Abstract
Introduction
Longitudinal studies can provide timely and accurate information to evaluate and inform COVID-19 control and mitigation strategies and future pandemic preparedness. The Optimise Study is a multidisciplinary research platform established in the Australian state of Victoria in September 2020 to collect epidemiological, social, psychological and behavioural data from priority populations. It aims to understand changing public attitudes, behaviours and experiences of COVID-19 and inform epidemic modelling and support responsive government policy.
Methods and analysis
This protocol paper describes the data collection procedures for the Optimise Study, an ongoing longitudinal cohort of ~1000 Victorian adults and their social networks. Participants are recruited using snowball sampling with a set of seeds and two waves of snowball recruitment. Seeds are purposively selected from priority groups, including recent COVID-19 cases and close contacts and people at heightened risk of infection and/or adverse outcomes of COVID-19 infection and/or public health measures. Participants complete a schedule of monthly quantitative surveys and daily diaries for up to 24 months, plus additional surveys annually for up to 48 months. Cohort participants are recruited for qualitative interviews at key time points to enable in-depth exploration of people’s lived experiences. Separately, community representatives are invited to participate in community engagement groups, which review and interpret research findings to inform policy and practice recommendations.
Ethics and dissemination
The Optimise longitudinal cohort and qualitative interviews are approved by the Alfred Hospital Human Research Ethics Committee (# 333/20). The Optimise Study CEG is approved by the La Trobe University Human Ethics Committee (# HEC20532). All participants provide informed verbal consent to enter the cohort, with additional consent provided prior to any of the sub studies. Study findings will be disseminated through public website (https://optimisecovid.com.au/study-findings/) and through peer-reviewed publications.
Trial registration number
Keywords: PUBLIC HEALTH, COVID-19, EPIDEMIOLOGIC STUDIES
Strengths and limitations of this study.
The Optimise Study is a longitudinal cohort of Victorian adults and their social networks (September 2020 to December 2024), where participants are followed for up to 24–48 months and data can be linked to map social connections.
It combines quantitative data collection with qualitative interviews and focus group discussions at key time points with purposively recruited cohort participants to capture in-depth information about opinions, attitudes and beliefs about and adoption of COVID-19 mitigation strategies.
The key study outcomes are timely empirical data on participants behaviours, attitudes and experiences of COVID-19 and government responses, from priority populations and identify factors that influence adoption of risk mitigation strategies.
It is a large social network study involving linked data from individuals and their social network in the form of contact diaries, to explore how social connection can influence attitudes and behaviours within networks and inform dynamic social network and transmission models.
Snowball sampling methods used for recruitment of social network data means that the study populations is not representative of the broader Victorian population.
Introduction
Since its emergence in late 2019, the SARS-CoV-2 (COVID-19) pandemic has caused substantial morbidity and mortality globally, with variants causing continuing waves of infection.1 In early 2020 Australia experienced its first wave of COVID-19 cases, which peaked at <1,000 cases/day in March-April 2020. COVID-19 cases in Australia then first declined in April 2020 after federal and state governments closed borders and introduced strict restrictions on population movement.2
Throughout 2020 and 2021, Australia experienced multiple, larger waves of infection concentrated in the states of Victoria and New South Wales, countered by COVID-19 mitigation strategies including case and contact identification and management (test, trace, isolate and quarantine) and vaccine rollout.3 Victoria, Australia’s second most populous state, was particularly affected, enduring multiple waves of infection and prolonged public health restrictions.4 Strategies included mandating masks in public indoor and outdoor settings to strict stay-at-home (‘lockdown’) orders, with people allowed to leave home for four reasons: to care for others, purchase groceries and medicine, exercise for an hour and perform essential work.5 Additional orders were closure of non-essential businesses, restriction of movement to within 5 km of home, curfews, domestic travel restrictions, border closures and mandatory hotel quarantine of returned travellers.6
Australia’s early public health responses to COVID-19 in 2020–2021 were successful, with fewer cases and deaths than most high-income Western countries throughout the first 2 years of the pandemic.7 This can be attributed to the strong and timely public health responses outlined above,8 high coverage of free COVID-19 testing through Australia’s universal health system, and implementation of high-volume PCR testing centres. Moreover, after an initially delayed vaccine roll-out,9–11 Australia achieved two-dose coverage of over 90% for people aged 12+ years by March 2022.12 Mathematical modelling has also informed the response.3 13–15 Ensuring models are parameterised with localised and real-time empirical data—both disease (eg, cases) and social (eg, estimated uptake of mitigation strategies) epidemiological data—has been critical to prediction accuracy and effective policies.
However, challenges remain. Since the Omicron variant emerged in Australia in December 2021, five distinct waves of transmission have occurred (>100,000 confirmed cases/week), 16 partly due to lower vaccine efficacy against newer variants, waning vaccine effectiveness, and diluted public health prevention strategies, increasing absenteeism and stress on hospital systems. 17 To 28 August 2022, 9 992 378 cases and 13 061 COVID-19-associated deaths were reported and 63 121 445 COVID-19 vaccine doses administered.18 Despite strict public health restrictions COVID-19 outbreaks occurred within ‘essential’ industries such as meat-processing factories and health and aged care settings.19–21 These outbreaks highlighted socioeconomic inequities, with many essential industries employing disadvantaged people such as migrant workers in low-wage positions on casual contracts.22 Many cannot work from home, have little or no sick leave, and eschew isolation or quarantine for fear of losing employment.23 Moreover, many migrant families and households live communally and share transportation, making physical distancing near impossible.24 The Victorian population is culturally and linguistically diverse (CALD), with 28% born overseas in more than 200 countries; another 21% have at least one parent born overseas. Twenty-six per cent speak a language other than English at home, including 3.2% Mandarin, 1.3% Arabic and 0.1% Dinka.25 Following early outbreaks of COVID-19 within Victorian African and Chinese communities and widespread media reporting,26 there arose concern about stigma towards these communities and the lack of culturally appropriate information.27 Collectively, these economic, behavioural and social factors increase risk of COVID-19 transmission among these and other priority populations. We refer to populations at heightened risk of COVID-19 transmission or illness as priority populations/groups; and understanding their transmission dynamics and social networks and predicting COVID-19 outbreaks to enable targeted support and resourcing is critical. Combatting new variants in coming years will require governments to respond rapidly to adaptive public health advice and sustain health system capacity. Crucially, future responses will occur in a context of community fatigue, related both to the disease and associated social restrictions. This will reduce government’s appetite and social licence to reintroduce mitigation policies and the community’s willingness to follow them, lowering their effectiveness. Government, public health officials and the community must balance the need to contain COVID-19 with the social, health and economic consequences of restrictions.
On 5 May 2023, WHO Director-General announced that given the disease was now well established and ongoing, COVID-19 no longer constituted a public health emergency of international concern. Globally, population-level immunity has increased significantly, due to vaccine uptake along with infection-induced immunity, or the combination of both (hybrid immunity). Countries have lifted most or all public health and social measures following significant reduction in rates of hospitalisation, admission to intensive care units and deaths across all age groups.28 29 While this health indicators clearly mark the end to a global emergency, the virus continues to spread and evolve and COVID-19 remains a threat, especially to older persons and adults with underlying health conditions. WHO has recently released a ‘Roadmap on uses of COVID-19 vaccines in the context of Omicron and high population immunity’30 which assumes that the virus will continue to evolve but cause less severe disease with possible surge in infections that will require booster doses to maintain protection in the high priority groups. High priority-use groups including older adults, other adults with multiple comorbidities that place them at risk of severe disease, were recommended to have additional booster doses 6–12 months after the last dose. Booster vaccine doses were also recommended for additional subpopulations with special considerations including people with severe immunocompromising conditions, pregnant adults/adolescents, health and care workers with direct contact with patients.
Understanding the experience and needs of high-priority groups, who may face additional barriers to accessing information and support, particularly around future vaccine boosters is vital. Moreover, determining how social relationships influence attitudes and behaviours within these communities, alongside other individual-level factors such as confidence in government and fear of COVID-19, can inform the development of culturally appropriate and effective information and support services.31 Given the rapid spread of information of COVID-19 through social media, it will be important to understand how perceptions and practices around COVID-19 could be influenced by social networks online both in Australia and internationally, and global news outlets.32 To inform ongoing COVID-19 control measures and help prevent harmful health consequences of COVID-19, including the growing burden of long COVID and the socioeconomic pressures of a prolonged pandemic, it is important to understand communities’ experiences, attitudes, behaviours and needs over time.
Objectives
The Optimise Study is a multidisciplinary research platform with four main objectives:
Collect empirical data (behaviours, attitudes and experiences of COVID-19 and government responses) from priority populations and identify factors that influence adoption of risk mitigation strategies.
Describe and monitor the unintended health, social and economic consequences of COVID-19 transmission prevention measures.
Collect empirical data on social contacts and mixing patterns, particularly for key priority groups, to inform dynamic social network and transmission models and explore how social connection influences attitudes and behaviours within networks.
Test the acceptability, feasibility and effectiveness of new and existing intervention strategies (diagnostic, therapeutic, behavioural and social) to guide the Australian Government’s COVID-19 response strategy.
Methods and analysis
The Optimise Study has three components:
A longitudinal cohort study of Victorian adults and their social networks (September 2020 to December 2024); participants’ are followed for up to 24–48 months and data can be linked to map social connections. In addition, brief snapshot surveys were introduced to gather rapid information about the acceptability of new policies and ongoing behaviours (September 2021 to August 2023).
Qualitative interviews and focus group discussions (FGDs) at key time points with purposively recruited cohort participants to capture in-depth information about opinions, attitudes and beliefs about and adoption of COVID-19 mitigation strategies.
Community engagement groups (CEGs), formed to interpret the cohort and qualitative interview research findings to inform recommendations for policy and practice.
Optimise Study collaborators implement additional substudies of specific priority populations to increase the breadth and depth of the findings. Information is reported frequently to governments and the community. We used the Standard Protocol Items: Recommendations for Interventional Trials reporting guidelines33 and details of Optimise Study registry information are detailed in online supplemental file 1 (table 1).
Table 1.
Seed participants by subgroups
| Target group | Target number of seed participants |
| Initial targets* | |
| Group 1 | |
| Recent COVID-19 cases | 30 |
| Group 2 | |
| Healthcare workers | 20 |
| Aged-care workers | 20 |
| High-risk workplace (factory/distribution workers) | 20 |
| People residing in regional centres | 30 |
| People with pre-existing chronic illnesses | 40 |
| People speaking a language other than English at home | 40 |
| Total | 200 |
| Additional targets* | |
| Group 1 | |
| Hotel quarantine workers | 20 |
| Group 2 | |
| People aged 18–24 | 20 |
| Arabic/Mandarin/Dinka (AMD)-speaking participants | 40 |
| Total | 80 |
*During 2021, young people and people working in hotel quarantine programmes emerged as groups with high COVID-19 incidence, so additional seed sets were added to the recruitment target. Recruitment targets for people who spoke AMD as their preferred language were added in response to concern about stigma towards African and Chinese communities and lack of culturally appropriate information.
bmjopen-2023-076907supp001.pdf (1.2MB, pdf)
Longitudinal cohort
Study design
The longitudinal cohort and social network study aims to recruit approximately 1000 Victorians. It involves social network analysis to inform responses to COVID-19, so uses snowball sampling for recruitment and collects data on the interactions and connections between participants to understand transfer of knowledge, attitudes and practices.34 35 It targets priority populations considered to be at risk of contracting COVID-19, developing severe COVID-19, experiencing negative impacts of government restrictions introduced to reduce COVID-19 transmission, or having difficulty understanding or following restrictions. ‘Seed’ participants are from selected priority populations, meaning the cohort does not represent the broader Victorian population.
Optimise recruits from two groups:
Group 1: people diagnosed with COVID-19 (within the past 7 days) or notified as ‘close contacts’ of a person with COVID-19.
Group 2: people not currently infected with COVID-19 but at heightened risk of infection and/or adverse outcomes of COVID-19 infection and/or public health measures (eg, worse employment conditions, housing or access to primary healthcare).
Over the study, participants complete 16 data collection tools at baseline (one key people nomination, one baseline survey, then 14 prospective daily diaries) then five data collection points each month (one monthly follow-up survey and four follow-up diaries), plus additional surveys if they test positive for COVID-19 or are a close contact.
Sampling and sample size
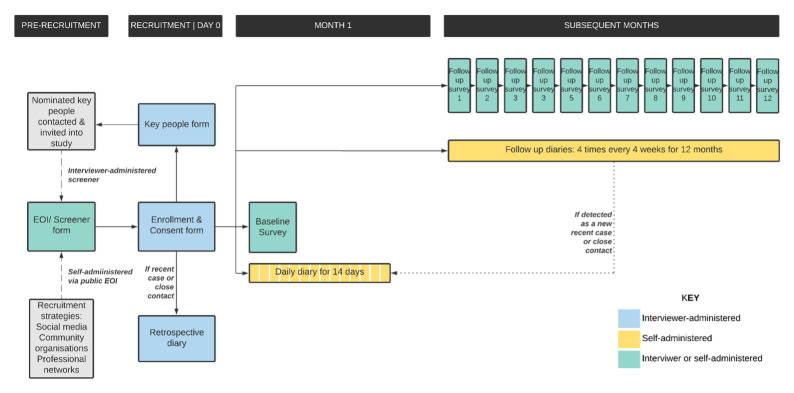
Snowball sampling was used to recruit individuals and their contacts. Seeds are sampled purposively from priority populations (layer 0) and asked to nominate people they consider ‘key’ in their day-to-day lives (meaning relatives, people with whom they live, discuss personal matters, give or receive practical support, interact frequently, and/or share hobbies or sport; ‘key people’ hereafter). Layer 0’s key people are recruited (layer 1 participants), and nominate their own key people (layer 2) (figure 1). Layer 2 participants are asked to nominate key people, for the purposes of social network analysis, but they are not recruited.
Figure 1.
Example of snowball recruitment for the Optimise Study.
The study aimed to recruit ~1000 participants, based on 200 seed participants and anticipating 1–2 key people recruited from each participant in layers 1 and 2. Sample size calculations were based on targets for priority groups. Layer 0 target numbers were revised as the study progressed to respond to pandemic dynamics and emerging priority populations, and because fewer key people (layers 1 and 2) were recruited than anticipated. Additional priority populations and targets were introduced throughout the follow-up period as the epidemiology evolved and new priority populations were identified. Priority populations and targets are shown in table 1. Definitions of priority populations, sampling strategies and COVID-19 case definitions are included in online supplemental file 1 (table 2).
Table 2.
Overview of data collection tools and scheduling
| Data collection tool | Participants | Administration | Expected time to complete (minutes) | Frequency | Schedule |
| Expression of interest/screener form | Layer 0 | Self | 5 | Once | Pre-recruitment |
| Layer 1 and 2 | Interviewer | 5 | Once | Day 0 | |
| Key people form (baseline) | All participants | Interviewer | 15 | Once | Day 0 |
| Retrospective diary | Participants classified as a recent COVID-19 case of close contact at recruitment | Interviewer | 15 | Once | Day 0 |
| Baseline surveys | All participants | Self or interviewer-administered | 30 | Once | Day 0–7 |
| Prospective daily diary | All participants | Self or interviewer-administered | 5–10 | Daily | Days 1–14 |
| Follow-up surveys | All participants | Self or interviewer-administered | 20 | Monthly | Every 4 weeks starting from week 5 |
| Key people form (follow-up) | All participants | Incorporated into follow-up surveys | N/A | Monthly | Repeated every 4 weeks |
| Follow-up diary | All participants | Self or interviewer-administered | 5–10 | 4 days/month | Starting from week 5 or directly after daily diary completed |
| COVID-19 event-based diaries | Participants classified as a recent COVID-19 case or close contact in diaries or surveys | Self or interviewer-administered | 5–10 | Trigged by event | Manually assigned at timepoint where the participant tests positive or is a household like contact |
| Snapshot surveys | All participants | Self or interviewer-administered | 5–10 | Ad hoc | September 2021 to August 2023 |
Participants
Participants are eligible if they are in a target group and meet the following inclusion criteria:
Aged ≥18 years.
Resident of Victoria, Australia.
Willing and able to provide informed consent to participate in a survey/interview over the phone in English, or in Arabic, Mandarin or Dinka (AMD) when a bilingual data collector is available.
Provide a valid email (Participants completing all tools by phone interview do not require an email address for study communications, but, if available it is recorded to assist with conflict resolution in social network analysis.) and phone number.
Have access to the internet to complete online surveys or a phone to undertake phone interviews.
Participants are excluded if they are:
In hospital or too unwell to participate at recruitment.
Not currently residing in Victoria.
Aged <18 years.
Recruitment
Seeds are recruited through paid and unpaid social media advertisements and flyers distributed via community and industry groups, community-based organisations and professional networks. Targeted social media advertisements reach priority groups based on age range, location, setting, gender and self-nominated interests (eg, health and social welfare). Advertisements and flyers direct potential participants to the study website, where they can submit an expression of interest (EOI).36 The EOI includes questions to categorise seeds and assess their eligibility (table 1).
In September 2021, specific recruitment and data collection strategies were developed to enable people born overseas or speaking a language other than English at home to participate.37 Trained bilingual data collectors from AMD-speaking communities were employed to support recruitment and data collection in participants’ languages. Data collectors use online advertisements, flyers and posters translated into AMD (with English). Flyers and posters are distributed to community service organisations and promoted on local AMD-language radio stations and social media platforms, including WeChat, Weibo and WhatsApp.
EOI forms translated into Arabic and simplified Chinese were available on the study website; Dinka is primarily a verbal language, so the EOI form is in English with some accompanying Dinka translation. Bilingual data collectors aimed to prioritise recruitment of participants who face additional barriers to accessing information and support during the COVID-19 pandemic. They used the following additional recruitment criteria: people with: low English proficiency, low technological proficiency (ie, could not self-complete surveys), have recently emigrated to Australia and are ineligible for government support.
When feasible, each participant is assigned a single data collector responsible for communication and follow-up to promote continuity and rapport. All potential participants receive an initial phone call from a data collector who explains the study, including its aims, procedures, participation requirements and reimbursements. When a potential participant expresses interest, the data collector administers the screening questions, confirms eligibility and records consent (see online supplemental file 2). Informed consents are provided by all participants to enter the cohort, collected verbally and documented in the study database, with additional consent provided prior to any of the substudies. Data collectors abandon recruitment after three unsuccessful contact attempts or if the study candidate declines.
Data collection procedures
We collect data across a broad range of domains, including sociodemographics, work and study circumstances, finances, health behaviours, access to services and information, social connectedness, mental health, knowledge of COVID-19, attitudes towards COVID-19 prevention measures and contact with people. Data collection follows a standardised and high-frequency procedure, including once-off surveys, baseline surveys and contact diaries, repeated monthly follow-up surveys, repeated weekly follow-up contact diaries, and COVID-19 event-based diaries. Recruitment into the longitudinal cohort commenced in September 2020 and closed in December 2021 when the target sample size was achieved. Once funding was secured to support recruitment of new priority populations, including from AMD-speaking communities, follow-up was extended and participants could complete up to 24 months of monthly follow-up surveys and diaries and annual surveys for up to 48 months to allow ongoing generation of data to inform public health policy (September 2020 to December 2024). In addition to the standardised longitudinal data collection, cross-sectional snapshot surveys were developed and deployed ad hoc across 2021–2023 to collect more in-depth data on participants’ behaviours and attitudes to new government policies and COVID-19 mitigation strategies.
Participants can withdraw from the study at any time by emailing the study team or sending an SMS. We unenrol participants who have not completed a baseline survey within 10 days of recruitment and are unresponsive to repeated follow-up attempts.
Baseline data collection
An interview guide for all data collection tools was translated into AMD through an accredited translation service and reviewed by our bilingual data collectors for cultural appropriateness. Following consent, participants complete a phone interview with a data collector who administers the key people form and asks participants to designate their preferred data collection method:
All tools are interviewer-administered by telephone in the relevant language.
Self-complete daily contact diaries and follow-up contact diaries in English, Mandarin and Arabic. Consent, key people, retrospective diary, baseline and follow-up surveys are administered over the phone with a bilingual data collector.
Participants who speak a language other than English at home and are fluent in English can self-complete all tools in English.
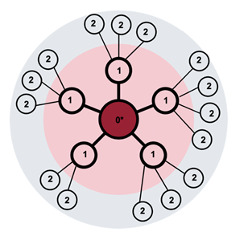
Participants are automatically assigned to the relevant data collection tools and subsequent schedule of surveys and diaries for the follow-up period (see figure 2 and table 2). For self-administered tools, the participant is sent a secure link by email and/or SMS (as preferred). Automated reminder emails or SMS are sent to participants with surveys due for completion each Monday at 08:00 am. For interviewer-administered tools, a data collector contacts participants when a survey or diary is due. Participants have 7 days to complete assigned tools before they expire. Up to three SMS, email and phone reminders prompt participants to complete baseline and follow-up surveys for interviewer-administered surveys. Individual reminders are not provided for daily diaries.
Figure 2.
Overview of standardised quantitative data collection tools and scheduling for a 12-month period*. *As recruitment was extended to include additional recruitment targets—the following up period was extended to a maximum of 24 months. EOI, expression of interest.
All participants complete a key people form during the baseline interview, allowing data collectors to target eligible individuals for recruitment. Participants can nominate a maximum of 50 key people all together, but a maximum of eight per participant are selected for attempted recruitment (layers 1 and 2). If the participant gives permission and contact details for more than eight key people, a key people with the most in-person contact, are prioritised for recruitment.
Participants then complete a baseline survey about demographics, impacts of COVID-19, baseline behaviours (including social, health and lifestyle factors) before the pandemic, and attitudes to, knowledge and uptake of COVID-19-related mitigation strategies. A baseline prospective daily diary is then completed online on days 1–14 after recruitment to collect information on participant’s health, isolation/quarantine status, mood and detailed data on their contacts on the previous day. For participants who complete the baseline diaries with the assistance of a data collector, instead of daily interviews, the diaries are completed across two interviews, with data collected retrospectively for the previous 7 days.
For participants who report testing COVID-19 positive or being a close contact in the 7 days before baseline (group 1), a retrospective diary is administered with interviewer assistance to establish a timeline of COVID-19 events and capture experiences of quarantine, isolation and adoption of public health directions.
Follow-up data collection
Follow-up commences 28 days after recruitment; all participants receive individualised links via email or SMS, or a phone call from a data collector, to complete a follow-up survey. The follow-up surveys collect the same content as the baseline surveys, but cover the previous 4 weeks. Follow-up surveys also ask participants about face-to-face and digital contact with key people in the previous 4 weeks and allow them to nominate new key people.
Participants are invited to complete four follow-up diaries in a month scheduled randomly for two weekdays and two weekend days to capture data on COVID-19 testing, COVID-related symptoms, being a ‘close contact’ in the previous 7 days, and information on mood and details of people with whom they interacted ‘yesterday’. The follow-up diaries are designed to assess social interactions, cooperation with government restrictions, and COVID-19-related health, and enable timely identification of COVID-19 diagnoses or close contacts and trigger a manual assignment of a COVID-19 event-based dairy (described below). After 12 months, all participants receive a message at the start of their next follow-up survey and follow-up diary congratulating them on their participation and informing them that the study is continuing. If they complete these tools, they are automatically assigned to another 12 months of follow-up surveys and diaries.
COVID-19 event-based diaries
If participants reported that they had tested positive for COVID-19 or are identified as a close contact in any of the monthly follow-up surveys or diaries, they are invited to complete an event-based diary to collect information on testing experience, health status, symptoms, disease severity and ability to complete their 7 days of isolation or quarantine. It also collects detailed data on personal interactions in the period starting 2 days before symptoms developed or they tested positive (whichever came first).
Snapshot surveys
To inform ongoing changes in Victorian Government policy during the pandemic, we design (on request, within 10 business days) and deploy ad hoc cross-sectional snapshot surveys to collect more in-depth data on participants’ opinions, behaviours and attitudes to new government policies and COVID-19 mitigation strategies. Distinct from the 24-month follow-up cohort schedule, snap-short surveys are deployed on an ad-hoc basis. All cohort participants are invited to complete a snapshot survey, self-completed and in English, within 7 days; meanwhile, bilingual data collectors administer 15 phone surveys in AMD.
Data collection tools
Data collection tools, their rationales and key domains are described below:
EOI/screen (see online supplemental file 3A): publicly available form to register interest in the study, assess study eligibility and key target recruitment group membership, collect contact details and preferences for data collector call-back.
Key people form (see online supplemental file 3B): collects data on key people to inform snowball recruitment, social network mapping and analysis of COVID-19 infection spread and social network influence on behaviours and attitudes. Based on previous social network analysis forms.38
Baseline retrospective daily diary (see online supplemental file 3C): collects data from participants recently diagnosed with COVID-19 and/or notified as a close contact in the previous 7 days. This interviewer-administered survey targets the timing and sequence of events surrounding COVID-19 transmission over the previous 14 days, including interactions with healthcare services and the Victorian Government COVID-19 contact tracing team, living arrangements, and isolation or quarantine. Data collected includes testing and diagnosis, potential exposure, and symptomatic period.
Baseline survey (see online supplemental file 3D): collects data (within 7 days of recruitment) on demographics; health and well-being; healthcare utilisation; COVID-related health and attitudes; vaccination attitude, uptake and barriers; and knowledge of and attitude to public health measures and restrictions. Questions on residence type, tenure and unpaid care and responsibilities follow the 2016 Census of Population and Housing.39 Occupation and industry questions follow the Australian and New Zealand Standard Industrial Classification, 2006.40 Financial hardship questions (eg, missing meals) follow the Household Expenditure Survey and Survey of Income and Housing 2009–2010. Social connectedness questions (eg, frequency of visiting friends) follow Dias et al.41 Long-term illness, age and disability questions follow the Australian Longitudinal Study on Women’s Health.42 Mental health was assessed by the Generalised Anxiety Disorder 7-item (GAD-7)43 and Personal Well-being Index-Adult.44 Questions about confidence in government agencies follow the 2019 Canterbury Well-being Survey.45
Baseline prospective daily diary (see online supplemental file 3E): collects data via self-administered online surveys every day for 14 days after recruitment and consent. Each diary asks about health (adapted from FluTracking),46 isolation/quarantine status, mood and personal interactions on the previous day. Data collected for each contact named includes details about the relationship, age and gender, location where contact occurred (inside/outside), purpose and duration of contact, and if physical contact occurred. If the participant cannot name all contacts due to high number, confidentiality or preference, they are asked to estimate the number of additional contacts per location.
Follow-up survey (see online supplemental file 3F): collects data every 4 weeks, starting from week 5. This survey includes the same domains as the baseline survey but targets current circumstances and changes in the previous 4 weeks to enable assessment of COVID-19 impacts and behaviours and attitudes.
Follow-up daily diary (see online supplemental file 3G): collects data for 2 weekdays and two weekend days every 4 weeks (average 1 day/week), starting from week 5. In addition to asking about contacts on the previous day, the follow-up diary elicits information on health, isolation and quarantine status in the previous 7 days. The 7-day recall enables detection of participants with new COVID-19 events, including diagnosis and notification as a close contact, and establish a timeline of related events. If new COVID-19 events are detected and confirmed with the participant (case or close contact), then the participant will be invited to complete a COVID-19 event-based diary.
COVID-19 event-based diary (see online supplemental file 3H): collects data from participants diagnosed with COVID-19 and/or notified as a close contact of a case during the follow-up period. They are manually assigned an event-based diary scheduled for 7 days after their date of diagnosis or notification of being a household contact. The diary captures participants’ health status and recent COVID-19 transmission or exposure information, including interaction with healthcare services and the Victorian Department of Health, living arrangements, and isolation or quarantine. Data collected includes testing and diagnosis, potential exposure, and symptomatic period.
Snapshot surveys (see online supplemental file 4A-F): collects data from participants at key time points in the epidemic to assess behaviours and attitudes to COVID-19 topics and government policies. Topics include behaviours over Summer 2021–2022, incentives and barriers to vaccination, concerns about children returning to school, influence of potential cessation of the Victorian pandemic declaration, impacts of long COVID, and COVID-19 testing, prevention and response in schools.
Reimbursement
Participants are reimbursed monthly for their efforts with electronic gift vouchers redeemable at major retailers. Initially, participants were reimbursed $A35 for the baseline survey and $15 if at least 10 (of 14) baseline prospective daily diaries were completed. For each month of follow-up, participants received $2.50 per follow-up daily diary and $25 per follow-up survey completed. Participants who test positive for COVID-19 or are a notified close contact are invited to complete an event-based diary each day for 14 days ($15). This was simplified in December 2020 to $50 for all recruitment and baseline data collection, $35 each month for completion if any follow-up was completed in that month (minimum one follow-up diary) and $15 for COVID-19 event-based diaries. If a participant is retained for 12 months, and completes a baseline and at least one follow-up survey a month, they are reimbursed $470. AMD-speaking participants are offered more flexible reimbursement methods (bank transfer or a mailed visa debit card) to overcome cultural and linguistic issues with electronic gift cards.
Data collection and management
To facilitate collection of social network data, we use NetCollect (V.2.1.94, SNA Toolbox), a purpose-built online data-capture platform.38 The software and data are hosted on the Burnet Institute’s local servers. NetCollect automatically sends survey links via email or SMS according to each participants’ data collection schedule, starting from date of consent. A data management plan and data dictionaries were developed and shared with all study collaborators. Quantitative data preparation, cleaning and analyses are conducted using R V.4.1.2.47 Data cleaning and analysis code is stored in Git for version control. Survey and network data are automatically extracted every fortnight via an application programming interface. To ensure timely identified of new COVID-19 cases and close contacts across the following period, NetCollect was programmed to notify Slack (a data communication platform) of notifications from survey responses. Slack prompts a data collector to contact the participant and invite them to complete retrospective diaries.
Data preparation for social network analysis
NetCollect offers data matching algorithms to identify and eliminate duplicate contact nominations within a person’s social networks. This conflict resolution process involves reviewing all study participants, key people and daily contacts for similarities in name and other characteristics and identifying probable matches according to specific rules. From this, Optimise and Swinburne University of Technology Social Network Research Lab study researchers review and verify matches manually through a separate algorithm. Multiple nominations of one individual are combined into a single record that contains all network information. Data analytics capacity is currently being integrated into NetCollect to support social network exploration and visualisation without data export to third-party software.
Data analysis and key outcomes
Each month the study executive identifies a topic for reporting, which informs the selection of key outcomes of interest. The topic is often related to a critical issue affecting the community and/or a government decision, such as a testing uptake, and acceptance of public health restrictions or a new vaccine roll-out. These topics inform the qualitative interviews and CEG discussions.
Data from the longitudinal surveys and diaries are analysed with respect to six focus areas:
Uptake of COVID-19 risk mitigation strategies including isolation, quarantine, vaccines, mask wearing, physically distancing.
Knowledge of COVID-19 restrictions and confidence in government decision-making.
Average number of contacts with key people per day and in different settings.
Changes in work and finances due to COVID-19 pandemic restrictions.
Changes in lifestyle and social engagement due to COVID-19.
Changes in physical and mental health due to COVID-19.
For monthly reporting, a specific relevant topic from the focus areas is selected and we report on key outcomes from each month:
What proportions of people are adopting risk mitigation strategies and are they experiencing any unintended health/financial/well-being consequences?
Do sociodemographic covariates influence adoption of risk mitigation strategies and experience of unintended health/financial/well-being consequences?
Does adoption of risk mitigation strategies and experience of unintended health/financial/well-being consequences vary over time?
Ordinal, nominal and binary data are summarised using frequencies and proportions for serial cross-sectional data. χ2 tests assess dependencies between survey responses for key outcomes and demographic variables, including gender, age group, employment status, healthcare worker status, if they have children (specifically in relation to vaccine uptake), country of birth, language spoken at home and household income. Continuous outcomes are assessed using mean, median and quantiles. T-tests and Wilcoxon tests are used to detect differences between demographic groups. Composite variables are formed as appropriate and any standard scales (ie, GAD-7 and Personal Well-being Index) are assessed using standard methodology.43 44 Missing data are assessed for causes (ie, missing completely at random, missing at random and missing not at random) and handled using multiple imputation or full information direct maximum likelihood if appropriate.
MPNet V.1.0448 is used for the statistical analysis of social network data using exponential random graph models and auto-logistic actor attribute models. This approach is used to consider whether individual mental health, vaccination attitudes and other characteristics are linked to specific network substructures in which individuals are embedded.
Qualitative interviews and focus groups
Study population and recruitment
Approximately 40 cohort participants are purposively sampled and recruited for in-depth interviews (n=25) and two FGDs (n=15) annually to capture experiences in different restriction periods and COVID-19 epidemic contexts. Participants invited to participate in a qualitative interview or FGD are sent an additional participant information and consent form; verbal consent is obtained before interview or FGD commencement and documented in a consent database.
Qualitative data collection tools and key measures
Interviews and FGDs are conducted by Zoom or telephone (interview only) and last approximately 1 hour. They are facilitated by an experienced qualitative researcher using a semi-structured guides (online supplemental file 5A-C) that evolve in line with changes in the COVID-19 context, trends identified in the quantitative data, and/or changes in state and federal government COVID-19 responses. Interview and FGD participants receive a $50 electronic gift voucher as reimbursement.
Data collection and management
Qualitative interviews and FGDs are audio-recorded and data transcribed verbatim by an external transcription service within 2 weeks. Audio files and transcripts are stored on a secure Burnet Institute server. Following transcription, the audio files are destroyed. De-identified transcripts and baseline demographic data are uploaded to a central NVivo (V.10) file49 stored securely on a Burnet Institute server.
Data analysis and key outcomes
Qualitative analysis has preliminary, rapid and in-depth components. For preliminary analysis, interviewers complete a participant template following an interview to provide a high-level summary and initial reflections based on audio recordings. For rapid analysis, interviewers spend approximately 1 hour coding transcripts using NVivo,49 applying pre-set coded themes and coding emerging themes. A summary of findings informs recommendations for policy and practice in monthly reports to the Victorian Government. In-depth inductive analyses, undertaken by members of the qualitative research team, identify new themes that are then aligned with existing evidence on COVID-19 and broader related community, health and resilience topics.
Community engagement groups
Study population and recruitment
To augment the longitudinal data, the CEGs provide interpretation of the cohort findings, generate new research topics/questions and assist in developing recommendations in response to these findings for government reports. The initial CEG comprised representatives of populations prioritised in the Optimise cohort (not participants): healthcare workers, international students, older people, people with chronic disease, young people, people who have had COVID-19, people living in regional Victoria and people living in crisis accommodation.
In September 2021, as additional target groups were added to the cohort, a CALD CEG was recruited to better represent the needs of multicultural (including Afghan, Fijian and Pasifika, Indian and South Asian) communities. Recruitment for both CEGs occurred through community leaders, representatives of community organisations and referrals through exiting organisational research networks.
CEG data collection tools and key measures
CEG teleconferences are held monthly with up to 10 participants per meeting. The topic under discussion is informed by the key issue identified for reporting in the monthly report provided to government (for more detail on topic guides see online supplemental file 6). A draft of the monthly Optimise report is provided to the CEG a week in advance of the meeting with the meeting agenda.
Each CEG meeting lasts approximately 90 min. Participants give their perceptions of the implications of the monthly report findings for their communities and their recommendations for government messaging or pandemic response.
CEG members receive a stipend of $112.50/meeting for their participation (including preparation time), paid as a digital gift voucher.
Data collection and management
Each CEG meeting is audio-recorded, detailed notes are taken and key quotations are transcribed by study researchers. Identifying information is redacted or concealed with pseudonyms. The digital records are stored on a password-protected La Trobe University network drive accessible only to study researchers.
Data analysis and key outcomes
CEG meeting data is analysed using framework thematic analysis, and summary notes of the discussion are circulated to members for approval. The CEG findings are then incorporated into the monthly Optimise report provided to the Victorian Government. Outcomes include:
Reflections on the monthly report findings based on personal experience and community insights.
Perceived implications of the findings for their communities.
Recommendations for government messaging or pandemic response.
Patient and public involvement
We piloted the study tools on a small group of COVID-19 patients and members of the public before recruitment began. Extensive consultation with bilingual data collectors was undertaken to inform translations of all study tools and adaptation of the study design for people unable to participate in English. Community representatives are invited to participate in CEGs, which review study findings and interpret research findings to inform policy and practice recommendations.
Ethics and dissemination
Ethical considerations
The Optimise longitudinal cohort and qualitative interviews are approved by the Alfred Hospital Human Research Ethics Committee (# 333/20). The Optimise Study CEG is approved by the La Trobe University Human Ethics Committee (# HEC20532). All participants provided informed verbal consent to enter the cohort, which is documented in the study database, with additional consent provided prior to any of the substudies. The Optimise Study involves collecting personal and identifiable data for social network analysis, participant follow-up and reimbursement. A distress protocol was developed to manage any participant who indicates significant distress or thoughts of self-harm or suicide during an interview, and a list of support services is offered after baseline and follow-up surveys. Data is treated confidentially with access restricted to the study team. Additional security measures and access restrictions apply to participant contact information for reimbursements. All participants and nominated contacts are automatically assigned a unique identification number. Deidentified data is extracted for data analysis from NetCollect using only the unique identifier and is only available to authorised study staff and collaborators. Identifiable data is extracted by the data management team and utilised by authorised staff for follow-up contact with participants, network data linkage and reimbursements. Data used for quality assurance, reporting and analysis is re-identifiable and is stored on a secure server at the Burnet Institute. Non-identifiable data is retained for 7 years.
Publication and dissemination
Reports are published on a public website: https://optimisecovid.com.au/study-findings/. Seventeen monthly reports and four special issue snapshot reports have been developed to date, on thematic topics including testing and strategies to improve uptake; vaccine confidence and preparedness; social networks and mixing patterns; gendered impacts of COVID-19; impact on income and finances, and impact of government restrictions on risk mitigation strategies; school-based testing; reimbursement for vaccination; and impact of COVID on CALD communities. Publications related to the Optimise Study and any substudies that are prepared and submitted to peer-reviewed journals.37 50–53
Study status
Recruitment into the longitudinal cohort component occurred from September 2020 to December 2021, with 24 months of follow-up. Monthly longitudinal surveys ceased in August 2022, after which data collection shifted to annual follow-up periods until December 2024. Data collection through qualitative FGDs, CEGs and snapshot surveys continued, with the most recent snapshot survey deployed in December 2022 to January 2023. Low COVID-19 case numbers in Victoria in 2020 and much of 202154 meant that recruitment of recent COVID-19 cases and close contacts into group 1 was limited, but recruitment into group 2 met or exceeded most recruitment targets (table 3). A total of 779 participants were recruited and completed a baseline survey and contributed to the longitudinal cohort between September 2020 and August 2022, of which 651 were still active in August 2022.
Table 3.
Active cohort participants, August 2022
| Total | ||
| n | % | |
| Total | 651 | 100 |
| Age | ||
| 15–24 | 99 | 15.3 |
| 25–34 | 131 | 20.2 |
| 34–44 | 105 | 16.2 |
| 45–54 | 108 | 16.7 |
| 55–64 | 115 | 17.7 |
| 64 | 90 | 13.8 |
| Sex | ||
| Male | 166 | 25.5 |
| Female | 484 | 74.3 |
| Other | 1 | 0.2 |
| Aboriginal or Torres Strait Islander | ||
| Yes | 3 | 0.5 |
| No | 648 | 99.5 |
| Country of birth | ||
| Australia | 417 | 64.1 |
| Other | 234 | 35.9 |
| Language spoken at home | ||
| English | 532 | 81.7 |
| Language other than English (LOTE) | 119 | 18.3 |
| LOTE spoken at home (top 3) | 119 | |
| Arabic | 32 | 26.9 |
| Mandarin | 32 | 26.9 |
| Hindi or Urdu | 11 | 9.2 |
| Group 1 target population | ||
| Recent COVID-19 case | 9 | 1.4 |
| Close contact | 17 | 2.6 |
| Quarantine worker | 29 | 7.6 |
| Group 2 target population* | ||
| Pre-existing chronic health condition | 170 | 26.3 |
| Aged care worker | 31 | 4.8 |
| Healthcare worker | 117 | 18.1 |
| Regional Victoria | 116 | 18.0 |
| High-risk workplace† | 31 | 4.8 |
| Culturally and linguistically diverse recruited through bilingual data collectors‡ | 71 | 10.7 |
| Arabic | 33 | 47.1 |
| Chinese | 29 | 41.4 |
| Dinka | 8 | 11.4 |
| Young people | 93 | 14.7 |
| Recruitment layer | ||
| 0 | 372 | 57.1 |
| 1 | 171 | 26.3 |
| 2 | 105 | 16.1 |
| 3§ | 2 | 0.3 |
| 4§ | 1 | 0.2 |
*Based on screener survey. Categories are not mutually exclusive and percentage does not total 100%.
†Includes factory, distribution and meat work settings.
‡Based on reporting speaking a LOTE at home or identifying as Aboriginal and/or Torres Strait Islander.
§Individuals that are nominated by layer 2 or layer 3 participants and had already been recruited into the study, are classified as layer 3 and 4.
As of August 2022, the Optimise Study had collected data from 712 participants; 651 participants remain active (table 3) and 51 participants have withdrawn.
Seven rapid snapshot surveys were deployed between September 2021 and January 2023. The August 2022 snapshot survey examined the frequency and impacts of long COVID; of 653 participants invited to complete the survey, 499 (76%) responded and almost half (243/499) of participants had been infected with COVID-19 at least once since the beginning of the pandemic (December 2019). Twenty-four semi-structured qualitative interviews have been conducted (7 in December 2020, 17 over May to June 2021), contributing to monthly reports. Three FGDs were held in July 2022 (n=20), targeting participants who reported having long COVID and generating insights into the snapshot survey reports. Seven CEG members were recruited in January 2021. They participated in 10 CEGs between February and November 2021, contributing to monthly reports. Twelve CALD CEG members were recruited in September 2021, and contributed to two CALD CEGs between September and October 2021. The two CEGs were combined and another four CEG meetings held between March and September 2022 to provide insights into the snapshot surveys.
Discussion
The is one of the largest social networks study conducted in Australia. Our baseline recruitment data demonstrates high willingness to engage in a complex, data-intensive longitudinal study of COVID-19. Localised and timely data collection is imperative for informing public health policy that is both community-centred and evidence-led. The Optimise platform provides empirical and timely information about key populations at risk of contracting COVID-19 and/or experiencing negative impacts of associated government restrictions. The frequent and detailed information being collected by the Optimise Study improves understanding of the economic and social barriers faced by priority populations. However, this study has some limitations that are important to consider. The social network study design meant seed participants were recruited from priority groups, therefore, the Optimise sample was not intended to be representative of the general population of Victoria. The snowball recruitment methodology and oversampling of key groups was by design and should be considered a strength of the study, as it can increase statistical power to detect differences in the outcomes between these groups. However, it does limit generalisability. Finally, due to low case numbers in Victoria in 2020 and much of 202154 the initial target to recruit participants into group 1 (COVID-19 cases and close contacts) was limited.
To date, the Optimise platform has generated 17 briefing reports and 8 publications, which have directly informed the Victorian Government’s COVID-19 policy and practice.8 14 15 37 50–53 It informs responsive government policy that is more likely to be accepted and adhered to because it reflects community values, attitudes and motivations.55–57 It also provides unique and detailed information about social contacts and mixing patterns to shape transmission models, and insights into how social connectedness influences behaviours, attitudes and perceptions.
Supplementary Material
Acknowledgments
Optimise is a partnership between the Burnet Institute and Peter Doherty Institute in collaboration with The University of Melbourne, Swinburne University, La Trobe University, Monash University, Victorian Department of Health and Human Services, Centre for Culture Ethnicity and Health, Health Issues Centre, Royal Children’s Hospital and Independent Multicultural Consultant. The authors gratefully acknowledge the generosity of the community members who participated in the study. The authors appreciatively acknowledge the work of all Optimise project team members and collaborators who have contributed to the ongoing delivery of the study. The authors acknowledge the contributions of the following people to this work: Stephanie Franet, Hellen Kibowen, Nick Dalziel (project staff), Amanda Rotberg (development of figures), Campbell Aitken (manuscript editing).
Footnotes
Twitter: @edwinkwong7, @CarolineHomer, @axcollie
Collaborators: Optimise is a partnership between the Burnet Institute and Peter Doherty Institute in collaboration with The University of Melbourne, Swinburne University, La Trobe University, Monash University, Victorian Department of Health and Human Services, Centre for Culture Ethnicity and Health, Health Issues Centre, Royal Children’s Hospital and Independent Multicultural Consultant. Members of the Advisory Committee provided initial input to study outcomes: Professor Allen Cheng, Professor Sally Green, Professor David Anderson, Dr Karen Block, Professor Nancy Baxter, Ms Ali Coelho, Professor Sophie Hill, Professor Jodie McVernon, Dr Lena Sanci, Dr Brett Sutton, Mr Danny Vadasz.
Contributors: AP, SF-L, LG, SH, NS, DL, MAS, KB, MH led the development of overall study design, data collection tools, oversight of the study and write-up of manuscript. AB, KH, AT, AW, SF-L, FS, BM, JO, AA, SC, TN, LN, KY, PK, DO, EJLK, MVC, RR, FS, JSD, NM, MD, AC and JK contributed to the study design, development of data collection tools, data collection, management and analysis. LG, AD, CH, SM, KB, DH, JW contributed to development of qualitative data tools and study design. SH, BM, RR, AP, FS, RP and DV contributed to development of community engagement groups and analysis of social media data. NS, NG, AA, AP, AB, MH and DL contributed to development of modelling questions and contact diaries design. AH, PW, GRPS, GR, CG, PM, BR, MAK, JC, CB and JK contributed to development of social network collection tools, study design and analysis. SF-L, AC, AT, KY, PK, DO, EJLK, MVC, TK, YZ, LE, AA-Q, DM and LG contributed to tailoring the methodology for inclusion of CALD participants, and overseeing translation of tools into three community languages. All authors contributed to study design, provided editorial comments and feedback and approved the final manuscript. The Optimise Executive Committee, comprised AP, SF-L, LG, SH, NS, DL, MS, KB and MH, directed and oversaw the study.
Funding: Optimise received funding support from the Victorian Government Department of Jobs, Precincts and Regions, the Victorian Department of Health, the Macquarie Group Foundation and Burnet Institute donors. The authors gratefully acknowledge the contribution to this work of the Victorian Operational Infrastructure Support Program received by the Burnet Institute. MH receives funding support from a National Health and Medical Research Council Investigator grant.
Competing interests: Burnet Institute has received investigator initiated clinical research funding form Gilead Sciences, AbbVie and Merck unrelated to this grant.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel Coronavirus (COVID-19). Int J Surg 2020;76:71–6. 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price DJ, Shearer FM, Meehan MT, et al. Early analysis of the Australian COVID-19 epidemic. Elife 2020;9:e58785. 10.7554/eLife.58785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stuart RM, Abeysuriya RG, Kerr CC, et al. Role of masks, testing and contact tracing in preventing COVID-19 Resurgences: a case study from New South Wales, Australia. BMJ Open 2021;11:e045941. 10.1136/bmjopen-2020-045941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saul A, Scott N, Spelman T, et al. The impact of three progressively introduced interventions on second wave daily COVID-19 case numbers in Melbourne, Australia. BMC Infect Dis 2022;22:514. 10.1186/s12879-022-07502-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manipis K, Street D, Cronin P, et al. Exploring the trade-off between economic and health outcomes during a pandemic: a discrete choice experiment of lockdown policies in Australia. Patient 2021;14:359–71. 10.1007/s40271-021-00503-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Victorian Department of Health and Human Services . Updates about the outbreak of the Coronavirus disease (COVID-19). 2021. Available: https://www.dhhs.vic.gov.au/coronavirus/updates
- 7.Pifarré i Arolas H, Acosta E, López-Casasnovas G, et al. Years of life lost to COVID-19 in 81 countries. Sci Rep 2021;11. 10.1038/s41598-021-83040-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saul A, Scott N, Crabb BS, et al. Impact of Victoria’s stage 3 lockdown on COVID-19 case numbers. Med J Aust 2020;213:494–496. 10.5694/mja2.50872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faasse K, Newby J. Public perceptions of COVID-19 in Australia: perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Front Psychol 2020;11:551004. 10.3389/fpsyg.2020.551004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacIntyre CR, Costantino V, Trent M. Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine 2022;40:2506–13. 10.1016/j.vaccine.2021.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trent M, Seale H, Chughtai AA, et al. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: a comparative survey of five large cities in the United States, United kingdom, and Australia. Vaccine 2022;40:2498–505. 10.1016/j.vaccine.2021.06.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Australian Government . COVID-19 vaccination – Sa3 geographic vaccination rates. 2021. Available: https://www.health.gov.au/sites/default/files/documents/2022/06/covid-19-vaccination-geographic-vaccination-rates-sa3-14-june-2022.pdf
- 13.Kerr CC, Stuart RM, Mistry D, et al. Covasim: an agent-based model of COVID-19 dynamics and interventions. PLoS Comput Biol 2021;17:e1009149. 10.1371/journal.pcbi.1009149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scott N, Palmer A, Delport D, et al. Modelling the impact of relaxing COVID-19 control measures during a period of low viral transmission. Med J Aust 2021;214:79–83. 10.5694/mja2.50845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scott N, Saul A, Spelman T, et al. The introduction of a mandatory mask policy was associated with significantly reduced COVID-19 cases in a major metropolitan city. PLoS One 2021;16:e0253510. 10.1371/journal.pone.0253510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Australian Government, Department of Health and Aged Care. COVID-19 Australia: epidemiology report 79; 2023. Commun dis Intell (2018) 10.33321/cdi.2023.47.72 [DOI]
- 17.Liu B, Stepien S, Dobbins T, et al. Effectiveness of COVID-19 vaccination against COVID-19 specific and all-cause mortality in older Australians: a population based study. Lancet Reg Health West Pac 2023;40:100928.:100928. 10.1016/j.lanwpc.2023.100928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Australian Government DoHaAC . COVID-19 Australia: epidemiology report 65 communicable diseases intelligence. 2022: 46. [Google Scholar]
- 19.COVID-19 outbreaks at meat plants: lessons from Victoria’s second wave, the FAIRR initiative. 2020. Available: https://www.fairr.org/news-events/insights/covid-19-outbreaks-at-meat-plants-lessons-from-victorian-second-wave
- 20.Quigley A, Stone H, Nguyen PY, et al. COVID-19 outbreaks in aged-care facilities in Australia. Influenza Other Respir Viruses 2022;16:429–37. 10.1111/irv.12942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCaffery KJ, Dodd RH, Cvejic E, et al. Health literacy and disparities in COVID-19-related knowledge, attitudes, beliefs and behaviours in Australia. Public Health Res Pract 2020;30:30342012. 10.17061/phrp30342012 [DOI] [PubMed] [Google Scholar]
- 22.Sidik SM. How COVID has deepened inequality - in six stark graphics. Nature 2022;606:638–9. 10.1038/d41586-022-01647-6 [DOI] [PubMed] [Google Scholar]
- 23.Reid A, Rhonda-Perez E, Schenker MB. Migrant workers, essential work, and COVID-19. Am J Ind Med 2021;64:73–7. 10.1002/ajim.23209 [DOI] [PubMed] [Google Scholar]
- 24.Wright CF, Clibborn S. COVID-19 and the policy-induced vulnerabilities of temporary migrant workers in Australia. Journal of Australian Political Economy 2020:62–70. [Google Scholar]
- 25.Victorian Multicultural Commission . Annual report 2020-21. State of Victoria, Australia: Victorian Multicultural Commission, 2021. [Google Scholar]
- 26.Fowler M, Booker C. Anger at hard lockdown for towers without confirmed virus cases. The Age 2020. [Google Scholar]
- 27.Silva DS. COVID-19 in the public housing towers of Melbourne: upholding social justice when invoking precaution. Aust N Z J Public Health 2020;44:430. 10.1111/1753-6405.13041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Otto M, Britton PN, Serpa Neto A, et al. COVID-19 related ICU admissions in Paediatric and young adult patients in Australia: a national case series 2020-2022. Lancet Reg Health West Pac 2023;36:100763. 10.1016/j.lanwpc.2023.100763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katikireddi SV, Cerqueira-Silva T, Vasileiou E, et al. Two-dose ChAdOx1 nCoV-19 vaccine protection against COVID-19 hospital admissions and deaths over time: a retrospective, population-based cohort study in Scotland and Brazil. Lancet 2022;399:25–35. 10.1016/S0140-6736(21)02754-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization . WHO SAGE Roadmap for prioritizing uses of COVID-19 vaccines: An approach to optimize the global impact of COVID-19 vaccines, based on public health goals, global and national equity, and vaccine access and coverage scenarios. REFERENCE NUMBER: WHO/2019-nCoV/Vaccines/SAGE/Prioritization/2023.1. Geneva: WHO, 2023. [Google Scholar]
- 31.Danchin M, Biezen R, Manski-Nankervis JA, et al. Preparing the public for COVID-19 vaccines: how can general practitioners build vaccine confidence and optimise uptake for themselves and their patients Aust J Gen Pract 2020;49:625–9. 10.31128/AJGP-08-20-5559 [DOI] [PubMed] [Google Scholar]
- 32.Schmelz K, Bowles S. Overcoming COVID-19 vaccination resistance when alternative policies affect the dynamics of conformism, social norms, and crowding out. Proc Natl Acad Sci U S A 2021;118:e2104912118. 10.1073/pnas.2104912118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krackhardt D. The strength of strong ties: The importance of philos in organizations. Boston: Harvard University Press, 1992. [Google Scholar]
- 35.Granovetter MS. The strength of weak ties. Am J Soc 1973;78:1360–80. 10.1086/225469 [DOI] [Google Scholar]
- 36.The Optimise study: optimising isolation QDfC. n.d. Available: https://optimisecovid.com.au/
- 37.Gibbs L, Thomas AJ, Coelho A, et al. Inclusion of cultural and linguistic diversity in COVID-19 public health research: research design adaptations to seek different perspectives in Victoria, Australia. Int J Environ Res Public Health 2023;20:2320. 10.3390/ijerph20032320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SNA Toolbox . Netcollect. Survey software for social network data collection. 2022. Available: https://www.snatoolbox.com/
- 39.Australian and New Zealand standard Indus classification (ANZSIC). n.d. Available: https://www.abs.gov.au/ausstats/abs@.nsf/mf/1292.0
- 40.Australian Bureau of Statistics . Household expenditure survey and survey of income and housing UG, Australia, 2009-10. n.d. Available: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/6503.02009-10
- 41.Dias A, Geard N, Campbell PT, et al. Quantity or quality? Assessing relationships between perceived social connectedness and recorded encounters. PLoS One 2018;13:e0208083. 10.1371/journal.pone.0208083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.2015 WsHAALSoWSH. 2015. Available: https://alswh.org.au/for-data-users/data-documentation/surveys/
- 43.Löwe B, Decker O, Müller S, et al. Validation and standardization of the generalized anxiety disorder Screener (GAD-7) in the general population. Med Care 2008;46:266–74. 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- 44.Index . ACoQoLMPW. n.d. Available: http://www.acqol.com.au/instruments#measures
- 45.Cantabrians . CaPHNStWo. n.d. Available: https://www.cph.co.nz/your-health/wellbeing-survey/
- 46.FluTracking. n.d. Available: https://info.flutracking.net/
- 47.R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Available: https://www.r-project.org/ [Google Scholar]
- 48.Wang P, Robins G, Pattison P, et al. PNet: program for the simulation and estimation of exponential random graph models. Melbourne School of Psychological Sciences, The University of Melbourne, 2009. [Google Scholar]
- 49.Ltd. QIP . Nvivo qualitative data analysis software. 2012.
- 50.Abeysuriya RG, Delport D, Stuart RM, et al. Preventing a cluster from becoming a new wave in settings with zero community COVID-19 cases. BMC Infect Dis 2022;22:232. 10.1186/s12879-022-07180-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heath K, Altermatt A, Saich F, et al. Intent to be vaccinated against COVID-19 in Victoria, Australia. Vaccines (Basel) 2022;10:209. 10.3390/vaccines10020209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nguyen T, Thomas AJ, Kerr P, et al. Recruiting and retaining community-based participants in a COVID-19 longitudinal cohort and social networks study: lessons from Victoria, Australia. BMC Med Res Methodol 2023;23:54. 10.1186/s12874-023-01874-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tse WC, Altermatt A, Saich F, et al. I know what you did last summer: a cross-sectional study of personal COVID-19 risk reduction strategies used by Victorian adults. Aust N Z J Public Health 2023;47:100068. 10.1016/j.anzjph.2023.100068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Victorian COVID-19 data. n.d. Available: https://www.coronavirus.vic.gov.au/victorian-coronavirus-covid-19-data
- 55.West R, Michie S, Rubin GJ, et al. Applying principles of behaviour change to reduce SARS-Cov-2 transmission. Nat Hum Behav 2020;4:451–9. 10.1038/s41562-020-0887-9 [DOI] [PubMed] [Google Scholar]
- 56.Ryan RE, Silke C, Parkhill A, et al. Communication to promote and support physical distancing for COVID-19 prevention and control. Cochrane Database Syst Rev 2023;10:CD015144. 10.1002/14651858.CD015144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leask J, Carlson SJ, Attwell K, et al. Communicating with patients and the public about COVID-19 vaccine safety: recommendations from the collaboration on social science and Immunisation. Med J Aust 2021;215:9–12. 10.5694/mja2.51136 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-076907supp001.pdf (1.2MB, pdf)