Abstract
Objective:
Challenges providing cleft/craniofacial care in rural communities are often reported, leading to disparities in resources available to clinicians. The purpose of this study was to identify the impact of rurality on caseloads and practice patterns of speech-language pathologists (SLPs) regarding speech and velopharyngeal function for children with cleft lip and/or palate (CL/P).
Design:
A national, survey of US-based SLPs (N=359 respondents) investigated resources, comfort level, caseloads, and practice patterns for children with CL/P. Sub-county classifications that delineated levels of rurality were utilized. Descriptive statistics and chi-square analyses were conducted to determine the impact of population density on assessment and referral decisions.
Results:
Nearly 83% of SLPs reported providing care for a child with CL/P and 41.4% of these SLPs reported five or more children with CL/P on caseload throughout their career. There were no significant differences in rurality of practice setting and the likelihood of treating a child with CL/P. Significant differences were present between rural, town, suburban, and metropolitan-based SLPs regarding available resources (p=0.035). SLPs in rural settings reported feeling uncomfortable treating children with CL/P compared to those in metropolitan settings (p=0.02). Distance to the cleft/craniofacial team and comfort levels impacted referral decisions.
Conclusions:
Most SLPs report having children with CL/P on caseload regardless of practice location. Rurality impacted assessment and referral decisions, especially surrounding access to resources and comfort levels engaging in team care. Findings have implications for developing support systems and reducing barriers for rural SLPs working with children born with CL/P.
INTRODUCTION
Globally, health care provision for individuals living in rural areas has been limited when compared with services available for those living in urban areas.1 Within the United States (US), nearly 21% of the population lives in rural areas.2 Challenges in providing care in rural communities are often reported, which can lead to disparities in resources available to clinicians, patients, and families.3 Thus, rurality has the potential to directly impact healthcare access and provision of services.4 Further, disparities related to rural healthcare and available resources have the potential to be exacerbated in rehabilitation settings when complex and/or low incidence diagnoses are encountered by providers.
Children with cleft lip and/or palate (CL/P) often present as complex clinical cases, given the heterogeneity associated with the condition. Care provision, beginning at birth and extending through early adulthood, is required for a variety of medical needs within this population. Although CL/P is a relatively low incidence condition compared to other populations seen by speech-language pathologists (SLPs), the impact of appropriate assessment and treatment recommendations is immense for these children.5,6 Speech errors related to CL/P are related to a variety of anatomical and learned factors. It has been reported that 66–84% of individuals with CL/P receive speech therapy at some point in their lives for speech errors related to the cleft diagnosis.7–9 Appropriate assessment and referrals are critical to identifying why speech errors are occurring and how to treat them within this population. Without the use of appropriate treatment strategies by SLPs, these individuals may be subjected to ineffective speech therapy throughout childhood, ultimately leading to decreased quality of life and a negative psychosocial impact.10
Treatment of children with cleft and craniofacial conditions relies upon cleft/craniofacial teams to initiate coordinated, interdisciplinary approaches to team care. These multi- and interdisciplinary teams and centers are the standard for ongoing assessment and treatment of children with craniofacial conditions11,12 Within these teams, SLPs play an important role in the care of children with CL/P, providing expertise in conducting comprehensive assessments of speech and velopharyngeal function and facilitating development of management plans Outside of centralized team care, community-based SLPs play an equally important role in the care team for each individual and are often the primary providers engaged in ongoing intervention for speech disorders associated with cleft palate. These providers help to facilitate communication between the patient, the family, and the cleft/craniofacial team, conduct ongoing screening/assessment, and make referrals, often to the cleft/craniofacial team, if there are concerns which cannot be addressed locally.
However, outside of craniofacial centers, healthcare professionals may be unfamiliar with appropriate assessment and intervention techniques for children with CL/P and may lack resources, including instrumentation or imaging such as nasometry and nasendoscopy or multiview videofluoroscopy, to support reliable and regular assessments.13–15 This problem has the potential to worsen in rural areas where healthcare resources are more likely to be limited or deficient. Many rural communities lack access to speech-language pathology services, despite the growing need.16 Rural hospital systems, in general, also frequently report insufficient resources17, which may extend to available resources on rural cleft/craniofacial teams. Further, differences in academic training, clinical training, and practice patterns of SLPs for children with CL/P have also been reported,14,15,18 which has the potential to negatively impact resource utilization and referral decisions for SLPs in general. These differences, however, have not been assessed relative to population density and practice location within the realm of craniofacial care, specifically related to SLP caseloads, resources, referrals, and decisions related to assessment and intervention for speech and velopharyngeal function in children with cleft conditions.
The purpose of this study was to examine the practice patterns (assessment resources, evaluation, and referral decisions) and caseloads of SLPs serving individuals with CL/P across areas of differing rurality (population density and geographic isolation). Based on the literature, it was hypothesized that practice patterns and the available resources for SLPs practicing in rural settings would differ from those of SLPs practicing in areas of greater population density. It was also hypothesized that differences in available resources would impact clinical decision making for children with CL/P.
METHODS
A national survey of the United States (US) was conducted to identify the impact of rurality on caseloads and practice patterns of SLPs regarding children with CL/P. All study procedures were approved by the Institutional Review Board (IRB) at the University of Virginia (IRB-SBS #3738), and an institutional affiliation agreement was obtained with the University of Wyoming. Informed consent was obtained prior to survey data collection.
Participants
Survey participants were licensed speech-language pathologists who hold the American Speech-Language Hearing Association certification/credentials of CCC-SLP (Certificate of Clinical Competence in Speech-Language Pathology) or CF-SLP (Clinical Fellow of Speech-Language Pathology). This indicated that the participants have completed at least a graduate-level education in the survey area of interest. Students, speech-language pathology assistants (SLP-As), and any practitioners that were not licensed or certified SLPs were excluded from the study. The electronic survey was disseminated online to SLPs. Electronic survey announcements were advertised and posted across multiple dissemination outlets, including social media (Instagram, Twitter, Facebook), on state association websites for speech-language pathology, and statewide early intervention groups.
Survey Development
Areas of interest were identified by the researchers based on related publications14,16,19 and content areas were assessed by experts in the field to ensure that questions captured the areas of interest. The survey questions were also reviewed by the university statistics and consulting group to ensure formatting of survey questions and response options matched the areas of inquiry. Demographic questions were additionally modeled from a previously conducted survey to allow for comparison to past results.14 The current survey was constructed and distributed using the Qualtrics XM software (Qualtrics XM, 2021, Provo, UT). The Qualtrics platform was also used to collect data for the anonymous survey. The survey consisted of three parts: 1) provider demographics and care provision, 2) resource availability, and 3) practice patterns. Survey questions can be located in Appendix 1.
Statistical Analyses
Data was analyzed using SPSS Statistics, v26. Descriptive statistics were used to identify differences in resources, comfort level, and current caseloads for SLPs treating children with CL/P across areas of varying rurality. Sub-county classifications that delineated different levels of rurality, including rural-urban commuting areas and frontier/remote area codes, were utilized. These classifications were based on the Institute of Education Sciences (IES) National Center for Education Statistics (NCES) Locale and Classification Criteria.20 The NCES framework utilizes four classification types (city, suburban, town, and rural). These classifications rely on the standard urban and rural definitions developed by the US Census Bureau.21 Using these data, respondents were classified as rural, town, suburb, or city/metropolitan. Chi-square analyses were conducted to examine the relationship between rurality, assessment decisions, and practice patterns.
RESULTS
Respondent Demographics & Care Provision for Children with Cleft Lip and/or Palate
The survey received 359 responses from SLPs over a three-month period. Given the electronic dissemination methods across social media platforms, state associations for speech-language pathology, and statewide early intervention groups, the overall response rate cannot be calculated. Responses were received from SLPs residing in 45 states and the District of Columbia. This demonstrated a broad distribution of respondents, covering approximately 90% of the United States (Figure 1).
Figure 1.
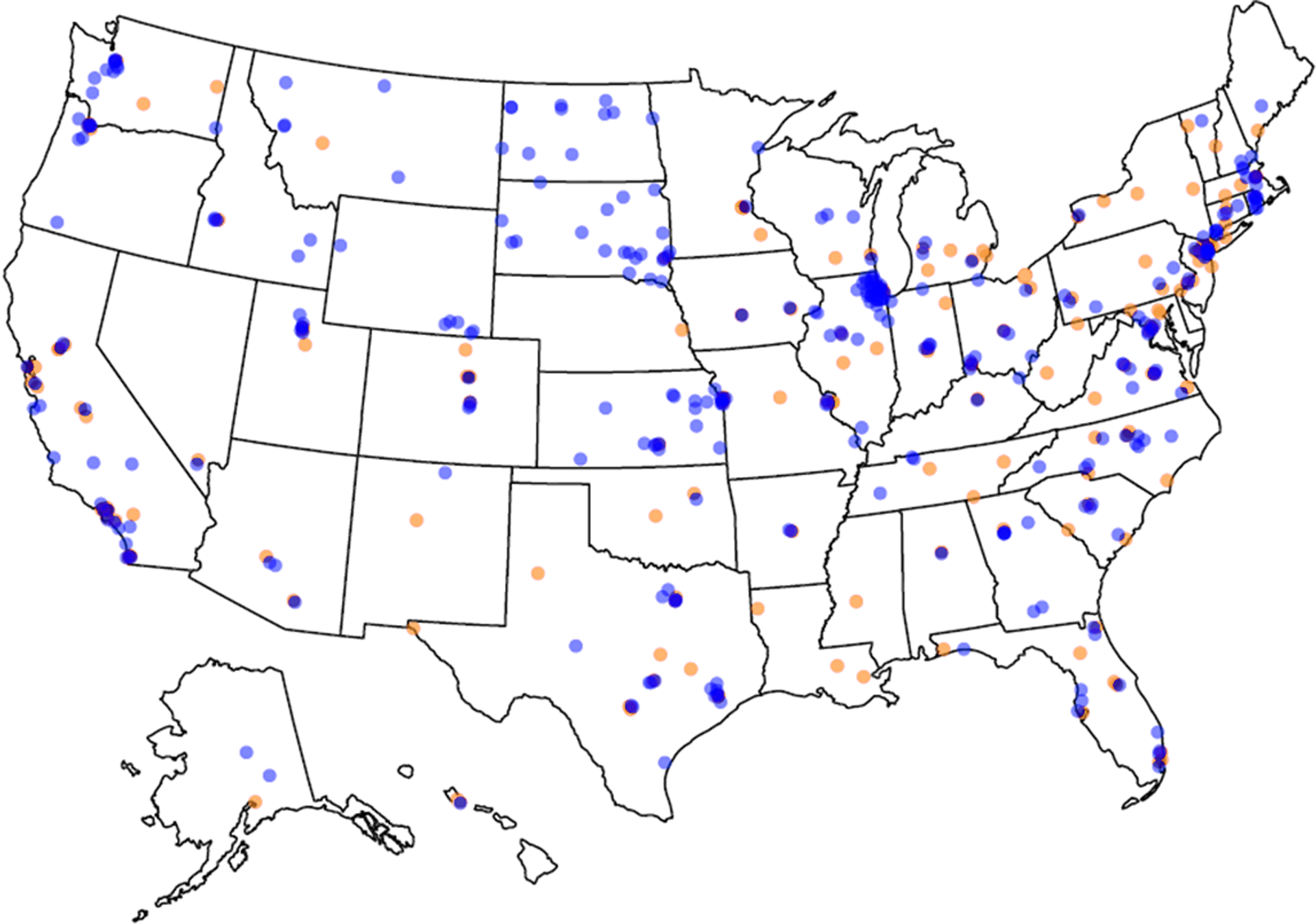
Density map of respondent locations (blue) and location of ACPA approved cleft/craniofacial teams (orange).
Respondents included SLPs with a range of experience spanning from approximately one year to 30+ years. The distribution of respondents related to years of experience was broad with approximately 37% of the sample (N=115) reporting between 6–20 years of experience and 35% (N= 110) reporting 5 years or less experience. Approximately 28% of respondents (N=88) reported over 20 years of experience in the field. Of that group, 41 individuals reported having over 30 years of experience. Given this distribution, results likely reflect a balanced perspective from clinicians with a wide range of experience in the field. Primary practice settings of respondents included early intervention, school-based, private practice/outpatient clinic, inpatient hospital-based, outpatient hospital-based, long-term acute care, home health, skilled nursing facility, college/university, and corporate speech-language pathology (Table 1).
Table 1.
Respondent Characteristics
| N | % | |
|---|---|---|
| Clinical Practice Setting(s) | 315 | 87.74 |
| Early Intervention | 73 | 20.3 |
| School-based | 147 | 40.9 |
| Private Practice/Outpatient Clinic | 67 | 18.7 |
| Inpatient Hospital-based | 43 | 12.0 |
| Outpatient Hospital-based | 64 | 17.8 |
| Long-term Acute Care | 6 | 1.7 |
| Home Health | 18 | 5.0 |
| Skilled Nursing Facility | 13 | 3.6 |
| College/University | 27 | 7.5 |
| Corporate Speech-Language Pathology | 7 | 1.9 |
| Retired | 9 | 2.5 |
| Other | 8 | 2.2 |
| Years in Clinical Practice | 313 | 87.18 |
| < 1 year | 25 | 8.0 |
| 1 – 5 years | 85 | 27.2 |
| 6 – 10 years | 67 | 21.4 |
| 11 – 15 years | 31 | 9.9 |
| 16 – 20 years | 17 | 5.4 |
| 21 – 25 years | 22 | 7.0 |
| 26 – 30 years | 25 | 8.0 |
| 30+ years | 41 | 13.1 |
| Have you ever provided care for a child with CLP? | 306 | 85.23 |
| Yes | 253 | 82.7 |
| No | 53 | 17.3 |
| Number of children with CLP seen over the course of your career | 243 | 67.68 |
| At least 1 | 26 | 10.7 |
| 2 – 4 | 87 | 35.8 |
| 5 – 9 | 45 | 18.5 |
| 10 – 14 | 17 | 7.0 |
| 15 – 19 | 9 | 3.7 |
| 20 – 49 | 17 | 7.0 |
| 50 – 99 | 9 | 3.7 |
| 100 – 499 | 15 | 6.2 |
| 500+ | 18 | 7.4 |
| Primary Practice Location | 315 | 87.74 |
| Rural (including Frontier & Remote) | 39 | 12.4 |
| Town | 70 | 22.2 |
| Suburb | 82 | 26.0 |
| City/Metropolitan | 124 | 39.4 |
| Knowledge of where nearest cleft team is located | 292 | 81.33 |
| Yes | 224 | 76.7 |
| No | 68 | 23.3 |
| Distance of Practice Location to Nearest Cleft/Craniofacial Team * | 224 | 100 |
| Less than 1 hour away | 113 | 50.5 |
| Approximately 1 hour away | 44 | 19.6 |
| Between 1–2 hours away | 38 | 16.9 |
| Between 2–4 hours away | 25 | 11.2 |
| Greater than 4 hours away | 4 | 1.8 |
Total Number of Survey Respondents = 359
Note: This question was only provided to respondents that indicated “yes” for the question related to knowledge of where the nearest cleft team is located (N=224)
Likelihood for Treating Individuals with Cleft Lip and/or Palate
Nearly 83% of respondents (N= 253) have provided care for an individual with CL/P. Approximately half of these respondents reported having had five or more individuals with CL/P on their caseload throughout their career (41.4%, N= 105). There were no significant differences in rurality of practice setting and the likelihood of treating an individual with CL/P, χ2(3)= 3.275, p = 0.351 (Figure 2).
Figure 2.
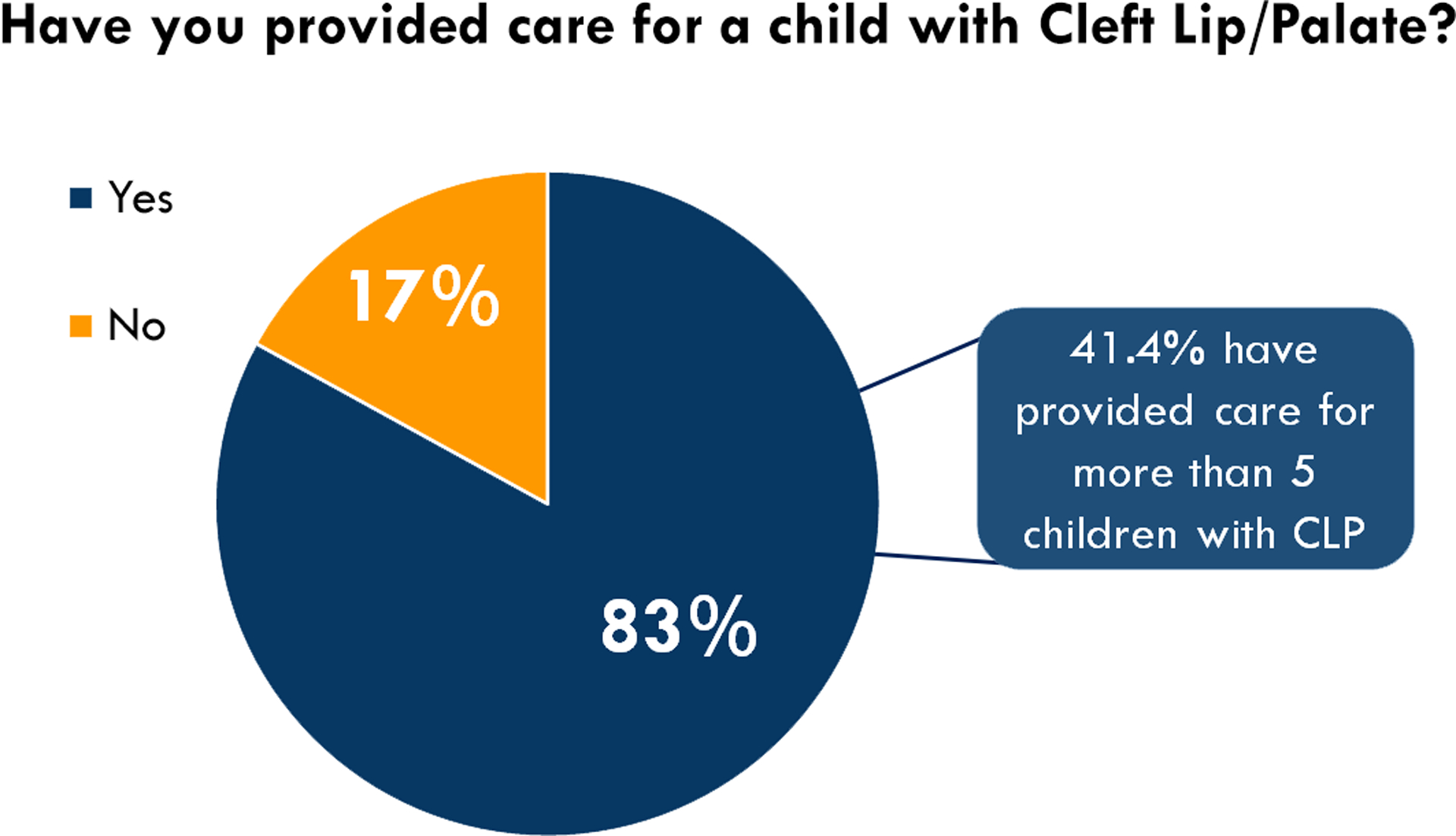
Percentage of SLPs that have had a child with CL/P on their caseload.
Impact of Rurality on Clinical Resource Availability and Resource Utilization
When asked what resources were available to conduct resonance evaluations for children with CL/P, significant differences were present between rural, town, suburban, and metropolitan based SLPs, χ2(9)= 17.97, p = 0.035. SLPs, as a whole, relied more heavily on perceptual assessments than other assessment tools (61.9%, N= 172 out of 278 responses). Metropolitan SLPs were more likely to identify that all clinical resources such as perceptual assessments, instrumentation, and imaging, were available at their place of employment (25.2%). In contrast, very few rural (0%), town (1.6%), and suburban (6.3%) SLPs reported having all available resources for assessment. Imaging was more likely to be an available resource in metropolitan settings, while instrumentation, such as nasometry, was more likely to be reported in town and suburban settings. Rural SLPs were more likely to indicate “no resources” (24.2%) compared to town (8.1%), suburb (7.9%), and metropolitan SLPs (1.4%) (Figure 3).
Figure 3.
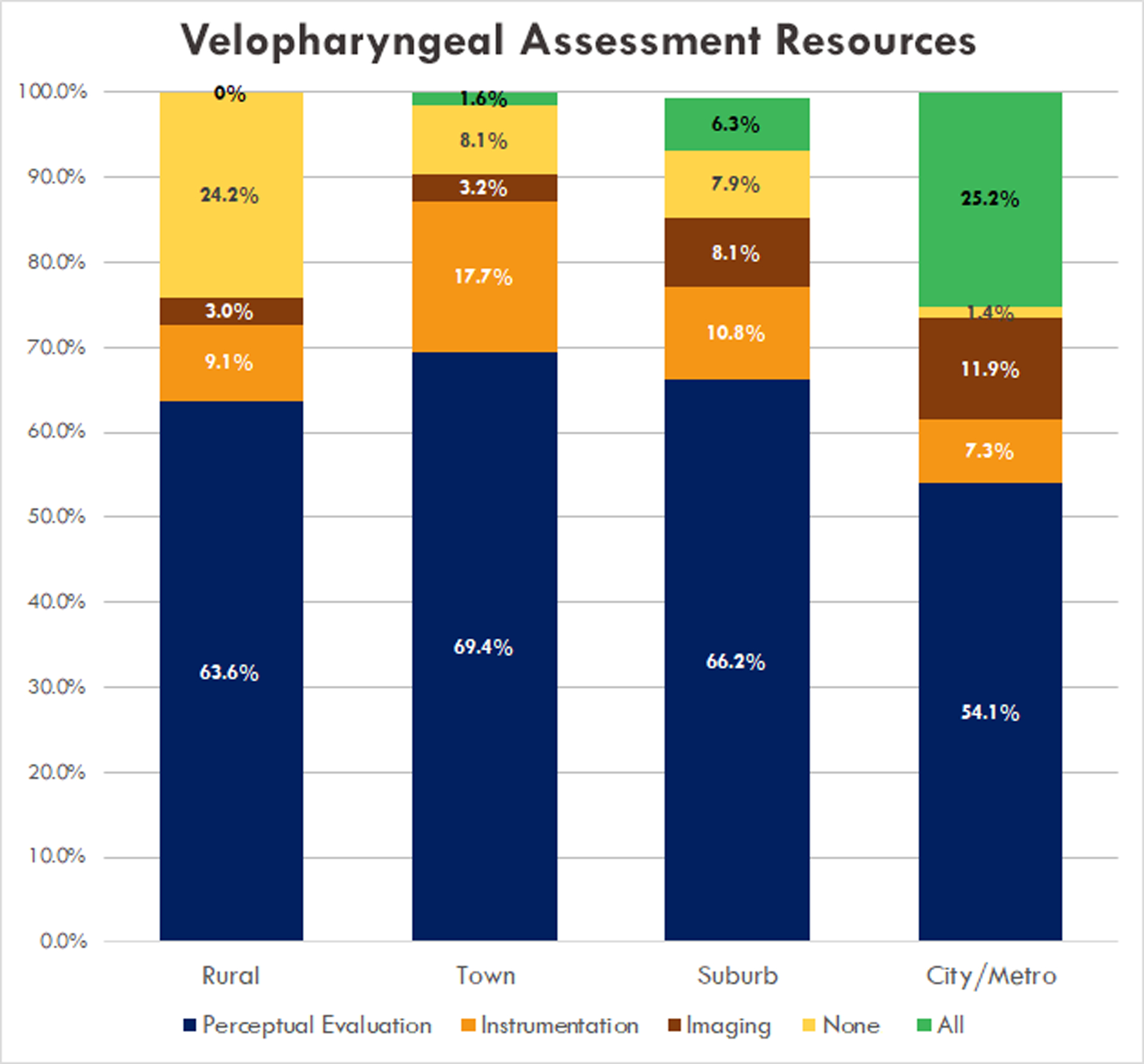
Clinical resource utilization across differing levels of rurality.
When asked which single resource SLPs were most likely to rely on to facilitate assessment decisions, such as the need for referral, need for surgery, or need for speech therapy, the majority of SLPs indicated that they utilized perceptual assessment (63.9%; N= 131 out of 205 responses), while 17.1% (N=35) indicated that instrumental assessment was most likely to be used, and 9.3% (N= 19) indicated that imaging was most likely to be used. Approximately 10% of respondents (9.8%, N= 20) indicated “none and would not assess”. Of this group, 40% were rural SLPs (N=8), 12.5% were town SLPs (N=5), 9.8% were suburb SLPs (N=6), and 1.2% were city SLPs (N=1).
Impact of Rurality on Referral Decisions
As a whole, 32.9% (N=80) of respondents indicated that they were not comfortable knowing when to refer to the cleft/craniofacial team. Significant differences were present between rural and city/metropolitan SLPs related to comfort level for referral decisions, χ2(1)= 5.43, p = 0.020. A greater percentage of SLPs in rural settings (46.2%) reported feeling uncomfortable knowing when to refer children to a cleft/craniofacial team for assessment compared to those in town (30.2%), suburb (34.8%), and city/metropolitan settings (29.6%) (Figure 4). However, most SLPs indicated they would refer a child to the cleft/craniofacial team if they had questions related to resonance (57%) and/or if the child had not seen the team in over a year (45%). Figure 5 summarizes reasons for referral to the cleft/craniofacial team. When asked to rank general comfort level on a five-point scale regarding contacting the local cleft/craniofacial team, rural SLPs were more likely to rank their comfort levels lower (mean rank 2.88; between uncomfortable and slightly uncomfortable) than city/metropolitan SLPs (mean rank 4.60; between comfortable and very comfortable). These findings were independent of years of clinical experience, χ2(7)= 7.27, p = 0.401.
Figure 4.
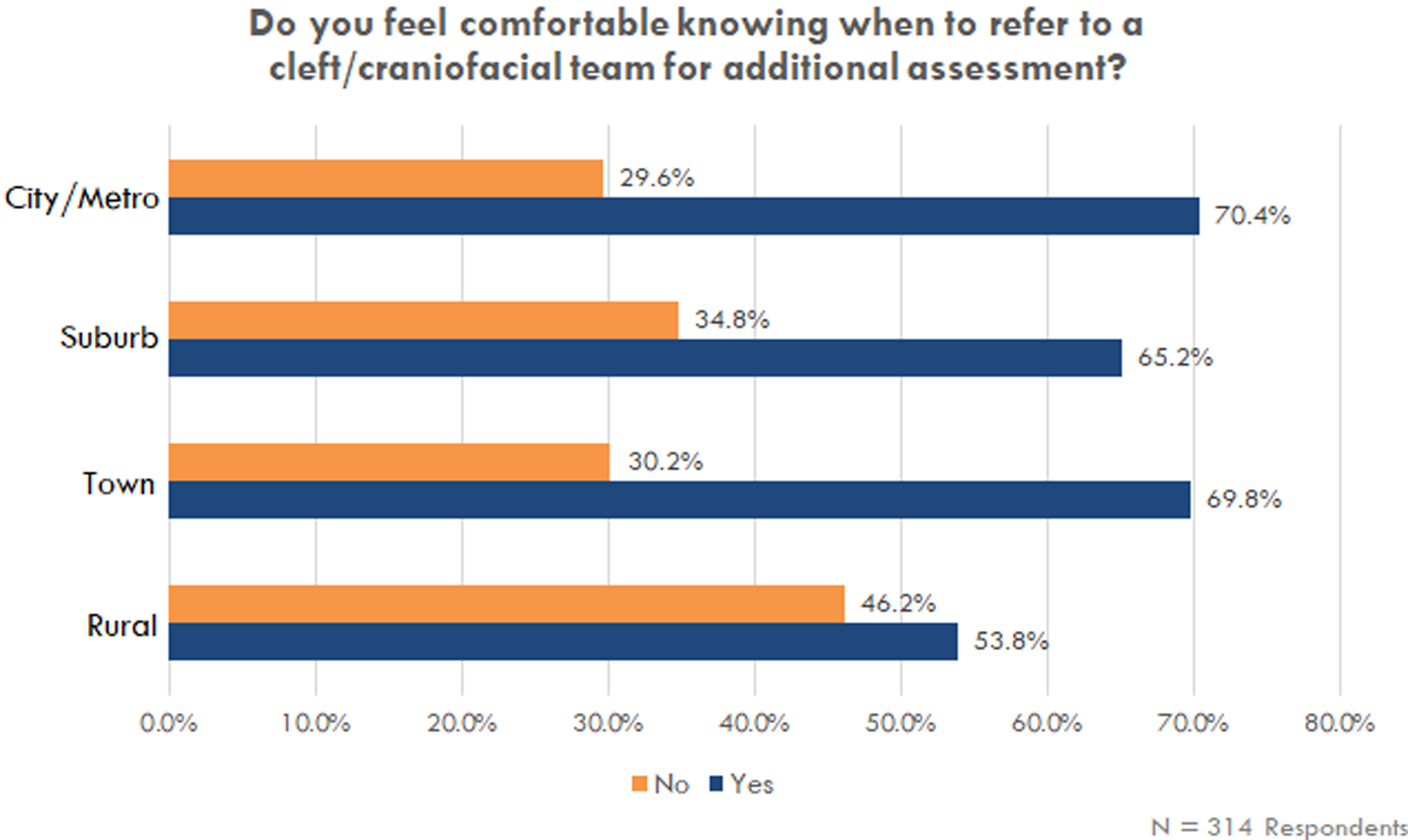
Respondent comfort level related to making referrals to cleft/craniofacial teams.
Figure 5.
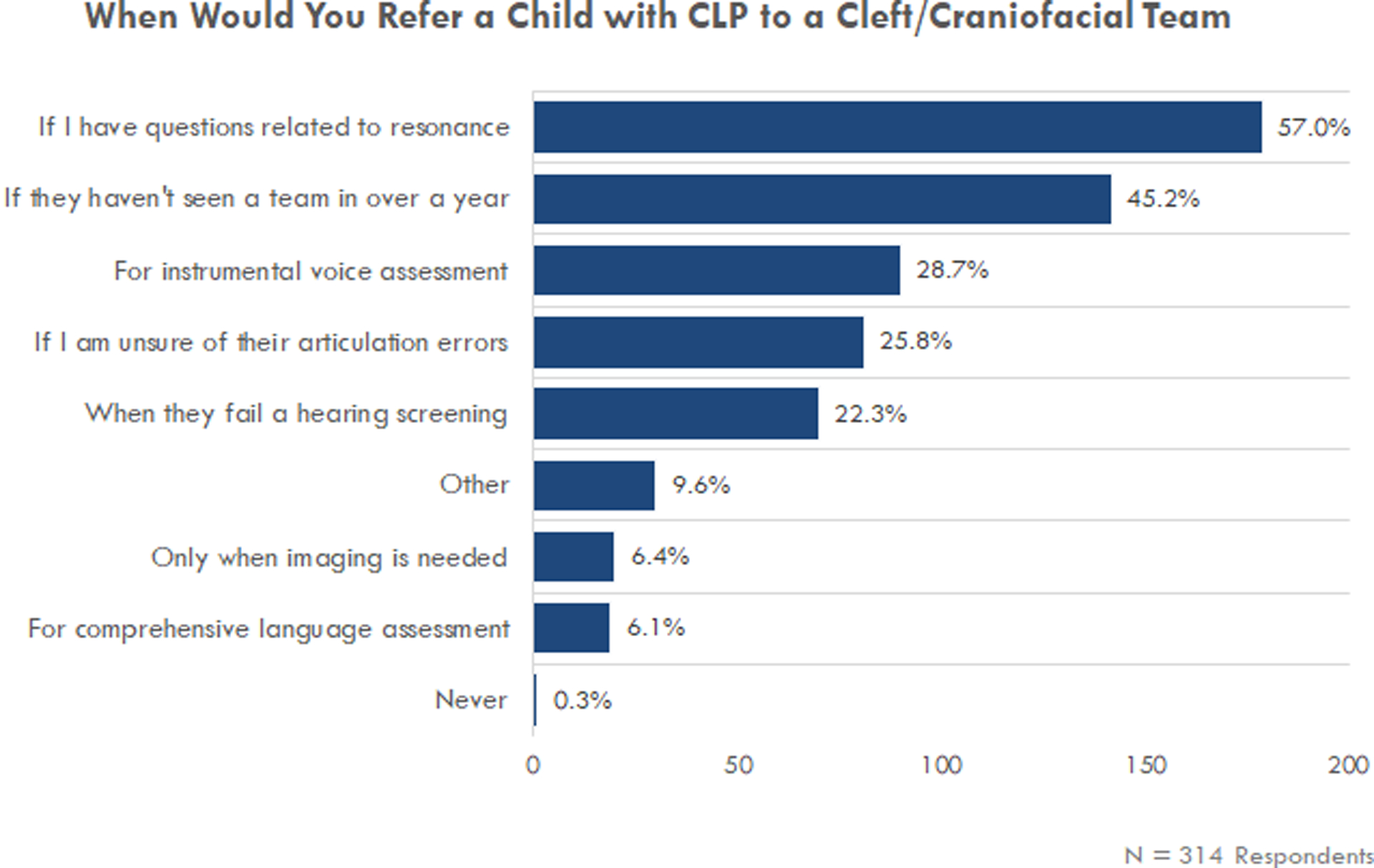
Respondent justification for when referrals would be made.
No significant differences were present across practice locations related to knowledge of where the nearest cleft/craniofacial team was located, χ2(3)= 0.639, p = 0.887. However, 23.3% (N= 68) of survey respondents reported that they did not know where the nearest cleft/craniofacial team was located, while 76.7% (N= 224) indicated that they had this information. The percentage of SLPs that did not know where the nearest cleft/craniofacial team was located was higher in rural practice locations (30.6%) than that of town (20.3%), suburb (21.5%), and city/metropolitan based settings (23.9%). For those that did know where the nearest cleft/craniofacial team was located, the majority reported that the nearest cleft/craniofacial team was less than to approximately one hour away (70.1%). Approximately one third of respondents indicated that the nearest cleft/craniofacial team was more than one hour away (29.9%). Of those reporting distances over one hour, 11.2% reported that the nearest team was between 2–4 hours away and 1.8% reported distances greater than four hours. SLPs in rural settings most often reported that the nearest cleft/craniofacial team was two or more hours away (40%), with 10% of rural SLPs reporting distances of more than four hours.
DISCUSSION
The available clinical resources and practice patterns of SLPs differed based on primary practice location, particularly related to rurality. Those practicing in more populated areas reported having more resources for velopharyngeal assessment, as well as feeling more comfortable engaging in team care and making referrals to cleft/craniofacial teams. In contrast, rurality appeared to impact available resources. This, in turn, impacted the decisions that SLPs made regarding how they would assess a child with CL/P and/or refer to the nearest cleft/craniofacial team.
Studies have identified disparities in access to care for children with complex healthcare needs based on geographic location.22 Access to care has also been reported to differ significantly by state.22 However, limited research has been conducted on SLPs’ experience and comfort level engaging in cleft-related care, particularly as care relates to areas of differing population density and rurality. The current study begins to fill this gap in the literature by reporting the experience, resources, and comfort levels of SLPs concerning care for children with CL/P.
Children with Cleft Lip and/or Palate on SLP Caseloads
An increase in the number of SLPs that reported having children with CL/P on their caseloads was observed. Compared to a prior report by Bedwinek and colleagues14, this number has increased by approximately 10%. SLPs across the United States were similarly likely to have a child with CL/P on their caseload at some point in their careers, regardless of rurality of practice setting. Numerous factors may be at play resulting in a greater likelihood for this population of patients to be on caseload, such as more awareness of speech/language needs for these children, longer lengths of time children with cleft may remain on SLP caseloads, and/or use of less effective treatment techniques due to decreases in graduate level training in cleft-related articulation disorders.14,15,18,23–25 This highlights a need to provide adequate resources for assessment and intervention for this population of patients.
Impact of Rurality on Clinical Resource Availability and Resource Utilization
Availability of clinical resources resulted in significant differences in assessment decisions by SLPs based on the rurality of their practice settings. Specifically, metropolitan SLPs demonstrated greater access to resources, including instrumentation and imaging resources, for assessing speech and velopharyngeal function in children with CL/P. Many of these assessment resources were more likely to be available in metropolitan areas and, consistent with Grames26, cleft/craniofacial teams as a resource are often affiliated with medical centers based in metropolitan areas. However, while not especially common, it is not unheard of for outpatient, university, and private practice clinics, as well as rural hospital systems in the United States, to have access to some instrumentation, such as nasometry, at their practice locations. These locations, at times, may not be affiliated with a cleft team. This is seen in our results on resources available to practitioners and highlights the variability of rurality on resource availability. Additionally, cleft teams can also be located in areas in the US that are considered to be rural (and potentially under-resourced in comparison to metropolitan areas), which may influence resources/practice patterns of those clinicians, despite being on a cleft team.
Rural SLPs consistently reported fewer resources to adequately assess children with CL/P. Responses indicated that the lack of resources for these rural-based SLPs resulted in reduced likelihood for assessment in this population of patients. A proportion of SLPs, approximately 10%, indicated they did not have resources and therefore would not assess children with CL/P at all; this included not conducting perceptual assessments of speech and resonance. The percentage of SLPs reporting that they would not assess was higher in rural areas than more populated areas.
Interestingly, minimal resources are necessary to conduct perceptual assessments of speech/resonance, and thus, would not be expected to be influenced by practice location. Perceptual assessment requires no tools other than the clinician’s trained ear and SLPs are likely to have access to the resources necessary to conduct perceptual analyses of speech and resonance, provided they have the educational foundation needed to assess and interpret data from perceptual assessment. Therefore, this difference in use of perceptual assessments across rurality may be related to access to training and continuing education for this area of clinical practice. Additional research is needed to determine how SLPs are obtaining their knowledge of assessment and treatment for individuals with CL/P and which continuing education resources would be most useful for the present day.
These findings underscore the need for organizations, such as ASHA and graduate training programs, to facilitate acquisition of knowledge and skills related to cleft/craniofacial care. Perceptual assessment should precede any instrumental assessment and assist the SLP in determining the need for additional diagnostics. These assessments for children with CL/P typically include classification of speech sound errors, assessment of resonance and nasal airflow, and correlating perceptual speech/resonance findings with orofacial exam findings.27 A free guide for speech sampling to facilitate perceptual assessment has been developed and is available through the American Speech-Language Hearing Association (ASHA) Practice Portal.28 Additional resources have been described by Mason et al.18, Grames and Stahl29, and Crowley et al.30 A variety of mechanisms are also regularly available through ASHA Special Interest Groups, the International Association of Communication Sciences and Disorders, and the American Cleft Palate/Craniofacial Association (ACPA).
Impact of Rurality on Referral Decisions
The majority of SLPs indicated that they were aware of where the nearest cleft/craniofacial team was located, but differences in comfort level making referrals to the team were seen across areas of differing rurality. Rural SLPs expressed greater levels of discomfort related to making referrals to the cleft/craniofacial team. This may be due to the greater distances reported between practice settings and cleft/craniofacial team locations. Peck et al.19 identified that travel distances of more than 1 hour may affect more than 25,000 (1 of 4) children with CL/P in the US. Within this geospatial survey, there was noted variation across geographic regions.19 These data, in combination with the current study, may help to better understand the impact of rurality on access to care and practitioner referral decisions. Survey findings also indicated that SLPs may choose to refer a child with a CL/P to a cleft/craniofacial team for assessment unrelated to velopharyngeal function (such as for audiological, voice, or language assessment). This may be due to cleft/craniofacial teams typically having more resources than community-based practice locations. It is unknown, however, what additional factors may play a role in referrals and comfort levels making these referrals. Additionally, while the study was framed in the context of patients with CL/P, survey questions also related broadly to velopharyngeal dysfunction and resonance assessment as well. While the survey didn’t specifically ask about children with submucous cleft or non-cleft VPD and comfort levels referring these specific patients, it is likely that referrals for these patients, who may not be known to the cleft/craniofacial team at birth, are lower and potentially delayed in the event referral occurs.31,32 SLP knowledge, experience, and/or comfort level in treating this population of patients may also play a role when choosing whether or not to make a referral for team care. However, treatment experience and treatment methodologies were not assessed in the current survey.
Grames and Stahl29 reported initial outcomes for a novel collaborative care program that engaged community-based SLPs with cleft/craniofacial team SLPs. Through this model, local SLPs can earn continuing education credits while gaining hands-on experience in cleft-related speech treatment. Results of this collaborative model provide SLPs with patient-specific knowledge and foster ongoing partnerships between the cleft/craniofacial team and treating clinicians within the community.29 While this is an ideal approach, it may not be accessible to those SLPs in rural areas where the nearest cleft/craniofacial team is several hours away. There may be additional opportunities to increase access for referring SLPs through telehealth collaboration, particularly for those in rural settings.33–35 Within the global context, telehealth has been reported to provide beneficial methods to improve access to care, particularly for evaluations in developing countries.36–38 Additionally, initiatives have been developed to provide advice and intervention to health care professionals for delivery of speech and language services for children with CL/P.39–41 Areas for collaborations between cleft/craniofacial teams and community SLPs, including relationships via telehealth, should continue be explored.
Clinical Implications
Continued knowledge of assessment processes and confidence referring to the cleft/craniofacial team is imperative to facilitate coordinated care and improve outcomes for children with CL/P. The impact of rurality for SLPs poses potential barriers to providing care for children with CL/P, particularly related to reduced comfort levels and reduced screenings/assessments to identify clinical needs for children with CL/P. Based on the findings of the present study, this may result in a reduction of necessary referrals for comprehensive team care at specialized cleft/craniofacial centers. Implications center on educational opportunities for SLPs and increased coordination with cleft/craniofacial teams. Increased experience during graduate training and accessible continuing education opportunities may further help to improve knowledge and increase comfort for providing care for children with CL/P.14,15,18 Future studies should assess available resources for continuing education for SLPs related to this population relative to rurality. Additional insights may be derived with a detailed understanding of preferred methods for receiving continuing education for SLPs practicing in differing areas of rurality. Continuing education models that facilitate increased comfort in both assessing and treating patients with CL/P and collaborating with cleft/craniofacial teams continue to be necessary.
There is also substantial evidence to support centralization of cleft care in large volume centers, specifically related to facilitating improved patient outcomes and resource utilization.42–44 Work assessing outcomes related to the centralization of cleft care supports high volume centers where specialist assessments take place.8,43,45–47 However, differences exist in the execution of centralized care among countries. Within the United Kingdom, a well-known network of National Health Service (NHS) cleft teams exist, which include local SLP practitioners.43,45,46 In contrast, cleft/craniofacial care in the United States is often positioned in well-organized, high-volume centers situated in individual hospital-based clinics in each state.44 This is often noted to help facilitate geographical access to care.44 These high-volume centers are essential in facilitating care in the United States, but efficacy is reduced if community-based SLPs are not consistently referring patients to the centers or actively engaging in coordinated team care. Additional opportunities for collaborations between the cleft centers and community-based SLPs may be beneficial in reducing barriers for coordinated care. The trends suggested by this study point to the need for cleft/craniofacial teams to facilitate better outreach in their states and/or regions and additional study is warranted. Communication and outreach from cleft centers about the services available from cleft centers, when to refer to these centers, and the process for referrals may better facilitate community-based SLPs in accessing team care for their patients. Increasing SLP knowledge of referral options for team care and other cleft-related services may additionally reduce feelings of isolation and increase comfort levels for making referrals when caring for children with CL/P. It remains unknown if increased comfort level and/or knowledge would result in increased referrals or engagement in team care.
Limitations and Future Directions
The design of the current study is subject to limitations consistent with survey studies. Therefore, caution should be exercised when generalizing the findings of this study. The impact of blank responses by participants is unknown. Respondents may have skipped questions because they lacked definitive views about the topic or were uncertain about the wording of a question.
Results demonstrated that more SLP respondents had caseloads with children with CL/P than prior studies. This may be due to sampling bias, specifically non-response bias, where SLPs that had encountered this population and/or had an interest in this population may have been more likely to respond to the survey than those who did not. Additionally, SLPs who have strong opinions or substantial knowledge may have been more willing to respond to the survey than those who did not. This may alternatively be due to an actual increase in this population on SLP caseloads compared to prior reports given that the distribution of survey respondents in regards to age, experience, clinical setting, and location/rurality was fairly balanced. Additional research is needed to determine whether the findings observed in this study are representative of the larger population of SLPs in the US.
Participant comfort level was not associated with years of clinical experience, but appeared to be influenced by rurality of practice location. However, it is worth noting that in addition to rurality, comfort could also be influenced by a number of external factors such as clinician knowledge, frequency of interactions with cleft/craniofacial teams (or lack thereof), quality of prior interactions with cleft/craniofacial teams, or individual practitioner characteristics. The survey did not explicitly ask respondents what made them more or less comfortable and additional studies are needed to determine if other factors, in addition to rurality, may influence comfort levels related to cleft/craniofacial team referrals.
Another limitation was that this survey did not ask about the modes of transportation when asking respondents about distance to the nearest cleft/craniofacial team. Therefore, we cannot rule out the possibility that respondents may have under- or over-estimated one-way travel distance and time. Further, it is unknown if results may be influenced by the number of cleft/craniofacial centers in each state. States with fewer cleft/craniofacial teams may result in fewer community-based providers being aware of their role, location, and availability. However, in rural states, these care centers are often located at larger, well-known metropolitan health care systems, which could result in more awareness of the cleft/craniofacial team as a resource. Additionally, distance to cleft/craniofacial team and rurality appeared to be associated with greater levels of discomfort related to cleft/craniofacial team referrals, regardless of years in clinical practice. It is unknown if other factors, such as socioeconomic status of the region(s) or access to transportation, may have influenced this association and additional study is warranted.
CONCLUSION
SLPs across the United States are very likely to have a child with CL/P on their caseload, regardless of rurality of practice setting. However, many SLPs in rural settings expressed greater levels of discomfort referring children to cleft/craniofacial teams. Reduced resources for assessment were additionally reported by rural SLPs across all practice settings compared to those in areas with a larger population. Rurality of practice location may impact treatment decisions related to the care of children with CL/P, especially surrounding access to instrumentation, imaging, and referrals for comprehensive team care. Furthermore, highly resourced cleft/craniofacial teams should consider the training and continuing professional development needs of rural SLPs to reduce barriers for collaboration and better support rural SLPs working with children born with CL/P.
ACKNOWLEDGEMENTS
This work was supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Numbers KL2TR003016/UL1TR003015. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to additionally acknowledge the contributions of Makaela Purcell, University of Virginia graduate student, and Katelan Rogers, University of Wyoming undergraduate student, for their assistance in survey dissemination and survey data pre-processing.
APPENDIX 1: SURVEY QUESTIONS
Provider Demographics
- Are you a licensed and/or ASHA Certified Speech-Language Pathologist or Clinical Fellow?
- Yes, ASHA Certified CCC-SLP
- Yes, Licensed SLP
- Yes, Clinical Fellow CF-SLP
- No
- Skip logic: If no is selected, skip to end of survey.
- How many years have you been a practicing SLP?
- < 1 year
- 1 – 5 years
- 6 – 10 years
- 11 – 15 years
- 16 – 20 years
- 21 – 25 years
- 26 – 30 years
- 30+ years
- In what setting(s) do you currently practice (select all that apply)?
- Early Intervention
- School-based
- Private Practice/Outpatient Clinic
- Inpatient Hospital-based
- Outpatient Hospital-based
- Long-term acute care hospital
- Home health
- Skilled Nursing Facility
- College/University
- Corporate Speech-Language Pathology
- Retired
- Other: __________________________
- In what zip code is your primary practice location located?
- Select or type zip code
- Is your primary practice location considered: Rural, Town, Suburb or City/Metropolitan? Please reference this website for more information about these classifications or to identify your classification based on zip code: https://nces.ed.gov/programs/maped/LocaleLookup/. This will be cross-referenced with your provided zip code.
- Rural
- Town
- Suburb
- City/Metropolitan
- Have you provided care for a child with repaired cleft lip/palate?
- Yes
- No
- If yes, approximately how many children with repaired cleft lip/palate have you seen in your caseload over the course of your entire career?
- 1
- 2 – 4
- 5 – 9
- 10 – 14
- 15 – 19
- 20 – 49
- 50 – 99
- 100 – 499
- 500+
- Do you know where your nearest cleft/craniofacial team is located?
- Yes
- No
- If yes, how far away is the nearest craniofacial team from where you practice?
- Less than 1 hour away
- Approximately 1 hour away
- Between 1–2 hours away
- Between 2–4 hours away
- Greater than 4 hours away
Resource Availability
- What resources are available at your place of employment to conduct resonance evaluations for children with repaired cleft lip/palate? (Select all that apply)
- Perceptual evaluations of speech and resonance
- Instrumentation (e.g.: nasometry)
- Imaging (e.g.: nasendoscopy or videofluoroscopy or MRI)
- None
Practice Patterns
- Do you conduct resonance (velopharyngeal function) assessments for children with cleft lip/palate at your place of employment?
- Yes
- No
- Which resource are you most likely to rely on for assessment decisions (i.e.: which resource most helps to inform a decision on the need for surgery, referral to cleft team, or need for speech therapy, etc.)?
- Perceptual evaluations of speech and resonance
- Instrumentation (e.g.: nasometry)
- Imaging (e.g.: nasendoscopy or videofluoroscopy)
- None and would not assess
- When would you refer a child with cleft lip and/or palate to a cleft/craniofacial team? (Select all that apply)
- When they fail a hearing screening
- If I have questions related to resonance
- If I am unsure of their articulation errors
- If they haven’t seen a team in over a year
- Only when imaging is needed
- For comprehensive language assessment
- For instrumental voice assessment
- Never
- Other: _______________________
- Do you feel comfortable knowing when to refer to a cleft/craniofacial team for additional assessment?
- Yes
- No
- Please rate your overall comfort level contacting your local cleft or craniofacial team from least comfortable (1) to most comfortable (5).
- Equal appearing interval scale
Footnotes
Conflict of Interest Declaration:
The work contained in this manuscript was presented at the American Cleft Palate/Craniofacial Association Annual Meeting in March 2022, Fort Worth, TX.
The authors of this manuscript have no conflicts of interest to disclose with respect to the research, authorship, and/or publication of this article.
REFERENCES:
- 1.Strasser R Rural health around the world: challenges and solutions1 | Family Practice | Oxford Academic. Family Practice. 2003;20(4):457–463. [DOI] [PubMed] [Google Scholar]
- 2.Valet RS, Perry TT, Hartert TV. Rural health disparities in asthma care and outcomes. Journal of Allergy and Clinical Immunology. 2009;123(6):1220–1225. doi: 10.1016/j.jaci.2008.12.1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galambos CM. Health care disparities among rural populations: a neglected frontier. Health and Social Work. 2005;30(3):179–182. [DOI] [PubMed] [Google Scholar]
- 4.O’Callaghan AM, McAllister L, Wilson L. Barriers to accessing rural paediatric speech pathology services: health care consumers’ perspectives. Aust J Rural Health. 2005;13(3):162–171. doi: 10.1111/j.1440-1854.2005.00686.x [DOI] [PubMed] [Google Scholar]
- 5.Kotlarek K, Krueger B. Treatment of speech sound errors in cleft palate: A tutorial for speech-language pathology assistants. Language, Speech, and Hearing Services in Schools. Under Review. [DOI] [PubMed] [Google Scholar]
- 6.Kummer AW. Speech and resonance disorders related to cleft palate and velopharyngeal dysfunction: a guide to evaluation and treatment. SIG 16 Perspectives on School-Based Issues. 2014;15(2):57–74. [Google Scholar]
- 7.Hardin-Jones MA, Jones DL. Speech production of preschoolers with cleft palate. The Cleft palate-craniofacial journal. 2005;42(1):7–13. [DOI] [PubMed] [Google Scholar]
- 8.Sell D, Grunwell P, Mildinhall S, et al. Cleft Lip and Palate Care in the United Kingdom—The Clinical Standards Advisory Group (CSAG) Study. Part 3: Speech Outcomes. The Cleft Palate-Craniofacial Journal. 2001;38(1):30–37. doi: 10.1597/1545-1569_2001_038_0030_clapci_2.0.co_2 [DOI] [PubMed] [Google Scholar]
- 9.Bardach J, Morris HL, Olin WH, et al. Results of Multidisciplinary Management of Bilateral Cleft Lip and Palate at the Iowa Cleft Palate Center. Plastic and Reconstructive Surgery. 1992;89(3):419. [PubMed] [Google Scholar]
- 10.Havstam C, Laakso K, Ringsberg KC. Making Sense of the Cleft: Young Adults’ Accounts of Growing Up with a Cleft and Deviant Speech. J Health Psychol. 2011;16(1):22–30. doi: 10.1177/1359105310367529 [DOI] [PubMed] [Google Scholar]
- 11.Parameters For Evaluation and Treatment of Patients With Cleft Lip/Palate or Other Craniofacial Differences. The Cleft Palate-Craniofacial Journal. 2018;55(1):137–156. doi: 10.1177/1055665617739564 [DOI] [PubMed] [Google Scholar]
- 12.Sharp HM. Ethical Decision-Making in Interdisciplinary Team Care. The Cleft Palate-Craniofacial Journal. 1995;32(6):495–499. doi: 10.1597/1545-1569_1995_032_0495_edmiit_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- 13.Blood GW, Thomas EA, Ridenour JS, Qualls CD. Job Stress in Speech-Language Pathologists Working in Rural, Suburban, and Urban Schools: Social Support and Frequency of Interactions. CICSD. 2002;29(Fall):132–140. doi: 10.1044/cicsd_29_F_132 [DOI] [Google Scholar]
- 14.Bedwinek AP, Kummer AW, Rice GB, Grames LM. Current training and continuing education needs of preschool and school-based speech-language pathologists regarding children with cleft lip/palate. Language, speech, and hearing services in schools. 2010;41(4):405–415. [DOI] [PubMed] [Google Scholar]
- 15.Mills B, Hardin -Jones Mary. Update on Academic and Clinical Training in Cleft Palate/Craniofacial Anomalies for Speech-Language Pathology Students. Perspectives of the ASHA Special Interest Groups. 2019;4(5):870–877. doi: 10.1044/2019_PERS-SIG5-2019-0023 [DOI] [Google Scholar]
- 16.Houn B, Trottier K. Meeting The Challenge of Rural Service Delivery. The ASHA Leader. 2003;8(21):2–15. doi: 10.1044/leader.MIW1.08212003.2 [DOI] [Google Scholar]
- 17.Ricketts TC. The Changing Nature of Rural Health Care. Annual Review of Public Health. 2000;21(1):639–657. doi: 10.1146/annurev.publhealth.21.1.639 [DOI] [PubMed] [Google Scholar]
- 18.Mason K, Sypniewski H, Perry J. Academic Education of the Speech-Language Pathologist: A Comparative Analysis on Graduate Education in Two Low-Incidence Disorder Areas | Perspectives of the ASHA Special Interest Groups. Perspectives of the ASHA Special Interest Groups. 2020;5(1):164–172. [Google Scholar]
- 19.Peck CJ, Parsaei Y, Lattanzi J, et al. The Geographic Availability of Certified Cleft Care in the United States: A National Geospatial Analysis of 1-Hour Access to Care. Journal of Oral and Maxillofacial Surgery. 2021;79(8):1733–1742. doi: 10.1016/j.joms.2021.02.043 [DOI] [PubMed] [Google Scholar]
- 20.National Center for Education Statistics. Locale and Classification Criteria. Education Demographic and Geographic Estimates. Published; 2021. https://nces.ed.gov/programs/edge/Geographic/LocaleBoundaries [Google Scholar]
- 21.Geverdt DE. Education Demographic and Geographic Estimates Program (EDGE): Locale Boundaries User’s Manual. NCES 2016–012 National Center for Education Statistics; 2015. Accessed January 29, 2023. https://eric.ed.gov/?id=ED577162 [Google Scholar]
- 22.Singh GK, Strickland BB, Ghandour RM, van Dyck PC. Geographic Disparities in Access to the Medical Home Among US CSHCN. Pediatrics. 2009;124(Supplement_4):S352–S360. doi: 10.1542/peds.2009-1255E [DOI] [PubMed] [Google Scholar]
- 23.del Carmen Pamplona M, Ysunza PA, Sarre P, Morales S, Sterling M. The effectiveness of mentoring speech and language pathology students when they face patients with cleft palate. IntJPediatrOtorhinolaryngol. 2015;79(10):1708–1713. [DOI] [PubMed] [Google Scholar]
- 24.Hardin-Jones M, Jones DL, Dolezal RC. Opinions of Speech-Language Pathologists Regarding Speech Management for Children With Cleft Lip and Palate. The Cleft Palate-Craniofacial Journal. 2020;57(1):55–64. doi: 10.1177/1055665619857000 [DOI] [PubMed] [Google Scholar]
- 25.Alighieri C, Bettens K, Verhaeghe S, Van Lierde K. Speech diagnosis and intervention in children with a repaired cleft palate: A qualitative study of Flemish private community speech–language pathologists’ practices. International Journal of Speech-Language Pathology. 2022;24(1):53–66. doi: 10.1080/17549507.2021.1946153 [DOI] [PubMed] [Google Scholar]
- 26.Grames L Advancing into the 21st century: Care for individuals with cleft palate or craniofacial differences. The ASHA Leader. 2008;13(6):10–12. [Google Scholar]
- 27.Comprehensive Assessment for Cleft Lip and Palate. American Speech-Language-Hearing Association. Accessed March 1, 2020. https://www.asha.org/Practice-Portal/Clinical-Topics/Cleft-Lip-and-Palate/Comprehensive-Assessment-for-Cleft-Lip-and-Palate/
- 28.Trost-Cardamone J Cleft Palate Speech: A Comprehensive 2-Part Set. American Speech-Language-Hearing Association; 2013. [Google Scholar]
- 29.Grames LM, Stahl MB. An Innovative Collaborative Treatment Model: The Community-Based Speech-Language Pathologist and Cleft Palate Team. The Cleft Palate-Craniofacial Journal. 2017;54(2):242–244. doi: 10.1597/16-119 [DOI] [PubMed] [Google Scholar]
- 30.Crowley C, Baigorri M, Sommer C. English Cleft Palate Speech Therapy: Evaluation & Treatment: LEADERSproject. Cleft Palate Speech and Feeding Video Tutorials. Published; 2017. https://www.leadersproject.org/2017/03/23/english-cleft-palate-speech-therapy-evaluation-treatment-playlist/ [Google Scholar]
- 31.Ha KM, Cleland H, Greensmith A, et al. Submucous Cleft Palate: An Often-Missed Diagnosis. Journal of Craniofacial Surgery. 2013;24(3):878. doi: 10.1097/SCS.0b013e31827fef4b [DOI] [PubMed] [Google Scholar]
- 32.Jefferson ND, Willging JP. Management of noncleft velopharyngeal insufficiency. Current Opinion in Otolaryngology & Head and Neck Surgery. 2021;29(4):283. doi: 10.1097/MOO.0000000000000735 [DOI] [PubMed] [Google Scholar]
- 33.Keck CS, Doarn CR. Telehealth Technology Applications in Speech-Language Pathology. Telemedicine and e-Health. 2014;20(7):653–659. doi: 10.1089/tmj.2013.0295 [DOI] [PubMed] [Google Scholar]
- 34.Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79(1):169–176. doi: 10.1038/pr.2015.192 [DOI] [PubMed] [Google Scholar]
- 35.Kotlarek KJ, Haenssler AE, Perry JL. Exploratory Study of Hybrid Telepractice and In-Person Treatment of Compensatory Articulation Errors in Cleft Palate. Communication Disorders Quarterly. 2021;Online Ahead of Print. doi: 10.1177/15257401211067940 [DOI] [Google Scholar]
- 36.Bedi G, Vyas KS, Chung MT, Morrison SD, Asaad M, Mardini S. Telemedicine in International Cleft Care: A Systematic Review. The Cleft Palate Craniofacial Journal. 2021;58(12):1547–1555. doi: 10.1177/1055665621989140 [DOI] [PubMed] [Google Scholar]
- 37.Ramkumar V, Rajendran A, Nagarajan R, Balasubramaniyan S, Suresh DK. Identification and Management of Middle Ear Disorders in a Rural Cleft Care Program: A Telemedicine Approach. American Journal of Audiology. 2018;27(3S):455–461. doi: 10.1044/2018_AJA-IMIA3-18-0015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Whitehead E, Dorfman V, Tremper G, Kramer A, Sigler A, Gosman A. Telemedicine as a Means of Effective Speech Evaluation for Cleft Palate Patients. Ann Plast Surg. 2012;68(4):415–417. doi: 10.1097/SAP.0b013e31823b6897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Balasubramaniyan S, Raghunathan V, Rajashekhar B, Sathiyasekaran BWC, Nagarajan R. Planning community-based intervention for speech for children with cleft lip and palate from rural South India: A needs assessment. Indian J Plast Surg. 2017;50(3):295–301. doi: 10.4103/ijps.IJPS_174_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wirt A, Wyatt R, Sell DA, Grunwell P, Mars M. Training Assistants in Cleft Palate Speech Therapy in the Developing World: A Report. Cleft Palate Journal. 1990;27(2):169–174. doi: 10.1597/1545-1569_1990_027_0169_taicps_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- 41.D’Antonio LL, Nagarajan R. Use of a Consensus Building Approach to Plan Speech Services for Children with Cleft Palate in India. FPL. 2003;55(6):306–313. doi: 10.1159/000073254 [DOI] [PubMed] [Google Scholar]
- 42.Shaw WC, Semb G, Nelson P, et al. The Eurocleft Project 1996–2000: overview. Journal of Cranio-Maxillofacial Surgery. 2001;29(3):131–140. doi: 10.1054/jcms.2001.0217 [DOI] [PubMed] [Google Scholar]
- 43.Ness AR, Wills AR, Waylen A, et al. Closing the Loop on Centralization of Cleft Care in the United Kingdom. The Cleft Palate Craniofacial Journal. 2018;55(2):248–251. doi: 10.1177/1055665617736779 [DOI] [PubMed] [Google Scholar]
- 44.Long RE, Hathaway R, Daskalogiannakis J, et al. The Americleft Study: An Inter-Center Study of Treatment Outcomes for Patients with Unilateral Cleft Lip and Palate Part 1. Principles and Study Design. The Cleft Palate Craniofacial Journal. 2011;48(3):239–243. doi: 10.1597/09-180.1 [DOI] [PubMed] [Google Scholar]
- 45.Ness AR, Wills AK, Waylen A, et al. Centralization of cleft care in the UK. Part 6: a tale of two studies. Orthodontics & Craniofacial Research. 2015;18(S2):56–62. doi: 10.1111/ocr.12111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scott JK, Leary SD, Ness AR, et al. Centralization of Services for Children Born with Orofacial Clefts in the United Kingdom: A Cross-Sectional Survey. The Cleft Palate Craniofacial Journal. 2014;51(5):102–109. doi: 10.1597/13-110 [DOI] [PubMed] [Google Scholar]
- 47.Fitzsimons KJ, Mukarram S, Copley LP, Deacon SA, van der Meulen JH. Centralisation of services for children with cleft lip or palate in England: a study of hospital episode statistics. BMC Health Serv Res. 2012;12(1):148. doi: 10.1186/1472-6963-12-148 [DOI] [PMC free article] [PubMed] [Google Scholar]


