Abstract
Objective
The Review of health services for children, young people and families within the NSW Health system identified that novel models of care were needed to improve access to clinical management for people with ADHD. The present study aimed to evaluate GPs’ knowledge of and attitudes towards ADHD and the challenges and opportunities for a more substantial role for GPs in ADHD management.
Method
An online survey of Australian GPs was conducted, with recruitment via email invitation.
Results
Out of 230 respondents, 213 surveys could be analysed. Of these, 97% believed ADHD was a genuine condition, with 90% identifying inattention as a primary symptom. Most (92%) had seen and diagnosed ADHD within the past year. Prevalent concerns included inadequate access to specialist assessment and treatment; 77% felt that GPs should have a more substantial role in ADHD management. Barriers included lack of time, knowledge and experience.
Conclusions
There was willingness amongst respondents take on a greater role in managing individuals with ADHD. However, a need for further training and education was highlighted. The Australian Evidence-Based Clinical Practice Guideline for ADHD may resolve an identified need for clinical guidance.
Keywords: general practitioners, attention-deficit hyperactivity disorder, ADHD in adults, Primary care, referral pathways
Attention-deficit hyperactivity disorder (ADHD) is characterised by inattention and/or hyperactivity/impulsivity and impaired functioning. It is estimated to affect 5%–8% of children1,2 and 1%–3% 3 of adults. Despite being designated a neurodevelopmental disorder, a lower prevalence of ADHD in adulthood may indicate that people generally cope better as they mature. However, the lifetime trajectories of ADHD suggest a more complex situation, with some adults being diagnosed who did not meet diagnostic criteria during childhood. 4 Furthermore, people who have been struggling to manage their lives with undiagnosed ADHD may present with secondary problems such as anxiety, depression or substance use disorder, which may mask the underlying ADHD.
For ADHD to be adequately recognised, diagnosed and managed, sufficient numbers of skilled practitioners are required. The prescription of stimulant medication for ADHD in Australia is overseen by both state and federal governments. With few exceptions, the legislation dictates that treatment should be initiated by paediatricians or psychiatrists. Ongoing treatment may involve a shared-care arrangement with the GP. In 2019 the Review of health services for children, young people and families within the NSW Health system (The Henry Review) 5 identified lack of access to ADHD services as a major issue. The Henry Review supports the development of novel models of care that include GP prescribing, for which they would require adequate skills. 6 A recent publication indicated widespread dissatisfaction among the ADHD support organisations about the shortage of trained specialists, the lack of provision for ADHD in the public sector and the high fees for private psychiatrists. 7 The issue of ADHD services in Australia is now being investigated with a Senate Inquiry.
Previous studies support the need for GP upskilling in order for them to take a more active role in the diagnosis and management of ADHD; however, barriers to this include time pressure and lack of formal training.8–10 Studies have also revealed wide variation in GPs’ understanding of ADHD and its treatment.11,12 For example, from survey responses, 55% of Queensland GPs considered ADHD over-diagnosed 12 and 79% of GPs in South London considered ADHD to be stigmatising to the individual. 13
However, despite lacking the time and knowledge for diagnosis and treatment, the Queensland GPs were comfortable with a supportive and monitoring role for their patients with ADHD. 12
This study aimed to survey Australian GPs regarding their understanding and attitudes towards ADHD and their perceptions about the capacity of their local services for accepting referrals for assessment of ADHD in children, adolescents and adults.
Methods
Based on findings from previous studies,9,11,12 a survey was developed to explore GPs’ knowledge of and attitudes towards ADHD, their current practices in managing patients and their perceptions of local referral pathways. A critical appraisal checklist 14 was utilised to develop the questionnaire items, which were then piloted with GPs and GP registrars. The electronic survey consisted of multiple-choice, rank-order scales, yes/no questions and free-text answer fields and was accessible via an email link to the survey platform (SurveyMonkeyTM).
The questionnaire was distributed across all Australian states between December 2020 and January 2022, via the local Primary Health Networks, with email contact to GP practices, social media GP groups and personal communication to GP colleagues. Demographic data were collected but no personal identifiers.
Analyses were mainly descriptive; free-text responses were collated and analysed thematically.
Ethics approval was granted for this study (Project Identifier 2019/ETHXXXX). All participants gave informed consent.
Results
A total of 230 responses were received from all Australian states and territories, apart from the Northern Territory, of which 214 were sufficiently complete to be included. There was a strong female predominance (72%). The sample characteristics are shown in Table 1.
Table 1.
Sample demographics
| No (%) | ||
|---|---|---|
| Gender | Female | 152 (71.4) |
| Male | 60 (28.2) | |
| Not specified | 1 | |
| State | New South Wales | 97 (45.5) |
| Victoria | 52 (24.4) | |
| Queensland | 27 (12.7) | |
| Western Australia | 14 (6.6) | |
| South Australia | 10 (4.7) | |
| Australian Capital Territory | 6 (2.8) | |
| Tasmania | 2 (0.9) | |
| Not specified | 5 (2.3) | |
| GP setting | Group practice | 188 (88.3) |
| Solo practice | 23 (10.8) | |
| Not specified | 2 | |
| Qualification | RACGP fellow | 174 (81.7) |
| ACRRM fellow | 3 (1.4) | |
| Non-VR GP | 4 (1.9) | |
| VR GP | 3 (1.4) | |
| GP registrar | 22 (10.3) | |
| Other | 7 (3.3) | |
| Experience in GP | 0–5 years | 56 (26.3) |
| 5–10 years | 54 (25.4) | |
| 10–20 years | 52 (24.4) | |
| 20+ years | 51 (23.9) | |
| Full or part time | Full time | 111 (52.1) |
| Part time | 98 (46) | |
| Not currently working | 4 (1.9) |
RACGP: The Royal Australian College of General Practitioners; ACRRM: The Australian College of Rural and Remote Medicine; VR GP: Vocationally recognised GP; Non-VR GP: Non-Vocationally recognised GP.
Many (42%) reported no previous training on ADHD; some had covered ADHD during their undergraduate (19%) or postgraduate (6%) training; 21% had attended a course or conference. Almost all respondents (97%) believed that ADHD was a genuine condition and most (94%) recognised that it could also affect adults. Only 23% considered ADHD over-diagnosed but 66% thought that the diagnosis of ADHD could be stigmatising.
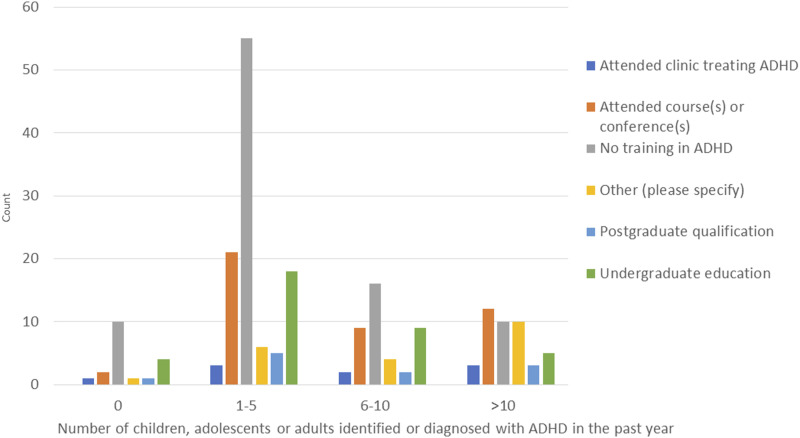
Over the previous year, 91% had identified or suspected ADHD among their patients (Figure 2). In free-text responses, 88% specified inattention, 66% hyperactivity and 24% impulsivity as primary symptoms of ADHD; 5% also specified emotional dysregulation. The most frequently volunteered common comorbidities were anxiety and depression (61% and 45%, respectively), autism spectrum disorder (ASD) (43%), substance misuse (18%) and oppositional defiant disorder (14%).
Figure 2.
Number of children, adolescents and adults identified or diagnosed with ADHD in relation to the General Practitioners' training in ADHD.
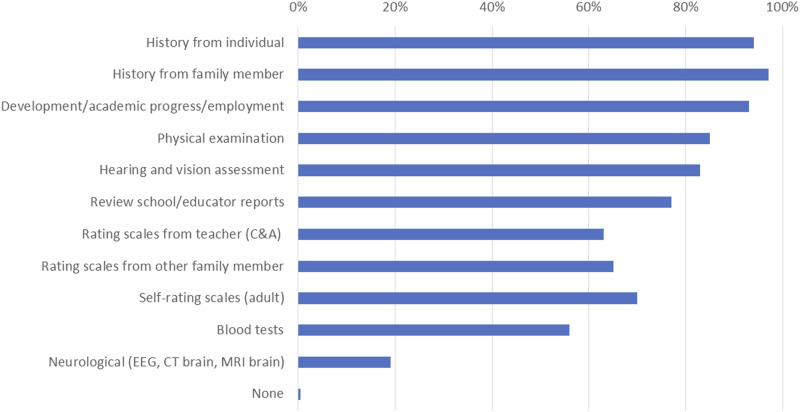
Almost all respondents (97%) considered it appropriate for a GP to take a medical history and perform a physical examination (Figure 1). Most also felt that GPs could arrange hearing and vision assessments (83%), review academic progress (77%), arrange rating scales (63%); 89% would find a diagnostic/screening tool helpful.
Figure 1.
Assessments and investigations felt appropriate for General Practitioners to perform and/or arrange for children, adolescents and adults with suspected ADHD.
Not all would refer every person with suspected ADHD to a specialist, however, 74% would refer at least 75% of children and adolescents, but only 51% would refer more than 75% of adults. Children and adolescents were predominantly referred to private paediatricians and adults to private psychiatrists. Some respondents (23%) reported no option of public sector referral for adults; for children and adolescents this was 6%. Lack of clear management guidelines and referral pathways were noted by 68% and 60%, respectively.
Most GPs expected specialists to diagnose ADHD (92%), start medication (79%) and provide an explanation (67%). Most GPs (93%) felt confident in referring patients for psychology, counselling or behavioural therapy.
When invited, 101 respondents (47%) provided free-text comments regarding their local referral pathways for ADHD (Table 2). These overwhelmingly reported difficulties, including lack of availability of specialist services (81), lengthy waiting periods (38), difficulty accessing mental health services (30) and lack of referral options for adults (20). Fourteen found referrals time- and effort-intensive and 29 noted that public services were either unavailable or difficult to access.
Table 2.
Sample of free-text comments provided by respondents regarding referral pathways for individuals with suspected or diagnosed ADHD
| ‘It is nearly impossible to get a timely appointment for a patient with possible ADHD’. |
| ‘Very hard and tedious process’. |
| ‘Difficult, almost impossible. … Time consuming for all’. |
| ‘All their books are closed or their waiting list is impossibly long. Absolutely frustrating’ |
| ‘There is frequently a rejection of any referral of adults…’ |
| ‘Currently very difficult to find any psychiatrists taken new patients for diagnosis of ADHD in adolescents or adults’. |
| ‘So few public options available’. |
Most of respondents felt that medication was appropriate 1st-line (53%) or 2nd-line (35%) therapy for ADHD; only 5% thought that medications should be reserved for severe ADHD, although 32% were concerned about medication abuse.
Most respondents (77%) were amenable to a greater role in the management of ADHD. Most (52%) were comfortable monitoring medication adherence and evaluating side effects. Two-thirds (63%) were willing to liaise with educational providers or employers. Half were confident in making adjustments to medications to improve efficacy (50%) or reduce side effects (51%).
Barriers to independent GP treatment were lack of time for assessment (68%) lack of diagnostic or screening tools (64%) and a lack of knowledge and experience (70%). Interestingly, 30% did not consider that specialist involvement was always necessary.
When the GPs’ views on medication for ADHD and the number of individuals they had identified with ADHD were analysed in relation to their years of experience, there were no consistent patterns. Similarly, for most of the group there was no significant relationship between training received and the identification of ADHD (Figure 2). However, there was a small group of 10 GPs among those who had identified >10 people with ADHD in the past year, who had either organised their own self-directed learning (8), had come across a lot of patients with ADHD (2) or had lived experienced of ADHD in their own family (3).
Discussion
Despite inconsistencies in training more than 90% of respondents recognised possible ADHD among their patients. Most could volunteer the two predominant symptom categories and name at least one common comorbidity. Almost all were happy to evaluate the presenting history and most were amenable to monitoring and supporting their patients with ADHD. Most referred to private specialists. However, their free comments expressed frustration with the inadequacy of referral pathways, particularly in the public sector and for adults.
A narrative review published in 2016 found widespread scepticism among GPs about the validity of ADHD as a diagnosis. 11 By contrast 97% of our respondents considered ADHD to be a genuine condition.
Our study contrasts with the 2002 survey of Queensland GPs 7 perhaps suggesting a reduction in the perception of overdiagnosis of ADHD among Australian GPs (23% vs 55%).
Our finding of a willingness among GPs to become more involved in ADHD management contrasts with previous studies.9,11,12 There were a few GPs who had successfully addressed their lack of formal training in ADHD.
With further training and the aid of clearer guidelines and/or a diagnostic tool, our respondents felt well-placed to gather information, refer for counselling or behavioural therapy, manage disordered sleep, and monitor medication adherence and side effects.
Formal shared-care arrangements have been established in the United Kingdom, where GPs can monitor and prescribe medication for ADHD, after initiation and titration by a specialist. 15 Such models might be applicable in Australia. The majority of respondents expected specialists to commence medication for patients with ADHD. This would be particularly important for individuals with complex comorbidities or with other conditions that could mimic ADHD, such as developmental trauma, depression, untreated bipolar spectrum disorder, severe personality disorder, substance use disorder and emerging psychosis.
The finding of frustration with the referral pathways among GPs is reflected in contemporaneous feedback from the ADHD community, 7 indicating that this is an Australian problem that needs to be addressed.
A strength of this study includes the number of survey responses from almost all states and territories in Australia. A limitation of this study includes the likely selection bias towards respondents already interested in ADHD. Even though our results may not reflect the full range of GPs’ opinions, they do indicate that there are GPs who are interested in ADHD and are concerned about the lack of provision of care. GPs are well-placed to participate more substantially in the care of these patients, given the traditional GP model of longitudinal, holistic, family-based care. GP management could be particularly suited to those individuals with less complex ADHD, which might include less severely affected relatives of individuals already diagnosed.
The role of the GP in the identification, diagnosis and treatment of individuals with ADHD, including the prescription of stimulants, needs to be further investigated with pilot studies of new models of care. 5 Participating GPs would need to be supported with specific education, skill-based training and specialist support and informed by evidence-based guidelines. 6 Ongoing collaboration between GPs, paediatricians and psychiatrists is suggested, including the RACGP Specific Interest Group in ADHD, ASD and Neurodiversity and the Australian ADHD Professionals Association, with the aim to co-design and develop educational resources and models of care. GPs would need to have access to specialists for managing ADHD associated with complex comorbidities, or situations when the diagnosis is unclear, together with training to recognise when referral is needed.
Conclusion
GPs who responded to the survey were aware of the existence of ADHD among their patients and were willing to play a more significant role in their management. In the longer term, upskilling and accrediting GPs for the identification, diagnosis and treatment of ADHD could supplement the existing referral pathways and relieve some of the frustration with treatment access.
Acknowledgements
The authors acknowledge the contribution of Dr Gary Low, who provided statistical advice.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: AP discloses personal fees and non-financial support from Shire/Takeda, outside the submitted work; and book royalties from Disruptive Publishing (ADHD Made Simple). The other authors declare no conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement
Ethics approval
Ethics approval was granted from the Nepean Blue Mountains Local Health District Human Research Ethics Committee (Project Identifier 2019/ETH11502). All participants gave informed consent.
ORCID iD
Alison Poulton https://orcid.org/0000-0002-5867-2403
References
- 1.Deloitte Access Economics . The social and economic costs of ADHD in Australia. London, UK: Deloitte, 2022. [Google Scholar]
- 2.Lawrence D, Hafekost J, Johnson SE, et al. Key findings from the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2016; 50: 876–886. DOI: 10.1177/0004867415617836. [DOI] [PubMed] [Google Scholar]
- 3.Ebejer JL, Medland SE, van der Werf J, et al. Attention deficit hyperactivity disorder in Australian adults: prevalence, persistence, conduct problems and disadvantage. PLoS One 2012; 7: e47404. DOI: 10.1371/journal.pone.0047404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caye A, Swanson J, Thapar A, et al. Life Span Studies of ADHD-Conceptual Challenges and Predictors of Persistence and Outcome. Curr Psychiatry Rep 2016; 18: 111. DOI: 10.1007/s11920-016-0750-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henry R. Young People and Families. Review of health services for children. Australia: NSW Health, 2019. [Google Scholar]
- 6.Australian ADHD Guideline Development Group . Australian evidence-based clinical practice guideline for attention deficit hyperactivity disorder (ADHD). Australia: ADHD, 2022. [Google Scholar]
- 7.Alison P. ADHD: community responds to new clinical guidelines, 2023, https://insightplus.mja.com.au/2023/22/adhd-community-responds-to-new-clinical-guidelines/ [Google Scholar]
- 8.French B, Perez Vallejos E, Sayal K, et al. Awareness of ADHD in primary care: stakeholder perspectives. BMC Fam Pract 2020; 21: 45. DOI: 10.1186/s12875-020-01112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adamis D, Tatlow-Golden M, Gavin B, et al. General practitioners' (GP) attitudes and knowledge about attention deficit hyperactivity disorder (ADHD) in Ireland. Ir J Med Sci 2019; 188: 231–239. DOI: 10.1007/s11845-018-1804-3. [DOI] [PubMed] [Google Scholar]
- 10.Rezel-Potts E, Kordowicz M, Downs J, et al. Attention-deficit/hyperactivity disorder: parent/carer perceptions of barriers to healthcare access. Arch Dis Child 2021; 106: 1125–1128. DOI: 10.1136/archdischild-2020-321362. [DOI] [PubMed] [Google Scholar]
- 11.Tatlow-Golden M, Prihodova L, Gavin B, et al. What do general practitioners know about ADHD? Attitudes and knowledge among first-contact gatekeepers: systematic narrative review. BMC Fam Pract 2016; 17: 129. DOI: 10.1186/s12875-016-0516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaw KA, Mitchell GK, Wagner IJ, et al. Attitudes and practices of general practitioners in the diagnosis and management of attention-deficit/hyperactivity disorder. J Paediatr Child Health 2002; 38: 481–486. DOI: 10.1046/j.1440-1754.2002.00033.x. [DOI] [PubMed] [Google Scholar]
- 13.Salt N, Parkes E, Scammell A. GPs’ perceptions of the management of ADHD in primary care: a study of Wandsworth GPs. Prim Health Care Res Dev 2005; 6: 162–171. DOI: 10.1191/1463423605pc239oa. [DOI] [Google Scholar]
- 14.Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. Bmj 2004; 328: 1312–1315. DOI: 10.1136/bmj.328.7451.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute for Health Care Excellence . Attention deficit hyperactivity disorder: diagnosis and management NG87. https://www.nice.org.uk/guidance/ng87/resources/attention-deficit-hyperactivity-disorder-diagnosis-and-management-pdf-1837699732933 [PubMed] [Google Scholar]