Abstract
Objectives
To our best knowledge, no study in France has comprehensively investigated the prehospital history of patients admitted for severe cases of COVID-19. ‘Patients’ voice is an excellent means to capture data on primary care pathways.
We aimed to identify clusters of COVID-19 hospitalised patients with similar prehospital symptom sequences, and to test whether these clusters were associated with a higher risk of poor clinical outcomes.
Design
Cross-sectional online survey using life-event calendars.
Setting
All patients hospitalised for COVID-19 between September 2020 and May 2021 in the Infectious Disease Departments in Nice and in Marseilles in France.
Participants
312 patients responded to the survey.
Main outcome measures
From the day of symptom onset to the day of hospitalisation, we defined a symptom sequence as the time-ordered vector of the successive symptom grades (grade 1, grade 2, grade 3). State sequence analysis with optimal matching was used to identify clusters of patients with similar symptom sequences. Multivariate logistic regressions were performed to test whether these clusters were associated with admission to intensive care unit (ICU) and COVID-19 sequelae after hospitalisation.
Results
Three clusters of symptom sequences were identified among 312 complete prehospital pathways. A specific group of patients (29%) experienced extended symptoms of severe COVID-19, persisting for an average duration of 7.5 days before hospitalisation. This group had a significantly higher probability of being admitted to ICU (adjusted OR 2.01). They were less likely to know a loved one who was a healthcare worker, and more likely to have a lower level of education. Similarly, this group of patients, who were more likely to have previously visited the emergency room without exhibiting severe symptoms at that time, may have been inclined to postpone reassessment when their health worsened.
Their relatives played a decisive role in their hospitalisation.
Conclusion and relevance
This study highlights the negative impact of delayed hospitalisation on the health outcomes of French patients with severe COVID-19 symptoms during the first wave and underscores the influence of socioeconomic factors, such as lower education levels and limited connections to the medical field, on patients’ experiences.
Keywords: COVID-19, Patient Navigation, Primary Health Care
Key points.
Question We wanted to better understand whether direct recourse to the hospital system by COVID-19 patients with serious symptoms was because of the natural history of the disease (ie, sudden clinical deterioration) or because of delays in the system’s primary care pathway.
Findings A specific group of patients in France with severe symptoms of COVID-19 during the first wave of the pandemic experienced a delay before hospitalisation which was detrimental to their health. Family and friends played a crucial role in hospitalisation, while lower education levels and lack of familiarity with healthcare professionals resulted in delays. Similarly, this group of patients, who were more likely to have previously visited the emergency room without exhibiting severe symptoms at that time, may have been inclined to postpone reassessment when their health worsened.
Meaning The processual approach revealed the interconnectedness of life, medical and clinical events in care pathways, emphasising the significance of biology, personal history and social context.
Introduction
Over the last decade, analysing patient experience has been one of the pillars for assessing the quality of care pathways.1 A care pathway can be understood as the outcome of clinical and non-clinical events related to the natural history of the disease and to the ways in which the patient interprets symptoms and mobilises his/her use of the health system.2 Care pathways have rarely been approached as a process, that is to say a trajectory unfolding over time and structured by sequences of events.3–5 In order to comprehensively assess the effect of time on care pathways, it is important to take into account the order of event sequences and the amount of time that passes for each sequence.6 7
The fight against COVID-19 not only involves therapeutic advances but also improved clinical management of symptomatic patients. The latter depends on how patients orientate themselves in the care system and whether they choose to access care or not. A national French study showed that during the first wave of COVID-19, nearly 20% of COVID-19 patients were admitted to hospital after arriving in an emergency department (ED); 11% of these were immediately admitted to an intensive care unit (ICU).8 In another study, a cohort of 2111 adults hospitalised at the Infectious Diseases Department of the University Hospital of Nice (CHU hereafter) and its sister department in Marseille (IHU hereafter), 53% were referred to these departments after arrival at the respective ED and three-quarters of all those who died had been admitted to hospital after arriving in an ED, including those immediately admitted to an ICU.9
To improve primary (ie, prehospital) care management for COVID-19, with a view to improving disease prognosis, it is important to study patients’ primary care pathways, particularly those of patients admitted immediately to an ICU after consulting in an ED.10
This study is the first to use patients’ experiences to describe and interpret all the events structuring primary (ie, prehospital) care pathways in persons hospitalised (ie, consulting in an ED and then either discharged or transferred to a hospital department) for COVID-19 in France during the pandemic’s first wave. Studying patients’ experiences during the first wave was a relevant methodological choice, as changes in health authority guidelines empowered people to make health management decisions, by requesting them to identify signs of severity and indications for diagnostic tests at home, and more generally, to decide on whether to go to a hospital ED or not.
We implemented an innovative mixed-method approach comprising a life-events calendar combined with a sequence analysis with a view to better understanding primary care management of patients with COVID-19, by giving priority to clinical events, to the chronological sequence of these events, and to the way actors (ie, patients and doctors) interpreted and reacted to them. More specifically, the study’s objectives were to (a) describe outpatient pathways by characterising the natural course of the disease and understanding how certain variables act at key time points in a care trajectory (ie, how they trigger hospitalisation); (b) identify patterns/clusters of patients with similar outpatient pathways using a state sequence analysis (SSA); (c) test whether these patterns/clusters were associated with a higher risk of poor clinical outcomes in terms of both admission to an ICU during hospitalisation, and COVID-19 sequelae after release from hospital.
Methods
Design and study population
We performed a cross-sectional online survey between 17 May and 2 July 2022. It targeted patients hospitalised for COVID-19 between September 2020 and May 2021 in the IHU and CHU. All patients were eligible irrespective of their mode of entry to the hospitals (ie, via ED, immediate admission, etc). Patients who died before the start of the survey were excluded. Because we anticipated a relatively low response rate, we did not apply any sampling to our target population. A phone interview was also proposed to patients whose physical condition might have hampered their ability to respond to the online questionnaire.
Life-events calendar method
This article presents the quantitative phase of a mixed-methods research study comprising an exploratory qualitative phase and a quantitative phase. The qualitative phase aimed to identify all the possible types of primary (ie, prehospital) care pathways and different outpatient patient management strategies for persons hospitalised with diagnosed COVID-19 infection in France. It also aimed to test the suitability of using the life-events calendar tool to prepare the questionnaire used during the quantitative phase. A life-events calendar is a retrospective data collection tool which highlights the chronological order and proximity of clinical events and major transitions in care trajectories, making it possible to simultaneously analyse several aspects of the patient’s global care pathway (ie, clinical history, diagnostic pathway, care pathway, therapeutic pathway) (online supplemental material 1).11 12
fmch-2023-002447supp001.pdf (1.3MB, pdf)
All materials and database of this study are openly available online (recherche.data.gouv.fr).13
Sample size and response rate
A phone number was retrieved for 2608 (80.0%) of the 3259 eligible patients. The former were asked to provide their email address if they wished to participate. Of the 944 who provided a valid email address to receive the link to the online questionnaire, 312 answered the survey. As sex, age and site (Marseille/Nice) all had a significant impact on participation, we decided to weight the sample. The final weights were created using an iterative process (ranking ratio estimation) involving data (sex, age and site) collected on the eligible population.
Assessment of COVID-19 symptom timeline
Patients were asked about their daily COVID-19 symptom timeline from illness onset (ie, day of symptom onset) to the beginning of their hospitalisation for COVID-19. This timeline allowed us to register the type and number of symptoms reported each day as well as the sequence in which each new symptom appeared. Patients could report up to 17 different symptoms for each day. We then classified the symptoms into three grades representing the level of clinical severity, with symptoms being cumulative.
Grade 1 symptoms: fever (moderate or intense), cough, muscular pain, fatigue (moderate or intense), headache (moderate or intense), nausea (moderate or intense), diarrhoea, anosmia/ageusia
Grade 2 symptoms: grade 1 symptoms+breathing difficulty (moderate or intense), oxygen desaturation.
Grade 3 symptoms: grade 1 and 2 symptoms+confusion, loss of consciousness.
These three grades made it possible to distinguish between symptoms that required: (a) ambulatory (ie, non-hospital based) management (grade 1); (b) hospitalisation (ie, ED consultation and possible admission to hospital (excluding ICU) (grade 2) according to the French Higher Authority for Health criteria); (c) admission (whether immediate or not) to an ICU (grade 3, life-threatening emergencies).
For each patient, we defined a symptom sequence as the time-ordered vector of their successive symptom grades (‘grade 1’, ‘grade 2’, ‘grade 3’). Therefore, the length of each individual sequence was not the same for all patients as it depended on the number of days which elapsed from the day of symptom onset to the day of hospitalisation for COVID-19. If symptoms from different grades were declared for the same day (eg, symptoms from grades 2 and 3), the symptom of the highest grade was retained.
Assessment of covariates
In order to evaluate factors likely to be associated with symptom onset sequences, we collected sociodemographic (age, sex, occupation and education level) and clinical (number of comorbidities/medical history, obesity and smoking status) data. Patients were asked whether they had consulted a general practitioner (GP), day hospital (ie, outpatient clinic at the IHU/CHU) or an emergency care service before their hospitalisation for COVID-19. They were also asked about the treatment(s) they had been prescribed.
The survey also collected data on patients’ difficulties to see a doctor and/or receive treatment before their hospitalisation, whether they knew a loved one (ie, family member or friend) who was a healthcare worker, and the person who decided the patient had to be hospitalised (GP, emergency care service, family member, patient him/herself).
Ascertainment of clinical outcomes
As regards the clinical outcomes, patients were asked about the length of their hospital stay, ICU admission, follow-up care/rehabilitation/home oxygen treatment after release from hospital, and whether they still had COVID-19 sequelae at the time of the survey.
Statistical analysis
To characterise the clinical history typology (ie, clusters of patients with similar symptom sequences), we performed an SSA. An SSA is a non-parametric method used to analyse sequential data. Key aspects include sequencing (the order of distinct state occurrence), duration (the length of spell in a specific health state (ie, grades 1, 2 and 3 here)) and timing (the moment of transition from one state to another).14 15 The method aims to compare all individual sequences with each other to establish a dissimilarity matrix between sequences. A clustering method can then be applied on this matrix to identify clusters of individuals with typical sequences. We chose optimal matching (OM) as the method to assess dissimilarity between symptom sequences.14 16 17 OM measures dissimilarity as the weighted sum of the number of virtual editing operations (substitution, insertion and deletion) required to transform one individual’s sequence into another’s. For this analysis, a constant substitution cost of 2 and an insertion/deletion cost of 1.5 were chosen. These values allowed us to take into account the different dimensions (sequencing, timing, duration and spell duration). We also tested three different combinations of substitution and insertion/deletion costs (1/2, 2/1 and 2/3) to check the robustness of our results. For the clustering step, we used a hierarchical cluster analysis (HCA) applied to the dissimilarity matrix. To compare clustering solutions based on different quality measures, we used the Weighted Cluster18 library in R. The prevalence of each cluster and the relevance of the solutions were also considered. Once clusters were defined, chronograms (cross-sectional distribution of states) and sequence index plots (longitudinal order of states) were plotted to visualise the typical sequences of symptoms for each cluster.
Cluster characteristics were compared using the χ2 test. We also performed two multivariate logistic regressions to test whether the clusters of symptom sequences were associated with ICU admission and COVID-19 sequelae at the time of the survey. Both models were adjusted for the main risk factors associated with a poor clinical outcome19 (ie, age, gender, number of comorbidities/clinical history, obesity and smoking status). Models were also adjusted for socioeconomic factors (ie, education level).
All analyses involved two-sided p values, with statistical significance defined as a p value ≤0.05. Data preparation, sequence creation, descriptive statistics and regression analyses were conducted using SAS V.9.4 (SAS Institute, Cary, NC, USA). SSA and HCA were performed using the TraMineR20 and WeightedCluster18 libraries in R V.4.2.2.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
The study population included 312 patients (table 1) hospitalised for COVID-19. The average time from the day of symptom onset to the beginning of hospitalisation was 6.7±3.6 days (min=1, max=16). As regards the clinical outcomes, the average hospital stay was 10.8±12.8 days, 50.6% were admitted to an ICU, and 52.6% had follow-up or rehabilitation care after being released from hospital. Half (49.1%) declared sequelae at the time of the survey, physical sequelae being most frequent (40.6%) followed by neurological sequelae (30.8%).
Table 1.
Study population characteristics (n=312)
| n* | %† | |
| Sex | ||
| Female | 128 | 41.1 |
| Male | 184 | 58.9 |
| Age | ||
| Mean (SD) | 65.2 (13.8) | |
| 18–49 | 47 | 15.0 |
| 50–64 | 97 | 31.1 |
| 65–79 | 106 | 34.1 |
| >79 | 62 | 19.7 |
| Site | ||
| Marseille | 248 | 79.7 |
| Nice | 64 | 20.3 |
| Period | ||
| 2020 | 112 | 35.8 |
| 2021 | 200 | 64.2 |
| Education | ||
| <General certificate of secondary education | 49 | 15.6 |
| General certificate of secondary education | 59 | 18.9 |
| High school diploma | 52 | 16.7 |
| ≥Diploma of higher education | 152 | 48.7 |
| Number of comorbidities/medical history | ||
| None | 97 | 31.1 |
| One | 85 | 27.3 |
| Two | 44 | 14.2 |
| Three | 42 | 13.4 |
| More than three | 44 | 14.0 |
| Daily smoker | 10 | 3.2 |
| Obesity (body mass index≥30 kg/m²) | 80 | 25.6 |
| Live alone | 77 | 24.6 |
| Works/has worked as a healthcare worker | 63 | 20.1 |
| Knows someone in his/her close circle who is a healthcare worker | 164 | 52.6 |
| Time from symptom onset to hospitalisation (days)—mean(SD) | 6.7 (3.6) | |
| Clinical outcomes | ||
| Length of hospital stay (days) (nmiss=1) | ||
| Mean (SD) | 10.8 (12.8) | |
| Transfer to intensive care unit | 158 | 50.6 |
| Follow-up/rehabilitation care after hospitalisation | 164 | 52.6 |
| Home oxygen treatment after hospitalisation | 176 | 56.6 |
| Still has sequelae of COVID-19 at the time of the survey | 153 | 49.1 |
| Physical sequelae | 126 | 40.6 |
| Neurological sequelae | 96 | 30.8 |
| Psychological sequelae | 57 | 18.2 |
| Sleep disorders sequelae | 51 | 16.5 |
*Weighted frequency otherwise stated; the sum may not add to 312 due to rounding.
†Weighted column percentages otherwise stated; the sum may not add to 100% due to rounding.
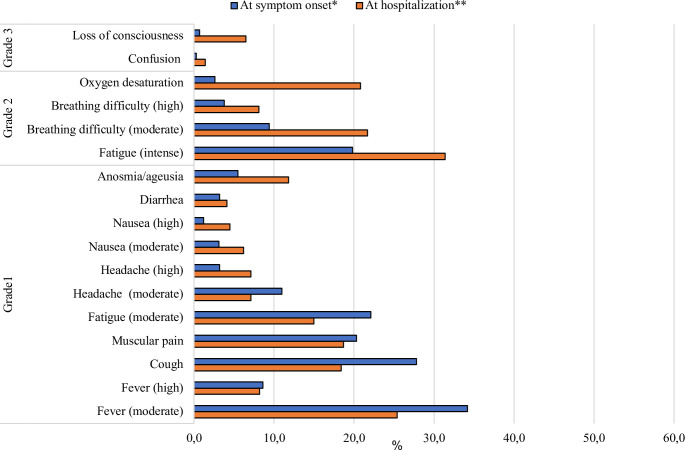
In terms of symptom onset, moderate fever was the most frequent symptom reported (34.2%) (figure 1), followed by a cough (27.8%), moderate fatigue (22.1%), muscular pain (20.3%) and intense fatigue (19.8%). Putting this in terms of grades, 88.1%, 28.6% and 1.0% reported at least one grade 1, grade 2 or grade 3 symptom, respectively. At the beginning of hospitalisation, intense fatigue (31.4%), moderate fever (25.4%), moderate breathing difficulties (21.7%) and oxygen desaturation (20.8%) were the most frequent symptoms. Putting this in terms of grades, 52.5%, 49.0% and 7.8% reported at least one grade 1, grade 2 or grade 3 symptom, respectively.
Figure 1.
Declared symptom(s) from symptom onset to hospitalisation (n=312).*First symptom(s) declared by the patient. **Last symptom(s) declared by the patient prior to hospitalization.
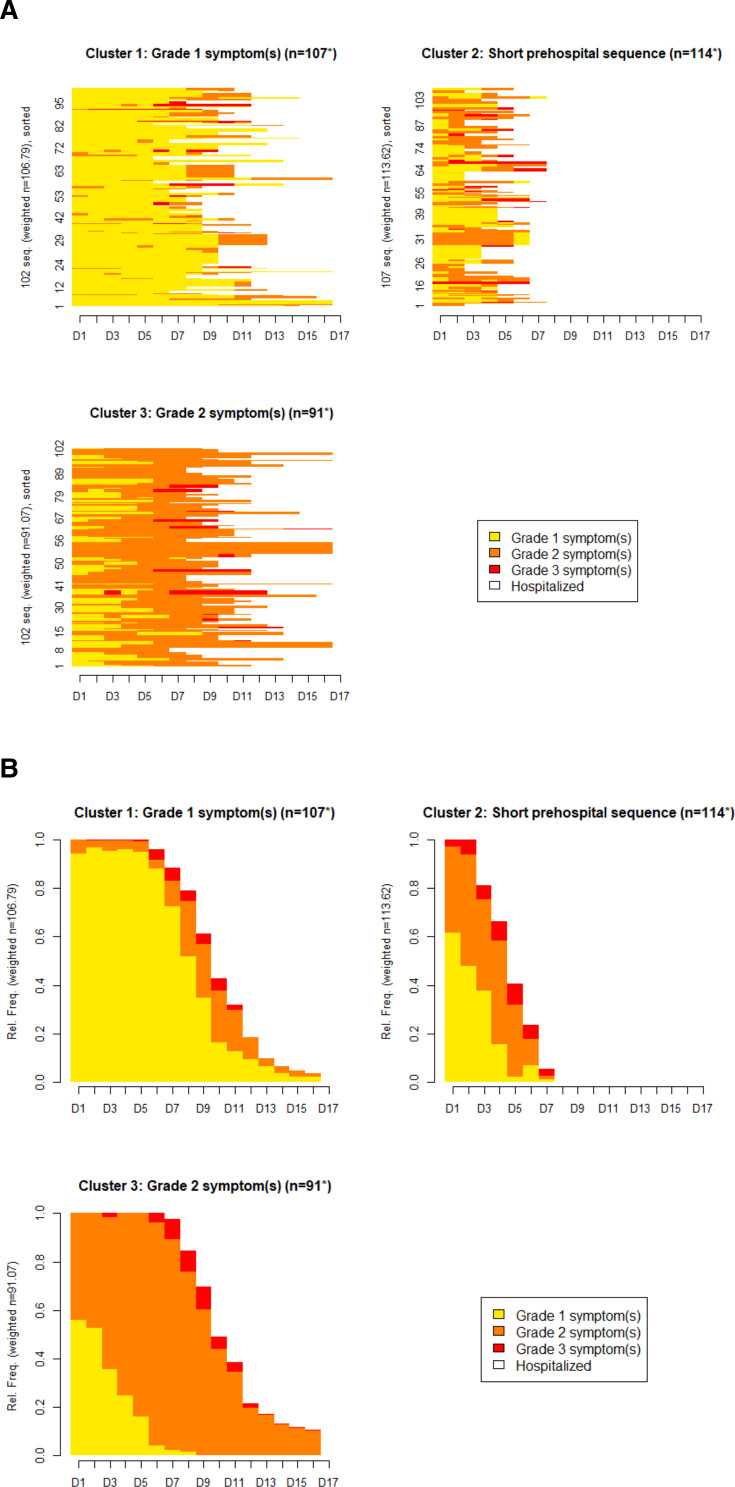
The SSA combined with the HCA (online supplemental material 2) identified three clusters (figure 2A,B, table 2), resulting in the typology of different symptom sequences from symptom onset to hospitalisation. To check the robustness of our clustering solution, we performed three sensitivity analyses in which we tested different combinations of substitution and insertion/deletion costs in the SSA analyses. The results were very stable (Cohen’s Kappa coefficient >0.84 between the four clustering solutions).
Figure 2.
(A) Sequence index plots (each line represents a participant’s symptom sequence). (B) Chronograms/state distribution plots (the plots show the distribution of states (grade 1, 2 and 3) for each time unit point (17 days). *Weighted frequency.
Table 2.
Sociodemographic and clinical profiles of the three clusters of symptom sequences (n=312)
| Grade 1 symptom(s) | Short prehospital sequence | Grade 2 symptom(s) | ||||
| n* | %† | n* | %† | n* | %† | |
| n | 107 | 114 | 91 | |||
| Sex | ||||||
| Female | 36 | 33.9 | 51 | 45.2 | 40 | 44.4 |
| Male | 71 | 66.1 | 62 | 54.8 | 51 | 55.6 |
| Age | ||||||
| Mean (SD) | 66.4 (13.9) | 65.3 (16.0) | 63.7 (10.9) | |||
| 18–49 | 15 | 14.0 | 21 | 18.4 | 11 | 12.0 |
| 50–64 | 30 | 27.8 | 29 | 25.6 | 38 | 41.8** |
| 65–79 | 40 | 37.2 | 36 | 31.5 | 31 | 33.9 |
| >79 | 22 | 21.0 | 28 | 24.5 | 11 | 12.4* |
| Site | ||||||
| Marseille | 87 | 81.4 | 93 | 82.2 | 68 | 74.4 |
| Nice | 20 | 18.6 | 20 | 17.8 | 23 | 25.6 |
| Period | ||||||
| 2020 | 33 | 31.1 | 40 | 35.5 | 38 | 41.8 |
| 2021 | 74 | 68.9 | 73 | 64.5 | 53 | 58.2 |
| Education | ||||||
| <General certificate of secondary education | 13 | 12.4 | 23 | 20.0 | 13 | 13.8 |
| General certificate of secondary education | 21 | 19.7 | 15 | 13.6 | 22 | 24.7 |
| High school diploma | 16 | 14.6 | 17 | 14.7 | 20 | 21.7 |
| ≥Diploma of higher education | 57 | 53.2 | 59 | 51.7 | 36 | 39.8* |
| Number of comorbidities/medical history | ||||||
| None | 29 | 27.1 | 40 | 35.6 | 27 | 30.0 |
| One | 29 | 27.1 | 28 | 24.4 | 28 | 31.1 |
| Two | 15 | 14.4 | 14 | 12.2 | 15 | 16.5 |
| Three | 19 | 17.7 | 14 | 12.4 | 9 | 9.7 |
| More than three | 15 | 13.7 | 17 | 15.3 | 12 | 12.7 |
| Daily smoker | 3 | 2.9 | 6 | 5.3 | 1 | 1.0 |
| Obesity (body mass index≥30 kg/m²) | 21 | 20.1 | 37 | 32.7* | 21 | 23.0 |
| Live alone | 23 | 21.8 | 30 | 26.2 | 24 | 25.8 |
| Works/has worked as a healthcare worker | 26 | 24.0 | 22 | 18.9 | 15 | 16.9 |
| Knows someone in his/her close circle who is a healthcare worker | 66 | 61.5* | 68 | 59.7 | 30 | 33.3*** |
| COVID-19 diagnosis confirmed after symptom onset | 76 | 71.4 | 72 | 63.7** | 77 | 84.7** |
| Number of negative tests prior to confirmed COVID-19 diagnosis | ||||||
| None | 89 | 83.5 | 87 | 76.9 | 77 | 84.7 |
| One | 14 | 13.2 | 11 | 9.8 | 8 | 8.9 |
| Two or more | 4 | 3.3* | 15 | 13.3** | 6 | 6.4 |
| Declares having difficulties to see a doctor | 31 | 28.7 | 24 | 21.0 | 28 | 30.6 |
| Declares having difficulties to get treatment | 23 | 21.5 | 20 | 18.0 | 30 | 33.2* |
| Has consulted a general practitioner‡ | 68 | 63.6 | 56 | 49.2* | 53 | 58.3 |
| Has consulted at ‘day hospital’‡ | 56 | 52.2 | 53 | 46.6 | 34 | 37.4 |
| Has consulted an emergency service‡ | 22 | 20.3 | 17 | 15.0 | 25 | 27.9* |
| Was aware of the seriousness of their health status prior to hospitalisation | 41 | 38.0 | 48 | 42.7 | 36 | 39.7 |
| Trigger of hospitalisation | ||||||
| Family member | 30 | 27.8 | 27 | 23.7 | 34 | 37.4* |
| General practitioner | 13 | 11.9 | 27 | 23.7* | 12 | 13.2 |
| Emergency service | 38 | 35.8 | 42 | 36.9 | 30 | 33.2 |
| Patient | 17 | 15.5 | 14 | 12.6 | 11 | 12.1 |
| Prehospital treatments | ||||||
| Antibiotics§ | 74 | 69.6** | 62 | 54.3 | 46 | 50.5 |
| No treatment¶ | 25 | 23.7* | 41 | 36.2 | 34 | 37.5 |
| Clinical outcomes | ||||||
| Length of hospital stay (days) (nmiss=1) | ||||||
| Mean (SD) | 12.4 (17.3) | 9.7 (10.7) | 10.4 (8.8) | |||
| Transfer to intensive care unit | 46 | 43.0* | 59 | 52.0 | 52 | 57.6 |
| Follow-up/rehabilitation care after hospitalisation | 56 | 52.4 | 53 | 46.7 | 55 | 60.2 |
| Home oxygen treatment after hospitalisation | 58 | 54.2 | 71 | 62.8 | 47 | 51.6 |
| Still has sequelae of COVID-19 at the time of the survey | 47 | 44.0 | 53 | 47.0 | 53 | 57.7* |
| Physical sequelae | 37 | 34.4 | 47 | 41.4 | 43 | 46.7 |
| Neurological sequelae | 36 | 33.5 | 34 | 30.1 | 26 | 28.4 |
| Psychological sequelae | 22 | 21.0 | 15 | 12.8 | 20 | 21.7 |
| Sleep disorders sequelae | 15 | 14.2 | 22 | 19.4 | 14 | 15.6 |
*p<0.05, **p<0.01, ***p<0.001, respectively (weighted χ2 test). The value in the cluster is compared to the remaining sample.
*Weighted frequency otherwise stated; the sum may not add to cluster size due to rounding.
†Weighted column percentages otherwise stated; the sum may not add to 100% due to rounding.
‡Between symptom onset and hospitalisation.
§Infectious diseases department of Marseille protocol included (hydroxychloroquine+azithromycin).
¶Paracetamol excluded.
fmch-2023-002447supp002.pdf (36.1KB, pdf)
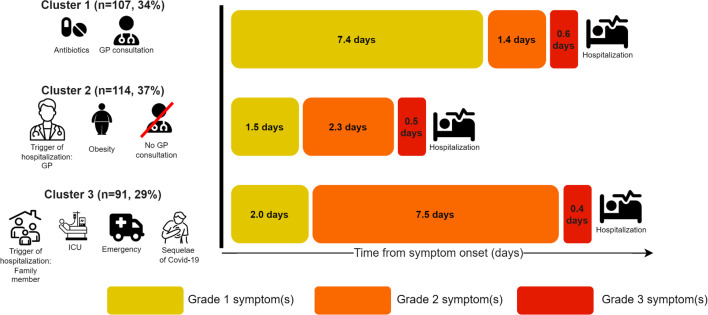
The first cluster (cluster 1, ‘grade 1 symptom(s)’) (n=107, 34.3%) comprised patients with relatively long primary (ie, prehospital) care sequences (9.4 days on average). Compared with the two other clusters, most patients in cluster 1 reported grade 1 symptoms from day 1 to day 9. Grade 2 symptoms were more frequently reported after day 9 (figure 2). On average, these patients reported grade 1 symptoms for 7.4 days, grade 2 symptoms for 1.4 days and grade 3 symptoms for 0.6 days prior to hospitalisation.
The second cluster (cluster 2, short prehospital sequence’) (n=144, 36.5%) comprised patients with relatively short primary care sequences compared with the two other clusters (4.3 days). On average, these patients reported grade 1 symptoms for 1.5 days, grade 2 symptoms for 2.3 days and grade 3 symptoms for 0.5 days prior to hospitalisation.
The last cluster (cluster 3, ‘grade 2 symptom(s)’) (n=91, 29.2%) comprised patients who reported grade 2 symptoms more frequently. The length of their primary care sequence was comparable to that for cluster 1 (ie, 9.9 days). However, in cluster 3, all patients reported at least one grade 2 symptom during their primary care sequence (vs 60.4% in cluster 1, p<0.001). On average, patients in cluster 3 reported grade 1 symptoms for 2.0 days, grade 2 symptoms for 7.5 days and grade 3 symptoms for 0.4 days prior to hospitalisation.
In bivariate analyses (table 2), patients assigned to cluster 1 showed a higher likelihood of knowing a loved one who was a healthcare worker (61.5% vs 57.9% in clusters 2 and 3, p=0.022). This cluster also demonstrated a reduced likelihood of having undergone two or more negative tests before the COVID-19 diagnosis compared with clusters 2 and 3 (3.3% vs 10.2%, p=0.032) and an increased likelihood of reporting treatment with antibiotics (69.6% vs 52.6%, p=0.004). The transfer to the ICU was also significantly lower in cluster 1 (43.0% vs 57.0%, p=0.050). In cluster 2, compared with clusters 1 and 3, the proportion of obese patients was significantly higher (32.7% vs 21.5%, p=0.028), and fewer patients declared that their COVID-19 diagnosis was confirmed after symptom onset (63.7% vs 77.5%, p=0.009). This cluster also exhibited a higher likelihood of having undergone two or more negative tests before the COVID-19 diagnosis (13.3% vs 4.8%, p=0.007). In a quarter of cases, it was a GP who decided the patient needed hospitalisation (23.7% vs 12.5%, p=0.011). Regarding the last cluster, compared with clusters 1 and 2, cluster 3 had a significantly lower proportion of patients aged >79 (12.4% vs 22.8%, p=0.036), a lower proportion of patients with a high education level (39.8% vs 52.4%, p=0.043), and a lower likelihood of knowing a loved one who was a healthcare worker (33.3% vs 60.6%, p<0.001). Furthermore, cluster 3 had a higher proportion of patients whose COVID-19 diagnosis was confirmed after symptom onset (84.7% vs 67.4%, p=0.002), a higher proportion of patients reporting difficulties in obtaining treatment (33.2% vs 19.7%, p=0.011), and a higher proportion of patients who had consulted an emergency service (27.9% vs 17.6%, p=0.039). In over one-third of cases, a family member determined the need for hospitalisation (37.4% vs 25.7%, p=0.038). Additionally, the proportion of patients declaring persistent sequelae of COVID-19 at the time of the survey was significantly higher (57.7% vs 45.5%, p=0.050).
After adjustment for the main risk factors (table 3), patients assigned to cluster 3 had, all things being equal, a significantly higher risk of admission to an ICU (adjusted OR 2.01 (95% CI 1.10 to 3.60)) compared with those in cluster 1. The proportion of patients who declared sequelae at the time of the survey was not significantly higher after adjustment for the main risk factors (1.54 (0.85 to 2.80), p=0.159).
Table 3.
Association of intensive care unit admission and of COVID-19 sequelae at time of survey with symptom sequences clusters; adjusted multivariate logistic regressions (n=312)
| Admission to intensive care unit | COVID-19 sequelae at the time of survey | |||
| aOR 95% CI* | P value | aOR 95% CI* | P value | |
| Female (ref. male) | 0.41 (0.24 to 0.68) | <0.001 | 1.54 (0.93 to 2.56) | 0.097 |
| Age (years) | 1.01 (0.99 to 1.03) | 0.429 | 0.98 (0.96 to 1.00) | 0.020 |
| Education level (ref. <general certificate of secondary education) | ||||
| General certificate of secondary education | 0.80 (0.34 to 1.88) | 0.612 | 1.96 (0.84 to 4.59) | 0.121 |
| High school diploma | 0.90 (0.38 to 2.15) | 0.809 | 2.69 (1.12 to 6.45) | 0.027 |
| ≥Diploma of higher education | 0.56 (0.26 to 1.19) | 0.131 | 1.18 (0.56 to 2.50) | 0.661 |
| Lived alone (ref. no) | 1.08 (0.60 to 1.92) | 0.805 | 1.07 (0.60 to 1.90) | 0.829 |
| Number of comorbidities/medical history (ref. none) | ||||
| One | 0.87 (0.45 to 1.66) | 0.669 | 2.54 (1.31 to 4.94) | 0.006 |
| Two | 1.16 (0.54 to 2.49) | 0.704 | 1.57 (0.73 to 3.37) | 0.246 |
| Three | 1.33 (0.60 to 2.95) | 0.485 | 2.01 (0.89 to 4.54) | 0.094 |
| More than three | 0.79 (0.34 to 1.82) | 0.576 | 2.06 (0.88 to 4.79) | 0.095 |
| Daily smoker (ref. no) | 1.23 (0.31 to 4.91) | 0.774 | 2.67 (0.58 to 12.26) | 0.207 |
| Obesity (ref. no) | 1.92 (1.09 to 3.38) | 0.023 | 1.48 (0.84 to 2.59) | 0.175 |
| Prehospital symptom sequence (ref. cluster 1: grade 1 symptom(s) sequence) | ||||
| Cluster 2: short prehospital sequence | 1.51 (0.85 to 2.65) | 0.157 | 1.10 (0.62 to 1.95) | 0.744 |
| Cluster 3: grade 2 symptom(s) sequence | 2.01 (1.10 to 3.67) | 0.024 | 1.54 (0.85 to 2.80) | 0.159 |
*Adjusted OR with 95% CI.
Discussion
Our study shows that a significant proportion of hospitalised patients (cluster 3) had symptoms of severe COVID-19 (grade 2) for a long period of time (7.5 days on average) before being hospitalised. Patients in this cluster were more likely to have previously visited an ED for COVID-19-like symptoms, and more likely reported more difficulties with primary care (ie, prehospital) treatment. Compared with the other two clusters, they were less likely to know a loved one who was a healthcare worker, and less likely to have a higher level of education (ie, diploma of higher education or higher).
These results suggest that this population was less integrated in the health system and had greater difficultly accessing primary care in general. Health inequalities, which have been the subject of a large number of publications, both on COVID and on the state of health in general.21–24
We have identified four key reasons that may explain the delayed hospitalisation in cluster 3 despite the severity of COVID-19 symptoms:
Lack of healthcare professionals in the personal network: individuals without close connections to healthcare professionals may experience delays in seeking hospitalisation. The absence of immediate access to medical advice can contribute to a delay in recognising the severity of symptoms.
Absence of higher education credentials: those without a higher education background might face challenges in understanding the gravity of their symptoms or may be less likely to seek prompt medical attention due to a potential lack of health literacy.
Postponing reevaluation after recent emergency room visit: patients who have recently visited the emergency room and did not exhibit severe symptoms at that time may be inclined to defer reevaluation when their health deteriorates. This delay could be attributed to a perceived lower risk based on the recent emergency room visit.
Perception of lower risk due to supposed health status: both patients and healthcare professionals may hold a misperception regarding the risk associated with individuals identified as belonging to a lower-risk population, such as those of intermediate age with fewer comorbidities. This collective misperception may lead to an underestimation of symptom severity, contributing to delays in hospitalisation despite the presence of alarming signs.
All these reasons may have prompted patients to postpone their decision to seek additional hospital care despite experiencing symptoms, waiting until a relative, friend or general practitioner expressed concern. The role of loved ones in triggering hospitalisation was a decisive resource for patients in cluster 3. The erratic primary care pathway described for patients in cluster 3 was detrimental, as they were two times as likely to be admitted to an ICU and to suffer from COVID-19 sequelae after release from hospital. These findings contrast with the pathway of comorbid patients at risk of severe COVID-19 infection who were closely monitored by their GP and who did not hesitate to be hospitalised very early after symptom onset. The results are summarised in figure 3.
Figure 3.
Timeline of prehospital care pathways and main clinical outcomes.
Strengths and weaknesses
This study has several potential limitations. First concern arises from selection bias, as our study exclusively includes survivors of COVID-19. It is recognised that non-survivors could constitute a more extreme subgroup, hinting at a potential fourth cluster marked by intensified symptoms before hospitalisation. This could affect the representativeness of our study population for all hospitalised COVID-19 patients. To address this, an alternative approach could involve interviewing patients on hospital admission, extracting clinical outcomes from medical databases and conducting a follow-up interview 1 year later to assess COVID-19 sequelae. Second, as the survey was conducted using self-administered questionnaires, it was not possible to make an objective evaluation of each symptom or clinical event. Third, patients may have been subject to memory bias as the survey—which investigated their prehospital symptoms—took place between 13 and 20 months after hospitalisation. However, previous studies show that in the case of traumatic events, such as hospitalisation, patients often retain good memory of the events that led to their hospitalisation.25–27
Despite these limitations, this study clearly identified a significant delay in management for patients with severe symptoms. The life-events calendar method allowed us to explore the clinical history of the patients with great precision, something we would not have otherwise been able to obtain. Specifically, the quantitative processing of care pathways7—made possible by OM—allowed us to (a) highlight important differences in care pathways, (b) test hypotheses to explain these pathways, (c) evaluate the impact of these care pathways on the clinical outbreak (admission to an ICU, sequelae after release from hospital) and (d) highlight the person who decided that the patient had to be hospitalised.
Suitability of the methodology used
In the literature to date, patient experience has been the domain of qualitative methods and patient reporting experience measures.28–33 Despite this, until now patients’ experience has not been studied in depth in a contextualised way34 35 that is to say, has not been studied in the various objective elements of the care pathway. By using a processual approach using the life-events calendar method and an SSA, we were able to combine patients’ subjective experience with objective contextual data (medical records describing their hospitalisation history and their socio-clinical profiles). This combination helped us acquire a better understanding of their primary care pathways before hospitalisation.
Implications for research and clinical practices
The multidimensional perspective emphasises that effective care goes beyond medical interventions. It underscores the importance of addressing practical challenges and barriers that patients encounter in their daily lives.2 This may involve collaboration with social services, community organisations, to ensure that patients have access to the necessary resources.
Conclusions
This study highlights the importance of temporality in primary care pathways and demonstrates that patients in France with severe symptoms of COVID-19 during the first wave of the pandemic experienced a delay before hospitalisation which was detrimental to their health. The processual approach revealed the interconnectedness of biology, personal history and social context.36
Footnotes
Contributors: RL, SC, LD, PP-W, JM, MB, LC, DT, GG, CP, TI, PB, ST, MC and SG collectively conceived and designed the study. RL, SC and LD conducted analyses. RL, SC and SG drafted the manuscript. RL, SC, LD, PP-W, JM, MB, LC, DT, GG, CP, TI, PB, ST, MC and SG critically revised the manuscript. SG is responsible for the overall content
Funding: This project was funded by Agence Nationale de la Recherche 'Résilience Covid-19' (ANR-21-COVR-0043).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All materials and database of this study are openly available on recherche.data.gouv.fr [dataset]. Cortaredona S, Gentile S, Lutaud R, et al. Expérience patient & parcours préhospitalier des patients COVID-19. 2023. https://doi.org/10.57745/7J9VEQ.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and was approved by French North West IV Ethics Committee (authorisation N° EudraCT/ID-RCB: 2021-A01138-33, 2 July 2021). The authors had no personal relationship with the participants. All the patients contacted received an information letter and a non-opposition form in accordance with this ethics committee’s guidelines. Participants gave informed consent to participate in the study before taking part.
References
- 1.Larson E, Sharma J, Bohren MA, et al. When the patient is the expert: measuring patient experience and satisfaction with care. Bull World Health Organ 2019;97:563–9. 10.2471/BLT.18.225201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meyers T. How is comorbidity lived. Lancet 2015;386:1128–9. 10.1016/S0140-6736(15)00210-X [DOI] [PubMed] [Google Scholar]
- 3.Roux J, Grimaud O, Leray E. Use of state sequence analysis for care pathway analysis: the example of multiple sclerosis. Stat Methods Med Res 2019;28:1651–63. 10.1177/0962280218772068 [DOI] [PubMed] [Google Scholar]
- 4.Vignier N, Desgrees Du Lou A, Pannetier J, et al. Social and structural factors and engagement in HIV care of sub-saharan african migrants diagnosed with HIV in the paris region. AIDS Care 2019;31:897–907. 10.1080/09540121.2019.1576842 [DOI] [PubMed] [Google Scholar]
- 5.Desgrées-du-Loû A, Pannetier J, Ravalihasy A, et al. Sub-saharan african migrants living with HIV acquired after migration, france, anrs parcours study, 2012 to 2013. Euro Surveill 2015;20. 10.2807/1560-7917.ES.2015.20.46.30065 [DOI] [PubMed] [Google Scholar]
- 6.Pailhé A, Robette N, Solaz A. Work and family over the life-course. A typology of french long-lasting couples using optimal matching. LLCS 2013;4:196–217. 10.14301/llcs.v4i3.250 [DOI] [Google Scholar]
- 7.Abbott A, Tsay A. Sequence analysis and optimal matching methods in sociology. Sociological Methods & Research 2000;29:3–33. 10.1177/0049124100029001001 [DOI] [Google Scholar]
- 8.Courtejoie N, Dubost C. Parcours hospitalier des patients atteints de la COVID-19 lors de la première vague de L’epidémie. In: DREES. 2020. Available: https://drees.solidarites-sante.gouv.fr/sites/default/files/2020-10/DD67.pdf [Google Scholar]
- 9.Arlotto S, Garès A, Giraud-Gatineau A, et al. Life-years lost by COVID-19 patients in public hospitals of marseille (APHM-south-eastern france): a limited death toll: a retrospective analysis. BMJ Open 2021;11:e049475. 10.1136/bmjopen-2021-049475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Le Borgne P, Oberlin M, Bassand A, et al. Pre-hospital management of critically ill patients with SARS-Cov-2 infection: a retrospective multicenter study. J Clin Med 2020;9:3744. 10.3390/jcm9113744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biographies D’Enquêtes. In: Biographies d’enquêtes - Bilan de 14 collectes biographiques - Groupe de réflexion sur l’approche biographique. Paris, 2009. 10.4000/books.ined.6518 [DOI] [Google Scholar]
- 12.Lutaud R, Verger P, Peretti-Watel P, et al. When the patient is making the (wrong?) diagnosis: a biographical approach to patients consulting for presumed lyme disease. Fam Pract 2022:cmac116. 10.1093/fampra/cmac116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cortaredona S, Gentile S, Lutaud R, et al. Data from: expérience patient & parcours préhospitalier des patients COVID-19. 2023. Available: 10.57745/7J9VEQ [DOI]
- 14.Studer M, Ritschard G. What matters in differences between life trajectories: a comparative review of sequence dissimilarity measures. J R Stat Soc Ser A Stat Soc 2016;179:481–511. 10.1111/rssa.12125 [DOI] [Google Scholar]
- 15.Cezard G, Sullivan F, Keenan K. Understanding multimorbidity trajectories in scotland using sequence analysis. Sci Rep 2022;12:16485. 10.1038/s41598-022-20546-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 17.Brzinsky-Fay C, Kohler U. New developments in sequence analysis. Sociological Methods & Research 2010;38:359–64. 10.1177/0049124110363371 [DOI] [Google Scholar]
- 18.Studer M. Weightedcluster library manual: a practical guide to creating typologies of trajectories in the social sciences with R. LIVES Work Pap 2013;24. [Google Scholar]
- 19.Ko JY, Danielson ML, Town M. n.d. Risk factors for COVID-19-associated hospitalization: COVID-19-associated hospitalization surveillance network and behavioral risk factor surveillance system. Epidemiology 10.1101/2020.07.27.20161810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gabadinho A, Ritschard G, Müller NS. n.d. Analyzing and visualizing state sequences in R with traminer. J Stat Soft;40. 10.18637/jss.v040.i04 [DOI] [Google Scholar]
- 21.Ginsburgh V, Magerman G, Natali I. COVID-19 and the role of inequality in french regional departments. Eur J Health Econ 2021;22:311–27. 10.1007/s10198-020-01254-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atlani-Duault L, Chauvin F, Yazdanpanah Y, et al. France’s COVID-19 response: balancing conflicting public health traditions. The Lancet 2020;396:219–21. 10.1016/S0140-6736(20)31599-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bajos N, Counil E, Franck J-E, et al. Social inequalities and dynamics of the early COVID-19 epidemic: a prospective cohort study in france. BMJ Open 2021;11:e052888. 10.1136/bmjopen-2021-052888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richard Z, Chabrol F, Gautier L, et al. Considering social inequalities in health in COVID-19 response: insights from a french case study. Health Promot Int 2023;38:daac173. 10.1093/heapro/daac173 [DOI] [PubMed] [Google Scholar]
- 25.Chemtob C, Roitblat HL, Hamada RS, et al. A cognitive action theory of post-traumatic stress disorder. Journal of Anxiety Disorders 1988;2:253–75. 10.1016/0887-6185(88)90006-0 [DOI] [Google Scholar]
- 26.Buckley TC, Blanchard EB, Neill WT. Information processing and PTSD: a review of the empirical literature. Clin Psychol Rev 2000;20:1041–65. 10.1016/s0272-7358(99)00030-6 [DOI] [PubMed] [Google Scholar]
- 27.Bardeen JR, Daniel TA, Gordon RD, et al. Individual differences in attentional control explain the differential expression of threat-related attentional bias among those with posttraumatic stress symptomatology and predict symptom maintenance up to one year later. Behav Res Ther 2020;133:103709. 10.1016/j.brat.2020.103709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandes S, Fond G, Zendjidjian XY, et al. Measuring the patient experience of mental health care: a systematic and critical review of patient-reported experience measures. Patient Prefer Adherence 2020;14:2147–61. 10.2147/PPA.S255264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang DE, Tsugawa Y, Figueroa JF, et al. Association between the centers for medicare and medicaid services hospital star rating and patient outcomes. JAMA Intern Med 2016;176:848–50. 10.1001/jamainternmed.2016.0784 [DOI] [PubMed] [Google Scholar]
- 30.Trzeciak S, Gaughan JP, Bosire J, et al. Association between medicare summary star ratings for patient experience and clinical outcomes in US hospitals. J Patient Exp 2016;3:6–9. 10.1177/2374373516636681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jenkinson C, Coulter A, Bruster S, et al. Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care 2002;11:335–9. 10.1136/qhc.11.4.335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kingsley C, Patel S. Patient-reported outcome measures and patient-reported experience measures. BJA Education 2017;17:137–44. 10.1093/bjaed/mkw060 [DOI] [Google Scholar]
- 33.Gleeson H, Calderon A, Swami V, et al. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open 2016;6:e011907. 10.1136/bmjopen-2016-011907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Drain M, Clark PA. Measuring experience from the patient ’ s perspective: implications for national initiatives; 2004.
- 35.Øvretveit J, Zubkoff L, Nelson EC, et al. Using patient-reported outcome measurement to improve patient care. Int J Qual Health Care 2017;29:874–9. 10.1093/intqhc/mzx108 [DOI] [PubMed] [Google Scholar]
- 36.Fassin D. Life: A Critical User’s Manual 1st edition. Cambridge, UK ; Medford, MA: Polity, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
fmch-2023-002447supp001.pdf (1.3MB, pdf)
fmch-2023-002447supp002.pdf (36.1KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All materials and database of this study are openly available on recherche.data.gouv.fr [dataset]. Cortaredona S, Gentile S, Lutaud R, et al. Expérience patient & parcours préhospitalier des patients COVID-19. 2023. https://doi.org/10.57745/7J9VEQ.