Abstract
Background:
Extreme heat and air pollution are important human health concerns; exposure can affect mental and physical well-being, particularly during periods of co-occurrence. Yet, the impacts on people are largely determined by underlying health conditions, coupled with the length and intensity of exposure. Preexisting adverse health conditions and prolonged exposure times are more common for people experiencing homelessness, particularly those with intersectional identity characteristics (e.g., disease, ability, age, etc.). Partially due to methodological limitations, such as data scarcity, there is a lack of research at the intersection of this at-risk population within the climate-health domain.
Objectives:
We have three distinct objectives throughout this article: a) to advance critical discussions around the state of concurrent high heat and air pollution exposure research as it relates to people experiencing homelessness; b) to assert the importance of heat and air pollution exposure research among a highly vulnerable, too-often homogenized population—people experiencing homelessness; and c) to underline challenges in this area of study while presenting potential ways to address such shortcomings.
Discussion:
The health insights from concurrent air pollution and heat exposure studies are consequential when studying unhoused communities who are already overexposed to harmful environmental conditions. Without holistic data sets and more advanced methods to study concurrent exposures, appropriate and targeted prevention and intervention strategies cannot be developed to protect this at-risk population. We highlight that a) concurrent high heat and air pollution exposure research among people experiencing homelessness is significantly underdeveloped considering the pressing human health implications; b) the severity of physiological responses elicited by high heat and air pollution are predicated on exposure intensity and time, and thus people without means of seeking climate-controlled shelter are most at risk; and c) collaboration among transdisciplinary teams is needed to resolve data resolution issues and enable targeted prevention and intervention strategies. https://doi.org/10.1289/EHP13402
Introduction
Extreme heat and air pollution exposures are well-known risks to human health globally.1,2 Together or separately, these environmental exposures can increase health risks and negatively impact overall well-being, with adverse health effects amplified during periods of co-occurrence.3–5 Those with stable and adequate shelter are afforded the ability to avoid prolonged exposure times. However, those without stable housing conditions may face lengthier stints of exposure to high heat and air pollution.6 Heightened exposure can interact with preexisting health conditions (e.g., comorbidities such as asthma or hypertension) to increase the overall risk of adverse health outcomes, as shown by studies on the general population.7–9 For example, Crank et al.7 found that 3.45% of schizophrenia hospitalizations in Maricopa County, Arizona were attributable to nonoptimal nighttime temperatures—a health care cost of nearly a year. Unfortunately, comorbidities are far more prevalent among those experiencing homelessness10,11 due to a lack of necessary resources to stave off undesirable health conditions.12,13 Further, no studies, to our knowledge, holistically examine the co-occurrence of high heat and air pollution exposures to those experiencing homelessness.
Extreme urban heat events are expected to continue increasing in the coming years due to a combination of climate change14,15 and urban sprawl.14–16 Higher temperatures generally increase ground-level ozone and particulate pollution due to higher sunlight- and temperature-driven photochemical reactions and drier conditions, respectively.17–19 Thus, the human health implications of co-exposures are of growing concern, especially in conjunction with projected population growth. Yet such exposure research focused on one of the most vulnerable populations—those experiencing unsheltered homelessness—is understudied.20,21 Indeed, our ability to quantify exposure to heat22 and air pollution23 at an individual level is complicated by variations in mobility across the general populace (as laid out in many recent studies23–26), but basic scientific understanding of climate exposures—for a myriad of social and political reasons—is far less mature for people experiencing homelessness.6 Therefore, we aim to a) advance critical discourse around the state of concurrent high heat and air pollution exposure research as it relates to populations at high risk of unmitigated exposure—focusing on the shortcomings of work pertaining to people experiencing homelessness—within a United States context; b) assert the importance of heat and air pollution exposure research among a highly vulnerable, too-often homogenized population of people experiencing homelessness; and c) highlight challenges in this area of study and present potential innovations in research and practice that can begin to address data gaps.
Scope
To advance these discussions, we focus on people experiencing homelessness in urban areas encountering high heat and air pollution levels within the United States. High heat and air pollution can add stress to the same physiological systems (e.g., alterations to cardiac autonomic control) within the human body,1,27 although at different time horizons, and are common dual hazards in American cities.28 People experiencing homelessness more often reside in urban areas and are one of the most exposed populations to poor environmental conditions.29 Given the unique sociopolitical underpinnings of this issue, starting to address this issue with a national scope allows more focus on the fundamental research challenges. Similarly, the outcomes and innovations we consider are limited to this predefined scope.
Definitions
Climate and social morphology—in terms of where and how people live, work, and govern—have a reciprocal relationship that alters the distribution of environmental co-exposures. Limited affordable housing, coupled with the rising cost of living, are some of the reinforcing mechanisms that alter the number of people experiencing some form of homelessness within the United States.30 As temperatures increase and poor urban air quality remains commonplace,15,17 individuals experiencing homelessness will face more intense, prolonged periods of unhealthy living conditions in many locations.6,20
There are a variety of homelessness definitions—and terms utilized to depict a person’s housing status—depending on discipline, context, and organization; the implications for US Department of Housing and Urban Development (HUD) definitions are perhaps the most broad and far-reaching (Table 1). Although individuals in these groups find themselves in precarious housing situations for disparate reasons, the commonality between groups is the inability to retain safe and stable shelter. In terms of environment, those most exposed to unhealthy conditions are the people who spend the most amount of their time unsheltered. Despite this, our work is relevant to all groups within these HUD distinctions, as they each find themselves at increased exposure relative to the general populace.20 Owing to the diverse drivers, identities, and health statuses underpinning the experiences of people who are experiencing homelessness, consideration of definitional complexities is paramount among climate, health, and social science researchers if the findings are to be relevant for practitioners.
Table 1.
Simplified “categories” of homelessness from the department of housing and urban development (HUD) definitions (see https://files.hudexchange.info/resources/documents/HomelessDefinition_RecordkeepingRequirementsandCriteria.pdf).
| Category | Name | Definition |
|---|---|---|
| 1 | Literally homeless | Primary nighttime residence is public and/or not meant for human habitation; the predominant public perception of homelessness. |
| 2 | Imminent risk of homelessness | Primary nighttime residence will be lost if immediate assistance is not provided; an incalculable and growing subsect of the population due to the COVID-19 pandemic and inflation. |
| 3 | Homeless under other federal statutes | Unaided youth under 25 years of age, or families with children, who lack housing stability; a rather vague category that is hard for those outside of the department to define. |
| 4 | Fleeing/attempting to flee domestic violence | Facing domestic abuse without the support network or resources necessary to obtain residency away from the abuser; an incalculable subsect of the population that is, most likely, underestimated. |
The Associations between Heat and Human Health
To better understand the societal consequences of extreme heat, epidemiology and demography have leveraged meteorological data sets. A paradigm shift spurred by interdisciplinary research over the last two decades suggests that many climate-related health outcomes are influenced by socioenvironmental characteristics, not merely the mercury in the thermometer.31 Widely referred to as social determinants of health, studies find that adverse health outcomes during times of high air temperatures are primarily attributed to age, underlying health status, occupation, income,31–35 and access to air conditioning.36 Although not addressed at length in this commentary, integrating the social determinants of health framework is imperative for advancing our understanding of concurrent exposures to high heat and air pollution as social factors that underpin substantial amounts of individual- and community-level risk. Older individuals (typically those ) are most at risk, as overall health tends to decline with age and comorbidities generally become more prevalent.34,35,37 In particular, cardiovascular and pulmonary ailments increase the risk of hospitalization during warm, humid days.34,38 Elevated air temperature exacerbating preexisting conditions is largely contingent upon exposure duration,33 which can be attributed to occupation and living conditions.31 Put succinctly, it is not the temperature itself but rather the vulnerability (or risk profile) of an individual during times of heightened temperatures that largely dictates heat-related health outcomes.39 As social science literature has unveiled, vulnerabilities are often a product of intersectional identity characteristics40—climatic vulnerabilities are no different.39
Geography also plays a role in heat risk, as communities exhibit unique perceptions and behaviors to adjust to extreme heat.41–43 Further, there are well-known physiological adaptations (acclimatization)—such as enhanced sweating, improved skin blood flow, and reduced cardiovascular strain—to the heat that people gain when exposed routinely to high heat for long periods and/or during exercise.44 Such adaptations would be expected in those spending long periods in extreme heat and are noted as important adaptation processes by the Intergovernmental Panel on Climate Change (IPCC),45 yet there are limits. For example, Fletcher et al.46 found that a 5°F increase in temperature was associated with a 9% increase in hospitalizations for renal disease in New York State between 1991 and 2004, approximately double the increase seen in similar studies for a typically warmer California. Such discoveries lead to the understanding that heat-related health research is far broader than mere episodes of hyperthermia. Despite the nuanced findings in risk factors, the majority of studies continue to focus on only the worst health outcomes: hospitalizations9,11,37,47 and mortality.31,39,48 Additionally, most studies are cross-sectional, thus missing out on spatial and temporal dimensions (i.e., are incongruent in space and time).22,49 Intersectional identity characteristics and geographic factors are particularly pertinent for the environmental vulnerabilities of people experiencing homelessness, as they often find themselves in unfriendly climate spaces50 and at higher risk for diseases like substance abuse disorders.10,29
Air Pollution and Its Impacts on Health
Early air pollution research—mostly situated in Europe during the mid-20th century—attempted to quantify the impacts of air pollution on human health,51 with a particular focus on urban areas where industrial-residential interfaces were commonplace.52 Pollutants such as particulate matter (most commonly examined at sizes and in diameter, or and , respectively) pose varying levels of risk to human health, with increased exposure adding to the long-term chances of developing respiratory and/or cardiovascular diseases like chronic obstructive pulmonary disease (commonly referred to as COPD).53 Another air pollutant strongly linked to health is ground-level ozone, an inorganic molecule that can infiltrate the respiratory tract and, depending on concentrations, cause inflammation and cell damage.54
Studies link personal risk factors—typically chronic health conditions such as pulmonary and cardiovascular diseases—to air pollution-related, acute health outcomes.55,56 Risk is largely associated with age, as the respiratory system is most vulnerable in younger and older age groups.51,57 In addition to personal characteristics, air pollution impacts differ spatially and temporally. Pollutant concentrations vary with anthropogenic output and weather conditions, creating seasonal and interannual variations in health risks.17,58 Perhaps most importantly, regardless of which pollutant type someone is exposed to, the length of exposure time throughout one’s lifespan is of consequence in determining health outcomes.27,56 Prolonged exposure can often be attributed to indoor-outdoor activity times dictated by occupation and/or outdoor comfortability (i.e., an area’s conduciveness to outdoor activities based on its climate).59 Contemporary work aims to further reconcile the importance of exposure time and acute vs. long-term consequences. Although much of the general populace can avoid prolonged time outdoors during dangerous air quality, many people experiencing homelessness have less autonomy in mediating their exposure. Thus, individuals experiencing homelessness should be top of mind when considering the impacts of poor air quality.
Consequences of Co-occurring Heat and Air Pollution
Since understanding the consequential effects of heat and air pollution and the synergistic implications for human health, research has begun investigating concurrent episodes of these hazards and resulting health outcomes. In particular, many studies have focused on elevated temperatures and high ozone due to the connections between sunny, warm, stable conditions and elevated ozone concentrations.4,9 However, particulate matter, nitrogen dioxide, sulfur dioxide, and carbon monoxide have also been investigated during heat waves.3,60,61 Findings from Kahle et al.62 indicate that elevated temperatures may inhibit the body’s ability to repair damage caused by pollutants, thus increasing the risk of adverse effects, especially for those with preexisting conditions. These concerns become all the more salient in urban areas where city design can alter ventilation and heat storage within the urban canopy layer, altering the natural flow of pollutants and excess heat dissipation.28,63 Tall building heights and narrow urban canyons—encapsulating a landscape of industry and other primary emitters—often reduce air flow, limiting ventilation and promoting pollutant buildup.63,64 Dense building materials simultaneously promote heat retention, as urban elements such as metal, asphalt, and concrete possess high thermal capacities, increasing the maximum temperature potential in cities.16,65 Owing to the health implications of these simultaneous exposures, some researchers have called for combined heat and acute air pollution research,60,66 as well as joint public health warning systems.67
The bulk of this growing research reiterates the highly heterogeneous impacts of concurrent events based on local geography, health, and other demographic factors.5,9,68–70 Additionally, exposure times as a contributing factor to health outcomes are reiterated, as reductions in outdoor exposure and access to air conditioning were seen to reduce mortality and morbidity.5,71 A conceptual model (Figure 1) of these drivers illustrates the complex, synergistic nature of socioenvironmental factors in dictating health outcomes relating to elevated air temperature and air pollution exposures. Based on this illustration, housing—a primary determinant of health12—is an overarching factor dictating the different exposure pathways for individuals. Social factors influence an individual’s access to housing, whereas environmental variables alter the quality of that housing; access and quality intersect to influence environmental exposure pathways (such as indoor/outdoor time).
Figure 1.
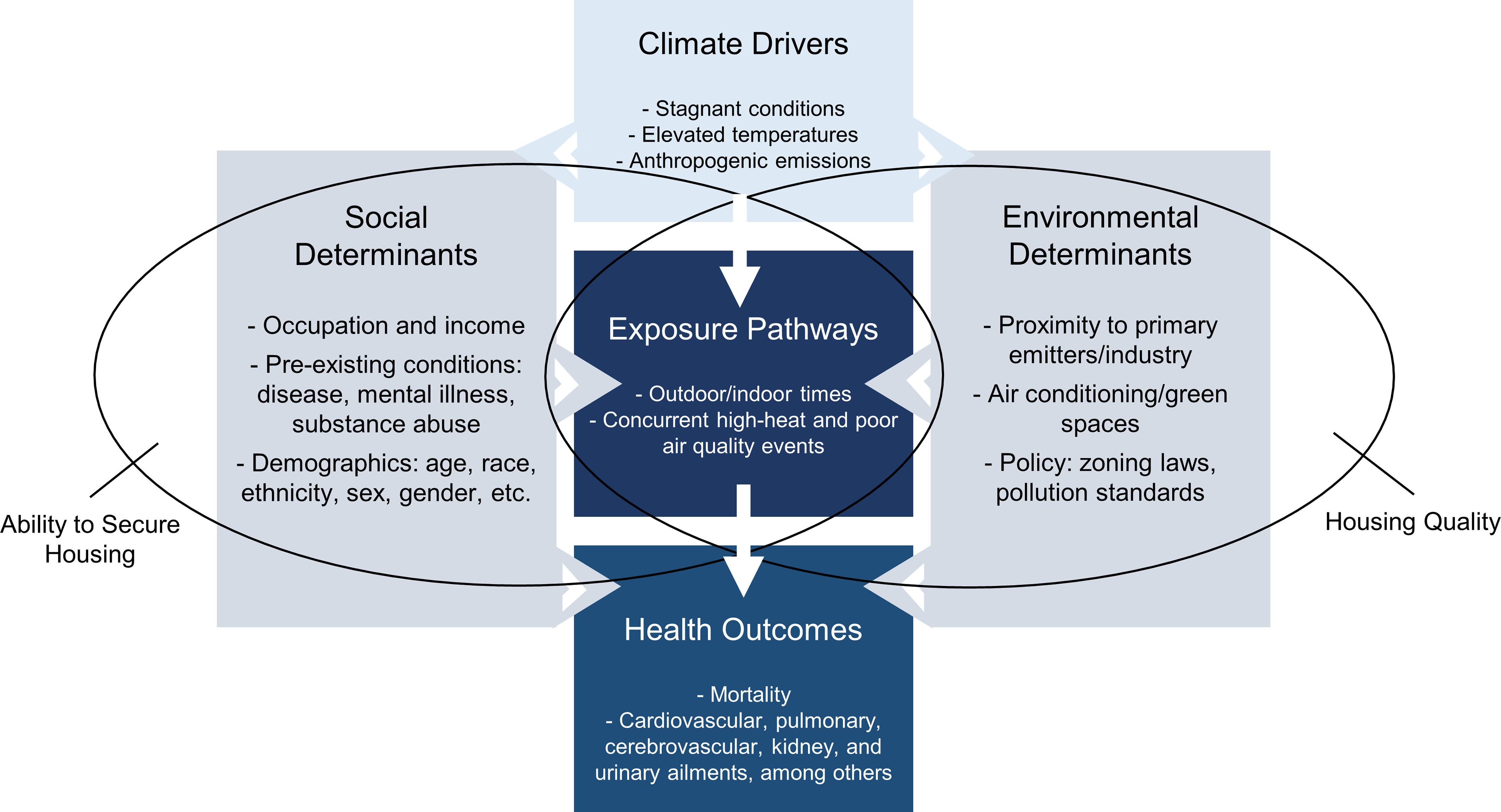
Climate drivers of heat and air pollution. Social and environmental factors play a substantial role in moderating health outcomes related to high temperatures and elevated levels of air pollution by increasing the amount of time an individual is exposed. The overlapping Venn diagram illustrates how social factors influence the ability of an individual to secure housing, whereas environmental factors determine the quality of such housing; the intersection of housing security and quality mediates environmental exposure pathways.
Discussion
Homelessness and Concurrent High Heat and Air Pollution
With the importance of economic status, underlying health conditions, and length of exposure to adverse health outcomes, the lack of studies involving people who are unhoused exposes a gap in our understanding of how this population experiences vulnerability. Research shows the socioeconomic disparities in air pollution and temperatures among the housed community at a census block/zip code level.72–74 However, it is far less understood how these discrepancies express themselves in more highly exposed populations, which may be missing due to the difficulty of surveying people who are unhoused in the same way as those who might take household surveys.
Individuals experiencing homelessness are more likely to visit the hospital11,75 compared to their housed counterparts—a trend that is exacerbated during heat waves.76 Underlying health conditions, such as mental illness and substance use disorder, are common catalysts for hospitalization among people who find themselves homeless.11 Additionally, cardiovascular conditions are particularly pervasive in this population.6 The risks related to air pollution and heat outlined above, in conjunction with the prevalence of preexisting conditions and increased exposure times, should theoretically impart more adverse environmental health risks to people experiencing homelessness. However, the actualities of such assumptions have yet to be broadly substantiated (Figure 2). Much of the inadequate understanding concerning this population can be attributable to the lack of reliable data available at finer spatial scales, a common drawback noted among heat and air pollution exposure research in general.22,27,29,49
Figure 2.
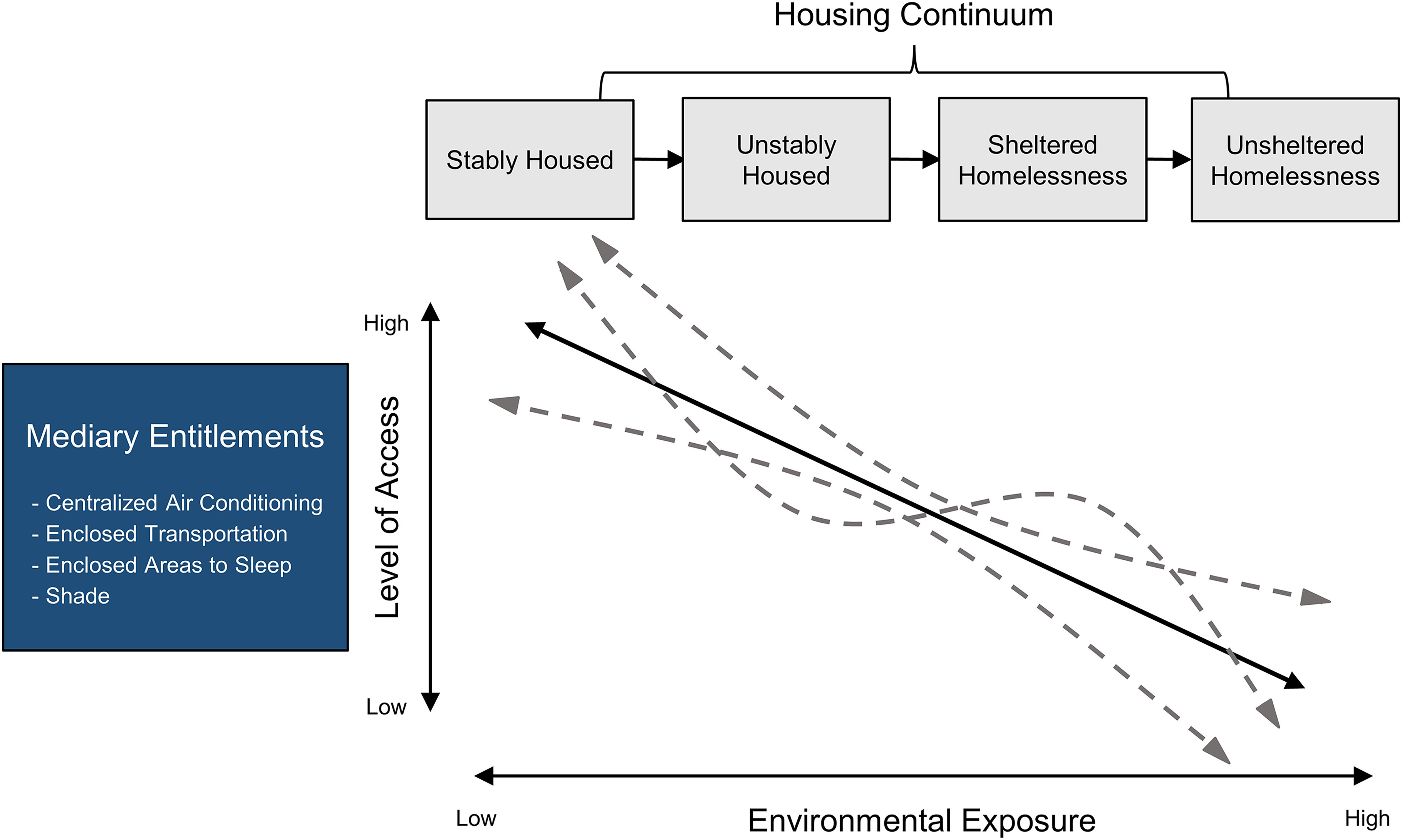
Heat and air pollution exposure as a function of housing status. The diagram illustrates how access to mediating factors (i.e., resources to help an individual cope with environmental hazards) differs based on housing status, impacting environmental exposures (such as heat and air pollution). The solid line denotes the assumption of decreasing access to mediary factors as housing status destabilizes. The dashed, curved lines depict the multitude of lived actualities when considering the role of intersectional identity characteristics (e.g., race, sex, income, disease, etc.) that coexist with housing status to create lived experiences.
Challenges in Environmental Health Research
The main obstacles in environmental health research involve data resolution, quality, and recording consistency. In some cases, cause of death data are not available or inconclusive (e.g., Medicare data—a large and often-used data provider—does not include the underlying cause of death and only reports individuals enrolled in Medicare).56 Even when such data are available, the quality may suffer due to inconsistencies in how the cause of death is determined. Of deaths recorded in 297 US counties between 1997 and 2006, Weinberger et al.77 estimate that 0.44% of deaths were caused by heat ( heat-attributable deaths per year). In comparison, the Centers for Disease Control and Prevention (CDC) estimated that people died due to heat each year in roughly (1999–2009) the same period.77 This discrepancy shows the lack of methodological consilience among heat attribution studies and points to potential undercounts of historical heat-related deaths. Even the numbers found by Weinberger et al.77 are likely higher or lower than reality, as the study did not consider interactions with air pollution.
A common practice in environmental health studies on heat and air pollution is to use publicly available medical data—such as data from a local municipality’s public health department—that are limited to formally reported cases of mortality and morbidity, making it difficult to find data representative of “hidden” populations, such as people experiencing homelessness.31 Further compounding data complexities, medical data must be paired with air pollution data. Typically, researchers choose to utilize existing monitoring networks, as hyperlocal data are scarce and difficult to construct ad hoc. Although networks are constantly improving, there are often questions about spatial coverage, interpolation strategies, and overall data quality, among others.78
Despite added complexity, health data become more informative and better reflect reality when combined with demographic data, such as housing status and related socioeconomic information, collected during admissions to the emergency room or for death reports. In addition to questions about methods, the lack of standardization in vernacular—such as “heat-related,” “heat-caused,” “vulnerable,” “susceptible,” and “at risk”—makes agreement across studies difficult to ascertain.79 These terms only further complicate the discrepancies among who is classified as “homeless” within society. When interacting with people experiencing homelessness through surveys or interviews, researchers are limited by their ability to build trust with enough individuals to collect representative data ethically. A historical legacy of stigmatization, concern for security on the streets,80 and previous negative interactions with service providers81 are some of the many reasons it can be difficult to establish trust with people who are experiencing homelessness. Further, individuals may fear that participating in a study could make them easier to locate, potentially putting them at risk of retribution or abuse from law enforcement, other individuals experiencing homelessness, or the community more broadly.82 Those most vulnerable are often those most difficult to locate and engage with (i.e., those accessing services are easier to find but are expected to be less at risk than people unaware or choosing not to access services).83,84 Lastly, all forms of survey and interview questions inject limitations and/or biases into responses and fail to fully contextualize lived experience; it can be difficult to capture the role of housing status and how the synergy of identities implicates itself in climate vulnerability.12
Perhaps some of the environmental health research shortcomings can be attributed to a lack of collaboration and a failure to embrace transdisciplinarity—bridging diverse disciplines and practitioners from different sectors of society—when designing studies and updating data sets. Much of the scientific literature calls for such collaboration efforts to close current knowledge gaps.39,85–87 In addition to study design questions, there is insufficient research on people experiencing homelessness in relation to climate, and existing studies lack rigor despite the community’s high-risk status.10,88 Currently, to the authors’ knowledge, no study investigates the implications of concurrent heat and high air pollution events for individuals experiencing homelessness and the impacts on their health. Although some papers, such as Ramin and Svoboda,6 draw connections between concurrent extreme temperature and elevated air pollution, a systematic review of reviews shows that targeted data are needed in this space.20 The lack of research is, at least partially, attributable to the challenges that arise when considering a historically underserved population—how do you collect accurate, representative data?
Early Attempts to Connect Exposure to Experience
As noted above, challenges in connecting fine-scale exposures (heat or air pollution) to health persist when studying the general population. These issues are exacerbated when studying populations that do not have an address and/or may be transient. Despite these complexities, three studies present potential, although limited, tools for expanding research among people who are experiencing homelessness. Longo et al.89 equipped 10 people experiencing homelessness in Phoenix, Arizona with iButton air temperature sensors to highlight the lack of data surrounding personal heat exposure metrics of unhoused community members. In a separate study, MacMurdo et al.90 estimated personal air pollution exposure among homeless individuals utilizing local knowledge maps curated by 62 participants and state stationary source emission data.
The results from these studies indicate that each individual experiences considerably different exposures due to their unique travel patterns, time outside, and location preferences.89,90 These findings mimic the exposure heterogeneity seen within the housed community. However, compared to a housed group of students, those experiencing homelessness who were a part of the study by Longo et al.89 experienced more than double the theoretical heat stress during the day. There was also a direct relation between air temperature exposures and the type of homelessness experienced, as those who were unsheltered experienced the highest levels of exposure to high air temperatures during the study period.89 In addition to high temperatures, a study in Tulare County, California found that those experiencing unsheltered homelessness were exposed to more pollutants than what is traditionally measured by ambient air pollution monitoring, as they spend the bulk of their time (both day and night) within of primary emitters.90
A true measure of heat stress requires additional meteorological variables, including absolute humidity, mean radiant temperature, and wind speed.49,91 Longo et al.89 use air temperature, yet refer to heat stress, defined as the number of minutes someone would theoretically be exposed to air temperatures above 29°C following guidance from previous research.92,93 In addition, the study lacks a large, comprehensive sample size and only uses high-frequency sampling over a 1-week period. The findings from MacMurdo et al.90 face similar constraints on sample size and were limited by the reliability of interpolated, sparse air quality data. Despite this, the studies succeed in their mission—pointing out the need for further research involving people experiencing homelessness—while raising important questions and considerations for climate-health research among people experiencing homelessness.
Using a mixed methods approach, Gabbe et al.94 leveraged existing data sets by combining sociodemographic data (census, point-in-time counts, emergency calls, etc.) with land surface temperatures (LST) and shade cover to guide targeted community-needs assessment interviews. The study unveils that heat perceptions are not of consequential importance to individuals experiencing homelessness in Santa Clara County, California when deciding where to stay, despite most residing in areas with increased heat risk. Although this study provides generalized (census-tract level) findings and subjective “heat risk” variables, it thoroughly outlines a methodology for more targeted outreach and innovation strategies. Further, Gabbe et al.94 provide an in-depth explanation of the challenges of finding and mapping data for people experiencing homelessness.
These preliminary studies with different methodological approaches highlight the importance of the diverse environmental exposures—such as uninhibited sunshine, industrial and vehicular air pollution, and the heat from surrounding surfaces—experienced by people experiencing homelessness and their potential implications for health outcomes. Despite their imperfections and difficulty to deploy at scale, hyperlocal instrumentation, targeted surveying, and local knowledge maps are illustrated as a starting point for researchers hoping to expand our knowledge of environmental exposures among people experiencing homelessness. Given that, to the authors’ knowledge, only three small studies exist, and there is a need for more research in this area, particularly research that marries air pollution and heat metrics when studying individuals experiencing homelessness.
Implications of Better Environmental and Health Data
Although there are regional, interannual, and decadal variations in air pollution due to natural climate variability, a warming world has the potential to alter the ventilation and dilution of pollutants.17 Variations in the prevalence and severity of heat waves and elevated air pollution events are of concern for those experiencing unsheltered homelessness due to their lack of social and physical coping infrastructure.6
Higher susceptibility—via potentially poor underlying health and a lack of access to health care and other resources—coupled with greater exposure to climate-related dangers among those experiencing homelessness necessitates more targeted research that embraces community-embedded methodologies. Research must fill the gaps—of which there are many—in co-occurring high heat and air pollution events to provide more context to the higher-than-average hospitalization rates among those experiencing homelessness during dangerous meteorological set-ups.11 Embracing place-based techniques, such as hyperlocal measurements, surveys, and health data collection, will allow for targeted approaches that ameliorate inequitable climate burdens.
For example, Karanja et al.95 investigated the efficacy of six different tent coverings commonly used by unhoused communities throughout Phoenix, Arizona in moderating in-tent air temperature. Leveraging in situ measurements, this study suggests that not all tent cover (shading) materials are created equal; some materials can exacerbate exposure to air temperature during the summer months.95 This same type of work could be done across other shelter domains (e.g., cars) and for environmental exposures beyond heat (i.e., various air pollutants). Exposures to heat and air pollution in various shelter types would be expected to decrease as climate control capabilities increase, but the variability within each shelter domain could differ according to the microclimate and surrounding environment (e.g., next to a busy road). These nuances will not be fully understood until dependable quantitative data—substantiated by qualitative data—are available across the climate-housing nexus.
Conclusions and Future Research Initiatives
This article advances critical dialogue around the state of concurrent high heat and air pollution exposure research, focusing on people experiencing homelessness while including lessons applicable to vulnerable populations at large. We highlight that concurrent high heat and air pollution exposure research is significantly underdeveloped considering the pressing human health implications. Further, we assert that people without quality shelter are most at risk, as the severity of physiological response is thought to be a product of intensity and exposure time. Lastly, we highlight the need for transdisciplinary teams of climate scientists and policymakers to work with mental and physical health care professionals, such as social workers, to gather data in a socially just way and use those data to guide tailored prevention and intervention strategies. Future work should progress in five vital aspects:
Increase the spatial and temporal resolution of day-to-day heat stress metrics and air pollution data utilizing hyperlocal, real-time technologies and/or leveraging innovative remote sensing technologies combined with in situ validation. Discern what these numbers mean regarding access to resources and overall health burdens for people experiencing homelessness via unintrusive/nonidentifiable means.
Work to understand the mental health and well-being implications of long-term heat and pollution exposures, particularly among populations experiencing homelessness with intersectional identity characteristics (e.g., race/ethnicity, gender identity, sexual orientation, ability, age, income, and citizenship status).
Review and improve hospital intake methods to ensure housing status is accurately, but privately, reflected.
Construct a standardized and improved method for counting heat and pollution-related deaths within the health care system to reflect the true toll more accurately.
Leverage community partnerships to investigate the role of existing housing policies and programs (such as Housing First96 and community shelters) in mitigating or exacerbating the impact of extreme heat and air pollution on health outcomes.
Only after the scientific community responds to the focal points above can risk mitigation tactics essential for safe, livable conditions via local adaptation efforts be optimized. How can one reduce heat and air pollution exposures if our understanding of that risk to the most vulnerable populations remains incomplete? People experiencing homelessness and lacking shelter deserve to be at the forefront of climate-health research in all facets: focus, planning, and implementation. Despite the current research challenges, the methodological ingenuity and progressive team structures that we outlined throughout this article provide hope for the future.
Acknowledgments
The authors are thankful to all participants in the Fall 2022 session of “SOS 591: Climate Change and Health” who aided in the formation of our perspectives outlined throughout this commentary.
References
- 1.Ebi KL, Capon A, Berry P, Broderick C, de Dear R, Havenith G, et al. 2021. Hot weather and heat extremes: health risks. Lancet 398(10301):698–708, PMID: , 10.1016/S0140-6736(21)01208-3. [DOI] [PubMed] [Google Scholar]
- 2.Li X, Jin L, Kan H. 2019. Air pollution: a global problem needs local fixes. Nature 570(7762):437–439, PMID: , 10.1038/d41586-019-01960-7. [DOI] [PubMed] [Google Scholar]
- 3.Analitis A, Michelozzi P, D’Ippoliti D, De’Donato F, Menne B, Matthies F, et al. 2014. Effects of heat waves on mortality: effect modification and confounding by air pollutants. Epidemiology 25(1):15–22, PMID: , 10.1097/EDE.0b013e31828ac01b. [DOI] [PubMed] [Google Scholar]
- 4.Khomsi K, Chelhaoui Y, Alilou S, Souri R, Najmi H, Souhaili Z. 2022. Concurrent heat waves and extreme ozone (O3) episodes: combined atmospheric patterns and impact on human health. Int J Environ Res Public Health 19(5):2770, PMID: , 10.3390/ijerph19052770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ren C, Williams GM, Mengersen K, Morawska L, Tong S. 2008. Does temperature modify short-term effects of ozone on total mortality in 60 large Eastern US communities?—an assessment using the NMMAPS data. Environ Int 34(4):451–458, PMID: , 10.1016/j.envint.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Ramin B, Svoboda T. 2009. Health of the homeless and climate change. J Urban Health 86(4):654–664, PMID: , 10.1007/s11524-009-9354-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crank PJ, Hondula DM, Sailor DJ. 2023. Mental health and air temperature: attributable risk analysis for schizophrenia hospital admissions in arid urban climates. Sci Total Environ 862:160599, PMID: , 10.1016/j.scitotenv.2022.160599. [DOI] [PubMed] [Google Scholar]
- 8.Martin-Latry K, Goumy M-P, Latry P, Gabinski C, Bégaud B, Faure I, et al. 2007. Psychotropic drugs use and risk of heat-related hospitalisation. Eur Psychiatry 22(6):335–338, PMID: , 10.1016/j.eurpsy.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Schwarz L, Hansen K, Alari A, Ilango SD, Bernal N, Basu R, et al. 2021. Spatial variation in the joint effect of extreme heat events and ozone on respiratory hospitalizations in California. Proc Natl Acad Sci USA 118(22):e2023078118, PMID: , 10.1073/pnas.2023078118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Subedi K, Ghimire S. 2022. Comorbidity profiles of patients experiencing homelessness: a latent class analysis. PLoS One 17(5):e0268841, PMID: , 10.1371/journal.pone.0268841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wadhera RK, Choi E, Shen C, Yeh RW, Joynt Maddox KE. 2019. Trends, causes, and outcomes of hospitalizations for homeless individuals. Med Care 57(1):21–27, PMID: , 10.1097/MLR.0000000000001015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaw M. 2004. Housing and public health. Annu Rev Public Health 25(1):397–418, PMID: , 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- 13.Swope CB, Hernández D. 2019. Housing as a determinant of health equity: a conceptual model. Soc Sci Med 243:112571, PMID: , 10.1016/j.socscimed.2019.112571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broadbent AM, Krayenhoff ES, Georgescu M. 2020. The motley drivers of heat and cold exposure in 21st century US cities. Proc Natl Acad Sci USA 117(35):21108–21117, PMID: , 10.1073/pnas.2005492117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCarthy MP, Best MJ, Betts RA. 2010. Climate change in cities due to global warming and urban effects. Geophys Res Lett 37(9):L09705, 10.1029/2010GL042845. [DOI] [Google Scholar]
- 16.Oke TR. 1973. City size and the urban heat island. Atmospher Environ (1967) 7(8):769–779, 10.1016/0004-6981(73)90140-6. [DOI] [Google Scholar]
- 17.Fiore AM, Naik V, Leibensperger EM. 2015. Air quality and climate connections. J Air Waste Manag Assoc 65(6):645–685, PMID: , 10.1080/10962247.2015.1040526. [DOI] [PubMed] [Google Scholar]
- 18.Lin M, Horowitz LW, Xie Y, Paulot F, Malyshev S, Shevliakova E, et al. 2020. Vegetation feedbacks during drought exacerbate ozone air pollution extremes in Europe. Nat Clim Chang 10(5):444–451, 10.1038/s41558-020-0743-y. [DOI] [Google Scholar]
- 19.Vautard R, Beekmann M, Desplat J, Hodzic A, Morel S. 2007. Air quality in Europe during the summer of 2003 as a prototype of air quality in a warmer climate. Comptes Rendus - Geosci 339(11–12):747–763, 10.1016/j.crte.2007.08.003. [DOI] [Google Scholar]
- 20.Bezgrebelna M, McKenzie K, Wells S, Ravindran A, Kral M, Christensen J, et al. 2021. Climate change, weather, housing precarity, and homelessness: a systematic review of reviews. Int J Environ Res Public Health 18(11):5812, PMID: , 10.3390/ijerph18115812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cusack L, van Loon A, Kralik D, Arbon P, Gilbert S. 2013. Extreme weather-related health needs of people who are homeless. Aust J Prim Health 19(3):250–255, PMID: , 10.1071/PY12048. [DOI] [PubMed] [Google Scholar]
- 22.Kuras ER, Richardson MB, Calkins MM, Ebi KL, Hess JJ, Kintziger KW, et al. 2017. Opportunities and challenges for personal heat exposure research. Environ Health Perspect 125(8):085001, PMID: , 10.1289/EHP556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steinle S, Reis S, Sabel CE. 2013. Quantifying human exposure to air pollution—moving from static monitoring to spatio-temporally resolved personal exposure assessment. Sci Total Environ 443:184–193, PMID: , 10.1016/j.scitotenv.2012.10.098. [DOI] [PubMed] [Google Scholar]
- 24.Chatzidiakou L, Krause A, Popoola OAM, Di Antonio A, Kellaway M, Han Y, et al. 2019. Characterising low-cost sensors in highly portable platforms to quantify personal exposure in diverse environments. Atmos Meas Tech 12(8):4643–4657, PMID: , 10.5194/amt-12-4643-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pantelic J, Nazarian N, Miller C, Meggers F, Lee JKW, Licina D. 2022. Transformational IoT sensing for air pollution and thermal exposures. Front Built Environ 8:971523, 10.3389/fbuil.2022.971523. [DOI] [Google Scholar]
- 26.Snyder EG, Watkins TH, Solomon PA, Thoma ED, Williams RW, Hagler GSW, et al. 2013. The changing paradigm of air pollution monitoring. Environ Sci Technol 47(20):11369–11377, PMID: , 10.1021/es4022602. [DOI] [PubMed] [Google Scholar]
- 27.Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. 2020. Environmental and health impacts of air pollution: a review. Front Public Health 8:14, PMID: , 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone B. 2005. Urban heat and air pollution: an emerging role for planners in the climate change debate. J Am Planning Assoc 71(1):13–25, 10.1080/01944360508976402. [DOI] [Google Scholar]
- 29.de Sousa T, Andrichik A, Cuellar M, Marson J, Prestera E, Rush K. 2022. The 2022 Annual Homelessness Assessment Report (AHAR) to Congress (Part 1: Point-In-Time Estimates of Homelessness). Washington, DC: U.S. Department of Housing and Urban Development. https://www.huduser.gov/portal/sites/default/files/pdf/2022-ahar-part-1.pdf [accessed 14 August 2023]. [Google Scholar]
- 30.U.S. Department of Housing and Urban Development. 2022. HUD Releases 2022 Annual Homeless Assessment Report. Washington, DC: U.S. Department of Housing and Urban Development. https://www.hud.gov/press/press_releases_media_advisories/HUD_No_22_253 [accessed 14 August 2023]. [Google Scholar]
- 31.Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB. 2013. Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa county, Arizona. Environ Health Perspect 121(2):197–204, PMID: , 10.1289/ehp.1104625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gronlund CJ. 2014. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep 1(3):165–173, PMID: , 10.1007/s40471-014-0014-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hondula DM, Kuras ER, Betzel S, Drake L, Eneboe J, Kaml M, et al. 2021. Novel metrics for relating personal heat exposure to social risk factors and outdoor ambient temperature. Environ Int 146:106271, PMID: , 10.1016/j.envint.2020.106271. [DOI] [PubMed] [Google Scholar]
- 34.Kenney WL, Craighead DH, Alexander LM. 2014. Heat waves, aging, and human cardiovascular health. Med Sci Sports Exerc 46(10):1891–1899, PMID: , 10.1249/MSS.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. 2012. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc Natl Acad Sci USA 109(17):6608–6613, PMID: , 10.1073/pnas.1113070109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ostro B, Rauch S, Green R, Malig B, Basu R. 2010. The effects of temperature and use of air conditioning on hospitalizations. Am J Epidemiol 172(9):1053–1061, PMID: , 10.1093/aje/kwq231. [DOI] [PubMed] [Google Scholar]
- 37.Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, et al. 2009. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 179(5):383–389, PMID: , 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- 38.Lin S, Luo M, Walker RJ, Liu X, Hwang S-A, Chinery R. 2009. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 20(5):738–746, PMID: , 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- 39.Putnam H, Hondula DM, Urban A, Berisha V, Iniguez P, Roach M. 2018. It’s not the heat, it’s the vulnerability: attribution of the 2016 spike in heat-associated deaths in Maricopa county, Arizona. Environ Res Lett 13(9):094022, 10.1088/1748-9326/aadb44. [DOI] [Google Scholar]
- 40.The 114th Arizona Town Hall. 2022. Mental Health, Substance Use, and Homelessness. Phoenix, Arizona: Morrison Institute for Public Policy. https://morrisoninstitute.asu.edu/sites/default/files/114_mental_health_substance_use_and_homelessness_background_report_web.pdf [accessed 13 April 2023]. [Google Scholar]
- 41.Howe PD, Marlon JR, Wang X, Leiserowitz A. 2019. Public perceptions of the health risks of extreme heat across US states, counties, and neighborhoods. Proc Natl Acad Sci USA 116(14):6743–6748, PMID: , 10.1073/pnas.1813145116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grundstein A, Williams C, Phan M, Cooper E. 2015. Regional heat safety thresholds for athletics in the contiguous United States. Applied Geography 56:55–60, 10.1016/j.apgeog.2014.10.014. [DOI] [Google Scholar]
- 43.Guardaro M, Hondula DM, Ortiz J, Redman CL. 2022. Adaptive capacity to extreme urban heat: the dynamics of differing narratives. Climate Risk Management 35:100415, 10.1016/j.crm.2022.100415. [DOI] [Google Scholar]
- 44.Périard JD, Racinais S, Sawka MN. 2015. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports 25(Suppl 1):20–38, PMID: , 10.1111/sms.12408. [DOI] [PubMed] [Google Scholar]
- 45.Barros VR, Field CB, Dokken DJ, Mastrandrea MD, Mach KJ. 2014. AR5 Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part B: Regional Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Mastrandrea PR, White LL, eds. Cambridge, UK: Cambridge University Press. [Google Scholar]
- 46.Fletcher BA, Lin S, Fitzgerald EF, Hwang S-A. 2012. Association of summer temperatures with hospital admissions for renal diseases in New York state: a case-crossover study. Am J Epidemiol 175(9):907–916, PMID: , 10.1093/aje/kwr417. [DOI] [PubMed] [Google Scholar]
- 47.Hajat S, Sarran CE, Bezgrebelna M, Kidd SA. 2023. Ambient temperature and emergency hospital admissions in people experiencing homelessness: London, United Kingdom, 2011–2019. Am J Public Health 113(9):981–984, PMID: , 10.2105/AJPH.2023.307351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hajat S, Kosatky T. 2010. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health 64(9):753–760, PMID: , 10.1136/jech.2009.087999. [DOI] [PubMed] [Google Scholar]
- 49.Guzman-Echavarria G, Middel A, Vanos J. 2022. Beyond heat exposure—new methods to quantify and link personal heat exposure, stress, and strain in diverse populations and climates: the journal Temperature toolbox. Temperature 10(3):358–378, 10.1080/23328940.2022.2149024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rita N, Garboden PME, Darrah-Okike J. 2022. You have to prove that you’re homeless”: vulnerability and gatekeeping in public housing prioritization policies. City Community 22(2):83–104, 10.1177/15356841221129791. [DOI] [Google Scholar]
- 51.Lave LB, Seskin EP. 1970. Air pollution and human health. Science 169(3947):723–733, PMID: , 10.1126/science.169.3947.723. [DOI] [PubMed] [Google Scholar]
- 52.Ayres SM, Buehler ME. 1970. The effects of urban air pollution on health. Clin Pharmacol Ther 11(3):337–371, PMID: , 10.1002/cpt1970113337. [DOI] [PubMed] [Google Scholar]
- 53.Schwarze PE, Øvrevik J, Låg M, Refsnes M, Nafstad P, Hetland RB, et al. 2006. Particulate matter properties and health effects: consistency of epidemiological and toxicological studies. Hum Exp Toxicol 25(10):559–579, PMID: , 10.1177/096032706072520. [DOI] [PubMed] [Google Scholar]
- 54.Nuvolone D, Petri D, Voller F. 2018. The effects of ozone on human health. Environ Sci Pollut Res Int 25(9):8074–8088, PMID: , 10.1007/s11356-017-9239-3. [DOI] [PubMed] [Google Scholar]
- 55.Cakmak S, Dales RE, Coates F. 2012. Does air pollution increase the effect of aeroallergens on hospitalization for asthma? J Allergy Clin Immunol 129(1):228–231, PMID: , 10.1016/j.jaci.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 56.Zanobetti A, Schwartz J. 2011. Ozone and survival in four cohorts with potentially predisposing diseases. Am J Respir Crit Care Med 184(7):836–841, PMID: , 10.1164/rccm.201102-0227OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bell ML, Zanobetti A, Dominici F. 2014. Who is more affected by ozone pollution? A systematic review and meta-analysis. Am J Epidemiol 180(1):15–28, PMID: , 10.1093/aje/kwu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vallero DA. 2014. The science of air pollution. In: Fundamentals of Air Pollution. 5th ed. Cambridge, MA: Academic Press, 43–82. [Google Scholar]
- 59.Atkinson RW, Butland BK, Dimitroulopoulou C, Heal MR, Stedman JR, Carslaw N, et al. 2016. Long-term exposure to ambient ozone and mortality: a quantitative systematic review and meta-analysis of evidence from cohort studies. BMJ Open 6(2):e009493, PMID: , 10.1136/bmjopen-2015-009493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O’Lenick CR, Wilhelmi OV, Michael R, Hayden MH, Baniassadi A, Wiedinmyer C, et al. 2019. Urban heat and air pollution: a framework for integrating population vulnerability and indoor exposure in health risk analyses. Sci Total Environ 660:715–723, PMID: , 10.1016/j.scitotenv.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 61.Vanos JK, Cakmak S, Kalkstein LS, Yagouti A. 2015. Association of weather and air pollution interactions on daily mortality in 12 Canadian cities. Air Qual Atmos Health 8(3):307–320, PMID: , 10.1007/s11869-014-0266-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kahle JJ, Neas LM, Devlin RB, Case MW, Schmitt MT, Madden MC, et al. 2015. Interaction effects of temperature and ozone on lung function and markers of systemic inflammation, coagulation, and fibrinolysis: a crossover study of healthy young volunteers. Environ Health Perspect 123(4):310–316, PMID: , 10.1289/ehp.1307986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Borrego C, Martins H, Tchepel O, Salmim L, Monteiro A, Miranda AI. 2006. How urban structure can affect city sustainability from an air quality perspective. Environ Model Softw 21(4):461–467, 10.1016/j.envsoft.2004.07.009. [DOI] [Google Scholar]
- 64.Zhang Y, Gu Z. 2013. Air quality by urban design. Nature Geosci 6(7):506, 10.1038/ngeo1869. [DOI] [Google Scholar]
- 65.Debbage N, Shepherd JM. 2015. The urban heat island effect and city contiguity. Comput Environ Urban Syst 54:181–194, 10.1016/j.compenvurbsys.2015.08.002. [DOI] [Google Scholar]
- 66.Harlan SL, Ruddell DM. 2011. Climate change and health in cities: impacts of heat and air pollution and potential co-benefits from mitigation and adaptation. Curr Opin Environ Sustain 3(3):126–134, 10.1016/j.cosust.2011.01.001. [DOI] [Google Scholar]
- 67.Pascal M, Wagner V, Alari A, Corso M, Le Tertre A. 2021. Extreme heat and acute air pollution episodes: a need for joint public health warnings? Atmos Environ 249:118249, 10.1016/j.atmosenv.2021.118249. [DOI] [Google Scholar]
- 68.Filleul L, Cassadou S, Médina S, Fabres P, Lefranc A, Eilstein D, et al. 2006. The relation between temperature, ozone, and mortality in nine French cities during the heat wave of 2003. Environ Health Perspect 114(9):1344–1347, PMID: , 10.1289/ehp.8328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shen J, Ma Y, Zhang Y, Zhang C, Wang W, Qin P, et al. 2023. Temperature modifies the effects of air pollutants on respiratory diseases. Environ Sci Pollut Res 30(22):61778–61788, 10.1007/s11356-023-26322-9. [DOI] [PubMed] [Google Scholar]
- 70.Singh N, Singh S, Mall RK. 2020. Urban ecology and human health: Implications of urban heat island, air pollution and climate change nexus. In: Urban Ecology. Verma P, Singh P, Singh R, Raghubanshi AS, eds. Amsterdam, Netherlands: Elsevier, 317–334, 10.1016/B978-0-12-820730-7.00017-3. [DOI] [Google Scholar]
- 71.Jhun I, Fann N, Zanobetti A, Hubbell B. 2014. Effect modification of ozone-related mortality risks by temperature in 97 US cities. Environ Int 73:128–134, PMID: , 10.1016/j.envint.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 72.Grineski S, Bolin B, Boone C. 2007. Criteria air pollution and marginalized populations: environmental inequity in metropolitan Phoenix, Arizona. Soc Sci Q 88(2):535–554, 10.1111/j.1540-6237.2007.00470.x. [DOI] [Google Scholar]
- 73.Lane HM, Morello-Frosch R, Marshall JD, Apte JS. 2022. Historical redlining is associated with present-day air pollution disparities in U.S. Cities. Environ Sci Technol Lett 9(4):345–350, PMID: , 10.1021/acs.estlett.1c01012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Saverino KC, Routman E, Lookingbill TR, Eanes AM, Hoffman JS, Bao R. 2021. Thermal inequity in Richmond, VA: the effect of an unjust evolution of the urban landscape on urban heat islands. Sustainability 13(3):1511, 10.3390/su13031511. [DOI] [Google Scholar]
- 75.Mitchell MS, León CLK, Byrne TH, Lin W-C, Bharel M. 2017. Cost of health care utilization among homeless frequent emergency department users. Psychol Serv 14(2):193–202, PMID: , 10.1037/ser0000113. [DOI] [PubMed] [Google Scholar]
- 76.Schwarz L, Castillo EM, Chan TC, Brennan JJ, Sbiroli ES, Carrasco-Escobar G, et al. 2022. Heat waves and emergency department visits among the homeless, San Diego, 2012–2019. Am J Public Health 112(1):98–106, PMID: , 10.2105/AJPH.2021.306557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Weinberger KR, Harris D, Spangler KR, Zanobetti A, Wellenius GA. 2020. Estimating the number of excess deaths attributable to heat in 297 United States counties. Environ Epidemiol 4(3):e096, PMID: , 10.1097/EE9.0000000000000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Verghese S, Nema AK. 2022. Optimal design of air quality monitoring networks: a systematic review. Stoch Environ Res Risk Assess 36(10):2963–2978, 10.1007/s00477-022-02187-1. [DOI] [Google Scholar]
- 79.Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS, et al. 2011. Particulate matter–induced health effects: who is susceptible? Environ Health Perspect 119(4):446–454, PMID: , 10.1289/ehp.1002255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Reilly J, Ho I, Williamson A. 2022. A systematic review of the effect of stigma on the health of people experiencing homelessness. Health Soc Care Community 30(6):2128–2141, PMID: , 10.1111/hsc.13884. [DOI] [PubMed] [Google Scholar]
- 81.Cloke P, Cooke P, Cursons J, Milbourne P, Widdowfield R. 2000. Ethics, reflexivity and research: encounters with homeless people. Ethics Place Environ 3(2):133–154, 10.1080/713665889. [DOI] [Google Scholar]
- 82.Amster R. 2008. Lost in Space: The Criminalization, Globalization, and Urban Ecology of Homelessness. El Paso, Texas: LFB Scholarly Publishing. [Google Scholar]
- 83.Batko S, Culhane D. 2023. Homelessness in the United States. In: The Routledge Handbook of Homelessness. Oxfordshire, UK: Routledge, 413–422. [Google Scholar]
- 84.Treglia D, Culhane D. 2023. Defining and counting homelessness. In: The Routledge Handbook of Homelessness. Bretherton J, Pleace N, eds. 1st ed. Oxfordshire, UK: Routledge, 35–47. [Google Scholar]
- 85.Gabbe CJ, Mallen E, Varni A. 2022. Housing and urban heat: assessing risk disparities. Housing Policy Debate 33(5):1078–1099, 10.1080/10511482.2022.2093938. [DOI] [Google Scholar]
- 86.Harlan SL, Chakalian P, Declet-Barreto J, Hondula DM, Jenerette GD. 2019. Pathways to climate justice in a desert metropolis. In: People and Climate Change: Vulnerability, Adaptation, and Social Justice. Reyes Mason L, Rigg J, eds. Oxford, UK: Oxford University Press, 23–50. [Google Scholar]
- 87.Hondula DM, Balling RC, Vanos JK, Georgescu M. 2015. Rising temperatures, human health, and the role of adaptation. Curr Clim Change Rep 1(3):144–154, 10.1007/s40641-015-0016-4. [DOI] [Google Scholar]
- 88.Kidd SA, Hajat S, Bezgrebelna M, McKenzie K, Climate-Homelessness Working Group. 2021. The climate change–homelessness nexus. Lancet 397(10286):1693–1694, PMID: , 10.1016/S0140-6736(21)00834-5. [DOI] [PubMed] [Google Scholar]
- 89.Longo J, Kuras E, Smith H, Hondula D, Johnston E. 2017. Technology use, exposure to natural hazards, and being digitally invisible: implications for policy analytics. Policy Internet 9(1):76–108, 10.1002/poi3.144. [DOI] [Google Scholar]
- 90.MacMurdo MG, Mulloy KB, Culver DA, Felix CW, Curtis AJ, Ajayakumar J, et al. 2022. Mapping mobility: utilizing local-knowledge-derived activity space to estimate exposure to ambient air pollution among individuals experiencing unsheltered homelessness. Int J Environ Res Public Health 19(10):5842, 10.3390/ijerph19105842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Parsons K. 2019. Measurement of heat stress. In: Human Heat Stress. Boca Raton, FL: CRC Press, 47–56. [Google Scholar]
- 92.Karner A, Hondula DM, Vanos JK. 2015. Heat exposure during non-motorized travel: implications for transportation policy under climate change. J Transport Health 2(4):451–459, 10.1016/j.jth.2015.10.001. [DOI] [Google Scholar]
- 93.Petitti DB, Hondula DM, Yang S, Harlan SL, Chowell G. 2016. Multiple trigger points for quantifying heat-health impacts: new evidence from a hot climate. Environ Health Perspect 124(2):176–183, PMID: , 10.1289/ehp.1409119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gabbe CJ, Chang JS, Kamson M, Seo E. 2023. Reducing heat risk for people experiencing unsheltered homelessness. Int J Disaster Risk Reduction 96:103904, 10.1016/j.ijdrr.2023.103904. [DOI] [Google Scholar]
- 95.Karanja J, Vieira J, Vanos J. 2023. Sheltered from the heat? How tents and shade covers may unintentionally increase air temperature exposures to unsheltered communities. Public Health Pract (Oxf) 6:100450, PMID: , 10.1016/j.puhip.2023.100450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.National Low Income Housing Coalition. 2023. The Case for Housing First. https://nlihc.org/sites/default/files/Housing-First-Research.pdf [accessed 6 September 2023].


