Abstract
Although not reliant on donor funding for health, the external assistance that Sri Lanka receives contributes to the improvement of the health system and health outcomes. In this study, we evaluated transition experiences of the expanded programme on immunization (EPI) that received Gavi funding to expand the vaccine portfolio and the Anti-Malaria Campaign (AMC) that received funding from the Global Fund for AIDS, Tuberculosis and Malaria to scale-up interventions to target and achieve malaria elimination. We assessed if EPI and AMC programmes were able to sustain coverage of previously donor-funded interventions post-transition and explain the facilitators and barriers that contribute to this. We used a mixed methods approach using quantitative data to assess coverage indicators and the financing mix of the health programmes and qualitative analysis guided by a framework informed by the Walt and Gilson policy triangle that brought together document review and in-depth interviews to identify facilitators and barriers to transition success. The EPI programme showed sustained coverage of Gavi-funded vaccines post-transition and the funding gap was bridged by mobilizing domestic financing facilitated by the Gavi co-financing mechanism, full integration within existing service delivery structures, well-established and favourable pharmaceutical procurement processes for the public sector and stewardship and financial advocacy by technically competent managers. Although the absence of indigenous cases of malaria since 2012 suggests overall programme success, the AMC showed mixed transition success in relation to its different programme components. Donor-supported programme components requiring mobilization of operational expenses, facilitated by early financial planning, were successfully transitioned (e.g. entomological and parasitological surveillance) given COVID-19-related constraints. Other key programme components, such as research, training, education and awareness that are dependent on non-operational expenses are lagging behind. Additionally, concerns of AMC’s future financial sustainability within the current structure remain in the context of low malaria burden.
Keywords: Donor transitions, external assistance, development assistance for health, malaria, immunization
Key messages.
General contributors of strong health system performance such as financial risk protection, close-to-client services and a well-established primary healthcare network were also facilitators of donor transitions.
Central control over equitable allocation of resources and structures in place to achieve national health goals were some governance-related factors identified for transition success in the Sri Lankan context. Health programmes with a historically strong domestic financing base, integration of service delivery of donor funded interventions within existing structures and formal phased transition mechanisms were other facilitators of transition.
The Sri Lankan experience also highlights the importance of factoring in future macroeconomic projections and policies that can impact fiscal space for health and political commitment that reflect public prioritization of diseases, during decision-making on health programmes’ structure and organization during donor transitions.
Introduction
The adoption of the Millennium Development Goals and the establishment of new global funding mechanisms for health in the early 2000s saw large increases in external development assistance for health up until 2009, which have not continued since (Dieleman et al., 2016; 2017; Bendavid et al., 2017). Contributory factors include shifting priorities of donor countries towards areas such as climate change, refugee crisis, and COVID-19 (Dieleman et al., 2016; Moon and Omole, 2017), fiscal constraints precipitated by the global financial crisis (Leach-Kemon et al., 2012) and slowness of the global financing architecture to engage emerging donors (Rannan-Eliya, 2022). In this context, most global health funders aim to transition countries from their support, which is fundamental to long term sustainability. Sustaining coverage of previously donor-funded interventions following transition is one important component of determining transition success that has received relatively less attention than financial sustainability. This is more complex than a financial transition alone and involves local/national ownership and restructuring of programmes for efficiency gains. In this study, we evaluate in-depth two health programmes in Sri Lanka that received external assistance for health from two funding organizations established in the early 2000s—Gavi and the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM). The analysis will aim to understand factors that have influenced sustained coverage of donor supported interventions post-transition.
Sri Lanka, although having limited donor reliance for health, with total financing from foreign sources on average around 2% of current expenditure on health (CEH) in the past three decades (Amarasinghe et al., 2021; Institute for Health Policy, 2021), provides an opportunity to study donor transitions for health from a unique perspective due to several distinctive health system features and interplay with large macroeconomic shifts during the period of donor assistance and post-transition. With 22.2 million people (Department of Census and Statistics, 2020), Sri Lanka is currently a lower-middle income country (LMIC), having moved to upper-middle income country status briefly in 2018 to reverse back to LMIC status in 2019 (World Bank, 2023). Over the past three decades, Sri Lanka has had limited fiscal space for health owing to chronic low and declining levels of general revenue tax collection (>15% of gross domestic product (GDP) in 2003 to <10% of GDP in 2020), high public debt (>100% of GDP in 2003 with a gradual decline to less than 70% of GDP in 2014 and rising again to >100% of GDP in 2021) and debt servicing commitments (Economic Research Department‚ Central Bank of Sri Lanka, 2021; International Monetary Fund, 2022). This has been associated with low public CEH at less than 2% of GDP, and substantial reliance on private financing of healthcare services (half of CEH) (Amarasinghe et al., 2021). Notwithstanding the limited spending on health, Sri Lanka’s health system is known to be high achieving in terms of health outcomes (Rannan-Eliya and Sikurajapathy, 2009). However, Sri Lanka has for a while now been facing substantial challenges due to an ageing population and an increasing non-communicable disease (NCD) burden (Rannan-Eliya et al., 2022; 2023). Limited fiscal space constrains expenditure increases necessary to respond to the demographic and epidemiological transition while continuing to maintain health services for Maternal and Child Health and communicable diseases (Smith, 2018; Asian Development Bank, 2019).
Previous research on donor transitions in Sri Lanka identified limited fiscal space for health, loss of technical assistance, inadequate national planning and health system challenges related to inefficiencies and increasing disease burden due to NCDs as challenges (Perera et al., 2019; Bharali et al., 2020). The prospect of achieving greater self-reliance was identified as an opportunity, with transition planning and sustainable funding choices identified as priorities in the transition context (Bharali et al., 2020). However, these general factors pertaining to health transitions can vary, particularly for specific health programmes for which targeted external support is provided. In this study, we evaluate transitions in-depth by focusing on two health programmes—the Expanded Programme on Immunization (EPI) and the Anti-Malaria Campaign (AMC)—that have received targeted grants and have transitioned away from external assistance within the past decade.
The EPI, established in 1978 and coordinated by the Epidemiology Unit of the Ministry of Health (MoH), is a well-established MoH programme achieving and sustaining some of the highest rates of vaccine coverage globally (UNICEF, 2018). Targeted funding by Gavi was used to expand the vaccine portfolio (introducing new antigens hepatitis B in 2003 and Haemophilus influenzae type B in 2008). In this study, we focus on the Gavi funding period 2003–2015. During this period, Gavi funding on average accounted for 47% of total financing for vaccines and supplies of the EPI and 0.34% of government expenditure on health (GEH) (Institute for Health Policy, 2021). A gradual decrease in the birth cohort from the time Gavi funding was initiated has eased the burden on the EPI over time. The reduction was 10% from 2003 (370 643) to end of the Gavi funding period in 2015 (333 097) and 12% (326 461) by 2017, two years after Gavi graduation (Department of Census and Statistics, 2022). Timelines relevant to Gavi funding for the EPI are illustrated in Figure 1.
Figure 1.
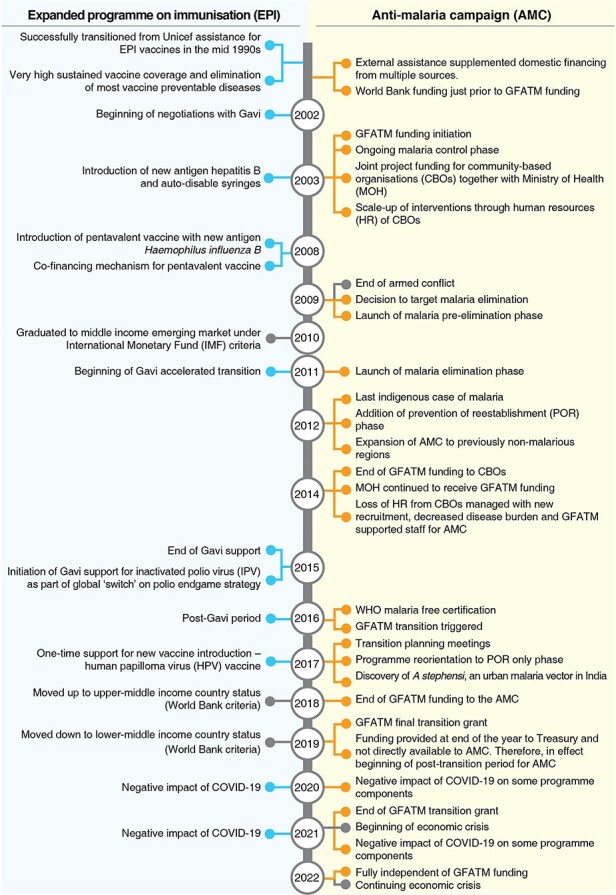
Timeline of events impacting donor funding and transition
The AMC, a deeply rooted, long-established semi-vertical programme of the MoH (first AMC established in 1911), successfully eliminated malaria, with Sri Lanka achieving malaria-free certification from the World Health Organization (WHO) in 2016 (Ministry of Health, 2016). External assistance to the AMC from GFATM played a crucial role in scaling up a wide range of anti-malaria interventions to achieve the goal of malaria elimination. During this period, the AMC underwent major programmatic changes associated with malaria elimination as well as the GFATM funding transition (Anti Malaria Campaign—MoH, 2018). GFATM funding on average accounted for 59% of total financing of the AMC and less than 0.4% of GEH until the GFATM funding transition (Institute for Health Policy, 2021). Timelines relevant to GFATM funding for the AMC are illustrated in Figure 1.
Theoretical framework
We used an adaptation of Walt and Gilson’s (1994) health policy analysis (HPA) framework to guide data collection and analysis. Sustaining effective coverage post-transition at levels seen during the funding period defines a successful transition from external assistance. This framework recognizes that understanding the level of success achieved or the potential level of success that can be achieved by a health programme following transition from external assistance can be evaluated by analysing four elements—content, context, process and actors. Content describes the health programme before and after transition in terms of the major health system inputs such as financing, service delivery, governance and leadership and other inputs such as human resources, procurement and health information systems. A systematic analysis of content can identify what and to which level health system inputs changed after transition. The framework then allows us to explain how these changes occurred considering the elements context, process and actors. Context allows the assessment of how political, social, economic and historical factors influenced transition. Process describes the expectation of transition in comparison to what happened including transition preparedness, planning and how transition fits into the broader health system objectives. The examination of actors recognizes the role of multiple stakeholders in health programme planning and decision-making and the contribution of influential stakeholders to the resulting health programme structure following transition. Applying this framework can help identify facilitators and barriers to sustaining coverage of key interventions following donor transitions. The different elements in the framework capture the complexity of transitions by allowing for multidimensionality and interplay between various elements. A detailed description of the theoretical framework is described elsewhere (Shroff et al., 2024).
Methods
Study design
We used a mixed methods approach. In the quantitative component, we assessed whether coverage of donor-funded interventions was sustained post-transition by using a time series of selected coverage indicators from administrative data sources for the EPI and AMC. At minimum, sustaining coverage of interventions post-transition at pre-transition levels was considered as transition success. In addition, a financial analysis using the Institute for Health Policy (IHP) Sri Lanka’s health account (SLHA) database evaluated domestic and donor contributions for the two health programmes over the donor funding period and post-transition period (Institute for Health Policy, 2021). In the qualitative component, to identify enablers and barriers of transition success, semi-structured interviews were conducted with a range of stakeholders from within and outside the AMC and EPI programmes and documentary review of both published and unpublished literature was carried out.
Selection of the AMC and EPI for in-depth analysis was based on meeting two inclusion criteria: (1) health programmes that transitioned away from external assistance in the past decade (beginning of the post-transition period for the EPI and AMC was 2016 and 2019, respectively); and (2) had a minimum three-year post-transition period at the time of study initiation.
Data collection
Coverage indicators
In selecting coverage indicators, we considered interventions that had major contributions from donors and those that reflect a direct impact of overall programme success. Expansion of the vaccine portfolio in the EPI through introduction of new antigens, hepatitis B from 2003 (hepatitis B monovalent from 2003–2007 and continued since 2008 in the pentavalent vaccine) and Haemophilus influenzae type B from 2008 (through introduction of pentavalent vaccine) were the main outcomes of Gavi funding from 2003–2015. Therefore, for the EPI, the third dose of hepatitis B vaccine coverage and pentavalent vaccine (using DTP3 coverage) and incidence of diphtheria, pertussis and neonatal tetanus were selected as the indicators of coverage and effective coverage.
The AMC received GFATM funding for a wide range of interventions. Considering the feasibility of collecting a time series of data, we selected two key interventions for the AMC—number of blood films screened from risk populations (parasitological surveillance) and total number of entomological surveillance days each year as coverage indicators along with the number of imported, introduced and indigenous malaria cases. The latter provides information on the overall effectiveness of the AMC. Data were collected from administrative records of the EPI and AMC, and any data gaps were addressed by direct queries to the two health programmes.
Financing mix
The domestic and external financing mix of the two health programmes was estimated to understand the changes in the level of financing pre- and post-transition. Financing mix was estimated using IHP databases that compile SLHA (Institute for Health Policy, 2021). IHP’s SLHA estimates fully comply with the System of Health Accounts which is the global standard for reporting health expenditures published by the Organization for Economic Cooperation and Development and WHO (OECD/Eurostat/WHO, 2017). In addition to the information from SLHA, detailed expenditure for Gavi-supported EPI vaccines was supplemented by data and information gathered from Gavi annual progress reports and other country specific Gavi reports (Gavi, The Vaccine Alliance, 2022b).
Documentary review
A documentary review of published and unpublished literature was carried out. The literature was identified using major academic search engines, publications of the EPI, AMC and MoH, thesis collections of the Post-Graduate Institute of Medicine which trains all specialist doctors in Sri Lanka, libraries of other local bodies and included documents forwarded by key informants upon our request. We used the documentary review to gather information by elements in the HPA framework. The review also helped identify gaps in information to be collected through key informant interviews.
In-depth interviews with key informants
Using purposive sampling, semi-structured interviews were conducted with 25 participants during the data collection period from November 2021 to December 2022. The number of key informants interviewed by health programme, national or sub-national level or other category (e.g. donors and technical advisory committees) is detailed in Table 1. We first approached key informants knowledgeable and/or experienced with delivery of relevant services under the AMC and EPI both past and present. Subsequent key informants were selected using snowball sampling (Creswell and Clark, 2017). We conducted in-depth interviews with key informants using a semi-structured interview guide developed to reflect the various elements in the HPA framework. We also used these interviews to corroborate/clarify information gathered through the documentary analysis. Interviews lasted between 45 and 60 minutes and were conducted in the respondent’s preferred language (Sinhala, Tamil or English). Interviews were recorded with consent and all interviews were transcribed for analysis. Interviews conducted in Sinhala or Tamil were transcribed and translated to English. Data saturation was used to determine the end point of the key informant interviews.
Table 1.
Key informant interviews by category and health programme
| Key informant category | Expanded Programme on Immunization (EPI) | Anti-Malaria Campaign (AMC) | Common to both programmes | Total |
|---|---|---|---|---|
| Top level managers of the Central MoH | 3 | 2 | 2 | 7 |
| Other Central MoH unit staff | 2 | 3 | 2 | 7 |
| Provincial level administrators | 1 | 1 | ||
| Regional level administrators | 1 | 1 | ||
| Regional level staff | 1 | 2 | 3 | |
| Technical advisory committees | 3 | 3 | ||
| Donors | 1 | 2 | 3 | |
| Total | 6 | 11 | 8 | 25 |
Data analysis
We followed a deductive content analysis approach to analyse the qualitative data from the documentary review and in-depth interviews (Patton, 2002). For the element content in the HPA framework the main health system components (service delivery, financing, human resources, procurement and information systems) that changed (or not) from pre- to post-transition were identified for each health programme (World Health Organization, 2007). Critical evaluation of a range of contextual factors, transition process and key actors together with coverage indicators, funding mix of health programmes and changes in other major health system components pre- and post-transition, were used to identify enabling and/or impeding factors of transition success.
Ethics approval was obtained from author’s institution ethical review board and administrative approval was obtained from the MoH on 26 October 2021.
Results
First, we present coverage indicators for each health programme to assess if coverage of key selected interventions was sustained post-transition. This is followed by a cross-programme analysis of facilitators and barriers to transition that was guided by the HPA framework and supplemented with information from the financial analysis. Programme-specific differences are discussed where relevant.
Coverage indicators
EPI
The third dose of the new antigen hepatitis B (hepB3), introduced with Gavi assistance in 2003 as hepatitis B monovalent and continued since 2008 with the pentavalent vaccine (captured in DTP3 coverage) shows sustained coverage pre- and post-Gavi transition (Table 2). Consistently low levels or absence of diphtheria, pertussis and neonatal tetanus, some of the target diseases of the pentavalent vaccine, suggest effective coverage of the vaccine.
Table 2.
Coverage indicators and domestic and Gavi financing mix for the expanded programme on immunization (EPI)
| Vaccine coverage (%)a | Expenditure for EPI (USD million (% of total))e | Co-financing share for pentavalent vaccine (%)g,h | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Gavi funding timelines | DTP3 | HepB3 | Cases per 100,000 population for incidence of diphtheriab | Cases per 100,000 population for incidence of whooping coughc | Cases per 100,000 population for incidence of tetanusd | Domesticf | Gavi | UN agencies | Total | Gavi | Domestic | |
| 2003 | Gavi funding initiation | Hepatitis B | 98 | 32 | 0 | 0.6 | 0.60 | 1.09 (68.6) | 0.50 (31.4) | 0.00 (0.0) | 1.60 (100.0) | – | – |
| 2004 | 92 | 62 | 0 | 0.2 | 0.60 | 2.27 (77.5) | 0.66 (22.5) | 0.00 (0.0) | 2.93 (100.0) | – | – | ||
| 2005 | 96 | 87 | 0 | 0.4 | 0.60 | 1.25 (59.2) | 0.86 (40.8) | 0.00 (0.0) | 2.11 (100.0) | – | – | ||
| 2006 | 94 | 91 | 0 | 0.2 | 0.01 | 1.39 (64.4) | 0.77 (35.6) | 0.00 (0.0) | 2.16 (100.0) | – | – | ||
| 2007 | 93 | 91 | 0 | 0.1 | 0.00 | 0.69 (58.0) | 0.50 (42.0) | 0.00 (0.0) | 1.20 (100.0) | – | – | ||
| 2008 | Pentavalent vaccine | 91 | 91 | 0 | 0.1 | 0.01 | 2.52 (29.3) | 6.08 (70.7) | 0.00 (0.0) | 8.60 (100.0) | 100 | 0 | |
| 2009 | 88 | 88 | 0 | 0.2 | 0.00 | 1.09 (51.9) | 1.01 (48.1) | 0.00 (0.0) | 2.10 (100.0) | 0 | 0 | ||
| 2010 | 92 | 92 | 0 | 0.1 | 0.00 | 1.38 (21.7) | 4.98 (78.3) | 0.00 (0.0) | 6.36 (100.0) | 87 | 13 | ||
| 2011 | Gavi accelerated transition | 94 | 94 | 0 | 0.3 | 0.00 | 1.59 (25.9) | 4.54 (74.1) | 0.00 (0.0) | 6.13 (100.0) | 79 | 21 | |
| 2012 | 100 | 100 | 0 | 0.3 | 0.00 | 1.27 (31.5) | 2.76 (68.5) | 0.00 (0.0) | 4.03 (100.0) | 71 | 29 | ||
| 2013 | 97 | 97 | 0 | 0.3 | 0.00 | 2.37 (42.5) | 3.21 (57.5) | 0.00 (0.0) | 5.58 (100.0) | 81 | 19 | ||
| 2014 | 99 | 99 | 0 | 0.4 | 0.00 | 4.32 (86.9) | 0.61 (12.3) | 0.04 (0.8) | 4.96 (100.0) | 11 | 89 | ||
| 2015 | 99 | 99 | 0 | 0.5 | 0.00 | 4.09 (75.0) | 1.30 (23.9) | 0.06 (1.1) | 5.44 (100.0) | 4 | 96 | ||
| 2016 | Post-Gavi period commences | 97 | 98 | 0 | 0.3 | 0.00 | 7.72 (99.1) | 0.04 (0.5)i | 0.03 (0.4) | 7.79 (100.0) | – | – | |
| 2017 | 96 | 96 | 0 | 0.1 | 0.00 | 4.80 (72.3) | 1.82 (27.4)i | 0.02 (0.3) | 6.64 (100.0) | – | – | ||
| 2018 | 96 | 96 | 0 | 0.05 | 0.00 | 5.22 (93.7) | 0.33 (5.9)i | 0.02 (0.4) | 5.56 (100.0) | – | – | ||
| 2019 | 98 | 98 | 0 | 0.2 | 0.00 | 5.66 (92.5) | 0.42 (6.8)i | 0.04 (0.7) | 6.11 (100.0) | – | – | ||
| 2020 | 96 | 96 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | – | – | ||
WHO/UNICEF Estimates of National Immunization Coverage (WUENIC) https://www.who.int/publications/m/item/wuenic_input, [accessed 13 February 2023].
Annual Health Bulletin 2019 http://www.health.gov.lk/moh_final/english/others.php?pid=110, [accessed 20 February 2023].
Annual Health Bulletin 2019 http://www.health.gov.lk/moh_final/english/others.php?pid=110, [accessed 20 February 2023].
Annual Health Bulletin 2019 http://www.health.gov.lk/moh_final/english/others.php?pid=110, [accessed 20 February 2023].
Expenditure data from Institute for Health Policy (IHP) Sri Lanka Health Accounts Database. Expenditure for 2019 is provisional.
Domestic financing includes expenditure for vaccines and injection safety supplies in the national immunization schedule, but excludes expenditures for human resources for delivery of immunization services and management of the EPI, cold chain maintenance and other expenditures.
Authors’ calculation using IHP Sri Lanka Health Account Database and Gavi annual progress reported 2008–2014 (https://www.gavi.org/country-documents/sri-lanka).
Sri Lanka initiated pentavalent vaccine administration on 1 January 2008 but suspended on 29 April 2008 following several deaths after administration of the vaccine. Following an investigation, the pentavalent vaccine was reintroduced in February 2010. This explains the absence of co-financing in 2009.
Gavi funding from 2015–2019 for IPV, 2017—HPV initiation grant and new vaccine support.
N/A indicates not available.
AMC
Compared to the average for the period of GFATM transition funding (2016–2018), the annual number of blood films screened from risk populations (nearly 1.1 million) was 6% higher in 2019 but declined in 2020 and 2021 by 27% and 40%, respectively (Table 3). Compared to the average number of annual entomological days (4617) for the same period (2016–2018), entomological days were 5% higher in 2019, 17% lower in 2020 and 1% higher in 2021. Key informants attributed the decrease in parasitological surveillance in 2020 and 2021 to the difficulty in implementing these interventions due to COVID-19 restrictions, and not due to a lack of finances to implement these interventions. For the AMC, it is important to highlight that due to multiple programmatic changes associated with the epidemiological shift in malaria, sustaining coverage post-transition at pre-transition levels should be considered with caution. To illustrate, the expected decrease in the level of interventions due to decreasing disease burden must be balanced with necessary interventions to maintain malaria-free status along with responding to new challenges. Relevant to maintaining this balance, key informants explained that overall coverage levels of the selected interventions reported in this study are not expected to decrease. This was attributed to expansion of preventive activities to previously malaria non-endemic regions in response to a shift in transmission risk associated with the greater incidence of imported malaria cases now occurring in previously non-malarious regions (Anti Malaria Campaign—MoH, 2018). This requires maintaining surveillance activities in both previously malaria-endemic as well as non-endemic regions, where decreases in some areas were offset by increases in others. While the optimum level of anti-malaria interventions may be difficult to determine, the ultimate success of the AMC is dependent upon maintaining malaria-free status and prevention of local malaria transmission. Since 2012, there were no indigenous malaria cases reported in Sri Lanka until the time of writing this study, thus illustrating the overall success of the AMC (Table 3).
Table 3.
Coverage indicators and domestic and GFATM financing mix for the Anti-Malaria Campaign (AMC)
| Malaria casesa | Expenditure for AMC (USD million (% of total))f | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | GFATM funding timelines | Indigenous | Imported | Introduced | Entomological surveillance daysd | Number of blood films screened from risk populationse | Domesticg | World Bank | GFATM | UN agencies | Total |
| 2003 | GFATM funding initiation | 10510h | – | – | N/A | 1 192 259 | 1.73 (40.8) | 0.11 (2.6) | 2.40 (56.6) | 0.00 (0.0) | 4.24 (100.0) |
| 2004 | 3720 h | – | – | N/A | 1 198 181 | 2.62 (60.5) | 0.00 (0.0) | 1.71 (39.5) | 0.00 (0.0) | 4.33 (100.0) | |
| 2005 | 1640 h | – | – | N/A | 973 861 | 1.02 (61.1) | 0.00 (0.0) | 0.65 (38.9) | 0.00 (0.0) | 1.67 (100.0) | |
| 2006 | 591 h | – | – | N/A | 1 076 121 | 2.38 (95.2) | 0.00 (0.0) | 0.12 (4.8) | 0.00 (0.0) | 2.50 (100.0) | |
| 2007 | 199 h | – | – | N/A | 1 044 403 | 1.40 (65.4) | 0.00 (0.0) | 0.74 (34.6) | 0.00 (0.0) | 2.14 (100.0) | |
| 2008 | 646 | 24 | – | N/A | 1 047 104 | 2.74 (41.1) | 0.00 (0.0) | 3.93 (58.9) | 0.00 (0.0) | 6.67 (100.0) | |
| 2009 | 531 | 27 | – | N/A | 909 632 | 1.42 (17.7) | 0.00 (0.0) | 6.59 (82.3) | 0.00 (0.0) | 8.01 (100.0) | |
| 2010 | 684 | 52 | – | 1898 | 1 098 779 | 1.17 (17.4) | 0.00 (0.0) | 5.57 (82.6) | 0.00 (0.0) | 6.74 (100.0) | |
| 2011 | 124 | 51 | – | 7067 | 1 243 040 | 1.23 (21.7) | 0.00 (0.0) | 4.38 (77.2) | 0.06 (1.1) | 5.67 (100.0) | |
| 2012 | 23 | 70 | – | 7052 | 1 186 165 | 0.56 (17.2) | 0.00 (0.0) | 2.62 (80.4) | 0.08 (2.4) | 3.26 (100.0) | |
| 2013 | 0 | 95 | 0 | 8129 | 1 236 579 | 0.60 (13.2) | 0.00 (0.0) | 3.88 (85.5) | 0.06 (1.3) | 4.54 (100.0) | |
| 2014 | 0 | 49 | 0 | N/A | 1 232 314 | 0.74 (23.8) | 0.00 (0.0) | 2.32 (74.6) | 0.05 (1.6) | 3.11 (100.0) | |
| 2015 | 0 | 36 | 0 | 4248 | 1 142 466 | 0.91 (58.0) | 0.00 (0.0) | 0.63 (40.1) | 0.03 (1.9) | 1.57 (100.0) | |
| 2016 | Transition | 0 | 41 | 0 | 4901 | 1 072 396 | 1.09 (55.1) | 0.00 (0.0) | 0.85 (42.9) | 0.04 (2.0) | 1.98 (100.0) |
| 2017 | 0 | 56 | 0 | 4321 | 1 089 290 | 0.89 (36.8) | 0.00 (0.0) | 1.52 (62.8) | 0.01 (0.4) | 2.42 (100.0) | |
| 2018 | 0 | 47 | 1b | 4628 | 1 129 070 | 0.97 (23.9) | 0.00 (0.0) | 3.08 (75.9) | 0.01 (0.2) | 4.06 (100.0) | |
| 2019 | GFATM post-transition commences | 0 | 53 | 0 | 4830 | 1 164 914 | 1.05 (99.1) | 0.00 (0.0) | 0.00 (0.0) | 0.01 (0.9) | 1.06 (100.0) |
| 2020 | 0 | 30 | 0 | 3830 | 820 210 | N/A | N/A | N/A | N/A | N/A | |
| 2021 | 0 | 22 | 1c | 4662 | 673 744 | N/A | N/A | N/A | N/A | N/A | |
| 2022 | 0 | 30i | 0 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |
Data for 2003–2005: (Abeyasinghe et al., 2012); 2006–2019: AMC Annual Reports (http://www.malariacampaign.gov.lk/en/resources/annual-reports, [accessed 10 February 2023]) and 2020–2021: Anti-Malaria Campaign, Ministry of Health Sri Lanka unpublished data; 2022 AMC website https://web.archive.org/web/20221126024221/http://amc.health.gov.lk/en/, [accessed 10 February 2023].
Introduced malaria case reported in 2018 (Karunasena et al., 2019).
Blood transfusion-induced malaria case reported in 2021 (Chulasiri et al., 2021).
Data for 2010–2019: AMC Annual Reports (http://www.malariacampaign.gov.lk/en/resources/annual-reports, [accessed 12 February 2023]) and 2020–2021: Anti-Malaria Campaign, Ministry of Health Sri Lanka unpublished data.
Data for 2003–2005: (Premaratne et al., 2019); 2006–2016, 2018–2019 AMC Annual Reports (http://www.malariacampaign.gov.lk/en/resources/annual-reports, [accessed 25 January 2023], 2007: (Gunasekera et al., 2021); and 2020–2021: Anti-Malaria Campaign, Ministry of Health Sri Lanka unpublished data.
Expenditure data from Institute for Health Policy (IHP) Sri Lanka Health Accounts Database. Expenditure for 2019 is provisional.
Domestic financing includes AMC directorate expenditure and medical supplies and other expenditures (e.g, equipment) supplied by the AMC directorate to the provinces. This excludes recurrent expenditure (salaries and other overheads) at the provincial level.
Disaggregation of cases as indigenous and imported are not available. AMC began classifying cases from 2008 onwards.
Total cases up to November.
N/A indicates not available.
Facilitators of transition
From the documentary analysis and key informant interviews and guided by the HPA framework, the changes in health system inputs pre- and post-transition are detailed in Supplementary Tables S (EPI) and S (AMC). In Table 4, we identify the facilitators and barriers to transition by each element of the HPA framework and for each of the two health programmes. In this section, we discuss the key facilitators and barriers to transition common to both health programmes as well as ones that are programme-specific.
Table 4.
Summary of facilitators, barriers and threats for sustaining coverage post-transition by themes of the Walt and Gilson’s (1994) health policy analysis framework
| Facilitator/barrier/threat | Expanded programme for immunization (EPI) | Anti-malaria campaign (AMC) |
|---|---|---|
| Context | ||
| Political commitment for health by successive governments—Sri Lankan health system is built on principles of financial protection, close-to-client services and primary health care | EPI is a national priority programme explicitly identified in health policies. Immunization services are free and accessible to all Sri Lankans through a network of decentralized 356 Medical Officer of Health (MOOH) units and health facilities covering the entire Sri Lankan population. EPI vaccines can be obtained free to those who access the private sector. | AMC over the years has received political commitment for malaria control and elimination efforts. Malaria being the highest priority health challenge in the Ministry of Health (MoH)’s formative period (1930–1960) influenced the MoH’s organizational structure and orientation and development of health facilities particularly in malaria endemic regions. Preventive and curative interventions are available free-of-charge and anti-malaria interventions are implemented island wide based on need. |
| Historically well-established programme with strong domestic financing base | Established in 1978. Prior experience of successful donor transition. | First anti-malaria unit established in 1911. Continuous domestic financing base although external assistance received from multiple donors over the years. |
| Tangible programme success reinforces political commitment | High vaccine coverage rates and zero or low incidence of vaccine preventable diseases. Public demand for immunization services. | Near elimination effort in 1963. Malaria-free certification in 2016. As observed historically, political commitment can wane due to low prioritization in the context of elimination. |
| Government health spending—relatively low, but stable | New vaccines added even without external support. | Domestic financing base maintained supplemented with external assistance. |
| Macroeconomic context—increasing GDP growth and movement of income bracket followed by economic downturn | Increasing GDP growth during Gavi transition. Sri Lanka graduated to middle income country status (IMF criteria), a reason to trigger Gavi accelerated transition. | Economy slowing down during GFATM transition. |
| Health system inputs Governance | ||
| Controlled devolution of health to subnational (provincial) level. Decentralized preventive health services under the purview of nine provincial ministries of health (PMoHs). Central MoH retained functions of policy development, procurement, human resources and training, monitoring and evaluation and stewardship | Epidemiology Unit of the central MoH holds the functions of policy development, monitoring and evaluation and stewardship. Procurement, human resources and training are further integrated within the larger health system. Immunization service delivery is under the purview of the PMoHs. EPI is fully integrated with maternal and child health (MCH) services. | A semi-vertical programme. Central directorate holds the functions of policy development, procurement, human resource training, monitoring and evaluation and stewardship. Decentralized at the regional level, regional malaria officers (RMOs) and their teams are responsible for programme implementation. Some limited integration with MOOH units for some activities. RMOs report to the PMoHs and are accountable to the AMC directorate. |
| Central responsibility for equitable allocation of resources to achieve national health goals including channelling of external assistance to subnational levels based on need | The Epidemiology Unit ensures equitable access to resources including that of external assistance for achieving national health goals (e.g, Gavi health systems strengthening grant channelled towards development of infrastructure and human resources (HR) to post-conflict areas). | The AMC directorate ensures equitable allocation of resources including that of external assistance for achieving national health goals. The AMC directorate negotiates external assistance on behalf of the provinces whose needs can vary based on disease burden and other reasons (e.g. underserved post-conflict areas). |
| Multi-tiered system of monitoring from regional, provincial to national level ensures subnational and national level health goals are met | The EPI is monitored at the regional, provincial and national level. Direct monitoring of programme implementers by the Epidemiology Unit occurs when needed. | Due to the semi-vertical nature of the AMC, RMOs at the regional level report directly to the provincial level and are accountable to the central directorate. |
| Advisory committees including experts from outside MoH provide technical input for evidence-based decision-making. Committee chaired by the director general of health services (DGHS) can facilitate support from the highest level of the MoH | The advisory committee on communicable diseases (ACCD) chaired by the DGHS functions as the equivalent of a national immunization technical advisory group (NITAG). Vaccines excluded from the EPI even when external assistance for vaccine initiation was available, based on evidence-based deliberations at the ACCD. | The technical support group (TSG) chaired by the DGHS, provides technical support to the AMC. Central MoH administration support for the AMC has been forthcoming even in the context of elimination likely contributed by the institutional memory of malaria among the current administration which can wane over time. |
| Opportunities for broader stakeholder participation | Forums such as national immunization summits organized by the Epidemiology Unit facilitate participation of a range of stakeholders for deliberations pertaining to immunization programme. This creates transparency enabling buy-in for implementation of the EPI and financial support from Ministry of Finance (MoF). | Decreased following malaria elimination. Community-based organizations (CBOs) were involved in the anti-malaria programme prior to malaria elimination. Collaborations with the military and international organizations (UNHCR and UNOPS) are stronger due to the nature of high imported malaria risk groups—UN Peacekeeping forces and refugees, respectively. |
| Service delivery | ||
| Level of integration | Gavi funded vaccine was incorporated within the EPI. EPI is fully integrated within MCH services implemented by MOOH units. | A semi-vertical programme. Limited integration in some programme components. Organization of the AMC largely unchanged even following several programmatic shifts following malaria elimination and GFATM funding transition. |
| Service delivery within existing structures | Delivery of Gavi funded vaccines fully integrated within the existing service delivery structures of the EPI. No parallel structures created due to Gavi funding. | Service delivery underwent several major changes due to: (1) scale-up of interventions until malaria elimination through creation of parallel structures for service delivery; (2) programmatic change by addition of interventions pertaining to prevention of reintroduction and re-establishement following elimination and expansion of AMC to previously malaria non-endemic regions due to geographical change in disease burden; and (3) programme reorientation to prevention of reintroduction (POR) only phase triggered by the GFATM funding transition. GFATM supported staff incorporated within existing structures. |
| Financing | ||
| Financing history of health programme—mix and level of domestic financing and donor support | EPI fully graduated from UNICEF funding for vaccines between the period from 1990–1995. EPI continued to receive limited but critical support from UNICEF and WHO for capacity building of staff and continuous quality improvement of the EPI. | Prior to GFATM funding initiation, AMC has received external support over the years through several different donors including technical assistance. These supplemented the existing domestic financing base. |
| Mix of financing sources for health programme components. The domestic and donor financing mix at central and provincial levels for different components of the health programme has implications for transition | Financing for vaccines integrated within overall budget for medicines and medical supplies of the central MoH’s medical supplies division (MSD). Gavi funding was predominantly for vaccines (∼80%). Therefore, a successful transition from Gavi predominantly required bridging the financing gap left by the donor by negotiating with the MoF to increase the vaccine budget under the MSD. EPI implementation (i.e. service delivery) predominantly under provincial health budgets. Negotiation at provincial level not required since Gavi funding not used for service delivery. | GFATM funding was used across all programme components with varying domestic and donor financing mix. This requires mobilization of domestic financing from both the central and provincial levels. In effect, the financial transition from GFATM for the AMC can be largely categorized as a transition for: (1) operational expenses for which domestic financing has largely been mobilized); (2) non-operational expenses for which domestic financing is harder to mobilize; and (3) anti-malarials and other commodities for which AMC has largely continued to seek external assistance. |
| Ear marked financing for health programme or components of health programme | A separate budget line item for vaccines in the MSD budget was implemented since 2008. No earmarked financing for other components of the EPI due to full integration with the Epidemiology Unit at the central level and within MCH services largely delivered at the provincial level. | A separate budget line item for the AMC directorate under the central MoH budget. |
| Human resources | ||
| Health resource (HR) arrangement to implement donor-funded components of the health programme | No parallel HR structures created for delivery of Gavi funded vaccines due to full integration within EPI. Part of Gavi health systems strengthening grant utilized for infrastructure development of training facility and training of HR recruited by MoH for delivery of immunization services, particularly in underserved areas. | Parallel HR structures created to scale-up interventions for malaria elimination during GFATM grants awarded to community-based organizations (CBOs) (2003–2014). GFATM-supported staff incorporated within same organization structure and salary scales throughout GFATM funding period. HR transition required with both GFATM funding transition as well as transition triggered programme reorientation to POR only phase. |
| HR recruitment policies adheres to overall MoH policies and beyond | Seemingly no major impact on HR for EPI due to service integration. | With malaria elimination, an additional programmatic component to the AMC focusing on rapid detection and follow-up of imported malaria cases resulted in expansion of the AMC to previous malaria non-endemic regions thus requiring new recruitment of RMOs and RMO teams Not all positions are filled due to HR recruitment policies beyond the control of the AMC. Furthermore, creating and recruiting specialized staff categories (e.g. GIS expertise) within existing structures is difficult, and can impede optimal programme implementation. |
| HR training for new staff and refresher training for existing staff conducted and coordinated by the MoH | Gavi supported training is fully integrated within educational and training programmes of the MoH. | GFATM supported training is fully integrated within educational and training programmes of the MoH. Training and refresher training often funded predominantly through GFATM and other external donors making this programme component vulnerable to lack of domestic financing and can be a threat to the quality of the AMC. |
| Procurement | ||
| Centralized procurement follows national procurement guidelines and coordinated by the MoH’s procurement division. Medicines procurement mechanism is effective in obtaining low prices for pharmaceuticals due to bulk purchase through global tenders facilitating sustainability by reducing financial cost barriers. Procurement cycles are lengthy | Vaccine procurement is integrated within pharmaceutical procurement, through a central procurement agency via international tenders. WHO prequalification of suppliers is an additional requirement for vaccines. Gavi-funded vaccines procured through UNICEF supply division during Gavi co-financing period. Following Gavi transition, although eligible for ‘Gavi prices’ for five years, the Epidemiology Unit continuously assessed if the MoH pharmaceutical procurement mechanism would yield prices lower than ‘Gavi prices’ and would choose which option for procurement based on the assessment. | Procurement requirement for anti-malarials, insecticides and other non-pharmaceutical commodities decreased with malaria elimination. Utilizing existing procurement methods was challenging due to lack of bidders or bidders quoting very high prices due to low volumes. As a result, anti-malarials obtained through various sources of external assistance. Previously predominantly GFATM financed non-pharmaceutical commodities also sought through other sources of external assistance following transition. |
| Information systems | ||
| Monitoring of donor-funded components integrated within information systems of the health programme | Grant monitoring utilizes existing information system of the EPI. | Prior to malaria elimination parasitological surveillance separately maintained by CBO in areas under their responsibility. Following elimination, all grant monitoring utilizes existing information system of the AMC. |
| Information systems utilized for decision making | Immunization records have been well maintained, recorded, monitored at multiple levels and is utilized to improve immunization coverage and monitor service quality. Paper-based information systems migrated to a web-based platform, an initiative supported by UNICEF. |
Maintains and utilizes four separate information systems for monitoring, evaluation and rapid response. Migrating and integrating these information systems to a single web-based platform to improve efficiency although a goal has not yet been achieved. |
| Transition process | ||
| Transition timelines known in advance | Transition timelines known even though transition triggered earlier than expected and Sri Lanka faced accelerated transition | Transition timelines known in advance and transition triggered due to malaria elimination and receipt of WHO malaria free certification. |
| Transition readiness assessment conducted | Conducted with technical assistance received through GFATM support. Occurred (in 2017) after transition was triggered (in 2016). | |
| Transition planning carried out | Co-financing model facilitated transition planning. Financial sustainability a key concern among technical officers of the Epidemiology Unit, worked together with MoF to ensure financial sustainability. | Transition required across multiple programmatic components requiring changes in different health systems inputs. GFATM funding transition also triggered the most recent technical/programmatic transition to POR only phase. Different components of the programme and health system inputs on different transition timelines. |
| Funding models to facilitate transition | Gavi co-financing model required Ministry of Finance (MoF) as signatory for implementation and awareness among MoF created at inception. Gradual increase in domestic co-financing component. Five year access to ‘Gavi prices’ post-transition. | GFATM transition grant negotiated to further aid the transition process using new funding model (2019–2021). Funding model designed to mobilize domestic resources by reimbursing Treasury at the end of the year based on the AMC achieving a defined pre-negotiated deliverable critical to facilitate transition for each of the three years of funding. |
| Actors | ||
| Political commitment | Public demand for vaccines and tangible gains of the EPI translate to political commitment. | Political commitment during elimination efforts show signs of waning post-elimination due to low disease burden and other health priorities. |
| Support from MoH administration | High priority and adequate support | Well supported. Institutional memory of malaria still present among current MoH leadership. |
| Programme administrators together with technical advisory committees play a lead role in guiding transition | Financial sustainability and improving and maintaining quality of the EPI are key priorities for officers of the Epidemiology Unit overseeing the EPI. New vaccine introductions follow evidence-based deliberations and not simply based on availability of external assistance for vaccine introductions. Officers of the Epidemiology Unit also actively seek ways for broader stakeholder consultation in order to establish greater commitment to the EPI. | Key actors that directed the transition were officers of the central directorate, technical advisors to the AMC, with inputs from the technical leads from the subnational level. These groups were also key decision-making to retain semi-vertical organization of the AMC, notwithstanding malaria elimination, GFATM transition and the programmatic transition to POR. Technical advisors play a key role in guiding POR in the absence of clear guidelines for POR from technical agencies. |
| Other key influencers of transition | MoF as observers of the consultative and transparent process of vaccine-related decision-making as well as tangible benefits of the EPI supports financial sustainability of the EPI. Donor-(Gavi-)initiated co-financing model facilitated transition. | GFATM helped facilitate the transition by supporting a transition readiness assessment, monitoring transition related to programmatic components, and by providing a final transition grant linked to facilitating transition particularly in key areas that were identified as impediments to a smooth transition. |
Source: Authors’ analysis of from documentary review and in-depth interviews.
Contextual factors
Several contextual factors served as overall enablers of transition common to both programmes. First, the Sri Lankan health system is built on several well-established general principles for strong health system performance and health programme success (Rannan-Eliya and Sikurajapathy, 2009; De Silva et al., 2016). These are also applicable to the EPI and AMC and include emphasis on financial risk protection, close-to-client services through a historically well-established health service delivery network and public sector primary health care available free of charge. Second, both programmes are historically well-established (EPI in 1978 and first AMC established in 1911) enjoying strong political commitment with a long-established domestic financing base. To illustrate, the EPI underwent a successful transition from UNICEF funding in the early 1990s and was almost wholly domestically financed prior to initiation of Gavi funding for new vaccines, thus illustrating high existing levels of political commitment towards the programme (UNICEF, 2019). Malaria, a historically important disease due to high disease burden has also received political commitment for elimination efforts (near elimination effort in the early 1960s) (Wijesundere and Ramasamy, 2017). Third, the macroeconomic context was favourable for Gavi transition (Economic Research Department‚ Central Bank of Sri Lanka, 2021). The revision of Gavi eligibility and co-financing policy in 2011 and Sri Lanka graduating to middle-income emerging market status according to the International Monetary Fund (IMF) criteria in 2010 (International Monetary Fund, 2010) triggered Gavi accelerated transition in 2011.
Factors related to health system content
Key features of the governance structure of both health programmes can be considered as facilitators for transition. These include decentralized service delivery, but with a strong central stewardship role that retains policy development and programme monitoring and ensures the equitable allocation of resources (including external assistance) to achieve national health goals. Decision-making for both programmes was supported by technical advisory committees with experts from both within and outside of the MoH (Wijesinghe et al., 2010; Datta et al., 2019). The EPI in particular allowed for broader stakeholder participation (e.g. physician groups, MoH and Ministry of Finance (MoF) officials) such as through national immunization summits. Key informants noted that deliberations in such summits afforded transparency and high acceptance of decisions reached in such forums. Furthermore, it helped build confidence among MoF officials, who were observers of the process, which in turn helped to garner MoF support for the EPI.
Some health system features related to service organization and financing can be identified as major facilitators of successful transition for the EPI compared to the AMC. This is related to what was externally funded, how this funding was channelled to the EPI and how services funded through external assistance were delivered. Approximately 80% of Gavi funding over the period from 2003–2015 was for vaccines (Gavi, The Vaccine Alliance, 2022a). Gavi-funded vaccines were made available from the centre throughout the country, and vaccine administration was fully integrated within the existing service delivery structures. Hence, no new parallel structures for service delivery nor deviation from central procurement resulted on account of Gavi funding. Furthermore, since Gavi funding was predominantly for vaccines and since pharmaceutical procurement for the public sector in Sri Lanka is centralized (Guyer, 2021), determining domestic financing requirements in the absence of the funder was relatively straightforward making the process of transition planning easier (this contrasts with that of the AMC, discussed later).
Process factors
While transition timelines were known well in advance for both health programmes, another major facilitator for the EPI was the Gavi co-financing mechanism, which gradually shifted the burden of vaccine financing to national governments over time (Table 2). As part of the co-financing policy, funding commitments were made known early on with both the MoH and MoF being signatories to the co-financing mechanism.
Actors
Technically qualified staff involved in programme planning and implementation also predominantly guided the transition process of both programmes. As noted by key informants, financial sustainability was an area of top priority for the officials of the Epidemiology Unit working closely with MoF officials (independent of Gavi funding) and they provided leadership to several activities that promoted broader stakeholder involvement in decision-making that helped build support for the EPI (e.g. through national immunization summits). Although both the EPI and AMC (for malaria elimination) received broad political support, community demand for immunizations helped further reinforce this support for the EPI.
Challenges/barriers to transition
Challenges/barriers to transition are more programme-specific and a larger number of challenges were identified for the AMC compared to that of the EPI. In part, this can be attributed to four major factors. One, the major programmatic changes in the AMC that occurred during the GFATM funding period on account of epidemiological shifts (Figure 1). Two, the wide heterogeneity in anti-malaria interventions that required raising significant domestic financing to bridge the funding gap left by GFATM through a range of sources. Three, although the success of the AMC was malaria elimination, this brought added challenges for prevention of re-establishment (POR) when malaria no longer remained a health priority in the context of elimination. Four, retention of the organizational structure of the AMC without changes despite the different programmatic phases and the GFATM funding transition required mobilizing adequate domestic financing to replace donor funding.
Contextual factors
Unlike during the EPI’s immediate post-transition years, the years immediately following the AMC transition from GFATM were not associated with a favourable macroeconomic outlook. In the first GFATM post-transition year in 2019, the economy slowed and government revenue fell to 12.6% of GDP from 14.1% of GDP in 2016, the first Gavi post-transition year (Economic Research Department‚ Central Bank of Sri Lanka, 2021). The next two years (2020 and 2021) saw an even greater decrease in government revenue further compounded by challenges due to COVID-19 (International Monetary Fund, 2022).
In addition to this, an important historical context for the AMC is its experience of a near malaria elimination effort in the early 1960s. Failure to eliminate during this time was attributed to a lack of focus on the AMC (low priority associated with the low disease burden) and has been cited as a main reason to continue to retain the organizational structure of the AMC without change (Anti Malaria Campaign—MoH, 2018). This can be challenging in the context of shrinking fiscal space coupled with malaria elimination. A main challenge for programme managers particularly at the sub-national level is having to justify financing for a resource-intensive organizational structure for a malaria-focused programme, which now has a low disease burden.
Factors related to health system content
Some health system features related to service organization and financing made transition for the AMC more challenging compared to that of the EPI. The disease-focused AMC, having a semi-vertical organizational structure, has no formal integration with other mosquito vector borne diseases or other infectious diseases. The challenges to mobilizing domestic financing to maintain this structure were noted above.
Furthermore, the AMC implements several key anti-malaria interventions, which have all received support from GFATM, but to varying degrees. Although these interventions have remained the same throughout the GFATM funding period and beyond, their mix and geographical coverage have changed with programmatic changes associated with the epidemiological shifts associated with malaria in Sri Lanka (details provided in Supplementary Table S2). To illustrate, along with the extent, target and scope of the different interventions, a shift in disease burden from imported cases to regions previously non-endemic to malaria resulted in an expansion of the geographical coverage of interventions to these regions as well (Anti Malaria Campaign—MoH, 2018). Thus, at a granular level, transition for the AMC must be viewed as having simultaneous multiple transitions across several different programme components in different geographical regions based on risk stratification (in contrast to the EPI where predominantly one component—vaccines—required transition), increasing the complexity of the transition process of the AMC.
This was further compounded by several other factors and is related to the interplay between the level of GFATM funding provided for each intervention, the optimal level of the intervention required to maintain POR and the source of domestic financing that must be tapped to bridge the financing gap. Thus, financial transition for the AMC can be largely categorized as a transition for programme components that require mobilizing domestic financing for: (1) operational expenses (e.g. entomological and parasitological surveillance, vector control, monitoring and evaluation); (2) non-operational expenses (information, education and communication activities, training, research, equipment); and (3) anti-malarials and other commodities (e.g. long lasting insecticide nets and rapid diagnostic tests).
Interventions that require mobilization of operational expenses have historically had a domestic financing base and this domestic base was supplemented with GFATM funding to scale up interventions during malaria elimination. In contrast to operational expenses, activities that require non-operational expenses have traditionally, in the Sri Lankan context, been poorly supported through domestic financing, with health programmes often relying on donor assistance to fund these activities (GFATM Country Coordinating Mechanism Sri Lanka, 2018). Key informants have reported adequate mobilization of domestic financing to meet operational expenses at both the central and provincial levels during the three years following GFATM transition (2019–2021). However, funding for non-operational expenses was reported to be harder to come by, and advocacy and training activities were further affected by COVID-19 suggesting a mixed transition success for the AMC. Furthermore, as noted by key informants, reliance on donors for pharmaceuticals and other essential commodities for the AMC continues due to low volume requirements that no longer yields low prices through the central procurement mechanism for pharmaceuticals in the public sector.
In addition to the financial transition, a human resource (HR) transition was required for GFATM supported staff in various positions at national and subnational levels of the AMC. Difficulty in predicting the exact level of POR interventions, which requires tailoring to country situations based on general guidelines (WHO Eastern Mediterranean Regional Office, 2007; Nasir et al., 2020), creates challenges in projecting HR needs. This, together with HR recruitment policies that are beyond AMC’s control are challenges in the HR transition that can hinder seamless implementation of POR (UCSF Global Health Group & Anti-Malaria Campaign - MOH, 2018), and which has made the GFATM transition more challenging.
Process factors
Transition planning for the AMC occurred relatively late (in 2017) after transition had already triggered (in 2016). The AMC additionally was given a final transition grant by GFATM to further aid the transition process particularly in three areas identified as critical for transition success—improving procurement efficiency, revising parasitological surveillance and programme orientation to reflect POR and HR transition (GFATM Country Coordinating Mechanism Sri Lanka, 2018; GFATM, 2022). Financial transition planning was initiated relatively early, and success is seen in having mobilized operational expenses for key malaria interventions that traditionally had a domestic financing base. In preparation for GFATM transition, subnational level managers were encouraged to submit their workplans and budgets to the provincial MoHs by increasing the level of domestic financing for operational expenses needed to implement these interventions (GFATM Country Coordinating Mechanism Sri Lanka, 2018; UCSF Global Health Group & Anti-Malaria Campaign - MOH, 2018). However, other areas such as HR and resources for key anti-malaria interventions that require mobilization of non-operational expenses have lagged. While a gradual transition was implemented for some programme components to aid transition (e.g. gradual reduction in the number of GFATM funded entomological surveillance days) (GFATM Country Coordinating Mechanism Sri Lanka, 2018), such mechanisms were not implemented for all programme components that received GFATM funding. Additionally, unlike in the EPI, no formal co-financing mechanism was implemented.
Actors
The decision to maintain the current organizational structure was predominantly shaped by technical leads from within and outside of the AMC who have made key contributions towards malaria elimination and POR (Datta et al., 2019). This occurred during programme reorientation discussions and meetings on transition planning held in 2017 (Anti Malaria Campaign—MoH, 2018), a time when the macroeconomic outlook was somewhat more favourable than immediately after transition (Economic Research Department‚ Central Bank of Sri Lanka, 2021), potentially giving rise to a disconnect between planning then and dual shocks to the health system with COVID-19 and the economic crisis immediately after transition.
Discussion
In one of the first such studies in Sri Lanka, we conducted an in-depth assessment of two well-established health programmes with strong domestic financing bases that transitioned away from external assistance for health within the past 10 years. Although external assistance, either before or after transition, did not bring about any major changes in programme organization or service delivery structure in either programme, a major difference between the two programmes was transition complexity. Whilst the EPI continued unchanged with respect to its workload before, during and after the period of external assistance (essentially a transition to the previous pre-GAVI state, and not a transition to a new condition), there were major changes in the scale and geographic coverage of service delivery for the AMC. This was a result of having to face and adapt to major changes in its targets and objectives with changing disease burden due to malaria elimination and threat from imported malaria cases. Importantly, having a zero disease burden had major implications for domestic budget prioritization.
Our findings indicate that transition success was achieved for the EPI. Gavi financing was predominantly utilized for vaccines, a component that Sri Lanka has domestically financed since the mid-1990s until Gavi funding initiation in 2003 to expand the vaccine portfolio. Therefore, sustaining the coverage of Gavi-funded vaccines required bridging the financing gap for vaccine procurement at the central level. This was successfully achieved through negotiations by the efforts of key officers at the Epidemiology Unit in collaboration with MoF and facilitated by the Gavi co-financing mechanism. A study by Saxenian et al. (2015) of transition readiness assessments conducted by Gavi in graduating national immunization programmes identified several key areas for transition success, of which Sri Lanka meets most criteria. These include favourable economic growth (at time of Gavi graduation) (Economic Research Department‚ Central Bank of Sri Lanka, 2021), political commitment (UNICEF, 2019), adequate technical capacity for vaccine planning and advocacy, vaccine procurement policies and practices (National Procurement Agency, 2006), national regulatory capacity, immunization technical advisory bodies and their effective functioning (Wijesinghe et al., 2010; Datta et al., 2019) and budgeting for vaccine purchase and cost tracking and estimates (Ministry of Health, 2017). A Gavi appraisal also concurred with this strong performance of Sri Lanka’s EPI (Gavi, The Vaccine Alliance, 2015).
For the AMC, GFATM funding was received for all programme components. Given the unchanged organizational structure following malaria elimination as well as the GFATM transition, bridging the financing gap left by GFATM for these multiple different programme components required mobilizing not only operational expenses, but also non-operational expenses at both the central and provincial levels, an increasingly difficult task in the context of elimination. Given the urgency for bridging the financing gap due to GFATM transition, as part of transition planning, developing a financial sustainability plan was given primacy compared to a number of other components of the AMC that also required transition (UCSF Global Health Group & Anti-Malaria Campaign - MOH, 2018). Our findings for selected indicators that required mobilization of operational expenses (e.g. parasitological and entomological surveillance) suggest sustained coverage, however, with some negative impact due to COVID-19 for parasitological surveillance. Sri Lanka, within and beyond the health sector, has performed poorly in mobilizing domestic resources for non-operational expenses, whereas operational expenses needed for healthcare service delivery and pharmaceutical and non-pharmaceutical commodities for health programmes have generally received financing priority (Amarasinghe et al., 2021). This general system-wide trend poses a challenge to components such as research, advocacy and awareness programmes, and (to an extent) training components required to maintain the quality of the AMC. All this points towards a mixed transition for the AMC, depending broadly on what type of financing was mobilized in response to transition, and which programme component benefited from this. Nevertheless, Sri Lanka has been able to achieve the objectives of POR (i.e. no indigenous cases of malaria since 2012) post-GFATM transition (Anti Malaria Campaign—MoH, 2022), pointing to overall programme success.
Although this study was initiated and conducted during 2020–2022 (during COVID-19 and economic crisis in Sri Lanka) both programmes had transitioned out of external assistance at that time and most data collection and findings predominantly relate to the period prior to these dual shocks to the economy and health system. The impact of the economic crisis has been severe with detrimental impacts observed throughout the health system in general with acute medicines shortages, lack of medical supplies and equipment, migration of healthcare professionals in large numbers and general fiscal tightening policies and recruitment restrictions to the public sector from which the two health programmes are also not immune (Bandara and Alwis, 2022). The economic crisis in particular has implications for financial sustainability of the two programmes in the future. However, there are important differences between the EPI and AMC that influence the likelihood of maintaining public support and hence political and financial commitment for the two programmes. Although the EPI has eliminated some diseases (e.g. polio) others remain relevant and challenging (e.g. HPV). In contrast, the AMC’s managers at the national and provincial levels must advocate for financing a disease in the context of elimination where the disease is no longer perceived as a priority among the public. Therefore, one key driver for financial prioritization (high disease burden) no longer exists for malaria and retaining the current structure of the AMC maybe unviable in the future for implementing POR. While deliberations as part of GFATM transition planning (in 2017) did consider the organizational structure of the AMC, it was decided to retain the same structure for the present time with the main intention of ensuring that the focus remains on malaria (Anti Malaria Campaign—MoH, 2018).
While the GFATM transition has been challenging in general due to its complexity, continued limited spending on health (Amarasinghe et al., 2021), other competing health priorities and increasing personnel in the MoH with a lack of institutional memory or experience with malaria, worsening fiscal space and looming economic crisis were not critical factors considered during the GFATM transition planning deliberations. Therefore, there is likely a potential disconnect between the scope (level and coverage) of the programme components of the AMC for POR decided during transition planning and current resource availability that may have detrimental impacts on the AMC. This may require a major rethink of its organizational structure and service delivery. Any such re-engineering of the AMC should ensure full engagement of all relevant stakeholders, something that is critical for long-term success (Nájera et al., 2011). In this regard, a phased implementation towards integration to build confidence and address stakeholder concerns could be the best approach. Given Sri Lanka’s success with providing integrated services (e.g. EPI), the AMC can look to model itself after successful programmes from within the health system as well as those from outside specifically looking at and learning from countries in the region that have made this transition (e.g. Singapore) (Ministry of Health‚ Singapore, 2017). While funders have generally been reluctant to fund such efforts (Rannan-Eliya, 2022), given the importance of programme sustainability to donors, funding the conceptualization of reengineering the programme up to the stage of implementation should be considered by donors such as GFATM even in the post-transition period.
There are several limitations of this study that are largely due to the complexity of the AMC that resulted from multiple programmatic changes in the course of malaria elimination as well as the GFATM funding transition. We were unable to obtain an expenditure breakdown by the different anti-malaria interventions due to the reporting structure of budgets thus preventing an exact assessment of the financial transition of the different programme components. Additionally, coverage indicators for all interventions, particularly the ones funded through non-operational expenses were difficult to obtain due to unavailability of a time series of collated information on these interventions. Nevertheless, for both these instances we have obtained qualitative inputs from the AMC staff past and present and corroborated with external experts. We are confident that the general trends presented in this study are accurate. Lastly, it must be acknowledged that assessing whether coverage was sustained for donor funded interventions pre- and post-transition must be viewed in the context of uncertainty surrounding the optimal levels of POR interventions.
Conclusion
This study on donor transitions of two health programmes in the same country, although having contextual and governance-related similarities, provides lessons in donor transitions within the country as well as outside of it. This study reiterates the importance of some well-established pre-requisites for strong health system performance and health programme success. These include health system principles of financial protection, close-to-client services and primary health care. Nationally prioritized and therefore well-established health programmes with a strong domestic financing base, central control over equitable allocation of resources and structures in place to achieve national health goals were some governance-related factors identified for transition success. Other key facilitators of transition as illustrated in the EPI experience are service integration and gradual phasing of funding over time. The cross-programme comparison between the EPI and AMC suggests the importance of early delineation of what programme components receive donor financing, and for each programme component, the level of coverage and extent of donor funding over time, domestic financing source at national/sub-national levels that need to be mobilized to bridge the financing gap left by donors or the available avenues to achieve efficiency during shortfalls in domestic financing. This planning process can help highlight key areas where domestic financing bottlenecks exist and where limited but continued donor funding can make substantial contributions to the health programme. The Sri Lankan experience also highlights the importance of factoring in contextual factors such as future macroeconomic projections and policies that can impact fiscal space for health and political commitment that reflect public prioritization of diseases during decision-making on health programmes’ structure and organization.
Supplementary Material
Acknowledgements
The authors thank the support received from the Anti-Malaria Campaign (AMC), particularly Drs Prasad Ranaweera and Pubudu Chulasiri, and the Epidemiology Unit, particularly Dr Deepa Gamage for facilitating this study. We are also grateful to WHO colleagues Drs Zubin Shroff and Susan Sparkes for their insights and feedback throughout this project, Dr Kamini Mendis for comments on the manuscript and all staff at IHP, particularly Dr Sarath Samarage, who supported this study. The authors would also like to thank Anas Ismail and Lorena Guerrero-Torres from the Alliance for Health Policy and Systems Research, WHO for their help with proofreading the paper.
Contributor Information
Prasadini N Perera, Institute for Health Policy (IHP), 72, Park Street, Colombo 02, Sri Lanka; Department of Pharmacy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka.
Sarasi N Amarasinghe, Institute for Health Policy (IHP), 72, Park Street, Colombo 02, Sri Lanka.
Sachini H Fonseka, Institute for Health Policy (IHP), 72, Park Street, Colombo 02, Sri Lanka.
Nihal Abeysinghe, Institute for Research & Development, Battaramulla, Sri Lanka.
Ravindra P Rannan-Eliya, Institute for Health Policy (IHP), 72, Park Street, Colombo 02, Sri Lanka.
Supplementary data
Supplementary data is available at Heath Policy and Planning Journal online.
Data availability
The data underlying this article are available in this article and in its online supplementary material. Part of the data cannot be shared publicly in order to maintain the privacy of individuals who participated in this study. The data will be shared on reasonable request to the corresponding author.
Funding
This work was supported by the Alliance for Health Policy and Systems Research, WHO in collaboration with the WHO Department of Health Governance and Financing and UHC 2030 [APW 202675851]. The Alliance was supported through core funding and project-specific designated funds. The full list of Alliance donors is available at https://ahpsr.who.int/about-us/funders.
Author contributions
Conception or design of the work: P.N.P. and R.P.R.E.
Data collection: P.N.P., S.N.A., S.H.F.
Data analysis and interpretation: All authors.
Drafting the article: P.N.P., S.N.A., S.H.F., R.P.R.E.
Critical revision of the article: N.A., R.P.R.E.
Final approval of the version to be submitted: All authors.
Reflexivity statement
The authors include a mix of women (P.N.P., S.N.A., S.H.F.) and men (N.A., R.P.R.E.) and all are from Sri Lanka reflecting varying levels of seniority supporting capacity building of junior health policy and systems researchers. Research expertise of the authors cover health systems, healthcare financing and costing, health policy and population health surveys.
Ethical approval
Ethics approval was obtained from the ethics review committee of the Faculty of Medicine, University of Colombo Sri Lanka and administrative approval was obtained from the MoH on 26 October 2021.
Conflict of interest statement
None declared.
References
- Abeyasinghe RR, Galappaththy GN, Gueye CS, Kahn JG, Feachem RG. 2012. Malaria control and elimination in Sri Lanka: documenting progress and success factors in a conflict setting. PLoS One 7: e43162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amarasinghe SN, Fonseka HSH, Dalpatadu KCS et al. 2021. Sri Lanka’s national health accounts: national health expenditures 1990-2019. Colombo: Institute for Health Policy. [Google Scholar]
- Anti Malaria Campaign - MoH . 2018. National strategic plan for prevention of re-introduction of Malaria in Sri Lanka 2018-2022. Colombo: Anti Malaria Campaign. [Google Scholar]
- Anti Malaria Campaign - MoH . 2022. Anti Malaria Campaign | Sri Lanka. Colombo: Anti Malaria Campaign. https://web.archive.org/web/20221126024221/http://amc.health.gov.lk/en/, accessed 5 March 2023. [Google Scholar]
- Asian Development Bank . 2019. Growing Old before Becoming Rich: Challenges of an Aging Population in Sri Lanka. Manila, Philippines: Asian Development Bank. [Google Scholar]
- Bandara S, Alwis I. 2022. Editorial: Sri Lanka’s health crisis. BMJ 379: e073475. [DOI] [PubMed] [Google Scholar]
- Bendavid E, Ottersen T, Peilong L et al. 2017. Development assistance for health. In: Jamison DT, Gelband H and Horton S et al. (eds). Disease Control Priorities: Improving Health and Reducing Poverty, 3rd edn. Washington: The World Bank, 299–313. [Google Scholar]
- Bharali I, Mao W, Huffstetler H et al. 2020. Perspectives on transitions away from donor assistance for health: a discrete choices experiment in Sri Lanka. The Lancet Global Health 8: S25. [Google Scholar]
- Chulasiri P, Ranaweera P, Sudarshan P et al. 2021. Transfusion-induced Plasmodium falciparum malaria in a beta thalassaemia patient during the prevention of re-establishment phase in Sri Lanka. Malar J 20: 352. doi: 10.1186/s12936-021-03881-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW, Clark VLP. 2017. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage publications. [Google Scholar]
- Datta R, Mendis K, Wikremasinghe R et al. 2019. Role of a dedicated support group in retaining malaria-free status of Sri Lanka. Journal of Vector Borne Diseases 56: 66–9. [DOI] [PubMed] [Google Scholar]
- Department of Census and Statistics . 2020. Statistical data sheet. Battaramulla: Department of Census and Statistics. [Google Scholar]
- Department of Census and Statistics . 2022. Number of births, deaths and marriages registered by district, 2000-2022. Battaramulla: Department of Census and Statistics. [Google Scholar]
- De Silva A, Ranasinghe T, Abeykoon P. 2016. Universal health coverage and the health Sustainable Development Goal: achievements and challenges for Sri Lanka. WHO South-East Asia Journal of Public Health 5: 82–8. [DOI] [PubMed] [Google Scholar]
- Dieleman JL, Campbell M, Chapin A et al. 2017. Future and potential spending on health 2015–40: development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. The Lancet 389: 2005–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieleman JL, Schneider MT, Haakenstad A et al. 2016. Development assistance for health: past trends, associations, and the future of international financial flows for health. The Lancet 387: 2536–44. [DOI] [PubMed] [Google Scholar]
- Economic Research Department‚ Central Bank of Sri Lanka . 2021. Sri Lanka: macroeconomic developments in charts, fourth quarter 2021. Colombo: Central Bank of Sri Lanka. [Google Scholar]
- Gavi, The Vaccine Alliance . 2015. Joint appraisal report - Sri Lanka. Geneva: Gavi. [Google Scholar]
- Gavi, The Vaccine Alliance . 2022a. Sri Lanka. Geneva: Gavi. https://www.gavi.org/programmes-impact/country-hub/south-east-asia/sri-lanka, accessed 5 July 2022. [Google Scholar]
- Gavi, The Vaccine Alliance . 2022b. Sri Lanka documents | Annual Progress Reports. Geneva: Gavi. https://www.gavi.org/country-documents/sri-lanka, accessed 1 July 2022. [Google Scholar]
- GFATM . 2022. Global Fund Data Explorer - Sri Lanka: Grants. https://data.theglobalfund.org/location/LKA/grants, accessed 30 June 2023.
- GFATM Country Coordinating Mechanism Sri Lanka . 2018. The Global Fund Funding Request Application Form: Tailored to Transition. https://data.theglobalfund.org/location/LKA/documents, accessed 20 July 2022.
- Gunasekera WM, Premaratne R, Fernando D et al. 2021. A comparative analysis of the outcome of malaria case surveillance strategies in Sri Lanka in the prevention of re-establishment phase. Malar J 20: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyer AL. 2021. Procurement of medicines in Sri Lanka: a case study. India Health Systems Project, Working Paper #4. Boston, MA: Department of Global Health and Population, Harvard T H Chan School of Public Health. [Google Scholar]
- Institute for Health Policy. 2021. Sri Lanka health accounts database. Colombo: Institute for Health Policy.
- International Monetary Fund . 2010. Second and third reviews under the stand-by arrangement - staff report. Country Report No. 2010/333. Washington DC: International Monetary Fund. [Google Scholar]
- International Monetary Fund . 2022. Sri Lanka: 2021 Article IV consultation-press release; staff report; and statement by the executive director for Sri Lanka. Washington, D.C: International Monetary Fund. [Google Scholar]
- Karunasena VM, Marasinghe M, Koo C et al. 2019. The first introduced malaria case reported from Sri Lanka after elimination: implications for preventing the re-introduction of malaria in recently eliminated countries. Malar J 18: 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach-Kemon K, Chou DP, Schneider MT et al. 2012. The global financial crisis has led to a slowdown in growth of funding to improve health in many developing countries. Health Affairs 31: 228–35. [DOI] [PubMed] [Google Scholar]
- Ministry of Health . 2016. Malaria elimination in Sri Lanka. National report for WHO certification. Colombo: Ministry of Health, Nutrition and Indigenous Medicine. [Google Scholar]
- Ministry of Health . 2017. Comprehensive multi-year plan for immunization 2017-2021. Colombo: Ministry of Health. [Google Scholar]
- Ministry of Health‚ Singapore . 2017. Communicable diseases surveillance in Singapore. Singapore: Ministry of Health. [Google Scholar]
- Moon S, Omole O. 2017. Development assistance for health: critiques, proposals and prospects for change. Health Economics, Policy, and Law 12: 207–21. [DOI] [PubMed] [Google Scholar]
- Nájera JA, González-Silva M, Alonso PL. 2011. Some lessons for the future from the Global Malaria Eradication Programme (1955–1969). PLoS Medicine 8: e1000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasir S, Amarasekara S, Wickremasinghe R et al. 2020. Prevention of re-establishment of malaria: historical perspective and future prospects. Malaria Journal 19: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Procurement Agency . 2006. Guidelines for procurement of pharmaceuticals and medical devices. Colombo: Ministry of Finance. [Google Scholar]
- OECD/Eurostat/WHO . 2017. A System of Health Accounts 2011: Revised Edition. Paris: OECD Publishing. [Google Scholar]
- Patton MQ. 2002. Qualitative Research and Evaluation Methods. Thousand Oaks, California: Sage Publications. [Google Scholar]
- Perera P, Huffstetler H, Dodoo JNO et al. 2019. Transitions away from development assistance for health: country perspectives from Sri Lanka. In: Global Transition 2019 conference. Beijing, China, 14–16 October, 2019. [Google Scholar]
- Premaratne R, Wickremasinghe R, Ranaweera D et al. 2019. Technical and operational underpinnings of malaria elimination from Sri Lanka. Malar J 18: 256. doi: 10.1186/s12936-019-2886-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rannan-Eliya RP. 2022. Financing malaria. PLoS Global Public Health 2: e0000609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rannan-Eliya RP, Sikurajapathy L. 2009. Sri Lanka: “Good Practice” in expanding health care coverage. Colombo: Institute for Health Policy. [Google Scholar]
- Rannan-Eliya RP, Wijemunige N, Perera P et al. 2022. Prevalence and associations of hypertension in Sri Lankan adults: estimates from the SLHAS 2018–19 Survey Using JNC7 and ACC/AHA 2017 Guidelines. Global Heart 17: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rannan-Eliya RP, Wijemunige N, Perera P et al. 2023. Prevalence of diabetes and pre-diabetes in Sri Lanka: a new global hotspot–estimates from the Sri Lanka Health and Ageing Survey 2018/2019. BMJ Open Diabetes Research & Care 11: e003160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxenian H, Hecht R, Kaddar M et al. 2015. Overcoming challenges to sustainable immunization financing: early experiences from GAVI graduating countries. Health Policy and Planning 30: 197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shroff Z et al. 2024. Managing transitions from External Assistance: cross-national learning about sustaining effective coverage. Health Policy Plan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith O. 2018. Sri Lanka: achieving pro-poor universal health coverage without health financing reforms. Universal Health Coverage Study Series No. 38. Washington, DC: World Bank Group. [Google Scholar]
- UCSF Global Health Group & Anti-Malaria Campaign - MOH. 2018. Sri Lanka Anti-Malaria Campaign Transition Readiness Assessment final report.
- UNICEF . 2018. Immunizational Regional Snapshot 2018 South Asia. Kathmandu, Nepal: Regional Office for South Asia (ROSA). [Google Scholar]
- UNICEF . 2019. Sustaining Vaccination Coverage- Continued national commitment to primary health care with a strong focus on community engagement: a case study from Sri Lanka. Kathmandu, Nepal: UNICEF Regional Office for South Asia. [Google Scholar]
- Walt G, Gilson L. 1994. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy and Planning 9: 353–70. [DOI] [PubMed] [Google Scholar]
- WHO Eastern Mediterranean Regional Office . 2007. Guidelines on Prevention of the Reintroduction of Malaria. EMRO Technical Publications series 34. Cairo: WHO Regional Office for the Eastern Mediterranean. [Google Scholar]
- Wijesinghe PR, Palihawadana P, Peiris TSR. 2010. Participatory decision-making through the advisory committee on communicable diseases: the Sri Lankan experience. Vaccine 28: A96–103. [DOI] [PubMed] [Google Scholar]
- Wijesundere DA, Ramasamy R. 2017. Analysis of historical trends and recent elimination of malaria from Sri Lanka and its applicability for malaria control in other countries. Frontiers in Public Health 5: 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank . 2023. World Bank Country and Lending Groups, Historical Classification by Income [Data file]. NW Washington: Headquarters, The world bank. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups, accessed 13 June 2023. [Google Scholar]
- World Health Organization . 2007. Everybody’s business—strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva, Switzerland: World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in this article and in its online supplementary material. Part of the data cannot be shared publicly in order to maintain the privacy of individuals who participated in this study. The data will be shared on reasonable request to the corresponding author.


