Abstract
Introduction:
Driving after cannabis use (DACU) and riding with a cannabis-impaired driver (RWCD) are national public health concerns. Though driving impairments and increased crash risk make DACU and RWCD two of the riskiest cannabis-related behaviors, many continue to drive after use and ride with others who are under the influence and do not view DACU or RWCD as dangerous. The current study examined the efficacy of an accessible, low-cost, mobile phone–based brief intervention aimed at reducing DACU and RWCD among college cannabis users in the context of a randomized three-group pilot trial.
Method:
Participants were 97 college cannabis users (67.4 % women; average age = 21.34; 80.4 % Caucasian) who endorsed DACU at least three times in the past three months. After completing baseline measures, the study randomly assigned participants to one of three conditions: a) a substance impaired–driving personalized feedback plus MI-style interactive text messaging intervention (PF + MIT); b) a substance impaired–driving personalized feedback only intervention (PF); and c) a substance information control condition (IC). All conditions completed outcome measures three months postintervention.
Results:
Generalized linear mixed models (GLMM) analyses indicated that after controlling for sex, cannabis users in the PF + MIT condition significantly reduced DACU and RWCD over time compared to those in the IC condition.
Conclusions:
These findings provide preliminary support for the short-term efficacy of a mobile phone–based intervention in decreasing DACU and RWCD among college cannabis users. Future research should determine whether these reductions in driving behaviors persist past three months.
Keywords: Cannabis, Driving, Text-messaging, Intervention, College
1. Introduction
Substance-impaired driving is a significant public health concern. Years of epidemiological and experimental research have demonstrated that cannabis use impairs driving ability (e.g., slower reaction time, delayed responses to road obstacles, impaired road tracking control) and cognitive functioning (e.g., memory, attention, decision making, impulse control) and increases risk for traffic accidents (Asbridge et al., 2012; Hartman & Huestis, 2013; Hostiuc et al., 2018; Kelly et al., 2004; Li et al., 2012). Although rates of driving after drinking have decreased over time (Hingson et al., 2017), rates of driving after cannabis use (DACU) continue to rise (Schulenberg et al., 2020). In 2018, 12 million US adults (4.7 %) reported driving after cannabis use (12.4 % for adults ages 21–25). Cannabis is the most prevalent illicit drug detected among drug-impaired drivers, and the most frequently used illicit drug among emerging adults (Brady & Li, 2013; Johnstonet al, n.d.). Rates of cannabis involved traffic fatalities have increased in states with recreational cannabis compared to their neighboring jurisdictions (Lane & Hall, 2019) and cannabis users who report DACU are significantly more likely to report being involved in a collision in the past year (Mann et al., 2007). In addition, data from recent roadside surveys suggest that positive tests for delta-tetrahydrocannabinol (THC) have increased in recent years and that drivers with a child in the car were much more likely to test positive for cannabis than for alcohol (14.1 % vs. 0.4 %; Berning et al., 2015; Romano et al., 2019). Given the increased prevalence of lifetime and daily cannabis use among emerging adults, DACU is becoming an increasingly urgent concern (Kerr et al., 2018; Melchior et al., 2019; Parnes et al., 2018).
Another risky impaired driving behavior that has received considerably less attention is riding with a cannabis-impaired driver (RWCD). Recent research demonstrates that many adolescents and young adults report riding with an impaired driver, with rates ranging from 20 % to 33 % in the past year depending on the sample (Carpino et al., 2020; Li et al., 2014, 2018). Attending a 4-year college and simultaneous use of alcohol and cannabis have been shown to increase the likelihood of riding with an impaired driver (Li et al., 2018; Patrick et al., 2021). Riding with an impaired driver has been linked to greater risk of problematic alcohol and cannabis use (Osilla et al., 2019) and driving under the influence of alcohol and cannabis (Li et al., 2018). Previous research has linked lower perceived risk of regular cannabis use to greater risk of DACU and RWCD (Carpino et al., 2020). Due to the high rates and potentially fatal consequences associated with RWCD, prevention and intervention efforts targeting RWCD are imperative.
Brief interventions (BIs) attempt to identify and correct faulty normative beliefs and highlight consequences of substance use (such as driving after substance use) to increase motivation to change a problematic behavior. BIs typically consist of one or two individual therapeutic meetings (approximately 50 min per session) delivered in motivational interviewing (MI) style and include personalized feedback (Carey et al., 2007; Miller & Rollnick, 2013). A series of questionnaires completed by the participant prior to their BI session make up the information provided in the personalized feedback document. Although specific feedback components may differ, studies typically include a personalized substance use profile, information on social norms, prior substance-related consequences experienced by the participant (including driving after substance use if endorsed), practical costs (e.g., money spent on substances), and information on strategies to limit substance-related risk (Miller et al., 2013). Recent meta-analyses indicate that brief alcohol interventions generally succeed in reducing alcohol use (frequency, quantity, level of intoxication) and a variety of alcohol-related problems, although effect sizes are typically small (Tanner-Smith & Lipsey, 2015).
Notably, personalized feedback interventions delivered to emerging adult cannabis users have demonstrated limited efficacy for decreasing cannabis use and problems (Halladay et al., 2019). A recent systematic review and meta-analysis by Halladay and colleagues (Halladay et al., 2019) on BIs for cannabis use in emerging adults examined evidence from 26 studies including 6318 participants (ages 16–29) and found that existing cannabis-related BIs resulted in small reductions in symptoms of cannabis use disorder and increased likelihood of cannabis abstinence but did not result in significant reductions in frequency of cannabis use and related problems. These findings parallel results from other meta-analyses conducted by Imtiaz et al. (2020) and Tanner-Smith et al. (2021) that showed BIs for cannabis use delivered in health care settings did not result in reductions in cannabis use. Though evidence for improving cannabis-related outcomes via BIs has been mixed, given the cost effectiveness of BIs and increased likelihood for engagement among emerging adults compared with longer-term psychosocial treatments, BIs remain important within a stepped-care approach to substance use and warrant further evaluation and development (Halladay et al., 2019).
Research suggests that personalized feedback delivered without a one-on-one, counselor-delivered intervention may effectively reduce alcohol use and problems at short-term follow-ups (up to 4 months), but direct comparisons of feedback only interventions vs. face-to-face interventions favor clinician contact and suggest that effects of interventions delivered without clinician contact tend to be smaller and dissipate at longer term follow-ups (Cadigan et al., 2015; Carey et al., 2012). In the only previously published study to examine the impact of a BI on DACU (as a secondary outcome), Walton et al. (2013) conducted a head-to-head test of a computer delivered vs. a therapist delivered cannabis BI and found a significant condition difference for driving under the influence (DUI) of cannabis, such that only participants who received the therapist delivered BI significantly reduced the frequency of cannabis related DUI (Walton et al., 2013).
Previous research has shown that in-person, counselor delivered BIs can successfully reduce alcohol impaired driving among DUI offenders, emergency department patients, and college students (Brown et al., 2010; D’Amico et al., 2018; Mun et al., 2021; Ouimet et al., 2013; Schermer et al., 2006; Teeters et al., 2015). In the past few years, a number of BIs using text-messaging to target substance use and problems have been developed and evaluated. Research by Heron et al. (2019) showed that among 1371 college students, 99.5 % owned smartphones, 94.6 % had unlimited texting, and 96.8 % reported texting at least once per day. Delivering BIs through text message allows for low-cost delivery to a large number of people and allows researchers to personalize information and interact with participants (Hall et al., 2015). A meta-analysis conducted by Mason et al. (2015) concluded that text-messaging interventions show a positive effect on reducing substance use behaviors (overall pooled effect size for 14 RCTs Cohen’s d =0.25; Mason et al., 2015). Research indicates that emerging adults rate text-messaging interventions as highly acceptable and prefer texting to emails and telephone calls (Common Sense, 2018; Mason et al., 2018).
Several recent studies have demonstrated greater effectiveness of interventions that include personal contact vs. those that are fully automated (Drislane et al., 2019; Riper et al., 2018). Teeters et al. (2018) conducted a pilot trial of a mobile phone–based intervention including personalized feedback and interactive text messages aimed at reducing alcohol-impaired driving among college students and found that students who received the mobile phone–based BI reported significantly greater reductions in likelihood of driving after drinking (OR = 0.016) and the number of drinks consumed prior to driving than students in the information condition at three-month follow-up (Teeters et al., 2018). To our knowledge, this was the first study to demonstrate that a mobile phone–based BI specifically targeting driving after drinking can reduce alcohol-impaired driving in this population. Additionally, Teeters et al. (2021) investigated whether the brief mobile-based intervention would lead to changes in DACU related cognitions and found that the personalized feedback and interactive text-messaging intervention were associated with larger increases over time in the perceived dangerousness of DACU compared to the control condition (p = .01; Cohen’s d = 0.79; Teeters et al., 2021). Although the results of Teeters et al. (2021) are promising, assuming that changes in explicit cognitions (dangerousness of DACU) will lead to behavior change is speculative (decreases in DACU over time).
To directly test this important question, the current study utilizes the same intervention model in an attempt to reduce DACU. The overall goal of the current study is to examine the efficacy of an accessible, low-cost, mobile phone–based BI aimed at reducing DACU among college cannabis users. Given the link between DACU and RWCD (Li et al., 2018), the study added a secondary outcome of RWCD post-hoc and examined it to determine if the intervention also resulted in reductions in this risky behavior. In the current study, the efficacy of an intervention with personalized feedback plus MI-style interactive text-messaging (PF + MIT) was compared to a) personalized feedback (PF) only and b) a substance informational control (IC) condition in the context of a randomized 3-group (PF + MIT vs. PF vs. IC) trial. The PF condition was included to parse out the unique contribution of the interactive text-messaging above and beyond the personalized feedback components.
2. Method
2.1. Participants
Participants were 97 undergraduate students from a public university in the mid-southern United States. The university resides in a small city with a population of approximately 67,600 individuals. To be eligible, students had to be at least 18 years or older, have access to a motor vehicle and a valid driver’s license, and report driving after cannabis use at least three times in the past three months. Additionally, participants had to have access to a smart phone, willingness to read intervention material and exchange a brief series of text messages via a secure mobile app with encryption technology postintervention with the study administrator. The study excluded individuals from the study if they were in treatment for substance use. Participants were 67.4 % women, 30.5 % men, and 80.4 % Caucasian, 7 % African American, 2 % Asian, 1 % Hispanic or Latino, 3 % other, and 8 % multiple selected. The average age of the participants was 21.34 years (SD = 4.24). A quarter of participants in the sample endorsed driving after combined use of alcohol and cannabis in the past 3 months, and 85.3 % of participants endorsed at least 1 heavy episodic drinking episode in the past month (4 or more drinks on one occasion for females and 5 or more drinks on one occasion for males). Rates of past month recreational drug use in the sample were as follows: cocaine (20.6 %), hallucinogens (30.9 %), heroin (1 %), methamphetamine (2.1 %), prescription pain killers (7.2 %), stimulants (19.6 %), and sedatives (13.4 %).
2.2. Measures
The study collected all measures at Time 1 (pre-intervention) and again at Time 2 (3 months postintervention).
2.2.1. Demographics
Participants completed a brief questionnaire that assessed participant sex, age, ethnicity, and past and present academic status.
2.2.2. Cannabis use
The study used a modified, brief computer-delivered Timeline Follow-Back (TLFB; Sobell et al., 1996) to assess cannabis use during the past 7 days prior to the baseline appointment. Additionally, participants were asked to report the number of days they used cannabis in the past month.
2.2.3. Driving after cannabis use
The study assessed driving after cannabis use via the following question, “In the past 3 months, how many times have you driven after using marijuana?” The study adapted this question from prior studies that asked students how many times they have driven after using cannabis in the past 3 months (Arterberry et al., 2017).
2.2.4. Riding with a driver under the influence of cannabis
Riding with a driver under the influence of cannabis was assessed via the question, “How many times in the past 3 months have you been the passenger in a vehicle with a driver who has been using marijuana?”
2.3. Procedures
The university Institutional Review Board approved all procedures and participants were assured that all data would be confidential. The study recruited participants through a mass university-wide email, the university subject pool, and flyers posted on campus. Following an eligibility screener survey, trained lab personnel contacted eligible participants by phone and invited them to participate in the clinical trial (clinicaltrials.gov NCT03496129). Eligible students who wished to participate were then sent a 30-minute baseline questionnaire via text-message to be completed remotely on their mobile phone via a secure web server. After completing the battery of online measurements, the study randomly assigned participants via a random number generator to one of three conditions (stratified by gender Fig. 1), 1) a substance impaired–driving personalized feedback plus MI-style interactive text messaging intervention (PF + MIT); 2) a substance impaired–driving personalized feedback only intervention (PF); and 3) a substance information control condition (IC). All conditions included a 3-month follow-up. The study gave participants a $20 Amazon gift card or 3 subject pool credits for completion of the baseline questionnaire and intervention, and a $15 Amazon gift card or 2 subject pool credits for the follow-up questionnaire. All data included in this manuscript come from the baseline assessment and 3-month follow-up for participants endorsing DACU (collected between August 2018 and December 2019). Data related to a 6-month follow-up were collected but due to the impact of the Covid-19 pandemic, the study team was unable to collect one fourth of 6-month follow-up data and we did not collect data from a planned 12-month follow-up.
Fig. 1.
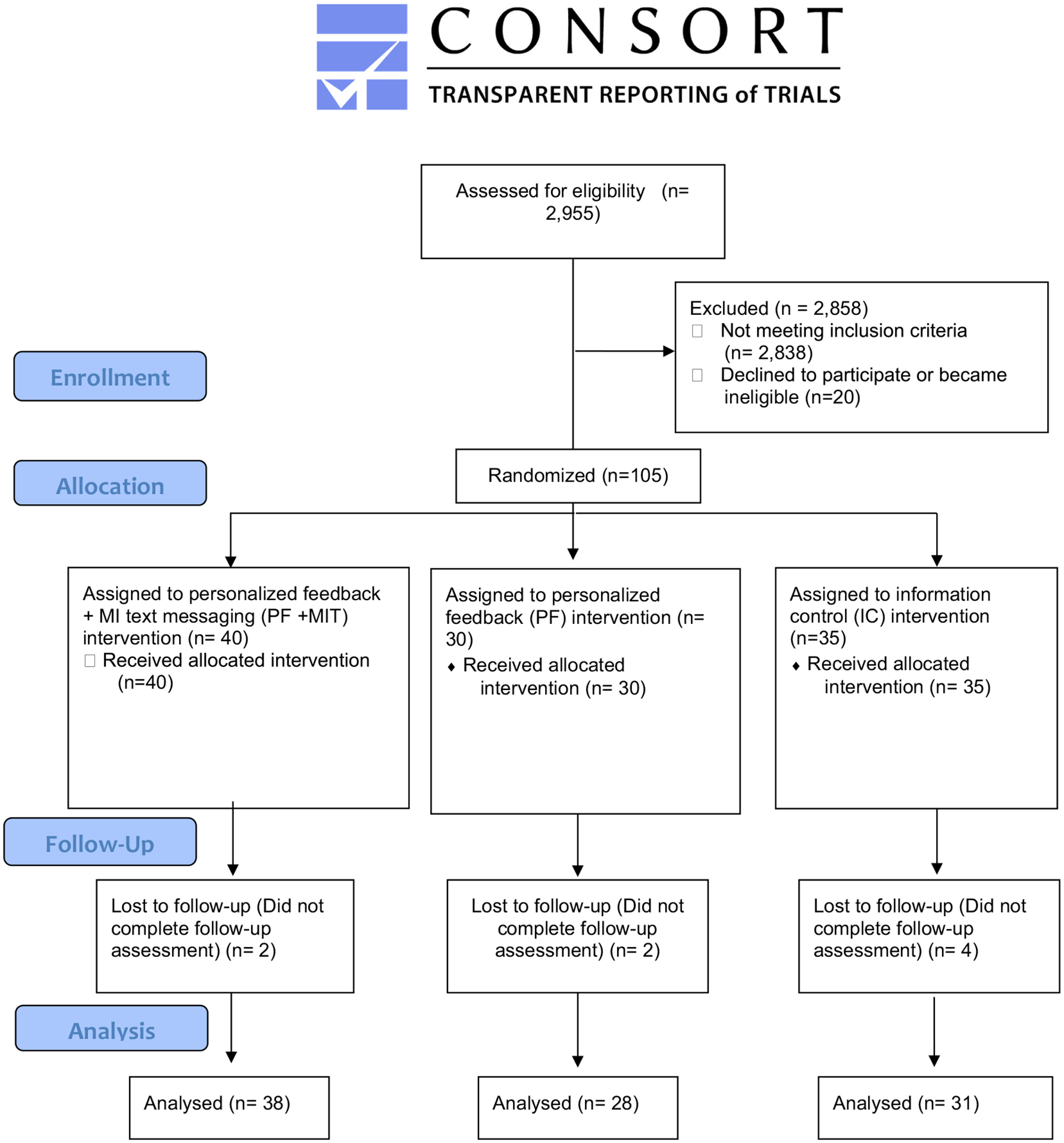
Flowchart illustrating recruitment, intervention and follow-up assessment for participants endorsing driving after cannabis use. All participation occurred remotely via text messages and email/web links.
2.3.1. Substance impaired–driving personalized feedback only intervention (PF)
Following the baseline assessment, the study sent participants in the PF condition a link via text message to a secure website containing personalized feedback. The feedback document included a personalized cannabis use profile and DACU profile and information on social norms related to cannabis use and DACU. The document also contained self-reported cannabis impairment and physical effects of cannabis use, costs associated with a DUI citation in Kentucky, and information on combined cannabis and alcohol impaired–driving risk (if endorsed). Participants were instructed to view the personalized feedback document and respond to a number of questions (determined based on participants’ responses to the questionnaires) embedded in the document as a comprehension and fidelity check. For example, the first question asks participants to choose the percentage of students who reported NO substance impaired–driving in the past 3-months (based on a figure provided in the personalized feedback).
2.3.2. Substance impaired–driving personalized feedback plus interactive text messaging intervention (PF + MIT)
Following the baseline assessment, the study sent participants in the PF + MIT condition a link via text message to a secure website containing personalized feedback (described above). In addition to viewing the feedback document and responding to the embedded attention checks, the study asked participants to reply via a text message to the study administrator to confirm receipt and processing of the feedback document. Next, a trained interventionist sent the participant text messages containing the following open-ended questions: 1) Of the information you just viewed, what was most interesting? 2) How would receiving a DUI impact your future career goals? 3) What is your plan for driving after substance use in the future? and 4) What specific goals would you be willing to set (if any) related to driving after substance use? Based on participants’ responses to these open-ended questions, the interventionist sent follow-up text messages to provide appropriate reflection/encouragement in motivational interviewing (MI) style. All interventionists were trained in MI, and a clinical psychologist with expertise in MI supervised the text messaging interactions. The intervention was a single session, and the average number of text messages exchanged between the interventionist and participants during the interactive texting portion of the intervention was 18 (range = 10–31). The average time to complete the intervention was 57 min.
2.3.3. Substance information condition (IC)
Participants randomized to the information condition received standard information about alcohol, cannabis, and substance impaired–driving via a link to a website delivered through text message. The informational document was roughly equivalent in length to the personalized feedback documents, contained the same number of attention checks, and provided detailed information about how alcohol, drugs, and combining alcohol and other drugs affect the brain and nervous system, memory, and driving performance. This intervention was designed to be similar to substance education programs commonly found on college campuses and contained no personalized information.
2.4. Data analysis plan
The study team conducted analyses using SPSS version 27.0 and R version 4.1.0. To minimize the impact of outliers, values >3.29 SDs above the mean on a given variable were Winsorized to one unit greater than the greatest nonoutlier value (Tabachnick & Fidell, 2013). Notably, all data reported were collected prior to the Covid-19 pandemic, which drastically impacted driving rates (Gupta et al., 2021).
The research team collected baseline descriptive characteristics of the overall sample, including demographic information (sex, age, ethnicity) as well as the means and standard deviations for the primary outcome variables (driving after cannabis use and riding with a cannabis impaired driver). Additionally, the team performed t-tests and chi square analyses to determine whether the conditions were significantly different at baseline on any demographic or cannabis-related variables (Table 1).
Table 1.
Descriptive statistics for outcome variables and covariates: baseline and 3-month follow-up.
| Total sample (N = 97) |
PF + MIT (n = 38) |
PF (n = 28) |
Information (n = 31) |
Statistical test χ2 Φ |
||
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | n = 29 (30.5 %) | n = 10 (34.5 %) | n = 10 (34.5 %) | n = 9 (31 %) | ||
| Female | n = 64 (67.4 %) | n = 25 (39.1 %) | n = 18 (28.1 %) | n = 21 (13.4 %) | ||
| Statistical test | 0.39 | 0.81 | ||||
| Ethnicity White | n = 78 (80.4 %) | n = 27 (34.6 %) | n = 25 (32.1 %) | n = 26 (33.3 %) | ||
| Non-White | n = 19 (19.6 %) | n = 11 (57.9 %) | n = 3 (15.8 %) | n = 5 (26.3 %) | ||
| Statistical test | 3.75 | 0.19 | ||||
| M (SD) | M (SD) | M (SD) | M (SD) | Statistical test | ||
| F | p | |||||
| Age | 21.34 (4.24) | 22.24 (5.37) | 21.21 (4.09) | 20.35 (4.26) | 1.71 | 0.19 |
| Driving after cannabis use Baseline | 25.16 (24.62) | 26.50 (26.55) | 22.43 (21.39) | 26.00 (25.46) | 0.243 | 0.79 |
| 3-Month | 19.92 (24.47) | 15.82 (19.81) | 22.36 (29.49) | 22.74 (24.78) | 0.877 | 0.42 |
| Riding with cannabis impaired driver Baseline | 14.49 (19.41) | 17.55 (22.51) | 14.18 (19.32) | 12.45 (20.21) | 0.399 | 0.80 |
| 3-Month | 9.52 (14.12) | 9.16 (16.44) | 8.07 (9.77) | 11.33 (14.62) | 0.383 | 0.82 |
| Driving after combined use of alcohol and cannabis Baseline | 0.98 (2.60) | 0.84 (2.59) | 0.89 (1.66) | 1.23 (3.31) | 0.20 | 0.81 |
| 3-Month | 0.51 (1.42) | 0.18 (0.69) | 0.57 (1.64) | 0.84 (1.79) | 1.18 | 0.15 |
| Past month cannabis use days Baseline | 20.44 (9.58) | 20.92 (8.67) | 20.89 (10.19) | 19.43 (10.27) | 0.238 | 0.79 |
| 3-Month | 17.77 (10.44) | 15.72 (10.60) | 18.68 (10.18) | 19.32 (10.42) | 1.15 | 0.32 |
Note: 4 participants did not identify as male or female.
The primary study analyses examined whether a statistically significant difference existed between intervention conditions on changes in driving after cannabis use or riding with a cannabis-impaired driver. The team conducted repeated measures mixed modeling analyses to examine study hypotheses: 1) participants in the PF + MIT and PF conditions will report greater reductions in DACU over time compared to participants in the IC condition, 2) participants in the PF + MIT condition will report greater reductions in DACU than participants in the PF condition, 3) participants in the PF + MIT and PF conditions will report greater reductions in RWCD over time compared to participants in the IC condition, and 4) participants in the PF + MIT condition will report greater reductions in RWCD than participants in the PF condition. Mixed modeling examines data similarly to repeated measures ANOVA; however, mixed modeling provides increased flexibility in handling missing data by utilizing all available data for each participant and provides ease of adaptation for multiple research designs (Hox, 2013).
Generalized linear mixed models (GLMM) represent an extension of linear mixed models to non-normal data. GLMM with a negative binomial distribution, which allows for over-dispersion in count outcomes, with a log link function were utilized for outcomes of non-normally distributed count data (i.e., total number of times driving after cannabis use and riding with a cannabis-impaired driver). The study used lme4 package in R to run these models. We found DACU and RWCD to be over dispersed (i.e., variance exceeds mean). For each model tested, DACU or RWCD served as the dependent variable. Given previous research showing sex differences in rates of cannabis use and evidence of sex differences in response to brief substance use interventions (Reinhardt et al., 2008), the study included sex a priori as a covariate in all models. The study estimated models with random intercepts and time as a fixed effect. Models included the dummy-coded variables for PF + MIT vs. IC as well as PF vs. IC as well as the two-way interactions between these dummy-coded variables and time (coded as 0 = Baseline and 1 = Follow-up) since study initiation. The study tested contrasts to compare baseline PF + MIT vs. PF as well as the two-way interactions of PF + MIT and PF with time post hoc by t-tests. The research team computed Cohen’s d effect sizes and interpreted them using the conventional metrics of d = 0.2, 0.5 and 0.8 indicating small, medium, and large effects (Cohen, 1992).
3. Results
3.1. Baseline and 3-month follow-up characteristics
Overall, participants reported driving after cannabis use an average of 25.2 times (SD = 24.62) in the past 3 months at baseline and 19.92 times (SD = 24.50) in the past 3 months at the 3-month follow-up. Participants reported riding with a driver who was under the influence of cannabis 14.49 times (SD = 19.41) at baseline and 9.52 times (SD = 14.12) in the past 3 months at 3-month follow-up. Participants reported using cannabis on an average of 20 days (SD = 9.55) in the past month at baseline and on an average of 17.8 days (SD = 10.44) at 3-month follow-up. Interestingly, 48 participants (49.5 %) reported using a ride-share service (i.e., Uber, Lyft) in the past 3 months after drinking alcohol whereas only 3 participants (3 %) reported using a ride-share service after using cannabis. The study found no significant baseline differences on demographic or outcome variables (see Table 1). Eight participants did not complete the 3-month follow-up (93.6 % overall follow-up rate; 2 from the PF condition, 4 from the IC condition, and 2 from the PF + MIT condition).
3.2. Analysis of study outcomes
We present results for the mixed models analyses in Table 2.
Table 2.
Fixed effects from generalized linear mixed models with sex as a covariate.
| Factor | Fixed Effects | SE | Z | 95 % CI |
|---|---|---|---|---|
| DACU: PF + MIT and PF vs. IC | ||||
| Intercept | 3.06 | 0.26 | 11.73*** | (2.551–3.575) |
| Condition - PF + MIT vs. IC | −0.13 | 0.28 | −0.45** | (−0.679−0.425) |
| Condition - PF vs. IC | −0.20 | 0.30 | −0.67 | (−0.783−0.385) |
| Sex (1 = women, 0 = male) | −0.10 | 0.22 | −0.45 | (−0.539−0.339) |
| Time (0 = baseline, 1 = follow-up) | −0.23 | 0.20 | −1.12 | (−0.621−0.169) |
| Condition - PF + MIT vs. IC × Time | −0.59 | 0.28 | −2.09* | (−1.133 to −0.037) |
| Condition - PF vs. IC × Time | −0.07 | 0.29 | −0.25 | (−0.647−0.502) |
| RWCD: PF + MIT and PF vs. IC | ||||
| Intercept | 1.93 | 0.32 | 6.03*** | (1.306−2.564) |
| Condition - PF + MIT vs. IC | 0.49 | 0.34 | 1.44 | (−0.177–1.161) |
| Condition - PF vs. IC | 0.16 | 0.36 | 0.45 | (−0.549−0.875) |
| Time (0 = baseline, 1 = follow-up) | −0.03 | 0.21 | −0.13 | (−0.449−0.391) |
| Sex (1 = women, 0 = male) | −0.06 | 0.28 | −0.20 | (−0.611−0.498) |
| Condition - PF + MIT vs. IC × Time | −1.15 | 0.30 | −3.88*** | (−1.725 to −0.568) |
| Condition - PF vs. IC × Time | −0.58 | 0.31 | −1.88 | (−1.194−0.025) |
Note: DACU = Driving after Cannabis use, RWCD = Riding with a Cannabis-Impaired Driver, PF + MIT = Personalized Feedback + MI style text messages, PF = Personalized Feedback only, IC = Information Control, CI = Confidence Interval. Sex was coded: 1 = women; 0 = men. Time was coded: 0 = baseline 1 = follow-up.
p < .05.
p < .01.
p < .001.
3.2.1. Driving after cannabis use
The study used generalized linear mixed models (GLMM) with a negative binomial distribution to determine whether participants in the PF + MIT condition displayed significantly greater reductions in DACU over time compared to participants in the IC and PF conditions. In a model with dummy-coded variables for PF + MIT and PF conditions (controlling for sex), the PF + MIT intervention was associated with significantly greater reductions in DACU over time compared to the IC condition (p < .05; Cohen’s d = 0.31). The study found no difference in slopes between the PF and IC conditions. When we examined post-hoc analyses comparing PF + MIT and PF conditions to one another, we did not find differences between these two interventions. PF + MIT participants (N = 38) significantly decreased their number of times DACU over time (Cohen’s d = 0.42), while participants in the PF condition (N = 28) did not change their number of times DACU (Cohen’s d = 0.00), and participants in the IC condition (N = 31) displayed slight decreases in DACU over time (Cohen’s d = 0.13; see Fig. 2).
Fig. 2.
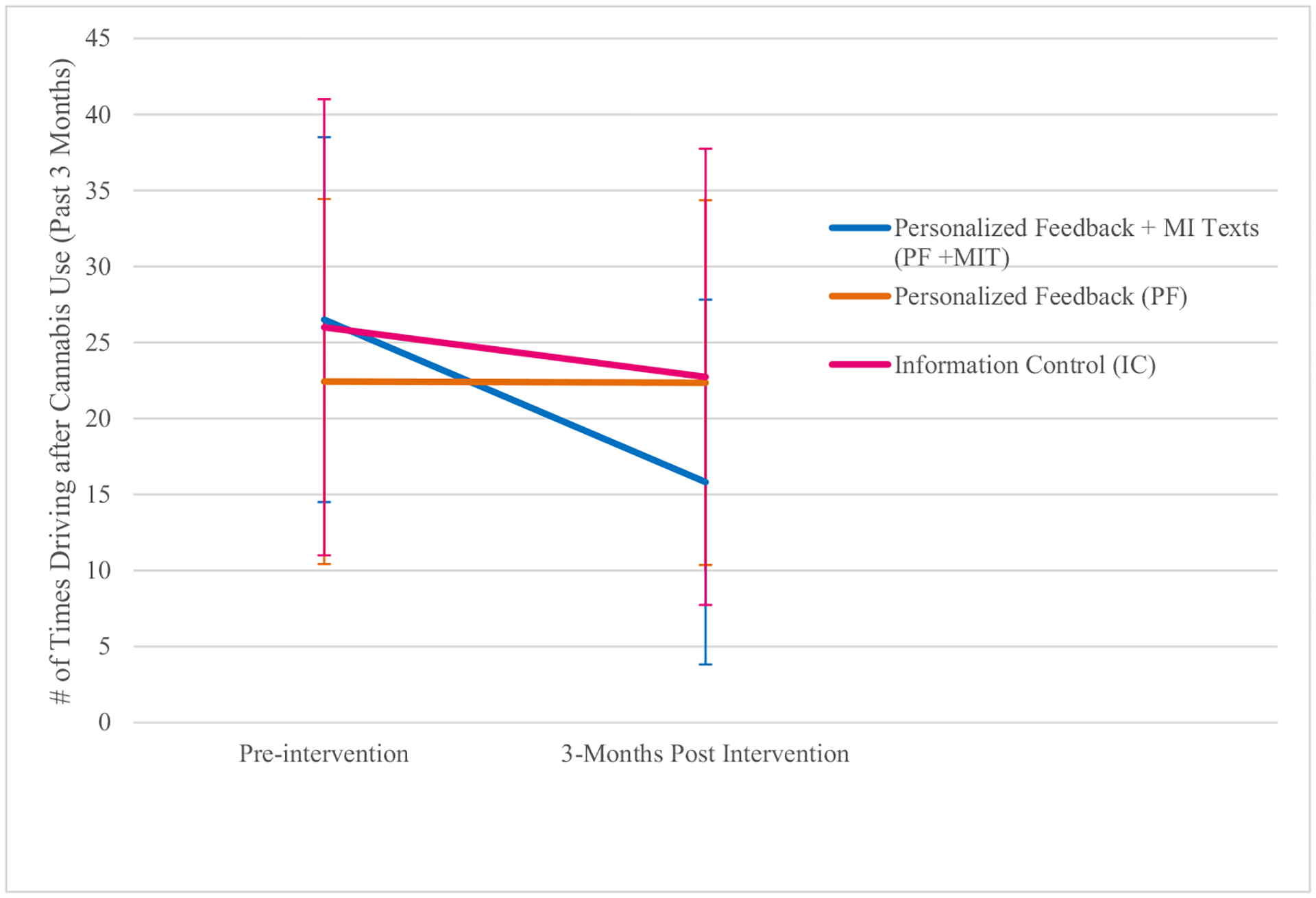
Number of times driving after cannabis use (+/−1 SEM) over time by condition (personalized feedback + MI text messages, feedback only, information only).
Note: SEM = standard error of mean.
3.2.2. Riding with a driver under the influence of cannabis
The study used generalized linear mixed models (GLMM) with a negative binomial distribution to determine whether participants in the PF + MIT condition displayed significantly greater reductions in RWCD over time compared to participants in the IC and PF conditions. In a model with dummy-coded variables for PF + MIT and PF conditions (controlling for sex), the PF + MIT intervention was associated with significantly greater reductions in RWCD over time compared to the IC condition (p < .001; Cohen’s d = 0.14). The study found no difference in slopes between the PF and IC conditions. When we examined post-hoc analyses comparing PF + MIT and PF conditions to one another, we did not find differences between these two. PFT participants (N = 38) significantly decreased their number of times riding with a driver who was under the influence of cannabis (Cohen’s d = 0.32), as did participants in the PF condition (Cohen’s d = 0.35). Participants in the IC condition (N = 31) displayed no differences in riding with a driver who was under the influence of cannabis (Cohen’s d = 0.04) (Fig. 3).
Fig. 3.
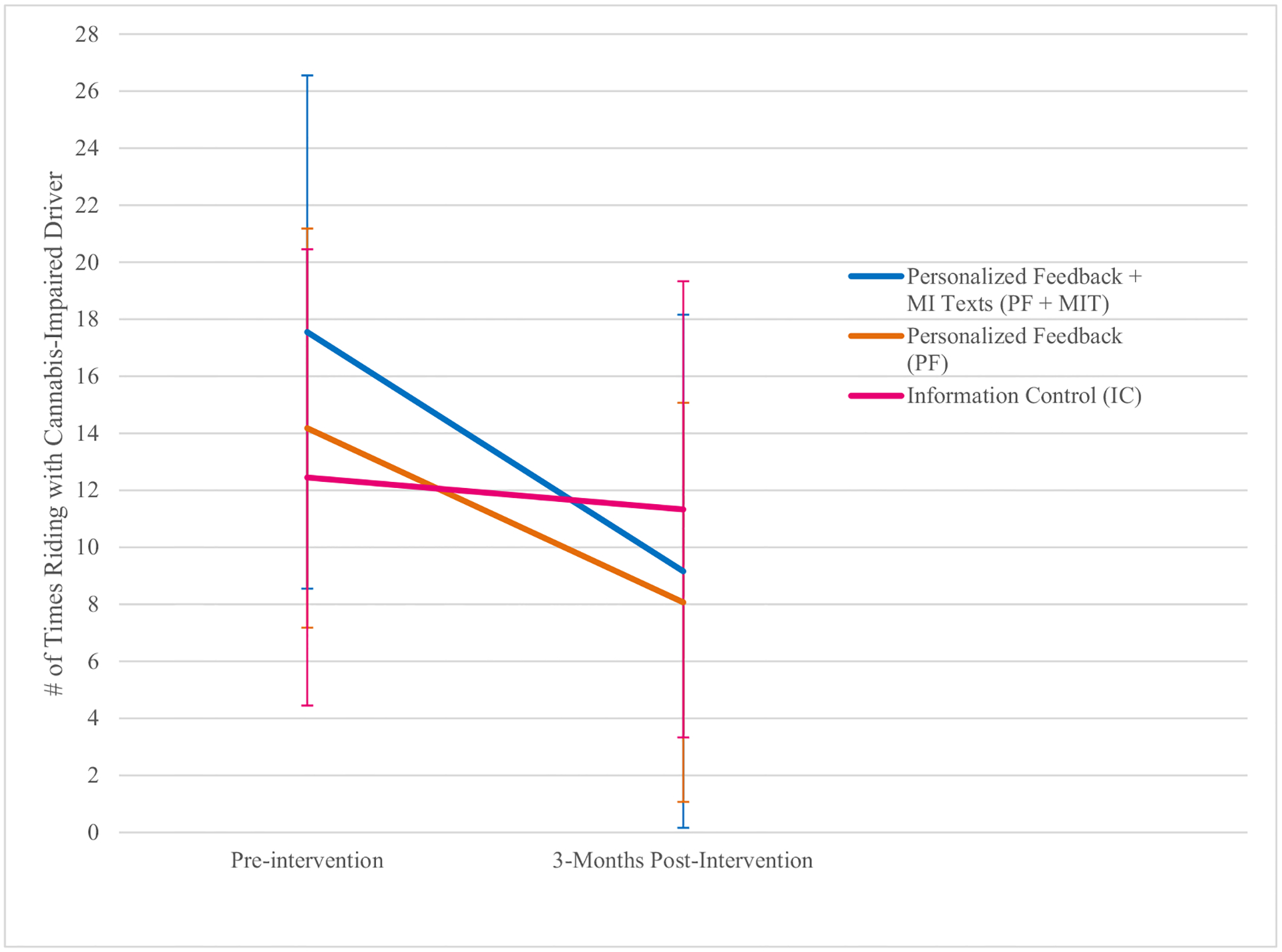
Number of times riding with a driver under the influence of cannabis (+/−1 SEM) over time by condition (personalized feedback + MI text messages, feedback only, information only).
Note: SEM = standard error of mean.
4. Discussion
Driving after cannabis use (DACU) and riding with a cannabis-impaired driver (RWCD) among emerging adults are significant public health concerns and represent two of the riskiest cannabis-related behaviors in terms of potential for fatal consequences. The current study evaluated a brief, mobile phone–based personalized feedback and MI-style interactive text messaging intervention to reduce DACU and RWCD among college cannabis users. The results provide initial support for the efficacy of this intervention. The article discusses specific findings below in conjunction with study limitations, implications, and future directions.
Consistent with previous research examining BIs to reduce alcohol-impaired driving among college students, DUI offenders, and emergency room patients (Brown et al., 2010; D’Amico et al., 2018; Mun et al., 2021; Ouimet et al., 2013; Schermer et al., 2006; Teeters et al., 2015), the current study found that a BI including personalized feedback led to significantly greater reductions in impaired driving compared to a control condition. These findings align with recently published findings by Mun and colleagues (Mun et al., 2021) that examined whether BIs reduce driving after drinking among college students. They compared: a) group motivational interviewing, b) BIs with stand-alone personalized feedback, and c) BIs including MI with personalized feedback and found that BIs including MI and personalized feedback outperformed the other two interventions in terms of reducing driving after 4+/5+ drinks. The findings of the current study extend these findings to DACU and RWCD, increasingly common risk behaviors reported by emerging adults. These results also add promising findings to the literature on cannabis-related BIs. Though meta-analyses and reviews of BIs targeting frequency of cannabis use have failed to show sustained reductions in frequency of cannabis use (Halladay et al., 2019; Imtiaz et al., 2020; Tanner-Smith et al., 2021), the results reported here provide preliminary evidence that a BI targeting a specific cannabis-related risk behavior, in this case driving after cannabis use, can successfully reduce this high-risk behavior without reducing overall cannabis-use frequency. Targeting specific risky behaviors associated with cannabis use, rather than focusing solely on frequency of use, is important from a harm reduction perspective and should be considered in future work aiming to reduce harm associated with cannabis use.
The findings of the current study also add to the literature on mobile-based interventions for substance impaired driving. Utilizing the same intervention approach with drinking drivers, Teeters et al. (2018) conducted a pilot trial with 84 college student drinkers (67.1 % women; average age = 23; 52.4 % Caucasian) who endorsed driving after drinking two or more drinks at least twice in the past three months. Generalized linear mixed modeling (GLMM) analyses revealed that students who received the mobile phone–based BI decreased their alcohol-impaired driving behaviors. The current study replicates and extends these findings in a sample of cannabis users endorsing recent DACU. Furthermore, these results show that the intervention not only resulted in changes in cognitions related to perceived dangerousness of DACU as found by Teeters et al. (2021), but also resulted in changes in cannabis-impaired driving behaviors.
Interestingly, the study found that the personalized feedback (PF) only condition did not result in significantly greater reductions in DACU than the information control (IC) condition. Though not significantly different from one another, the mean number of times DACU in the control condition decreased slightly over time while the mean number of times DACU in the PF condition remained almost identical from baseline to 3-month follow-up. While surprising, this finding may have been due to the nature of the control condition used in this study. Rather than using an assessment only or waitlist control, the current study included an informational control that was visually similar to the personalized feedback document (same number of graphics and pages) and included similar content (information on risks associated with substance use and substance-impaired driving). The only difference between the personalized feedback and the information conditions were that the information document contained only generic information and did not include any personalized content based on participants’ responses to the baseline questionnaire. The study team chose this control condition in an attempt to match information typically provided to students through general substance education programs, such as AlcoholEdu (an online program required by many college campuses prior to starting classes). In reality, the control condition likely provided much more information on the impact of cannabis use on driving abilities than is typical in standardized programs required by college campuses, which may have accounted for our finding that both the PF and IC conditions led to decreases in DACU over time.
Notably, effect size reductions in DACU were greater over time for participants in the PF + MIT condition compared to participants in the PF and IC conditions. Previous research directly comparing feedback only interventions vs. face-to-face interventions favor clinician contact and suggest that effects of interventions delivered without clinician contact tend to be smaller and dissipate at longer term follow-ups (Cadigan et al., 2015; Carey et al., 2012). Given these findings, we expected that the PF + MIT intervention would lead to significantly greater decreases in DACU compared to the PF intervention due to the MI text-messages. The current findings suggest that the extra resources associated with training an interventionist to deliver the MI text-messaging portion of the intervention may have been justified given that participants in the PF + MIT condition showed the greatest decreases over time in DACU. However, this conclusion remains speculative as the PF + MIT condition was not compared to an automated text-messaging condition, making it impossible to determine if employing an interventionist was crucial to these findings. Future research comparing personalized feedback and clinician delivered text-messaging to personalized feedback with automated text-messaging is especially important given that the interventionist component may reduce scalability of intervention dissemination.
4.1. Limitations
The current study has several limitations that should be considered when interpreting these findings. The sample size was lower than anticipated due to the Covid-19 pandemic. A planned second wave of data collection that would have resulted in a sample of 150 participants (50 per condition) was not able to be collected due to the pandemic coinciding with the termination of the grant funding period. The team paused data collection at the outbreak of the pandemic due to the drastic reductions in driving rates due to lockdown measures (Gupta et al., 2021). However, that significant effects were detected between the PF + MIT intervention vs. the information control condition is extremely promising given the lower-than-anticipated power to detect small effects. Future research replicating this procedure in a larger sample of emerging adults would lend increased confidence to the current findings. Furthermore, the study collected all cannabis use data via retrospective self-reports and measures did not account for how much cannabis was used before driving, timeframe of use, type of product, or potency of product used. Accurate assessments of cannabis use are common problems within cannabis research (Cuttler & Spradlin, 2017). Future research should include additional details related to cannabis use to gain a more nuanced assessment of intoxication and impairment levels prior to driving. While self-report measures can be subject to biases, research comparing self-reported cannabis use to biological measures (hair and urine sample) showed that self-reported frequency of use was the best predictor of clinician rated cannabis dependence (Curran et al., 2019). Furthermore, the study examined intervention effects only from baseline to 3 months postintervention, making it impossible to determine if effects would have persisted following this 3-month period. Future research should include longer-term follow-ups as previous research has shown that effects of BIs tend to shrink over time (Foxcroft et al., 2016). The current research is also limited in terms of generalizability given that the majority of the sample were White (80.1 %), female (67.4 %) college students. Future research should include more diverse samples to determine the efficacy of this intervention. Despite these limitations, the study has potential public health implications as it shows promising outcomes for changes in DACU and RWCD using a highly accessible, brief mobile phone–based intervention with personalized feedback and interactive text messaging.
4.2. Implications
Overall, the current study provides preliminary evidence that a mobile delivered BI with personalized feedback and MI-style interactive text-messaging results in significantly greater decreases in DACU and RWCD compared to an informational control. This is the first study to recruit based on recent DACU and specifically target DACU and RWCD. In addition to replicating the intervention in a larger sample and including longer-term follow-ups, future research should examine the impact of the intervention on driving after the combined use of alcohol and cannabis, an extremely risky behavior that is becoming more prevalent among emerging adults. Future research should also include noncollege emerging adults given recent increases in daily cannabis use among this population. Additionally, recent research on event-level predictors of alcohol-impaired driving using ecological momentary assessment suggests that momentary subjective judgments (perceptions of intoxication levels and dangerousness of driving after drinking) are the strongest predictors of intentions to drive after drinking (Motschman et al., 2020). Future work should determine if these findings replicate with intentions to drive after cannabis use. If so, an optimal intervention to reduce DACU and RWCD may combine a BI approach with just-in-time messages designed to increase perceptions of dangerousness and/or provide information on intoxication level in-the-moment in naturalistic settings.
Acknowledgements
This project was supported by the National Institute of General Medical Sciences (#8P20GM103436; PI: Teeters).
Footnotes
CRediT authorship contribution statement
Jenni Teeters: Funding acquisition, Conceptualization, Methodology, Formal analysis, Writing Original Draft, Revisions.
Nicole Armstrong: Data analyses and Table 2.
Shelby King: Writing- Original Draft; Writing- reviewing and editing.
Sterling Hubbard: Writing- Original Draft; Writing- reviewing and editing.
Declaration of competing interest
None.
References
- Arterberry BJ, Treloar H, & McCarthy DM (2017). Empirical profiles of alcohol and marijuana use, drugged driving, and risk perceptions. Journal of Studies on Alcohol and Drugs, 78(6), 889–898. 10.15288/jsad.2017.78.889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asbridge M, Hayden JA, & Cartwright JL (2012). Acute cannabis consumption and motor vehicle collision risk: Systematic review of observational studies and meta-analysis. BMJ, 344(feb09 2). 10.1136/bmj.e536. e536–e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berning A, Compton R, & Wochinger K (2015). Results of the 2013–2014 national roadside survey of alcohol and drug use by drivers. Journal of Drug Addiction, Education, and Eradication, 11(1), 47. [Google Scholar]
- Brady JE, & Li G (2013). Prevalence of alcohol and other drugs in fatally injured drivers: Alcohol and other drugs in drivers. Addiction, 108(1), 104–114. 10.1111/j.1360-0443.2012.03993.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TG, Dongier M, Ouimet MC, Tremblay J, Chanut F, Legault L, & Ng Ying Kin NMK (2010). Brief motivational interviewing for DWI recidivists who abuse alcohol and are not participating in DWI intervention: A randomized controlled trial. Alcoholism: Clinical and Experimental Research, 34, 292–301. [DOI] [PubMed] [Google Scholar]
- Cadigan JM, Haeny AM, Martens MP, Weaver CC, Takamatsu SK, & Arterberry BJ (2015). Personalized drinking feedback: A meta-analysis of in-person versus computer-delivered interventions. Journal of Consulting and Clinical Psychology, 83(2), 430–437. 10.1037/a0038394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, & Maisto SA (2007). Which heavy drinking college students benefit from a brief motivational intervention? Journal of Consulting and Clinical Psychology, 75(4), 663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Garey L, & Carey MP (2012). Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review, 32(8), 690–703. 10.1016/j.cpr.2012.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpino M, Langille D, Ilie G, & Asbridge M (2020). Cannabis-related driving and passenger behaviours among high school students: A cross-sectional study using survey data. CMAJ Open, 8(4), E754–E761. 10.9778/cmajo.20200081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1992). Quantitative methods in psychology: A power primer. Psychological Bulletin. [DOI] [PubMed] [Google Scholar]
- Curran HV, Hindocha C, Morgan CJA, Shaban N, Das RK, & Freeman TP (2019). Which biological and self-report measures of cannabis use predict cannabis dependency and acute psychotic-like effects? Psychological Medicine, 49(9), 1574–1580. 10.1017/S003329171800226X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuttler C, & Spradlin A (2017). Measuring cannabis consumption: Psychometric properties of the daily sessions, frequency, age of onset, and quantity of cannabis use inventory (DFAQ-CU). PLoS One, 12(5), e0178194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Parast L, Shadel WG, Meredith LS, Seelam R, & Stein BD (2018). Brief motivational interviewing intervention to reduce alcohol and marijuana use for at-risk adolescents in primary care. Journal of Consulting and Clinical Psychology, 86 (9), 775–786. 10.1037/ccp0000332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drislane LE, Waller R, Martz ME, Bonar EE, Walton MA, Chermack ST, & Blow FC (2019). Therapist and computer-based brief interventions for drug use within a randomized controlled trial: Effects on parallel trajectories of alcohol use, cannabis use, and anxiety symptoms. Addiction, 115(1), 158–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foxcroft DR, Coombes L, Wood S, Allen D, Almeida Santimano NM, & Moreira MT (2016). Motivational interviewing for the prevention of alcohol misuse in young adults. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD007025.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta M, Pawar NM, & Velaga NR (2021). Impact of lockdown and change in mobility patterns on road fatalities during COVID-19 pandemic. Transportation Letters, 13(5–6), 447–460. 10.1080/19427867.2021.1892937 [DOI] [Google Scholar]
- Hall AK, Cole-Lewis H, & Bernhardt JM (2015). Mobile text messaging for health: A systematic review of reviews. Annual Review of Public Health, 36(1), 393–415. 10.1146/annurev-publhealth-031914-122855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halladay J, Scherer J, MacKillop J, Woock R, Petker T, Linton V, & Munn C (2019). Brief interventions for cannabis use in emerging adults: A systematic review, meta-analysis, and evidence map. Drug and Alcohol Dependence. , Article 107565. 10.1016/j.drugalcdep.2019.107565 [DOI] [PubMed] [Google Scholar]
- Hartman RL, & Huestis MA (2013). Cannabis effects on driving skills. Clinical Chemistry, 59(3), 478–492. 10.1373/clinchem.2012.194381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron KE, Romano KA, & Braitman AL (2019). Mobile technology use and mHealth text message preferences: An examination of gender, racial, and ethnic differences among emerging adult college students. MHealth, 5(2), 1–13. 10.21037/mhealth.2019.01.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Zha W, & Smyth D (2017). Magnitude and trends in heavy episodic drinking, alcohol-impaired driving, and alcohol-related mortality and overdose hospitalizations among emerging adults of college ages 18–24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs, 78(4), 540–548. 10.15288/jsad.2017.78.540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostiuc S, Moldoveanu A, Negoi I, & Drima E (2018). The association of unfavorable traffic events and cannabis usage: A meta-analysis. Frontiers in Pharmacology, 9, 99. 10.3389/fphar.2018.00099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hox JJ (2013). Multilevel regression and multilevel structural equation modeling. The Oxford Handbook of Quantitative Methods, 2(1), 281–294. [Google Scholar]
- Imtiaz S, Roerecke M, Kurdyak P, Samokhvalov AV, Hasan OSM, & Rehm J (2020). Brief interventions for cannabis use in healthcare settings: Systematic review and meta-analyses of randomized trials. Journal of Addiction Medicine, 14(1), 78–88. 10.1097/ADM.0000000000000527 [DOI] [PubMed] [Google Scholar]
- Johnston et al. , n.d., Johnston LD Miech RA O’Malley PM Bachman JG Schulenberg JE Patrick ME (n.d.). 2018. overview key findings on adolescent drug use. 127. [Google Scholar]
- Kelly E, Darke S, & Ross J (2004). A review of drug use and driving: Epidemiology, impairment, risk factors and risk perceptions. Drug and Alcohol Review, 23(3), 319–344. [DOI] [PubMed] [Google Scholar]
- Kerr DCR, Bae H, & Koval AL (2018). Oregon recreational marijuana legalization: Changes in undergraduates’ marijuana use rates from 2008 to 2016. Psychology of Addictive Behaviors, 32(6), 670–678. 10.1037/adb0000385 [DOI] [PubMed] [Google Scholar]
- Lane TJ, & Hall W (2019). Traffic fatalities within US states that have legalized recreational cannabis sales and their neighbours. Addiction, 114(5), 847–856. 10.1111/add.14536 [DOI] [PubMed] [Google Scholar]
- Li K, Ochoa E, Vaca FE, & Simons-Morton B (2018). Emerging adults riding with marijuana-, alcohol-, or illicit drug–impaired peer and older drivers. Journal of Studies on Alcohol and Drugs, 79(2), 277–285. 10.15288/jsad.2018.79.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K, Simons-Morton BG, Vaca FE, & Hingson R (2014). Association between riding with an impaired driver and driving while impaired. Pediatrics, 133(4), 620–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M-C, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, & Li G (2012). Marijuana use and motor vehicle crashes. Epidemiologic Reviews, 34(1), 65–72. 10.1093/epirev/mxr017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann RE, Adlaf E, Zhao J, Stoduto G, Ialomiteanu A, Smart RG, & Asbridge M (2007). Cannabis use and self-reported collisions in a representative sample of adult drivers. Journal of Safety Research, 38(6), 669–674. 10.1016/j.jsr.2007.09.004 [DOI] [PubMed] [Google Scholar]
- Mason M, Ola B, Zaharakis N, & Zhang J (2015). Text messaging interventions for adolescent and young adult substance use: A meta-analysis. Prevention Science, 16(2), 181–188. 10.1007/s11121-014-0498-7 [DOI] [PubMed] [Google Scholar]
- Mason MJ, Zaharakis NM, Russell M, & Childress V (2018). A pilot trial of text-delivered peer network counseling to treat young adults with cannabis use disorder. Journal of Substance Abuse Treatment, 89(865), 1–10. 10.1016/j.jsat.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M, Nakamura A, Bolze C, Hausfater F, El Khoury F, Mary-Krause M, & Azevedo Da Silva M (2019). Does liberalisation of cannabis policy influence levels of use in adolescents and young adults? A systematic review and meta-analysis. BMJ Open, 9(7), Article e025880. 10.1136/bmjopen-2018-025880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Leffingwell T, Claborn K, Meier E, Walters S, & Neighbors C (2013). Personalized feedback interventions for college alcohol misuse: An update of Walters & Neighbors (2005). Psychology of Addictive Behaviors, 27(4), 909–920. 10.1037/a0031174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2013). In Motivational interviewing: Helping people change (3rd ed., p. 482). Guilford Press. pp. xii. [Google Scholar]
- Motschman CA, Hatz LE, McCarty KN, Merkle EC, Trull TJ, & McCarthy DM (2020). Event-level predictors of alcohol-impaired driving intentions. Journal of Studies on Alcohol and Drugs, 81(5), 647–654. 10.15288/jsad.2020.81.647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mun E-Y, Li X, Lineberry S, Tan Z, Huh D, Walters ST, Zhou Z, Larimer ME, & in Collaboration with Project INTEGRATE Team. (2021). Do brief alcohol interventions reduce driving after drinking among college students? A two-step meta-analysis of individual participant data. Alcohol and Alcoholism. , Article agaa146. 10.1093/alcalc/agaa146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osilla KC, Seelam R, Parast L, & D’Amico EJ (2019). Associations between driving under the influence or riding with an impaired driver and future substance use among adolescents. Traffic Injury Prevention, 20(6), 563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimet MC, Dongier M, Di Leo I, Legault L, Tremblay J, Chanut F, & Brown TG (2013). A randomized controlled trial of brief motivational interviewing in impaired driving recidivists: A 5-year follow-up of traffic offenses and crashes. Alcoholism: Clinical and Experimental Research, 37(11), 1979–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parnes JE, Smith JK, & Conner BT (2018). Reefer madness or much ado about nothing? Cannabis legalization outcomes among young adults in the United States. International Journal of Drug Policy, 56, 116–120. 10.1016/j.drugpo.2018.03.011 [DOI] [PubMed] [Google Scholar]
- Patrick ME, Graupensperger S, Dworkin ER, Duckworth JC, Abdallah DA, & Lee CM (2021). Intoxicated driving and riding with impaired drivers: Comparing days with alcohol, marijuana, and simultaneous use. Drug and Alcohol Dependence, 225, Article 108753. 10.1016/j.drugalcdep.2021.108753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhardt S, Bischof G, Grothues J, John U, Meyer C, & Rumpf H (2008). Gender differences in the efficacy of brief interventions with a stepped care approach in general practice patients with alcohol-related disorders. Alcohol and Alcoholism, 43 (3), 334–340. 10.1093/alcalc/agn004 [DOI] [PubMed] [Google Scholar]
- Rideout V, & Robb MB (2018). Social media, social life: Teens reveal their experiences. Common Sense Media. https://www.commonsensemedia.org/sites/default/files/uploads/research/2018_cs_socialmediasociallife_fullreport-final-release_2_lowres.pdf. [Google Scholar]
- Riper H, Hoogendoorn A, Cuijpers P, Karyotaki E, Boumparis N, Mira A, Andersson G, Berman AH, Bertholet N, Bischof G, Blankers M, Boon B, Boß L, Brendryen H, Cunningham J, Ebert D, Hansen A, Hester R, Khadjesari Z Smit JH, … (2018). Effectiveness and treatment moderators of internet interventions for adult problem drinking: An individual patient data meta-analysis of 19 randomised controlled trials. PLoS Medicine, 15(12), Article e1002714. 10.1371/journal.pmed.1002714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano E, Kelley-Baker T, Hoff S, Eichelberger A, & Ramírez A (2019). Use of alcohol and cannabis among adults driving children in Washington state. Journal of Studies on Alcohol and Drugs, 80(2), 196–200. 10.15288/jsad.2019.80.196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schermer CR, Moyers TB, Miller WR, & Bloomfield LA (2006). Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. Journal of Trauma and Acute Care Surgery, 60(1), 29–34. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Johnston L, O’Malley P, Bachman J, Miech R, & Patrick M (2020). Monitoring the Future national survey results on drug use, 1975–2019: Volume II, college students and adults ages 19–60. [Google Scholar]
- Sobell LC, Brown J, Leo GI, & Sobell MB (1996). The reliability of the alcohol timeline followback when administered by telephone and by computer. Drug and Alcohol Dependence, 42(1), 49–54. 10.1016/0376-8716(96)01263-X [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. 10.1016/j.jsat.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, Parr NJ, Schweer-Collins M, & Saitz R (2021). Effects of brief substance use interventions delivered in general medical settings: A systematic review and meta-analysis. Addiction, 1–13. 10.1111/add.15674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, Borsari B, Martens MP, & Murphy JG (2015). Brief motivational interventions are associated with reductions in alcohol-impaired driving among college drinkers. Journal of Studies on Alcohol and Drugs, 76(5), 700–709. 10.15288/jsad.2015.76.700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, King SA, & Hubbard SM (2021). A mobile phone–based brief intervention with personalized feedback and interactive text messaging is associated with changes in driving after cannabis use cognitions in a proof-of-concept pilot trial. Experimental and Clinical Psychopharmacology, 29(2), 203–209. 10.1037/pha0000442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, Soltis KE, & Murphy JG (2018). A mobile phone–based brief intervention with personalized feedback and text messaging is associated with reductions in driving after drinking among college drinkers. Journal of Studies on Alcohol and Drugs, 79(5), 710–719. 10.15288/jsad.2018.79.710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Bohnert K, Resko S, Barry KL, Chermack ST, Zucker RA, Zimmerman MA, Booth BM, & Blow FC (2013). Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: One year outcomes. Drug and Alcohol Dependence, 132(3), 646–653. 10.1016/j.drugalcdep.2013.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]


