Abstract
Objectives
The increase in the number of jurisdictions legalising medical assistance in dying (MAiD) has contributed to a growth in the number of family and friends who may face unique elements of grief and bereavement. The aim of this study was to review the literature of grief and bereavement of family and friends following MAiD, and to summarise findings for the development of community resources and programming.
Methods
We performed a scoping review with workshop consultation of stakeholders. Six electronic databases and the grey literature were searched for qualitative, quantitative and review articles. Content-analytical techniques and multidisciplinary discussions led to the development of concepts and a conceptual framework.
Results
Twenty-eight articles met the inclusion criteria. We identified five concepts that impact the grief and bereavement of family/friends: relationships between family/friends and the patient as well as healthcare providers; aspects of MAiD grief which can include secrecy and/or anticipatory grief; preparations which may include family/friends and should be centralised and harmonised; end of life as an opportunity for ceremony; and the aftereffects during which mental health outcomes are studied.
Conclusion
This multidisciplinary scoping review incorporates stakeholder consultation to find that support is needed to address the complicated and changing emotions of family/friends before, during and after a MAiD death. Furthermore, additional societal normalisation of MAiD is necessary to reduce secrecy and stigma and improve the accessibility of resources for family/friends.
Keywords: Bereavement, End of life care, Quality of life, Terminal care
WHAT IS ALREADY KNOWN ON THIS TOPIC
Past reviews have shown that grief and bereavement associated with medical assistance in dying (MAiD) are affected by secrecy and stigma.
Family/friends may require ongoing psychosocial support.
WHAT THIS STUDY ADDS
Grief and bereavement surrounding MAiD may start early and involve the concepts of: relationships, aspects of MAiD grief, preparations, end of life and aftereffects.
MAiD experiences create emotions that change over time and can be complicated by secrecy or fear of stigma.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Bereavement resources are necessary before and after MAiD.
Research regarding MAiD bereavement should occur at multiple time points.
Introduction
Changes in legislation and cultural values have increased the prevalence of medical assistance in dying (MAiD). Currently, assisted death is recognised by 5 of 6 Australian states, 11 of 50 states of the USA, Canada, Luxembourg, Belgium, Netherlands, Switzerland, New Zealand, Colombia, Spain and Italy.1–4 The increasing prevalence suggests a corresponding increase in the number of bereaved individuals following MAiD.
The focus of MAiD is often on the patient, although family/friends are the ones who bereave, whether they were supporters or not of MAiD. Previous research suggests improved bereavement with MAiD due to the opportunity for closeness, saying goodbye, or copreparing for end of life (EOL).5–7 Nonetheless, with a limited number of jurisdictions permitting MAiD, factors such as social isolation, stigma or religious acceptance can impact the expression of grief and bereavement.8 9 These factors can change over time and the increasing legalisation of MAiD reflects shifting attitudes towards EOL options. It is important to continuously study contributors and circumstances that affect the natural bereavement experience of family/friends during all stages of MAiD.
The psychosocial aftereffects of MAiD has been studied in previous reviews. Reviews focusing on caregiver or family experiences around assisted dying or hastened death recommend professional support for families during the MAiD process.7 10 Given the many challenges around MAiD, grief and bereavement are the focus of only a handful of studies. In the review of Andriessen et al,5 MAiD experiences are considered not to be worse compared with other types of death when assessing for grief, mental health and posttraumatic stress outcomes.5 The authors also introduce unique considerations following MAiD including coping with social stigma and confronting moral and relational conflicts within families. Although Andriessen et al 5 provide a summary to explain the occurrence of psychosocial outcomes related to MAiD, no review has previously examined the factors contributing to grief and bereavement throughout the MAiD process. Furthermore, a unique contribution of this review is its engagement of key stakeholders to determine how to adapt findings from the literature for community resource development.
There are many people and processes involved in MAiD. Therefore, we will clarify the terminology to remove ambiguity within this article. Both euthanasia and physician-assisted suicide refer to a hastened death wherein a medical professional administers or prescribes a lethal drug to a patient; and MAiD encompasses both processes.3 11 The cause of death is often a severe or terminal disease whereas one mechanism to control the manner of death is MAiD. There are certain jurisdictions where a terminal disease is not a prerequisite to acquiring MAiD. Non-MAiD deaths will simply be referred to as death, whereas MAiD will be identified as a specific means of death when referring to active euthanasia or assisted dying. Although previous literature used ‘natural death,’ it is important to not conceptualise MAiD as unnatural to avoid pejorative connotations.
We identify the individual who considers and/or receives MAiD as the patient. We recognise that “patient” is associated with biomedicalised processes, whereas critics of the biomedicalisation of death argue that death ought to be viewed through a social lens.12 Given how MAiD is currently under the purview of medical professionals in all the jurisdictions listed above, ‘patient’ is currently an appropriate descriptor although it neglects the non-medical, psychosocial aspects of this identity.1 2 13–15 Similarly, the individuals who provide professional assistance in the form of evaluation, administration and psychological support will be referred to as healthcare professionals (HCPs). HCPs can include physicians and nurse practitioners who provide MAiD, but also physicians, nurses, social workers, psychologists, caregivers and institutions who provide additional logistical or supports before, during and after MAiD. The focus of this scoping review will be on the family/friends of the patient, who are most likely to be the bereaved. This term includes friends, family, neighbours, caregivers or anyone with a social or professional relationship with the patient who may grieve or bereave.16
Grief and bereavement are natural responses after experiencing loss. Currently, MAiD is still a relatively unfamiliar or novel EOL option in many jurisdictions, and its effect on grief and bereavement requires continued exploration. Our scoping review aimed first to summarise the current literature regarding the comprehensive grief and bereavement experiences of family/friends of a patient who received MAiD. Second, our review aimed to translate findings to help community organisations better develop resources or programming. Building on the concepts from our content-analyses of included articles, we intended to build a conceptual framework for the purposes of our second aim. The population includes people who supported individuals who had MAiD, the exposure is MAiD, and the outcomes are quantitative outcomes and qualitative themes related to grief and bereavement experiences.
Methods
This scoping review search was informed by the framework developed by Arksey and O’Malley17 and expanded by Levac et al.18 Therefore, the authors (1) identified the research question; (2) identified relevant studies; (3) selected final studies for inclusion; (4) charted the data; (5) collated, summarised and reported the results and (6) consulted stakeholders to provide insights beyond the literature. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses19 extension for scoping reviews was used for steps (2) and (3).
The focus of the research question was developed by group consensus among members of the research committee, which included family of a patient who received MAiD. An additional purpose of question development was to guide bereavement programming and resource development for community organisations supporting MAiD, such as MAiDHouse. How can a summary of the literature regarding grief and bereavement of family/friends following MAiD help in the development of community programming and resources?
Search strategy
Published and grey literatures were searched and analysed. The included databases for published academic studies were: MEDLINE, EMBASE, AgeLine, CINAHL, PsycINFO and Scopus. Grey literatures were searched through: Google, Google Scholar, Health Systems Evidence and Grey Literature Report. Searches were carried out between June and August 2021, and updated on 25 June 2022.
The key terms combined concepts of MAiD and bereavement. MAiD was searched using terms such as “medical assistance in dying,” “euthanasia,” “assisted suicide,” “physician aid in dying,” “right to die” and “assisted death.” The concept of bereavement was searched using terms such as “grief,” “grieving,” “bereave(ment)” and “mourn.” We conducted peer review of the search strategy with an academic health sciences librarian, who verified the search strategy (online supplemental appendix 1).
spcare-2022-003715supp001.pdf (260.8KB, pdf)
A targeted scan of organisational websites was conducted. The scan did not yield additional results that met eligibility criteria.
Eligibility criteria
Articles were screened for the following inclusion criteria: (1) legalised MAiD intervention as focus of study; (2) participants provided data regarding grief or bereavement experiences of family/friends following MAiD and (3) qualitative or quantitative outcomes related to experiences around MAiD. Publication types included reviews and empirical studies of qualitative or quantitative methodologies. Grey literature included books, editorials, conference proceedings or conference abstracts. Exclusions included: (1) Non-English articles; (2) focus not on family/friends; (3) results did not address grief or bereavement; (4) studied death was not legalised MAiD, and (5) non-academic publication media such as newspaper articles, book reviews or advertisements. There were no restrictions based on date of publication, setting of MAiD, timing of MAiD, context leading to MAiD (i.e., diagnosis) or administration method.
Screening and reviewing
Each author screened 20 articles to calibrate and refine the inclusion criteria and screening process. All titles and abstracts were double-screened; JB screened all and TH, MK, SRI, NH and AK each screened 20%. Full-text review was conducted in one phase. JB screened all full texts and TH, MK, SRI and AK screened 25% each. Discrepancies were flagged and resolved through group discussion. All articles were blind reviewed by two people: an experienced qualitative researcher, as well as a different member of our multidisciplinary team.
Data collection and coding
The full texts of the included articles were analysed using content-analytical20 21 techniques. Two authors, JB and HY, independently extracted data from included articles, and charted participant demographics and data. The data charting forms were developed on Google Drive after discussions among our research team. Codes were generated through a discursive process of analysis. After each researcher read all included articles, thematic codes were generated using combination of deductive and inductive approaches. Deductive codes included stage of MAID journey, response to MAiD, and relation to the patient. Specific topics presented in each study were then coded inductively as they emerged through the coding process. Quantitative data were also summarised narratively to allow for coding and relational comparisons. Exploratory analyses were conducted in NVivo22 by generating matrix queries, specifically by exploring emerging concepts at each stage of the MAID journey. Quotes were collected to support emerging themes. Findings were regularly discussed with the multidisciplinary research team to inductively generate concepts. This was achieved by grouping similar codes and abstracting larger ideas.
Conceptual framework development and stakeholder consultation
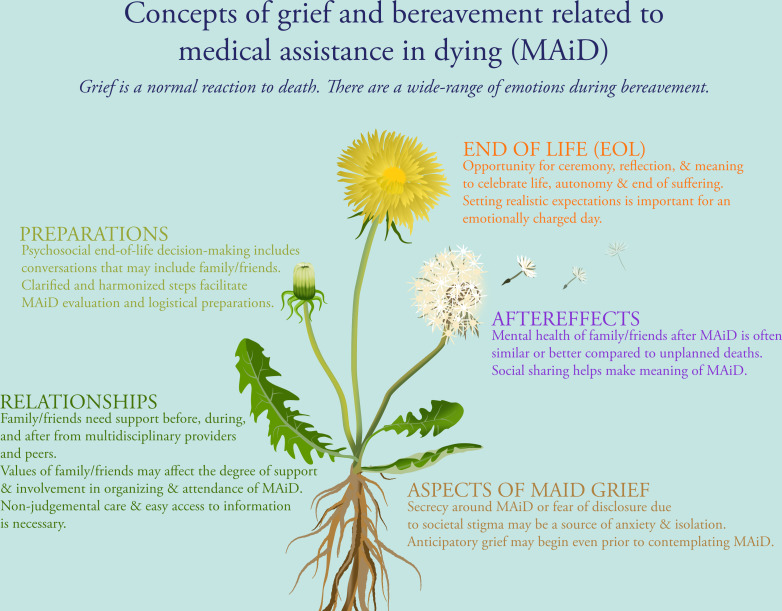
The initial themes were presented at a virtual workshop organised by MAiDHouse (online supplemental appendix 2). This was attended by Canadian MAiD providers, researchers and family/friends who supported someone who had MAiD. Comments were incorporated into the development of final themes. The interdisciplinary research team chose to use visual imagery in the conceptual framework to convey MAiD concepts in response to workshop feedback. The dandelion was ultimately chosen as a representative image because it evolves through different phases and is open to different interpretations by readers.
spcare-2022-003715supp002.pdf (246.1KB, pdf)
Results
Search results and included studies
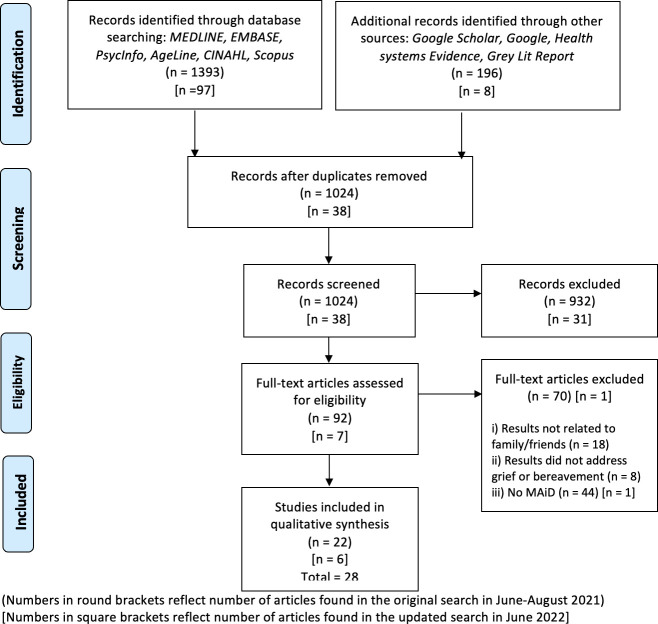
The initial search was screened with an 8% discrepancy rate between reviewers. Details of screening and reasons for exclusion are found in figure 1. Ultimately, our review included 28 academic journal articles, including 6 published literature reviews and 22 empirical studies (tables 1 and 2). Most studies were published in Canada (n=15).6 23–36 Other jurisdictions included Switzerland (n=3),37–39 Netherlands (n=3),16 40 41 USA (n=2),42 43 Australia44 or multiple jurisdictions or not specified (n=4).5 7 10 32 45 Of the 22 identified empirical studies, almost half employed exploratory qualitative methodology (n=13),23–26 28 30 31 33 34 36 37 43 44 with the remainder being either observational quantitative studies (n=6)29 38–40 42 44 or mixed-methods studies (n=3).6 27 35 All 13 qualitative studies conducted interviews, the quantitative studies used validated questionnaires or specifically designed surveys, and the mixed-methods studies employed the above methods as well as focus groups and unstructured conversations. There were seven studies among the empirical studies that reported ethnicity of participants, and all were Caucasian.6 23–25 31 42 43 The empirical studies had study populations that most often consisted of family, friends or caregivers (n=17). There were five studies that included the perspectives of HCPs on a family/friend’s bereavement, with two studies30 33 including only physicians, nurses, case workers and social workers, and another study29 including only physicians. A few studies had specific research questions regarding a MAiD patient subpopulation or the setting of MAiD: Swarte et al 40 focused on MAiD within the context of patients with cancer; Hashemi et al 6 studied MAiD cases which took place at home; and Pronk et al 41 studied family/friends of patients with mental health in relation to MAiD. There were four studies34 35 40 42 that compared family/friend’s bereavements of those who received MAiD and those who did not.
Figure 1.
PRISMA flowchart for initial and updated searches.
Table 1.
Overview of included review articles relating to grief and bereavement of family/friends
| Author, year | Jurisdiction | Study type | Subjects/texts (time since MAiD) | Demographics | Type of MAiD | Main question | Main findings/concepts |
| Andriessen et al, 20205 | Multiple/not specified | Systematic Review | 10 primary research articles | NS | Multiple | Assess grief and mental health of people bereaved by euthanasia | Bereaved individuals following euthanasia had similar to lower scores of disordered grief, mental health, and PTSD Secrecy and lack of social support increase grief |
| Gamondi et al, 201910 | Multiple/not specified | Systematic Review | 19 primary research articles | NS | Multiple | Review family experiences of assisted dying | Themes that represent experiences: Context of the decision Grounding the decision Cognitive and emotional work Experiencing the final farewell Grief and bereavement |
| Goldberg et al, 202145 | Multiple/not specified | NS | Qualitative and quantitative articles | NS | Multiple | Summarise experiences and perspectives of caregivers | Caregivers viewed MAID more favourably than dying by natural causes It is unclear leads to better outcomes for caregivers, but psychosocial support is needed |
| Lowers et al, 20207 | Multiple/not specified | Narrative synthesis | 34 end-of-life caregiving studies eleven hastened death caregiving studies |
NS | Multiple | Explore experiences of family and friends providing care at home at end of life for hastened death | Caregivers actively work toward patient’s goal of a peaceful death in hastened death studies HCPs play a major role in natural death and hastened death, and their understanding of legal abilities and personal willingness to provide practical support affect caregivers’ satisfaction |
| Ontario HIV Treatment Network, 2017 | Multiple/not specified | NS | NS | ‘mostly white… college educated’ | Multiple | Identify impact of MAID on family and friends | There are shared responsibilities between patients, family members and HCPs Opportunity to discuss death is important |
| Roest et al, 201916 | Netherlands | Systematic Review | 14 primary research articles | NS | Multiple | Explore family member involvement in MAID in the Netherlands | Four themes identified: Family-related reasons not to request MAID Responsibilities during decision-making and performance of MAID Grief after MAID is complicated Physician-family relationship is important |
HCPs, healthcare professionals; MAiD, medical assistance in dying; NS, not significant; PTSD, post-traumatic stress disorder .
Table 2.
Overview of included empiric articles relating to grief and bereavement of family/friends
| Beuthin et al, 202123 | Canada | Qualitative (semistructured interviews) | 9 bereaved family and friends (average 15 months; range 4–36 months) |
All caucasian, middle to older-aged women | Euthanasia | Explore bereavement experiences | Grief-bereavement is an extended period that includes predeath to the present MAiD/certainty of death creates ‘parade of lasts’ |
| Brown et al, 2020a(25) | Canada | Qualitative (semistructured interviews) | 5 patients, 11 family members, 14 HCP | 100% Caucasian; 77% female; ages >40 | Euthanasia | Explore patient, family, HCP experiences with MAID | Care considerations in four domains: Emotional (unique facets associated with MAID) Physical (eligibility, location, procedural) Spiritual (honouring choice, acknowledging loss) Relational (supporting the circle of support) |
| Brown et al, 2020b(24) | Canada | Qualitative (semistructured interviews) | 5 patients, 11 family members, 14 HCP | All Caucasian; 77% female; ages>40 | Euthanasia | Explore perspectives on MAiD access and care delivery | Care pathway has ambiguity, causing gaps in knowledge, participation, institutional supports Quality improvement processes are needed to improve legal barriers and clarify HCP roles |
| Frolic et al, 202026 | Canada | Qualitative (semi-structured interviews) | 16 family members (“months after MAiD”) |
56% female | Euthanasia | Understand Hamilton MAiD programme and MAiD legacy impact | Four domains of opposing tensions: Autonomy/ambivalence Time as gift/burden Decreased suffering/time Individual’s legacy/family’s bereavement |
| Gamondi et al, 201537 | Switzerland | Qualitative (semistructured interviews) |
11 bereaved family members (median 24 months; range 12–72 months) |
54% female | Assisted suicide | Explore family involvement in decision-making and subsequent bereavement | All described moral dilemmas during decision-making Barriers causing isolation stem from concerns from stigma and secrecy |
| Ganzini et al, 200942 | US | Quantitative (validated scales or questionnaires) |
Family members of those who received MAiD (n=95) and those who did not (n=63) (range 4–36 months) |
MAiD group: 100% Caucasian; 69% Female; Mean age 60.9 Comparator: 97% Caucasian; 79% Female; Mean age 60.1 |
Assisted suicide | Compare grief symptoms and mental health of family caregivers between those who received MAiD and not | No differences between groups in measures of prolonged grief (2% vs 0%) or depression symptoms (11% vs 14%), or mental health service use (44% vs 52%) Quality of life in last 7 days rated higher by family for those who received MAiD (4.2 vs 2.9, p=0.03) |
| Hales et al, 201927 | Canada | Mixed-methods (focus groups, unstructured conversations, survey) | 11 bereaved family members | NS | Euthanasia | Understand perspectives, identify improvement | There should be improvements to the process, clarifications to the scheduling and 10-day period of reflection Burden associated with patient privacy, clinician objective, lack of bereavement resources following MAiD |
| Ho et al, 2020 | Canada | Qualitative (semistructured interviews) | 26 HCPs | 88% female; 46% nurses, 27% physicians, 19% social workers, 8% spiritual health | Euthanasia | Explore HCPs challenges and resource recommendations | There are inadequate psychological and professional support for family/friends. Resources are needed to ease family distress regardless of whether patients receive MAiD |
| Hashemi et al, 20216 | Canada | Mixed-methods (semistructured interviews, validated questionnaires) | 13 caregivers of home MAiD (average 18 months; range 10–28 months) |
100% Caucasian; 69% female; mean age 60.1 | Euthanasia | Explore quality of bereavement for home MAID | MAiD was easier to accept, family/friends accepted and ready for death All participates had positive experience, and none suffered from complicated grief (IES-R mean=9.2 and BGQ mean=2.1) |
| Holmes et al, 201828 | Canada | Qualitative (semistructured interviews) |
18 family or friends (before and after MAiD) |
NS | Euthanasia | Explore bereavement experiences | Planned death day is odd, although often peaceful, with valued time to say goodbye |
| Laperle et al, 202134 | Canada | Qualitative (semistructured interviews) | Bereaved family members, 8 after euthanasia, 8 after natural death (range 6–48 months) | 75% female; mean age 49.4 | Euthanasia | Offer insights into the relational landscape of bereavement experienced in anticipated death Draft an interpretive model of grief |
The bereaved are active agents who co-construct their experience with their social environment Bereaved family experience four landscapes: I feel open and visited I feel far away, along with the deceased I feel besieged I feel I am expanding and invested with a message |
| Laperle et al, 202235 | Canada | Mixed-methods (semistructured interviews, questionnaires) | Bereaved, 25 after MAiD, 36 after death with palliative care (average 11.8 months) |
85% female; mean age 16 | Euthanasia | Describe the grief experiences of individuals who have lost a loved one through MAid or natural death | No differences between groups in measures of prolonged grief disorder (Prolonged Grief-13) or psychopathological symptomatology of grief (Revised Grief Experience Inventory) Neither MAiD or death with palliative care favour prolonged grief; although there may be less social stigma in Quebec, Canada |
| Oczkowski et al, 202130 | Canada | Qualitative (semi-structured interviews) |
20 HCPs | 45% female | Euthanasia | Describe HCP perspectives, identify successes and suggestions | Need for centralised portal to cover technical and logistics Emotional support for patients and families before, during and after through SW, spiritual care |
| Philippkowskil et al, 2020 | Australia | Quantitative (validated scales) | 164 adults randomised to read one of four vignettes | 79% female | Assisted suicide | Investigate the cause of death and age of the deceased on emotional responses to the bereaved, desire for social distance, and grief expectations | The age of death affected grief experiences The mode of death did not affect grief experiences (p=0.33) |
| Pronk et al, 202141 | Netherlands | Qualitative (semistructured interviews) | 12 family/friends of individuals with mental illness who requested or received MAiD | 50% female | Euthanasia (lethal prescription or injestion) | Examine experiences of relatives of patients that requested MAiD due to mental illness | When patients with mental health request MAiD, family/friends generally feel ambivalence. Family/friends more strongly want to be involved in decision-making and have their views heard by HCPs and the patient. |
| Schutt, 201131 | Canada | Qualitative (semistructured interviews) |
seven bereaved family members | 100% Caucasian; 57% female | Euthanasia | Explore insights from family members’ experience of MAiD | Procedural aspect of MAID augmented perception of biomedical process Should be presented with palliative philosophy |
| Smolej et al, 202236 | Canada | Qualitative (semistructured interviews) | eleven caregivers of individuals who requested or received MAiD | 91% female; average age 54.5 | Euthanasia | Explore the experiences and support needs of family caregivers who are or have provided care peri-MAiD | |
| Srinivasan, 201943 | USA | Qualitative (interviews) |
22 bereaved family members (‘bereaved within 3 years’) |
100% Caucasian; 68% female; age range 61–80 | Assisted suicide | Explore bereavement experiences | Themes identified with assisted death: General grief reactions Anticipatory grief Sense of control Level of agreement with assisted death Grief expression and stigma |
| Swarte et al, 200340 | Netherlands | Quantitative (validated questionnaires) |
Bereaved family and friends of terminally ill patients with cancer who received MAiD (n=189) and those who did not (n=316) | MAiD group: 54% female; mean age=48 Comparator: 58% female; mean age=49 |
Euthanasia (lethal prescription or injestion) | Assess how euthanasia affects grief of family and friends | Bereaved family and friends of those who died by euthanasia had less traumatic grief symptoms (adjusted difference −5.29 (95% CI −8.44 to −2.15)), less current feeling of grief (adjusted difference 2.93 (0.85 to 5.01)); and less post-traumatic stress reactions (adjusted difference −2.79 (-5.33 to -0.25)) |
| Trouton et al, 202029 | Canada | Quantitative (survey) |
18 physicians who provided MAID | NS | Euthanasia | Explore physician practices for bereavement support to patients | Importance of bereavement support recognised (72.2%), but physicians do not have time or resources to provide support Bereavement following MAID is unique due to unfamiliarity and potential for stigma |
| Wagner et al, 2011 | Switzerland | Quantitative (validated questionnaires) |
85 relatives or friends (mean 20 months) |
56% female; mean age=60.15 | Assisted suicide | Examine the effects of perceived social acknowledgement on symptoms of post-traumatic stress and complicated grief | General disapproval, rather than family disapproval or recognition, were correlated with PTSD (rs=0.50=0.56) and complicated grief scores (rs=0.63–0.71) |
| Wagner et al, 2012 | Switzerland | Quantitative (validated questionnaires) |
85 relatives or friends (mean 19 months) |
56% female; mean age=60.15 | Assisted suicide | Examine the impact of witnessing assisted suicide on mental health | Compared with general Swiss population, survey found slightly higher rates of PTSD (13%) and depression (16%) Rates of complicated grief were comparable (4.9%) |
BGQ, Brief Grief Questionnaire; HCP, healthcare professional; IES-R, Impact of Event Scale - Revised; MAiD, medical assistance in dying; NS, not significant; PTSD, post-traumatic stress disorder; SW, social work.
Identified concepts from scoping review
In our attempt to study grief and bereavement of family/friends in relation to MAiD, we identified five concepts from the coding: relationships, aspects of MAiD grief, preparations, EOL and the aftereffects. Within each concept, we present results specific to grief and bereavement as it relates to MAiD (online supplemental table S1).
spcare-2022-003715supp003.pdf (56.5KB, pdf)
Relationships
The interactions and the development of relationships over time can largely impact how family/friends experience grief. The defining relationship is often between family/friends and the patient,34 41 but interactions with HCPs can be impactful.
With the patient
There are many different relations between family/friends and the patient. Roest et al 16 summarised several studies, noting that partners, children and siblings are the most common relations. However, this group can also contain neighbours, friends, nurses and more. Many aspects of these relationships can affect grief or bereavement. Specifically, having shared values and established common goal-setting facilitate acceptance of MAiD.7 37 Family/friends’ involvement in MAiD is often based on personal values and perceptions of MAiD.7 45 Conflicting values can impact the level of moral dilemma felt during the process.10 41
The patient’s role through MAiD is relatively straightforward whereas family/friends can either be actively or passively involved in planning or attending MAiD, or be unaware until after the death. Specifically, family/friends can be described in two ways: those who are involved and those who are aware. In other words, being involved includes planning and/or attending the death; whereas being aware is recognition of MAiD without direct participation.37 Interestingly, some patients will even ask for the consent of family/friends to be involved as they recognise MAiD may not be viewed favourably by everyone.16 The complicated web of players can be unique in each situation, creating multifaceted emotions and consequences. Pre-emptive support for those actively and passively involved in MAiD29 30 41 can better address specific grief and bereavement needs—before, during and after MAiD.
With healthcare providers
HCPs can ameliorate the quality of grief for friends/family. Despite the obligations towards the patient, family/friends have many interactions with the care team before and after the day of MAiD and investment into this relationship is important.24 25 34 46 In some jurisdictions, HCPs consider the future bereavement of the family when deciding to grant MAiD.41 In other jurisdictions, it is unclear who should initiate the discussions around MAiD. Family/friends may believe that the responsibility to learn about EOL options falls on them. This is further complicated by HCPs or family/friends who may have a preference not to participate in MAID.25 27 33 These unclear roles or conflicting values create stress and anxiety that can lead to complicated bereavement.
It is repeatedly recommended that a centralised MAiD referral portal would help improve role delineation and enhance delivery of information. Confusion and inconsistency in EOL planning adds anxiety and increases complicated grief.7 27 Although physicians often deal with clinical symptom management of the individual receiving MAiD, a more diverse group of HCPs are needed to provide psychosocial support to family/friends.6 23 30 Bereavement support includes facilitation of communication around death, and counselling or physician referrals if necessary.6 One study highlighted that although physicians believe it is their professional or moral duty to provide bereavement support, they did not have the appropriate time or resources.29 Therefore, many studies suggested that additional roles and responsibilities can be addressed by an interdisciplinary care team, which includes social workers, spiritual care providers, specialised nurses or even ‘death doulas’.23 24 36
Ultimately, when considering how HCPs can ‘support the circle of support,’24 greater structure, funding and resources are needed. Currently, the full obligation and duration of the relationship between HCPs and family/friends is ambiguous and variable.16 Several studies suggested that support for family/friends should be provided before and after MAiD, with trust established over time.24 41 45
Aspects of MAiD grief
MAiD has two distinctive features for family/friends which impact bereavement. Specific to MAiD, there are concerns around disclosure, producing anxiety related to secrecy and stigma. Additionally, with a confirmed date of death, anticipatory grief can manifest during contemplation of MAiD. These facets are commonly referenced in our included studies, although not ubiquitous phenomena in all MAiD cases.
Disclosure and secrecy
The patient, with or without help from family/friends, may decide to keep MAiD a secret. This presents a distinctive feature of MAiD compared with other deaths.5 26 45 Concerns around disclosure include fear of societal stigma,43 concern for relatives’ reactions,6 or avoiding a possibly politically charged topic. Even following MAiD, the fear of being judged negatively impacts bereavement.33 37 For some, MAiD is perceived as a secret that acts as a heavy burden throughout the process.27 37 In an attempt to study disclosure of MAiD quantitatively, Wagner et al 38 reported general social disapproval as having the strongest correlation with post-traumatic stress disorder (PTSD) and complicated grief, whereas family disapproval can correlate with specific aspects of grief. In contrast, there is one study6 involving home MAiD deaths in Toronto, where the majority of family members considered themselves advocates of MAiD and were very public with their decisions. Philippkowski et al 44 used vignettes regarding the mode of death to understand the perspectives of Australian adults. They found mode of death had no interaction effect for emotional reactions, desire for social distance, or expectations of grief symptomatology. Ultimately, Gamondi et al 10 encouraged development of open spaces to discuss death freely and extensively, even long before there would be a medical reason to discuss death.
Anticipatory grief
MAiD provides an opportunity to choose a set date and prepare and plan for EOL. Although anticipatory grief is not unique to MAiD, it is recognised as grief associated with the expectation of an upcoming death. The certainty of an ultimate date intensifies ‘a parade of lasts’ or a countdown.23 43 46 This can both be seen as a blessing to plan goodbyes or as a cause of apprehension. For some, recognising the EOL as the end of suffering can be comforting.28 34
Bereavement support should start before MAiD, and requires a continued and interdisciplinary approach.25 27 46 It is common that family/friends may set aside their own feelings to focus on the patient’s needs.7 Counsellors, resources and education to help recognise the need for support should be readily available and accessible from many locations and throughout the process. Physicians believe that bereavement of an assisted death is unique because of the newness and unfamiliarity of MAiD.29 36 Even when contemplating MAiD, grief of family/friends can start and evolve throughout the process.25 27 34 46
Preparations
Coming to the decision to pursue MAiD is the first step of a long journey. The subsequent preparations, which involve value-based evaluations and logistical arrangements, can be daunting.
Values and decision-making
The contemplation for MAiD can be contentious if there are conflicting values among patient, family/friends and HCPs. The source of conflict can be driven by ambivalence, religious beliefs, desire to have more time, or feeling responsible for a premature death.7 10 26 46 MAiD provides a timed death and a definitive end.16 These concepts seem contrary to societal or medical norms, thus creating conflict. However, belief in patient autonomy can supersede other values. Generally, there is less conflict from family/friends if MAiD seems to fit with longstanding values of the patient.16 28 36
Grief can be proportional to the level of agreement with the decision to undergo MAiD.41 43 On the one hand, family/friends who agreed to participate in MAiD could sometimes feel guilt over being a facilitator of death.23 Even some who were only passively involved felt culpable because they perceived that MAiD broke social rules.37 On the other hand, family/friends who made a joint decision to pursue MAiD alongside the patient felt more accepting of the death.41 Overall, establishing mutual commitment to choice and dignity affected the outlook of family/friends. The confidence of the patient in their decision also influenced the degree of comfort felt by families.31 Even in early stages of precontemplation, family/friends can already start shouldering a heavy burden.7 43
Schutt31 explored the framing of MAiD under either a biomedical or palliative lens. Biomedical decision-making focuses on the individual and the treatment. In contrast, palliative care is driven by relational ethics and involves the agency of family/friends and caregivers while focusing on comfort. They recommended having early conversations involving family/friends around EOL options to minimise suffering for patients and caregivers. This shared decision-making model is supported by many studies to improve the quality of grief and bereavement.5 6 10 41
Logistics and arrangements
The logistics and information required to initiate the MAiD process can be a barrier, complicating how family/friends mentally process the death.30 36 Examples of barriers include having a rapidly progressing disease, undergoing psychiatric evaluation(s), and finding a practitioner who is able to write or administer the prescription. Lack of clarity regarding the process creates unnecessary complexity.7 27 Having committed to a decision regarding MAiD, each step can be an unpredictable hurdle to achieving an established goal.25 33 36 43 The timing and number of eligibility visits require sensitivity and consideration from HCPs. Brown et al 24 recommended opportunities for debrief if assessment outcomes are not what were anticipated. Families/friends of patients who requested but did not receive MAiD had greater regrets regarding the death.42 The fear of the loss of capacity by the patient to proceed with MAiD can be emotionally devastating for all.16 24 27 Although the assessments seem to take a painstakingly long time, family/friends also struggle with processes that are too fast or shorten a lifespan prematurely.10 26 27 46 Oczkowski et al 30 advocated for harmonised referral systems and intake practices as well as systematised targets for time between MAiD assessments to align expectations. Setting expectations and establishing normalcy help foster healthy grieving.
The actual communal planning of death, such as deciding on a date and location, inviting attendees, and finding the appropriate HCPs can seem very strange.7 16 28 37 46 For many family/friends, the planning of a death day was unusual and described as ‘an unpredictable care terrain, (resulting) in emotional uncertainty’.24 28 36 A confirmed date can help facilitate grieving if time is allowed to complete unfinished business, enact wishes, restore lost relationships or celebrate specific events.6 7 28 46 However, issues of lack of available space or human resources to perform MAiD can pose added challenges.27 Purported institutional conscientious objections or unseemly locations negatively impact the experience.25
It is a long path from contemplation to planning the final details of MAiD. Similar to other large life events, finding common ground for expectations can largely impact important memories.
End of life
Death is rarely seen as a ‘good thing’. The death of an individual is seldom celebrated. MAiD allows a reinvention on how death is perceived. The common goal of patients, family/friends and HCPs has shifted towards providing a good death, which can then encourage healthy grieving and bereavement.
Location
An appropriate location is paramount for the comfort of the patient as well as creating appropriate memories of those attending MAiD. A location should allow for the comfort of the patient, minimising physical pain during transportation.25 28 Family/friends may not want to associate their home with death nor want to gather in a hospital. Another logistical barrier arises if institutions that provide residence for the patient prohibits MAiD due to faith-influenced policies or inadequate space for family/friends.24 The location, time and people present must accommodate for the patient’s accessibility, well-being, and privacy. This day is emotionally charged and heavily impacts the bereavement—it is the responsibility of HCPs to set expectations and deliver a good experience for the patient as well as their family/friends.27 35 Some participants of MAiD may have imagined what they believe MAiD would look like. Unexpected outcomes, especially if manifested as patient discomfort, aggressive movements or uncertainty about MAiD effectiveness can easily be a source for mental trauma.35
Ceremony
The death itself can be considered a meaningful ritual or ceremony,23 with focus on the ability to spend time and say goodbye. In comparison with other experiences of death, family/friends believed MAiD was more peaceful and provided an opportunity for a well-controlled legacy or message.26 35 MAiD can seem abnormal with the knowledge that there will be a final goodbye. Nonetheless, MAiD can afford a greater sense of control for family/friends and patients, because there has been time to cognitively and emotionally prepare.43 Furthermore, the knowledge that suffering has been minimised can be a cognitive comfort.6 26 28 31 46
Aftereffects
Overall, many family/friends generally described a positive MAiD experience. Rarely, MAiD was described to be ‘aggressive’ or ‘painful’.35 When finding factors for the perceived positivity around MAiD, reasons include starting the healing process before death, avoiding a prolonged dying process, avoiding escalating care needs, mitigating pain and suffering, and facilitating acceptance through a set date.6 7 16 45 46
Following most deaths, it is expected for family/friends to grieve. The experience and quality of grief can be impacted by the concepts outlined above. An optimised bereavement will minimise the mental and psychiatric distress of family/friends. The psychosocial distress following death has historically been called complex grief, recently called persistent complex bereaved disorder in the Diagnostic and Statistical Manual-5 (DSM-5), and just renamed in March 2022 to be prolonged grief disorder (PGD) in the updated DSM-5-TR.47 Given the changing terminology and varying psychometric scales used to study this phenomenon, the included studies have inconsistently measured PGD, among other forms of distress.
Specific quantitative research on post-MAiD grief and bereavement of family/friends is limited, highlighting the continued invisibility of the patient’s support system.45 Among the included studies, only one39 reported a higher prevalence of PTSD and depression in family/friends who were present at MAiD compared with the general Swiss population. This was measured through validated questionnaires completed by 85 participants, with no direct comparison group. In Switzerland, physicians generally prescribe a lethal dose of medication and patients often administer the medication at home with the help of non-profit organisations.39
Several other quantitative studies did not find greater psychosocial differences following MAiD. Ganzini et al 42 from Oregon directly compared family members of those who had lethal prescription or ingestion (n=95) and family members of those who died from amyotrophic lateral sclerosis (n=63). They found no difference when measuring prolonged grief, depression symptoms, or use of mental health services. Similarly in Quebec, Laperle et al 35 evaluated 25 participants following MAiD compared with 35 participants following death with palliative care. There were no participants who met criteria for PGD. Hashemi et al 6 reported no complicated grief on average for caregivers following a home-based MAiD death in Canada. Participants completed two questionnaires approximately 18 months following MAiD. In a large survey by Swarte et al conducted in the Netherlands,40 bereaved family and friends of cancer patients who died by MAiD had fewer traumatic grief symptoms, and fewer PTSD reactions compared with those who experienced death due to cancer. This study compared 189 family/friends following euthanasia with a control group of 316 family/friends of matched control patients. Lastly, a systematic review5 on grief and mental health of family/friends found similar or lower measures of disordered grief, mental health, and PTSD when comparing people’s bereavement following MAiD compared with other deaths.
Synthesis and conceptual framework
The concepts from our scoping review are highlighted and summarised with our conceptual framework, an image of a dandelion, carefully chosen to represent the ongoing multifaceted aspects of MAiD and the ever-evolving emotions related to grief and bereavement (figure 2).
Figure 2.
Conceptual framework for grief and bereavement of family/friends. The stages of budding, flowering and seeding parallel the preparation, end of life and aftereffects found in our content analyses. The leaves reflect the relationships and the roots represent the distinct aspects of MAiD grief.
The dandelion was chosen to represent MAiD-related grief as a natural flowering plant with a multitude of phases and interpretations. The dandelion reflects differing opinions and levels of acceptance of MAiD. The stages of budding, flowering and seeding parallel the preparations, EOL, and aftereffects found in our content analyses. The thorny leaves reflect the relationships and the many people (family/friends, HCPs) who support the process of death. The roots are hidden beneath the soil, similar to the distinct aspects affecting MAiD-related grief and bereavement. As a dandelion seeds, buds, grows, flowers, and disperses its seeds, the effects of MAiD-related grief metamorphose with time and can potentially have lasting impacts.
Discussion
This scoping review was developed to explore how the experience of MAiD would impact grief and bereavement, as reported in qualitative, quantitative and review literature. Grief associated with all forms of death is normal, although some of the aspects of MAiD may impact how grief is experienced. Included articles with comparative populations demonstrate that MAiD created similar or slightly better experiences for family/friends.6 35 42 A secondary aim of this review is to help develop community bereavement programme and support resources. As such, the methods, theme development, and conceptual framework were guided by a research group and a Canadian virtual workshop including family/friends, the population of study.
Although there is an array of complex emotions and changes felt by family/friends throughout the MAiD journey, we have highlighted five concepts that impact how grief is experienced. First, the relationships between family/friends and the patient and the interactions between family/friends and HCPs can largely impact bereavement. These relationships can further be impacted by differences in values, causing unease or stress during EOL decision-making. Family/friends can be involved, actively helping to make decisions and attending the death, or just be aware without witnessing MAiD. Second, distinctive aspects of MAiD may be causes of future distress. Notably, anticipatory grief may occur before MAiD, and moreover, an aura of secrecy around MAiD can be complicated to navigate. Third, the preparations can become a foreign process that would benefit from establishing simplistic and standard timelines and expectations within each jurisdiction. Fourth, EOLwith MAiD is a challenge but can be a rewarding opportunity for ceremony. Last, the aftereffects for family/friends are poorly studied with mixed results depending on jurisdiction regarding the prevalence of PGD and PTSD. Nonetheless, all studies with comparison groups reported the same or better grief experiences for family/friends following MAiD.
The death of one individual through MAiD involves many people.34 Some HCPs and involved or aware family/friends may hold specific religious or cognitive views regarding MAiD.6 28 43 The manifestation of these views will impact the quality of interactions. Our results demonstrate that unified planning and early shared decision-making of involved family/friends can improve the quality of bereavement.7 31 37
Previous literature has demonstrated that symptoms of grief can be tremendously different based on whether the deceased was a sibling, spouse, close friend or other relationship.48 In their analysis of older people in Switzerland with 10-year follow-up, d’Epinay et al 49 reported severe increases in depressive symptoms after losing a close friend with shared values in comparison to a sibling, but also worsened functional status if an individual lost a child or spouse. Although this review did not include non-English studies, it is important to study diverse family and social structures of different cultures and how MAiD could impact grief or bereavement in those settings. Similarly, the jurisdiction may dictate whether family/friends experience euthanasia or assisted suicide, as well as the cultural acceptance of MAiD. With regard to relationships with HCPs, research has already demonstrated the benefit of HCP support on positive grief reactions, although there are gaps in educating HCPs around MAiD-related grief.33 50 51 Despite being taught about death didactically, Sikstrom et al 51 suggest the need for self-reflection and role-play exercises to reduce the anxiety of HCPs when discussing death and helping family/friends through complex emotions. HCPs can further help reduce confusion by setting expectations early and promoting clarified and harmonised procedures within a jurisdiction.6 7 30 The relative novelty of MAiD alongside the complex and evolving family/friends’ roles (caregiver, MAiD planner, MAiD attendee or bereaved) add nuance when identifying and describing the experiences of grief.
Our review demonstrates that current barriers of MAiD disclosure include fears of social stigma, differing values and beliefs and the novelty of this EOL option.5 26 37 45 MAiD is often considered taboo, similar to other politicised biosocial medical issues, and can cause further isolation following the death of the patient. It is important to reduce stigma with early discussions exploring MAiD options in current EOL support programmes.29 30 It has previously been shown that emotional secrecy can negatively mediate physical and subjective well-being,52 53 whereas social sharing is beneficial to norm clarification and enhanced social cohesion.54 55 There can also be tremendous benefit from peer support when shared experiences can be verbalised. Having informal opportunities for sharing spontaneous feelings is critical for the expression of grief.41 46 56 The ongoing discussion around death, loss and grief throughout the MAiD process can be therapeutic to family/friends.
Anticipatory grief, also known as preloss grief, often occurs prior to death when there is advanced disease or a terminal diagnosis.57 The knowledge of a final farewell can provide cognitive relief or distress.35 In a study of dementia caregivers, factors that augment distressing anticipatory and complicated grief include ambiguity, frustration and guilt.58 Although family counselling already exists to address impending loss, the unique features of an impending MAiD death should be considered in bereavement support as well.
Implications
This review identified distinctive relationships and aspects of MAiD, and enumerated contributors to grief during the preparations, EOL and aftereffects that shape the experience of family/friends.
Identified areas of research translation are presented in the conceptual framework for the purpose of programme and resource development for community organisations. Throughout MAiD, family/friends may be burdened with concerns about stigma resulting in secrecy or experiencing anticipatory grief before the day of MAiD. Guided discussions among all groups at stages of contemplation, decision-making and preparations are beneficial. HCPs can normalise MAiD as a natural and accepted EOL option, supporting anticipatory grief and preloss. In places where non-profit organisations have guided family/friends through MAiD, it may be helpful to connect those grieving with similar experiences. Social sharing can also help set realistic expectations. Unification and harmonisation within jurisdictions of the MAiD evaluation and logistical steps can minimise HCP confusion and differences in practice.
In our review of the aftereffects, only three articles28 36 41 included perspectives of family/friends prior to MAiD. Given the possibility of anticipatory grief, it would be worthwhile to study the prevalence of PGD and other psychosocial measures prior to MAiD. Future research may consider multiple timepoints and documenting experiences iteratively, now that there is a standardised definition within the DSM-5-TR. With an increasing incidence of MAiD, comparisons can also be made within and between different jurisdictions for more nuanced understanding of risk factors.
Strengths and limitations
This study is strengthened by the comprehensive search through academic and grey literature and the inclusion of empiric and review studies. Furthermore, the screening, coding and development of the conceptual framework were completed by a multi-disciplinary group of researchers that included a family member following MAiD, a physician and MAiD provider, palliative-care researchers, social scientists and a lawyer. Theme development was further improved by a Canadian workshop during which comments from MAiD providers, researchers and family/friends were incorporated.
There are several limitations within this review. A scoping review is limited in its methodology and defined scope. First, this review had exclusion criteria for articles that were not in English. Therefore, there are experiences that may be expressed in other languages and cultures regarding grief and bereavement around MAiD that are not captured. Moreover, the included studies themselves had participants of similar ethnic and racial backgrounds. Second, this review suffers from the selection bias of all included studies, largely composed of qualitative semistructured interviews. Although we report that family/friends generally report a positive experience with MAiD,6 7 16 45 46 it is conceivable that those with negative experiences are less likely to participate in research. Third, it is described that anticipatory grief is a distinctive aspect of MAiD which may occur prior to death, yet only three studies included interviews with family/friends of patients who were considering (but had not yet undergone) MAiD. A comprehensive description of MAiD bereavement requires understanding experiences of family/friends at earlier stages. Lastly, although 28 articles are presented here, there are not enough articles with the same research question to compare grief and bereavement experiences between or among jurisdictions. It was outside the scope of this review, but a worthwhile area of further investigation in the future.
Conclusions
This scoping review provides a comprehensive description of qualitative, quantitative and summative literature to generate themes that capture the grief and bereavement experience surrounding MAiD. Concepts around relationships, distinctive aspects of MAiD, preparation, EOL and the aftereffects suggest a need for normalisation of MAiD, and its recognition as one mode of dying among others. Stakeholder feedback emphasised the importance of precise and inclusive language when discussing MAiD. Existing resources should be modified to include MAiD to reduce stigma. Although MAiD is relatively novel as an EOL option in certain jurisdictions, grief is a common occurrence. HCPs can support family/friends with bereavement throughout the MAiD process, which may contain anticipatory grief that starts long before the death. The circle of care should be expanded to address the complicated and changing emotions of family/friends before, during and after MAiD.
Acknowledgments
We would like to thank the workshop participants who contributed their time and expertise to review our key concepts within our scoping review. Thank you to Alicia Freeborn, Allyson Oliphant, Celia Chandler, Chelsea Peddle, Cynthia Clark, David Kenneth Wright, Helen Long, Jill Taylor-Brown, Kath Kortes-Miller, Kelsey Goforth, Lauren Clark, Mary Ellen Macdonald, Megan Sheldon, Nikki Gouzopoulos, Pauline Abrahams, Susa Cadell, and Rosanne Beuthin. We would also like to thank Allyson Oliphant and Helen Long for reviewing the final manuscript.
Footnotes
Twitter: @hanyan2013, @sarina_isenberg, @arimap, @maidhouseto
Contributors: HY and JB contributed equally to this work. Conception of the project and administrative support provided by TH. The manuscript written, and the conceptual framework designed by HY. Data collection and analysis led by JB and performed by JB, SRI, AK, NH, MK and TH. The final manuscript was reviewed by all authors.
Funding: This work was funded by the Canadian Association of MAiD Assessors and Providers (CAMAP).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Grosse C, Grosse A. Assisted suicide: models of legal regulation in selected European countries and the case law of the European Court of human rights. Med Sci Law 2015;55:246–58. 10.1177/0025802414540636 [DOI] [PubMed] [Google Scholar]
- 2. Nicol J, Tiedemann M. Bill C-7: An act to amend the criminal code (medical assistance in dying). In: Parliamentary information ears. Ottawa, Canada: Library of Parliament Legislative Summaries, 2021: p. 20. [Google Scholar]
- 3. Dyer O, White C, García Rada A. Assisted dying: law and practice around the world. BMJ 2015;351:h4481. 10.1136/bmj.h4481 [DOI] [PubMed] [Google Scholar]
- 4. Paterlini M. Paraplegic man is first person to be allowed to die by assisted suicide in Italy. BMJ 2021;375:n2927. 10.1136/bmj.n2927 [DOI] [PubMed] [Google Scholar]
- 5. Andriessen K, Krysinska K, Castelli Dransart DA, et al. Grief after euthanasia and physician-assisted suicide. Crisis 2020;41:255–72. 10.1027/0227-5910/a000630 [DOI] [PubMed] [Google Scholar]
- 6. Hashemi N, Amos E, Lokuge B. Quality of bereavement for caregivers of patients who died by medical assistance in dying at home and the factors impacting their experience: a qualitative study. J Palliat Med 2021;24:1351–7. 10.1089/jpm.2020.0654 [DOI] [PubMed] [Google Scholar]
- 7. Lowers J, Scardaville M, Hughes S, et al. Comparison of the experience of caregiving at end of life or in hastened death: a narrative synthesis review. BMC Palliat Care 2020;19:154. 10.1186/s12904-020-00660-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lapierre S, Castelli Dransart D, St-Amant K, et al. Religiosity and the wish of older adults for physician-assisted suicide. Religions 2018;9:66. 10.3390/rel9030066 [DOI] [Google Scholar]
- 9. Prigerson HO, Jacobs SC. Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In: Stroebe MS, Hansson RO, Stroebe W HS, eds. Handbook of bereavement research: consequences, coping, and care: American psychological association, 2001: 613–45. [Google Scholar]
- 10. Gamondi C, Fusi-Schmidhauser T, Oriani A, et al. Family members' experiences of assisted dying: a systematic literature review with thematic synthesis. Palliat Med 2019;33:1091–105. 10.1177/0269216319857630 [DOI] [PubMed] [Google Scholar]
- 11. Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, et al. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada, and Europe. JAMA 2016;316:79–90. 10.1001/jama.2016.8499 [DOI] [PubMed] [Google Scholar]
- 12. Burgess MM. The medicalization of dying. J Med Philos 1993;18:269–79. 10.1093/jmp/18.3.269 [DOI] [PubMed] [Google Scholar]
- 13. End of life choice act 2019, 2019.
- 14. Choices C. States where medical aid in dying is authorized, 2021. Available: https://compassionandchoices.org/resources/states-or-territories-where-medical-aid-in-dying-is-authorized
- 15. Technology QUo. voluntary assisted dying: Australian centre for health law research, 2021. Available: https://end-of-life.qut.edu.au/assisteddying
- 16. Roest B, Trappenburg M, Leget C. The involvement of family in the Dutch practice of euthanasia and physician assisted suicide: a systematic mixed studies review. BMC Med Ethics 2019;20:23. 10.1186/s12910-019-0361-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 18. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 20. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 21. Morgan DL. Qualitative content analysis: a guide to paths not taken. Qual Health Res 1993;3:112–21. 10.1177/104973239300300107 [DOI] [PubMed] [Google Scholar]
- 22. NVivo qualitative data analysis software 2015.
- 23. Beuthin R, Bruce A, Thompson M, et al. Experiences of grief-bereavement after a medically assisted death in Canada: bringing death to life. Death Stud 2022;46:1–10. 10.1080/07481187.2021.1876790 [DOI] [PubMed] [Google Scholar]
- 24. Brown J, Goodridge D, Harrison A, et al. Care considerations in a Patient- and Family-Centered medical assistance in dying program. J Palliat Care 2022;37:341–51. 10.1177/0825859720951661 [DOI] [PubMed] [Google Scholar]
- 25. Brown J, Goodridge D, Harrison A, et al. Medical assistance in dying: patients', families', and health care providers' perspectives on access and care delivery. J Palliat Med 2020;23:1468–77. 10.1089/jpm.2019.0509 [DOI] [PubMed] [Google Scholar]
- 26. Frolic AN, Swinton M, Murray L, et al. Double-Edged MAID death family legacy: a qualitative descriptive study. BMJ Support Palliat Care 2020. doi: 10.1136/bmjspcare-2020-002648. [Epub ahead of print: 18 Dec 2020]. [DOI] [PubMed] [Google Scholar]
- 27. Hales BM, Bean S, Isenberg-Grzeda E, et al. Improving the medical assistance in dying (MAID) process: a qualitative study of family caregiver perspectives. Palliat Support Care 2019;17:590–5. 10.1017/S147895151900004X [DOI] [PubMed] [Google Scholar]
- 28. Holmes S, Wiebe E, Shaw J, et al. Exploring the experience of supporting a loved one through a medically assisted death in Canada. Can Fam Physician 2018;64:387–93. [PMC free article] [PubMed] [Google Scholar]
- 29. Trouton K, Beuthin R, Thompson M. Attitudes and expectations regarding bereavement support for patients, family members, and friends: findings from a survey of MAID providers. BC Med J 2020;62:18–23. [Google Scholar]
- 30. Oczkowski SJW, Crawshaw D, Austin P, et al. How we can improve the quality of care for patients requesting medical assistance in dying: a qualitative study of health care providers. J Pain Symptom Manage 2021;61:513–21. 10.1016/j.jpainsymman.2020.08.018 [DOI] [PubMed] [Google Scholar]
- 31. Schutt KCH. Exploring how family members experience medical assistance in dying (MAID): Trinity Western university 2011.
- 32. Network OHT . Impact of medical assistance in dying on family and friends 2017.
- 33. Ho A, Joolaee S, Jameson K, et al. The seismic shift in end-of-life care: palliative care challenges in the era of medical assistance in dying. J Palliat Med 2021;24:189–94. 10.1089/jpm.2020.0185 [DOI] [PubMed] [Google Scholar]
- 34. Laperle P, Achille M, Ummel D. The relational landscape of bereavement after anticipated death: an interpretive model. Death Stud 2021:1–13. 10.1080/07481187.2021.1975177 [DOI] [PubMed] [Google Scholar]
- 35. Laperle P, Achille M, Ummel D. To lose a Loved one by medical assistance in dying or by natural death with palliative care: a mixed methods comparison of grief experiences. Omega 2022;302228221085191:003022282210851. 10.1177/00302228221085191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Smolej E, Malozewski M, McKendry S, et al. A qualitative study exploring family caregivers' support needs in the context of medical assistance in dying. Palliat Support Care 2022:1–7. 10.1017/S1478951522000116 [DOI] [PubMed] [Google Scholar]
- 37. Gamondi C, Pott M, Forbes K, et al. Exploring the experiences of bereaved families involved in assisted suicide in southern Switzerland: a qualitative study. BMJ Support Palliat Care 2015;5:146–52. 10.1136/bmjspcare-2013-000483 [DOI] [PubMed] [Google Scholar]
- 38. Wagner B, Keller V, Knaevelsrud C, et al. Social acknowledgement as a predictor of post-traumatic stress and complicated grief after witnessing assisted suicide. Int J Soc Psychiatry 2012;58:381–5. 10.1177/0020764011400791 [DOI] [PubMed] [Google Scholar]
- 39. Wagner B, Müller J, Maercker A. Death by Request in Switzerland: posttraumatic stress disorder and complicated grief after witnessing assisted suicide. Eur Psychiatry 2012;27:542–6. 10.1016/j.eurpsy.2010.12.003 [DOI] [PubMed] [Google Scholar]
- 40. Swarte NB, van der Lee ML, van der Bom JG, et al. Effects of euthanasia on the bereaved family and friends: a cross sectional study. BMJ 2003;327:189. 10.1136/bmj.327.7408.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pronk R, Willems DL, van de Vathorst S. What about us? experiences of relatives regarding physician-assisted death for patients suffering from mental illness: a qualitative study. Cult Med Psychiatry 2021;41. 10.1007/s11013-021-09762-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ganzini L, Goy ER, Dobscha SK, et al. Mental health outcomes of family members of Oregonians who Request physician aid in dying. J Pain Symptom Manage 2009;38:807–15. 10.1016/j.jpainsymman.2009.04.026 [DOI] [PubMed] [Google Scholar]
- 43. Srinivasan EG. Bereavement and the Oregon death with dignity act: how does assisted death impact grief? Death Stud 2019;43:647–55. 10.1080/07481187.2018.1511636 [DOI] [PubMed] [Google Scholar]
- 44. Philippkowski S, O'Connor M, Eisma MC, et al. Does voluntary assisted dying cause public stigma for the bereaved? A vignette-based experiment. Palliat Support Care 2021;19:558–62. 10.1017/S1478951520001352 [DOI] [PubMed] [Google Scholar]
- 45. Goldberg R, Nissim R, An E, et al. Impact of medical assistance in dying (MAID) on family caregivers. BMJ Support Palliat Care 2021;11:107–14. 10.1136/bmjspcare-2018-001686 [DOI] [PubMed] [Google Scholar]
- 46. Levac, Colquhoun, O_Brien - 2010 - Scoping studies advancing the methodology-annotated(1).pdf 2010. [DOI] [PMC free article] [PubMed]
- 47. Lenferink LIM, Eisma MC, Smid GE, et al. Valid measurement of DSM-5 persistent complex bereavement disorder and DSM-5-TR and ICD-11 prolonged grief disorder: the traumatic grief Inventory-Self report plus (TGI-SR+). Compr Psychiatry 2022;112:152281. 10.1016/j.comppsych.2021.152281 [DOI] [PubMed] [Google Scholar]
- 48. Weiss R. Grief, bonds, and relationships. In: Stroebe MS, Hansson RO, Stroebe W, et al., eds. Handbook of bereavement research: Conssequences, coping, and care: American psychological association, 2001: 47–62. [Google Scholar]
- 49. d'Epinay CJL, Cavalli S, Guillet LA. Bereavement in very old age: impact on health and relationships of the loss of a spouse, a Child, a sibling, or a close Friend. Omega 2009;60:301–25. 10.2190/OM.60.4.a [DOI] [PubMed] [Google Scholar]
- 50. Gordon TA. Good grief: exploring the dimensionality of grief experiences and social work support. J Soc Work End Life Palliat Care 2013;9:27–42. 10.1080/15524256.2012.758607 [DOI] [PubMed] [Google Scholar]
- 51. Sikstrom L, Saikaly R, Ferguson G, et al. Being there: a scoping review of grief support training in medical education. PLoS One 2019;14:e0224325. 10.1371/journal.pone.0224325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Finkenauer C, Rimé B. Keeping emotional memories secret: health and subjective well-being when emotions are not shared. J Health Psychol 1998;3:47–58. 10.1177/135910539800300104 [DOI] [PubMed] [Google Scholar]
- 53. Slepian ML. A process model of having and keeping secrets. Psychol Rev 2022;129:542-563. 10.1037/rev0000282 [DOI] [PubMed] [Google Scholar]
- 54. Rimé B, Bouchat P, Paquot L, et al. Intrapersonal, interpersonal, and social outcomes of the social sharing of emotion. Curr Opin Psychol 2020;31:127–34. 10.1016/j.copsyc.2019.08.024 [DOI] [PubMed] [Google Scholar]
- 55. Yzerbyt V, Kuppens T, Mathieu B. When talking makes you feel like a group: the emergence of group-based emotions. Cogn Emot 2016;30:33–50. 10.1080/02699931.2015.1045454 [DOI] [PubMed] [Google Scholar]
- 56. Breen LJ, O'Connor M. Acts of resistance: breaking the silence of grief following traffic crash fatalities. Death Stud 2010;34:30–53. 10.1080/07481180903372384 [DOI] [PubMed] [Google Scholar]
- 57. Nielsen MK, Neergaard MA, Jensen AB, et al. Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin Psychol Rev 2016;44:75–93. 10.1016/j.cpr.2016.01.002 [DOI] [PubMed] [Google Scholar]
- 58. Chan D, Livingston G, Jones L, et al. Grief reactions in dementia carers: a systematic review. Int J Geriatr Psychiatry 2013;28:1–17. 10.1002/gps.3795 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
spcare-2022-003715supp001.pdf (260.8KB, pdf)
spcare-2022-003715supp002.pdf (246.1KB, pdf)
spcare-2022-003715supp003.pdf (56.5KB, pdf)