Introduction
Terra firma-forme dermatosis (TFFD) is a benign disorder that was first described by Duncan, Tschen, and Knox in 1987.[1] The disease is also commonly known as Duncan’s dirty dermatosis. The term “terra firma” has Latin roots and is translated to “dry land” in English, owing to the distinct clinical appearance which resembles the Sun-dried clods of land.[2] Often, the condition is misdiagnosed as dermatitis neglecta (DN), contributing to its wide underestimation.
Epidemiology
The estimated prevalence of TFFD according to a retrospective study conducted over a period of 1 year in children under the age of 18 years has been 2.19%.[3] There is no known gender predilection or familial preponderance for TFFD. There is a bimodal peak of incidence with the first peak seen during the first 10 years of life and a second peak during 60–80 years of age.[4,5,6] TFFD has virtually been reported in all ethnic groups, namely, Asians, Afro-Americans, Hispanics, Middle Eastern, and Caucasians.[5,6,7,8]
Pathogenesis
Different authors have laid down various theories in an attempt to explain the complex pathogenesis. One school of thought believes that the nidus of TFFS is retention hyperkeratosis triggered by delayed keratinocyte maturation responsible for impaired desquamation along with an accumulation and dirt and sebum.[9,10] However, Berk et al. have proposed that TFFD is largely a papillomatous disorder with acanthosis and orthohyperkeratosis that can trap dirt, sebum, or other environmental debris.[11] According to Erkek et al., there is an inhibition of the epidermal keratinoplastic activities which inhibits the detachment of keratinocytes and triggers retention hyperkeratosis and clumping of corneocytes.[12]
The three most commonly cited factors in the etiopathogenesis of DN are the role of microbia, physical factors, and genetic susceptibility with a complex interplay between these agents. Shan et al. and Trave et al. have postulated the role of Malassezia species in the pathogenesis of TFFD. In fact, even saprophytic organisms have been considered as a possible trigger.[13,14]
1. Physical factors
The development of TFFD on sites adjacent to a surgical wound, poor hygiene in physically or mentally disable individuals, over flexures, and underneath a piece of jewelry-clad site, all favor the role of physical factors. Other physical factors incriminated in the pathogenesis of TFFD are prolonged sun exposure, xerosis, sebum, and sweat accumulation.[15,16]
2. Genetic susceptibility
A few case reports have suggested the role of genetic predisposition in TFFD; however, the literature on its genetic inheritance is still inconclusive.[4,6] A genetic disorder of delayed keratinization could explain the first peak of TFFD seen in patients between 0 and 10 years of age. Although there is no racial predilection,[17,18] fillagrin gene mutation also plays a minor role.
Clinical features
Classical TFFD is characterized by the development of brownish-gray to black macules and patches having a typical dirt-like appearance [Figure 1]. Other variants include verrucous [Figure 2], papillomatous, and reticular [Figure 3] patterns with islands of spared normal skin between the lesions.[18]
Figure 1.
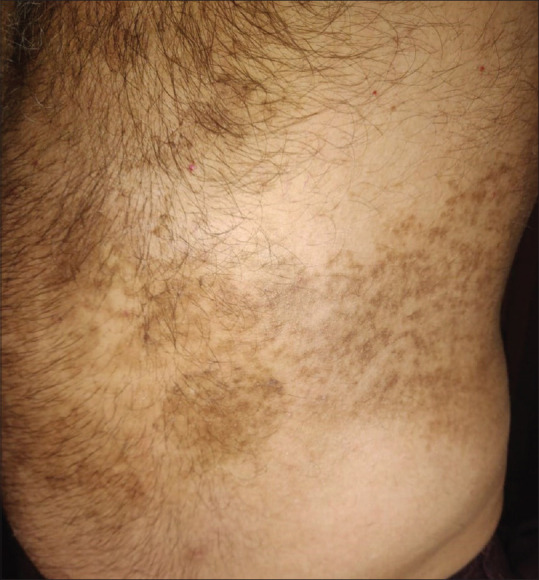
Classical TFFD over flank
Figure 2.

Verrucous TFFD over axillary area
Figure 3.

Generalized reticular TFFD in a 10-year-old boy
On palpation, often the lesions have a smooth, velvety, or scaly texture with fine scales. Often the ailment goes unnoticed owing to its asymptomatic nature. The most commonly involved sites are face, neck, trunk, navel, ankle, and concave contours of body.[19] In pediatric cases, navel is a commonly affected site, where TFFD is often falsely diagnosed as omphalitis or melanocytic nevi.[4] TFFD in postoperative period over surgical sites is also a common presentation.[9] Dermoscopic features include brown scales and large, polygonal brown clods interrupted with furrows and arranged in a linear pattern, creating a mosaic appearance [Figure 4].[2,20]
Figure 4.

Keratin whorl in the stratum corneum (H and E, 400×)
Histopathology
Histopathology reveals the presence of lamellar hyperkeratosis and retention hyperkeratosis, with focal areas of compact and whorled orthokeratosis, keratin whorls and globules, marked acanthosis, and papillomatosis, along with basal layer hypermelanosis [Figure 5]. The dermis has the presence of mild perivascular lymphocytic infiltration. The periodic acid Schiff stain can reveal yeast aggregates within the whorled orthokeratosis.[15] Unlike DN, there is the absence of anastomosing rete ridges in TFFD.[20]
Figure 5.

Dermoscopic images of a case with TFFD showing plate-like scales represented as polygonal clods in mosaic pattern (DermLite DL3, magnification ×10)
Differential diagnosis
TFFD is a differential diagnosis for a large number of dermatoses. The most common differential diagnoses in children are DN and the so-called dirty neck sign in atopic dermatitis.[21] Other differential diagnoses include post-inflammatory hyperpigmentation, tinea versicolor, ichthyosis, confluent and reticulated papillomatosis, and acanthosis nigricans.[22,23,24,25] Other differential diagnoses have been enlisted in Table 1.
Table 1.
Differential diagnosis of TFFD
| Diagnosis | Clinical manifestations | Histopathological features | Identifying features |
|---|---|---|---|
| Dermatitis neglecta | Adherent hyperpigmented papules, polygonal plaques, or verrucous lesions with poor hygiene | Hyperkeratosis, acanthosis, papillomatosis, and lamellar orthokeratosis | Hyperpigmented well-define cornflake-like waxy scales on dermoscopy Soap-water test is positive |
| Acanthosis nigricans | Hyperpigmented velvety plaques and increased skin markings over intertriginous areas | Hyperkeratosis, papillomatosis, minimal to no acanthosis, no hypermelanosis | Dark brownish clods with crista cutis on dermoscopy |
| Confluent and reticulated papillomatosis | Persistent erythematous to hyperpigmented scaly macules or papillomatous papules and coalescing confluent plaques distributed centrally and exhibiting a reticular pattern over the edges over upper trunk | Hyperkeratosis, papillomatosis with superficial dermal perivascular lymphocytic infiltration | Cobblestone pattern formed by polygonal flat-topped globules surrounded by whitish striae on dermoscopy |
| Dirty neck syndrome | Reticulate or rippled hyperpigmentation in patients with atopic dermatitis, predominantly involving the anterolateral aspects of the neck | Acanthosis, basement membrane thickening, epidermal hypermelanosis, dermal melanophages | Presence of other clinical features of atopic dermatitis |
| Postinflammatory hyperpigmentation | Hyperpigmented macules or patches over sites of healed inflammation | Epidermal or dermal melanosis | |
| Icthyosis | Genodermatoses with impairment in keratinization | Icthyosis vulgaris: moderate hyperkeratosis hypogranulosis X-linked icthyosis: hyperkeratosis with hypergranulosis | Positive family history |
| Intertriginous granular parakeratosis | Hyperpigmented hyperkeratotic papules and coalescing plaques over intertriginous areas | Acanthosis, hyperparakeratosis and papillomatosis, with basophilic keratohyalin granules | |
| Verrucous epidermal nevus | Congenital to early-acquired fleshy-to-brown, papillomatous papules and coalescing plaques, along Blaschko’s lines | Acanthosis, hyperkeratosis, papillomatosis, and epidermolytic hyperkeratosis | Thick brown branched lines and circles, terminal hairs with dotted vessels on dermoscopy |
| Frictional melanosis | Hyperpigmented patches over bony sites and friction-prone regions | Epidermal hypermelanosis, dermal melanophages | Brownish structureless zones in reticular pattern on dermoscopy |
| Macular amyloidosis | Pruritic hyperpigmented patches in ripple-like patterns over extremities and upper back | Basal layer hyperpigmentation. Globular deposits of amyloid material in papillary dermis and melanophages | Central brown to white hub at the center with brown fine radiating streaks, leafy projections, and dots on dermoscopy |
| Tinea versicolor (pigmented pityriasis versicolor) | Discreet to coalescent brown, hyperkeratotic scaly patches over head and neck | Orthohyperkeratosis and budding spores in stratum corneum with silent dermis | Yellow-green fluorescence on wood lamp |
| Ashy dermatosis | Round to oval ashy-colored hyperpigmented macules symmetrically involving the trunk | Lichenoid infiltration with macrophages | Irregular brown-grey linear dots and globules over pinkish-brown background. Irregular linear vascular pattern on dermoscopy |
| Dowling–Degos syndrome | Genodermatosis with macular or papular folliculocentric lesions. Arrangement of lesion in a lacy or reticular pattern predominantly over folds | Elongated or branched rete ridges having increased melanin deposition over the tips. Suprapapillary epithelium sparing | Irregular brownish projections around central hypopigmented, indicative of follicular epithelium on dermoscopy |
| Acroangiodermatitis of Mali | Purplish-blue to brown papules and plaques located on the medial and lateral malleoli | Hyperparakeratosis, epidermal hyperplasia, pseudo-sarcomatous capillary proliferation, and perivascular inflammation in the dermis, with extravasated red blood cells and hemosiderin deposits | Red or blue lacunae, white rail lines, with whitish veil along with scattered hemorrhagic crusts over a pinkish background on dermoscopy |
| Epidermolytic hyperkeratosis of the nipple and areola | Warty, hyperpigmented papules or plaques on the nipple and/or areola | Orthohyperkeratosis, filiform acanthosis, papillomatosis, and keratin plugging, hyperpigmented rete ridges, and a dermal lymphocytic infiltrate | Whitish papillomatous surface with white scales and brown hyperkeratotic deposits distributed on the cristae on dermoscopy |
| Scalp discoloration from selenium sulfide shampoo | Red-brown discoloration of scalp skin and appendages with/without desquamation | Pigment deposit within keratotic debris and parahyperkeratosis | Suggestive clinical history |
1. Dermatitis neglecta
DN is the most common misdiagnosis of TFFD.[21] Although many authors have highlighted that the differences between these two entities are more semantic than practical, there are still some key differences between these two dermatoses which have been tabulated in Table 2.
Table 2.
Differentiating features between terra firma-forme dermatosis and dermatitis neglecta
| Terra firma-forme dermatosis | Dermatitis neglecta | |
|---|---|---|
| Synonym | Duncan’s dirty dermatosis | Dermatitis passivata |
| Etiology | Unknown Genetic predisposition | An acquired disorder in patients with unclean habits |
| Pathogenesis | Delayed maturation and retention of corneocytes and melanocytes | Accumulation of sebum, sweat, and dirt within the keratin layers |
| Hygiene status | Good Adequate cleansing | Poor Inadequate skin cleansing |
| Clinical features | Brown grey velvety patches and plaques. Verrucous, papillomatous, or reticular patterns with islands of sparing | Hyperpigmented macules and plaques with corn-flake-like brown scales |
| Histopathological feature | Lamellar hyperkeratosis, whorled orthokeratosis, keratin whorls, marked acanthosis, basal layer hypomelanosis, papillomatosis, and perivascular lymphohistiocytic infiltration | Orthokeratotic hyperkeratosis and mild acanthosis with anastomosing rete ridges |
| Dermatoscopic features | Hexagonal brown plate-like scales, which are organized in cobblestone or mosaic patterns | Waxy cornflake-like brownish scales |
| Soap-water test | Wiping with soap-water does not clear the lesions | Wiping with soap-water clears the lesions |
| The alcohol swab test | 70% isopropyl alcohol swab clears lesions | 70% isopropyl alcohol swab clears lesions |
| Management | 70% isopropyl alcohol wipe, emollients, keratolytics, alpha-hydroxy acids, topical retinoids, and CO2 laser (for resistant cases) | Regular bathing and good hygiene practice Keratolytics for recurrent cases |
| Prognosis | Poor response to treatment and frequent recurrences | Good response to treatment |
The alcohol swab test is one useful test which can differentiate TFFD from DN. While simple soap water can wipe off DN, in order to wipe off the scales of TFFD, only 70% isopropyl alcohol has been found to be effective.
Associated conditions
The most frequently associated disease is atopic dermatitis. Other ailments include xerosis, asthma, allergic rhinitis, and acne. There is also a possible association between TFFD and pregnancy (periareolar lesions), acanthosis nigricans (flexural lesions), insulin resistance, and pituitary adenoma.[2,12]
Treatment
The usage of isopropyl alcohol in 70% is both diagnostic and therapeutic for TFFD. However, unlike DN, soap-water test is negative [Figure 6]. As TFFD is primarily a disorder of hyperkeratotic retention, keratolytics are used as its first-line treatment. In case of early onset, genital, facial, or generalized TFFD, the patients benefit from a combination of keratolytics and topical calcineurin inhibitors, alpha hydroxy acids, topical retinoids, or salicylic acid. Localized hyperkeratotic TFFD, on the other hand, is better dealt with stronger solvents like acetone or a higher concentration of keratolytics. In fact, recently even fractional CO2 laser has been utilized as an effective treatment modality by Chun et al.[26]
Figure 6.

Negative soap-water test
Indian scenario
Despite its wide prevalence, a quick PubMed search reveals that there are only a handful of reports on TFFD from India in the past 8 years [Table 3].[17,27,28,29,30,31] This lack of recognition and research on TFFD in India highlights the need for increased awareness and understanding of this condition within the medical community.
Table 3.
Reports on TFFD from the Indian subcontinent
| Authors | Type of report | Clinical features |
|---|---|---|
| Kumar et al.[17] | Observational study | 46 cases; Classical dirt-like plaques (80.43%), reticulate (6.5%), verrucous (4.34%), stuck-on appearance (4.34%), and linear lesions (4.34%) |
| Panchal et al.[28] | Case report | 19-year-old female; extensive TFFD with symmetrical brownish-black verrucous papules and plaques over the chest and medial aspect of thighs |
| Naveen et al.[29] | Case report | 20-year-old male; multiple hyperpigmented plaques of TFFD over healing lesions of chicken pox on the trunk and back. |
| Verma et al.[30] | Case report | 40-year-old male; on treatment for psoriasis. TFFD following erratic application of heavy emollient and betamethasone valerate-salicylic acid ointment over bilateral legs. Dermatoscopic features: cobblestone appearance. |
| Saha et al.[31] | Case report | 8-year-old boy; TFFD lesions with hyperkeratotic papules over neck and upper chest. |
Till date, there has only been one major clinical study on TFFD in India, conducted by Kumar et al. The most common clinical pattern in their study was classical dirt-like plaques in 80.43% cases, followed by 6.5% cases of reticular TFFD, and 4.34% cases each of verrucous and linear TFFD.[17]
Conclusion
TFFD is a common but hugely underreported dermatosis with a predilection for the pediatric population. The diagnosis of TFFD in clinically suspected cases can be diagnosed by a positive alcohol swab test but a negative soap-water test. A consistent finding in histopathology is whorled hyperkeratosis. Noninvasive modalities like dermoscopy could aid in the rapid diagnosis, averting the need for histopathological analysis. A dermatologist must always be on the lookout to proficiently differentiate TFFD from other similar-looking conditions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Duncan WC, Tschen JA, Knox JM. Terra firma-forme dermatosis. Arch Dermatol. 1987;123:567–9. [PubMed] [Google Scholar]
- 2.Sechi A, Patrizi A, Savoia F, Leuzzi M, Guglielmo A, Neri I. Terra firma-forme dermatosis: A systematic review. Int J Dermatol. 2021;60:933–43. doi: 10.1111/ijd.15301. [DOI] [PubMed] [Google Scholar]
- 3.Akçay G, Alataş ET, Doğan G. A retrospective analysis of cases with terra firma-forme dermatosis: Is it an entity related to allergic diseases? Van Med J. 2019;26:1–28. [Google Scholar]
- 4.Berk DR, Bruckner AL. Terra firma-forme dermatosis in a 4-month-old girl. Pediatr Dermatol. 2011;28:79–81. doi: 10.1111/j.1525-1470.2010.01220.x. [DOI] [PubMed] [Google Scholar]
- 5.Mattessich S, Aubert P, Rees A. Bilateral brown plaques behind the ears. Cutis. 2018;102:E1–3. [PubMed] [Google Scholar]
- 6.Özuğuz P, Kaçar SD, Kurtipek GS, Tunçez Akyürek FATMA. The early onset case of terra firma forme dermatosis. Tıp AraştırmalarıDergisi. 2015;13:137–9. [Google Scholar]
- 7.Berk DR. Terra firma-forme dermatosis: A retrospective review of 31 patients. Pediatr Dermatol. 2012;29:297–300. doi: 10.1111/j.1525-1470.2011.01422.x. [DOI] [PubMed] [Google Scholar]
- 8.Abdalla JE, Cruse A, Patel N, Brodell R. Terra firma-forme dermatosis, keratotic form. SKIN J Cutan Med. 2019;3:212–4. [Google Scholar]
- 9.O’Brien TJ, Hall AP. Terra firma-forme dermatosis. Australas J Dermatol. 1997;38:163–4. doi: 10.1111/j.1440-0960.1997.tb01138.x. [DOI] [PubMed] [Google Scholar]
- 10.Kurtipek GS, Akyürek FT, Ataseven A, Kocaoğlu Ç. Terra firma-forme €dermatosis in childhood: Two cases. J Turk Acad Dermatol. 2015;9:1591c2. [Google Scholar]
- 11.Berk DR, Mutizwa MM. Comment regarding the histopathology of terra firma-forme dermatosis. J Cutan Pathol. 2012;39:300–1. doi: 10.1111/j.1600-0560.2011.01818.x. [DOI] [PubMed] [Google Scholar]
- 12.Erkek E, Sahin S, Çetin ED, Sezer E. Terra firma-forme dermatosis. Indian J Dermatol Venereol Leprol. 2012;78:358–60. doi: 10.4103/0378-6323.95455. [DOI] [PubMed] [Google Scholar]
- 13.Shan SJ, Xu TH, Liu J, Lin J, Yin S, Hong Y, et al. Cutaneous dirt-adherent disease with single apparent transverse leukonychia on the fingernails. Arch Dermatol. 2009;145:1070–1. doi: 10.1001/archdermatol.2009.208. [DOI] [PubMed] [Google Scholar]
- 14.Trave I, Burlando M, Cozzani E, Parodi A. Could terra firma-forme dermatosis induce eczematous halo dermatitis? An hypothesis. G Ital Dermatol Venereol. 2020;155:241–3. doi: 10.23736/S0392-0488.18.05945-X. [DOI] [PubMed] [Google Scholar]
- 15.Lora V, Ardigò M, Catricalà C, Cota C. Terra firma-forme dermatosis. J Cutan Pathol. 2014;41:141–3. doi: 10.1111/cup.12241. [DOI] [PubMed] [Google Scholar]
- 16.Berk DR. Terra firma-forme dermatosis: A retrospective review of 31 patients. Pediatr Dermatol. 2012;29:297–300. doi: 10.1111/j.1525-1470.2011.01422.x. [DOI] [PubMed] [Google Scholar]
- 17.Kumar R, Singh A, Badyal R, Jain SK, Nyati A. Terra firma-forme dermatosis: A hospital-based clinico-epidemiological study at a tertiary care centre in northern India. Pigment Int. 2020;7:44–9. [Google Scholar]
- 18.Pallure V, Ameline M, Plantin P, Bessis D. [Terra firma-forme dermatosis] Ann Dermatol Venereol. 2013;140:693–8. doi: 10.1016/j.annder.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Sechi A, Patrizi A, Savoia F, Neri I. Terra firma-forme dermatosis. Clin Dermatol. 2021;39:202–5. doi: 10.1016/j.clindermatol.2020.10.019. [DOI] [PubMed] [Google Scholar]
- 20.Moon J, Kim M, Park JS, Lee J, Mun JH. Terra firma-forme dermatosis developed after thyroidectomy: Clinical and dermoscopic features. Ann Dermatol. 2018;30:499–501. doi: 10.5021/ad.2018.30.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han YJ, Kim SY, Choi HY, Myung KB, Choi YW. A case of dermatitis neglecta. Ann Dermatol. 2008;20:257–9. doi: 10.5021/ad.2008.20.4.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lucas JL, Brodell RT, Feldman SR. Dermatosis neglecta: A series of case reports and review of other dirty-appearing dermatoses. Dermatol Online J. 2006;12:5. [PubMed] [Google Scholar]
- 23.Schwartz RA. Acanthosis nigricans. J Am Acad Dermatol. 1994;31:1–19. doi: 10.1016/s0190-9622(94)70128-8. [DOI] [PubMed] [Google Scholar]
- 24.Davidson MB. Clinical implications of insulin resistance syndromes. Am J Med. 1995;99:420–6. doi: 10.1016/s0002-9343(99)80191-0. [DOI] [PubMed] [Google Scholar]
- 25.Roberts SO, Lachapelle JM. Confluent and reticulate papillomatosis (Gougerot-Carteaud) and pityrosporum orbiculare. Br J Dermatol. 1969;81:841–5. doi: 10.1111/j.1365-2133.1969.tb15954.x. [DOI] [PubMed] [Google Scholar]
- 26.Aslan NÇ, Güler Ş, Demirci K, Isiyel E. Features of terra firma-forme dermatosis. Ann Fam Med. 2018;16:52–4. doi: 10.1370/afm.2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chun SW, Lee SY, Kim JB, Choi HM, Ro BI, Cho HK. A case of terra firma-forme dermatosis treated with salicylic acid alcohol peeling. Ann Dermatol. 2017;29:83–5. doi: 10.5021/ad.2017.29.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panchal K, Bhalla N, Salunke P, Jerajani H. Extensive terra firma forme dermatosis [TFFD]: A rare presentation. Indian Dermatol Online J. 2015;6:458–9. doi: 10.4103/2229-5178.169742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naveen KN, Hegde S, Sharatchandra B. Terra firma-forme dermatosis. J Pak Assoc Dermatol. 2015;25:52–4. [Google Scholar]
- 30.Verma SB, Ghosh K. A curious story of terra firma forme dermatosis in a patient of psoriasis: Documentation by camera, dermatoscope, and microscope. Dermatol Ther. 2021;34:e14523. doi: 10.1111/dth.14523. [DOI] [PubMed] [Google Scholar]
- 31.Saha A, Malakar R, Baherjee R, Dhar S. Terra firma-forme dermatosis following episode of irritant contact dermatitis. Indian J Paediatr Dermatol. 2020;21:241–2. [Google Scholar]


