Background.
Stigma associated with psychological problems is a major concern that negatively affects people living with different symptomatology, sometimes with serious consequences for their health. The principal purpose of this paper was to carry out an updated systematic review to explore the relationship between the stigma associated with mental health problems and the risk of suicide in the clinical population, as well as to study the variables involved in this relationship.
Method.
A search was carried out in the PsycInfo, Pubmed and Scopus databases, using keywords related to stigma, suicide, and limiting the studies to clinical samples. The search included articles in English and Spanish from January 2012 to December 2020.
Results.
A total of 12 articles met the inclusion criteria and were selected for analysis. The results suggest that increased self-stigma toward mental health problems is associated with increased risk of suicide in clinical population. Also, variables involved in this relationship are suggested, such as depression, hopelessness, loss of vital sense, unemployment or decrease of support networks.
Conclusion.
The stigma associated with mental health problems could be a potential therapeutic target for reducing the risk of suicide in the clinical population. Exhaustive studies, with control groups random assignment, and more heterogeneous samples are necessary to know the phenomenon in greater depth.
Keywords: Stigma, suicides, suicidal risk, mental disorders, mental health.
IMPLICACIONES DEL ESTIGMA HACIA LOS PROBLEMAS DE SALUD MENTAL EN EL RIESGO DE SUICIDIO EN PERSONAS CON PROBLEMAS DE SALUD MENTAL: UNA REVISIÓN SISTEMÁTICA
Introducción.
El estigma asociado a los problemas psicológicos es una cuestión preocupante que afecta negativamente a las personas que conviven con diferentes sinto- matologías, en ocasiones con graves consecuencias para su salud. El objetivo principal de este trabajo fue realizar una revisión sistemática actualizada para explorar la relación entre el estigma asociado a los problemas de salud mental y el riesgo de suicidio en la población clínica, así como estudiar las variables implicadas en esta relación.
Método.
Se realizó una búsqueda en las bases de datos PsycInfo, Pubmed y Scopus, utilizando palabras clave relacionadas con el estigma, el suicidio, y limitando los estudios a muestras clínicas. La búsqueda incluyó artículos en inglés y español desde enero de 2012 hasta diciembre de 2020.
Resultados.
Un total de 12 artículos cumplieron los criterios de inclusión y fueron seleccionados para el análisis. Los resultados sugieren que el aumento del auto estigma hacia los problemas de salud mental se asocia con un mayor riesgo de suicidio en población clínica. Asimismo, se sugieren variables implicadas en esta relación, como la depresión, la desesperanza, la pérdida de sentido vital, el desempleo o la disminución de las redes de apoyo.
Conclusiones.
El estigma asociado a los problemas de salud mental podría ser una potencial diana terapéutica para reducir el riesgo de suicidio en la población clínica. Son necesarios estudios exhaustivos, con aleatorización, grupos de control, y muestras más heterogéneas para conocer el fenómeno en mayor profundidad.
INTRODUCTION
Over time, people with mental health problems have been misunderstood and subjected to discrimination by the general population, and different types of stigma associated with these kind of problems can be distinguished. A classic definition of this phenomenon is that of Erving Goffman in his Stigma: Notes on the Management of Spoiled Identity (1). Here he argues that stigma is an attribute that is inferred on a person, one that is extremely devaluing and would define him or her as deviant, limited and undesirable.
Stigma could thus be operationalised as a label attached to a group, highlighting a number of negative differences. Consequently, these differences create two separate groups ("them" and "us"). This leads to a loss of status and discrimination (2,3). In other words, stigma is a process composed of the recognition of the person as "mentally ill", the activation of stereotypes and, finally, the emergence of prejudice or discrimination towards the person (4).
Recently, Fox et al. (5), suggest the "Mental Illness Stigma Framework" (MISF), an explanatory theoretical framework in which they differentiate between stigmatizing and stigmatized perspectives, to refer to the different types of stigma. The stigmatizing point of view includes structural stigma, which refers to how public and private entities discriminate against people with mental health problems (6,7), as well as the social or public stigma, referring to how society embodies stereotypes and acts negatively towards these people (7,8). On the other hand, from the stigmatized perspective, it is possible to distinguish internalized stigma (IS), understood as the process of internalizing stigma in a particular socio-cultural context (7). This perspective also comprises experienced stigma (ES), defined as directly suffering from experiences of discrimination or rejection (1,9), and the anticipated stigma (AS), described as stereotypes, prejudices and discrimination that a person with mental health problems expects in the future (10). In addition, these authors point out yet another concept as a link between both perspectives, the perceived stigma (PS), which manifests as perceptions of social beliefs, feelings and behaviours towards people with mental health problems (5).
The other variable whose definition seems relevant to the present research is that of suicide. De Leo et al. (11) describe it as an act with fatal consequences, which the person who carries it out initiates with the purpose of death. But as with stigma, suicide is a complicated term to define and has multiple nomenclatures for different phenomena. In this regard, Van Orden et al. (12) divide suicidal tendencies into suicidal ideation (thoughts), suicidal communications and suicidal behaviours. Furthermore, these behaviours would be self-initiated, and may vary in the presence or absence of intent to die. These authors report that suicide attempts would have a number of defining characteristics. They are potentially harmful, self-initiated actions, with intent to die, but without fatal consequences. When these consequences are fatal, then it is called suicide. The authors note in their study that both suicidal ideation and non-fatal attempts are much more common than suicide deaths. They point out that theories to date do not take this detail into account and view the phenomenon of suicide as a unitary construct. They argue that, if there is no clear difference between suicidal thoughts, non-fatal suicide attempts and suicide deaths, theories to date are inconsistent.
To operationalise the construct of suicide risk, they propose the Interpersonal Theory of Suicidal Behaviour (12). This theory is based on three primary constructs. Two of them are related to the desire to die (frustrated belongingness and perceived burden) and the other is related to the acquired capacity to commit the suicidal act. In their theory, the authors argue that the need for belonging is a central focus for the development of suicidal desires. Furthermore, they comment that this frustrated belongingness is a multidimensional construct. In the model, it would be a variable with two subordinate factors: loneliness and lack of reciprocal care. As for perceived burden, the authors argue that it is a common factor generated by other suicide risk factors such as family conflict, unemployment and physical illness. In this theory, perceived burden comprises two dimensions of interpersonal functioning, the belief that the self is so flawed that it is a burden to others, and self-hating cognitions. Lastly, for the suicidal act to be completed, the conjunction of frustrated belonging and perceived burden with the acquired capacity for suicide has to occur (12). This means having a certain loss of fear of actions that end in suicide, and a high tolerance for physical pain.
Stigma in all its forms can have negative effects affecting the recovery (13), self-esteem (14), quality of life and well-being (15) and even going so far as to increase the risk of suicide of the people with psychological problems (16). Different studies suggest that at least 87% to 90% of people who die by suicide may have had some kind of previous psychological problem (17). Moreover, the literature has identified three ways in which stigma contributes to suicide. The first relates to the coping theory of stress. Under this theory, if it were to exceed the individual's coping capacities, stigma would be a stressor that could lead to social isolation, hopelessness and negative emotions. The second is that stigma contributes to the social isolation of people with mental health problems, which is a recognised risk factor for suicide (18). Lastly, selfstigma has been shown to be a potent barrier to seeking professional help (19,20). These findings support the theory that stigma is associated with a higher risk of suicide. Although they do not prove that the relationship is real, they provide a basis for future research in this area.
In summary, stigma is a complex and frequent phenomenon that people with mental health problems have to deal with on a daily basis. The negative consequences that prejudice and discrimination can have on their lives, such as loss of social relationships, diminished self-esteem or feelings of burden, can lead to emotional states compatible with suicide risk. That is, stigma can be such a heavy burden that it leads the person to end their life. This imbues this relationship with significant relevance and need for attention.
However, despite the evidence of the relationship between stigma and suicidal behaviour, available literature reviews focus on the stigma experienced by suicide survivors (21), the stigma associated with suicidal bereavement (22), or else the stigma associated with suicide in general (23). The existence of a review on studies developed in clinical samples is unknown, samples which would be interesting to analyse the phenomenon in depth.
The aim of this study is therefore, to carry out an updated systematic review of the existing research regarding the relationship between the stigma associated with mental health problems in all their forms and the risk of suicide, in people with this type of problem. In addition, as a second aim, the potential variables involved in the relationship between these two constructs are studied.
Considering the literature reviewed and the data presented, the main hypothesis of this study is that the stigma associated with mental health problems has a positive relationship with the risk of suicide in the population with mental health problems.
Another hypothesis is the potential existence of mediating variables in this relationship, such as higher levels of depression or hopelessness.
METHODS
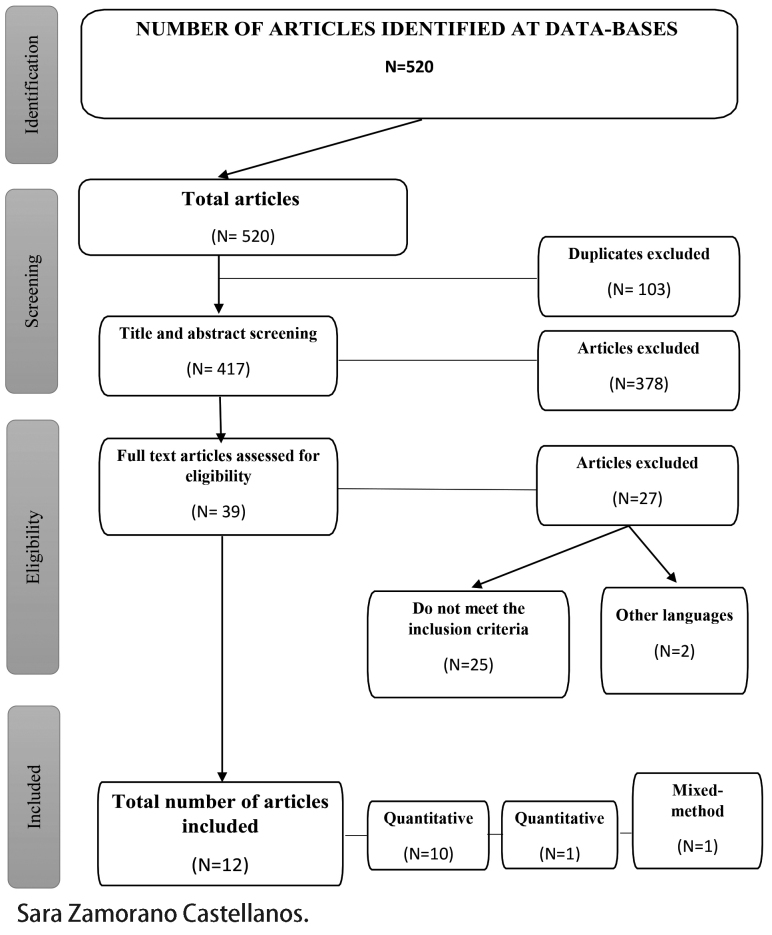
The current study was elaborated following the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines (24).
Data sources and search strategies
To identify studies for this review, PsycINFO, Pubmed and Scopus databases were searched up to December 2020 from January 2012. Multiple combinations were made, using thesauri to delimit subjects and keywords, as well as boolean operators and truncated words. The search strategy in databases was as follows, both in English and Spanish: (Stigma OR Stig*) AND ("Suicides & suicide attempts" OR suici* OR "suicidal ideation" OR "suicidal risk" OR "suicidal behavior" OR suicide OR "self harm" OR "self injury" OR "self destructive" OR autol*) AND ("mental disorders" OR "mental illness" OR "mental health"). The specific searches for each database can be seen in Appendix 1.
Study selection criteria
The search strategy is summarized in Figure 1. The inclusion criteria were: 1) had to be empirical studies (quantitative, qualitative or mixed), 2) published after 2012, 3) peer-reviewed, 4) published in scientific journals, 5) in Spanish or English, 6) reporting data on direct or indirect measures of stigma, 7) with a clinical population with any diagnosis of mental disorder either through Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) or ICD-10 (WHO, 1992), 8) containing measures of suicidal behaviour or ideation, and 9) discussing the relationship between stigma and suicide risk in population with mental health problems. Excluded from the review were: 1) any other type of publication other than scientific articles, 2) in other languages, 3) dealing with the stigmatization of suicidal behaviour itself, as this is a different type of stigma, or 4) not containing DSM or ICD diagnoses, as it is required to meet the objective of the review to be certain that the sample suffers from a diagnosed mental health problem.
Figure 1.
PRISMA diagram to illustrate the article inclusion process*.
These study selection processes were: 1) duplicate elimination, 2) title review, 3) abstract review and 4) full- text review. Once this last selection had been made, a total of 12 articles were included in the present review.
Data extraction and methodological quality measures
Data was extracted on the studies' location, objectives, methodological design, participants, stigma and suicidal behaviours measures, variables related to the sample, and results and studies' limitations. The methodology of each study and its statistical data were taken into account to assess the methodological quality of the articles.
Data synthesis and analysis
Data obtained in the present review were synthesized by categorizing, summarizing and interpreting the different results across 12 articles. The themes identified reflect the approach of the present work. A review of the studies is presented in Table 1.
Table 1.
Summary table of the studies included in the review
| Article | Sample size and type | Measurements | Results |
|---|---|---|---|
| Sharaf et al. (2012) England | N= 200; stable outpatient psychiatric clinic patients (schizophrenia). | Diagnosis: DSM-IV-TR. Scales/indexes: SPS, IS, ISMI, PANSS. Dichotomous interview of suicidal behaviours (yes/no). |
Suicide risk correlates with insight (r=.55, p <.001), internalized stigma (r=.79, p <.001) and depression (r=.78, p <.001). Correlation between internalized stigma and depression (r=.74, p <.001). The effect of internalized stigma (B=.47, p =.45, t=7.76, p <.001) and depression (B=4.49, β =.38, t=6.34, p <.001) increase the risk of suicide. |
| Latalova et al. (2014) Switzerland | N=198; hospitalized patients with anxiety and affective disorders. | Diagnosis: ICD-10. Scales/indexes: CGI, BAI, BDI-II, ISMI, SDS, DAI-10, DES, MADRS-10. | Subjective and objective suicide ratios with ISMI (r=.43, r=.33, p <.0001). Linear regression between subjective suicide rate (item 9 BDI) and ISMI (F = 40.86 DFn 1.000 DFd 144.0; p <.0001). Linear regression between MADRS item 10 (suicide) and ISMI (F = 15.94 DFn 1,000 DFd 177.0; p <0.0001). |
| Farrelly et al. (2015) England | N total= 198; N subsample = 58; major depression, bipolar disorder or schizophrenia spectrum disorder. |
Diagnosis: ICD -10. Scales/indexes: SBQ, DISC, SSS, BHS, ISMI. Qualitative interview. | Significant effects of internalized stigma on hopelessness (coefficient: .681; 95% CI 0.507-0.855, p<.01; standardized coefficient: .474). Hopelessness showed a significant effect on suicide risk (coefficient: .146, 95% CI 0.015-0.146, p<.01; standardized coefficient: .544). |
| Wang et al. (2016) USA | N= 184; schizophrenia, schizoaffective disorder, bipolar disorder and major depression. | Diagnosis: DSM-IV (SCID-IV). Scales/indexes: PDDS, TAS-20, ISFS. Dichotomous interview of suicidal behaviours (yes/no). | Correlation between deficits in emotional clarity and suicide risk (r=.20, p=.02). Perceived stigma positively and significantly associated with suicide risk when emotional clarity is low (b = .19, SE = .07, t = 2.55, p = .01, 95% CI: 0.04, 0.33). If demographic and clinical data are input, the interaction between stigma and emotional clarity approaches significance (b = .08, SE = .05, t = 1.77, p = .08, 95% CI: -0.01,0.18). |
| Oexle et al. (2017) Germany | N baseline= 222, N 1 year= 174; N 2 years= 15; affective disorders, personality disorders, schizophrenia and schizoaffective disorders. | Diagnosis: ICD -10. Scales/indexes: SCL- 90-R (suicidal ideation, GSI), ISMI. | On all three measures, suicidal ideation correlates significantly with greater self-stigma (r = .41, r = .42 and r = .39 respectively, p < .001) and with greater Global Severity Index at baseline (r = .43, r = .40 and r = .37, respectively, p < .001). Higher self-stigma at baseline was significantly associated with suicidal ideation at baseline (p = .004, R2 Nagelkerke = .29) and at 1 year (p = .035, R2 Nagelkerke = .52). |
| Stip et al. (2017) USA | N= 30; schizophrenia spectrum disorder recently discharged from hospitalization. | Diagnosis: DSM-IV-TR. Scales/indexes: SSI (dependent variable), PBIQ-R, SES, RLI, SSICS, PANSS, CDS, SS, SPS. | The contribution of perceived cognitive dysfunction and stigmatization to the suicidal ideation is significant on all three measures (T1: 41.7.5%, p=.000; T2: 35.2%, p=.001; T3: 21.5%, p=.012). At T1, only stigmatization contributes significantly (β = 0.518; p=.002). At T2, both variables contribute significantly: stigmatization (β = 0.394; p=.025) and perceived cognitive dysfunction (p=0.349; p=.046). At T3, only perceived cognitive dysfunction contributes to ideation (β = 0.438; p=.016). |
| Xu et al. (2018) Germany | N baseline= 186; N 1 year= 152; N 2 years= 141; affective disorders, substance use disorders and psychotic disorders. | Diagnostico: ICD -10. Scales/indexes: SSS, ISMI, RSES, BPRS (suicide and symptoms). | Correlation between suicidal ideation at 2 years and self-stigma (r=.21, p <.05). Fit: (χ2 = 10.57, df = 10, χ2/df = 1.06, p =.39; RMSEA = 0.02, CFI = 0.992, TLI = 0.970, WRMR = 0.489). Significant effect of the mediation of self-stigma and self-esteem on suicidal ideation (beta= 0.04, 95% CI 0.003 to 0.123). The link between self-stigma at 1-year follow-up and suicidal ideation at 2 years is mediated by a decrease in self-esteem at 1-year follow-up (β = 0.20, 95% CI 0.030 to 0.377). The model explains 25% of the variance. |
| Tourino et al. (2018) Spain | N=71; outpatients diagnosed with schizophrenia and attending Psychosocial Rehabilitation Centres. | Diagnosis: ICD -10. Scales/indexes: ISMI, RSES, SCS, SUMD, CDS (current suicide risk), BHS, GCI-SCH. Evaluation of prior suicidal behaviour. | Patients with internalized stigma show higher prevalence of suicidal ideation in the last year (p=.007) and higher number of suicide attempts (p=.03). They also show lower scores in self-compassion (p <.001). Higher risk of suicide according to item 8 of the CDS (p=.004). |
| Oexle et al. (2018) England | N=1; patients diagnosed with affective, schizophrenia spectrum and dissociative disorders. | In-depth individual interviews until data saturation. Diagnosis: not specified. | Five main themes are identified: a) awareness of stereotypes; b) lack of understanding from others; c) avoidant behaviour; d) internalization of stereotypes (self-stigma); e) emotional stress. Participants report stereotypes associated with their mental illnesses that generate unfair treatment and restricted opportunities. |
| Vrbova et al (2018) New Zealand | N= 48; stable patients with a diagnosis of schizophrenia. | Diagnosis: ICD -10. Scales/indexes: MINI (suicide), PANSS, CGI, BDI-II, ISMI, ADHS. LSAS, TCI-R. | Self-stigma correlates positively and significantly with suicide rate (r=.51, adjusted p <.01, large effect size). Hope correlates negatively and significantly with suicide rate (r=-.43, adjusted p <.05, medium effect size). |
| Wastler et al. (2019) USA | N= 248; war veterans with diagnoses of schizophrenia, schizoaffective disorder, bipolar disorder or major depression with psychotic symptoms. | Diagnosis: not specified. Scales/ indexes: ISMI, SOBI, BSI. | Internalized stigma correlates with sense of belonging (r=-.651, p <.01) and with suicidal ideation (r=.239, p <.01). Sense of belonging and internalized stigma interact to predict suicidal ideation, controlling for the variable depression (b= -0.0150, t= -2.3721, p=.0185, 95% CI [-0.0275, -0.0025]). Results suggest that the association between internalized stigma and suicidal ideation is stronger when the sense of belonging is lower (b= 0.256, t= 1.94, p= .054, 95% CI [-0.0046, 0.516]). |
| Alemayehu et al. (2020) Africa | N=415; patients admitted to hospital with a diagnosis of major depressive disorder. | Diagnosis: according to DSM criteria. Scales/indexes: ISMI, MARS, OSSS, CGI, EUROHIS-QOL 8, interviews. | More self-stigma to more suicide attempts 2.33 times greater than those without such history (AOR=2.33, 95% CI: 0.35, 3.99), p=0.002. More self-stigma to more disorder duration 3.21 times greater (AOR=3.21, 95% CI: 1.66, 6.19), p=0.001 More self-stigma to less adherence of 2.93 (AOR=2.93, 95% CI:1.62, 5.29), p<0.001 More selfstigma to worse social support of 4.72. (AOR=4.72, IC 95%:2.09, 10.64) |
ADHS: Adult Dispositional Hope Scale; BAI: Beck Anxiety Scale; BDI-II: Beck Depression Inventory; BHS: Beck Hopelessness Scale; BPRS: Brief Psychiatric Rating Scale; BSI: Brief Symptom Inventory; CDS: Calgary Depression Scale; CGI: Clinical Global Impression; DAI-10: Drug Attitude Questionnaire; DES: Dissociative Experience Scale; DISC: Discrimination and Stigma Scale EUROHIS QOL 8: European Health Interview Survey Quality of Life; IS: Insight Scal; ISFS: Illness-related Social Functioning Scale; ISMI: Internalized Stigma of Mental Illness Scale; LSAS: Liebowitz Social Anxiety Scale; MADRS: Montgomery & Asberg Depression Rating Scale; MARS: Medication Adherence Rating Scale; MINI: Mini Interrnational Neuropsychiatric Interview; OSS: Oslo Social Support Scale; PANSS: Positive and Negative Syndrome Scale; PBIQ-R: Personal Beliefs about Illness Questionnaire-Revised; PDDS: Perceived Devaluation- Discrimination Scale; RSES: Rosenberg Self-Steem Scale; SCL-90-R: Symptom Check-list 90 Revised; SCS: Self-Compassion Scale; SDS: Sheehan Disability Scale; SOBI: Sense of Belonging Inventory; SPS: Suicide Probability Scale; SPS: Social Provisions Scale; SS: Stigmatization Scale; SSI: Scale of Suicidal Ideation; SSICS: Subjective Scale to Investigate Cognition in Schizophrenia;SS: Stigma Stress Scale; SUMD: Scale to assess Unawareness of Mental Disorder; TAS-20: Toronto Alesithymia Scale; TCI-R: Temperament and Character Inventory-Revised.
RESULTS
Studies characteristics
Among the studies found, 7 were cross-sectional (25-31), 3 were longitudinal studies (32-34), 1 qualitative (35) and 1 mixed- method (36). All articles used convenience sampling, except one (25), which used systematic sampling. About 83% of the studies explored the relationship between different suicidal behaviours and IS. On the other hand, the only articles that do not focus exclusively on IS are Wang et al. (30), who focused their study on perceived stigma, and Farrelly et al. (36), who focused on experienced discrimination, in addition to IS. Regarding measurements of the constructs studied, the most widely used instrument was the Internalized Stigma of Mental Illness Scale (37), and the great heterogeneity of measures for suicidal risk is noteworthy.
Study sample sizes ranged from 13 to 415 participants, with ages between 17 and 65, including all the studies participants of both sexes, and regarding the location of the articles, most were published in European countries (n=7). Finally, concerning the sample profile, the analysed articles collected data from patients with diagnoses made from ICD- 10, DSM-IV-TR and DSM-IV, although all but two studies (25,26) worked only with a severely mentally ill population.
Main results
Demographic features, stigma and suicide risk.
The studies included in the current systematic review report moderate to high levels of IS and suicide risk. Regarding the variable age of participants, Xu et al. (34), reported significant relationships between age and IS and Sharaf et al. (27), also found that age correlated positively and significantly with suicidal risk. In relation to employment status, by Sharaf et al. (27) described that unemployed patients in their sample presented a higher suicide risk. Alemayehu et al. (25), also found that those who were unemployed showed higher levels of IS (p<0.02). By contrast, Vrbova et al. (29), found no relationship between employment status and higher levels of IS or suicidal risk, but they found a relationship between perceiving a disability pension and higher autolytic risk, with a large effect size.
According to the onset and duration of mental disorders, two studies found a negative and significant correlation between suicide risk and symptom onset (26,29). In addition, Alemayehu et al. (25), reflected a higher likelihood of IS the longer the duration of symptoms (AOR=3.21, 95% CI: 1.66, 6.19, p=0.001). However, Sharaf et al. (27), found no significant correlation between these variables. As for other sociodemographic variables such as educational level, ethnicity or socioeconomic status, the articles did not find significant relationships.
Results from qualitative and mixed studies.
Within the purely qualitative study included in this review, Oexle et al. (35) explored the experiences and consequences of stigma in 13 suicide attempt survivors and concluded that stigma towards mental health problems, both at the social and internalized levels, could increase the risk of suicide. Additionally, Farrelly et al. (36), in a mixed- method article, (N = 198) suggested that discrimination was associated with suicide risk in the sample through loss of confidence in receiving help, social isolation and negative thoughts.
Results of cross-sectional studies.
Regarding cross-sectional studies, in general, a relationship was found between IS and suicide risk. Significant positive relationships between measures of suicidal tendency or ideation and total IS scores were found in the articles by Sharaf et al. (27), Latalova et al. (26) and Wastler et al. (31). In the same approach, Tourino et al. (28), exposed that people with a higher level of IS showed a higher prevalence of suicidal ideation, as well as a higher total number of suicide attempts and higher current risk of suicide. For their part, Alemayehu et al. (25) found significant associations between high IS and a history of suicide attempts (AOR = 2:33, 95% CI: 1.35, 3.99).
However, in some other studies, the relationship between stigma and suicidal risk seems less clear. Vrbova et al. (29), despite finding a relationship between IS and suicidal risk, conducted a regression analysis using ISMI as an independent variable, without resulting in a significant predictor for suicide risk. Following the same approach, Wang et al. (30) found no significance with regard to the relationship between perceived stigma and suicide risk.
Results from longitudinal studies
Oexle et al. (32) found a positive and significant association between suicidal ideation and higher levels of IS, both at baseline and at one- and two-year measures. Following this approach, the article by Xu et al. (34) also reflected a positive and significant correlation between IS and suicidal ideation at the 2-year follow-up measure. Stip et al. (33), meanwhile, suggested that both stigmatization and perceived cognitive dysfunction contributed directly and lastingly to variance in suicidal ideation.
Moderating variables
Some studies reported variables moderating the relationship between IS and suicidal risk. Depressive symptomatology was the variable that most studies found moderating this association (26-29,31,35). Wastler et al. (31), found negative and significant association between IS and the sense of belonging with this variable seeming to be a moderator predicting the suicidal ideation. And in relation to self-esteem, Xu et al. (34) in their mediation model included decreased self-esteem as a mediating variable between IS and suicidal ideation.
Other moderating variables between IS and suicidal risk found in the studies were greater insight (27), greater hopelessness (28,29,35,36), lower self-compassion (28), greater cognitive dysfunction (33), and greater dissociation (26).
Risk of bias in included studies
Random sequence generation: most studies report following a convenience sampling technique, except one (25), which used systematic sampling. High risk of selection bias.
Allocation concealment: studies do not report allocation concealment because they do not have control groups. Unclear risk of selection bias, because they seek to confirm a particular hypothesis (relationship between stigma and suicide risk).
Blinding of participants and personnel: they also do not report blinding, as there are no control groups. Groups are composed of people with mental health problems. Unclear risk of realisation bias.
Blinding of outcome assessment: as participants do not receive any intervention, it is difficult to assess this indicator in the studies presented. Unclear risk of detection bias.
Incomplete outcome data: in longitudinal studies (32-34), we found losses to follow-up, which is to be expected in these type of studies. Low risk of attrition bias.
Selective reporting of results: in the studies consulted, no selective reporting of results was found, as they report both significant and non-significant results. Low risk of reporting bias.
Other sources of bias: non-randomised studies, studies focusing on the relationship between two variables (correlational).
DISCUSSION
The purpose of the present review was to assess whether stigma towards mental health problems, at any level, can be a risk factor for suicide in the clinical population. In this regard it should be noted that, although the initial search for studies included any type of stigma, most of the research focused only on IS.
In general, the IS and suicide risk levels found in the studied samples are presented as moderate or high. Moreover, in most studies, a positive and significant relationship between IS and self-injury risk is observed. This association also appears in longitudinal studies, which could mean that IS has a cumulative effect enhancing the autolytic risk. However, it is not possible to state categorically that IS predicts suicide risk due to the fact that, in other studies, when this type of stigma has been explored as a predictor, it has not been found to be significant (29). Furthermore, it is noteworthy that studies incorporating other stigma variables found that perceived stigma was not related to suicidal risk (30), but discrimination experienced was (36). This suggest that perhaps for stigma to carry a risk of suicide, it must have been personally experienced and internalized.
An explanation for the association may be based on the studies by Reynders et al. (38) and Carpiniello & Pinna (39), which suggest that certain risk factors that may affect suicide arise from stigmatization derived from mental health problems. This approach is similar to hypotheses defining stigma as a stressor associated with hopelessness (40) and social isolation (18,40). The findings of the present review seem to support these approaches by pointing out the various moderating variables of the association between IS and suicide risk.
Concerning the characteristics of the samples studied and the sociodemographic variables, it is noteworthy that all but two studies (25,26), included only people with a diagnosis of severe mental disorder. However, in both exceptions the samples consisted of hospitalized people, so that, in any case, the diagnoses should be considered as severe. This inclusion of samples only with people with severe mental disorders is consistent with a recent review and meta-analysis of IS that points out how samples with other diagnoses are a clear minority in the research (41). There is, therefore, a need for more studies carried out on other diagnoses and mental health problems. With regard to the age variable, one explanation for the relationship between IS, suicide risk and the sociodemographic variable of older age could be that the longer a person lives with stigma or mental health problems, and the more chronicity, the greater the likelihood that this stigma will be internalized and cause adverse effects. As for the role of unemployment in the relationship between IS and suicide risk, one hypothesis would be that unemployed people may develop a certain feeling of meaninglessness in their lives, and a sense of worthlessness.
The current research has several limitations. First, methodological limitations of the articles studied should be noted. These include the majority of cross-sectional studies, type of sampling and characteristics of the samples in terms of size and lack of cultural diversity. Furthermore, the review process also has some limitations such as language bias by including articles only in English and Spanish, and publication bias. There is also a lack of consensus on the definition and nomenclature of the different types of stigma and it is noteworthy the complexity of suicide risk prediction and so consequently, it is complicated to define both constructs. As for stigma, as the majority of the articles measure IS, it is difficult to have a broad idea of how all types of stigma affect the risk of suicide in mental health problems.
Overall, the findings suggest that that the initial hypotheses are met. It seems to be a positive and significant relationship between IS and suicide risk in the clinical population. This association is mediated by multiple variables, such as depression, hopelessness, loss of the sense of life, unemployment, and diminished support networks. Thus, the stigma associated with mental health problems could be a potential therapeutic target for reducing the risk of suicide in the clinical population. Prevention and intervention efforts are needed at community and individual levels, although further studies in this area are considered necessary in order to understand the link between the two variables in greater depth.
Disclosure
Authors declare that they have no conflict of interest
Deontological Commission
This research did not require analysis by an ethics committee, as it did not involve working directly with individuals, but rather the analysis of a number of studies with their corresponding ethical guarantees.
ACKNOWLEDGMENTS
Not applicable
APPENDICES
Appendix I. Database searches.
- Psycinfo:
su(Stigma OR Stig*) AND su("Suicides & suicide attempts" OR suici* OR "suicidal ideation" OR "suicidal risk" OR "suicidal behavior" OR suicide OR "self harm" OR "self injury" OR "self destructive" OR autol*) AND su ("mental disorders" OR "mental illness" OR "mental health")
(su(Stigma OR Stig*) AND su("Suicides & suicide attempts" OR suici* OR "suicidal ideation" OR "suicidal risk" OR "suicidal behavior" OR suicide OR "self harm" OR "self injury" OR "self destructive" OR autol*) AND su("mental disorders" OR "mental illness" OR "mental health")) AND (rtype.exact("Peer Reviewed Journal") AND me.exact("Empirical Study" OR "Quantitative Study" OR "Qualitative Study" OR "Longitudinal Study" OR "Clinical Trial") AND PEER(yes))
- Pubmed:
(((Stigma[Title] OR Stig*[Title])) AND ("Suicides & suicide attempts"[Title/Abstract] OR suici*[Title/Abstract] OR "suicidal ideation"[Title/Abstract] OR "suicidal risk"[Title/Abstract] OR "suicidal behavior"[Title/Abstract] OR suicide[Title/Abstract] OR "self harm"[Title/Abstract] OR "self injury"[Title/Abstract] OR "self destructive"[Title/Abstract] OR autol*[Title/ Abstract])) AND ("mental disorders" OR "mental illness" OR "mental health")
- Scopus:
TITLE-ABS (stigma OR stig*) AND TITLE-ABS ("Suicides & suicide attempts" OR suici* OR "suicidal ideation" OR "suicidal risk" OR "suicidal behavior" OR suicide OR "self harm" OR "self injury" OR "self destructive" OR autol*) AND TITLE-ABS ("mental disorders" OR "mental illness" OR "mental health") AND (LIMIT-TO (SRCTYPE, "j")) AND (LIMIT-TO (DOCTYPE, "ar") OR LIMIT-TO (DOCTYPE, "re")) AND (LIMIT-TO (SUBJAREA, "PSYC")) AND (LIMIT-TO (PUBYEAR, 2020) OR LIMIT-TO (PUBYEAR, 2019) OR LIMIT- TO (PUBYEAR, 2018) OR LIMIT-TO (PUBYEAR, 2017) OR LIMIT-TO (PUBYEAR, 2016) OR LIMIT-TO (PUBYEAR, 2015) OR LIMIT-TO (PUBYEAR, 2014) OR LIMIT-TO (PUBYEAR, 2013) OR LIMIT-TO (PUBYEAR, 2012)) AND (LIMIT-TO (LANGUAGE, "English") OR LIMIT-TO (LANGUAGE, "Spanish")) AND (LIMIT-TO (EXACTKEYWORD, "Human") OR LIMIT- TO (EXACTKEYWORD, "Humans"))
Funding Statement
Funding
No funding sources
REFERENCES
- 1.Gerlinger G, Hauser M, De Hert M, Lacluyse K, Wampers M, Correll CU. Personal stigma in schizophrenia spectrum disorders: A systematic review of prevalence rates, correlates, impact and interventions. World Psychiatry. 2013;12(2):155–64. doi: 10.1002/wps.20040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interes Suppl. 2014;15(2):37–70. doi: 10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- 3.Pedersen D. Estigma y exclusión en la enfermedad mental: Apuntes para el análisis y diseño de intervenciones. Acta Psiquiatr Psicol Am Lat. 2009;55(1):39–50. [Google Scholar]
- 4.Overton SL, Medina SL. The stigma of mental illness. J Couns Dev. 2008;86(2):143–51. [Google Scholar]
- 5.Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and measuring mental illness stigma: The mental illness stigma framework and critical review of measures. Stigma Heal. 2018;3(4):348–76. doi: 10.1037/sah0000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corrigan PW, Kleinlein P. The Impact of Mental Illness Stigma. 2005 [Google Scholar]
- 7.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med [Internet] 2010;71(12):2150–61. doi: 10.1016/j.socscimed.2010.09.030. Available from: http://dx.doi.org/10.1016/j.socscimed.2010.09.030 . [DOI] [PubMed] [Google Scholar]
- 8.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002 Feb;1(1):16–20. [PMC free article] [PubMed] [Google Scholar]
- 9.Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a Barrier to Recovery: The Consequences of Stigma for the Self-Esteem of People With Mental Illnesses. Psychiatr Serv. 2001 Dec;52(12):1621–6. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- 10.Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma: Advances in Theory and Research. Basic Appl Soc Psych. 2013 Jan;35(1):1–9. [Google Scholar]
- 11.De Leo D, Milner A, Fleischmann A, Bertolote Y, Collings S, Amadeo S et al. The who start study suicidal behaviors across different areas of the world. Crisis. 2013;34(3):156–63. doi: 10.1027/0227-5910/a000193. [DOI] [PubMed] [Google Scholar]
- 12.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The Interpersonal Theory of Suicide. Psychol Rev. 2010 Apr;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim WJ, Song YJ, Ryu HS, Ryu V, Kim JM, Ha RY et al. Internalized stigma and its psychosocial correlates in Korean patients with serious mental illness. Psychiatry Res [Internet] 2015;225(3):433–9. doi: 10.1016/j.psychres.2014.11.071. Available from: http://dx.doi.org/10.1016/j.psychres.2014.11.071 . [DOI] [PubMed] [Google Scholar]
- 14.Jahn DR, Leith J, Muralidharan A, Brown CH, Drapalski AL, Hack S et al. The influence of experiences of stigma on recovery: Mediating roles of internalized stigma, self-esteem, and self-efficacy. Psychiatr Rehabil J. 2020;43(2):97–105. doi: 10.1037/prj0000377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schauman O, MacLeod AK, Thornicroft G, Clement S. Mental illness related discrimination: The role of self-devaluation and anticipated discrimination for decreased well-being. Stigma Heal. 2019 Feb;4(1):11–8. [Google Scholar]
- 16.Rusch N, Zlati A, Black G, Thornicroft G. Does the stigma of mental illness contribute to suicidality? Vol. 205, British Journal of Psychiatry. Royal College of Psychiatrists. 2014:257–9. doi: 10.1192/bjp.bp.114.145755. [DOI] [PubMed] [Google Scholar]
- 17.Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry. 2004;4:1–11. doi: 10.1186/1471-244X-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schomerus G, Evans-Lacko S, Rusch N, Mojtabai R, Angermeyer MC, Thornicroft G. Collective levels of stigma and national suicide rates in 25 European countries. Epidemiol Psychiatr Sci. 2015 Apr 15;24(2):166–71. doi: 10.1017/S2045796014000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keller S, McNeill V, Honea J, Miller LP. A look at culture and stigma of suicide: Textual analysis of community theatre performances. Int J Environ Res Public Health. 2019 Feb 1;16(3) doi: 10.3390/ijerph16030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schomerus G, Stolzenburg S, Freitag S, Speerforck S, Janowitz D, Evans-Lacko S et al. Stigma as a barrier to recognizing personal mental illness and seeking help: a prospective study among untreated persons with mental illness. Eur Arch Psychiatry Clin Neurosci. 2019 Jun 1;269(4):469–79. doi: 10.1007/s00406-018-0896-0. [DOI] [PubMed] [Google Scholar]
- 21.Hanschmidt F, Lehnig F, Riedel-Heller SG, Kersting A. The Stigma of Suicide Survivorship and Related Consequences—A Systematic Review. PLoS One. 2016 Sep;11(9):e0162688. doi: 10.1371/journal.pone.0162688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cvinar JG. Do Suicide Survivors Suffer Social Stigma: A Review of the Literature. Perspect Psychiatr Care. 2005 Jan;41(1):14–21. doi: 10.1111/j.0031-5990.2005.00004.x. [DOI] [PubMed] [Google Scholar]
- 23.Sudak H, Maxim K, Carpenter M. Suicide and Stigma: A Review of the Literature and Personal Reflections. Acad Psychiatry. 2008;32(2):136–42. doi: 10.1176/appi.ap.32.2.136. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alemayehu Y, Demilew D, Asfaw G, Asfaw H, Alemnew N, Tadesse A. Internalized Stigma and Associated Factors among Patients with Major Depressive Disorder at the Outpatient Department of Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia, 2019: A Cross-Sectional Study. Pilc A, editor. Psychiatry J. 2020;2020:7369542.. doi: 10.1155/2020/7369542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Latalova K, Prasko J, Kamaradova D, Ociskova M, Cinculova A, Grambal A et al. Self-stigma and suicidality in patients with neurotic spectrum disorder - A cross sectional study. Neuroendocrinol Lett. 2014;35(6):474–80. [PubMed] [Google Scholar]
- 27.Sharaf AY, Ossman LH, Lachine OA. A cross-sectional study of the relationships between illness insight, internalized stigma, and suicide risk in individuals with schizophrenia. Int J Nurs Stud [Internet] 2012;49(12):1512–20. doi: 10.1016/j.ijnurstu.2012.08.006. Available from: http://dx.doi.org/10.1016/j.ijnurstu.2012.08.006 . [DOI] [PubMed] [Google Scholar]
- 28.Tourino R, Acosta FJ, Giraldez A, Alvarez J, González JM, Abelleira C et al. Suicidal risk, hopelessness and depression in patients with schizophrenia and internalized stigma. Actas Esp Psiquiatr. 2018 [PubMed] [Google Scholar]
- 29.Vrbova K, Prasko J, Ociskova M, Holubova M, Kantor K, Kolek A et al. Suicidality, self-stigma, social anxiety and personality traits in stabilized schizophrenia patients - A cross-sectional study. Neuropsychiatr Dis Treat. 2018;14:1415–24. doi: 10.2147/NDT.S162070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang K, Weiss NH, Pachankis JE, Link BG. Emotional Clarity as a Buffer in the Association Between Perceived Mental Illness Stigma and Suicide Risk. Stigma Heal. 2016 Nov;1(4):252–62. doi: 10.1037/sah0000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wastler H, Lucksted A, Phalen P, Drapalski A. Internalized Stigma, Sense of Belonging, and Suicidal Ideation Among Veterans With Serious Mental Illness. Psychiatr Rehabil J. 2019 doi: 10.1037/prj0000386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oexle N, Rüsch N, Viering S, Wyss C, Seifritz E, Xu Z et al. Self-stigma and suicidality: a longitudinal study. Eur Arch Psychiatry Clin Neurosci. 2017 Jun 1;267(4):359–61. doi: 10.1007/s00406-016-0698-1. [DOI] [PubMed] [Google Scholar]
- 33.Stip E, Caron J, Tousignant M, Lecomte Y. Suicidal Ideation and Schizophrenia: Contribution of Appraisal, Stigmatization, and Cognition. Can J Psychiatry. 2017;62(10):726–34. doi: 10.1177/0706743717715207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu Z, Müller M, Lay B, Oexle N, Drack T, Bleiker M et al. Involuntary hospitalization, stigma stress and suicidality: a longitudinal study. Soc Psychiatry Psychiatr Epidemiol [Internet] 2018;53(3):309–12. doi: 10.1007/s00127-018-1489-y. Available from: http://dx.doi.org/10.1007/s00127-018-1489-y . [DOI] [PubMed] [Google Scholar]
- 35.Oexle N, Herrmann K, Staiger T, Sheehan L, Rüsch N, Krumm S. Stigma and suicidality among suicide attempt survivors: A qualitative study. Death Stud [Internet] 2019;43(6):381–8. doi: 10.1080/07481187.2018.1474286. Available from: https://doi.org/10.1080/07481187.2018.1474286 . [DOI] [PubMed] [Google Scholar]
- 36.Farrelly S, Jeffery D, Rüsch N, Williams P, Thornicroft G, Clement S. The link between mental health-related discrimination and suicidality: Service user perspectives. Psychol Med. 2015;45(10):2013–22. doi: 10.1017/S0033291714003158. [DOI] [PubMed] [Google Scholar]
- 37.Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003 Nov;121(1):31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 38.Reynders A, Kerkhof AJFM, Molenberghs G, Van Audenhove C. Stigma, Attitudes, and Help-Seeking Intentions for Psychological Problems in Relation to Regional Suicide Rates. Suicide Life-Threatening Behav. 2016 Feb 1;46(1):67–78. doi: 10.1111/sltb.12179. [DOI] [PubMed] [Google Scholar]
- 39.Carpiniello B, Pinna F. The reciprocal relationship between suicidality and stigma. Front Psychiatry. 2017 MAR;8:1–9. doi: 10.3389/fpsyt.2017.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Heeringen K. Stress-diathesis model of suicidal behavior. Neurobiol basis suicide. 2012;51:113.. [Google Scholar]
- 41.Del Rosal E, González-Sanguino C, Bestea S, Boyd J, Muñoz M. Correlates and consequences of internalized stigma assessed through the Internalized Stigma of Mental Illness Scale for people living with mental illness: A scoping review and meta-analysis from 2010. Stigma Heal. 2020 [Google Scholar]