Abstract
Background:
Pain perception and management vary across cultural contexts; yet, little is known about pain approaches in the general population of Palestine. Existing research lacks specific knowledge about how pain is coped with in this region.
Objective:
To explore pain management among Palestine’s general population, studying prevalence, characteristics, and sociodemographic influences. It aims to uncover treatment choices and understand cultural impacts on pain experiences, offering insights into Palestinian pain perception and coping strategies.
Methods:
Convenience and snowball sampling methods were employed to collect data from 646 adults in Palestine. Participants’ sociodemographic characteristics, pain experiences, and pain management strategies were examined. Descriptive statistics, chi-square tests, and binary logistic regression followed by multiple logistic regressions were used for data analysis.
Results:
A significant portion of participants reported experiencing pain, with chronic pain being predominant. Pain prevalence varied across age groups, with higher rates in the elderly, followed by middle-aged and younger participants. Marital status and education level were linked to pain prevalence. Participants employed diverse pain management strategies, such as self-medication, physician visits, complementary medicine, and physical therapy. Age, gender, marital status, and education level influenced choices in pain management approaches. For instance, the elderly favored traditional medical interventions, while higher education levels were associated with reduced inclination toward conventional treatments.
Conclusion:
This study underscores the complex interaction of sociodemographic factors, pain experiences, and treatment preferences in pain management. It emphasizes personalized strategies considering age, marital status, education, and gender. Integrating these aspects improves treatment and satisfaction. The findings empower healthcare providers to create precise strategies, enhancing patient experiences for better outcomes.
Keywords: Pain perception, coping strategies, prevalence, alternative medicines, self-medication
Introduction
Pain is a complex and multifaceted phenomenon that affects millions of people worldwide and its management remains a major challenge for healthcare systems. 1 In Palestine, pain management represents a critical issue that is compounded by ongoing political conflict, economic hardship, and limited healthcare resources. Despite the high burden of pain in this context, there is limited research on how the general population approaches their pain, including their beliefs, attitudes, and behaviors related to pain management. This study aims to address this gap by investigating the prevalence, characteristics, and determinants of pain among adults in Palestine. 2
Pain is a leading cause of disability and reduced quality of life globally, affecting people of all ages, genders, and socioeconomic backgrounds. 3 In the Eastern Mediterranean region, which includes Palestine, the prevalence of chronic pain ranges from 16% to 60%, depending on the population and setting. 4
Pain is a common reason for seeking healthcare, and it affects people across the lifespan, from children with cancer to elderly patients with chronic conditions. However, pain management in Palestine is often inadequate, fragmented, and stigmatized, due to factors such as limited resources, political instability, and cultural norms. 5
Culture and social context play a crucial role in shaping the experience and management of pain. 6 Moreover, gender, age, and socioeconomic status can influence access to pain treatment and the willingness to disclose pain-related concerns. For instance, women in Palestine may face cultural barriers to seeking healthcare for pain, due to social norms that prioritize their caregiving roles over their own health needs. Similarly, marginalized groups, such as refugees or people living in poverty, may have limited access to pain medication or specialized care. 7
Pain management in Palestine is primarily provided by the public healthcare system, which faces significant challenges in terms of resource allocation, infrastructure, and workforce. 8 Pain medication, particularly opioids, is often scarce or restricted, due to regulatory barriers and security concerns. Moreover, the lack of specialized pain clinics or trained healthcare providers can limit the options for effective pain management. On the policy level, pain management is not yet recognized as a priority area in the national health agenda, and there is a need for evidence-based guidelines and regulations to ensure the availability and quality of pain treatment. 9
Existing research has explored pain perception and management across various populations and cultural contexts but there is limited specific knowledge about how the general population in Palestine approaches and copes with pain. This article addresses this gap by conducting a cross-sectional study focused on pain management practices in the region. It adds valuable insights into the cultural, social, and contextual factors influencing pain experiences and coping mechanisms within the population. The findings of this study will contribute to a better understanding of pain management in Palestine and inform the development of targeted interventions and strategies for improving overall well-being in this context.
This study aims to investigate how the general population in Palestine perceives and addresses pain. The study seeks to evaluate the prevalence and characteristics of pain experiences within this population and explore the potential impact of sociodemographic variables such as age, gender, marital status, and education level on individuals’ approaches to pain perception and management. In addition, the research aims to examine the array of therapeutic interventions chosen by the general population in Palestine to alleviate their pain. By doing so, the study aims to offer valuable insights into the cultural, social, and contextual factors that play a role in shaping pain experiences and management strategies among Palestinians.
Methods
Design and participants
This cross-sectional study in Palestine adhered to the Strengthening the Reporting of Observational Studies in Epidemiology Guidelines, encompassing an approximate total population of 5,000,000, with around 3,000,000 adults aged 18 years and above (source: http://www.pcbs.gov.ps). 10 The study employed nonprobability sampling methods, specifically convenience and snowball sampling methods to recruit participants, which were selected to suit the scope and nature of the study. Convenience sampling was used as an initial approach due to its practicality and ease of data collection. Snowball sampling was subsequently utilized to enhance the representativeness of the sample. The sample size was determined using a single proportion formula, with a reference proportion of 50%, within the framework of a cross-sectional study design. In this design, n denoted the required sample size (n = Z(α/2) 2 * pq/d2) for a 95% confidence interval and a 5% margin of error. Consequently, a sample size of 385 was established to represent the larger population. Ultimately, we received 673 responses, with 27 individuals declining to participate, resulting in data collected from 646 respondents between June and December 2022, forming the basis for all subsequent calculations.
The statistics provided by the Palestinian Central Bureau of Statistics indicate that in early 2023, there were 4.38 million active cellular mobile connections for individuals aged 10 years and above. 10 This figure represented a very high portion of the total population in Palestine. The widespread use of mobile connections within this demographic was a pivotal factor influencing our decision to employ online platforms such as WhatsApp and Facebook for disseminating the questionnaire. Participant enrolment occurred through electronic communication, where an online questionnaire, accessible via a Google Form link, was distributed via email and public social media platforms like Facebook and WhatsApp. Respondents completed the electronic survey and submitted their answers, which were then transmitted back to the researchers. The study included individuals aged 18 years or older who reside in Palestine and have electronic access to email and public social media platforms like Facebook and WhatsApp and could complete the online questionnaire, while the exclusion criteria included individuals who declined participation, lacked access to social media or a telephone, and those less than 18 years of age. Ethical approval for the study was granted by the Institutional Review Board of An-Najah University in Nablus, located in the West Bank of Palestine (Reference: Med. November 2020/2). The study adhered to the principles of the Helsinki Declaration regarding human research. Prior to inclusion, all participants provided written informed consent to take part in the study.
Data collection and assessment tool
A specialized data collection notebook was created to meticulously document the participants’ details. The survey employed in this investigation comprised closed-ended inquiries, categorized into sections encompassing participants’ demographic and clinical characteristics, pain management techniques, and utilized treatments. Except for demographic and clinical data, the responses were based on binary questions that elicited either affirmative or negative answers. The questionnaire was conducted in Arabic, aligning with the predominant language spoken in Palestine. Prior to distribution to participants, the questionnaire underwent thorough scrutiny by experts in the fields of public health, medicine, and pharmacy. A pilot study involving a sample of 50 participants, which constitutes approximately 13% of the estimated sample size (385 participants), was conducted to test the survey questions. Following this, a sequence of revisions was undertaken to ensure a strong internal consistency, measured using Cronbach’s alpha. The calculated Cronbach’s alpha coefficient for the questions reached a value of 0.755.
Pain intensity assessment involved the use of the Visual Analogue Scale (VAS) and the Numerical Rating Scale (NRS), both ranging from 0 (indicating no pain) to 10 (representing the worst imaginable pain). Pain levels were classified into three categories: Mild Pain (1–3), Moderate Pain (4–6), and Severe Pain (7–10). 11 The pain was classified according to its duration in acute pain (pain lasting less than 3 months) and chronic pain (pain lasting over 3 months). 12 On the other hand, the body mass index (BMI) was categorized as Underweight: BMI is less than 18.5. Healthy weight: BMI is 18.5 to <25. Overweight: BMI is 25.0 to <30. Obesity: BMI is 30.0 or higher. 13 In addition, participants were organized into specific age groups for a comprehensive analysis, with the “young group” comprising individuals aged 15–47 years, the “middle-aged group” encompassing participants aged 48–63 years, and the “elderly group” including those aged 64 years and older. 14
Statistical analysis
Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS v.25). The entire study population had complete data points for all collected information. An initial descriptive analysis was executed, portraying data through frequency and percentage representations for categorical variables. The comparison of categorical variables involved the utilization of either the chi-squared test or Fisher’s exact test. A value of p < 0.05 was considered statistically significant.
Binary logistic regression was employed to evaluate the associations between therapeutics utilized by participants encountering pain and therapeutic strategies employed for pain management. In addition, multiple logistic regressions were performed, incorporating variables that exhibited statistical significance alongside other variables of clinical importance.
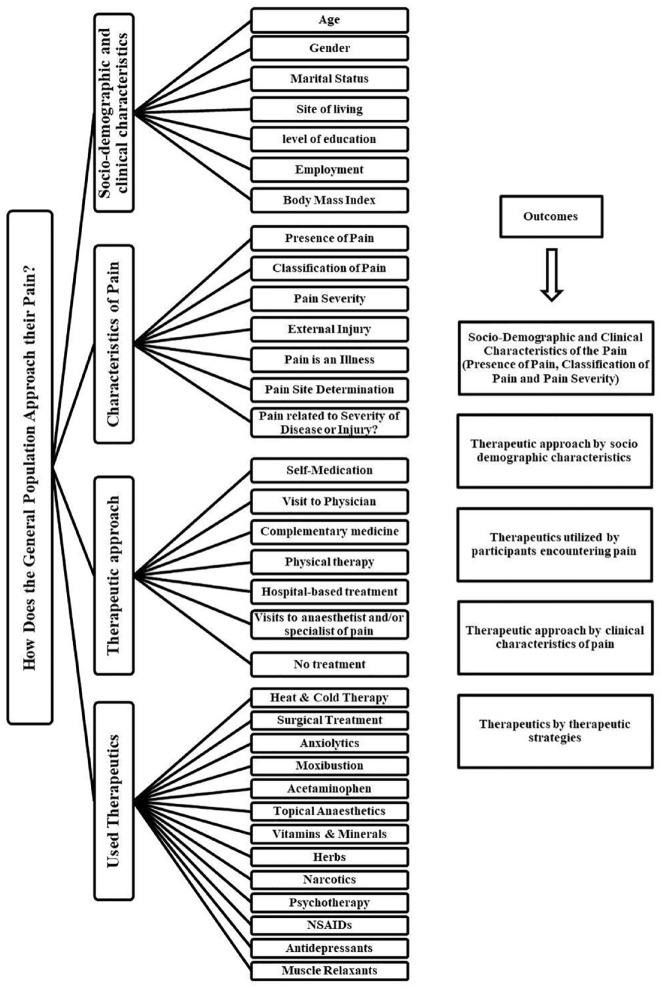
Figure 1 shows a diagram depicting the schematic representation of the different variables and outcomes.
Figure 1.
Diagrammatic illustration of diverse research outcomes.
Results
Sociodemographic and clinical characteristics of the participants
A total of 646 questionnaires were examined, with the majority of respondents being young (N = 563, 87.2%), and approximately 71% were females. Regarding the participants’ residential areas, over half resided in urban areas (N = 349, 54.0%). Furthermore, more than a quarter of the participants were employed (N = 184, 28.5%), while over half identified themselves as students (N = 359, 55.6%), and 65.3% reported being unmarried (N = 422). Moreover, when calculating the BMI for over half of the participants (N = 330, 51.1%), it was determined that their weight fell within the normal range (i.e., BMI: 18.5–24.9) (Table 1).
Table 1.
Sociodemographic and clinical characteristics of the participants.
| Variables | Presence of pain | Total, N = 646 | p-Value | Classification of pain | Total, N = 237 | p-Value | Pain severity | p-Value | Total, N = 237 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No, % | Yes, % | Acute < 3 months, % | Chronic ⩾ 3 months% | Mild, % | Moderate, % | Severe, % | |||||||
| Age | 0.000 | 0.000 | 0.000 | ||||||||||
| Elderly | 16.7 | 83.3 | 6 | 0.0 | 100 | 5 | 40.0 | 20.0 | 40.0 | 5 | |||
| Middle age | 22.1 | 77.9 | 77 | 10.0 | 90.0 | 60 | 46.7 | 35.0 | 18.3 | 60 | |||
| Young | 69.4 | 30.6 | 563 | 25.6 | 74.4 | 172 | 48.8 | 36.1 | 15.1 | 172 | |||
| Gender | 0.511 | 0.135 | 0.591 | ||||||||||
| Female | 64.1 | 35.9 | 457 | 24.4 | 75.6 | 164 | 46.3 | 35.4 | 18.3 | 164 | |||
| Male | 61.4 | 38.6 | 189 | 13.7 | 86.3 | 73 | 52.1 | 35.6 | 12.3 | 73 | |||
| Marital status | 0.000 | 0.000 | 0.002 | ||||||||||
| Married | 53.1 | 46.9 | 213 | 13 | 87.0 | 100 | 47.0 | 38.0 | 15.0 | 100 | |||
| Separated/divorced | 55.6 | 44.4 | 9 | 25 | 75.0 | 4 | 50.0 | 25.0 | 25.0 | 4 | |||
| Unmarried | 69.0 | 31.0 | 422 | 27.5 | 72.5 | 131 | 49.6 | 33.6 | 16.8 | 131 | |||
| Widowed | 0.0 | 100.0 | 2 | 0.0 | 100.0 | 2 | 0.0 | 50.0 | 50.0 | 2 | |||
| Site of living | 0.923 | 0.822 | 0.824 | ||||||||||
| Camp | 60.7 | 39.3 | 28 | 9.1 | 90.9 | 11 | 36.4 | 45.4 | 18.2 | 11 | |||
| City | 63.9 | 36.1 | 349 | 23 | 77.0 | 126 | 45.2 | 38.9 | 15.9 | 126 | |||
| Village | 62.8 | 37.2 | 269 | 20 | 80.0 | 100 | 53.0 | 30.0 | 17.0 | 100 | |||
| Level of education | 0.000 | 0.000 | 0.000 | ||||||||||
| Literacy study | 0.0 | 100.0 | 3 | 0.0 | 100.0 | 3 | 0.0 | 0.0 | 100.0 | 3 | |||
| Elementary school | 11.1 | 88.9 | 9 | 0.0 | 100.0 | 8 | 25.0 | 37.5 | 37.5 | 8 | |||
| Middle school | 49.0 | 51.0 | 51 | 23.1 | 76.9 | 26 | 26.9 | 27.7 | 15.4 | 26 | |||
| University study | 68.4 | 31.6 | 531 | 23.2 | 76.8 | 168 | 52.4 | 32.7 | 14.9 | 168 | |||
| Postgraduate studies | 38.5 | 61.5 | 52 | 15.6 | 84.4 | 32 | 53.1 | 34.4 | 12.5 | 32 | |||
| Employment | 0.000 | 0.000 | 0.000 | ||||||||||
| Employed | 50.0 | 50.0 | 184 | 13.0 | 87.0 | 92 | 53.2 | 34.8 | 12.0 | 92 | |||
| Home duties | 27.3 | 72.7 | 44 | 15.6 | 84.4 | 32 | 34.4 | 37.5 | 28.1 | 32 | |||
| Retired | 40.0 | 60.0 | 5 | 33.3 | 66.7 | 3 | 33.3 | 33.3 | 33.3 | 3 | |||
| Student | 76.6 | 23.4 | 359 | 33.3 | 66.7 | 84 | 52.4 | 32.1 | 15.5 | 84 | |||
| Unemployed | 51.9 | 48.1 | 54 | 15.4 | 84.6 | 26 | 34.6 | 46.2 | 19.2 | 26 | |||
| Body mass index | 0.224 | 0.258 | 0.624 | ||||||||||
| Underweight | 70.7 | 29.3 | 58 | 17.6 | 82.4 | 17 | 41.2 | 35.3 | 23.5 | 17 | |||
| Healthy weight | 64.5 | 35.5 | 330 | 24.8 | 75.2 | 117 | 49.6 | 35.0 | 15.4 | 117 | |||
| Overweight | 62.8 | 37.2 | 172 | 20.3 | 79.7 | 64 | 50.0 | 31.3 | 18.7 | 64 | |||
| Obesity | 54.7 | 45.3 | 86 | 12.8 | 87.2 | 39 | 43.6 | 43.6 | 12.8 | 39 | |||
p-values obtained from chi-square, Bold p-values are statistically significant. Young: (15–47 years old). Middle age: (48–63 years old). Elderly: (64 and older). Underweight: BMI is less than 18.5. Healthy weight: BMI is 18.5 to <25. Overweight: BMI is 25.0 to <30. Obesity: BMI is 30.0 or higher.
Among the participants, a total of 237 individuals (36.7%) reported experiencing pain. Out of these, 79% were identified as having chronic pain, indicating a duration of 3 months or longer. In addition, when assessing the pain levels using the VAS and NRS, it was found that 114 participants (48.1%) reported mild pain, 84 participants had moderate pain (35.4%), and 39 individuals suffered from severe pain (16.5%) (Table1).
The occurrence of pain demonstrated a significantly higher prevalence among the elderly which included a limited number of respondents, followed by the middle-aged and young groups (p < 0.001). Furthermore, unmarried participants exhibited the lowest percentage of pain compared to those who were married or previously married, and this difference was statistically significant (p < 0.001). The prevalence of pain was notably higher among individuals with lower educational levels, specifically those who had completed only a literacy study or elementary school (p < 0.001). In addition, retired participants and individuals with home duties displayed a higher percentage of pain (p < 0.001). Conversely, no statistical differences were observed in terms of gender, residential location, or BMI (Table 1).
The participants’ pain was categorized into two groups based on its duration: acute pain (lasting less than 3 months) and chronic pain (lasting 3 months or longer). Significantly higher rates of chronic pain were reported among the elderly participants, followed by the middle-aged and younger individuals (p < 0.001). Notably, unmarried participants exhibited a lower percentage of chronic pain compared to those who were married or previously married, with this difference being statistically significant (p < 0.001). Furthermore, individuals with lower educational levels, specifically those who had completed only literacy studies or elementary school, experienced a significantly higher prevalence of chronic pain (p < 0.001). Retired participants and those with home duties demonstrated a higher percentage of chronic pain (p < 0.001). On the other hand, no statistically significant differences were found in terms of gender, residential location, or BMI (Table 1).
The elderly participants reported significantly elevated levels of severe pain, followed by the middle-aged and younger individuals (p < 0.001). Interestingly, among the various groups, those who were widowed exhibited a notable increase in the percentage of severe pain, with this distinction proving to be statistically significant (p < 0.05). Moreover, individuals with lower educational backgrounds, particularly those who had completed only literacy studies or elementary school, encountered a significantly higher prevalence of severe pain (p < 0.001). Notably, retired participants and those with domestic responsibilities displayed a higher proportion of severe pain (p < 0.001). Conversely, gender, residential location, and BMI yielded no statistically significant differences (Table 1).
Participants utilized various therapeutic approaches to manage their pain, including the following: no treatment, self-medication, visits to physicians, complementary medicine, physical therapy, hospital-based treatment, and visits to anesthesiologists or pain medicine specialists. The numbers and percentages of participants who used these approaches and experienced pain were as follows: no treatment (64, 27%), self-medication (81, 34.2%), visits to physicians (51, 21.5%), complementary medicine (25, 10.5%), physical therapy (36, 15.2%), hospital-based treatment (29, 12.2%), and visits to anesthesiologists or pain medicine specialists (34, 14.3%).
Table 2 illustrates the association between age groups and therapeutic approaches. The elderly group exhibited a significant association with visits to physicians, physical therapy, and hospital-based treatments (p < 0.05). Conversely, the middle age group displayed a negative association with self-medication (p < 0.05). No significant differences were found regarding complementary medicine or no treatment.
Table 2.
Therapeutic approach by sociodemographic characteristics.
| Variables | Therapeutic strategies of 237 participants (yes answer) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SF% | p-Value | VP% | p-Value | CM% | p-Value | PT% | p-Value | HT% | p-Value | VAPS% | p-Value | NT% | p-Value | Total N = 237 | |
| Age | 0.004 | 0.006 | 0.061 | 0.003 | 0.030 | 0.061 | 0.119 | ||||||||
| Elderly | 40.0 | 60.0 | 40.0 | 40.0 | 40.0 | 20.0 | 0.0 | 5 | |||||||
| Middle age | 16.7 | 31.7 | 6.7 | 26.7 | 18.3 | 23.3 | 20.0 | 60 | |||||||
| Young | 40.1 | 16.9 | 11.0 | 10.5 | 9.3 | 11.0 | 30.2 | 172 | |||||||
| Gender | 0.755 | 0.107 | 0.552 | 0.226 | 0.407 | 0.009 | 0.174 | ||||||||
| Female | 33.5 | 24.4 | 9.8 | 17.1 | 13.4 | 18.3 | 24.4 | 164 | |||||||
| Male | 35.6 | 15.1 | 12.3 | 11.0 | 9.6 | 5.5 | 32.9 | 73 | |||||||
| Marital status | 0.409 | 0.522 | 0.017 | 0.771 | 0.024 | 0.623 | 0.508 | ||||||||
| Married | 30.0 | 23.0 | 10.0 | 17.0 | 14.0 | 17.0 | 27.0 | 100 | |||||||
| Separated/divorced | 25.0 | 0.0 | 50.0 | 25.0 | 50.0 | 25.0 | 0.0 | 4 | |||||||
| Unmarried | 38.2 | 20.6 | 9.2 | 13.7 | 9.2 | 12.2 | 28.2 | 131 | |||||||
| Widowed | 0.0 | 50.0 | 50.0 | 0.0 | 50.0 | 0.0 | 0.0 | 2 | |||||||
| Site of living | 0.011 | 0.684 | 0.175 | 0.833 | 0.107 | 0.318 | 0.466 | ||||||||
| Camp | 72.7 | 27.3 | 18.2 | 9.1 | 27.3 | 18.2 | 18.2 | 11 | |||||||
| City | 35.7 | 23.0 | 7.1 | 15.9 | 8.7 | 11.1 | 30.2 | 126 | |||||||
| Village | 28.0 | 19.0 | 14.0 | 15.0 | 15.0 | 18.0 | 24.0 | 100 | |||||||
| Level of education | 0.918 | 0.000 | 0.006 | 0.176 | 0.000 | 0.032 | 0.251 | ||||||||
| Literacy study | 33.3 | 100 | 66.7 | 66.7 | 66.7 | 33.3 | 0.0 | 3 | |||||||
| Elementary school | 25.0 | 37.5 | 12.5 | 12.5 | 50.0 | 50.0 | 25.0 | 8 | |||||||
| Middle school | 34.6 | 42.3 | 15.4 | 15.4 | 19.2 | 19.2 | 11.5 | 26 | |||||||
| University study | 33.3 | 17.3 | 10.7 | 14.3 | 9.5 | 11.9 | 28.6 | 168 | |||||||
| Postgraduate studies | 40.6 | 15.6 | 0.0 | 15.6 | 6.3 | 12.5 | 34.4 | 32 | |||||||
| Employment | 0.984 | 0.007 | 0.085 | 0.001 | 0.426 | 0.299 | 0.284 | ||||||||
| Employed | 35.9 | 16.3 | 4.3 | 12.0 | 8.7 | 13.0 | 32.6 | 92 | |||||||
| Home duties | 31.3 | 43.8 | 12.5 | 15.6 | 15.6 | 25.0 | 15.6 | 32 | |||||||
| Retired | 33.3 | 33.3 | 33.3 | 100 | 33.3 | 33.3 | 0.0 | 3 | |||||||
| Student | 34.5 | 15.5 | 13.1 | 13.1 | 11.9 | 10.7 | 25.0 | 84 | |||||||
| Unemployed | 30.8 | 30.8 | 19.2 | 23.1 | 19.2 | 15.4 | 30.8 | 26 | |||||||
| Body mass index | 0.384 | 0.418 | 0.248 | 0.098 | 0.198 | 0.054 | 0.215 | ||||||||
| Underweight | 29.4 | 35.3 | 23.5 | 35.3 | 11.8 | 35.3 | 5.9 | 17 | |||||||
| Healthy weight | 39.3 | 19.7 | 8.5 | 12.0 | 12.8 | 12.0 | 27.4 | 117 | |||||||
| Overweight | 31.3 | 18.8 | 12.5 | 15.6 | 6.3 | 10.9 | 31.3 | 64 | |||||||
| Obesity | 25.6 | 25.6 | 7.7 | 15.4 | 20.5 | 17.9 | 28.2 | 39 | |||||||
SF: self-medication; VP: visit to the physician; CM: complementary medicine; PT: physical therapy; HT: hospital-based treatment; VAPS: visits to anesthetist and/or specialist of pain; NT: no treatment.
p-values obtained from chi-square, bold p-values are statistically significant.
Regarding gender, being female showed a significant association with visits to anesthesiologists or pain specialists (p < 0.05). The use of complementary medicines and hospital-based treatments exhibited a negative association with the unmarried group, whereas higher percentages were observed among the married, separated/divorced, and widowed groups (p < 0.05).
Regarding education level, the results indicated that higher levels of education were associated with lower percentages of visits to physicians (p < 0.001), the use of complementary medicine (p < 0.05), hospital-based treatment (p < 0.05), and visits to anesthesiologists or pain medicine specialists (p < 0.05). On the other hand, retired participants and those with home duties showed significantly higher percentages of visits to physicians and physical therapy (p < 0.05). No differences were observed in relation to body mass index.
Table 3 displays the correlation between therapeutic approaches used by participants who experienced pain. The analysis reveals a significant association between the presence of external injury and the self-medication approach (p < 0.05). Furthermore, pain severity, indicating a link to disease or injury severity, is significantly associated with the hospital-based treatment approach (p < 0.05). Participants who perceive their pain as an independent illness exhibit significantly higher percentages in the following approaches: visits to physicians, hospital-based treatment, and visits to anesthetists and/or pain specialists (p < 0.05). Conversely, individuals who do not view their pain as a distinct illness show an association with physical therapy (p < 0.05). Severe pain demonstrates a significant association with visits to anesthetists and/or pain specialists (p < 0.001). However, the duration of pain and determination of the pain site do not exhibit significant differences between groups across various therapeutic approaches.
Table 3.
Therapeutic approach by clinical characteristics of pain.
| Variables | Therapeutic strategies of 237 participants (yes answer) | Total N = 237 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SM | p-Value | VP | p-Value | CM | p-Value | PT | p-Value | HT | p-Value | VAPS | p-Value | NT | p-Value | ||
| Duration of pain | 0.328 | 0.285 | 0.239 | 0.286 | 0.323 | 0.324 | 0.858 | ||||||||
| Acute <3 months, % | 40.0 | 16.0 | 6.0 | 20.0 | 8.0 | 10.0 | 28.0 | 50 | |||||||
| Chronic ⩾3 months, % | 32.6 | 23.0 | 11.8 | 13.9 | 13.4 | 15.5 | 26.7 | 187 | |||||||
| External injury | 0.034 | 0.345 | 0.336 | 0.097 | 0.245 | 0.460 | 0.328 | ||||||||
| No, % | 32.1 | 22.3 | 11.2 | 14.0 | 13.0 | 14.9 | 27.9 | 215 | |||||||
| Yes, % | 54.5 | 13.6 | 4.5 | 27.3 | 4.5 | 9.1 | 18.2 | 22 | |||||||
| Pain related to the severity of disease or injury? | 0.800 | 0.892 | 0.487 | 0.294 | 0.047 | 0.133 | 0.282 | ||||||||
| No% | 33.6 | 21.2 | 11.6 | 17.1 | 8.9 | 11.6 | 29.5 | 146 | |||||||
| Yes% | 35.2 | 22.0 | 8.8 | 12.1 | 17.6 | 18.7 | 23.1 | 91 | |||||||
| Pain is an illness | 0.354 | 0.024 | 0.256 | 0.039 | 0.044 | 0.006 | 0.087 | ||||||||
| Maybe | 33.9 | 20.2 | 8.9 | 9.7 | 12.1 | 10.5 | 33.1 | 124 | |||||||
| No | 42.9 | 9.5 | 7.1 | 23.8 | 2.4 | 7.1 | 21.4 | 42 | |||||||
| Yes | 29.6 | 31.0 | 15.5 | 19.7 | 18.3 | 25.4 | 19.7 | 71 | |||||||
| Pain site determination | 0.935 | 0.335 | 0.339 | 0.185 | 0.745 | 0.931 | 0.461 | ||||||||
| No | 35.0 | 30.0 | 5.0 | 5.0 | 10.0 | 15.0 | 20.0 | 124 | |||||||
| Yes | 34.1 | 20.7 | 11.1 | 16.1 | 12.4 | 14.3 | 27.6 | 42 | |||||||
| Pain severity | 0.275 | 0.303 | 0.192 | 0.563 | 0.090 | 0.000 | 0.778 | ||||||||
| Mild pain | 36.8 | 19.3 | 10.5 | 14.9 | 7.9 | 8.8 | 25.4 | 114 | |||||||
| Moderate pain | 35.7 | 20.2 | 7.1 | 13.1 | 14.3 | 11.9 | 29.8 | 84 | |||||||
| Severe | 23.1 | 30.8 | 17.9 | 20.5 | 20.5 | 35.9 | 25.6 | 39 | |||||||
SM: self-medication; VP: visit to the physician; CM: complementary medicine; PT: physical therapy; HT: hospital-based treatment; VAPS: visits to anesthetist and/or specialist of pain; NT: no treatment.
p-values obtained from chi-square, bold p-values are statistically significant. Young: (15–47 years old). Middle age: (48–63 years old). Elderly: (64 and older). Underweight: BMI is less than 18.5. Healthy weight: BMI is 18.5 to <25. Overweight: BMI is 25.0 to <30. Obesity: BMI is 30.0 or higher.
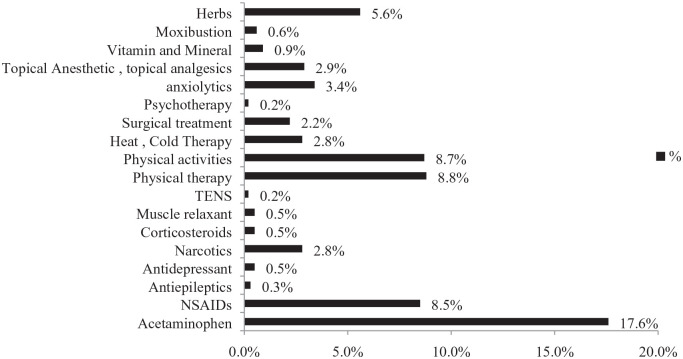
Figure 1 illustrates the distribution of therapeutics utilized by participants experiencing pain. Acetaminophen demonstrated the most substantial occurrence, followed by physical therapy, engagement in physical activities, and the incorporation of herbal treatments. By contrast, the least employed interventions encompassed more advanced methods, including sophisticated treatments like Transcutaneous Electrical Nerve Stimulation (TENS), psychotherapies, and anti-epileptic medications.
Table 4 shows that receiving anxiolytics was significantly related to increased odds of self-medication (odds ratio (OR) = 3.321, 95% confidence interval (CI) (0.865–8.427)). Moreover, when examining individual factors associated with visits to physicians for pain management, the analysis revealed a significant association with the usage of acetaminophen, topical anesthetics, vitamins, minerals, and herbal remedies. Subsequent findings indicated that individuals who indicated using acetaminophen had notably higher odds of visiting physicians for pain management (OR = 2.913; 95% CI (1.399–6.1)). Likewise, those who reported utilizing topical anesthetics exhibited increased likelihood (OR = 3.219, 95% CI (1.080–9.601)), along with individuals who consumed vitamins and minerals (OR = 13.341, 95% CI (2.168–82.1)) and herbal remedies (OR = 2.597, 95% CI (1.120–6.021)), respectively, demonstrating higher probabilities of seeking medical attention from physicians for pain management.
Table 4.
Therapeutics by therapeutic approach.
| Variable (ref.: answer with no) | Therapeutic approach | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SF% | p-Value | VP% | p-Value | CM% | p-Value | PT% | p-Value | HT% | p-Value | NT% | p-Value | VAPS% | p-Value | |
| Odds ratio with 95% CI | Odds ratio with 95% CI | Odds ratio with 95% CI | Odds ratio with 95% CI | Odds ratio with 95% CI | Odds ratio with 95% CI | Odds ratio with 95% CI | ||||||||
| Heat and cold therapy, yes | 1.946 (0.658–5.754) | 0.229 | 0.647 (0.171–2.444) | 0.521 | 1.788 (0.325–9.833) | 0.504 | 3.901 (1.229–12.382) | 0.021 | 0.301 (0.026–3.489) | 0.337 | 0.410 (0.087–1.942) | 0.261 | 0.827 (0.173–3.941) | 0.811 |
| Surgical treatment, yes | 0.0 (0.000) | 0.998 | 0.985 (0.221–4.386) | 0.984 | 2.398 (0.369–15.6) | 0.360 | 2.298 (0.551–9.6) | 0.253 | 222.984 (22.8–2181.6) | 0.000 | 0.0 (0.000) | 0.998 | 10.3 (2.703–39.244) | 0.001 |
| Anxiolytics, yes | 3.321 (1.184–9.316) | 0.023 | 2.7 (0.865–8.427) | 0.087 | 0.759 (0.108–5.312) | 0.781 | 0.641 (0.160–2.570) | 0.530 | 1.218 (0.209–7.1) | 0.826 | 0.509 (0.152–1.707) | 0.274 | 1.197 (0.292–4.906) | 0.803 |
| Moxibustion, yes | 0.0 (0.000) | 0.999 | 0.494 (0.023–10.5) | 0.651 | 2.446 (0.090–66.539) | 0.596 | 2.439 (0.216–27.6) | 0.471 | 3.201 (0.249–41.1) | 0.372 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 |
| Acetaminophen, yes | 1.482 (0.813–2.703) | 0.199 | 2.913 (1.399–6.1) | 0.004 | 1.103 (0.384–3.169) | 0.855 | 0.396 (0.176–0.889) | 0.025 | 4.541 (1.417–14.6) | 0.011 | 0.546 (0.289–1.031) | 0.062 | 1.087 (0.445–2.658) | 0.855 |
| Topical anesthetics, yes | 0.754 (0.241–2.361) | 0.628 | 3.219 (1.080–9.601) | 0.036 | 0.091 (0.003–2.954) | 0.177 | 0.226 (0.025–2.1) | 0.189 | 6.780 (1.778–25.847) | 0.005 | 0.261 (0.056–1.217) | 0.087 | 4.882 (1.411–16.9) | 0.012 |
| Vitamins and minerals, yes | 4.169 (0.710–24.5) | 0.114 | 13.341 (2.168–82.1) | 0.005 | 0.0 (0.000) | 0.999 | 1.007 (0.108–9.382) | 0.995 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 2.252 (0.211–22.991) | 0.493 |
| Herbs, yes | 1.390 (0.633–3.053) | 0.411 | 2.597 (1.120–6.021) | 0.026 | 12.742 (1.120–6.021) | 0.000 | 1.402 (0.534–3.677) | 0.492 | 1.688 (0.464–6.147) | 0.427 | 0.937 (0.404–2.174) | 0.879 | 1.338 (0.407–4.403) | 0.632 |
| Narcotics, yes | 0.803 (0.231–2.789) | 0.730 | 2.461 (0.729–8.304) | 0.147 | 9.706 (2.284–41.240) | 0.002 | 0.884 (0.210–3.726) | 0.867 | 1.901 (0.306–11.818) | 0.491 | 1.059 (0.323–3.5) | 0.924 | 5.545 (1.579–19.5) | 0.008 |
| Psychotherapy, yes | 0.0 (0.000) | 1.000 | 0.0 (0.000) | 1.000 | 0.0 (0.000) | 1.000 | 0.0 (0.000) | 1.000 | 0.0 (0.000) | 1.000 | 0.0 (0.000) | 1.000 | 0.0 (0.000) | 1.000 |
| NSAIDs, yes | 1.541 (0.777–3.056) | 0.216 | 1.848 (0.847–4.033) | 0.123 | 2.270 (0.743–6.933) | 0.150 | 0.924 (0.376–2.269) | 0.863 | 1.218 (0.369–4.027) | 0.746 | 0.539 (0.244–1.193) | 0.127 | 4.427 (1.739–11.3) | 0.002 |
| Antidepressants, yes | 0.0 (0.000) | 0.998 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 2.436 (0.118–50.178) | 0.564 | 5.322 (0.168–168.533) | 0.343 |
| Muscle relaxants | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 0.0 (0.000) | 0.999 | 2.406 (0.143–40.474) | 0.542 | 23.5 (1.551–355.005) | 0.023 |
SF: self-medication; VP: visit to the physician; CM: complementary medicine; PT: physical therapy; HT: hospital-based treatment; VAPS: visits to anesthetist and/or specialist of pain; NT: no treatment; NSAIDs: nonsteroidal anti-inflammatory drugs.
p-values obtained from binary logistic regression, bold p-values are statistically significant.
In terms of obtaining herbs and narcotics for pain management, a notable association was observed with higher probabilities of seeking complementary medicine for pain management, as highlighted in the data presented (Table 4). Consequently, individuals who received herbs for pain management displayed an increased tendency to opt for complementary medicinal approaches (OR = 12.742, 95% CI (1.120–6.021)). Similarly, those who were administered narcotics for pain management also exhibited an elevated likelihood of utilizing complementary medicine for pain management (OR = 9.706, 95% CI (2.284–41.240)).
Furthermore, when examining factors associated with physical therapy, a univariate analysis (Table 4) revealed distinct trends. Receiving heat and cold therapy demonstrated a significant correlation with heightened probabilities of seeking physical therapy for pain management. Conversely, the reception of acetaminophen for pain management was notably linked to reduced odds of pursuing physical therapy for pain management. To elaborate, individuals who received heat and cold therapy exhibited a substantial inclination toward utilizing physical therapy for pain management (OR = 3.901, 95% CI (1.229–12.382)). On the other hand, those who indicated their usage of acetaminophen (OR = 0.396, 95% CI (0.176–0.889)) demonstrated a decreased likelihood of opting for physical therapy as a means of managing pain.
In addition, individuals who underwent surgical treatment (OR = 222.984, 95% CI (22.8–2181.6)), those who used acetaminophen (OR = 4.541, 95% CI (1.417–14.6)), and those who employed topical anesthetics (OR = 6.780, 95% CI (1.778–25.847)) displayed a markedly heightened likelihood of seeking medical attention at hospitals for pain management. The findings indicated that individuals who received surgical treatment utilized topical anesthetics, took narcotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and muscle relaxants exhibited significantly increased odds of visiting anesthetists in relation to pain management. Consequently, the outcomes revealed that participants who underwent surgical treatment (OR = 10.3, 95% CI (2.703–39.244)), those who employed topical anesthetics (OR = 4.882, 95% CI (1.411–16.9)), individuals who used narcotics (OR = 5.545, 95% CI (1.579–19.5)), those who took NSAIDs (OR = 4.427, 95% CI (1.739–11.3)), and those who utilized muscle relaxants (OR = 23.5, 95% CI (1.551–355.005)) were notably more inclined to seek consultations with anesthetists for pain management. To validate the aforementioned findings, a multivariate analysis was conducted, and the results substantiated the associations mentioned earlier.
Discussion
The present study examined the sociodemographic and clinical characteristics of participants in relation to their pain experience, therapeutics, and therapeutic approaches for pain management. The findings highlighted several important trends and associations that contribute to our understanding of pain prevalence, intensity, and management strategies within the studied population. The study revealed that a significant proportion of participants experienced pain, with the chronic type being predominant among those reporting pain. The prevalence of pain differed across age groups, with higher rates observed in the elderly, followed by middle-aged individuals, and then younger participants; however, the results from this subgroup are based on a limited number of respondents in this age group and should be interpreted with caution. This pattern is consistent with previous research indicating an increased likelihood of pain among older individuals probably due to age-related physiological changes and associated medical conditions.15,16
Marital status and educational level demonstrated significant associations with pain prevalence. Married participants reported higher pain prevalence compared to unmarried individuals, which might be attributed to the additional stressors and responsibilities that come with marriage and family life. 17 Furthermore, lower educational levels were associated with higher pain prevalence, potentially reflecting differences in health knowledge, access to healthcare, and occupational factors, Nevertheless, it is important to note that the outcomes within this specific subgroup rely on a relatively small number of, and thus, they should be approached with care. 18 It is worth noting that literacy and elementary rates in Palestine are among the lowest in the world, which could explain the limited number of respondents. 19
Participants utilized a variety of approaches to manage their pain, including self-medication, visits to physicians, complementary medicine, and physical therapy. Notably, the elderly group showed a preference for traditional medical interventions, such as visits to physicians and hospital-based treatments. These findings align with age-related preferences for healthcare-seeking and management strategies. 20 On the other hand, elderly patients often favor traditional medical interventions, such as visits to physicians and hospital-based treatments, probably due to their trust in established healthcare practices, familiarity and comfort with these settings, long-term physician–patient relationships, and the perception of comprehensive care, health insurance coverage, and limited exposure to alternative healthcare options. 21
Gender disparities in pain management approaches were evident, as women demonstrated a greater propensity to seek consultations with anesthesiologists or pain specialists. This pattern aligns with the broader recognition of gender-based distinctions in chronic pain experiences. Studies indicate that women tend to grapple with chronic pain conditions, like fibromyalgia and migraines, at elevated rates compared to men. 22 Hormonal factors, linked to fluctuations in estrogen levels, are believed to play a role in shaping pain perception, potentially contributing to the observed preference for specialized care. 23 These findings suggest that gender-specific pain experiences and variations in healthcare-seeking behaviors may underpin these disparities. 22
Various factors played a pivotal role in shaping the selection of therapeutic strategies for pain management. Notably, individuals with higher educational attainment exhibited a decreased inclination toward conventional medical interventions, including consultations with physicians, hospital-based treatments, and seeking guidance from anesthesiologists or pain specialists. This trend might be attributed to the heightened awareness of self-medicating practices among individuals possessing advanced education. 24
The distribution of therapeutics utilization among participants experiencing pain is depicted in Figure 2. Notably, acetaminophen emerged as the most prevalent choice, exhibiting the highest proportion among respondents. Following acetaminophen, other commonly adopted strategies encompass physical therapy, engagement in physical activities, and the incorporation of herbal treatments. By contrast, the least frequently employed interventions comprised more specialized methods, such as TENS, psychotherapies, and anti-epileptic medications. These findings underscore the prominence of accessible and familiar treatments like acetaminophen, physical therapy, and herbal remedies in the participants’ repertoire for pain management while also indicating a lower inclination toward more advanced interventions like TENS, psychotherapy, and anti-epileptic drugs.25,26
Figure 2.
Distribution of therapeutics utilized by participants encountering pain.
The data reveal noteworthy associations between certain factors and the choices participants made regarding pain management strategies. It is intriguing to note that the utilization of anxiolytics correlated with the practice of self-medication. This association might stem from the intricate nature of pain and its broader implications on daily life. It suggests that individuals grappling with symptoms beyond pain, such as anxiety, sleep disturbances, mood fluctuations, or a diminished sense of well-being, could potentially turn to self-medication as a means to alleviate both their emotional distress and physical discomfort. 27 Similarly, certain specific medications like acetaminophen and topical anesthetics demonstrated a linkage to seeking medical consultation from physicians. This trend indicates a preference for expert intervention when engaging with these medications, underscoring the inclination toward professional guidance in managing pain in conjunction with these substances. 28
The data also highlight the associations between certain medications and the increased probability of seeking complementary medicine for pain management. Participants who received herbs or narcotics for pain management showed a heightened likelihood of utilizing complementary approaches. This finding suggests that individuals who use herbal remedies or narcotics might be more open to alternative or holistic interventions, seeking a multifaceted approach to pain relief. 29
The study’s findings elucidate the associations between certain interventions and participants’ inclination to choose physical therapy for pain management. Specifically, receiving heat and cold therapy was significantly correlated with a higher probability of seeking physical therapy. Conversely, participants who reported using acetaminophen were less likely to opt for physical therapy. These results indicate probably that individuals who engage in active interventions like heat and cold therapy might be more receptive to physical therapy as a complementary treatment strategy. On the other hand, those who rely solely on medication might not perceive the need for physical therapy.
The associations between specific interventions and seeking medical attention from anesthesiologists or pain specialists are also worth noting. Participants, who underwent surgical treatment, used topical anesthetics, consumed narcotics, NSAIDs, or muscle relaxants were significantly more inclined to seek consultations with anesthesiologists for pain management. These findings suggest that individuals who undergo surgical procedures require specific medications might perceive a need for specialized pain management expertise beyond what primary care physicians can provide. 30 The insights gained from these associations have practical implications for clinical practice. Healthcare providers need to be attuned to patients’ preferences and experiences when recommending pain management approaches. Tailoring interventions based on factors such as age, gender, medical history, and medication usage can lead to more effective and patient-centered pain management strategies. 31 Communication between healthcare providers and patients is crucial to ensuring that individuals make informed choices about their pain management options. 32
The study offers valuable insights into the subject under investigation. However, it is imperative to acknowledge and emphasize the inherent limitations of this research. The cross-sectional design, while informative, inherently constrains the ability to establish causal relationships between variables. Future research endeavors employing longitudinal designs are essential to unravel the intricate dynamics and causal pathways underpinning various factors and pain management choices over time.
Moreover, delving deeper into the intricate web of cultural and socioeconomic factors is imperative to gain a more comprehensive understanding of how these elements influence the general population’s approach to pain management. Cultural factors encompass a wide array of beliefs, traditions, and practices that can significantly shape individuals’ perceptions of pain and their strategies for coping with it. These might include cultural attitudes toward stoicism, expression of pain, and the use of alternative or traditional healing methods. Understanding these nuances could illuminate why some communities might be more prone to underreporting or overlooking pain issues, while others are more proactive in seeking help or treatments.
Socioeconomic factors, on the other hand, play a crucial role in determining access to healthcare and the quality of available treatments. People from different socioeconomic backgrounds often face distinct challenges when it comes to pain management. For instance, individuals with higher income levels may have easier access to pain specialists, advanced treatments, and prescription medications. Conversely, those with limited financial resources might be forced to prioritize economic concerns over their pain, potentially leading to delayed or inadequate pain management.
Investigating these cultural and socioeconomic factors more thoroughly in future iterations of research can shed light on how they intersect and influence pain management decisions. By doing so, we can better tailor healthcare interventions and policies to address the specific needs of diverse populations, ultimately improving the overall approach to pain management across society.
It is also crucial to recognize that the study’s voluntary survey may have introduced selection bias, as respondents who volunteered to participate might differ from those who did not. While the findings provide valuable insights into the general population’s approach to pain in Palestine, they should be interpreted with the understanding that they may not be fully generalizable to all groups.
In light of these considerations, this study represents an initial step in understanding how the general population in Palestine approaches pain. The commitment is to address the limitations of this current research and expand the knowledge in this area through future studies, as outlined above. This commitment reflects the dedication to advancing the field and contributing to evidence-based healthcare practices and policy development in the context of pain management.
Limitations
This study’s limitations include possible selection bias due to snowball sampling methods. Its cross-sectional design limits the establishment of causal relationships. The sample consists of internet and social media users, potentially excluding others. Addressing these limitations in future research is essential for a more comprehensive understanding of pain management practices among diverse populations.
Conclusion
This study has provided valuable insights into the intricate interplay between sociodemographic characteristics, pain experiences, and the choices of therapeutic approaches for pain management. The findings underscore the importance of tailoring pain management strategies to align with individual characteristics such as age, marital status, education level, and gender-specific preferences. These findings highlight the significance of considering these factors in the design of pain management interventions, aiming to enhance treatment outcomes and overall patient satisfaction. Moreover, the associations identified in this research offer a comprehensive perspective for healthcare providers to develop personalized pain management interventions. By recognizing the nuanced relationships between specific factors and preferred pain management strategies, healthcare professionals are better equipped to offer targeted and effective care. This knowledge empowers healthcare practitioners to optimize the patient experience and ensure that pain management strategies are aligned with individual needs and preferences, ultimately contributing to more patient-centered and successful outcomes.
Acknowledgments
We thank all participants who gave their time to make this project a reality. In addition, we express our thanks and gratitude to the faculty of medicine and health sciences, at An-Najah National University for their kind cooperation.
Footnotes
Authors’ contributions: All authors contributed equally.
Data availability: The data that support the findings of this study are available from the corresponding author upon reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Trial registration: Not applicable.
ORCID iD: Anas Hamdan  https://orcid.org/0000-0002-1511-2916
https://orcid.org/0000-0002-1511-2916
References
- 1. Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb Mortal Wkly Rep 2023; 67: 1001–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Riad M, Reyala A. Nursing students’ knowledge and attitude toward pain management in Gaza Strip, Palestine. J Clin Anesth Pain Manag Open Access 2020; 4: 101–106. [Google Scholar]
- 3. Wu A, March L, Zheng X, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med 2020; 8: 299–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. El-Metwally A, Shaikh Q, Aldiab A, et al. The prevalence of chronic pain and its associated factors among Saudi Al-Kharj population; A cross sectional study. BMC Musculoskelet Disord 2019; 20: 177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Health conditions in the occupied Palestinian territory, including east Jerusalem, and in the occupied Syrian Golan, https://apps.who.int/iris/handle/10665/2399 (2023, accessed 14 August 2023).
- 6. Rogger R, Bello C, Romero CS, et al. Cultural framing and the impact on acute pain and pain services. Curr Pain Headache Rep 1916; 27: 429–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bates K, Leone T, Ghandour R, et al. Women’s health in the occupied Palestinian territories: contextual influences on subjective and objective health measures. PLoS One 2017; 12(10): e0186610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Abu-Odah H, Molassiotis A, Liu J. Challenges on the provision of palliative care for patients with cancer in low- and middle-income countries: a systematic review of reviews. BMC Palliat Care 2020; 19: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lohman D, Schleifer R, Amon JJ. Access to pain treatment as a human right. BMC Med 2010; 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. PCBS | The International Population Day, 11/07/2023, https://www.pcbs.gov.ps/post.aspx?lang=en&ItemID=4544 (2023, accessed 14 August 2023).
- 11. Omer ZQ. Prospective study of oral health, pain and discomfort and success rates following insertion of orthodontic mini-implants. Sulaimani Dent J 2018; 5: 38–48. [Google Scholar]
- 12. King W. Acute pain, subacute pain, and chronic pain. In:Gebhart GF, Schmidt RF. (eds.) Encyclopedia of pain. Berlin, Heidelberg: Springer, 2013, pp. 60–63. [Google Scholar]
- 13. Weir CB, Jan A. BMI classification percentile and cut off points. StatPearls, https://www.ncbi.nlm.nih.gov/books/NBK541070/ (2023, accessed 16 October 2023). [PubMed]
- 14. Lin Z, Yang R, Li K, et al. Establishment of age group classification for risk stratification in glioma patients. BMC Neurol 2020; 20: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth 2019; 123: e273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. You DS, Ziadni MS, Hettie G, et al. Comparing perceived pain impact between younger and older adults with high impact chronic pain: a cross-sectional qualitative and quantitative survey. Front Pain Res 2022; 3: 850713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim GE, Kim EJ. Factors affecting the quality of life of single mothers compared to married mothers. BMC Psychiatry 2020; 20: 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Atkins N, Mukhida K. The relationship between patients’ income and education and their access to pharmacological chronic pain management: a scoping review. Can J Pain 2022; 6: 142–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. PCBS | The International Literacy Day on 08/09/2023, https://www.pcbs.gov.ps/post.aspx?lang=en&ItemID=4575 (2023, accessed 19 October 2023).
- 20. Rafati S, Baniasadi T, Dastyar N, et al. Prevalence of self-medication among the elderly: a systematic review and meta-analysis. J Educ Health Promot 2023; 12: 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Butterworth JE, Campbell JL. Older patients and their GPs: shared decision making in enhancing trust. Br J Gen Pract 2014; 64: e709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Casale R, Atzeni F, Bazzichi L, et al. Pain in women: a perspective review on a relevant clinical issue that deserves prioritization. Pain Ther 2021; 10: 287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jablonska B, Soares JJF, Sundin O. Pain among women: associations with socio-economic and work conditions. Eur J Pain 2006; 10: 435–447. [DOI] [PubMed] [Google Scholar]
- 24. Akbar N, Teo SP, Artini Hj-Abdul-Rahman HN, et al. Barriers and solutions for improving pain management practices in acute hospital settings: perspectives of healthcare practitioners for a pain-free hospital initiative. Ann Geriatr Med Res 2019; 23: 190–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Milani DAQ, Davis DD. Pain management medications. StatPearls, https://www.ncbi.nlm.nih.gov/books/NBK560692/ (2023, accessed 15 August 2023). [PubMed]
- 26. Hamdan A, Luna JD, Del Pozo E, et al. Diagnostic accuracy of two questionnaires for the detection of neuropathic pain in the Spanish population. Eur J Pain 2013; 18(1): 101–109. [DOI] [PubMed] [Google Scholar]
- 27. Moreira de Barros GA, Calonego MAM, Mendes RF, et al. The use of analgesics and risk of self-medication in an urban population sample: cross-sectional study. Braz J Anesthesiol 2019; 69: 529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Johnson A, Booker SQ. Population-focused approaches for proactive chronic pain management in older adults. Pain Manag Nurs 2021; 22: 694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jahromi B, Pirvulescu I, Candido KD, et al. Pharmaceutics herbal medicine for pain management: efficacy and drug interactions. Pharmaceutics 2021; 13(2); 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gauntlett-Gilbert J, Brook P. Living well with chronic pain: the role of pain-management programmes. BJA Educ 2018; 18: 3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haverfield MC, Giannitrapani K, Timko C, et al. Patient-centered pain management communication from the patient perspective. J Gen Intern Med 2018; 33: 1374–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hammel J. Technology and the environment: supportive resource or barrier for people with developmental disabilities? Nurs Clin North Am 2003; 38: 331–349. [DOI] [PubMed] [Google Scholar]