Abstract
Rationale and objectives
Our multicentric study analysed clinical, radiologic and pathologic features in patients with atypical ductal hyperplasia (ADH) diagnosed with vacuum-assisted biopsy (VAB), to identify factors associated with the risk of upgrade, to develop a scoring system to support decision making.
Materials and methods
Patients with ADH on VAB under stereotactic/tomosynthesis guidance (2012–2022) were eligible. Inclusion criteria were availability of surgical histopathological examination of the entire lesion or radiologic follow-up (FUP) ≥ 24 months. VAB results were compared with surgical pathological results or with imaging FUP evolution to assess upgrade. A backward stepwise linear regression was used to identify predictors of upgrade. The discriminatory power of the model was calculated through the area under the receiver operating curve (ROC–AUC); the Hosmer–Lemeshow test was used to assess model calibration. The points system was developed based on the selected risk factors, and the probability of upgrade associated with each point total was determined.
Results
112 ADH lesions were included: 91 (91/112, 81.3%) underwent surgical excision with 20 diagnosis of malignancy, while 21 (21/112, 18.7%) underwent imaging FUP with one interval change (mean FUP time 48 months). Overall upgrade rate was 18.7% (21/112). Age, menopausal status, concurrent breast cancer, BIRADS classification and number of foci of ADH were identified as risk factors for upgrade. Our model showed an AUC = 0.85 (95% CI 0.76–0.94). The points system showed that the risk of upgrade is < 2% when the total score is ≤ 1.
Conclusion
Our scoring system seemed a promising easy-to-use decision support tool for management of ADH, decreasing unnecessary surgeries, reducing patients’ overtreatment and healthcare costs.
Keywords: Atypical ductal hyperplasia, Upgrade, Vacuum-assisted biopsy, Underestimation, Scoring system
Introduction
Atypical ductal hyperplasia (ADH) is an intraductal clonal epithelial cell proliferation which involves the terminal ductal lobular units (TDLUs). ADH shares with low-grade ductal carcinoma in situ (DCIS) the same histological and architectural features but, when no more than one TDLU is involved and the size of the low-grade intraductal proliferation is less than 2 mm, a diagnosis of ADH is made [1]. ADH usually presents as microcalcifications on mammograms, so its incidence increased after the introduction of population-based screening mammography [2] and it accounts about 15% of pathologic finding of minimally invasive breast biopsies [3, 4].
ADH is classified as lesion “with uncertain malignant potential”, or a “B3" lesion and it is considered a direct but nonobligate precursor as well as an independent risk factor for breast cancer [1]. To date, the last consensus conference on B3 lesions recommends surgical excision of ADH cases (considering follow-up only in special situations after multidisciplinary discussion) [5] due to its risk of upgrade at surgical excision of approximately 25% [6–9]. Therefore, the majority of surgical biopsies for ADH results in benign findings and in a substantially unnecessary surgical procedure. This emphasizes the need to identify women who are more likely to have a cancer and really need surgical excision, avoiding unnecessary surgical breast biopsies with surgical risk for the patient and healthcare costs.
In recent years, there has been an increasing debate over whether selected cases of ADH could receive only follow-up and many studies examined the radiological and histologic characteristics of ADH on percutaneous breast biopsies to determine features that would predict the risk of upgrade at surgical excision [10, 11]. Previous studies and a recent meta-analysis reported that the upgrade rate is lower when stereotactic biopsy is performed, a larger calliper of needle is used and targeted lesion is completely removed [12–15]. However, all data in literature are from single-institution studies.
Our multicentric study analysed clinical, radiologic and pathologic features in a large cohort of patients with ADH diagnosed with VAB under stereotactic/tomosynthesis (DBT) guidance, to identify factors associated with the risk of upgrade to cancer to develop a scoring system to support risk–benefit-based decision making.
Materials and methods
Study population
This is a multicentric observational retrospective study. Data were collected at three sites in Italy, and each single-centre study was approved by the local Institutional Review Board (IRB) (Protocol number 0078775/2023, 21/04/2023). Informed consent was obtained from all individual participants included in the study. Data collection and aggregation were performed in a fully anonymized way and in line with international legislation. The study was performed in accordance with the Declaration of Helsinki statement for medical research involving human subjects.
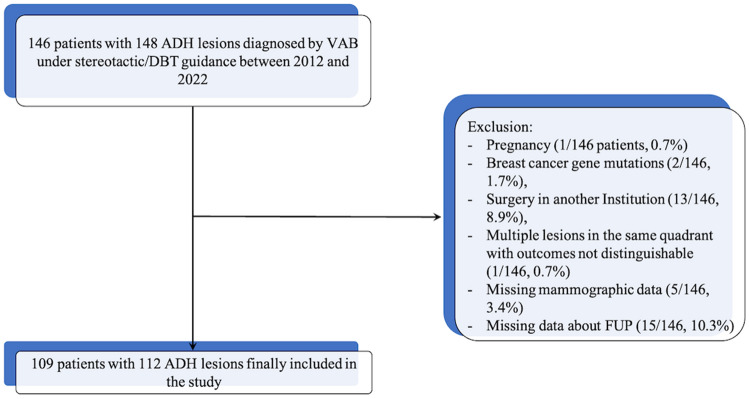
Patients with a diagnosis of ADH on VAB under stereotactic/tomosynthesis guidance from 2012 to 2022 were eligible for this study. Inclusion criteria were: availability of diagnostic surgical excision with histopathological examination of the entire lesion or radiologic follow-up (FUP) ≥ 24 months. A total of 146 women with 148 ADH lesions diagnosed by VAB under stereotactic/DBT guidance were initially identified. Pregnant women (1 of 146 patients, 0.7%), women with breast cancer gene mutations (2 of 146 patients, 1.7%), women who underwent surgery in another institution (13 of 146 patients, 8.9%), those with missing mammographic data (5 of 146 patients, 3.4%) or those without data about FUP (15 of 146, 10.3%) and those with multiple lesions in the same quadrant with outcomes not distinguishable (1 of 146 patients, 0.7%) were excluded. Patients with concurrent ipsilateral breast cancer were included when the sites of BC and ADH were separate, with the possibility to identify the surgical histopathological examination of ADH lesion. Finally, 109 patients with 112 ADH lesions were included in the analysis. The data selection process is given in Fig. 1.
Fig. 1.
Flow chart diagram of patient selection
Biopsy procedure
All stereotactic or DBT-guided breast biopsies were performed using 9G (Eviva or Suros ATEC® by Hologic, Marlborough, MA) or 11G (Mammotome® by Devicor Medical Products, Cincinnati, OH, USA) VAB devices, with 6–12 cores obtained from each biopsy site. When more than one target lesion in the same patient was identified, each one of them was biopsied and individually analysed.
Data collection
Clinical analysed data were abstracted from the electronic medical record and comprised age, premenopausal or postmenopausal status, family history of breast cancer, hormonal therapy, prior malignancy of the breast and concurrent ipsilateral or contralateral breast cancer.
Imaging and histologic features were collected with blinding to the outcome of cancer upgrade. The readings were performed by on-site readers. For each case, the pre-VAB magnified views (if target lesion was microcalcifications) and the pre- and post-biopsy mammograms were reviewed by two breast radiologist for Institution (with > 5 years’ experience in breast imaging) for the following imaging features: breast density, size of target lesion (maximum diameter), lesion type (opacity, microcalcifications, architectural distortion, asymmetry), American College of Radiology Breast Imaging Reporting and Data Systems (BI-RADS) 5th edition assessment category [16], microcalcifications in the retrieved cores (if target lesion was microcalcifications), complete removal of target lesion (checked with mammogram performed immediately after the biopsy) and radiology–pathology correlation. Mammographic breast density, Breast Imaging Reporting and Data System (BIRADS) category of suspicion and radiology–pathology correlation were assigned by the two breast radiologists in consensus.
Original slides from the VAB were reviewed by a pathologist of each Institution (all with more than 20 years’ experience and with special interest in breast pathology), for the following histologic features: number of foci of ADH, ADH pattern (solid, cribriform, micropapillary, other), ADH only in cores with microcalcifications (if target lesion was microcalcifications) and presence of any other B3 lesion.
Statistical analysis
The VAB examination results were compared with the surgical pathological results or with the imaging follow-up evolution to assess upgrade. The finding of cancer at surgical excision or during FUP is termed “upgrade”.
A backward stepwise linear regression was used to identify possible predictors of the outcome (ADH upgrade). At each step, variables were eliminated based on p values. The discriminatory power of the model was calculated through the ROC AUC. The Hosmer–Lemeshow test was used to assess model calibration.
To adapt the model to clinical work, a procedure similar to the development of the Framingham Risk Score [17] was applied. The points system was developed based on the risk factors of the multivariate model. The risk factors were organized into categories; if a risk factor is continuous (e.g. age), contiguous classes were set up. Reference values for each category were determined. A base category for each risk factor was chosen and the base category is the category assigned 0 points in the scoring system while categories reflecting worse (higher risk of upgrade) states of the risk factor were assigned positive points and categories reflecting better (lower risk of upgrade) states were assigned negative points. How far each category is from the base category was computed first in terms of regression units and then in points dividing the result by a constant (B, arbitrarily chosen). Finally, the risks (probability of upgrade) associated with each point total were determined [17].
Statistical analyses were performed using SPSS version 12.0 software (SPSS, Chicago, IL).
Results
Study population
One hundred and nine patients with 112 ADH lesions were included in the analysis. The mean age at diagnosis was 54 ± 9 (SD) years (range 39–83 years), and the mean lesion size was 19.6 ± 17.8 mm (SD). Figure 1 shows the flow chart of the study.
Of those 112 lesions, 91 (91/112, 81.3%) underwent surgical excision and 20 were diagnosed with a malignancy. Final pathology demonstrated 5 invasive cancers and 15 DCIS only. Of the five invasive cancers, two were tubular carcinomas and three were grade 1 invasive ductal carcinomas (one microinvasive). The remaining 21 ADH lesions (21/112, 18.7%) underwent surveillance by annual follow-up with mammogram and ultrasound (mean follow-up time 48 months), due to patient’s preference or patient’s comorbidities. Further sampling with VAB was performed in 1 cases with confirmation of ADH diagnosis. During follow-up, changes in mammographic findings leading to surgical excision were found in only one patient and pathological analysis of surgical excision revealed a malignant lesion (intermediate-grade invasive ductal carcinoma).
The overall upgrade rate was 18.7% (21/112), with a 5.3% (6/112) upgrade rate to invasive cancer and 13.4% (15/112) upgrade rate to DCIS only. Upgrade rates for surgically excised lesions and lesions treated with follow-up were 22.0% (20/91) and 4.8% (1/21), respectively.
Predictors of upgrade
Table 1 summarizes patient characteristics (clinical, radiologic and histopathologic factors). Backward stepwise regression analysis identified age, menopausal status, concurrent breast cancer, BIRADS classification and the number of foci of ADH as risk factors for subsequent ADH upgrade (Table 2). Our model showed an AUC = 0.85 (95% CI 0.76–0.94) (Fig. 2).
Table 1.
Patient characteristics and cancer upgrade
| N (%) of total (n = 112) | N (%) with upgrade (n = 21) | |
|---|---|---|
| Clinical features | ||
| Age | 54 ± 8.79 | 59 ± 9.93 |
| Menopausal status | ||
| Premenopausal | 55 (49.1) | 10 (18.2) |
| Postmenopausal | 57 (50.9) | 11 (19.3) |
| Family history of breast cancer | ||
| Yes | 33 (29.5) | 6 (18.2) |
| No | 79 (70.5) | 15 (19.0) |
| Hormone therapy | ||
| Yes | 33 (29.5) | 6 (18.2) |
| No | 79 (70.5) | 15 (19.0) |
| History of breast cancer | ||
| Yes | 4 (3.6) | 1 (25.0) |
| No | 108 (96.4) | 20 (18.5) |
| Concurrent breast cancer (ipsi or controlateral) | ||
| Yes | 4 (3.6) | 3 (75.0) |
| No | 108 (96.4) | 18 (16.7) |
| Radiologic features | ||
| Breast density | ||
| ACR category a–b | 48 (42.9) | 11 (22.9) |
| ACR category c–d | 64 (57.1) | 10 (15.6) |
| Type of mammographic lesion | ||
| Calcifications | 98 (87.5) | 17 (17.3) |
| Others (mass, architectural distortion, asymmetry) | 14 (12.5) | 4 (28.6) |
| Lesion size (maximum diameter) | ||
| < 2 cm | 75 (67.0) | 9 (12.0) |
| > 2 cm | 37 (33.0) | 12 (32.4) |
| BIRADS classification | ||
| 3–4A | 42 (37.5) | 4 (9.5) |
| 4B–4C–5 | 70 (62.5) | 17 (24.3) |
| Guidance | ||
| Stereotactic | ||
| Tomosynthesis | ||
| Biopsy needle gauge | ||
| 11G | 57 (50.9) | 7 (12.3) |
| 9G | 55 (49.1) | 14 (25.4) |
| Post-biopsy residual lesion | ||
| Yes | 66 (58.9) | 15 (22.7) |
| No | 46 (41.1) | 6 (13.0) |
| Histopathological variables | ||
| Number of foci ADH | ||
| Single | 65 (58.0) | 4 (6.1) |
| Multiple | 47 (42.0) | 17 (36.2) |
| Pattern of ADH | ||
| Micropapillary | 9 (8.0) | 2 (22.2) |
| Other | 57 (50.9) | 15 (26.3) |
| Missing | 46 (41.1) | 4 (8.7) |
| ADH only in cores with microcalcifications | ||
| Yes | 51 (45.5) | 11 (52.4) |
| No | 61 (54.5) | 10 (47.6) |
| Presence of any other high-risk lesion | ||
| Yes | 76 (67.9) | 14 (18.4) |
| No | 36 (32.1) | 7 (19.4) |
| Radio-pathological discordance | ||
| Yes | 9 (8.0) | 3 (33.3) |
| No | 103 (92.0) | 18 (17.5) |
Numeric data are presented as mean ± standard deviation. Nonnumeric data are presented as numbers of lesions with percentages in parentheses
ACR, American College of Radiology; ADH, atypical ductal hyperplasia; BIRADS, Breast Imaging Reporting and Data System
Table 2.
Multivariate logistic regression model
| Variables | OR | 95% CI | P value |
|---|---|---|---|
| Age | 2.54 | 1.05–6.16 | 0.038 |
| Menopausal status | |||
| Premenopausal | Reference | ||
| Postmenopausal | 0.18 | 0.033–0.99 | 0.049 |
| Concurrent breast cancer (ipsi or controlateral) | |||
| Yes | 31.82 | 1.20–843.81 | 0.039 |
| No | Reference | ||
| BIRADS classification | |||
| 3–4A | Reference | ||
| 4B–4C–5 | 5.60 | 1.06–29.52 | 0.042 |
| Number of foci ADH | |||
| Single | Reference | ||
| Multiple | 7.48 | 2.11–26.60 | 0.002 |
ADH, atypical ductal hyperplasia; BIRADS, Breast Imaging Reporting and Data System; CI, confidence interval; OR, odds ratio
Fig. 2.
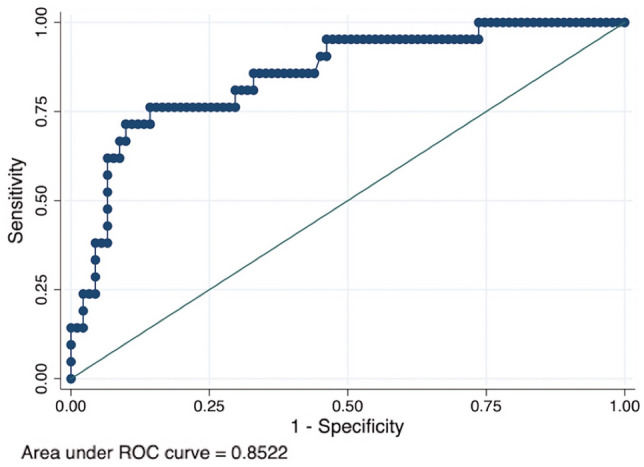
The receiver operating characteristic (ROC) curve for the scoring system. Area under the ROC curve = 0.85 (95% confidence interval 0.76–0.94)
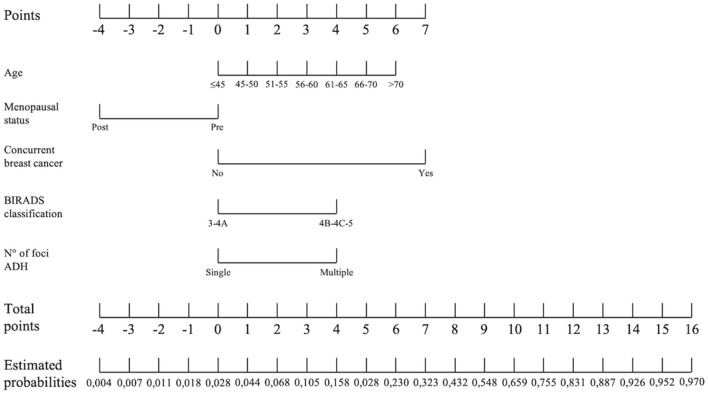
Scoring system
Based on the selected independent risk factors, we developed a points system to predict the probability of upgrade. The reference values, beta coefficients and points of each category of the significant factors in the multivariate model are shown in Table 3. Table 4 shows the estimated probabilities of upgrade associated with each point total, with increasing risk when the score increases (Fig. 3). Based on these results, a nomogram was created (Fig. 4). When the total score is ≤ 1, the risk of upgrade is less than 2% (Fig. 5).
Table 3.
Reference values, beta coefficients and points of each category of the significant factors in the multivariate model
| Risk factor | Categories | Reference value (Wi) | Beta | Beta (Wi-Wref) | B | Beta (Wi-Wref)/B |
|---|---|---|---|---|---|---|
| Age | < = 45 | 42,5 | 0,093424 | 0 | 0,467120 | 0 |
| > 45–50 | 47,5 | 0,093424 | 0,46712 | 0,467120 | 1 | |
| > 50–55 | 52,5 | 0,093424 | 0,93424 | 0,467120 | 2 | |
| > 55–60 | 57,5 | 0,093424 | 1,40136 | 0,467120 | 3 | |
| > 60–65 | 62,5 | 0,093424 | 1,86848 | 0,467120 | 4 | |
| > 65–70 | 67,5 | 0,093424 | 2,3356 | 0,467120 | 5 | |
| > 70 | 72,5 | 0,093424 | 2,80272 | 0,467120 | 6 | |
| Menopausal status | Pre | 0 | − 1,714877 | 0 | 0,467120 | 0 |
| Post | 0 | − 1,714877 | − 1,714877 | 0,467120 | − 4 | |
| Concurrent breast cancer | No | 0 | 3,460178 | 0 | 0,467120 | 0 |
| Yes | 0 | 3,460178 | 3,460178 | 0,467120 | 7 | |
| BIRADS classification | 3–4A | 0 | 1,723341 | 0 | 0,467120 | 0 |
| 4B–4C–5 | 0 | 1,723341 | 1,723341 | 0,467120 | 4 | |
| N° of foci ADH | Single | 0 | 2,012696 | 0 | 0,467120 | 0 |
| Multiple | 0 | 2,012696 | 2,012696 | 0,467120 | 4 |
ADH, atypical ductal hyperplasia; BIRADS, Breast Imaging Reporting and Data System; CI, confidence interval; OR, odds ratio
Table 4.
Estimated probabilities of upgrade of each point total of the scoring system
| Points | Estimated probabilities |
|---|---|
| − 2 | 0004 |
| − 1 | 0007 |
| 0 | 0011 |
| 1 | 0018 |
| 2 | 0028 |
| 3 | 0044 |
| 4 | 0068 |
| 5 | 0105 |
| 6 | 0158 |
| 7 | 0230 |
| 8 | 0323 |
| 9 | 0432 |
| 10 | 0548 |
| 11 | 0659 |
| 12 | 0755 |
| 13 | 0831 |
| 14 | 0887 |
| 15 | 0926 |
| 16 | 0952 |
| 17 | 0970 |
The estimated probabilities are expressed as decimal
Fig. 3.
Line graph showing the relationship between the point total (x-axis) and the risk of upgrade (y-axis)
Fig. 4.
Nomogram for predicting the risk of ADH upgrade
Fig. 5.
An example of the use of the model. Mediolateral oblique a, craniocaudal b and magnification c views of the right breast in a 46 years woman (1 point) in post-menopausal status (-4 points), without concurrent breast cancer (0 points), with microcalcifications classified as BIRADS 4B (4 points), with flat epithelial atypia with a single focus of ADH at VAB histopathological analysis (0 points) d. Using the developed points system, a final score of 1 was assigned with a corresponding risk < 2%. This lesion underwent surgical excision with only benign findings
Discussion
The present study is the first to develop a scoring system to predict the probability of upgrade in patients diagnosed with ADH at stereotactic/DBT-guided VAB. ADH is still a challenge for breast specialists: although most ADH is benign, surgical excision is still recommended because in the impossibility of identifying a subgroup of these lesions with a sufficiently low upgrade rate to obviate surgery [11, 15]. This leads to a huge number of unnecessary surgical excisions that represent an overtreatment, especially in the era of de-escalation where even for DCIS there is growing evidence that monitoring select cases is a safe alternative to standard surgical therapy [18, 19].
We selected only ADH diagnosed with stereotactic/DBT-guided VAB to reduce heterogeneity of data. Moreover, previous studies and a recent meta-analysis demonstrated that upgrade rate is significantly lower (about half) in this type of biopsy if compared to US-guided or MRI-guided biopsies [12–15], probably related to lesion type (prevalence of microcalcifications), larger core specimens and using the vacuum-assisted device, so a part of these lesions could be potentially suitable for follow-up instead of surgical excision, if correctly identified. We also decided to exclude mutations carrier patients, due to the high malignancy association of B3 lesions in this category of patients, which suggests that these lesions must always be surgically excised in high-risk women [20].
In our study, the underestimation rate was 18.7%, in line with previously published results [9, 10, 15, 21] and, even when only upgrade rate to invasive cancers is considered, a 5.3% of underestimation was found, indicating a too high percentage to safely avoid surgery. The present study identified higher age, concurrent breast cancer, 4b/4c/5 BIRADS classification and multiple foci of ADH as independent predictors of upgrade, while post-menopausal status was a negative predictor. We found that younger and pre-menopausal women are at higher risk of upgrade, as previously found by several studies [22–24]. Also, BIRADS classification of the lesion was confirmed to be a factor associated with upgrade [11]. The presence of an ipsilateral or contralateral BC resulted significantly associated with the risk of upgrade, justifying the simultaneous excision of both the breast cancer and the site of ADH (with one large lumpectomy or two separate lumpectomies) to accomplish the goal of removing the known cancer and ruling out additional malignancy at the site of ADH. Our results also confirmed that multiple foci of ADH on biopsy are associated with more frequent upgrade, as previously reported in several previous studies, using a cut-off of either < 2 foci [25, 26] or < 3 foci [27, 28]. We did not found a statistically significant difference in the upgrade rate between stereotactic and DBT guidance: most of ADH lesions (87.5% in our cohort) present as microcalcifications that can be correctly identified and biopsied under stereotactic guidance, without a significant improvement when DBT guidance is used (as we would expect for architectural distortions, better depicted with DBT). The complete removal of the target lesion did not enter our model. This factor was first considered as a safe condition to justify follow-up, but was subsequently demonstrated that the upgrade rate (also in cases with complete removal of target lesion) was still too high and the recommendation for follow-up in these cases was removed from the second edition of the consensus conference on B3 lesions [5]. The dimension of the lesion was not identified as a predictor of upgrade, too, while most of the previously published studies found a significant association between residual lesion and upgrade [11, 25, 26] and also the univariate analysis of our data demonstrated an association between diameter of the lesion and upgrade (p = 0.012, data not shown). However, since the purpose of our study is to identify possible predictors of the outcome (ADH upgrade) to build a scoring system, we used a backward stepwise linear regression, which builds a regression model from a set of candidate predictor variables by removing predictors based on p values, in a stepwise manner, using an automated method. Stepwise regression did not confirm the results of univariate analysis, probably because the diameter of the lesion has a less significant impact on upgrade if compared to the other predictors that entered the model. About ADH pattern, contrasting results have been published [25, 27] and our results did not find that micropapillary pattern significantly increased the risk of malignancy. Previous studies reported that the upgrade rate is significantly reduced when ADH is found only in specimens showing microcalcifications [11], while our data did not confirm this association. Finally, our data confirmed previously published results which showed that there is no association between ADH upgrade and the presence of other B3 lesions [12, 29–32]; it seems that, when ADH is present, its own risk of upgrade overwhelms the risk associated with other B3 lesions such as FEA, LN, papilloma or RS.
Our model showed an AUC = 0.85 (95% CI 0.76–0.94), indicating a good discriminatory power. A scoring systems was then developed as a statistical tool to predict the probability of upgrade and assist clinicians in decision-making. Ko et al. [33] previously proposed a scoring system for ADH diagnosed at ultrasound-guided CNB based on clinical, imaging and pathologic features, but they tested this score in only 34 patients and a subsequent validation study [34] demonstrated the low reproducibility of this score. The present scoring system demonstrated a high diagnostic performance to identify women at low risk (< 2%) of malignant upgrade when the total score is ≤ 1, thus this cut-off value can be used to define a subset of “probably benign” lesions, corresponding to a BIRADS category 3. These lesions could be safely sent to follow-up, reducing over-treatment and consequently morbidity and economic burden. Even if novel approaches, such as artificial intelligence [35, 36] or molecular markers [37, 38], seem to be promising ways forward, our tool, based on clinical, radiological and histopathological data, easy to retrieve in any reality, can be a useful tool in daily practice.
Limitations of the present study include its retrospective design and lack of a dataset to validate the performance of our model so we are working to validate our work prospectively on a larger, independent cohort. Moreover, our model is built only on ADH diagnosed with VAB under stereotactic/DBT guidance so it can be useful for decision-making only for a subset of ADH diagnosis. Lastly, we included in the study also women who did not undergo surgery (21/112, 18.7%) so, even if the median follow-up time is relatively long (48 months), it could be possible that indolent low-grade in situ cancer in patients who were managed conservatively may have not become evident in the imaging follow-up period.
In conclusion, our scoring system, based on clinical, radiologic and histopathologic parameters, seemed a promising easy-to-use decision support tool for management of ADH, decreasing unnecessary surgeries, reducing patients’ overtreatment and healthcare costs. Further work is needed to validate our model on independent datasets.
Funding
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The study was performed in accordance with the Declaration of Helsinki statement for medical research involving human subjects.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tavassoli FA (1999) Pathology of the Breast. Stamford, CT: Appleton & Lange
- 2.Georgian-Smith D, Lawton TJ. Controversies on the management of high risk lesions at core biopsy from a radiology/pathology perspective. Radiol Clin North Am. 2010;48(5):999–1012. doi: 10.1016/j.rcl.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Sutton T, Farinola M, Johnson N, Garreau JR. Atypical ductal hyperplasia: clinicopathologic factors are not predictive of upgrade after excisional biopsy. Am J Surg. 2019;217(5):848–850. doi: 10.1016/j.amjsurg.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 4.McGhan LJ, Pockaj BA, Wasif N, Giurescu ME, McCullough AE, Gray RJ. Atypical ductal hyperplasia on core biopsy: an automatic trigger for excisional biopsy? Ann Surg Oncol. 2012;19(10):3264–3269. doi: 10.1245/s10434-012-2575-0. [DOI] [PubMed] [Google Scholar]
- 5.Rageth CJ, O'Flynn EAM, Pinker K, et al. Second international consensus conference on lesions of uncertain malignant potential in the breast (B3 lesions) Breast Cancer Res Treat. 2019;174(2):279–296. doi: 10.1007/s10549-018-05071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mariscotti G, Durando M, Ruggirello I, et al. Lesions of uncertain malignant potential of the breast (B3) on vacuum-assisted biopsy for microcalcifications: Predictors of malignancy. Eur J Radiol. 2020;130:109194. doi: 10.1016/j.ejrad.2020.109194. [DOI] [PubMed] [Google Scholar]
- 7.Eby PR, Ochsner JE, DeMartini WB, Allison KH, Peacock S, Lehman CD. Frequency and upgrade rates of atypical ductal hyperplasia diagnosed at stereotactic vacuum-assisted breast biopsy: 9-versus 11-gauge. AJR Am J Roentgenol. 2009;192(1):229–234. doi: 10.2214/AJR.08.1342. [DOI] [PubMed] [Google Scholar]
- 8.Forester ND, Lowes S, Mitchell E, Twiddy M. High risk (B3) breast lesions: what is the incidence of malignancy for individual lesion subtypes? A systematic review and meta-analysis. Eur J Surg Oncol. 2019;45(4):519–527. doi: 10.1016/j.ejso.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Lucioni M, Rossi C, Lomoro P, et al. Positive predictive value for malignancy of uncertainmalignant potential (B3) breast lesions diagnosed on vacuum-assisted biopsy (VAB): is surgical excision still recommended? Eur Radiol. 2021;31(2):920–927. doi: 10.1007/s00330-020-07161-5. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen CV, Albarracin CT, Whitman GJ, Lopez A, Sneige N. Atypical ductal hyperplasia in directional vacuum-assisted biopsy of breast microcalcifications: considerations for surgical excision. Ann Surg Oncol. 2011;18(3):752–761. doi: 10.1245/s10434-010-1127-8. [DOI] [PubMed] [Google Scholar]
- 11.Nicosia L, Latronico A, Addante F, et al. Atypical ductal hyperplasia after vacuum-assisted breast biopsy: can we reduce the upgrade to breast cancer to an acceptable rate? Diagnostics (Basel) 2021;11(6):1120. doi: 10.3390/diagnostics11061120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rageth CJ, Rubenov R, Bronz C, et al. Correction to: Atypical ductal hyperplasia and the risk of underestimation: tissue sampling method, multifocality, and associated calcification significantly influence the diagnostic upgrade rate based on subsequent surgical specimens. Breast Cancer. 2021;28(1):246. doi: 10.1007/s12282-020-01186-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams KE, Amin A, Hill J, et al. Radiologic and pathologic features associated with upgrade of atypical ductal hyperplasia at surgical excision. Acad Radiol. 2019;26(7):893–899. doi: 10.1016/j.acra.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Zhang C, Wang EY, Liu F, Ruhul Quddus M, James SC. Type of architecture, presence of punctate necrosis, and extent of involvement in atypical ductal hyperplasia can predict the diagnosis of breast carcinoma on excision: a clinicopathologic study of 143 cases. Int J Surg Pathol. 2021;29(7):716–721. doi: 10.1177/10668969211010954. [DOI] [PubMed] [Google Scholar]
- 15.Schiaffino S, Calabrese M, Melani EF, et al. Upgrade rate of percutaneously diagnosed pure atypical ductal hyperplasia: systematic review and meta-analysis of 6458 lesions. Radiology. 2020;294(1):76–86. doi: 10.1148/radiol.2019190748. [DOI] [PubMed] [Google Scholar]
- 16.American College of Radiology (2013) ACR BI-RADS atlas: breast imaging reporting and data system (5th ed.), Reston, Virginia
- 17.Sullivan LM, Massaro JM, D'Agostino RB., Sr Presentation of multivariate data for clinical use: the framingham study risk score functions. Stat Med. 2004;23(10):1631–1660. doi: 10.1002/sim.1742. [DOI] [PubMed] [Google Scholar]
- 18.Narod SA, Iqbal J, Giannakeas V, Sopik V, Sun P. Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol. 2015;1(7):888–896. doi: 10.1001/jamaoncol.2015.2510. [DOI] [PubMed] [Google Scholar]
- 19.van Seijen M, Lips EH, Thompson AM, et al. Ductal carcinoma in situ: to treat or not to treat, that is the question. Br J Cancer. 2019;121(4):285–292. doi: 10.1038/s41416-019-0478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piccolo CL, Mallio CA, Messina L, et al. Radiological features of b3 lesions in mutation carrier patients: a single-center retrospective analysis. Appl Sci. 2023;13:4994. doi: 10.3390/app13084994. [DOI] [Google Scholar]
- 21.Bicchierai G, Pugliese F, Amato F, De Benedetto D, Boeri C, Vanzi E, Di Naro F, Bianchi S, Cossu E, Miele V, Nori J. Percutaneous vacuum-assisted excision (VAE) of breast lesions of uncertain malignant potential (B3 lesions): a preliminary single-centre Italian experience. Radiol Med. 2023;128(5):528–536. doi: 10.1007/s11547-023-01626-5. [DOI] [PubMed] [Google Scholar]
- 22.Degnim AC, Visscher DW, Berman HK, et al. Stratification of breast cancer risk in women with atypia: a Mayo cohort study. J Clin Oncol. 2007;25(19):2671–7. doi: 10.1200/JCO.2006.09.0217. [DOI] [PubMed] [Google Scholar]
- 23.London SJ, Connolly JL, Schnitt SJ, Colditz GA. A prospective study of benign breast disease and the risk of breast cancer. JAMA. 1992;267(7):941–439. doi: 10.1001/jama.1992.03480070057030. [DOI] [PubMed] [Google Scholar]
- 24.Dupont WD, Page DL. Relative risk of breast cancer varies with time since diagnosis of atypical hyperplasia. Hum Pathol. 1989;20(8):723–725. doi: 10.1016/0046-8177(89)90063-4. [DOI] [PubMed] [Google Scholar]
- 25.Peña A, Shah SS, Fazzio RT, et al. Multivariate model to identify women at low risk of cancer upgrade after a core needle biopsy diagnosis of atypical ductal hyperplasia. Breast Cancer Res Treat. 2017;164(2):295–304. doi: 10.1007/s10549-017-4253-1. [DOI] [PubMed] [Google Scholar]
- 26.Wagoner MJ, Laronga C, Acs G. Extent and histologic pattern of atypical ductal hyperplasia present on core needle biopsy specimens of the breast can predict ductal carcinoma in situ in subsequent excision. Am J Clin Pathol. 2009;131(1):112–121. doi: 10.1309/AJCPGHEJ2R8UYFGP. [DOI] [PubMed] [Google Scholar]
- 27.Allison KH, Eby PR, Kohr J, DeMartini WB, Lehman CD. Atypical ductal hyperplasia on vacuum-assisted breast biopsy: suspicion for ductal carcinoma in situ can stratify patients at high risk for upgrade. Hum Pathol. 2011;42(1):41–50. doi: 10.1016/j.humpath.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 28.Sneige N, Lim SC, Whitman GJ, et al. Atypical ductal hyperplasia diagnosis by directional vacuum-assisted stereotactic biopsy of breast microcalcifications Considerations. for surgical excision. Am J Clin Pathol. 2003;119(2):248–253. doi: 10.1309/0GYV4F2LLJAV4GFN. [DOI] [PubMed] [Google Scholar]
- 29.Ely KA, Carter BA, Jensen RA, Simpson JF, Page DL. Corebiopsy of the breast with atypical ductal hyperplasia: a probabi-listic approach to reporting. Am J Surg Pathol. 2001;25:1017–1021. doi: 10.1097/00000478-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Bianchi S, Caini S, Renne G, et al. Positive predictive value for malignancy on surgical excision of breast lesions of uncertain malignant potential (B3) diagnosed by stereotactic vacuum-assisted needle core biopsy (VANCB): a large multi-institutional study in Italy. Breast. 2011;20(3):264–270. doi: 10.1016/j.breast.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 31.Co M, Kwong A, Shek T. Factors affecting the under-diagnosis of atypical ductal hyperplasia diagnosed by core needle biopsies—a 10-year retrospective study and review of the literature. Int J Surg. 2018;49:27–31. doi: 10.1016/j.ijsu.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 32.de Mascarel I, Brouste V, Asad-Syed M, Hurtevent G, Macgrogan G. All atypia diagnosed at stereotactic vacuum-assisted breast biopsy do not need surgical excision. Mod Pathol. 2011;24(9):1198–206. doi: 10.1038/modpathol.2011.73. [DOI] [PubMed] [Google Scholar]
- 33.Ko E, Han W, Lee JW, et al. Scoring system for predicting malignancy in patients diagnosed with atypical ductal hyperplasia at ultrasound-guided core needle biopsy. Breast Cancer Res Treat. 2008;112(1):189–195. doi: 10.1007/s10549-007-9824-0. [DOI] [PubMed] [Google Scholar]
- 34.Bendifallah S, Defert S, Chabbert-Buffet N, et al. Scoring to predict the possibility of upgrades to malignancy in atypical ductal hyperplasia diagnosed by an 11-gauge vacuum-assisted biopsy device: an external validation study. Eur J Cancer. 2012;48:30–36. doi: 10.1016/j.ejca.2011.08.011. [DOI] [PubMed] [Google Scholar]
- 35.Bahl M, Barzilay R, Yedidia AB, Locascio NJ, Yu L, Lehman CD. High-risk breast lesions: a machine learning model to predict pathologic upgrade and reduce unnecessary surgical excision. Radiology. 2018;286(3):810–818. doi: 10.1148/radiol.2017170549. [DOI] [PubMed] [Google Scholar]
- 36.Aslan Ö, Oktay A, Katuk B, et al. Prediction of malignancy upgrade rate in high-risk breast lesions using an artificial intelligence model: a retrospective study. Diagn Interv Radiol. 2023;29(2):260–267. doi: 10.5152/dir.2022.211047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lopez-Garcia MA, Geyer FC, Lacroix-Triki M, Marchió C, Reis-Filho JS. Breast cancer precursors revisited: molecular features and progression pathways. Histopathology. 2010;57(2):171–192. doi: 10.1111/j.1365-2559.2010.03568.x. [DOI] [PubMed] [Google Scholar]
- 38.Polat AK, Soran A, Kanbour-Shakir A, Menekse E, Levent Balci F, Johnson R. The role of molecular biomarkers for predicting adjacent breast cancer of atypical ductal hyperplasia diagnosed on core biopsy. Cancer Biomark. 2016;17(3):293–300. doi: 10.3233/CBM-160641. [DOI] [PubMed] [Google Scholar]