Abstract
Objective
This study aims to characterise respondents who have COVID-19 and long COVID syndrome (LCS), and describe their symptoms and healthcare utilisation.
Design
Observational cross-sectional survey.
Setting
The one-time online survey was available from June 2022 to November 2022 to capture the experience of residents in Manitoba, Canada.
Participant
Individuals shared their experience with COVID-19 including their COVID-19 symptoms, symptoms suggestive of LCS and healthcare utilisation. We used descriptive statistics to characterise patients with COVID-19, describe symptoms suggestive of LCS and explore respondent health system use based on presenting symptoms.
Results
There were 654 Manitobans who responded to our survey, 616 (94.2%) of whom had or provided care to someone who had COVID-19, and 334 (54.2%) reported symptoms lasting 3 or more months. On average, respondents reported having 10 symptoms suggestive of LCS, with the most common being extreme fatigue (79.6%), issues with concentration, thinking and memory (76.6%), shortness of breath with activity (65.3%) and headaches (64.1%). Half of the respondents (49.2%) did not seek healthcare for COVID-19 or LCS. Primary care was sought by 66.2% respondents with symptoms suggestive of LCS, 15.2% visited an emergency department and 32.0% obtained care from a specialist or therapist. 62.6% of respondents with symptoms suggestive of LCS reported reducing work, school or other activities which demonstrate its impact on physical function and health-related quality of life.
Conclusion
Consistent with the literature, there are a variety of symptoms experienced among individuals with COVID-19 and LCS. Healthcare providers face challenge in providing care for patients with a wide range of symptoms unlikely to respond to a single intervention. These findings support the value of interdisciplinary COVID-19 clinics due to the complexity of the syndrome. This study confirms that data collected from the healthcare system do not provide a comprehensive reflection of LCS.
Keywords: COVID-19, Public health, Primary Health Care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Results of this study are not generalisable, those who chose to respond may have been different compared with those who did not respond.
Asymptomatic patients, patients with mild symptoms or patients who did not experience long COVID syndrome (LCS) may have been less likely to participate.
The retrospective nature of this study may have introduced recall bias and resulted in over-reporting and under-reporting of symptoms.
The survey captured experiences of patients with and without health system use providing insight into community-based experiences with COVID-19 and in particular LCS.
Introduction
SARS-CoV-2, also known as COVID-19, is a multisystemic disease with a range of symptoms and severity. First diagnosed in December 2019, a number of symptoms have been documented largely affecting the respiratory system but also affecting the heart, kidney, liver, muscles, skin and nervous systems. Clinical manifestations in the initial phase of COVID-19 may include fever, cough, fatigue, sore throat, loss of taste and smell, congestion and headaches.1–3 The severity of initial symptoms among Canadian adults varies considerably with 5.2% asymptomatic, 34.2% having mild symptoms, 43.9% having moderate symptoms and 16.7% reporting severe symptoms that significantly impacted their daily life.1
Reports of long COVID syndrome (LCS), also known as post COVID condition, have become increasingly common over time.1 4–8 LCS is characterised as symptoms present 3 or more months from the onset of COVID-19 that cannot be explained by another condition.1 3 4 The most common symptoms may include fatigue, cognitive impairment/dysfunction, shortness of breath, headaches, chest pain and mental health conditions. These symptoms may fluctuate or relapse over time.1 4–6 9 10 Estimates of LCS vary, ranging from 10% to 35% due to differences in study cohorts including criteria for defining the condition.1 3 8 9 Statistics Canada1 found, in a national survey, that 14.8% of Canadians who had or thought they had COVID-19 experienced symptoms 3 or more months after their initial infection.1 Risk of LCS is thought to be influenced by infection severity, type of variant, patient characteristics and vaccination status; however, understanding of this condition is still growing.1 3 8 In addition, research has shown a negative impact of LCS on quality of life, activities of daily living as well as on the ability to return to work, school or regular activities following recovery.7 10 11
Estimates of LCS have largely relied on cohort studies or medical records of patients with severe COVID-19 infection, which may underestimate the true prevalence.1 3 12 The majority of individuals who had COVID-19 had mild or no symptoms and may not present to the healthcare system.3 There is an increasing number of patients who were asymptomatic or had mild COVID-19 presenting with LCS symptoms.3 5 9 10 13 Identifying and managing this condition have challenged healthcare providers due to the wide range of symptoms as well as a lack of diagnostic tests and validated treatment options. Management of LCS may require a whole-patient approach from an interdisciplinary team that can attend to acute symptoms, sequelae, secondary prevention and rehabilitation.9
Healthcare use is expected to increase among patients with LCS.8 This study aimed to supplement research from health system use with community-based experiences with COVID-19 and in particular LCS. We present self-reported experiences with COVID-19 and LCS, and respondent health system use based on presenting symptoms. An understanding of the experiences of patients with LCS may inform health system planning and help providers promptly recognise and manage LCS.3
Methods
Study setting
Manitoba is located in central Canada with a population of ~1.4 million people, representing ~4% of the Canadian population.14 The majority of the Manitoba population (54%) lives in Winnipeg; however, Manitoba also includes many northern and remote communities. In Canada, healthcare delivery is a provincial/territorial responsibility whereby medically necessary services including hospital, emergency department, primary care and specialist services are provided via single-payer, publicly funded insurance. Typically, the first point of contact with the health system is primary care which is delivered by family physicians, nurse practitioners and community paediatricians at independently operated community-based clinics. Physiotherapists, occupational therapists, respiratory therapists and speech therapists can be accessed at private fee-for-service clinics or by referral and are not always covered by health insurance.
COVID-19 was first diagnosed in Manitoba, in March 2020, leading to the implementation of several public health policies intended to prevent the spread of COVID-19. As of 9 November 2022, when community wide surveillance was discontinued, there were an estimated 152 072 cases of COVID-19 in Manitoba.15 This number is likely an underestimate of the true number of cases of COVID-19 due to reliance on provincial laboratory records, which only captured formal testing of individuals meeting certain criteria. Free rapid testing kits have been widely distributed around Manitoba and positive results are not captured in provincial records.
Data collection
We created an online survey, informed by symptoms documented in published literature,1 12 16–19 comprised of 23 questions to capture acute COVID-19 symptoms, symptoms present ≥3 months after initial infection and healthcare utilisation. There were seven questions related to initial COVID-19 infection, four questions related to LCS, seven questions related to health service utilisation and four demographic questions (online supplemental material A). The survey was available online for all Manitobans from June to October 2022, and advertised using social media, traditional media and poster distribution. Advertisement requested feedback from participants about their experience with COVID-19 (online supplemental material B). The survey was anonymous and therefore participants did not receive an honorarium for participating. Prior to accessing the survey, participants were provided with a description of the study (online supplemental material A) including the sentence ‘by continuing and completing the survey, you are consenting to participate’. Therefore, participation was presumed to be an indication of consent. In June 2022, the survey was shared in Manitoba news media and talk radio. Further to this, the survey was shared on three social media platforms, Facebook, Twitter and Instagram, from June to August 2022. Social media advertising was promoted using organisation sites and media releases. In September and October 2022, paid social media for Facebook, Instagram and Twitter was used to increase participation in our survey. Throughout the length of the study, the research team promoted the survey using posters, community groups and healthcare organisation.
bmjopen-2023-075301supp001.pdf (121.9KB, pdf)
bmjopen-2023-075301supp002.pdf (74.6KB, pdf)
Data analysis
We used descriptive statistics to characterise respondents, describe symptoms of COVID-19 and describe symptoms suggestive of LCS (present ≥3 months after initial infection). We used Χ2 and t-test to assess differences between populations who did, and did not, report experiencing symptoms suggestive of LCS. Further to this, we explored symptoms of COVID-19 and symptoms suggestive of LCS in relation to healthcare use including primary care, emergency department, hospitalisation, specialists and therapists. Missing responses were omitted from analyses. Urban residency was determined using the first three characters from the respondent’s postal code. Due to small numbers, education less than high school was grouped with high school or equivalent. We thematically analysed the open-ended survey questions related to ‘other symptoms’ and ‘not attending healthcare’.
Patient and public involvement
To develop this survey, a pilot survey was implemented in a small sample of Manitobans. This pilot survey enabled the research team to integrate feedback from Manitobans into the survey. Further, in this survey (online supplemental material A), Manitobans were invited to share their experience with COVID-19. We provided open-ended questions to allow participants to elaborate on their symptoms and healthcare use; these responses were thematically analysed and presented in the results.
Results
There were 654 individuals who responded to our survey and had a Manitoba postal code. The majority of respondents had contracted COVID-19 (94.2%, 616 of 654), 549 reported having contracted COVID-19 themself, 42 had a child who had COVID-19 and 25 provided care to another person with COVID-19 (online supplemental material C).
bmjopen-2023-075301supp003.pdf (81.7KB, pdf)
Among respondents, the majority were female (78.6%, 474 of 603) and had a mean age of 45.9 years (SD 14.6). Respondents frequently had a university degree (29.7%, 188 of 654 had an undergraduate degree; and 23.1%, 151 of 654 had a postgraduate degree) and an income greater than or equal to $100 000 (34.7%, 227 of 654). Respondents had COVID-19 between Spring 2020 and Fall 2022; however, the majority of respondents had COVID-19 in the Winter 2021/2022 (28.2%, 174 of 616) and Spring 2022 (34.4%, 212 of 616) (online supplemental material D), which corresponds with the highest rates of infection in Manitoba.
bmjopen-2023-075301supp004.pdf (246.8KB, pdf)
Respondents with COVID-19 infection
The majority of respondents (88.1%, 543 of 616) had COVID-19 confirmed with a PCR or rapid antigen test. Most respondents (76.6%, 472 of 616) had received one or more COVID-19 vaccinations at the time of infection. Table 1 describes the respondents who contracted COVID-19. Forty-one per cent of respondents (253 of 616) who had COVID-19 did not report any persistent symptoms. Among these 253 respondents, 49.8% (126 of 253) had COVID-19 less than 3 months prior to responding, and 50.2% (127 of 253) reported no symptoms lasting ≥3 months. There were 334 respondents who reported symptoms ≥3 months after their initial infection; on average, these respondents were older than those without persistent symptoms (47.4 years (SD 14.2) vs 44.5 years (SD 14.9), p=0.017).
Table 1.
Characteristics of survey respondents with COVID-19, both with and without LCS symptoms
| Variable | Respondents with COVID-19* | COVID-19 but no symptoms ≥3 months after infection† | COVID-19 with symptoms for ≥3 months | P value (respondents with vs without symptoms for ≥3 months) |
| Urban residency, n (%) | 450/616 (73.1) | 199/253 (78.7) | 230/334 (68.9) | 0.008 |
| Sex (female), n (%) | 437/553 (79.0) | 199/247 (80.6) | 248/317 (78.2) | 0.46 |
| Age, mean (SD) | 46.1 (14.6) | 44.5 (14.9) | 47.4 (14.2) | 0.017 |
| Age group, n (%) | ||||
| <19 | 12/558 (2.2) | 6/244 (2.5) | 6/314 (1.9) | 0.112 |
| 20–29 | 63/558 (11.3) | 32/244 (13.1) | 31/314 (9.9) | |
| 30–39 | 106/558 (19.0) | 52/244 (21.3) | 54/314 (17.2) | |
| 40–49 | 139/558 (24.9) | 64/244 (26.2) | 75/314 (23.9) | |
| 50–59 | 127/558 (22.8) | 44/244 (18.0) | 83/314 (26.4) | |
| 60–69 | 83/558 (14.9) | 33/244 (13.5) | 50/314 (15.9) | |
| 70+ | 28/558 (5.0) | 13/244 (5.3) | 15/314 (4.8) | |
| Education, n (%) | ||||
| High school or less | 86/561 (15.3) | 31/247 (12.5) | 55/313 (17.6) | 0.035 |
| College | 110/561 (19.6) | 43/247 (17.4) | 67/313 (21.4) | |
| Apprenticeship | 33/561 (5.9) | 11/247 (4.5) | 22/313 (7.0) | |
| University degree | 177/561 (31.6) | 82/247 (33.2) | 95/313 (30.4) | |
| Postgraduate degree | 140/561 (25.0) | 75/247 (30.4) | 65/313 (20.8) | |
| Prefer not to answer | 15/561 (2.7) | 5/247 (2.0) | 9/313 (2.9) | |
| Income, n (%) | ||||
| <$30 000 | 35/566 (6.2) | 11/247 (4.5) | 24/318 (7.6) | 0.276 |
| $30 000–54 999 | 62/566 (11.0) | 24/247 (9.7) | 38/318 (12.0) | |
| $55 000–99 999 | 153/566 (27.0) | 68/247 (27.5) | 85/318 (26.7) | |
| ≥$100 000 | 216/566 (38.2) | 102/247 (41.3) | 114/318 (35.9) | |
| Prefer not to answer | 100/566 (17.7) | 42/247 (17.0) | 57/318 (17.9) | |
Bold text indicates signficance at alpha 0.05.
*Survey questions were not mandatory, and some participants did not provide a response to all questions.
†Includes patients who had COVID-19 less than 3 months ago and patients reporting no persistent symptoms.
LCS, long COVID syndrome.
Respondents reported experiencing on average 10 (SD 5.3) symptoms when they first had COVID-19. The most common COVID-19 symptoms reported by respondents were extreme fatigue (88.1%, 543 of 616), headaches (79.5%, 490 of 616), cough/noisy breathing (73.4%, 452 of 616) and general muscle weakness (72.1%, 444 of 616) (table 2). Respondents who experienced symptoms ≥3 months after infection had a greater number of symptoms during the initial COVID-19 infection (12 (SD4.4) vs 8 (SD 5.0), p<0.001). On average, respondents reported 10 (SD 5.4) symptoms lasting ≥3 months. The most common symptoms suggestive of LCS included extreme fatigue (79.6%, 266 of 334), issues with concentration, thinking and memory (76.6%, 256 of 334), shortness of breath with activity (65.3%, 218 of 334) and headaches (64.1%, 214 of 334) (table 2). Sixty-two per cent of respondents experiencing symptoms suggestive of LCS (209 of 334) reported symptoms that were severe enough to reduce work, school or other activities, and over 10% (34 of 334) required assistance with day-to-day activities (eg, walking, using the bathroom, bathing, changing, etc).
Table 2.
COVID-19 symptoms experienced by respondents
| Symptoms | COVID-19 symptoms N=616 |
Symptoms ≥3 months after infection n=334 |
| Extreme fatigue, n (%) | 543 (88.1) | 266 (79.6) |
| Headaches, n (%) | 490 (79.5) | 214 (64.1) |
| Cough/noisy breathing, n (%) | 452 (73.4) | 174 (52.1) |
| General muscle weakness, n (%) | 444 (72.1) | 191 (57.2) |
| Muscle or joint pain, n (%) | 435 (70.6) | 196 (58.7) |
| Shortness of breath with activity, n (%) | 402 (65.3) | 218 (65.3) |
| Issues with concentration, thinking and memory, n (%) | 395 (64.1) | 256 (76.6) |
| Issues with pain or discomfort, n (%) | 384 (62.3) | 174 (52.1) |
| Difficulty sleeping, n (%) | 320 (51.9) | 203 (60.8) |
| Anxiety, n (%) | 317 (51.5) | 205 (61.4) |
| Shortness of breath at rest, n (%) | 301 (48.9) | 156 (46.7) |
| Dizziness, faint, loss of consciousness, n (%) | 256 (41.6) | 164 (49.1) |
| Chest pain at activity, n (%) | 247 (40.1) | 137 (41.0) |
| Depression, n (%) | 247 (40.1) | 176 (52.7) |
| Chest pain at rest, n (%) | 224 (36.4) | 107 (32.0) |
| Difficulty eating, drinking and swallowing, n (%) | 215 (34.9) | 73 (21.8) |
| Difficulty walking, n (%) | 180 (29.2) | 103 (30.8) |
| Difficulty controlling movement of the body, n (%) | 130 (21.1) | 75 (22.5) |
| Other, n (%) | 190 (30.8) | 71 (21.3) |
| Change in taste and smell | 49 (8.0) | 24 (7.2) |
| Sore throat | 48 (7.8) | 8 (2.4) |
| Congestion | 31 (5.0) | <5 (<1.5) |
| Gastrointestinal symptoms | 30 (4.9) | 10 (3.0) |
| Runny nose | 27 (4.4) | <5 (<1.5) |
| Fever | 27 (4.4) | 0 |
| Rapid or irregular heart rate | 17 (2.8) | 16 (4.8) |
| Chills/night sweats | 13 (2.1) | <5 (<1.5) |
| Tinnitus and earache | 11 (1.8) | 82 (2.4) |
| Inflammation and numbness | 10 (1.6) | 17 (5.1) |
| Malaise | 9 (1.5) | 0 |
| Sore eyes and changes in vision | 8 (1.3) | 6 (1.8) |
| Rash | 7 (1.1) | 8 (2.4) |
Questions were not mandatory; not all respondents responded to each question.
Bold indicates most commonly reported symptoms.
Healthcare utilisation
Primary healthcare services were accessed by 43.0% (265 of 616) of respondents due to symptoms of COVID-19 or symptoms suggestive of LCS. There were 55.8% (148 of 265) of patients who indicated they saw their primary care provider for COVID-19 symptoms. The most common symptoms reported among these respondents were extreme fatigue (95.9%), headaches (92.6%), cough/noisy breathing (89.2%) and shortness of breath with activity (87.8%) (figures 1 and 2 and online supplemental material E).
Figure 1.
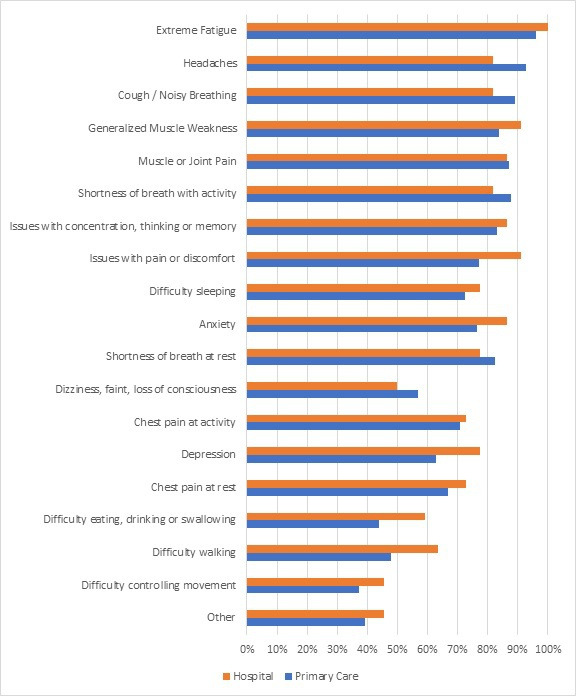
Respondents’ self-reported healthcare use for initial COVID-19 infection, by symptoms. Order of symptoms was determined by the percentage of symptoms experienced by respondents as outlined in table 2.
Figure 2.
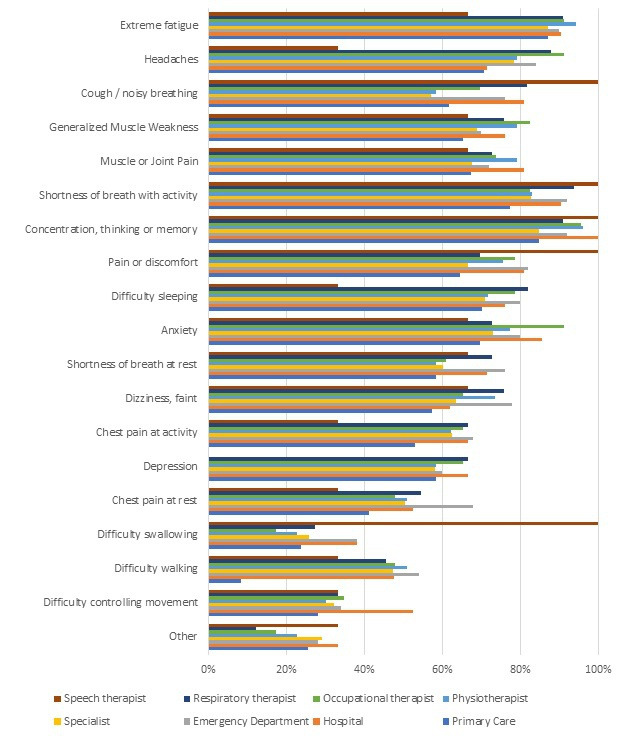
Respondents’ self-reported healthcare use for symptoms of long COVID syndrome, by symptoms. Order of symptoms was determined by the percentage of symptoms experienced by respondents as outlined in table 2.
bmjopen-2023-075301supp005.pdf (58.1KB, pdf)
Hospitalisation for COVID-19 was reported by 3.6% (22 of 616) of respondents; almost all of these patients (21 of 22) reported experiencing symptoms suggestive of LCS. Patients hospitalised reported chest pain (72.7% during COVID-19, 66.7% LCS), depression (77.3% during COVID-19, 66.7% LCS) and difficulty walking (63.6% during COVID-19, 47.6% LCS) (figures 1 and 2 and online supplemental material E).
Among participants who reported symptoms suggestive of LCS (n=334), there were 211 patients (66.2%) who sought primary care most commonly due to extreme fatigue (87.2%). There were 50 respondents (15.2%) who sought care at an emergency department and 107 respondents (32.0%) who saw a specialist or therapist due to symptoms suggestive of LCS. Symptoms are presented in table 2. The majority of respondents who saw a specialist or therapist for symptoms suggestive of LCS (89.7%, 96 of 107) reduced their work, school or activities due to persistent symptoms, and 20.6% required assistance with day-to-day activities.
There were 303 (49.2%) respondents who did not seek healthcare; of these, 95 patients reported experiencing symptoms ≥3 months after initial infection. The most common symptoms experienced during COVID-19 infection among respondents who did not seek healthcare services were extreme fatigue (88.4%, 268 of 303), headaches (80.2%, 243 of 303), cough and noisy breathing (71.3%, 216 of 303), and generalised muscle weakness (68.6%, 208 of 303). The majority (84.8%, 257 of 303) of participants who did not seek healthcare services for COVID-19 or symptoms suggestive of LCS indicated that they ‘did not need to’ because their symptoms were mild or there are no treatments available. Other reasons for not seeking healthcare services are listed in table 3.
Table 3.
Reasons for not seeking healthcare for COVID-19 or symptoms suggestive of LCS (N=303)
| Reason | N (%) |
| Did not need to (eg, mild symptoms, no treatment available, did not impact work) | 257 (84.8) |
| Personal difficulties (eg, too sick or weak, out of province, did not want to take more time off work) | 14 (4.6) |
| Healthcare access barriers (eg, no family doctor, difficulty making an appointment) | 15 (5.0) |
| Personal concerns (eg, would not be taken seriously, do not like the health system, system is overburdened and busy) | 8 (2.6) |
| Did not want to spread COVID-19 | 6 (2.0) |
| Uncertain if symptoms were COVID-19 or another condition | 5 (1.7) |
| Accessed other services (eg, called provincial telephone health support line, online support groups) | <5 |
Some respondents indicated more than one reason they did not seek healthcare.
LCS, long COVID syndrome.
Discussion
Since COVID-19 was first identified, national survey estimates suggest that almost one-third of Canadians have tested positive for COVID-19.1 Rates of both COVID-19 and LCS are expected to increase.1 3 8 9 A recent national survey reported that 14.8% of individuals who contracted COVID-19 experienced LCS.1 This is significantly lower than our less systematic province-specific survey, where 54.2% of respondents experienced symptoms lasting 3 or more months. Advertisement of our survey may have prompted people experiencing LCS to respond. Further, when compared with the Manitoba data in the Canadian Census, survey respondents were more likely to be female (78.4% vs 50.3%), live in an urban location (79.0% vs 55.9%), have a university degree (29.7% vs 21.1%) and self-report a higher annual household income.20 Similar to other studies, we found disease severity during the initial COVID-19 illness was associated with experiencing symptoms suggestive of LCS,1 12 13 16–18 21–23 particularly persistent physical and mental fatigue.18 Nasserie et al reported that independent of patient age, persistent COVID-19 symptoms were frequently reported among hospitalised patients.16 In our survey, respondents who reported hospitalisation or who experienced a greater number of symptoms during their initial COVID-19 infection were significantly more likely to have symptoms ≥3 months after initial infection. However, both populations with mild COVID-19 infection as well as those who did not use healthcare services still experienced symptoms suggestive of LCS. Research on COVID-19 typically recruits clinical cohorts. Our findings demonstrate that reliance on healthcare data to identify individuals experiencing LCS likely undercapture individuals experiencing symptoms suggestive of LCS.
Variation in symptoms of COVID-19 and LCS appears to have implications for the health system.16 Respondents who sought primary care experienced more respiratory symptoms, whereas respondents who visited the emergency department had more neurological symptoms, those who saw a specialist had more anxiety and rehabilitation services were more frequently accessed by patients reporting musculoskeletal concerns.1 16 17 Primary care providers are challenged to provide care to patients with a wide range of symptoms and with no diagnostic tests to confirm LCS.24 Consistent with literature, the most common COVID-19 symptoms reported in our study were extreme fatigue, cognitive dysfunction and shortness of breath.1 12 16–18 The majority of COVID-19 signs and symptoms, including those reported in our study, have poor diagnostic accuracy.21 25 Evidence suggests that only anosmia or ageusia may indicate specific COVID-19 infection21 25; however, anosmia or ageusia was infrequently reported by our respondents. Further, symptoms appear to fluctuate throughout the course of infection16 requiring healthcare services to be oriented according to stage of COVID-19 infection. In addition to symptom variation, little is known about effective treatments for LCS, which may contribute to infrequent referrals to specialists and therapists, and rehabilitation services are not always covered by health insurance plans. Additionally, there is mixed evidence on suggested treatments such as the role of vaccination in preventing or decreasing LCS.26 LCS clinics that comprised of interdisciplinary healthcare teams, currently available in some Canadian provinces, but not in Manitoba, provide comprehensive care to patients experiencing LCS who are unlikely to respond to a single intervention.9
LCS can significantly impact an individual’s physical function and health-related quality of life.12 16–18 Many individuals experience 10 or more symptoms suggestive of LCS including debilitating physical and mental fatigue and shortness of breath.12 16 23 Although respondents who sought healthcare reported a greater impact on their quality of life, even respondents who did not seek healthcare reported impacts on their day-to-day activities due to the symptoms suggestive of LCS. Multisystem LCS symptoms are often experienced for months resulting in significant impact on an individual’s lifestyle.12 Davis et al reported that 85.9% of participants with LCS experienced relapsing-remitting symptoms most commonly post-exertional malaise or cognitive dysfunction,12 which may contribute to activity limitations in this group. We found that respondents who did not seek healthcare felt that healthcare providers could not address their symptoms, or they reported uncertainty of the signs and symptoms of COVID-19 and LCS. Uncertainty in the signs and symptoms of COVID-19 and LCS and lack of appropriate referral pathways can hinder health service access, early diagnosis and potential treatment. Additionally, public health measures including a robust social safety net can provide adequate time for recovery and flexibility in activities as symptoms resolve.12
While the results of this study are not generalisable, they provide insight into experiences of individuals with symptoms suggestive of LCS and demonstrate that there is a significant population experiencing COVID-19 symptoms 3 months or more post-infection who do not seek healthcare. It is important to consider that those who chose to respond may have been different compared with those who did not respond, which may have contributed to a response bias. For example, asymptomatic patients, patients with mild symptoms or patients who did not experience LCS may have been less likely to participate. Similar to this study, other research suggests that women respond to surveys in greater proportion than men.27 Further, the retrospective nature of this study may have led to recall bias when reporting symptoms experienced and healthcare services sought. Recall bias may have led to both over-reporting and under-reporting of symptoms. Although this survey did provide the option to report additional symptoms experienced, we focused on key symptoms as reported in other literature. The survey was completed online requiring respondents to have access to a stable internet connection to complete the survey and therefore may have excluded populations who lacked access to the internet or have low digital literacy. Future research should explore the relationship between education and income in relation to experiencing symptoms suggestive of LCS with a larger sample size.
Conclusion
This study provides supplemental information available from health system use about experiences with COVID-19 and in particular LCS. The most frequent symptoms reported are consistent with the literature and reflect the multisystem nature of this condition. Health records capture a proportion of COVID-19 and LCS cases but could leave out a significant segment of the population who did not use health services, thus underestimating the burden of the problem. As symptoms suggestive of LCS continue and our understanding of LCS grows, we may see an increase in the supply of healthcare services offered to this group of patients. Understanding LCS and its symptoms can help providers promptly recognise and manage this condition. More specifically, understanding the relationship between symptoms and use of healthcare services can help identify the needs of patients with this condition. Furthermore, an understanding of the experiences of patients with LCS may inform knowledge translation activities, health system planning and resource allocation to address the needs of this growing group of patients.
Supplementary Material
Acknowledgments
The study team would like to acknowledge Alyzia Horsfall for her assistance in drafting and creating the online survey link, Lisa Labine for her assistance in drafting the survey, and Jennifer Pepneck, Samantha Prokopich and Catherine Campos for their assistance with survey dissemination and recruitment.
Footnotes
Twitter: @Leanne_kos, @Dr_DianaSanchez, @AlanKatz6
Contributors: LK, AK and DCS-R contributed substantially to conception and design of this study. LK prepared the survey, collected survey responses and conducted analyses. LK prepared the first draft of the manuscript. LK, AK and DCS-R assisted in interpreting the data and manuscript preparation. The authors read and approve the final manuscript. LK and AK, as guarantors, take responsibility for the finished work, had access to the data, and controlled the decision to publish.
Funding: This work was supported by grants from the Canadian Institutes of Health Research (award number: N/A) awarded to AK and from the Manitoba Lung Association (award number: N/A) awarded to DCS-R.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Aggregate survey data have been provided within the article and as online supplemental information. Individual-level anonymous survey data used in this study are available upon reasonable request and with appropriate approvals from the research team by emailing the corresponding author.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by the Health Research Ethics Board at the University of Manitoba (HS25090(H2021:279)). Information about the study was provided to participants prior to entering the survey (access online). Respondents were informed that continuing to complete the study was ‘implied consent’. This study did not collect any personal health information and there was no way to identify who completed the survey; therefore, our ethics board felt implied consent was sufficient.
References
- 1.Canada S. Long-term symptoms in Canadian adults who tested positive for COVID-19 or suspected an infection January 2020 to August 2022, . 2022Available: https://www150.statcan.gc.ca/n1/daily-quotidien/221017/dq221017b-eng.htm [Accessed Nov 2022].
- 2.WHO . Coronavirus disease (COVID-19). Access February 2023 from, Available: https://www.who.int/health-topics/coronavirus#tab=tab_1
- 3.van Kessel SAM, Olde Hartman TC, Lucassen PLBJ, et al. Post-acute and LCS-19 symptoms in patients with mild diseases: a systemic review. Fam Pract 2022;39:159–67. 10.1093/fampra/cmab076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . A clinical case definition of post COVID-19 conditin by A Delphi consensus, . 2021Available: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 [Accessed Feb 2023]. [DOI] [PMC free article] [PubMed]
- 5.Sykes DL, Holdsworth L, Jawad N, et al. Post-COVID-19 symptom burden: what is LCS and how should we manage it. Lung 2021;199:113–9. 10.1007/s00408-021-00423-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandler CX, Wyller VBB, Moss-Morris R, et al. LCS and post-infective fatigue syndrome: a review. Open Forum Infect Dis 2021;8:ofab440. 10.1093/ofid/ofab440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanchez-Ramirez DC, Normand K, Zhaoyun Y, et al. Long-term impact of COVID-19: a systematic review of the literature and meta-analysis. Biomedicines 2021;9:900. 10.3390/biomedicines9080900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McNaughton CD, Austin PC, Sivaswamy A, et al. Post-acute health care burden after SARS-Cov-2 infection: a retrospective cohort study. CMAJ 2022;194:E1368–76. 10.1503/cmaj.220728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenhalgh T, Knight M, A’Court C, et al. Management of post-acute COVID-19 in primary care. BMJ 2020;370:m3026. 10.1136/bmj.m3026 [DOI] [PubMed] [Google Scholar]
- 10.Tabacof L, Tosto-Mancuso J, Wood J, et al. Post-acute COVID-19 syndrome negatively impacts physical function, cognitive function, health-related quality of life, and participation. Am J Phys Med Rehabil 2022;101:48–52. 10.1097/PHM.0000000000001910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campos C, Prokopich S, Loewen H, et al. Long-term effect of COVID-19 on lung imaging and function, cardiorespiratory symptoms, fatigue, exercise capacity, and functional capacity in children and adolescents: a systematic review and meta-analysis. Healthcare (Basel) 2022;10:12.:2492. 10.3390/healthcare10122492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021;38:101019. 10.1016/j.eclinm.2021.101019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang Y, Pinto MD, Borelli JL, et al. COVID symptoms, symptom clusters, and predictors for becoming a long-Hauler looking for clarity in the haze of the pandemic. Clin Nurs Res 2022;31:1390–8. 10.1177/10547738221125632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manitoba . Quarterly Demographic Estimates, January . 2022Available: https://www.gov.mb.ca/mbs/publications/mbs305_pop_bulletin_2022_m01.pdf [Accessed Nov 2022].
- 15.Manitoba . Provincial Respiratory Surveillance Report: COVID-19, Available: https://www.gov.mb.ca/health/publichealth/surveillance/covid-19/index.html [Accessed Dec 2022].
- 16.Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systemic review. JAMA Netw Open 2021;4:e2111417. 10.1001/jamanetworkopen.2021.11417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Surapaneni KM, Singhal M, Saggu SR, et al. A Scoping review on long COVID-19: physiological and psychological symptoms post-Acture, long-post and persistent post COVID-19. Healthcare (Basel) 2022;10:2418. 10.3390/healthcare10122418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blomberg B, Mohn KG-I, Brokstad KA, et al. Long COVID in a prospective cohort of home-isolated patients. Nat Med 2021;27:1607–13. 10.1038/s41591-021-01433-3 Available: 10.1038/s41591-021-01433-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.University of Leeds, Sivan M, Halpin S, et al. Assessing long term rehabilitation needs in COVID-19 survivors using a telephone screening tool (C19-YRS tool). ACNR 2020;19:14–7. 10.47795/NELE5960 Available: [DOI] [Google Scholar]
- 20.Statistics Canada . Census profile. 2021 census of population. Statistics Canada catalogue No.98-316-X2021001.Ottawa. released March 29, 2023. 2023. Available: https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/index.cfm?Lang=E [Accessed 13 Apr 2023].
- 21.Matta J, Wiernik E, Robineau O, et al. Association of self-reported COVID-19 infection and SARS-Cov-2 Serology test results with persistent physical symptoms among French adults during the COVID-19 pandemic. JAMA Intern Med 2022;182:19–25. 10.1001/jamainternmed.2021.6454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan Sui Ko A, Candellier A, Mercier M, et al. Number of initial symptoms is more related to long COVID-19 than acute severity of infection: a prospective cohort of hospitalized patients. Int J Infect Dis 2022;118:220–3.:S1201-9712(22)00141-2. 10.1016/j.ijid.2022.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sudre CH, Murray B, Varsavsky T, et al. Attributes and Predicators of long COVID. Nat Med 2021;27:626–31. 10.1038/s41591-021-01292-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis HE, McCorkell L, Vogel JM, et al. Longcovid: major findings, mechanisms and recommendations. Nat Rev Microbiol 2023;21:133–46.:408. 10.1038/s41579-023-00896-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Struyf T, Deeks JJ, Dinnes J, et al. Signs and symptoms to determine if patient presenting in primary care or hospital outpatient settings has COVID-19. Cochrane Database Syst Rev 2021;2:CD013665. 10.1002/14651858.CD013665.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Notarte KI, Catahay JA, Velasco JV, et al. Impact of COVID-19 Vaccinations on the risk of developing long-COVID and on existing long-COVID symptoms: A systematic review. EClinicalMedicine 2022;53:101624. 10.1016/j.eclinm.2022.101624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kwak N, Radler B. A comparison between mail and web surveys: response pattern, respondent profile, and data quality. J Off Stat 2002;18:257–73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-075301supp001.pdf (121.9KB, pdf)
bmjopen-2023-075301supp002.pdf (74.6KB, pdf)
bmjopen-2023-075301supp003.pdf (81.7KB, pdf)
bmjopen-2023-075301supp004.pdf (246.8KB, pdf)
bmjopen-2023-075301supp005.pdf (58.1KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Aggregate survey data have been provided within the article and as online supplemental information. Individual-level anonymous survey data used in this study are available upon reasonable request and with appropriate approvals from the research team by emailing the corresponding author.


