Abstract
Background:
Nursing and midwifery students do not feel adequately prepared during their clinical training to support women who breastfeed, demanding more effective communication skills and knowledge.
Aim:
The aim was to evaluate changes in students' breastfeeding knowledge.
Methods:
This was a mixed-methods quasi-experimental design. Forty students voluntarily participated. Using a 1:1 ratio, 2 groups were randomly created and completed the validated questionnaire ECoLaE (pre-post). The educational program consisted of focus groups, a clinical simulation, and a visit to the local breastfeeding association.
Findings:
The control group's posttest scores ranged from 6 to 20 (mean = 13.1, standard deviation [SD] = 3.0). The intervention group ranged from 12 to 20 (mean = 17.3, SD = 2.3). A Student's t test for independence samples was calculated (P < .005, t = 4.5, median = 4.2). The intervention group had a mean difference of 10 points in improvement (mean =10.53, SD = 2.20, min = 7, max = 14), whereas the control group had a mean of 6 points (mean = 6.80, SD = 3.03, min = 3, max = 13). The multiple linear regression explained the intervention's effect. The regression model had statistical significance (F = 4.87, P = 0.004), with an adjusted R2 = 0.31. The linear regression between the posttest scores and group variables after adjusting by age showed an increment of 4.1 points in the intervention posttest scores (P < .005, 95% confidence interval [CI] = 2.1-6.1).
Conclusions:
The educational program “Engage in breaking the barriers to breastfeeding” improved nursing students' knowledge.
Keywords: baccalaureate, breastfeeding, education, nursing, patient simulation, students
Breastfeeding provides nourishment and immune protection to newborns and infants. Additionally, it includes other benefits such as the decrease of the risk of cardiovascular disease, type 2 diabetes, and ovarian and breast carcinoma.1–3 However, although breastfeeding benefits are well known, exclusive breastfeeding rates are less than 40% in infants younger than 6 months, and plummet after the infant is older than 6 months. As a result, there is no compliance with World Health Organization (WHO) recommendations of maintaining breastfeeding up until 2 years or when the dyad (mother-child) decides to do so.3,4 In Spain, exclusive breastfeeding rates during the first 6 weeks of the infant's life are 68%, but they decrease to 53% at 3 months of life and to 25% at 6 months.5 Regarding why mothers stop breastfeeding or do not even contemplate it, studies have found several barriers that can be prevented. These barriers can cluster in 2: the dyad's breastfeeding challenges and those that come from professional counseling, advice, and practice. Notwithstanding, all might be addressed by nurses working as supporters and guides to overcome them.6–14 On one hand, the most common dyad's breastfeeding challenges are finding the best position for the baby to latch on the breast and developing sore nipples or mastitis. On this matter, the development of mastitis, without nursing support and guidance, can lead mothers to misbelieve that breastfeeding will no longer be an option or that they might have a low milk supply. Furthermore, family support or the lack thereof can also present breastfeeding challenges when the partner does not involve in the decisions or the grandmothers interfere, alleging that their own experiences are the best way to act. This barrier might also be prevented or solved with the guidance of nurses or midwives at the consult.8,11–13 Breastfeeding barriers that health professionals create are related to the lack of breastfeeding knowledge or clinical experience. Early formula supplementation should be considered carefully in the presence of low baby weight gain because it predicts earlier weaning.9,10 Breastfed babies usually lose more weight during the first weeks after being born than formula-fed ones. Common problems regarding excessive weight loss (>10%) are related to poor latches or low quantity of feedings.10,15 Ignoring these facts when advising about supplementation could lead to breastfeeding cessation, which could be prevented with feeding observation and education. Another professional related barrier is regarding breastfeeding-medication interactions, jaundice, or the breastfeeding observation. Anstey et al6 found lacking evidence-based practices among health professionals that counseled breastfeeding cessation due to “conservative interpretations by hospital nurses on test results for jaundice or hypoglycemia and providers telling mothers to stop breastfeeding when taking medications, without referring to any of the current literature.” Understanding predictors of early breastfeeding cessation, misbeliefs, and overcoming lactation knowledge gaps in health professionals are issues of clinical importance. It has been shown that establishing breastfeeding with initial success is paramount to creating long-term continuation. Women who breastfeed for 6 to 8 weeks are more likely to continue for 6 to 12 months.16 On this point, general nurses take care of healthy newborns and their mothers, confronting the first problems and questions in situ and dissolving existing misbeliefs and errors while reassuring mothers.4,17,18 However, breastfeeding knowledge and attitudes of general/registered nurses and midwives are sometimes low or lack evidence-based background.19,20 In addition, breastfeeding training in both knowledge and clinical skills starts in college, where the conscience that nurses and midwives are breastfeeding promoters should be encouraged. Several reviews and cross-sectional studies reveal that nursing and midwifery students do not feel adequately prepared during their clinical training to support women who breastfeed, demanding more effective communication skills and knowledge.22–30 There are validated tools to assess breastfeeding knowledge in health professionals and nursing students,31,32 which allow health professionals and educators to create interventions to improve breastfeeding knowledge. Nonetheless, few interventions regarding nursing students' improvement in breastfeeding knowledge have been developed.33–36 The study aimed to evaluate changes in nursing students' breastfeeding knowledge by using a multicenter approach intervention, including theoretical, communication, and clinical training skills.
METHODS
Design
The present study was developed using a quasi-experimental pre-/postdesign using a mixed-methods approach. Pre- and posttests were used for data collection to make comparisons between them.
Sample
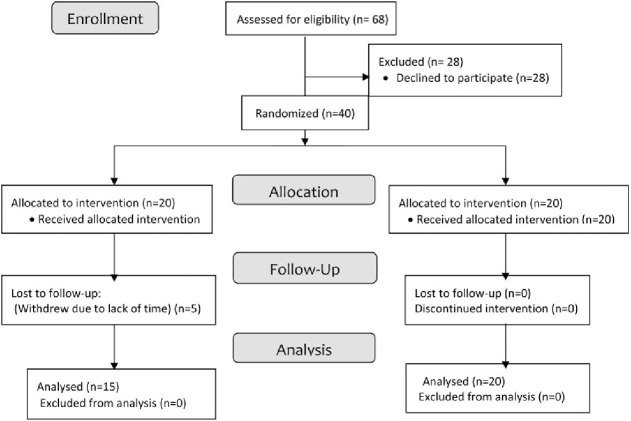
A convenience sample was selected from all the third-year nursing baccalaureate volunteers who were enrolled in the “Maternal and Paediatrics Nursing” subject in the Catholic University in Ávila in September 2019. Being 68 enrolled in the subject, a total of 40 students were willing to participate after the project's explanation and all participants signed an informed consent form. A randomized sample of 20 participants was selected among all 40 to take part in the intervention group; the other 20 students formed the control group. The inclusion criterion was being enrolled in the subject for the first time. The exclusion criterion was having had any experience from any clinical rotation in any Maternity and/or Paediatrics services. During the intervention, 5 students withdrew from the intervention group alleging lack of time. Figure 1 shows participants' progress in the study.
Figure 1.
CONSORT 2010 flow diagram.
Intervention
The educational program carried out with the intervention group was named “Engage in breaking the barriers to breastfeeding.” It comprised 3 actions centered on finding the breastfeeding barriers that participants had and breaking them during the course of the first semester (September 2019 to January 2020) using different approaches. See calendar and program's overview in the Supplemental Digital Content Table (available at: http://links.lww.com/JPNN/A34). The first action consisted of a focus group. Following the requirements for the proper development of a focus group, which states that a focus group should not be comprised of more than 10 persons, participants were split into 2 groups of 10; thus, 2 focus groups were developed.37 Several themes were proposed to discuss in these focus groups such as students' own definition and duration of lactation, the kind of nourishment they had as babies and motives given by their mother, attitudes toward breastfeeding/formula feeding, mother's autonomy and support on the kind of nourishment given to her children, and whether they could name barriers to breastfeeding. This action took place before the beginning of the Maternal and Paediatrics subject at the university. The second action involved a clinical simulation and debriefing performed at the university's clinical skills and simulated hospital in which students ought to practice their communication skills and implement the Registered Nurses' Association of Ontario best practice guide about breastfeeding,38 which was handed to them in both extent and summarize versions prior to the action. Due to space limits, this action was developed twice and carried out using the same 2 groups from the focused group. Nursing students were presented with a scenario of a woman who had recently delivered her baby accompanied by the grandmother to their nursing appointment. Both the woman and the grandmother were played by experienced role-play university staff who worked at the simulated hospital developing several clinical simulations, and the baby was a simulation baby. The scenario revolved around the first baby's growth spurt without mentioning it, so students could guess it and educate the patients avoiding breastfeeding cessation and creating reassurance on the dyad. Two volunteer students would role-play as nurses while the rest of the group watched the performance in the debriefing classroom and could give their opinions to the researchers. During the consultation, the baby would be crying unless 1 of the 2 students picked the baby up or asked the mother to feed the baby to observe the breastfeeding technique (latch on the breast, position). The mother showed weariness and discomfort, and the grandmother would push bottle-feeding, arguing “shortness of milk” from the mother, baby weight loss, her good experiences with bottle-feeding, and the imperious need to stop the baby from crying. The grandmother would stop second-guessing the mother and the students when students addressed the information about growth spurt and baby weight loss. After the simulation there was a debriefing where students discussed their opinions on their scenario and the implication of the action to their own knowledge and experience. This action was performed in the middle of the semester when students had more knowledge on the subject. In the third action, students visited the city's breastfeeding association, so they could hear the mothers' experiences with breastfeeding and formula-feeding and saw and practice positions and latches from different babies in a less clinical environment. Eleven mothers with their lactating children from 4 months to 5 years old assisted to the action. The president of the association spoke about her breastfeeding barriers and how she overcame them through breastfeeding books and sorority. This action happened 1 week before the end of the subject. Finally, one last focus group was carried out 1 week before the examination to draw conclusions regarding misbeliefs and barriers to breastfeeding and evaluate the intervention.
All intervention actions were commanded and delivered by 2 nursing researchers from the university who were not related to the Maternal and Paediatrics subject and taught the students other subjects. The control group was exposed only to the Maternal and Paediatrics classes, which were taught by a midwife and a pediatric nurse who worked also in the field as registered nurses. The theoretical content of the subject related to breastfeeding included the definition and characteristics of breastfeeding, promotion, care, and recommendations regarding breastfeeding and pathological breastfeeding. At the end of the semester, researchers gave all the information from the intervention to the control group and the rest of the class. Feasibility was granted through the acceptance of the subject's professors to cooperate with the researchers in avoiding any exposure to the information regarding the intervention to preserve the information blindness between the control and intervention groups. All the students in the intervention group agreed to maintain silence about the formative actions occurring in the intervention to their peers in the control group and those nonparticipative students.
Data collection and instruments
Variation in knowledge between groups was the endpoint, which was analyzed using a validated questionnaire, the Lactation Knowledge Questionnaire, ECoLa in Spanish,30 in its nursing format ECoLaE.31 The ECoLaE questionnaire was found to have reliability with a Cronbach α coefficient of 0.86. The questionnaire contained 22 questions in which 14 of them were dichotomous true-false questions, 7 were multiple-choice questions with 1 correct option, and 1 was an open question. The evaluated areas of knowledge included characteristics of breastfeeding, common problems/barriers that lead to abandoning breastfeeding, mastitis, growth spurts, caesarean, limited weight gain, cracked nipples, and pharmacology treatment, latches techniques, WHO recommendations, breastfeeding counsel and the nursing role in breastfeeding, and formula feeding knowledge. There were also 2 extra questions concerning whether the students considered that nurses should be breastfeeding experts (yes/no) and whether they find themselves prepared to take care of the lactating dyad. This last question consisted of a 5-item Likert scale ranging from “absolutely not” to “completely prepared.” This last question did not score. The instrument scored based on the total number of correct answers thus, 22 points, in which less than 55% of correct answers meant very inadequate knowledge, 55% to 70% scored as inadequate knowledge, 70% to 85% scored as good knowledge, and more than 85% scored as excellent. Students from both groups completed the pretest questionnaire during the explanation session on the first day of the semester before any class had started. They completed the posttest a week before the final examination took place. The sociodemographic variables collected were age, sex, number of children, and professional experience. Furthermore, the intervention group generated qualitative data in both focus groups. All conversations were recorded and transcribed verbatim to be further analyzed. In the clinical simulation and visit to the city's breastfeeding association, students were asked about the implications, educational benefits, and pertinence of the actions using ad hoc auto-administered questionnaires evaluating the interventions and their breastfeeding knowledge progress. These questionnaires had 5 open questions. All conversations about the debriefing of the clinical simulation were recorded and transcribed verbatim to be further analyzed. The mothers who participated at the association's gathering answered 3 open questions regarding their feelings about the interaction with students. These qualitative data were recorded to consider whether further implication with the association would be useful for everyone.
Ethical considerations
Every participant in the study was a volunteer. The academic and research commission of the University approved the study. The researchers asked the students to register the last 3 digits of their ID number on the tests to compare individual scores maintaining confidentiality. All participants from both the control and intervention groups signed an informed consent in which they agreed to collaborate and acknowledge that the divulgation of the findings would be anonymous and the possibility of freely withdrawing from it at any time. Student data were handled and controlled by the principal researcher and kept in a locked environment. Students were protected from ethical harm by the former arguments. At the end of the study, all information provided to the intervention group was offered to every student enrolled in the subject.
Data analysis
Statistical analysis was carried out using IBM SPSS Statistics v25. Test scores were calculated from both the control and intervention groups and a group mean was calculated within groups. Means were evaluated using an F test to determine whether the variances were equal to select the correct t test. To determine whether the control and intervention groups had different pre- and posttest scores, the t test for unpaired samples was calculated. To determine students' improvement, a t test for paired samples was calculated. The intervention effect in the posttest scores was calculated using multiple linear regression adjusted by age, having a child of their own, and nursing assistant experience. The generated qualitative data were recorded verbatim and transcribed.
RESULTS
A total of 20 students comprised the control group and 15 the intervention group. Table 1 shows the descriptive results of the characteristics of both groups. All participants were female in the control group and 93% of the intervention group with 1 male.
Table 1. Characteristics of the sample.
| Group | Age | Health assistant | Own children | |||
|---|---|---|---|---|---|---|
| Intervention | n = 15 | Mean = 21 years old | Yes n = 1 | 7% | No n = 15 | 100% |
| 43% | Min 19, max 25 | No n = 14 | 93% | |||
| Control | n = 20 | Mean = 25 years old | Yes n = 6 | 30% | Yes n = 1 | 5% |
| 57% | Min 19, max 52 | No n = 14 | 70% | No n = 19 | 95% | |
Quantitative findings: Breastfeeding knowledge
The control group's pretest scores ranged from 2 to 12 (mean = 6.25, standard deviation [SD] = 2.67, 95% confidence interval [CI] = 5.00-7.50), and the scores of the intervention group ranged from 2 to 12 (mean = 6.73, SD = 2.54, 95% CI = 5.32-8.14; see Table 2). There was no difference between groups in the pretest using Student's t test for independence samples (P = .59, t = 0.54, mean difference = 0.48, 95% CI = −1.33 to 2.30). Table 3 resumes the pre- and posttest correct responses of students. The control group's posttest scores ranged from 6 to 20 (mean = 13.05, SD = 3.01, 95% CI = 11.64-14.46) and the scores of the intervention group ranged from 12 to 20 (mean = 17.27, SD = 2.28, 95% CI = 16.00-18.53). A Student's t test for independence samples was performed on the posttest of both groups showing a statistical significance between groups (P < .005, t = 4.52, mean difference = 4.21, 95% CI = 2.32-6.11). A Student's t test for paired samples was performed in both pre- and posttest scores of the 35 students presenting statistical significance (P < .005, t = 15.22; 95% CI = 7.27-9.52). The intervention group had a mean difference of 10 points in improvement (mean = 10.53, SD = 2.20, min = 7, max = 14), whereas the control group had a mean of 6 points (mean = 6.80, SD = 3.03, min = 3, max = 13). The multiple linear regression explained the intervention's effect. The regression model had statistical significance (F = 4.87, P = .004), with an adjusted R2 = 0.31. After the variable adjustment, students' age, having a child of their own, and nursing assistant experience, the test score incremented in 4.1 points for the intervention group regarding the control group (95% CI = 2.1-6.1) with statistical significance (P < .005).
Table 2. Score means pre- and post-test between groups.
| Mean | Score percentage | Quality score | 95% confidence interval | Standard deviation | ||
|---|---|---|---|---|---|---|
| Pretest | Intervention | 6.73 | 35.59% | Very inadequate | 5.32-8.14 | 2.54 |
| Control | 6.25 | 28.4% | Very inadequate | 5.00-7.50 | 2.67 | |
| Posttest | Intervention | 17.27 | 78.5% | Good knowledge | 16.00-18.53 | 2.28 |
| Control | 13.05 | 59.54% | Inadequate | 11.64-14.46 | 3.01 | |
Table 3. Percentages of control intervention and total groups that responded correctly.
| Items (translated from Spanish) | Pretest | Posttest | ||||
|---|---|---|---|---|---|---|
| Control, % | Intervention, % | Total, % | Control, % | Intervention, % | Total, % | |
| 1. Having mastitis should be a cause for breastfeeding cessation (F) | 50 | 53 | 51 | 95 | 100 | 97 |
| 2. 15-min feedings from both breasts every 2-3 h should be recommended (F) | 5 | 7 | 6 | 65 | 87 | 74 |
| 3. Exclusive bottle-feeding is associated with a high risk of morbidity/mortality (T) | 15 | 13 | 14 | 60 | 79 | 68 |
| 4. Most caesarean-born babies require formula supplementation in the first hours (F) | 40 | 87 | 60 | 70 | 86 | 77 |
| 5. In case of supplementation (formula or breast milk), it is highly recommended to avoid the feeding bottle, especially during the first weeks after being born (T) | 30 | 13 | 24 | 45 | 93 | 66 |
| 6. A high frequency of breast-feedings lowers the risk of needing phototherapy (T) | 25 | 7 | 17 | 75 | 86 | 79 |
| 7. A healthy newborn needs to be tested in Apgar and get the prophylactic treatment for hemorrhages prior to breastfeed (F) | 15 | 73 | 9 | 10 | 33 | 20 |
| 8. In preemies born <32-wk gestation, breast milk is the best choice, followed by bank breast milk and leaving preemies' formula supplementation as the last alternative (T) | 35 | 53 | 44 | 55 | 87 | 69 |
| 9. A 15-h newborn who needs to be awakened to feed is considered an at-risk baby (F) | 35 | 13 | 26 | 21 | 60 | 38 |
| 10. After 12 mo of breastfeeding, the milk has fewer nutrients than the breast milk from the first year (F) | 20 | 20 | 20 | 50 | 71 | 59 |
| 11. A healthy breastfed baby who does not gain weigh needs formula supplementation (F) | 10 | 13 | 11 | 60 | 93 | 74 |
| 12. After 6-mo breastfeeding, feedings should be reduced to 2-3 times a day and introduce the other food (F) | 25 | 13 | 20 | 65 | 80 | 71 |
| 13. The “watery milk” is the foremilk, which is the first milk that flows at the star of pumping or nursing (T) | 20 | 27 | 23 | 90 | 93 | 91 |
| 14. The following picture shows an effective latch (F) | 50 | 33 | 43 | 80 | 100 | 89 |
| 15. WHO recommendations about breastfeeding time (option c) | 35 | 47 | 40 | 90 | 87 | 89 |
| 16. Possible taken cares with a mother having sore or cracked nipples (option c) | 5 | 7 | 6 | 55 | 73 | 63 |
| 17. Clinical case showing growth spurt (option b) | 15 | 33 | 25 | 47 | 86 | 64 |
| 18. Characteristics of an effective latch | 50 | 53 | 51 | 95 | 100 | 97 |
| 19. Attitude toward a mother with intentions of bottle-feeding her baby (option b) | 60 | 80 | 69 | 70 | 100 | 83 |
| 20. Legislation of free formula milk samples (option a) | 20 | 20 | 21 | 42 | 67 | 53 |
| 21. Interactions pharmacological treatment and breastfeeding (option e) | 5 | 0 | 3 | 10 | 7 | 9 |
| 22. Breastfeeding observation (option d) | 25 | 27 | 27 | 80 | 93 | 85 |
| 23. Nurses as breastfeeding experts (yes) | 65 | 87 | 81 | 88 | 100 | 93 |
| 24. Do you feel prepared to take care of a breastfeeding dyad?a (5 = Completely prepared) | 20 | 7 | 14 | 10 | 7 | 9 |
| 24. Do you feel prepared to take care of a breastfeeding dyad? (4 = Mostly prepared) | 15 | 20 | 17 | 10 | 26 | 17 |
| 24. Do you feel prepared to take care of a breastfeeding dyad? (3 = More or less prepared) | 20 | 13 | 17 | 40 | 60 | 49 |
| 24. Do you feel prepared to take care of a breastfeeding dyad? (2 = A little prepared) | 10 | 40 | 22 | 25 | 7 | 17 |
| 24. Do you feel prepared to take care of a breastfeeding dyad? (1 = Absolutely not prepared) | 20 | 20 | 20 | ... | ... | ... |
Abbreviations: F, false; T, true; WHO, World Health Organization.
a3 answers missing from the control group.
Qualitative findings: Focus group, clinical simulation, and visit to the local breastfeeding association
From the first focus group, when asked about their own kind of nourishment, 66.66% of participants had been breastfed, 20% had been fed with formula, and 13.34% mixed fed (breast milk and formula). The early breastfeeding cessation problems and the percentages of breastfeeding duration are shown in Table 4. When asked about their attitudes toward breastfeeding/formula feeding, students did not have a strong position, giving mothers absolute autonomy to make the choice. About the barriers mentioned, mastitis was the most mentioned, followed by poor milk quality/quantity. The second action proved to be well received by the students expressing their need to practice some communication skills prior to confront actual patients: P3: “At first, it was really stressful so, being able to think a little because you know that it is a simulation it is really helpful. Communicate when a baby is crying with a mother absolutely exhausted it not easy, I think we should practice this kind of things more often.” P5: “There was a time when I didn't know how to talk to them because you know the right thing to do but don't know how to communicate it properly in such circumstances [...] I think it was really cool to be able to at least practice these skills that you are supposed and you know, expected to have.” P2: “I think the most difficult part for me was to communicate good, you know, properly, like to know the mother was listening and understanding [...] I was not ready to deal with three people all talking at the same time and at first it was really stressful.” P7: “If I have learned something today, it is that communication must be practiced and exercised, they weren't really sick, they just needed to talk and get a little guidance [...] I don't feel myself prepared yet.” The third action (meeting with mothers from the local breastfeeding association) was unanimously the best rated: P14: “It was the most interesting activity from the project [...] having a direct contact with mothers who are healthy and whose babies are also healthy was terrific, how they told us their experiences and also, we could actually be there while breastfeeding. Brilliant.” P4: “It has been really helpful to know that if you don't know something you can always recommend them to go visit the association [...] they were really charming and understandable. The best way to end the project.” P12: “Having this experience, all relaxed, having the opportunity to make all kinds of questions [...] I actually learned properly all the theory we have been studying in one afternoon. Awesome.” P15: “Learning from the mother's experiences was new to me and it was really humbling, you don't really think about the impact you made on people and this made me think.” Association mothers found the interaction with students a groundbreaking activity in which they could feel heard and considered rather than been advised to. The fact that the interaction was placed in the association's grounds permits them to feel being in a secure environment where they were the educators. M5: “I felt nervous at first because they were really listening, you don't see that every day.”
Table 4. Problems encountered leading to breastfeeding cessation.
| Percentage | Problems encountered leading to breastfeeding cessation | |
|---|---|---|
| <6-mo breastfeeding | 41.66% (n = 5) | No gain weight, poor milk quality, low milk, mastitis, difficult delivery process |
| 6-mo breastfeeding | 33.34% (n = 4) | Going back to work. Baby was eating solid food |
| >6-mo Breastfeeding | 25% (n = 3) |
M8: “I had really bad experiences with nurses when my baby was born, you know, I knew what I wanted to do [...] I didn't feel supported [...] these students were interested, hopefully my words will make them more emphatic.” From the last focus group their attitudes toward breastfeeding/formula feeding had changed, pivoting toward breastfeeding while respecting the mother's choice when properly informed. About the barriers, they agreed that health professionals might act as one and identified others such as mastitis, poor milk quality/quantity, incorrect latching/position, growth spurts, and family support.
DISCUSSION
The educational program reached higher breastfeeding knowledge and awareness among nursing students from the intervention group than the control group. Notwithstanding that fact, all participants gained expertise throughout the research because overall, all students scored higher in the posttest.
The current results add more scientific data regarding the improvement of breastfeeding knowledge in nursing students, which is currently an underdeveloped area, finding few similar researches using pre- and posttests in nursing students.33,35,36 Both Bozzette and Posner33 and Deloian et al35 used as an intervention both audiovisual and written materials. Folker-Maglaya et al36 employed a breastfeeding toolkit that contained theoretical information, case studies and demonstrations, and role-play in the intervention group. We believed that adding a mixed-methods approach could facilitate, record, and analyze students' opinions on the matter and create a discussion enhancing the whole experience and learning process. Regarding used the questionnaire, the ECoLa and ECoLaE questionnaires are employed in the Spanish-speaking countries by physicians and nurses for surveys,20,30 or as a measuring tool for educational interventions obtaining knowledge improvement in breastfeeding.39 However, there is no evidence that this questionnaire was employed in an educational intervention in nursing students before this research, opening a new opportunity for research in these countries. When analyzing the scores, the question with the lowest correct percentage in the pretest remained low in the posttest. The question asked: “Where would you look for pharmacological breastfeeding interaction?” This question refers to a webpage: e-lactancia.org, where health professionals and parents can easily verify whether their treatment and/or diet is breastfeeding compatible.40 This issue was managed by sending the answered questionnaire and emphasizing this website tool after the first semester ended. On this point, in the question: “How well prepared do you feel to take care and give solutions to a lactate dyad?” the intervention group in the posttest scored higher than the control group. However, this result should be considered cautiously because these scores could be explained by the Dunning-Kruger effect (ignorance tends to make people feel more ready for a task),41 and some students felt more prepared in the pretest when they had yet to receive any breastfeeding training. Concerning the first action of the educational program, we prioritized the focus group in order to help surface all misbeliefs and barriers they already had, and by asking and talking about the kind of nourishment students had in their lactation period as a baby, it provided them the opportunity of determining that even though 60% of the intervention students breastfed, only 2 of them did it up until 2 years and the other 40% had some misbeliefs involved such as mastitis, “bad or poor milking,” low baby weight gain, inadequate latching, or lack of family support. Deloian et al35 found that 34% of their participants thought that mothers should stop breastfeeding due to mastitis. Rhodes and Burgess14 also found during their workshop that students had the same thought about mastitis. In their survey on nursing students, Khriesat and Ismaile25 found the same issue in 53% of participants (n = 234). This misconception goes far back to 2006 when Spear28 detected that 29% of nursing students thought that mastitis was a reason to stop using the affected breast until the problem was resolved, and 52% of them expressed that the milk of the breast with mastitis should be pumped and discarded. Identifying these misbeliefs within their lives helped them empathize and take the task and intervention more seriously. Ahmed et al21 found in their survey on nursing students (n = 115) that 63% believed “having low milk” equals artificial milk supplementation. Confronting the existent barriers and be able to break them or at least talk about them with their peers before learning any new information may help them to acquire and use the learned evidence-based practice to support the breastfeeding dyad rather than relying on emotion, intuition, or tradition.42
The clinical simulation allowed them to express and practice the gained knowledge in a stressful yet controlled environment, enduring their communication skills and resilience.43 Students confirmed that this action taught them to maintain calm and confront one of the most common visits to the pediatrician nurse consult, the first growth spurt, which is one of the first barriers to breastfeeding if the mother thinks she has “low or weak milk flow,” does not know how to react, or health professionals do not bring the necessary support and understanding.17,44 Clinical simulation can reinforce knowledge and allow students to implement what they have learned.
Regarding the third action—visiting the city's breastfeeding association—to the author's knowledge, there is no research done uniting nursing students and breastfeeding associations to date. The breastfeeding association visitation was the best-rated action from the educational program. Students' comments showed great satisfaction. Furthermore, they reported that being able to experience and discuss the implications of breastfeeding children older than 3 years opened their minds, normalizing this practice, which reinforces the results of Zhuang et al.4 This action made students aware that counting with the associations is a win-win situation. We believe that this action should be considered by professors and clinicians alike to be further researched.
As limitations, we did not explore diversity, equity, inclusion, or racial implications, making our results not fully extrapolated. The convenience sample might have left behind those students who are less interested in learning about breastfeeding and may retain some breastfeeding barriers. Implementing the educational program for every student could mitigate this. This educational program needs to be studied and tested in other universities using a larger sample to evaluate its efficiency more accurately. More evidence is necessary to support the use of the program as a helpful learning tool, and further longitudinal research is needed in order to explore whether the knowledge and awareness remain over time.
CONCLUSION
The educational program named “Engage in breaking the barriers to breastfeeding” is effective and improves students' breastfeeding knowledge and awareness. Nurses are one of the leading workforces that can improve breastfeeding rates and create effective dyads capable of breaking myths, errors, and fears. Working with a multicenter educational approach enhances students' learning process and allows them to immerse in both theoretical and practical spheres of the matter.
Supplementary Material
Footnotes
Disclosure: The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
Each author has indicated that he or she has met the journal's requirements for Authorship.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (www.jpnnjournal.com).
Submitted for publication: November 25, 2022; accepted for publication: March 10, 2023.
Contributor Information
María del Valle Ramírez-Durán, Email: valleramirez@unex.es.
Carmen Gutiérrez-Alonso, Email: albapanda6@hotmail.com.
Luis Moreno-Casillas, Email: luis.moreno@ucavila.es.
Alicia Del Río-Gutiérrez, Email: zipangoyuju2@gmail.com.
Sergio González-Cervantes, Email: sergio.gonzalez@ucavila.es.
Valle Coronado-Vázquez, Email: valle.coronado@ufv.es, valleramirez@unex.es.
References
- 1.Chowdhury R, Sinha B, Sankar MJ, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr Int J Paediatr. 2015;104:96–113. doi:10.1111/apa.13102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen B, Jin K, Ding D. Breastfeeding and maternal cardiovascular risk factors and outcomes: a systematic review. PLoS One. 2017;12(11):1–27. doi:10.1371/journal.pone.0187923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Victora CG, Bahl R, Barros AJD, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. doi:10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 4.Zhuang J, Hitt R, Goldbort J, Gonzalez M, Rodriguez A. Too old to be breastfed? Examination of pre-healthcare professionals' beliefs about, and emotional and behavioral responses toward extended breastfeeding. Health Commun. 2020;35(6):707–715. doi:10.1080/10410236.2019.1584739. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Breastfeeding. http://www.who.int/topics/breastfeeding/en/ Published 2016
- 6.Anstey EH, Coulter M, Jevitt CM, et al. Lactation consultants' perceived barriers to providing professional breastfeeding support. J Hum Lact. 2018;34(1):51–67. doi:10.1177/0890334417726305. [DOI] [PubMed] [Google Scholar]
- 7.Brown A. What do women really want? Lessons for breastfeeding promotion and education. Breastfeed Med. 2016;11(3):102–110. doi:10.1089/bfm.2015.0175. [DOI] [PubMed] [Google Scholar]
- 8.DiTomasso D, Wambach KA, Roberts MB, Erickson-Owens DA, Quigley A, Newbury JM. Maternal worry about infant weight and its influence on artificial milk supplementation and breastfeeding cessation. J Hum Lact. 2022;38(1):177–189. doi:10.1177/08903344211000284. [DOI] [PubMed] [Google Scholar]
- 9.Dozier AM, Brownell EA, Thevenet-Morrison K, Martin H, Hagadorn JI, Howard C. Predicting maintenance of any breastfeeding from exclusive breastfeeding duration: a replication study. J Pediatr. 2018;203:197–203.e2. doi:10.1016/j.jpeds.2018.07.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flaherman VJ, Cabana MD, McCulloch CE, Paul IM. Effect of early limited formula on breastfeeding duration in the first year of life: a randomized clinical trial. JAMA Pediatr. 2019;173(8):729–735. doi:10.1001/jamapediatrics.2019.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li R, Fein SB, Chen J, Grummer-Strawn LM. Why mothers stop breastfeeding: mothers' self-reported reasons for stopping during the first year. Pediatrics. 2008;122(suppl 2). doi:10.1542/peds.2008-1315i. [DOI] [PubMed] [Google Scholar]
- 12.Morrison AH, Gentry R, Anderson J. Mothers' reasons for early breastfeeding cessation. MCN Am J Mateen Child Nurs. 2019;4(6):325–330. doi:10.1097/NMC.0000000000000566. [DOI] [PubMed] [Google Scholar]
- 13.Topolyan I, Xu X. Beliefs about the benefits of breastfeeding: formation and effects on breastfeeding intention and persistence. J Interdiscip Econ. 2019;31(2):143–164. doi:10.1177/0260107918809878. [Google Scholar]
- 14.Rhodes B, Burgess A. An innovative educational intervention to improve nursing students' knowledge, attitudes, and skills surrounding breastfeeding. Teach Learn Nurs. 2018;13(4):197–201. doi:10.1016/j.teln.2018.05.003. [Google Scholar]
- 15.Thulier D. Weighing the facts: a systematic review of expected patterns of weight loss in full-term, breastfed infants. J Hum Lact. 2016;32(1):28–34. doi:10.1177/0890334415597681. [DOI] [PubMed] [Google Scholar]
- 16.Gerd AT, Bergman S, Dahlgren J, Roswall J, Alm B. Factors associated with discontinuation of breastfeeding before 1 month of age. Acta Paediatr Int J Paediatr. 2012;101(1):55–60. doi:10.1111/j.1651-2227.2011.02405.x. [DOI] [PubMed] [Google Scholar]
- 17.Wagner LPB, de Azevedo Mazza V, Souza SRRK, Chiesa A, Lacerda MR, Soares L. Strengthening and weakening factors for breastfeeding from the perspective of the nursing mother and her family. Rev da Esc Enferm USP. 2020;54:e03563. doi:10.1590/S1980-220×2018034303564. [DOI] [PubMed] [Google Scholar]
- 18.Yang SF, Burns E, Salamonson Y, Schmied V. Expectations and experiences of nursing students in supporting new mothers to breastfeed: a descriptive qualitative study. J Clin Nurs. 2019;28(11–12):2340–2350. doi:10.1111/jocn.14836. [DOI] [PubMed] [Google Scholar]
- 19.Gavine A, MacGillivray S, Renfrew MJ, Siebelt L, Haggi H, McFadden A. Education and training of healthcare staff in the knowledge, attitudes and skills needed to work effectively with breastfeeding women: a systematic review. Int Breastfeed J. 2017;12(1):1–10. doi:10.1186/s13006-016-0097-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.González Vereda J, Luque RB, Dorado Díaz A, Martín Pérez P, Maté Enríquez T, Martín VN. ¿Cuánto saben de lactancia los sanitarios del área materno-infantil? Estudio de los 14 hospitales públicos de Castilla y León. Prediatría Atención Primaria. 2019;21(84):133–46. http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1139-76322019000200003&lng=es&nrm=iso. [Google Scholar]
- 21.Ahmed A, Bantz D, Richardson C. Breastfeeding knowledge of university nursing students. MCN Am J Matern Child Nurs. 2011:36(6):361–367. doi:10.1097/NMC.0b013e31822de549. [DOI] [PubMed] [Google Scholar]
- 22.Natan MB, Haikin T, Wiesel R. Breastfeeding knowledge, attitudes, intentions, and perception of support from educational institutions among nursing students and students from other faculties: a descriptive cross-sectional study. Nurse Educ Today. 2018;68:66–70. doi:10.1016/j.nedt.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 23.Blackman I, Sweet L, Byrne J. Using Rasch analysis to identify midwifery students' learning about providing breastfeeding support. Women Birth. 2015;28(3):228–235. doi:10.1016/j.wombi.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Dodgson JE, Bloomfield M, Choi M. Are health science students' beliefs about infant nutrition evidence-based? Nurse Educ Today. 2014;34(1):92–99. doi:10.1016/j.nedt.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 25.Khriesat W, Ismaile S. Negative attitudes & misinformation to breastfeeding among young generation in a nursing program. Aust J Med. 2017;10(11):934–940. doi:10.21767/AMJ.2017.3177. [Google Scholar]
- 26.Linares AM, Parente ADN, Coleman C. Attitudes, practices, and knowledge about human lactation among nursing students. Clin Lact. 2018;9(2):59–65. doi:10.1891/2158-0782.9.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pajalic Z. Nursing students' views on promoting successful breastfeeding in Sweden. Glob J Health Sci. 2014;6(5):63–69. doi:10.5539/gjhs.v6n5p63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spear HJ. Baccalaureate nursing students' breastfeeding knowledge: a descriptive survey. Nurse Educ Today. 2006;26(4):332–337. doi:10.1016/j.nedt.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Yang SF, Schmied V, Burns E, Salamonson Y. Breastfeeding knowledge and attitudes of baccalaureate nursing students in Taiwan: a cohort study. Women Birth. 2019;32(3):e334–3e40. doi:10.1016/j.wombi.2018.08.167. [DOI] [PubMed] [Google Scholar]
- 30.Gómez Fernández-Vegue M, Menéndez Orenga M. Validación de un cuestionario sobre conocimientos y habilidades en lactancia materna. An Pediatr. 2015;83(6):387–396. doi:10.1016/j.anpedi.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Lechosa Muñiz CL, Cobo Sánchez JL, Herrera Castanedo S, Cornejo del Río E, Mateo Sota S, Sáez de Adana Herrero M. ECoLaE: validación de un cuestionario sobre conocimientos y habilidades en lactancia materna para enfermería. Atención Primaria. 2020;52(6):373–380. doi:10.1016/j.aprim.2019.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marzalik PR. Breastfeeding Education in University Nursing Programs. Chicago, IL: University of Illinois, Health Sciences Center, ProQuest Dissertation Publishing; 2004:312–6830. [Google Scholar]
- 33.Bozzette M, Posner T. Increasing student nurses' knowledge of breastfeeding in baccalaureate education. Nurse Educ Pract. 2013;13(3):228–233. doi:10.1016/j.nepr.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 34.Cianelli R, Villegas N, Azaiza K, Henderson S, Hooshmand M, Peragallo N. Developing and testing an online breastfeeding training among undergraduate nursing students. Clin Nurs Stud. 2015;3(1):82–88. doi:10.5430/cns.v3n1p82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deloian BJ, Lewin LO, O'Connor ME. Use of a web-based education program improves nurses' knowledge of breastfeeding. J Obstet Gynecol Neonatal Nurs. 2015;44(1):77–86. doi:10.1111/1552-6909.12534. [DOI] [PubMed] [Google Scholar]
- 36.Folker-Maglaya C, Pylman ME, Couch KA, Spatz DL, Marzalik PR. Implementing a breastfeeding toolkit for nursing education. J Perinat Neonatal Nurs. 2018;32(2):153–163. doi:10.1097/JPN.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 37.Bender DE, Ewbank D. The focus group as a tool for health research: issues in design and analysis. Health Transition Review. 1994;4,63–79. https://www.jstor.org/stable/40652078?seq=3 [PubMed] [Google Scholar]
- 38.Registered Nurses' Association of Ontario. Lactancia Materna-Fomento y Apoyo al Inicio, la Exclusividad y la Conti-nuación de la Lactancia Materna para Recién Nacidos, Lactantes y Niños Pequeños. https://rnao.ca/sites/rnao-ca/files/bpg/translations/BPG_Lactancia_Materna.pdf. Published 2018.
- 39.Villalobos M. Estrategia de Enseñanza Aprendizaje Basado en Problemas para Mejorar el Conocimiento y Habilidades sobre la Consejería en Lactancia Materna en Médicos del Primer Nivel de Atención de la Unidad de Medicina Familiar No. 11 de Aguas Calientes. http://bdigital.dgse.uaa.mx:8080/xmlui/bitstream/handle/123456789/1467/426099.pdf?sequence=1&isAllowed=y. Published 2018.
- 40.Paricio-Talayero JM, Mena-Tudela D, Cervera-Gasch Á, et al. Is it compatible with breastfeeding? Int J Med Inform. 2020;14:104199. doi:10.1016/j.ijmedinf.2020.104199. [DOI] [PubMed] [Google Scholar]
- 41.Dunning D. The Dunning-Kruger effect. On being ignorant of one's own ignorance. Adv Exp Soc Psychol. 2011;44:247–296. doi:10.1016/B978-0-12-385522-0.00005-6. [Google Scholar]
- 42.Angell C, Taylor AM. Alien knowledge: preparing student midwives for learning about infant feeding-Education practice at a UK university. Nurse Educ Today. 2013;33(11):1411–1415. doi:10.1016/j.nedt.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 43.Chuisano SA, Anderson OS. Assessing application-based breastfeeding education for physicians and nurses: a scoping review. J Hum Lact. 2020;36(4):699–709. doi:10.1177/0890334419848414. [DOI] [PubMed] [Google Scholar]
- 44.Terzioğlu F, Yücel Ç, Koç G, et al. A new strategy in nursing education: from hybrid simulation to clinical practice. Nurse Educ Today. 2016;39:104–108. doi:10.1016/j.nedt.2016.01.009. [DOI] [PubMed] [Google Scholar]