Highlights
-
•
LACC patients sought information about treatment options, side effects, disease causes/symptoms, and patient experiences.
-
•
One-third of LACC patients sought a second opinion to confirm their diagnosis or to find a more favorable physician.
-
•
Challenges in information searches included use of medical jargon, finding relevant information, and assessing credibility.
-
•
Physicians fostered confidence in treatment plans by addressing patients’ concerns and offering understandable information.
-
•
Most LACC patients felt knowledgeable to participate in treatment decisions and felt engaged in shared decision-making.
Keywords: Locally advanced cervical cancer, Information needs, Patient engagement, Qualitative research
Abstract
Objective
This study aimed to identify the information needs and factors for making informed treatment decisions among a diverse group of locally advanced cervical cancer (LACC) patients.
Methods
Semi-structured interviews were conducted with LACC patients of diverse demographic and socioeconomic backgrounds within two years of their cancer diagnosis. Trained moderators asked open-ended questions about patients’ cancer journeys. Transcripts were analyzed using NVivo software to identify emergent themes.
Results
In 2022, 92 LACC patients in the United States (n = 26), Brazil (n = 25), China (n = 25), and Germany (n = 16) participated in the study. Physicians were valued sources of information, providing patients with details on prognosis, treatment options, and side effects. While most patients trusted their physicians, one-third sought a second opinion to validate their diagnosis or find a more trusted physician.
Most patients conducted their own research on treatment options, side effects, causes of LACC, symptoms, and others’ experiences. Challenges to information searches included understanding medical terms, finding relevant information, and evaluating source credibility.
Overall, patients felt knowledgeable enough to participate in treatment decisions, either by accepting the recommended treatment or collaborating with their physicians. Nearly one-third of patients desired a more significant role in the decision-making process.
Conclusion
This study highlights the importance of physicians providing LACC patients comprehensive and understandable information, while involving them in the decision-making process. Understanding LACC patients’ motivations to seek information and their willingness to actively engage in treatment decisions can lead to improved patient satisfaction in their cancer care.
1. Introduction
Patients with LACC face difficult medical decisions that may have long-term implications on their health, fertility, and sexuality (Hanprasertpong et al., 2017), which can lead to psychological distress (Adler et al., 2008). Cancer information can play a pivotal role in reducing the psychological burden associated with decision-making and empowering patients to confidently navigate their treatment journey (Eisfeld, Apr. 2020, Loiselle, 2019, Epstein and Jr, 2007, Wang et al., 2021, Rutten et al., 2005, Miller et al., 2003). By gaining a clear understanding of their diagnosis, patients can anticipate what to expect, plan for the future, and evaluate the potential benefits, risks, and outcomes of treatment options (Eisfeld, Apr. 2020, Loiselle, 2019).
Information can also play an important role in motivating patients to participate actively in the treatment decision-making process. Several studies have demonstrated that most cancer patients prefer to be involved in their treatment decisions and be well-informed about their cancer diagnosis (Epstein and Jr, 2007, Rutten et al., 2005, Hahlweg, 2020, Germeni and Schulz, 2014, Nagler, 2010, Stewart, 2000, Gwede, 2005). Providing patients with this information can lead to better clinical outcomes, psychological well-being, and treatment satisfaction (Epstein and Jr, 2007; Wang et al., 2021; Hahlweg, 2020; Kane et al., 2014). In our previous study on the information needs of metastatic, recurrent, and persistent cervical cancer (mrpCC) patients, we found that obtaining individualized and credible information on treatment options and prognosis resulted in feelings of empowerment and confidence in their care (Szamreta et al., 2022).
Cultural differences can influence information-seeking behaviors, needs, and preferences for information distribution (Lu et al., 2022). Stigmas surrounding human papillomavirus (HPV) infection, which accounts for approximately 91% of cervical cancer (CC) cases (Hopenhayn, 2014), may discourage people from seeking information in some cultures (Peterson, 2021). Low health literacy can also affect how patients understand or seek information (Samoil et al., 2021). In Asian countries, physicians are often heavily relied upon because of the cultural emphasis on interpersonal communication, but time constraints and cultural factors that discourage the disclosure of negative information may hinder their provision of information (Wang et al., 2021); studies regarding unmet information needs of Brazilian and German advanced cancer patients are lacking. Therefore, it is important to consider these cultural differences when assessing the information needs of LACC patients.
This study investigated the information-seeking behaviors of a diverse group of LACC patients from the United States (US), Brazil (BR), China (CN), and Germany (DE) to understand how patients acquire information and make treatment decisions. Additionally, we aimed to identify key factors that contribute to confident and informed decision-making.
2. Methods
2.1. Study design
Semi-structured 60-minute telephone interviews were conducted from March to November 2022 with LACC patients from Brazil, China, Germany, and the United States. These countries were selected to represent diverse demographic and socioeconomic backgrounds, with regard to race/ethnicity and urbanity/rurality, as well as distinct healthcare systems. In response to studies, including our own previous findings, indicating a cultural inclination among Chinese mrpCC patients to have limited involvement in their treatment decisions (Xie et al., 2020, Szamreta et al., 2022), we aimed to gather meaningful insights from Chinese patients who actively engaged in shared decision-making. To ensure a diverse range of perspectives, we included a subgroup of 10 Chinese patients who played an active role in their treatment decisions.
Convenience sampling was used in this study. Multiple channels were utilized to recruit a diverse sample of patients in each country, including physician referrals, patient advocacy groups, databases of patients who have opted into research studies, social media, direct marketing, and website banner placements. Our methodological approach to this study mirrored our previous study in mrpCC, with the exception of eligibility criteria and some interview questions tailored to LACC patients. Detailed information on recruitment sub-quotas and procedures, interview guide development based on COM-B (Michie et al., 2014), moderator selection, interview procedures, and deductive and inductive analysis has been previously described (Szamreta et al., 2022). A sample size of 16 to 26 per country was sufficient to attain information saturation, and no new key themes emerged in successive interviews.
The study was reviewed by the Pearl IRB and received Exemption Status on February 14, 2022.
2.2. Eligibility criteria
Eligible participants included high-risk LACC patients (FIGO 2014 stage IB2-IIB with node-positive disease or stage III-IVA) (Grigsby, 2020) who were diagnosed within two years prior to the interview and had already made a treatment decision. Patients who had already undergone and/or completed their treatment were included in the study. To ensure reliable recall of treatment modalities, a two-year window was chosen, which is supported by existing literature (Gast, et al., 2019; Simensen, 2019). Patients who had already made their treatment decision were selected to avoid potentially influencing their treatment decisions.
Patients excluded from the study were those who: 1) were initially diagnosed with stage IA, IVB, or metastatic cancer; 2) received definitive surgical, radiation, or systemic therapy for CC, including investigational agents or immunotherapy prior to their LACC diagnosis; 3) were not fluent in the local language; 4) did not provide informed consent; or 5) had hearing difficulties that would make a telephone conversation challenging.
3. Results
Between March and November 2022, we conducted one-on-one qualitative interviews with 92 patients diagnosed with LACC from Brazil (n = 25), China (n = 25), Germany (n = 16), and the US (n = 26). Sample sizes varied for each topic as not all topics were discussed with each patient.
Tables 1 and S1 present patient characteristics and demographics of the study. Our analysis of the qualitative data revealed four themes: motivations for information-seeking, patient confidence in their physician and treatment plan, patient engagement in the treatment decision, and challenges in searching for information.
Table 1.
Patient Characteristics.
| Characteristic | United States (n = 26) |
Brazil (n = 25) |
China (n = 25) |
Germany (n = 16) |
Total Patients (n = 92) |
|---|---|---|---|---|---|
| Age Median (SD) |
38 (9.0) |
35 (5.5) |
44 (14.5) |
51 (7.8) |
41 (11.0) |
| Min, Max | 28, 45 | 26, 49 | 30, 60 | 31, 87 | 26, 87 |
| Current stage at study recruitment Stage I |
0 (0.0%) |
4 (16.0%) |
1 (4.0%) |
1 (6.3%) |
6 (6.5%) |
| Stage II | 2 (7.6%) | 11 (44.0%) | 7 (28.0%) | 8 (50.0%) | 28 (30.4%) |
| Stage III | 21 (81.0%) |
8 (32.0%) |
16 (64.0%) |
2 (12.5%) |
47 (51.1%) |
| Stage IV | 3 (11.5%) |
2 (8.0%) |
1 (4.0%) |
0 (0.0%) |
6 (6.5%) |
| Don’t know/Don’t recall | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (6.3%) | 1 (1.1%) |
| Current treatment status Decided on a plan, but have not started Currently receiving treatment Completed treatment |
6 (23.1%) 6 (23.1%) 14 (53.8%) |
1 (4.0%) 7 (28.0%) 17 (68.0%) |
4 (16.0%) 14 (56.0%) 7 (28.0%) |
1 (6.3%) 0 (0.0%) 15 (93.8%) |
12 (13.0%) 27 (29.3%) 53 (57.6%) |
Note: These data were self-reported during the patient interviews; therefore, not all respondents may be represented. Percentages may not total 100% because of rounding.
SD, standard deviation; US, United States.
3.1. Theme 1: Motivations for Information-Seeking
3.1.1. Information shared with LACC patients
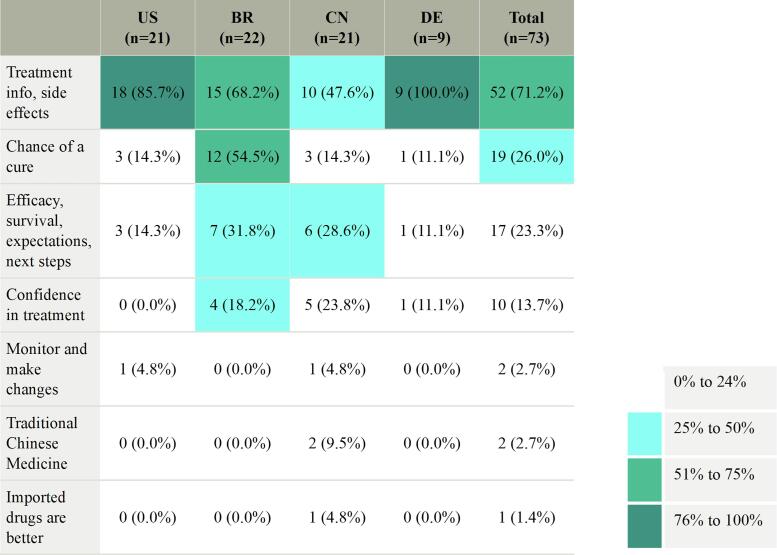
As patients embarked on their LACC journey, they empowered themselves through knowledge about their diagnosis. Physicians were a valued source of information, providing details regarding prognosis, treatment, potential side effects, and expectations during treatment. Fig. 1 provides details regarding treatment information shared by physicians. Several patients reported their physician discussed the chance of being cured after surgery or treatment, particularly in Brazil. Some were informed of having a 90% or higher chance of a cure, which made patients feel encouraged.
Fig. 1.
Information Shared by Physicians by Country.
However, some physicians were cautious when discussing prognosis with their patients and did not want to guarantee a cure. Two patients explained:
They told me that if it all went well, I could anticipate very good chances of a cure. If they removed everything and there weren’t any problems, …I wouldn’t have to deal with other treatment options such as radiation or chemotherapy. (DE24)
[The physician] said there is no recipe when it comes to cancer. …However, in stage II, [the] chances of getting cured are high. (BR04)
While most physicians provided valuable information to their patients, a significant number of patients (30/81) stated their physician did not discuss or “did not know” the cause of their CC. This lack of information left some patients uninformed or misinformed about their cancer. Notably, 18 out of 81 patients attributed their CC to causes other than HPV. These perceived causes included genetics, inflammation, promiscuous sex, or having an abortion. One patient explained:
[The physician] told me several possible causes, including promiscuous sex and premature sex. He said he did not know the specific cause. I asked why I had got the disease. I had only had three boyfriends altogether. That was not a high number. (CN10)
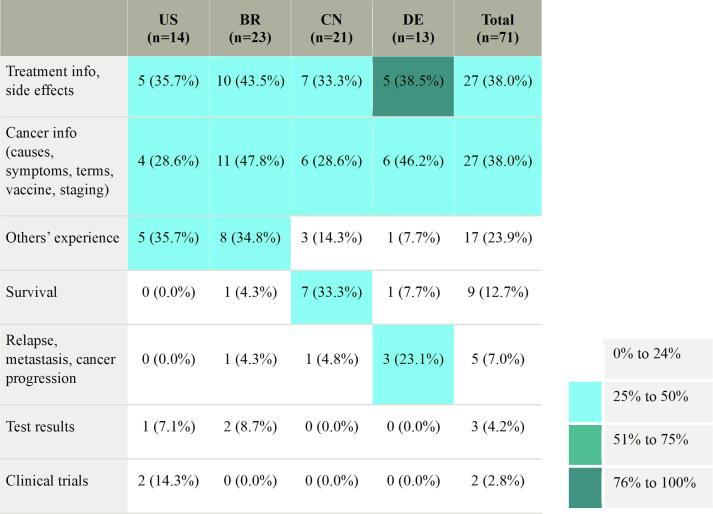
3.1.2. Information sought by LACC patients
Most patients in Brazil (23/25), China (21/25), and Germany (13/15) pursued research to gain a better understanding of LACC; however, only half of US patients (14/26) conducted their own research. Fig. 2 presents the information patients researched. Most research focused on treatment options, side effects, the causes and symptoms of LACC, and patient experiences with LACC. Among all countries, Chinese patients were more curious about survival (7/9), whereas German patients were more inclined to seek information about relapse, metastasis, and cancer progression (3/5). One German patient explained:
I looked at what could happen if the surgery was not enough… I did research that it could spread into the abdomen or uterus. I have also informed myself about the possibility of chemotherapy or radiation therapy. Then, it also goes on to uterus removal, ovary removal, or often surrounding organs. (DE04)
Fig. 2.
Information Researched by Patients by Country.
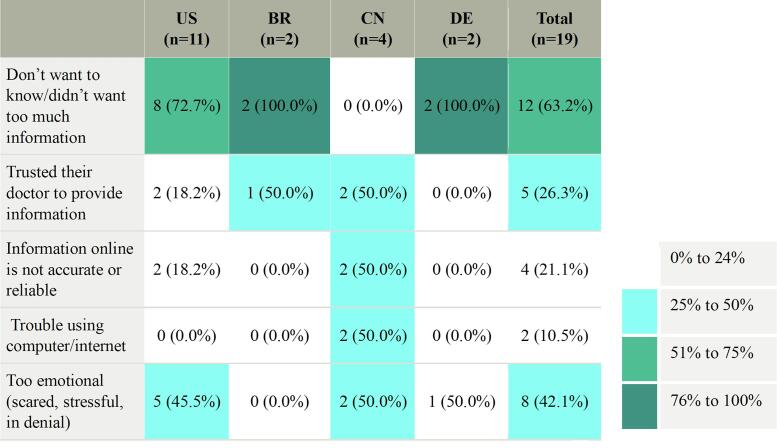
Most patients independently pursued research regarding their diagnosis and treatment options (71/91); however, nearly half US patients refrained from doing so (12/26). Among those who did not conduct an information search, the most common reason reported was feeling too scared, overwhelmed, or in denial about the situation (Fig. 3).
I get really scared and overwhelmed. …I did ask questions to the doctor…, but I didn't look at anything online. I don't want to look at all the scary stuff; I just want to know what I have to know. (US15)
Fig. 3.
Reasons Why Research was Not Performed by Country.
3.2. Theme 2: Patient confidence in their physicians and treatment plan
3.2.1. Seeking a second opinion
Patients generally expressed confidence in their physicians. Over half of patients stated they did not seek a second opinion (55/90), with 42 patients citing trust and confidence in their physician as the primary reason. One patient expressed:
I trusted [the physician] and the medical team. I felt embraced during the whole treatment. As I said, it is a good hospital that offers good assistance to the patient. (BR28)
However, one-third of patients (29/90) sought a second opinion to validate their initial diagnosis (16/29 patients who sought a second opinion) or because of disliking or mistrusting their first physician (8/29). Negative experiences, such as being ignored or dismissed, led some patients to seek care elsewhere. Three patients explained:
He was very rude. After he examined me, he was very prejudiced. (BR26)
I had previously noticed that I was having lower abdominal pain and bleeding, so I went to my doctor. He said it wasn’t a big deal. I solicited a second opinion, and then they did a smear. There was an anomaly. (DE17)
They put in the IUD that was supposed to prevent cancer; that’s what they told me. …I felt that the obstetrician-gynecologist was so damn arrogant like, “Oh, you’re fine.” He basically said don’t be dumb or a hypochondriac; you’re never going to have cancer. (US03)
Chinese patients were most likely to seek a second opinion (13/29) to confirm their diagnosis (10/13 Chinese patients who sought a second opinion). This seemed to be both emotionally and rationally driven, as several shared they could not accept the diagnosis and thought there may be a mistake. One patient explained:
When [the physician] told me about the diagnostic result, I was unwilling to accept it and questioned whether they made a mistake. I went to see other doctors. …The final diagnostic result remained the same. So, I had to accept it. (CN08)
Brazilian and US patients were most likely to seek a second opinion because of mistrust in their physician (4/8 Brazilian patients and 4/6 US patients), while nearly all German patients did not seek one. Some patients were unable to receive a second opinion due to cost/insurance (3/55 patients who did not seek a second opinion), while others could not wait because of urgent symptoms or not wanting to wait to receive one (6/55).
3.2.2. Deciding on a treatment plan
In addition to expressing trust in their physicians, many patients conveyed confidence in their treatment plans. Table S2 illustrates the emotions experienced by patients after deciding on their treatment plan. Over half felt positive, confident, relieved, or hopeful after deciding on a treatment plan. Many expressed having a plan gave them a sense of control over their uncertain future. Patients explained:
I was excited to get started [and] that I had taken control to decide that was what I wanted to do. (US20)
[I felt] calm and peace because I knew I had already decided, having the greatest amount of information in hand, making the best decision for me. (BR01)
However, one-fifth of patients said they felt terrified, depressed, worried, or anxious after deciding on a treatment plan, often citing they were afraid of chemotherapy or treatment side effects. Some felt indifferent about deciding on a treatment plan, seeing it as a necessary step toward recovery without any other options. Others had mixed feelings, feeling both relieved to have a plan and apprehensive about what it might entail. One patient explained:
[I had] fear…[regarding] whether [the treatment] would even have an effect, or maybe I was just receiving it because other people make a lot of money off of it and I’d still die in the end. …It was fear of the unknown. (DE17)
3.3. Theme 3: Patient engagement in the treatment decision
3.3.1. Engagement through understanding their CC
Shared decision-making centered on informing patients, inviting them to discuss treatment options, and preparing them to participate in the decision-making process. Patients largely felt they had knowledge to participate in their treatment decisions. Nearly one-third of patients expressed having all the information they needed to make an informed decision (27/47), with physicians being their primary source of information. Patients explained:
[The physician] helped me with this decision because she gave me a lot of information. (DE25)
I pretty much made an informed decision to an extent because they did tell me what all the side effects were going to be, what was going to happen to my body. (US21)
We found that nearly two-thirds of patients felt their physicians answered their questions in a thorough and clear manner, and their physicians were patient with them (35/54). Patients valued the time their physicians took to address their concerns, which helped them understand the information discussed during their appointment. One patient explained:
[The physician] took his time. Time is important for understanding what treatment options there are and for asking questions. It also allowed the doctor to be empathetic. It was important to be asked from time to time: “Did you understand everything? Do you still have questions?” I just had the feeling that there was simply time. (DE03)
Others refrained from asking questions when they received their diagnosis, as they felt too overwhelmed or scared during the appointment (10/54). Patients explained:
[I didn’t ask any questions], as I was alone. I was so scared that I did not ask much. (BR25)
Knowing I got cancer, I was pretty down. I dare not ask him. But even if I did, he won’t tell me, so I didn’t ask him questions at that time. (CN18)
I didn’t [have all my questions answered], but I believed the problem was myself. At that moment, I had no idea what questions I should ask my doctor. (CN06)
I didn’t have the chance [to ask questions]. I was too stunned. (US26)
Additionally, some patients reported that their physicians answered only some of their questions or their responses were vague or unclear (7/54).
3.3.2. Engagement in the treatment decision
Most patients felt they were actively involved in the decision-making process (74/90), with Chinese patients reporting a higher level of participation compared to other countries (23/25). However, it should be noted that we recruited a subgroup of 10 Chinese patients who participated actively in their treatment decisions; this decision was based on the understanding that Chinese patients are less inclined to participate in the decision-making process (Xie et al., 2020). Among those who felt involved, over half described their role as accepting the recommended treatment, although the final decision rested with them (39/74 patients who participated in their treatment decision). Patients explained:
As I wanted all of this to end, I did not discuss it. I just accepted…it. …I did not question it. I was a layperson regarding this subject. I trusted their word. (BR28)
I thought that my treatment plan was determined by the physician. After he chose a treatment plan, he explained to me basic knowledge about the disease and the treatment….I could accept the treatment plan recommended by the physician. (CN23)
I accepted [the treatment plan]. I don't know what else I should have done. I can't treat myself. If he says it has to be like this, then I say: “OK, I have to do it.” (DE19)
It felt there wasn’t another option, so I don’t feel like I sat there and made a decision. I think I just accepted what I had to do. (US23)
In contrast, nearly half of patients described a collaborative role, where they made decisions with their physicians (32/74). Notably, Brazilian patients were more likely to emphasize this collaborative dynamic (10/18). One patient explained:
He made me feel confident about what he was going to do and thinking to do. However, he has always said to me it was my decision. In this case, I think it is hard to make a decision against the doctor, mainly when you imagine he is doing the right thing. However, if I said, “No, I do not want to do surgery or chemotherapy,” it was not going to happen. He sent me what was best, and I believed him and did it. (BR04)
However, approximately 20–25% of Brazilian (5/23), German (3/16), and US (6/26) patients and 8% of Chinese patients (2/25) expressed a lack of involvement or having no choice in their treatment decisions. One patient explained:
It was “that's what you're going to do, you're going to do chemo, radio, and brachy.” (BR11)
Overall, over two-thirds of patients said they were satisfied with their role in the decision-making process (18/26). Many expressed that even if they didn’t have a key role, they trusted their physician to make the decision and were content with accepting what the physician suggested. Two patients explained:
I think it isn’t my subject, and I simply trust him. He knows his way around this better, and he knows what he’s doing. (DE23)
I did feel comfortable because she explained it all very well why surgery was not an option and why the other treatment option is better. (US23)
The remaining one-third desired to have a bigger role (8/26). Two patients explained:
I wish my doctor could give a clear introduction on various plans and let me make the decision myself. (CN08)
I would have liked to [receive] information and [feel] like I had time to make a decision. I felt very rushed in all of the…decisions. They were very, “This is what to do. We need to do it now.” (US20)
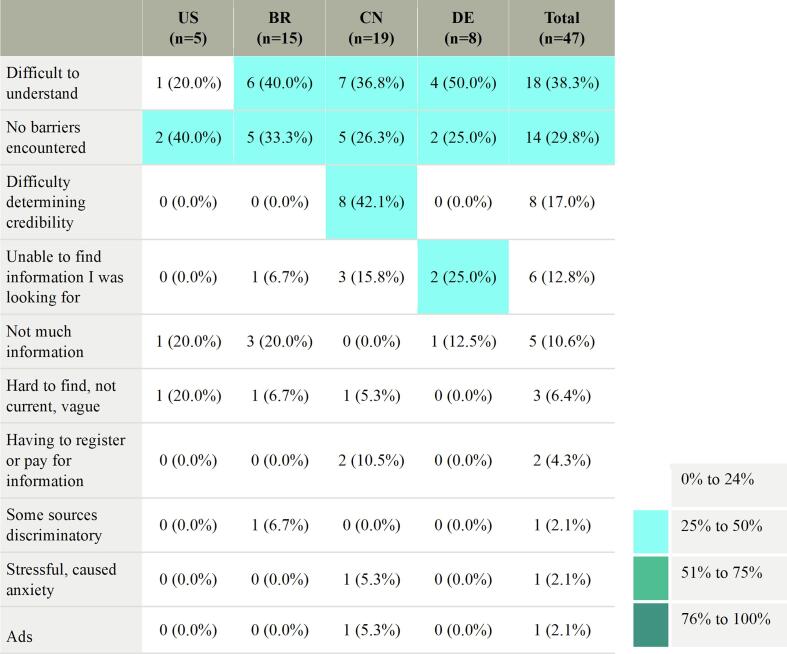
3.4. Theme 4: Challenges in information search
While most patients conducted research to understand their diagnosis and treatment options, approximately 70% encountered barriers to their information search (Fig. 4). Common challenges included understanding medical terms, finding relevant information, and evaluating source credibility. Some patients desired more general information, with one individual suggesting giving the “basics” through bullet points.
Fig. 4.
Barriers to Information Search by Country.
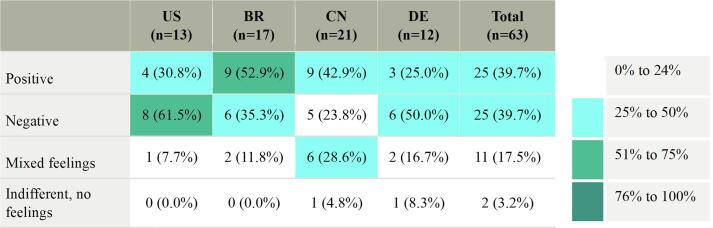
The impact of information searches on patients' emotions varied, evenly divided between positive and negative experiences (Fig. 5). US and German patients experienced more negative experiences. Some patients encountered troubling and conflicting information, which contributed to their negative experiences. Others chose to avoid information searches to achieve a sense of peace.
I googled “cervical cancer with a positive lymph node.” It basically said it’s stage III, and I only had a 36% chance of beating it. I was convinced I was going to die. I was really confused why my doctor [said] a couple of days later, “Oh yeah, you’ve got an 80% chance.” Why is he saying 80% chance, but the internet is telling me I’m likely going to die from this? (US11)
It was no use searching for relevant information since I had no idea whether the information I found was authoritative or reliable. So, I stopped searching. (CN10)
I can’t say [the information search] was useful. It was more unsettling… It’s so hard to understand with all these terms. Here, it says one thing, and somewhere else it says something different. You don’t know what the truth is. (DE17)
Fig. 5.
Feelings About Information Search by Country.
Of those who had positive experiences, their information search proved empowering, fostering feelings of confidence, control, and assurance that the information provided by their physicians was trustworthy.
The load of information that I have makes me feel more at ease each day. Each day I am more relaxed. I know I have a problem, but I'm treating it, and I will get better. I'm on the right track. (BR29)
Some patients had trouble discussing their diagnosis with family and friends due to the stigma surrounding their diagnosis (13/68). This was particularly true for Brazilian patients (7/13) and the US (5/13 US). In contrast, German and Chinese patients rarely mentioned or did not express this concern.
4. Discussion
Our study highlights the role of information in empowering LACC patients during their treatment journey. Having sufficient knowledge about treatment options is essential for patients to make informed decisions, including understanding the benefits, limitations, and uncertainties associated with each option (Kane et al., 2014). We found that LACC patients most commonly sought information to understand their prognosis, prepare for treatment, and anticipate potential side effects. Those who conducted information searches, regardless of their participation in shared decision-making, experienced empowerment and reduced uncertainty. Previous studies show that educating patients about their condition empowers them to anticipate and strategize for the future, enabling them to make informed decisions regarding their treatment (Eisfeld, 2020; Loiselle, 2019). By understanding patients’ information needs, physicians can promote positive interactions with the healthcare system, improve treatment satisfaction, and provide optimism for the future.
For LACC patients to feel confident in their treatment plans, it is crucial to provide patients with credible and easily understandable information. Many cancer patients often seek additional information to supplement, clarify, or verify the information provided by healthcare professionals (Germeni and Schulz, 2014). However, we found barriers exist, such as understanding medical terms, finding relevant information, and evaluating source credibility. These obstacles align with observations made in prior studies on breast cancer and other gynecological malignancies. McRoy et al. noted that materials currently provided to breast cancer survivors only address a fraction of their questions, ranging from one-third at best to one in eight at worst (McRoy et al., 2018). Information is often filled with medical jargon, impeding patient comprehension (Lu et al., 2020). Furthermore, a recent study reported that 25% of gynecologic content on TikTok contained significant misinformation (Morton, 2023). Physicians can alleviate these barriers by directing patients to user-friendly and reliable information resources.
Our study found that physicians may omit information about the potential causes of CC, leaving patients misinformed or uninformed. Several patients in our study misunderstood their CC to have causes other than HPV, attributing it to genetics, inflammation, promiscuous sex, or having an abortion. By ensuring that patients have an accurate understanding of their disease, physicians can alleviate confusion; prevent feelings of guilt, regret, and self-stigma; and promote confidence and empowerment.
In comparing the information needs of LACC patients to the advanced CC patients in our previous study (Szamreta et al., 2022), several key findings emerged. Both groups sought information about treatment, patient experiences, survival, and CC knowledge. Additionally, patients in both groups relied on their physicians as a reliable source of information, and their confidence in physicians was closely tied to their confidence in treatment plans. Studies have shown that effective physician communication regarding a patient's cancer and treatment options can foster higher levels of trust (Epstein and Jr, 2007; Hillen et al., 2011), leading to improved information exchange, informed decision-making, reduced anxiety, improved treatment compliance, and higher patient satisfaction (Kane et al., 2014; Hillen et al., 2011). Physicians also possess the ability to create a supportive setting where patients feel comfortable asking questions, empowering patients to feel confident and make informed healthcare decisions (Szamreta et al., 2022; Wiltink et al., 2020). Interestingly, despite trusting their physicians, LACC patients were more likely than those with advanced CC to question their diagnosis and seek a second opinion. Studies have noted the impact on health-related quality of life (HRQL) and psychological distress during LACC treatment with curative intent, but not for palliative treatment for metastatic CC (Wiltink et al., 2020). However, further research is needed to understand whether anticipated treatment burden in LACC is connected to questioning diagnosis.
LACC and advanced CC patients shared similar challenges when seeking information. However, LACC patients reported physicians discussing prognosis, treatment confidence, and the potential for a cure, whereas advanced CC patients encountered physician hesitancy when discussing prognosis. As a result, advanced CC patients independently sought this information.
4.1. Strengths
This study's strength lies in its qualitative approach, capturing the patient narrative and emotions often missed in quantitative research. By interviewing patients within two years of their cancer diagnosis, patients could recall emotions and experiences more accurately.
Our study stands out for its diverse sample, being the first global study to interview LACC patients from multiple countries with different healthcare systems. Additionally, we obtained a diverse sample for each country by considering factors like residence, insurance plan, community type, race, and education level.
4.2. Limitations
Due to our sample size, some subgroups may be underrepresented. Over half of Chinese patients had not completed treatment at the time of the interviews, which could affect our findings. The applicability of our findings to transgender men or immigrants who are not fluent in the local language remains unknown. It should be noted that self-selection bias may be present in the education level of the participants, as a certain level of disease understanding was required for the study.
5. Conclusion
LACC patient experiences with treatment and overall cancer care can vary, encompassing both positive and negative aspects. After diagnosis, patients may feel fear, anxiety, and helplessness. However, information can alleviate these emotions, empowering patients with a sense of confidence, control, and comfort throughout their CC journey. Various challenges impede information accessibility, including difficulties understanding medical terminology, not finding information specific to a patient’s cancer type, and evaluating source credibility. Physicians are pivotal in addressing these challenges by providing patients with credible and understandable information, while also creating a supportive environment that addresses their questions and concerns. This physician-patient interaction not only fosters emotional support but also enhances shared decision-making, ultimately instilling hope and confidence in patients' treatment plans.
Funding source
The study was funded by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA (MSD).
Ethical conduct of research
The authors state that this study received exemption status from full or expedited ethical review by Pearl IRB, that they have followed the principles outlined in the Declaration of Helsinki for all human or experimental investigations, and informed consent was obtained electronically from the patients involved.
CRediT authorship contribution statement
Elizabeth A. Szamreta: Conceptualization, Methodology, Supervision, Writing – review & editing. Emily Mulvihill: Conceptualization, Formal analysis, Investigation, Methodology, Writing – review & editing, Writing – original draft. Katherine Aguinaga: Conceptualization, Methodology, Writing – review & editing. Kaitlan Amos: Conceptualization, Data curation, Formal analysis, Software, Writing – review & editing. Heather Zannit: Conceptualization, Methodology, Writing – review & editing. Ritu Salani: Conceptualization, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: R. Salani received funding from MSD to provide research consulting services on this study. E. Mulvihill, K. Aguinaga, K. Amos, and H. Zannit are employees of Oracle Life Sciences who received funding from MSD to conduct this study. E.A. Szamreta is an employee of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA and stockholder of Merck & Co., Inc., Rahway, NJ, USA. Oracle Life Sciences also received funding from MSD for writing assistance in the creation of this article.
Acknowledgments
The authors acknowledge Stephanie Ritz, PhD of Oncology Intellect, LLC for her assistance with medical writing, and Kathleen Beusterien, MPH for her contributions to the qualitative research and study design.
Footnotes
Prior presentationResults from the study were presented as a poster at the ISPOR Europe 2023 Conference, as a poster at the 2023 Society of Gynecologic Oncology Annual Meeting and as an online abstract for the 2023 American Society of Clinical Oncology Annual Meeting.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.gore.2023.101321.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Adler, N.E., Page, A.E. Eds., 2008. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington (DC). doi: 10.17226/11993. [PubMed]
- Eisfeld H., et al. Importance of and Satisfaction with Information about Their Disease in Cancer Patients. J. Cancer Educ. Apr. 2020;35(2):403–411. doi: 10.1007/s13187-019-1480-7. [DOI] [PubMed] [Google Scholar]
- Epstein, R.M., R. L. S. Jr, 2007. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering, Natl. Cancer Inst. NIH Publ., vol. No. 07-6225.
- Gast, K.C. et al. 2019. Accuracy of self-reported cancer treatment data in young breast cancer survivors., J. Patient-Rep. Outcomes, vol. 3, no. 1, p. 24, doi: 10.1186/s41687-019-0114-5. [DOI] [PMC free article] [PubMed]
- Germeni E., Schulz P.J. Information seeking and avoidance throughout the cancer patient journey: two sides of the same coin? A synthesis of qualitative studies. Psychooncology. Dec. 2014;23(12):1373–1381. doi: 10.1002/pon.3575. [DOI] [PubMed] [Google Scholar]
- Grigsby P.W., et al. FIGO 2018 staging criteria for cervical cancer: Impact on stage migration and survival. Gynecol. Oncol. Jun. 2020;157(3):639–643. doi: 10.1016/j.ygyno.2020.03.027. [DOI] [PubMed] [Google Scholar]
- Gwede C.K., et al. Treatment decision-making strategies and influences in patients with localized prostate carcinoma. Cancer. Oct. 2005;104(7):1381–1390. doi: 10.1002/cncr.21330. [DOI] [PubMed] [Google Scholar]
- Hahlweg P., et al. Cancer patients’ preferred and perceived level of involvement in treatment decision-making: an epidemiological study. Acta Oncol. Stockh. Swed. Aug. 2020;59(8):967–974. doi: 10.1080/0284186X.2020.1762926. [DOI] [PubMed] [Google Scholar]
- Hanprasertpong J., Geater A., Jiamset I., Padungkul L., Hirunkajonpan P., Songhong N. Fear of cancer recurrence and its predictors among cervical cancer survivors. jgo. 2017;28(6) doi: 10.3802/jgo.2017.28.e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillen M.A., de Haes H.C.J.M., Smets E.M.A. Cancer patients’ trust in their physician-a review. Psychooncology. Mar. 2011;20(3):227–241. doi: 10.1002/pon.1745. [DOI] [PubMed] [Google Scholar]
- Hopenhayn C., et al. Prevalence of human papillomavirus types in invasive cervical cancers from 7 US cancer registries before vaccine introduction. J. Low. Genit. Tract Dis. Apr. 2014;18(2):182–189. doi: 10.1097/LGT.0b013e3182a577c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane H.L., Halpern M.T., Squiers L.B., Treiman K.A., McCormack L.A. Implementing and evaluating shared decision making in oncology practice. CA. Cancer J. Clin. Dec. 2014;64(6):377–388. doi: 10.3322/caac.21245. [DOI] [PubMed] [Google Scholar]
- Loiselle C.G. Cancer information-seeking preferences linked to distinct patient experiences and differential satisfaction with cancer care. Patient Educ. Couns. Jun. 2019;102(6):1187–1193. doi: 10.1016/j.pec.2019.01.009. [DOI] [PubMed] [Google Scholar]
- Lu L., Liu J., Yuan Y.C. Cultural differences in cancer information acquisition: cancer risk perceptions, fatalistic beliefs, and worry as predictors of cancer information seeking and avoidance in the U.S. and China. Health Commun. Sep. 2022;37(11):1442–1451. doi: 10.1080/10410236.2021.1901422. [DOI] [PubMed] [Google Scholar]
- Lu H., Xie J., Gerido L.H., Cheng Y., Chen Y., Sun L. Information Needs of Breast Cancer Patients: Theory-Generating Meta-Synthesis. J. Med. Internet Res. 2020;22(7):e17907. doi: 10.2196/17907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRoy S., Rastegar-Mojarad M., Wang Y., Ruddy K.J., Haddad T.C., Liu H. Assessing unmet information needs of breast cancer survivors: exploratory study of online health forums using text classification and retrieval. JMIR Cancer. 2018;4(1):e10. doi: 10.2196/cancer.9050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Atkins L., West R. The behaviour change wheel.“ A guide to designing interventions. G. B. Silverback Publ. 2014;1003:1010. [Google Scholar]
- Miller B.E., Pittman B., Strong C. Gynecologic cancer patients’ psychosocial needs and their views on the physician’s role in meeting those needs. Int. J. Gynecol. Cancer. Feb. 2003;13(2):111. doi: 10.1136/ijgc-00009577-200303000-00002. [DOI] [PubMed] [Google Scholar]
- Morton M., et al. Tampa; Florida: 2023. “‘More than just a song and dance’: an analysis of gynecologic content on TikTok”, presented at the Society of Gynecologic Oncology. [Google Scholar]
- Nagler R.H., et al. Differences in information seeking among breast, prostate, and colorectal cancer patients: results from a population-based survey. Patient Educ. Couns. Dec. 2010;81(Suppl):S54–S62. doi: 10.1016/j.pec.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C.E., et al. Stigma and cervical cancer prevention: A scoping review of the U.S. literature. Prev. Med. Dec. 2021;153 doi: 10.1016/j.ypmed.2021.106849. [DOI] [PubMed] [Google Scholar]
- Rutten L.J.F., Arora N.K., Bakos A.D., Aziz N., Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003) Patient Educ. Couns. Jun. 2005;57(3):250–261. doi: 10.1016/j.pec.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Samoil, D., Kim, J., Fox, C., Papadakos, J.K. 2021. The importance of health literacy on clinical cancer outcomes: a scoping review. vol. 5, 2021, [Online]. Available: https://ace.amegroups.com/article/view/6259.
- Simensen V.C., et al. Survivors’ knowledge of their diagnosis, treatment and possible late adverse effects after autologous stem cell transplantation for lymphoma. Acta Oncol. Stockh. Swed. Sep. 2019;58(9):1315–1322. doi: 10.1080/0284186X.2019.1637538. [DOI] [PubMed] [Google Scholar]
- Stewart D.E., et al. Information needs and decisional preferences among women with ovarian cancer. Gynecol. Oncol. Jun. 2000;77(3):357–361. doi: 10.1006/gyno.2000.5799. [DOI] [PubMed] [Google Scholar]
- Szamreta E.A., Wayser G.R., Prabhu V.S., Mulvihill E., Aguinaga K., Salani R. Information needs during cancer care: qualitative research with advanced cervical cancer patients in Brazil, China, Germany, and the United States. Gynecol. Oncol. Rep. 2022:101131. doi: 10.1016/j.gore.2022.101131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T., Molassiotis A., Chung B.P.M., Zheng S.-L., Huang H.-Q., (Benjamin) Tan J.-Y. A qualitative exploration of the unmet information needs of Chinese advanced cancer patients and their informal caregivers. BMC Palliat. Care. 2021;20(1):83. doi: 10.1186/s12904-021-00774-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiltink, L.M. et al., 2020. A systematic review of the impact of contemporary treatment modalities for cervical cancer on women’s self-reported health-related quality of life., Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer, vol. 28, no. 10, pp. 4627–4644, doi: 10.1007/s00520-020-05554-2. [DOI] [PubMed]
- Xie J., Xie S., Cheng Y., He Z. Beliefs and information seeking in patients with cancer in Southwest China: Survey Study. JMIR Cancer. 2020;6(2):e16138. doi: 10.2196/16138. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.