Abstract
Lateral ankle sprain is a common injury with a substantial negative impact on physical function, quality of life and health economic burden. Chronic lateral ankle instability (CLAI) as a sequela of lateral ankle sprain can lead to the development of posttraumatic ankle osteoarthritis in the long term. In this article, we explore the epidemiology, burden and definition of CLAI for the appropriate clinical assessment and imaging evaluation of patients with lateral ankle sprain and CLAI. Following that, recent advances and evidence on management of CLAI is critically distilled and summarized.
1. Introduction
Ankle sprain is a very common musculoskeletal injury with approximately 2 million acute ankle sprains annually in the United States of America1,2 and close to 5600 acute ankle sprains presenting to the Emergency Department daily in the United Kingdom.3, 4, 5 Amongst these ankle sprains, the lateral ligament complex is the most commonly affected where the anterior talofibular ligament (ATFL) which is the primary restraint for anterior talar translation is most frequently injured followed by the calcaneofibular ligament (CFL) as the second most commonly injured structure in a lateral ankle sprain.6, 7, 8 Interestingly, isolated ATFL injury alone accounts for approximately two-thirds of ankle sprains.6, 7, 8
The lateral ankle sprain is not only common but more prevalent in the active sporting population. It is particularly prevalent in the athletic population and in the military where intensive and demanding physical activities are required with an incidence rate of 58.4 per 1000 person-years.9 In the elite athletes, it ranges from 0.495 per 1000 elite athletic exposure (AE) to 1.196 per 1000 elite AE10 and rated as one of the commonest foot and ankle injuries in the UEFA Champions League.11 On top of that, it is not as harmless as what it was thought to be due to the significant negative impact after the injury because there is no simple lateral ankle sprain similarly echoed by both Kerkhoffs et al. and van Dijk et al.12,13 Up to 40% of patients with lateral ligament complex injuries from lateral ankle sprain can continue to experience residual deficits in terms of pain, swelling, recurrent instability and loss of function while many other studies have reported close to 70% of patients can develop chronic lateral ankle instability (CLAI) leading to long term disability.14, 15, 16, 17 Besides, a recent review has also summarized the significant detrimental effects of lateral ankle sprain by illustrating the high rates of reinjury and CLAI followed by the development of posttraumatic ankle osteoarthritis (PTAO) with reduction in physical activity levels and health-related quality of life (QoL) in the longer term.17 In addition, the focus on the financial impact of ankle sprains including both the direct and indirect medical costs on the healthcare system and societal perspective further showed that the burden of lateral ankle sprain does not only affect the physical function and QoL but also leads to profound negative healthcare economic consequences.17
The risk of reinjury is high following an initial lateral ankle sprain leading to the development of CLAI.1,5,17, 18, 19, 20 Up to 34% of patients will suffer at least another ankle re-sprain following an acute lateral ankle sprain at 1 year.19 In fact, one of the most common risk factors for lateral ankle re-sprain is a history of a prior ankle sprain.1,5,17, 18, 19, 20 This is also supported by a recent prospective cohort study where CLAI prevalence was noted to be 40% at 1 year after an index lateral ankle sprain.18 In addition, a recent systematic review of 3804 patients reported that the overall prevalence of CLAI was 25% (range: 7%–53%) while the prevalence of CLAI in patients with prior ankle sprain was almost double at 46% (range: 9%–76%).20
CLAI is characterized by repeated episodes of ankle sprains or perception of an unstable ankle giving way with a collection of symptoms such as pain, swelling, reduced range of motion and diminished self-reported function after an initial ankle sprain.5,21, 22, 23 Mechanical instability is the actual anatomical instability where there is structural tissue damage from the index injury leading to laxity from excessive range of motion exceeding the physiological limit of the joint.21, 22, 23 This laxity is usually demonstrable clinically via anterior drawer test for the ATFL and talar tilt for the CFL respectively.21, 22, 23 On the other hand, functional instability was defined by Freeman as the perception of the foot and ankle giving way without any objective radiological or clinical deviation of the ankle joint motion outside the physiological limit in 1965.21,23, 24, 25, 26 In this group of patients, the symptoms were attributed to proprioceptive deficits secondary to partial deafferentiation of the afferent nerve fibres in the capsule and ligaments of the foot and ankle sustained during the initial injury which leads to impairment of reflex stabilization during locomotion.24, 25, 26 However, further studies have provided that proprioceptive deficit alone cannot account for functional instability but it was a combination of sensorimotor impairment such as altered postural stability, abnormal balancing, poor motor control of muscles proximal to the affected ankle and weakened peroneal muscle strength with slower reaction time to inversion/supination.21,23,27, 28, 29
CLAI is a result of interactions between mechanical and functional instability with a continuum of diseases where these two groups can exist independently or in combination.17,21,23,29 In fact, there have been recent reports that the diagnosis of functional instability may be contributed by an isolated injury of the superior fascicle of ATFL resulting in minor or occult instability which leads to chronic anterolateral ankle pain called “microinstability”.17 Takao et al. first described morphologic ATFL abnormality on arthroscopic assessment for a series of 14 patients diagnosed with functional instability due to no clinically demonstrable lateral ankle laxity.30 These patients subsequently underwent anatomic reconstruction of the ATFL with improved outcomes at 2 years.30 Following that, Vega et al. reviewed the outcomes of 36 patients who underwent ankle arthroscopy with anterolateral ankle pain and functional instability after an ankle sprain with no demonstrable lateral ankle laxity.31 The authors reported morphologic ATFL abnormality in all these patients and proposed that some degree of occult instability can occur due to the deficiency of the ATFL.31 Few years later, Vega et al. again reviewed 232 patients with possible ankle microinstability using their ankle arthroscopy video records and illustrated 4 different patterns of injury involving the superior fascicle of ATFL which was only ascertained arthroscopically.32 In addition, anatomical studies have demonstrated that the presence of the bifascicular ATFL where an isolated tear of the superior ATFL fascicle which is intra-articular can be difficult to recognize with clinical examination.33 Most importantly, the clinical relevance of the bifascicular ATFL was corroborated with a very recent biomechanical study by Dalmau-Pastor et al.34 that the sectioning of only the superior ATFL fascicle leads to excessive internal rotation of the talus while sectioning of the entire ATFL caused significantly reduced resistance in internal rotation, anterior translation, and inversion of the talus confirming the different elements of restraint provided by the superior and inferior fascicles of the ATFL to the ankle joint. The authors concluded that isolated rupture of the superior fascicle of ATFL alone may lead to ankle microinstability without objective clinical findings of lateral ankle laxity via the usual clinical evaluation maneuver.34 Therefore, the spectrum of disease in CLAI depends on the interplay between mechanical and functional instability with the possibility of co-existence.
2. Clinical assessment
Clinically, standing hindfoot alignment should be assessed for the presence of hindfoot varus as it is a risk factor for CLAI with poorer outcomes after surgical repair.23,35 Following that, mechanical stability is routinely tested using the anterior drawer and talar tilt tests for the integrity of the ATFL and CFL respectively.23,36 The positions of the ankle when performing these examinations are of utmost importance because the ATFL is at optimal tension during ankle plantarflexion while the CFL is at optimal tension with the ankle in dorsiflexion.36,37 One should always allow the knee to be flexed (to relax the gastrocnemius muscle) and the ankle to be plantarflexed before performing the anterior drawer test. The tibia is typically held stable with the dominant hand at the distal shin while the other hand holds the hindfoot and translating them anteriorly. A positive test would demonstrate anterior translation, pain or suction sign.38 (Fig. 1) On the other hand, the anterolateral drawer test which was modified from a technique described by Mann in 1999 accounts for the rotatory laxity component.38 Phisikul et al.38 described this anterolateral drawer test in their cadaveric study where the ability to diagnose lateral ankle instability was improved compared to the routine anterior drawer test. In this anterolateral drawer test, the hindfoot is held with the fingers cupping the heel but the thumb is placed overlying the lateral ankle joint line while the ankle is placed in a resting position of 10–15° plantarflexed. The heel is translated anteriorly to visualize the internal rotation of the talus with the foot unrestrained. One should be able to palpate the step-off between the anterior fibula and the lateral talus in a positive test. A follow-up study by the same authors reported that the anterolateral drawer test has high sensitivity, reliability and correlation with the gold standard (anterior drawer test) regardless of examiner's experience.39 This anterolateral drawer test could well be utilized to explain the loss of internal rotation restraint in patients with isolated rupture of the superior fascicle of ATFL as reported by Dalmau-Pastor et al.34 when the conventional anterior drawer test is negative for anterior translation due to intact fibers of the inferior fascicles of the ATFL.
Fig. 1.
1A illustrates the anterior drawer test with the ankle in plantarflexion and the dominant hand holding the distal shin stable while the other hand holds the hindfoot and translating them anteriorly. 1B shows a positive test where there is an anterior translation of the hindfoot.
In terms of assessing the CFL, a talar tilt test can be performed with the ankle in a neutral position to lock the talus in the ankle mortise while inverting the hindfoot in relation to the tibia along the coronal plane.23,36 (Fig. 2) A few cadaveric studies have shown that isolated sectioning of the CFL can increase talar tilt such as that from Kamiya and colleagues who reported 2.9° ± 1.5° to 11.1° ± 5.6° increment in cadavers with CFL deficiency.40 A comparison with the unaffected lower limb will be helpful as the talar tilt test can be confounded by subtalar motion which can be abnormal in certain groups of patients with subtalar instability. On top of that, other modalities for assessment of functional instability measure postural control, balancing and proprioceptive responses using star excursion balance test (SEBT), single leg balance test, single heel raise test, landing pattern, peroneal muscle reaction time and ground reaction forces with time to peak torque.23,36
Fig. 2.
2A and 2B depict the talar tilt test where the ankle is held in a neutral position to lock the talus in the ankle mortise while inverting the hindfoot in relation to the tibia along the coronal plane.
3. Imaging assessment
The main imaging modalities to assess ankle instability include radiographs and magnetic resonance imaging (MRI) scans.23,36,41 Plain radiographs utilizing weightbearing anteroposterior, mortise and lateral views are important to assess for ankle joint alignment and concomitant pathologies such as widening of the syndesmosis and avulsion fractures of the ATFL and/or CFL.41 Stress radiography is an objective assessment performed with the ankle at rest and the ankle during the anterior drawer and/or talar tilt test.36,42 The aim of this stress imaging modality for the anterior drawer test is to demonstrate anterior translation of 10.0 mm on the affected ankle or at least a 5.0 mm difference when compared to the unaffected ankle.36,42 Likewise, the talar tilt test under stress radiographs should show 10° or at least a 5° difference between ankles.36,42
Alternatively, diagnostic ultrasound can also be used as an imaging tool to visualize the lateral ligaments in both static and dynamic modes. It is portable, inexpensive and easily available although it is still very operator-dependent in terms of the quality of image acquisition. Recent evidences suggest that diagnostic ultrasound had a sensitivity in identifying acute ATFL injuries ranging from 94% to 100% while the specificity ranged from 50% to 100%.43 Although it is a feasible imaging modality for lateral ankle instability, the evidence is inconclusive especially for identifying true negative cases.43
MRI scan is still the main workhorse in visualizing the lateral ligament complex for CLAI as well as any concomitant injuries in the ankle. Several studies have reported abnormal ATFL and CFL abnormalities in MRI images of patients with CLAI.36,44 However, the limitation is that these are static images without stress or motion and therefore only morphologic abnormalities can be reported which may not be correlated to clinical findings. Nonetheless, a recent study using 3D volumetric MRI on 30 healthy volunteers has shown that the individual fascicles of the ATFL can be seen on MRI and this is clinically relevant because isolated superior ATFL fascicle injury could potentially be identified routinely in MRI as a cause for microinstability.45 (Fig. 3) In addition, MRI is also very useful in identifying associated injuries. Khor and Tan performed MRI of the ankle for 64 consecutive patients with acute ankle inversion injury.46 They found that only 22% had isolated lateral ligament complex injuries but 78% of the patients had concomitant injuries such as osteochondral lesions, deltoid ligament injuries, bone bruising, and occult fractures.46
Fig. 3.
3A is the sagittal cut of a normal 2D MRI demonstrating the presence of the superior fascicle of ATFL (white arrow) and the inferior fascicle of ATFL (yellow arrow) connected to the CFL via the arciform fibers (red arrow). 3B is the same sagittal cut but taken 1 slice more medial illustrating the superior (white arrow) and inferior (yellow arrow) fascicles inserting to the lateral border of the talar body. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Correspondingly, in a consensus study by a group of international foot and ankle surgeons (ESSKA-AFAS Ankle Instability Group) on the approach to CLAI, the authors concluded that standard plain radiographs (standing) of the ankle and MRI are the two necessary imaging modalities for CLAI.41 Stress radiographs were only used by 40% of the responding surgeons because the rest were confident with the clinical examination findings for lateral ligament laxity which is in concurrence with the literature that stress radiographs only have diagnostic value if they are positive (high specificity: 100% but low sensitivity: 57%).36,41,47
4. Management
4.1. Non-surgical treatment
Regardless of whether the CLAI is functional or mechanical in nature, the first line of treatment is always a rehabilitation programme.23,36,41 Rehabilitation involves proprioceptive training such as SEBT and wobble board training to improve proprioceptive reflexes.23,48, 49, 50, 51, 52 It also aids in developing core ankle stability and coordination skills to improve balance.23,48, 49, 50, 51, 52 Peroneal muscle strengthening is critical in controlling the excessive supination of the ankle joint complex and therefore is an important dynamic stabilizer.23,48, 49, 50, 51, 52 Peroneal strengthening exercises help to improve dynamic stability of the ankle and isokinetic dynamometry can be used to monitor the progress of peroneal muscle strengthening exercises. In addition, strengthening of the muscles proximal to the ankle is also important especially in jump-landing tasks because it has been shown that altered landing kinematics and deficits in postural stability occur in patients with CLAI.51 Hence, rehabilitation after an acute ankle sprain is the key to preventing the development of CLAI and this has been supported by various studies including a systematic overview of systematic reviews that provided strong evidence to suggest exercise therapy and bracing are vital to prevent the development of CLAI after an acute ankle sprain.1,3, 4, 5,52
The duration and intensity of rehabilitation are controversial without a clear guideline. Nonetheless, a consensus study by a group of international foot and ankle surgeons has recommended at least 3 months (93.3%) of appropriate rehabilitation for those with functional instability whereas the majority (56.6%) proposed at least 3–6 months of rehabilitation before surgery should be considered.41 In those with mechanical instability, the majority of surgeons will propose surgery after at least 3 months of rehabilitation when clinical signs of instability were present although special consideration for earlier surgical intervention was reserved for elite athletes with acute grade III injuries as supported by studies with reported benefits such as reduced downtime and shorter time needed to return to sports.7,12,13,17,22,41 As a reference, they have recommended a treatment algorithm for CLAI based on available literature and expert opinions as there is a lack of high-level evidence to make such as recommendation.41
4.2. Surgical treatment
Surgical treatment for CLAI entails restoration of ankle stability with surgical repair or reconstruction. Surgical repair techniques are categorized into anatomic direct repair or nonanatomic procedures while surgical reconstruction can be further classified into those utilizing autografts or those using allografts. Anatomic direct repair which was first described by Brostrom in 1966 involved the primary repair of the ruptured ligaments where both ends of the ruptured ligaments (ATFL and CFL) were sutured with midsubstance imbrication.53 This technique has become one of the most widely used techniques with many modifications such as the Gould modification where the primary repair was reinforced with proximal advancement of the inferior extensor retinaculum (IER) for additional stability. This technique has subsequently been described as the Brostrom-Gould procedure to improve the strength of the repair.54 There is also another modification by Karlsson et al. where the ATFL and CFL are shortened and repaired to the fibula anatomic footprint through drill holes although the use of suture anchors in place of drill holes has gain popularity in recent years.55 Direct anatomic repair has been shown to produce reliable and excellent outcomes in many studies despite the plethora of modifications.22,23,36,41 In fact, it is regarded as the gold standard and first-line treatment in most patients with CLAI except for patients with poor or insufficient residual ligamentous tissue for direct repair, revision cases with previous failed direct anatomic repair, generalized ligamentous laxity and high body mass index.22,23,36,41
For direct anatomic repair procedures, the technical differences are the main points for discussion such as the need for concomitant CFL repair and the need for augmentation procedures such as the Gould modification or suture tape. The need for CFL repair to address CFL incompetency during direct anatomic repair procedures has been highlighted in a cadaveric study where biomechanical differences were compared between the combined ATFL and CFL repair group versus isolated ATFL repair group in 10 matched pairs of cadaveric ankles.56 The authors found that CFL repair is warranted as they contribute significantly to ankle stability in CLAI.56 However, recent anatomical studies have shown that the CFL is connected to the inferior fascicle of the ATFL via the arciform fibers forming the lateral fibulotalocalcaneal ligament complex (LFTCL) and it is functionally capable to transmit tension from one structure to the other, supporting the feasibility of isolated ATFL repair as a truly anatomical repair even though there might be injuries to both the ATFL and CFL.33,57 The only caution to this approach is that the CFL must be damaged more proximally to maintain the connecting arciform fibres. Therefore, it is not surprising that other studies have reported long-term good outcomes with ATFL repair alone in patients with CLAI.58,59 Lee et al. reported long-term outcomes for modified Brostrom procedure without CFL repair for CLAI at a mean follow-up of 10.6 years with good to excellent outcomes in terms of functional, clinical and radiographic assessment (stress radiography).58 Two large series on modified Brostrom procedure without CFL repair on elite athletes have also demonstrated good outcomes in terms of the ability to return to preinjury sports with low reinjury rates.60,61 The authors suggested that the repair of ATFL back to the fibula footprint provided stabilization of the CFL via the arciform fibres linking the ATFL and CFL.60,61 Furthermore, Hong et al. in a recent imaging study demonstrated that the individual fascicles of the ATFL and the LFTCL complex can be visualized sufficiently on MRI potentially allowing surgeons to identify the loss of arciform fibres which can change treatment plan to include CFL repair in cases with LFTCL complex injuries while isolated ATFL repair alone is sufficient in those with preserved LFTCL complex.45 (Fig. 3).
The use of IER augmentation as part of the Gould modification has been examined by several studies without clear consensus. One of the most cited studies by Aydogan et al. compared biomechanical resistance to inversion stress between the Brostrom and the Brostrom-Gould procedures in 9-matched pair cadavers.62 They reported that the group with IER augmentation resisted higher stress to failure and concluded that IER augmentation can protect the primary ATFL repair.63 Conversely, Behrens et al. showed no difference in biomechanical stability whether the IER augmentation was performed or not in a cadaveric ankle instability model.63 Besides, several anatomic and clinical studies have reported that IER augmentation may not be necessary as clinical and radiologic outcomes appear to be similar to those treated without IER augmentation.36,64, 65, 66
In those patients with poor ligamentous tissue for direct repair or revision cases, the use of a synthetic suture tape augmentation has been proposed to improve time-zero construct stability of the direct anatomic repair by protecting the repaired ligament during healing and contributing to scar formation.67 (Fig. 4) Biomechanical studies68,69 have reported similar biomechanical stability conferred by the suture tape augmentation when compared to native ATFL while several clinical studies have demonstrated improved outcome scores and clinical stability (anterior drawer and talar tilt tests).67,70 A recent systematic review of 7 clinical trials reported that suture tape augmentation yielded excellent results and is a safe technique comparable to the Brostrom repair without major differences detected in clinical and radiological outcomes or complications.67 The authors also highlighted that recurrence of instability and revision surgeries tended to occur more frequently after Brostrom repair while irritation of the peroneal nerve and tendons occurred more often with suture tape augmentation although postoperative rehabilitation was notably more accelerated in the suture tape augmentation group.67 Martin et al. reported 93 CLAI patients treated with the Brostrom procedure augmented with a suture tape construct and demonstrated excellent outcomes without subsequent failure at 48 months despite the early accelerated rehabilitation.70 Perhaps, the concern about the use of suture tape augmentation lies more in the degree of tightening needed in the construct due to concerns of overtightening and alteration of ankle joint kinematics given the lack of any physiologic ability to stretch or relax in this synthetic suture tape construct. Therefore, the suture tape construct should be used and tightened with the ankle in slight plantarflexion and/or a hemostat under the tape to serve as a check rein rather than a primary repair construct (Fig. 4). Alternatively, there have been good outcomes reported from a procedure involving biological augmentation using a periosteal flap to reinforce the Brostrom repair for patients with CLAI.71, 72, 73 Although there are no studies with head-to-head comparison for now, a matched-pair study comparing modified Brostrom-Gould procedure with or without periosteal flap augmentation (24 patients in each group) reported that the periosteal flap augmentation did not improve outcomes (AOFAS scores and recurrence rate) of the modified Brostrom-Gould procedure in the absence of risk factors.71 It is possible that this form of biological augmentation may improve the quality of repair via scarring and thickening of the repaired structure although the stability of this repaired structure is questionable.
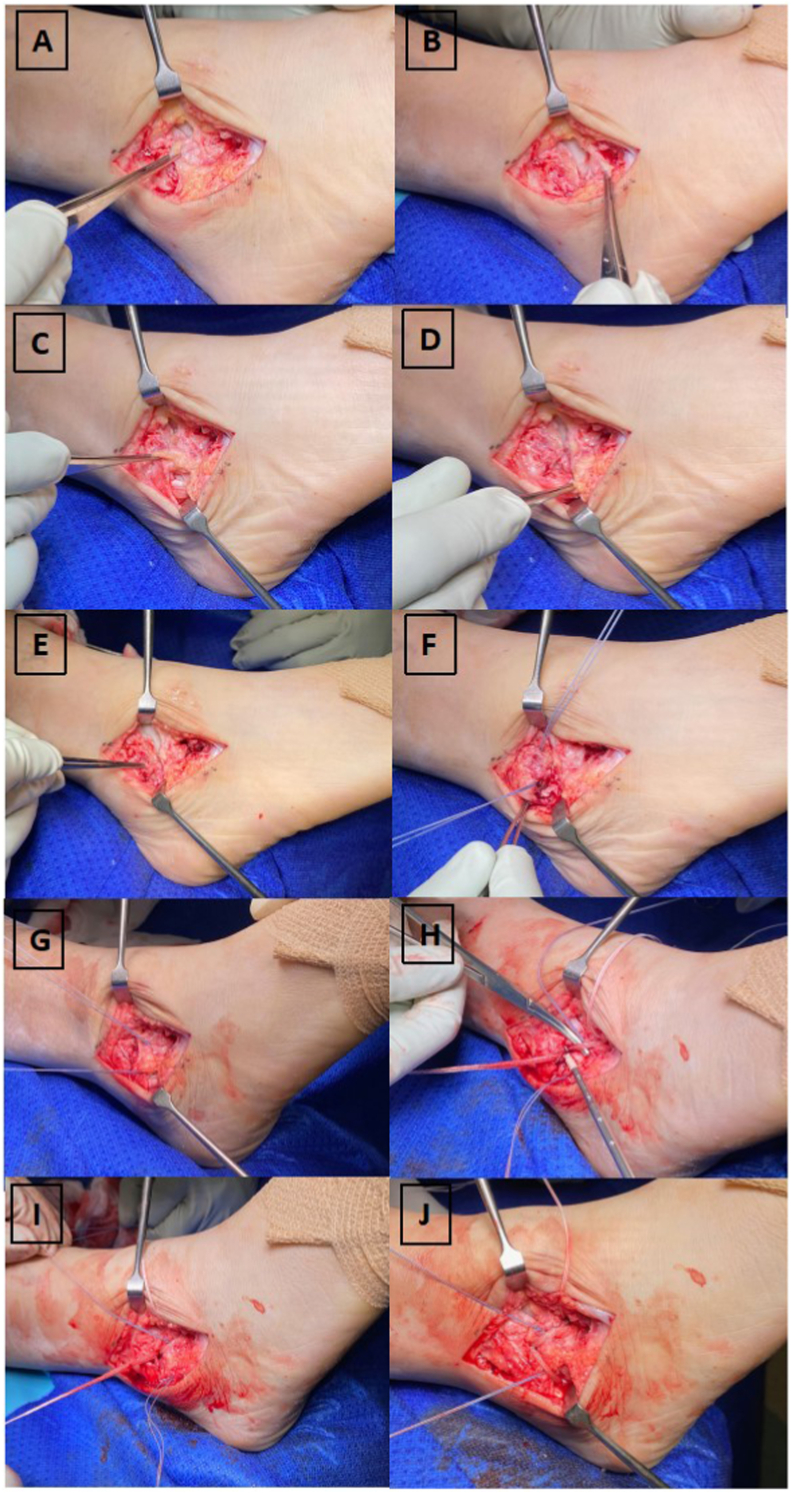
Fig. 4.
4A and 4B depict the ATFL ligament and its insertion on the fibula footprint while 4C and 4D demonstrate the CFL ligament and its insertion on the fibula footprint which is inferior to the ATFL while it runs deep to the peroneal tendons inserting to the calcaneus. 4E shows the location of the obscure tubercle which is an important landmark differentiating the insertion of ATFL and CFL. 4F illustrates the insertion of suture anchors at the ATFL and CFL footprint respectively where ATFL is superior to the obscure tubercle while CFL is inferior to it. 4G shows the modified Brostrom-Gould repair where both ATFL and CFL were shortened and repaired to the fibula footprints using suture anchors. 4H demonstrates the use of a synthetic suture tape for augmentation over the ATFL repair highlighting the hemostat under the suture tape to prevent overtightening (check rein) during the final tightening of the suture tape construct. 4I and 4J depicts the extension of the suture tape augmentation for the CFL repair as well. One should take note that the suture tape inserts at the obscure tubercle on the fibula in between both the primary ATFL and CFL repair footprint.
Nonanatomic procedure was first popularized by Watson-Jones in 1952 where the entire peroneus brevis tendon was detached proximally while preserving the distal insertion to the base of the 5th metatarsal and passed through the posterior fibula to anterior fibula at the ATFL footprint followed by tenodesis to the lateral talar neck.74 Following that, the Evans procedure which was technically easier was introduced where the peroneus brevis tendon was resected proximally but passed through from the anterior fibula footprint to the posterior fibula instead to replicate a lateral restraint to an inversion injury.75 Notably, these two techniques were not anatomical as the rerouted peroneus brevis tendon does not restore the native ATFL and CFL restraints on the ankle joint kinematics and the ability for dynamic eversion conferred by the peroneal brevis was obliterated. Chrisman and Snook subsequently described a new technique to recreate the ATFL and CFL by weaving a split peroneus brevis tendon through the distal fibula anteroposteriorly and tenodesing the stump to the lateral part of the calcaneus to replicate both the ATFL and CFL restraint while preserving part of the peroneus brevis dynamic eversion function.76 However, multiple biomechanical and clinical studies have continually showed that the ankle and subtalar joint physiologic kinematics are not restored but cause alterations in the range of motion specifically stiffness of the ankle and subtalar joints.36,66,77, 78, 79 In addition, Sammarco reported that wound complication rates were higher in nonanatomic procedures when compared to those undergoing anatomic direct repair procedures.80 A systematic review of the literature on nonanatomical and anatomical direct repair for CLAI with at least 10 years of follow-up on 801 ankles with a mean follow-up of 15.3 years demonstrated that restricted range of motion and secondary osteoarthritis was more frequent after nonanatomical repair when compared to anatomical direct repair.81 As a result of these concerning findings as well as the excellent outcomes from anatomic direct repair procedures, nonanatomic procedures have declined in their usage.
Anatomic reconstruction has been used more frequently now especially in CLAI patients with failed previous anatomical direct repair, generalized ligamentous laxity, attenuated remnant lateral ligaments due to repetitive injuries and high BMI.22,23,36,41,66,82, 83, 84, 85 Anatomic reconstruction can be performed with either autografts or allografts with promising results in recent years. Biomechanically, it has been shown by Clanton et al. that the anatomic reconstruction of the ATFL with semitendinosus allograft demonstrated similar strength and stiffness to the native ATFL ligament at time zero.86 Similarly, Prisk et al. showed that autograft peroneus brevis tendon used in anatomic reconstruction of the ATFL and CFL closely approximates the native ATFL tensile strength.87 Several clinical studies have also reported good outcomes after anatomic reconstruction using either autografts or allografts although these are mostly short-term outcomes.85,88,89 Nevertheless, although anatomic reconstruction is a viable option supported by both biomechanical and clinical data, graft options remain controversial. Both autografts and allografts have been shown to produce good results and no randomized controlled trials comparing autograft versus allograft currently exist. The standard advantage of autografts includes superior tissue quality from the host with no risks of disease transmission although the inherent disadvantage is donor site morbidity while allografts negate the risk of donor site morbidity with shorter surgical time and lesser postoperative pain despite some risk of infectious disease transmission, delayed biological healing and higher cost.36,66 In the same vein, Brambilla et al. have reported in a systematic review of 12 studies in which 357 patients had anatomic reconstruction performed for CLAI that due to the low numbers of studies and internal heterogeneity, it is not possible to determine whether allograft or autograft is a better graft option.89
Arthroscopic techniques for anatomic direct repair (Fig. 5) and anatomic reconstruction of the lateral ligaments for CLAI are emerging and increasingly popular.22,23,36,41,66 Open versus arthroscopic Brostrom procedure has been compared biomechanically by Giza et al. and the authors demonstrated no statistical difference in the strength or stiffness of the conventional open repair versus arthroscopic repair.90 Similarly, Drakos et al. compared the stability of the ankles with open versus arthroscopic Brostrom repair and reported no significant differences in terms of translation and total combined ankle motion during talar tilt testing.91 Lee et al. also performed a biomechanical study comparing 11 matched-pair cadaveric ankles and found that the working construct stiffness and load to failure were not significantly different between the open Brostrom-Gould procedure and all-inside arthroscopic Brostrom procedure.92 On top of sound biomechanical data, multiple studies have reported good outcomes of arthroscopic Brostrom procedure despite the plethora of technical variations.93, 94, 95 Even though there are several comparative studies between open versus arthroscopic anatomic direct repair in the current literature, these studies are mostly retrospective in nature with short-term outcomes.95 A recent systematic review and meta-analysis of open versus arthroscopic Brostrom surgery for CLAI reviewed 8 comparative studies where 7 studies were retrospective case-control studies while only 1 study was a prospective randomized controlled trial and found that while arthroscopic techniques may be technically more demanding, it was superior to open surgery in terms of AOFAS scores, VAS pain score and time to return to weight bearing.95 Notably, the operative time, clinical stability and complications were comparable but long-term outcomes were lacking for the arthroscopic cohort.95
Fig. 5.
5A to 5C illustrates the torn ATFL from the fibula with synovitis in the lateral gutter followed by debridement and preparation of the footprint. 5D shows the ATFL ligament held with grasping sutures. 5E depicts the drilling of the suture anchor drill hole. 5F and 5G demonstrates the introduction of the knotless suture anchor and insertion of the suture anchor into the drill hole while bringing the entire remnant ATFL to the fibula footprint closing the redundant lateral gutter space. 5H shows the probing of the final repair construct and its stability.
Likewise, arthroscopic anatomic reconstruction of the lateral ligament was first described by Guillo et al.96 in 2014 and the authors reported the moderate term outcome review at a mean of 48.7 ± 19 months demonstrating improvement in functional outcome scores that are comparable with other arthroscopic techniques in 2021.85 Following that, the percutaneous technique (Perc-AntiRoLL) was introduced.97 Recently, a newer hybrid technique combining the advantages of both Perc-AntiRoLL and arthroscopic technique was proposed.98 It was designed to replace the highly demanding technical requirements for CFL reconstruction using subtalar arthroscopy instead with the Perc-AntiRoLL steps to create the calcaneal tunnel under fluoroscopic guidance.98 Although several short to moderate-termlong-term outcomes for arthroscopic anatomic reconstruction of the lateral ligaments have yielded good outcomes, more clinical studies are needed to establish the long term outcomes as well as whether arthroscopic techniques are indeed reproducible since it is quite technically demanding.36,66,85
4.3. Impact of chronic lateral ankle instability
One of the concerning impacts from CLAI if left untreated is the development of osteochondral lesions of the talus and subsequently PTAO due to altered ankle joint biomechanics and repetitive injury to the cartilage.1,5,17 Recently, Tavana et al. evaluated in vivo ankle joint kinematics and contact strains using non-invasive digital volume correlation and MRI images which showed normal ankle bones translate independently from each other and these movements produce compressive, peak tensile and shear strains that were localized (87.5%) at the medial and lateral zones of the talar dome which could suggest anatomical predisposition of osteochondral lesions in these regions particularly in the presence of ankle instability.99 Furthermore, an in vivo kinematic study of the tibiotalar joints in CLAI patients demonstrated increased internal rotation, anterior translation, and superior translation of the talus in the joint.100 Likewise, Bischof et al. reported that in vivo peak cartilage contact strains are increased at the anteromedial ankle joint with significant medial translation and anterior translation at 100% body weight in patients with CLAI.101 Thereafter, Wainright and colleagues showed in their in-vivo kinematic study of the ankle joints in CLAI patients’ pre- and post-repair using modified Broström-Gould technique that there was statistically significant restoration of the abnormal ankle joint motion to a status almost similar to the uninjured ankle further promoting the importance of restoring mechanical stability to an unstable ankle.102
Clinically, intra-articular cartilage injuries such as chondral lesions were found in 89% of acute ankle sprains while those with chronic ankle sprains had a higher percentage of concomitant chondral lesions at 95%.103 Correspondingly, Takao et al. reported that 40.3% of 72 patients had osteochondral lesions after an arthroscopic assessment for residual ankle pain following the initial ankle sprains.104 Additionally, May et al. reported that 32% of 41 patients had concomitant OLT diagnosed during lateral ligament reconstruction for CLAI.105 Interestingly, Hong and Calder reported that there were only 6.8% of patients with OLT compared to the current literature ranging from 24% to 55% in their series of 147 elite athletes with early lateral ligament repair for grade III acute lateral ligament injuries.60 The authors posit that this notable difference is because current literature reported OLT in patients with CLAI while their cohort of patients had acute lateral ligament injury.60 They also proposed that early surgical stabilization for Grade III lateral ankle stability can potentially confer a stable mechanical environment for the cartilage from repetitive injury due to chronic instability as their series on early restoration of ankle stability resulted in a reinjury rate of 2%.60 Furthermore, Gribble et al. have suggested that the true prevalence of cartilage damage after ankle sprains may be underestimated as it was only reported in the literature for patients who were surgically treated.5 Therefore, it is possible that the development of cartilage injuries after ankle sprains can occur from the lack of early and appropriate clinical assessment and treatment.1,5,12,13,17,18,60,103
5. Summary
CLAI arises most commonly from an initial acute ankle sprain which is the single most common risk factor followed by repetitive trauma causing injuries to the already damaged stabilizing structures resulting in incompetency of the lateral ligament complex both mechanically and functionally within the spectrum of disease. Clinically, the anterior drawer and talar tilt test can demonstrate the presence of a mechanically unstable ankle while the anterolateral drawer test may possibly detect the loss of internal rotation restraint due to the ruptured superior fascicle of the ATFL. Weightbearing radiographs and MRI are the two main imaging modalities in the evaluation of CLAI. Nonsurgical treatment should always be instituted to improve neuromuscular strength, balancing and proprioception. After a period of appropriate nonsurgical therapy for 3–6 months, surgical options such as anatomic direct repair is the gold standard with reliable long-term outcomes. Nonanatomic procedures are no longer favourable as it does not restore the anatomic motion and kinematics of the hindfoot. Reconstruction of the lateral ligaments using autografts or allografts has shown promising results in certain cohorts of patients although the decision for use of autograft or allograft is still contentious. Arthroscopic techniques for anatomic direct repair and reconstruction are gaining popularity with good to excellent outcomes in the short to medium terms although long-term results are still lacking. With the significant negative impact of CLAI on the physical function, QoL and health economic burden, interventions such as early bracing, proprioceptive and neuromuscular training are very useful in preventing the recurrence of ankle sprains resulting in the development of CLAI. Additionally, there is a role for early surgical intervention in elite athletes in the acute phase to reduce downtime from the failure of nonsurgical treatment coupled with a more predictable time to return to sports. Therefore, early interventions following a lateral ankle sprain are paramount to prevent CLAI which potentially reduces the risk of repetitive trauma to the ankle joint leading to osteochondral lesions and postraumatic osteoarthritis.
Funding
There is no funding for this study.
Authors’ contribution
CCH, KJT, JC: Conceptualization, Methodology, Software. CCH: Data curation, Writing- Original draft preparation. CCH: Visualization, Investigation. CCH, KJT, JC: Supervision. CCH: Software, Validation. CCH, KJT, JC: Writing- Reviewing and Editing.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: James Calder reports a relationship with Arthrex that includes: speaking and lecture fees.
References
- 1.Herzog M.M., Kerr Z.Y., Marshall S.W., Wikstrom E.A. Epidemiology of ankle sprains and chronic ankle instability. J Athl Train. 2019 Jun;54(6):603–610. doi: 10.4085/1062-6050-447-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waterman B.R., Owens B.D., Davey S., Zacchilli M.A., Belmont P.J., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010 Oct 6;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 3.Cooke M.W., Lamb S.E., Marsh J., Dale J. A survey of current consultant practice of treatment of severe ankle sprains in emergency departments in the United Kingdom. Emerg Med J. 2003 Nov;20(6):505–507. doi: 10.1136/emj.20.6.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lamb S.E., Marsh J.L., Hutton J.L., Nakash R., Cooke M.W. Collaborative Ankle Support Trial (CAST Group). mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009 Feb 14;373(9663):575–581. doi: 10.1016/S0140-6736(09)60206-3. [DOI] [PubMed] [Google Scholar]
- 5.Gribble P.A., Bleakley C.M., Caulfield B.M., et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016 Dec;50(24):1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 6.Hunt K.J., Fuld R.S., III, Sutphin B.S., Periera H., D'Hooghe P. Return to sport following lateral ankle ligament repair is under-reported: a systematic review. J ISAKOS. 2017;2:234–240. [Google Scholar]
- 7.D'Hooghe P., Cruz F., Alkhelaifi K. Return to play after a lateral ligament ankle sprain. Curr Rev Musculoskelet Med. 2020 Jun;13(3):281–288. doi: 10.1007/s12178-020-09631-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boardman D.L., Liu S.H. Contribution of the anterolateral joint capsule to the mechanical stability of the ankle. Clin Orthop Relat Res. 1997 Aug;(341):224–232. [PubMed] [Google Scholar]
- 9.Waterman B.R., Belmont P.J., Jr., Cameron K.L., Deberardino T.M., Owens B.D. Epidemiology of ankle sprain at the United States military academy. Am J Sports Med. 2010 Apr;38(4):797–803. doi: 10.1177/0363546509350757. [DOI] [PubMed] [Google Scholar]
- 10.Roos K.G., Kerr Z.Y., Mauntel T.C., Djoko A., Dompier T.P., Wikstrom E.A. The epidemiology of lateral ligament complex ankle sprains in National Collegiate athletic association sports. Am J Sports Med. 2017 Jan;45(1):201–209. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 11.Waldén M., Hägglund M., Ekstrand J. Time-trends and circumstances surrounding ankle injuries in men's professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013 Aug;47(12):748–753. doi: 10.1136/bjsports-2013-092223. [DOI] [PubMed] [Google Scholar]
- 12.van Dijk C.N., Vuurberg G. There is no such thing as a simple ankle sprain: clinical commentary on the 2016 International Ankle Consortium position statement. Br J Sports Med. 2017 Mar;51(6):485–486. doi: 10.1136/bjsports-2016-096733. [DOI] [PubMed] [Google Scholar]
- 13.Kerkhoffs G.M., Kennedy J.G., Calder J.D., Karlsson J. There is no simple lateral ankle sprain. Knee Surg Sports Traumatol Arthrosc. 2016 Apr;24(4):941–943. doi: 10.1007/s00167-016-4043-z. [DOI] [PubMed] [Google Scholar]
- 14.Gerber J.P., Williams G.N., Scoville C.R., Arciero R.A., Taylor D.C. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998 Oct;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 15.Anandacoomarasamy A., Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005 Mar;39(3):e14. doi: 10.1136/bjsm.2004.011676. ; discussion e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konradsen L., Bech L., Ehrenbjerg M., Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002 Jun;12(3):129–135. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 17.Hong C.C., Calder J. The burden of the "simple ankle sprains": a review of the epidemiology and long-term impact. Foot Ankle Clin. 2023 Jun;28(2):187–200. doi: 10.1016/j.fcl.2022.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Doherty C., Bleakley C., Hertel J., Caulfield B., Ryan J., Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016 Apr;44(4):995–1003. doi: 10.1177/0363546516628870. [DOI] [PubMed] [Google Scholar]
- 19.van Rijn R.M., van Os A.G., Bernsen R.M., Luijsterburg P.A., Koes B.W., Bierma-Zeinstra S.M. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008 Apr;121(4):324–331.e6. doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 20.Lin C.I., Houtenbos S., Lu Y.H., Mayer F., Wippert P.M. The epidemiology of chronic ankle instability with perceived ankle instability- a systematic review. J Foot Ankle Res. 2021 May 28;14(1):41. doi: 10.1186/s13047-021-00480-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hertel J., Corbett R.O. An updated model of chronic ankle instability. J Athl Train. 2019 Jun;54(6):572–588. doi: 10.4085/1062-6050-344-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guillo S., Bauer T., Lee J.W., et al. Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99(8 Suppl):S411–S419. doi: 10.1016/j.otsr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Hong C.C.T.K. Concepts of ankle instability: a review. OA Sports Med. 2014;2(1):3. [Google Scholar]
- 24.Freeman M.A. Treatment of ruptures of the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):661–668. [PubMed] [Google Scholar]
- 25.Freeman M.A. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669–677. [PubMed] [Google Scholar]
- 26.Freeman M.A., Dean M.R., Hanham I.W. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 27.Tropp H., Ekstrand J., Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12(3):185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- 28.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 29.Hiller C.E., Kilbreath S.L., Refshauge K.M. Chronic ankle instability: evolution of the model. J Athl Train. 2011 Mar-Apr;46(2):133–141. doi: 10.4085/1062-6050-46.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takao M., Innami K., Matsushita T., Uchio Y., Ochi M. Arthroscopic and magnetic resonance image appearance and reconstruction of the anterior talofibular ligament in cases of apparent functional ankle instability. Am J Sports Med. 2008 Aug;36(8):1542–1547. doi: 10.1177/0363546508315537. [DOI] [PubMed] [Google Scholar]
- 31.Vega J., Peña F., Golanó P. Minor or occult ankle instability as a cause of anterolateral pain after ankle sprain. Knee Surg Sports Traumatol Arthrosc. 2016 Apr;24(4):1116–1123. doi: 10.1007/s00167-014-3454-y. [DOI] [PubMed] [Google Scholar]
- 32.Vega J., Malagelada F., Dalmau-Pastor M. Ankle microinstability: arthroscopic findings reveal four types of lesion to the anterior talofibular ligament's superior fascicle. Knee Surg Sports Traumatol Arthrosc. 2021 Apr;29(4):1294–1303. doi: 10.1007/s00167-020-06089-z. [DOI] [PubMed] [Google Scholar]
- 33.Vega J., Malagelada F., Manzanares Céspedes M.C., Dalmau-Pastor M. The lateral fibulotalocalcaneal ligament complex: an ankle stabilizing isometric structure. Knee Surg Sports Traumatol Arthrosc. 2020 Jan;28(1):8–17. doi: 10.1007/s00167-018-5188-8. [DOI] [PubMed] [Google Scholar]
- 34.Dalmau-Pastor M., El-Daou H., Stephen J.M., Vega J., Malagelada F., Calder J. Clinical relevance and function of anterior talofibular ligament superior and inferior fascicles: a robotic study. Am J Sports Med. 2023 Jul;51(8):2169–2175. doi: 10.1177/03635465231172196. [DOI] [PubMed] [Google Scholar]
- 35.Yoshimoto K., Noguchi M., Maruki H., Tominaga A., Okazaki K. Hindfoot alignment and ankle stability following arthroscopic lateral ankle ligament repair. Foot Ankle Int. 2023 Jun 30 doi: 10.1177/10711007231181123. [DOI] [PubMed] [Google Scholar]
- 36.Chang S.H., Morris B.L., Saengsin J., et al. Diagnosis and treatment of chronic lateral ankle instability: review of our biomechanical evidence. J Am Acad Orthop Surg. 2021 Jan 1;29(1):3–16. doi: 10.5435/JAAOS-D-20-00145. [DOI] [PubMed] [Google Scholar]
- 37.Bahr R., Pena F., Shine J., et al. Mechanics of the anterior drawer and talar tilt tests. A cadaveric study of lateral ligament injuries of the ankle. Acta Orthop Scand. 1997 Oct;68(5):435–441. doi: 10.3109/17453679708996258. [DOI] [PubMed] [Google Scholar]
- 38.Phisitkul P., Chaichankul C., Sripongsai R., Prasitdamrong I., Tengtrakulcharoen P., Suarchawaratana S. Accuracy of anterolateral drawer test in lateral ankle instability: a cadaveric study. Foot Ankle Int. 2009 Jul;30(7):690–695. doi: 10.3113/FAI.2009.0690. [DOI] [PubMed] [Google Scholar]
- 39.Vaseenon T., Gao Y., Phisitkul P. Comparison of two manual tests for ankle laxity due to rupture of the lateral ankle ligaments. Iowa Orthop J. 2012;32:9–16. [PMC free article] [PubMed] [Google Scholar]
- 40.Kamiya T., Kura H., Suzuki D., Uchiyama E., Fujimiya M., Yamashita T. Mechanical stability of the subtalar joint after lateral ligament sectioning and ankle brace application: a biomechanical experimental study. Am J Sports Med. 2009 Dec;37(12):2451–2458. doi: 10.1177/0363546509339578. [DOI] [PubMed] [Google Scholar]
- 41.Michels F., Pereira H., Calder J., et al. Searching for consensus in the approach to patients with chronic lateral ankle instability: ask the expert. Knee Surg Sports Traumatol Arthrosc. 2018 Jul;26(7):2095–2102. doi: 10.1007/s00167-017-4556-0. [DOI] [PubMed] [Google Scholar]
- 42.Hoffman E., Paller D., Koruprolu S., et al. Accuracy of plain radiographs versus 3D analysis of ankle stress test. Foot Ankle Int. 2011 Oct;32(10):994–999. doi: 10.3113/FAI.2011.0994. PMID: 22224329. [DOI] [PubMed] [Google Scholar]
- 43.Gribble P.A. Evaluating and differentiating ankle instability. J Athl Train. 2019 Jun;54(6):617–627. doi: 10.4085/1062-6050-484-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jung H.G., Kim N.R., Kim T.H., Eom J.S., Lee D.O. Magnetic resonance imaging and stress radiography in chronic lateral ankle instability. Foot Ankle Int. 2017 Jun;38(6):621–626. doi: 10.1177/1071100717693207. [DOI] [PubMed] [Google Scholar]
- 45.Hong C.C., Lee J.C., Tsuchida A., et al. Individual fascicles of the ankle lateral ligaments and the lateral fibulotalocalcaneal ligament complex can be identified on 3D volumetric MRI. Knee Surg Sports Traumatol Arthrosc. 2023 Jun;31(6):2192–2198. doi: 10.1007/s00167-022-07275-x. [DOI] [PubMed] [Google Scholar]
- 46.Khor Y.P., Tan K.J. The anatomic pattern of injuries in acute inversion ankle sprains: a magnetic resonance imaging study. Orthop J Sports Med. 2013 Dec 20;1(7) doi: 10.1177/2325967113517078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frost S.C., Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999 Jan;9(1):40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 48.Verhagen E., van der Beek A., Twisk J., Bouter L., Bahr R., van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004 Sep;32(6):1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 49.Wright C.J., Linens S.W., Cain M.S. A randomized controlled trial comparing rehabilitation efficacy in chronic ankle instability. J Sport Rehabil. 2017 Jul;26(4):238–249. doi: 10.1123/jsr.2015-0189. [DOI] [PubMed] [Google Scholar]
- 50.Rivera M.J., Winkelmann Z.K., Powden C.J., Games K.E. Proprioceptive training for the prevention of ankle sprains: an evidence-based review. J Athl Train. 2017 Nov;52(11):1065–1067. doi: 10.4085/1062-6050-52.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chan L.Y.T., Sim Y.T.N., Gan F.K., Bin Abd Razak H.R. Effect of chronic ankle instability on lower extremity kinematics, dynamic postural stability, and muscle activity during unilateral jump-landing tasks: a systematic review and meta-analysis. Phys Ther Sport. 2022 May;55:176–188. doi: 10.1016/j.ptsp.2022.04.005. [DOI] [PubMed] [Google Scholar]
- 52.Doherty C., Bleakley C., Delahunt E., Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017 Jan;51(2):113–125. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 53.Broström L. Sprained ankles. VI. Surgical treatment of "chronic" ligament ruptures. Acta Chir Scand. 1966 Nov;132(5):551–565. [PubMed] [Google Scholar]
- 54.Gould N., Seligson D., Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980 Sep;1(2):84–89. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- 55.Karlsson J., Bergsten T., Lansinger O., Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988 Apr;70(4):581–588. PMID: 3356725. [PubMed] [Google Scholar]
- 56.Hunt K.J., Pereira H., Kelley J., et al. The role of calcaneofibular ligament injury in ankle instability: implications for surgical management. Am J Sports Med. 2019 Feb;47(2):431–437. doi: 10.1177/0363546518815160. [DOI] [PubMed] [Google Scholar]
- 57.Cordier G., Nunes G.A., Vega J., Roure F., Dalmau-Pastor M. Connecting fibers between ATFL's inferior fascicle and CFL transmit tension between both ligaments. Knee Surg Sports Traumatol Arthrosc. 2021 Aug;29(8):2511–2516. doi: 10.1007/s00167-021-06496-w. [DOI] [PubMed] [Google Scholar]
- 58.Lee K.T., Park Y.U., Kim J.S., Kim J.B., Kim K.C., Kang S.K. Long-term results after modified Brostrom procedure without calcaneofibular ligament reconstruction. Foot Ankle Int. 2011 Feb;32(2):153–157. doi: 10.3113/FAI.2011.0153. [DOI] [PubMed] [Google Scholar]
- 59.Maffulli N., Del Buono A., Maffulli G.D., et al. Isolated anterior talofibular ligament Broström repair for chronic lateral ankle instability: 9-year follow-up. Am J Sports Med. 2013 Apr;41(4):858–864. doi: 10.1177/0363546512474967. [DOI] [PubMed] [Google Scholar]
- 60.Hong C.C., Calder J. Ability to return to sports after early lateral ligament repair of the ankle in 147 elite athletes. Knee Surg Sports Traumatol Arthrosc. 2023 Oct;31(10):4519–4525. doi: 10.1007/s00167-022-07270-2. [DOI] [PubMed] [Google Scholar]
- 61.White W.J., McCollum G.A., Calder J.D. Return to sport following acute lateral ligament repair of the ankle in professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016 Apr;24(4):1124–1129. doi: 10.1007/s00167-015-3815-1. [DOI] [PubMed] [Google Scholar]
- 62.Aydogan U., Glisson R.R., Nunley J.A. Extensor retinaculum augmentation reinforces anterior talofibular ligament repair. Clin Orthop Relat Res. 2006 Jan;442:210–215. doi: 10.1097/01.blo.0000183737.43245.26. [DOI] [PubMed] [Google Scholar]
- 63.Behrens S.B., Drakos M., Lee B.J., et al. Biomechanical analysis of Brostrom versus Brostrom-Gould lateral ankle instability repairs. Foot Ankle Int. 2013 Apr;34(4):587–592. doi: 10.1177/1071100713477622. Epub 2013 Feb 7. PMID: 23391625. [DOI] [PubMed] [Google Scholar]
- 64.Jeong B.O., Kim M.S., Song W.J., SooHoo N.F. Feasibility and outcome of inferior extensor retinaculum reinforcement in modified Broström procedures. Foot Ankle Int. 2014 Nov;35(11):1137–1142. doi: 10.1177/1071100714543645. [DOI] [PubMed] [Google Scholar]
- 65.Lee S.H., Cho H.G., Yang J.H. Additional inferior extensor retinaculum augmentation after all-inside arthroscopic anterior talofibular ligament repair for chronic ankle instability is not necessary. Am J Sports Med. 2021 Jun;49(7):1721–1731. doi: 10.1177/03635465211008097. [DOI] [PubMed] [Google Scholar]
- 66.Yasui Y., Shimozono Y., Kennedy J.G. Surgical procedures for chronic lateral ankle instability. J Am Acad Orthop Surg. 2018 Apr 1;26(7):223–230. doi: 10.5435/JAAOS-D-16-00623. [DOI] [PubMed] [Google Scholar]
- 67.Wittig U., Hohenberger G., Ornig M., et al. Improved outcome and earlier return to activity after suture tape augmentation versus Broström repair for chronic lateral ankle instability? A systematic review. Arthroscopy. 2022 Feb;38(2):597–608. doi: 10.1016/j.arthro.2021.06.028. [DOI] [PubMed] [Google Scholar]
- 68.Viens N.A., Wijdicks C.A., Campbell K.J., Laprade R.F., Clanton T.O. Anterior talofibular ligament ruptures, part 1: biomechanical comparison of augmented Broström repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014 Feb;42(2):405–411. doi: 10.1177/0363546513510141. [DOI] [PubMed] [Google Scholar]
- 69.Schuh R., Benca E., Willegger M., et al. Comparison of Broström technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2016 Apr;24(4):1101–1107. doi: 10.1007/s00167-015-3631-7. [DOI] [PubMed] [Google Scholar]
- 70.Martin K.D., Andres N.N., Robinson W.H. Suture tape augmented Broström procedure and early accelerated rehabilitation. Foot Ankle Int. 2021 Feb;42(2):145–150. doi: 10.1177/1071100720959015. [DOI] [PubMed] [Google Scholar]
- 71.Tay K.S., Chew C.P., Lie D.T.T. Effect of periosteal flap augmentation on outcomes of modified Broström-Gould procedure for chronic lateral ankle instability. Foot Ankle Orthop. 2020 Jul 30;5(3) doi: 10.1177/2473011420934735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Choi H.J., Kim D.W., Park J.S. Modified Broström procedure using distal fibular periosteal flap augmentation vs anatomic reconstruction using a free tendon allograft in patients who are not candidates for standard repair. Foot Ankle Int. 2017 Nov;38(11):1207–1214. doi: 10.1177/1071100717726303. [DOI] [PubMed] [Google Scholar]
- 73.Kirk K.L., Schon L.C. Technique tip: periosteal flap augmentation of the Brostrom lateral ankle reconstruction. Foot Ankle Int. 2008 Feb;29(2):254–255. doi: 10.3113/FAI.2008.0254. [DOI] [PubMed] [Google Scholar]
- 74.Watson-Jones R. Recurrent forward dislocation of the ankle joint. J Bone Joint Surg Br. 1952;134:519. [Google Scholar]
- 75.Evans D.L. Recurrent instability of the ankle; a method of surgical treatment. Proc Roy Soc Med. 1953 May;46(5):343–344. doi: 10.1177/003591575304600507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chrisman O.D., Snook G.A. Reconstruction of lateral ligament tears of the ankle. an experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am. 1969 Jul;51(5):904–912. [PubMed] [Google Scholar]
- 77.Bahr R., Pena F., Shine J., Lew W.D., Tyrdal S., Engebretsen L. Biomechanics of ankle ligament reconstruction. An in vitro comparison of the Broström repair, Watson-Jones reconstruction, and a new anatomic reconstruction technique. Am J Sports Med. 1997 Jul-Aug;25(4):424–432. doi: 10.1177/036354659702500402. [DOI] [PubMed] [Google Scholar]
- 78.Hollis J.M., Blasier R.D., Flahiff C.M., Hofmann O.E. Biomechanical comparison of reconstruction techniques in simulated lateral ankle ligament injury. Am J Sports Med. 1995 Nov-Dec;23(6):678–682. doi: 10.1177/036354659502300607. [DOI] [PubMed] [Google Scholar]
- 79.Karlsson J., Bergsten T., Lansinger O., Peterson L. Lateral instability of the ankle treated by the Evans procedure. A long-term clinical and radiological follow-up. J Bone Joint Surg Br. 1988 May;70(3):476–480. doi: 10.1302/0301-620X.70B3.3372575. [DOI] [PubMed] [Google Scholar]
- 80.Sammarco V.J. Complications of lateral ankle ligament reconstruction. Clin Orthop Relat Res. 2001 Oct;(391):123–132. doi: 10.1097/00003086-200110000-00013. [DOI] [PubMed] [Google Scholar]
- 81.Noailles T., Lopes R., Padiolleau G., Gouin F., Brilhault J. Non-anatomical or direct anatomical repair of chronic lateral instability of the ankle: a systematic review of the literature after at least 10 years of follow-up. Foot Ankle Surg. 2018 Apr;24(2):80–85. doi: 10.1016/j.fas.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 82.Dierckman B.D., Ferkel R.D. Anatomic reconstruction with a semitendinosus allograft for chronic lateral ankle instability. Am J Sports Med. 2015 Aug;43(8):1941–1950. doi: 10.1177/0363546515593942. [DOI] [PubMed] [Google Scholar]
- 83.Karlsson J., Bergsten T., Lansinger O., Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988 Apr;70(4):581–588. [PubMed] [Google Scholar]
- 84.Takao M., Glazebrook M., Stone J., Guillo S. Ankle arthroscopic reconstruction of lateral ligaments (ankle anti-ROLL) Arthrosc Tech. 2015 Oct 23;4(5):e595–e600. doi: 10.1016/j.eats.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guillo S., Odagiri H., van Rooij F., Bauer T., Hardy A. All-inside endoscopic anatomic reconstruction leads to satisfactory functional outcomes in patients with chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2021 Apr;29(4):1318–1324. doi: 10.1007/s00167-020-06130-1. [DOI] [PubMed] [Google Scholar]
- 86.Clanton T.O., Viens N.A., Campbell K.J., Laprade R.F., Wijdicks C.A. Anterior talofibular ligament ruptures, part 2: biomechanical comparison of anterior talofibular ligament reconstruction using semitendinosus allografts with the intact ligament. Am J Sports Med. 2014 Feb;42(2):412–416. doi: 10.1177/0363546513509963. [DOI] [PubMed] [Google Scholar]
- 87.Prisk V.R., Imhauser C.W., O'Loughlin P.F., Kennedy J.G. Lateral ligament repair and reconstruction restore neither contact mechanics of the ankle joint nor motion patterns of the hindfoot. J Bone Joint Surg Am. 2010 Oct 20;92(14):2375–2386. doi: 10.2106/JBJS.I.00869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jung H.G., Shin M.H., Park J.T., Eom J.S., Lee D.O., Lee S.H. Anatomical reconstruction of lateral ankle ligaments using free tendon allografts and biotenodesis screws. Foot Ankle Int. 2015 Sep;36(9):1064–1071. doi: 10.1177/1071100715584848. [DOI] [PubMed] [Google Scholar]
- 89.Brambilla L., Bianchi A., Malerba F., Loppini M., Martinelli N. Lateral ankle ligament anatomic reconstruction for chronic ankle instability: allograft or autograft? A systematic review. Foot Ankle Surg. 2020 Jan;26(1):85–93. doi: 10.1016/j.fas.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 90.Giza E., Shin E.C., Wong S.E., et al. Arthroscopic suture anchor repair of the lateral ligament ankle complex: a cadaveric study. Am J Sports Med. 2013 Nov;41(11):2567–2572. doi: 10.1177/0363546513500639. Epub 2013 Aug 27. PMID: 23982396. [DOI] [PubMed] [Google Scholar]
- 91.Drakos M.C., Behrens S.B., Paller D., Murphy C., DiGiovanni C.W. Biomechanical comparison of an open vs arthroscopic approach for lateral ankle instability. Foot Ankle Int. 2014 Aug;35(8):809–815. doi: 10.1177/1071100714535765. [DOI] [PubMed] [Google Scholar]
- 92.Lee K.T., Kim E.S., Kim Y.H., Ryu J.S., Rhyu I.J., Lee Y.K. All-inside arthroscopic modified Broström operation for chronic ankle instability: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2016 Apr;24(4):1096–1100. doi: 10.1007/s00167-014-3159-2. [DOI] [PubMed] [Google Scholar]
- 93.Matsui K., Takao M., Miyamoto W., Matsushita T. Early recovery after arthroscopic repair compared to open repair of the anterior talofibular ligament for lateral instability of the ankle. Arch Orthop Trauma Surg. 2016 Jan;136(1):93–100. doi: 10.1007/s00402-015-2342-3. [DOI] [PubMed] [Google Scholar]
- 94.Matsui K., Burgesson B., Takao M., Stone J., Guillo S., Glazebrook M., ESSKA AFAS Ankle Instability Group Minimally invasive surgical treatment for chronic ankle instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016 Apr;24(4):1040–1048. doi: 10.1007/s00167-016-4041-1. [DOI] [PubMed] [Google Scholar]
- 95.Attia A.K., Taha T., Mahmoud K., Hunt K.J., Labib S.A., d'Hooghe P. Outcomes of open versus arthroscopic Broström surgery for chronic lateral ankle instability: a systematic review and meta-analysis of comparative studies. Orthop J Sports Med. 2021 Jul 21;9(7) doi: 10.1177/23259671211015207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014 Sep 22;3(5):e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Glazebrook M., Stone J., Matsui K., Guillo S., Takao M., ESSKA AFAS Ankle Instability Group Percutaneous ankle reconstruction of lateral ligaments (Perc-Anti RoLL) Foot Ankle Int. 2016 Jun;37(6):659–664. doi: 10.1177/1071100716633648. [DOI] [PubMed] [Google Scholar]
- 98.Iwashita K., Jujo Y., Inokuchi R., Glazebrook M., Stone J., Takao M. Hybrid ankle reconstruction of lateral ligaments. Arthrosc Tech. 2021 Feb 22;10(3):e931–e939. doi: 10.1016/j.eats.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tavana S., Clark J.N., Hong C.C., Newell N., Calder J.D., Hansen U. In vivo evaluation of ankle kinematics and tibiotalar joint contact strains using digital volume correlation and 3 T clinical MRI. Clin Biomech (Bristol, Avon) 2023 Jun 16;107 doi: 10.1016/j.clinbiomech.2023.106032. [DOI] [PubMed] [Google Scholar]
- 100.Caputo A.M., Lee J.Y., Spritzer C.E., et al. In vivo kinematics of the tibiotalar joint after lateral ankle instability. Am J Sports Med. 2009 Nov;37(11):2241–2248. doi: 10.1177/0363546509337578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bischof J.E., Spritzer C.E., Caputo A.M., et al. In vivo cartilage contact strains in patients with lateral ankle instability. J Biomech. 2010 Sep 17;43(13):2561–2566. doi: 10.1016/j.jbiomech.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wainright W.B., Spritzer C.E., Lee J.Y., et al. The effect of modified Broström-Gould repair for lateral ankle instability on in vivo tibiotalar kinematics. Am J Sports Med. 2012 Sep;40(9):2099–2104. doi: 10.1177/0363546512454840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Taga I., Shino K., Inoue M., Nakata K., Maeda A. Articular cartilage lesions in ankles with lateral ligament injury. An arthroscopic study. Am J Sports Med. 1993 Jan-Feb;21(1):120–126. doi: 10.1177/036354659302100120. ; discussion 126-7. [DOI] [PubMed] [Google Scholar]
- 104.Takao M., Uchio Y., Naito K., Fukazawa I., Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005 May;33(5):686–692. doi: 10.1177/0363546504270566. [DOI] [PubMed] [Google Scholar]
- 105.May N.R., Driscoll M., Nguyen S., Ferkel R.D. Analysis of return to play after modified Broström lateral ankle ligament reconstruction. Orthop J Sports Med. 2022 Feb 2;10(2) doi: 10.1177/23259671211068541. [DOI] [PMC free article] [PubMed] [Google Scholar]