Abstract
Linear and whorled nevoid hypermelanosis is a rare skin pigmentation disorder, characterized by linear streaks and whorls of hyperpigmented macules along Blaschko’s lines. Lesions are commonly restricted to the trunk, neck, and extremities, sparing the face, palms, soles, and mucosae. Associated with this, certain cardiovascular, musculoskeletal, neurological, and developmental anomalies have been reported in the literature. Herein, we present a rare case of linear and whorled nevoid hypermelanosis involving the face, with musculoskeletal, genital, aural, and ocular abnormalities.
Keywords: Blaschko’s lines, linear and whorled nevoid hypermelanosis, pigmentation disorders
Introduction
Linear and whorled nevoid hypermelanosis (LWNH), also known as zosteriform hyperpigmentation, zosteriform lentiginous nevus, reticulate-pigmentation of Iijima and zebra-like pigmentation is an uncommon sporadic pigmentary disorder.[1] It manifests as swirls and streaks of hyperpigmentation along the lines of Blaschko, usually over the trunk and extremities. Lesions begin as hyperpigmented macules, without any preceding inflammation or palpable lesion, within the first 2 years of life. Rarely it may be associated with depigmentation and certain developmental anomalies such as microcephaly, arhinencephaly, ventricular septal defects, tetralogy of Fallot, deafness, brachydactyly, and facial and body asymmetry.[2,3] We present an uncommon case of LWNH with facial involvement, associated with skeletal, genital, aural, and ocular abnormalities, probably the first reported case with these associations.
Case Report
A 21-year-old girl presented to our outpatient department with complaints of asymptomatic dark skin lesions over the body since birth. According to the patient’s mother, the lesions initially began over the trunk and eventually progressed to involve both upper limbs, lower limbs, neck, face, and back within the next 2 years. The lesions darkened with age and the condition stabilized after 10 years of age without the appearance of new lesions. No history of erythema or vesiculobullous or warty lesions was present prior to the onset of these pigmented lesions. There was no history suggestive of any recurrent lower respiratory infections or involvement of the cardiovascular, central nervous system, developmental delay, or ocular abnormalities. Further medical history revealed skeletal deformities since birth, deafness in the right ear since 9 years of age, and primary amenorrhea. She presented a documented medical record of chromosome analysis of peripheral blood lymphocytes, done in 2019, in view of primary amenorrhea which was found to be normal. There was no history of consanguinity or recurrent fetal deaths or similar skin lesions in the family.
Systemic examination was unremarkable except for the musculoskeletal system which revealed scoliosis, short stature, syndactyly, brachydactyly of toes, sandal gap deformity of left foot; swan neck deformity of fingers [Figures 1a, 2a, and b]. There were no dental anomalies. Secondary sexual characters were well developed. Dermatological examination revealed multiple bilaterally symmetrical whorls of hyperpigmented macules along the lines of Blaschko over the chest, abdomen, and back. Similar skin lesions were arranged linearly over the face, neck, bilateral upper limbs, and lower limbs along the Blaschko’s lines [Figures 1a-c, and 3]. Ocular examination revealed left eye macular degeneration and audiometry revealed unilateral (right) sensorineural hearing loss.
Figure 1.
(a) Scoliosis and whorled pattern of hyperpigmentation on the back (b) Linear pattern of pigmentation over the lowerlimbs (c) Linear hyperpigmented lesions along blaschko’s lines over abdomen
Figure 2.

(a) Brachydactyly of 3rd, 4th, 5th toes of bilateral feet and incomplete syndactyly of 2nd and 3rd toes of bilateral feet and sandle gap deformity between 1st and 2nd toes in the left foot (b) Swan neck deformity of the distal interphalangeal joints of 2nd, 3rd, 4th, 5th fingers in the right hand and in 3rd, 4th, 5th distal interphalangeal joints of left hand
Figure 3.

Streaks of hyperpigmented lesions along blaschko’s lines over the face
Routine blood investigations, ECG (electrocardiogram), and 2D ECHO (Echocardiography) were normal. Ultrasound abdomen revealed bilateral small ovaries and uterine hypoplasia. Histopathological evaluation of the skin lesion revealed increased melanin in the basal layer [Figure 4]. There was no pigmentary incontinence. Clinico-pathological evaluation of the patient pointed towards the diagnosis of LWNH. Reassurance was given to the patient in view of the benign nature of the skin disease. However, as the face was also involved, chemical peeling and/or laser therapy were suggested to the patient for cosmetic improvement. Also, periodic follow up at ophthalmology, gynecology, otorhinolaryngology, dermatology, and orthopedics clinics were advised. However, the patient was lost to follow-up.
Figure 4.
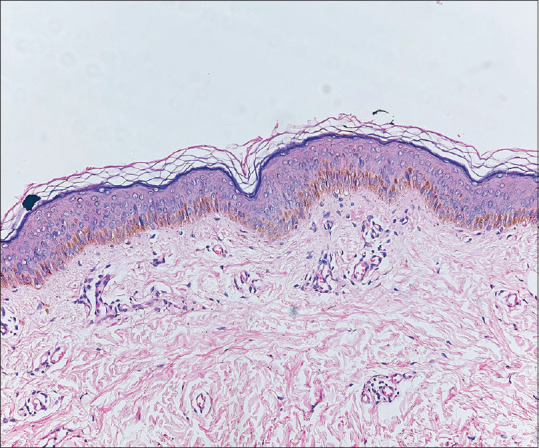
Increased melanin in basal layer (H&E, 10x)
Discussion
Pigmentary mosaicism describes the varied pigmentation patterns of the skin due to genetic heterogeneity of the skin cells.[4] It has been classified into genomic mosaicism (when there is post-zygotic somatic or germline mutation, leading to a genetically different clones of cells) and epigenetic mosaicism (when there is an epigenetic mutation). Clinically seven patterns have been described based on the presentation,[4]
Type 1a: Narrow bands
Type 1b: Broadbands
Type 2: The checkerboard pattern
Type 3: Phylloid pattern
Type 4: Patchy pattern without midline separation
Type 5: Lateralization pattern
Type 6: Sash-like pattern.
Linear and whorled nevoid hypermelanosis, a rare disorder of cutaneous pigmentary mosaicism was first described by Kalter et al. in 1988.[2] It is characterized by linear and whorled hyperpigmented streaks along the Blaschko lines. The onset of the disease is usually within the first two years of life; however, a late-onset form has also been described.[5] There is sparing of face, palms, soles, and mucosae in LWNH, but our case had an unusal presentation, with hyperpigmented linear streaks over the face following the Blaschko lines.
LWNH is majorly sporadic in occurrence, few familial cases have however been reported.[6] The exact cause of LWNH is not fully understood, but in a few cases, somatic mosaicism (mosaic trisomy of 7, 14, 18, 20; X-chromosomal mosaicism) was considered to be the cause.[6] Cytogenetic analysis of the peripheral blood lymphocytes or dermal fibroblasts from the affected skin may reveal abnormal mosaic karyotypes in a few patients.[4] Exome genome sequencing can be an alternative investigation in cases of pigmentary mosaicism.[4]
Chromosome analysis of peripheral blood lymphocytes in our patient did not reveal any chromosomal aberrations or mosaicisms. This could probably be due to a small point mutation or any epigenetic mutations that could have gone undetected in this routine chromosome analysis test. Further investigations like chromosome microarray analysis and exome genome sequencing of the lymphocytes, fibroblasts, and keratinocytes may reveal the cause of this mosaic state.[4]
Extracutaneous features like skeletal anomalies (facial and body asymmetry, brachydactyly), cardiovascular diseases (ventral septal defect, tetralogy of Fallot), and central nervous system diseases (microcephaly, mental retardation, epilepsy), deafness can be associated with LWNH.[1,4,5,6] Our patient had scoliosis and swan neck deformity of fingers, genital abnormalities like small ovaries, uterine hypoplasia, ocular abnormalities like left eye macular degeneration in addition to the brachydactyly of toes, and deafness which were the new associations seen in this case. One case of LWNH with genital abnormalities (female-type external genitalia with dysgenic testes and mildly atrophic uterus) due to chromosomal mosaicisms has been reported previously in a young girl by Kubota et al.[7] Another case report of LWNH associated with scoliosis, pigmentation also involving the face and genital region in a 20-year-old male has been described in 2007 by Yuksek et al.[1]
Histology of LWNH shows increased pigmentation in the basal layer and prominence or vacuolization of melanocytes.[3] Pigmentary incontinence is usually absent. Our case also had findings consistent with LWNH. A differential diagnosis of the hyperpigmented stage of incontinentia pigmenti (IP) and progressive cribriform zosteriform hyperpigmentation (PCZH) can be considered[3,8] [Table 1]. The absence of the sequential appearance of the vesicular, verrucous stages prior to the hyperpigmented stage, other extracutaneous features and basal cell degeneration, eosinophilia, and pigment incontinence on histology rules out the possibility of IP in this case, and the presence of disseminated skin lesions with associated extracutaneous features in the current case rules out PCZH.[3,6]
Table 1.
Differences between LWNH, incontinentia pigmenti and progressive cribriform zosteriform hypermelanosis (PCZH)
| LWNH | Incontinentia pigmenti | PCZH | |
|---|---|---|---|
| Genetic causes | Chromosomal mosaicism, (mosaic trisomy of 7, 14, 18, 20; X-chromosomal mosaicism) may be the causative factor | Caused due to mutation in a gene called NEMO, located on chromosome Xq28 | Somatic mosaicism is considered as the cause of PCZH |
| Age of onset | Usually at birth or within first two years of birth | At birth or within first few weeks after birth | At birth with gradual extension of lesions or most commonly in the second decade |
| Cutaneous features | Characterized by linear and whorled hyperpigmented streaks along Blaschko lines; usually more generalized | Cutaneous manifestations in IP sequentially appear as vesicular, verrucous, whorls or streaks of hyperpigmented and hypopigmented/ atrophic stages or there may be overlapping of stages | Presents as localized uniformly tan cribriform macular pigmentation in zosteriform distribution |
| Extracutaneous features | Has various associated skeletal, cardiovascular, CNS, ocular and aural abnormalities | Multisystem disorder, most commonly with dental anomalies (hypodontia, peg shaped teeth, delayed eruption), CNS, skeletal and ocular abnormalities | Absence of other associated cutaneous or systemic abnormalities |
| Dermoscopy | Parallel arrangement of curved and circular brownish streaks | Bluish – grey dots | Net like brown pigmentation with finger print like structures or rosettes |
| Histology | Increase in basal layer pigmentation, elongation of rete ridges in few cases | Necrotic keratinocytes; pigment incontinence can be seen. | Increase in basal layer melanin, absence of nevus cells; dermal melanophages and interface dermatitis may be seen in few cases |
LWNH = Linear and whorled nevoid hypermelanosis, IP = Incontinentia pigmenti, PCZH = Progressive cribriform and zosteriform hyperpigmentation, NEMO = Nuclear factor kappa B essential modulator, CNS = Central nervous system
Table 1 shows differences between LWNH, incontinentia pigmenti, and progressive cribriform zosteriform hyperpigmentation.[3,8,9]
Assessment of a patient with pigmentary mosaicism has to be done with a thorough prenatal, birth, developmental, and family history and a proper physical, cutaneous and systemic examination.[4] A multidisciplinary approach has to be followed in patients with cutaneous mosaicism, for the possibility of involvement of other extracutaneous systems. Successful management of skin lesions in these cases is rare, however, laser therapies may offer considerable pigment reduction in a few patients. Genetic counseling has to be advised to the patient.
Treatment options in LWNH include lasers (532 nm QS Nd YAG (Q-Switched Neodymium-doped Yttrium Aluminium Garnet) laser, 755 nm QS alexandrite laser, QS 694 nm ruby laser), chemical peels, depigmenting creams, and cosmetic camouflage. Among these, 694 nm QS ruby laser and 532 nm QS Nd-YAG laser have shown some promising results in LWNH patients as per previous case reports.[10]
Conclusion
LWNH itself being a rare pigmentary skin disorder, with involvement of the face, associated skeletal, ocular, aural, and genital abnormalities, and normal chromosomal analysis of peripheral blood lymphocytes make this an interesting case report and to the best of our knowledge, this is most probably the first case report of LWNH with these associations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Authors have declared it to be self-funded.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I would like to acknowledge the contribution made by Dr. Nithin Diwagar, Assistant professor, Department of Pathology, Saveetha medical college and hospital by providing the histopathology picture of this case.
References
- 1.Yuksek J, Sezer E, Erbil AH, Arca E, Taştan HB, Kurumlu Z, et al. Linear and whorled nevoid hypermelanosis. Dermatol Online J. 2007;13:23. [PubMed] [Google Scholar]
- 2.Kalter DC, Griffiths WA, Atherton DJ. Linear and whorled nevoid hypermelanosis. J Am Acad Dermatol. 1988;19:1037–44. doi: 10.1016/s0190-9622(88)70269-8. [DOI] [PubMed] [Google Scholar]
- 3.Sinha P, Chatterjee M, Singh KK, Sood A. Linear and whorled nevoid hypermelanosis with depigmentation. Indian Dermatol Online J. 2017;8:131–3. doi: 10.4103/2229-5178.202274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kromann AB, Ousager LB, Ali IKM, Aydemir N, Bygum A. Pigmentary mosaicism: A review of original literature and recommendations for future handling. Orphanet J Rare Dis. 2018;13:39. doi: 10.1186/s13023-018-0778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandes C, Waddell A, Jean SÉ. Linear and whorled nevoid hypermelanosis and Joubert syndrome: A novel association: A case report and literature review. SAGE Open Med Case Rep. 2019;7 doi: 10.1177/2050313X19876725. 2050313X19876725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saleh J, Vasicek B, Reserva J, Lake E, Speiser J. Linear and whorled nevoid hypermelanosis: A rare case report. Dermatol Case Rep. 2019;4:148. [Google Scholar]
- 7.Kubota Y, Shimura Y, Shimada S, Tamaki K, Amamiya S. Linear and whorled nevoid hypermelanosis in a child with chromosomal mosaicism. Int J Dermatol. 1992;31:345–7. doi: 10.1111/j.1365-4362.1992.tb03953.x. [DOI] [PubMed] [Google Scholar]
- 8.Gutte RM. Progressive cribriform and zosteriform hyperpigmentation. Indian Dermatol Online J. 2014;5:38–40. doi: 10.4103/2229-5178.126027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahuja R, Mustari AP, Bhari N. Hyperpigmented stage of incontinentia pigmenti. Indian Dermatology Online J. 2020;12:371–3. doi: 10.4103/idoj.IDOJ_628_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi Z, Duan X, Jiang M, Zhang C, Xiang L. Treatment of linear and whorled nevoid hypermelanosis using QS 694-nm ruby laser. J Cosmet Laser Ther. 2022;24:56–9. doi: 10.1080/14764172.2022.2066135. [DOI] [PubMed] [Google Scholar]



