Dear Editor,
Pyoderma gangrenosum (PG), a rapidly progressing, non-infectious, neutrophilic disorder is associated in about 70% of cases with conditions such as inflammatory bowel disease (64%), rheumatoid and inflammatory arthritides (16%), hematological/visceral malignancies (11%), and intake of drugs. Diagnosis is clinical; dense neutrophilic dermal infiltrate histopathologically may exclude differentials and be corroborative.
COVID-19 infection can develop cutaneous manifestations such as pseudochilblains, vesicular, urticarial, maculopapular exanthemata, livedo reticularis, and necrosis. Covishield[R] vaccination (ChAdOx1 nCoV-19, recombinant, replication-deficient chimpanzee adenovirus vector vaccine encoding SARS-CoV-2 Spike (S) glycoprotein manufactured by Serum Institute of India) entails two 0.5 ml intramuscular injections, 14-16 weeks apart, each containing 5 × 1010 virus particles.[1] It is followed often by a delayed large local reaction and sometimes by injection site reactions, urticarial/morbilliform eruptions, chilblains, erythromelalgia, pityriasis rosea-like reactions, herpes zoster, flares of herpes simplex, erythema multiforme, etc.[2]
Case summaries [Table 1], clinical [Figure 1], and histopathological [Figure 2] photographs illustrative of the three patients of PG involving the female breast are presented. We discuss the overlapping inflammatory cytokine profile linking the COVID-19 infection/its vaccination with PG and also the salient features of the cases of PG involving breast reported hitherto.
Table 1.
Case summaries
| Case 1 [Figure 1: a-b] | Case 2 [Figure 1: c-d] | Case 3 [Figure 1: e-f] | |
|---|---|---|---|
| Age | 42 years | 37 years | 40 years |
| Comorbidities | _ | Pemphigus vulgaris since 8 Y (Body mass index—31.8 kg/m2) | Systemic lupus erythematosus since 5 months |
| Vaccination | Unvaccinated | Two doses | One dose |
| RT-PCR for COVID-19 | Positive | _ | _ |
| Presentation | Incision and drainage of “abscess” soon followed by rapidly enlarging, painful granulating ulcer of the left breast. | One painful ulcer over right breast, each a week after Covishield[R] injection | Painful ulcer right breast, a fortnight after single injection of Covishield[R] |
| Laboratory | |||
| TLC/Neutrophils% | 3900/mm3/51% | 13200/mm3/74% | 11900/mm3/91% |
| ESR | 72 mm | 53 mm | 87 mm |
| CRP | 35 mg/dL | 15.5 mg/dL | 86 mg/dL |
| Urine protein | Trace | Nil | Trace |
| D-dimer | 4800 mg/L FEU | Normal | Normal |
| Dsg 3 | - | 108.1 RU/ml | - |
| ANA | - | - | 1:100 |
| dsDNA, U1-SnRNP, Ro 52/60 | - | - | + |
| Treatment | Parenteral>oral steroids×10 weeks Intra-lesional triamcinolone acetonide 10 mg/ml on ulcer edge Cyclosporine 200 mg OD×4 weeks. | Prednisolone 30 mg/day×5 weeks Oral dapsone 100 mg BD | IV methylprednisolone 250 mg OD×3 days IV cyclophosphamide 1/2 g fortnightly; six cycles Hydroxychloroquine 200 mg OD |
| Prognosis | Death following sepsis | Improved | Improved |
Figure 1.

Case 1 (a) on presentation and (b), on day 75; Case 2 (c) on presentation, white arrow indicate first and second ulcer and (d) after 35 days, Case 3 (e) on day 1, and (f) on day 60
Figure 2.
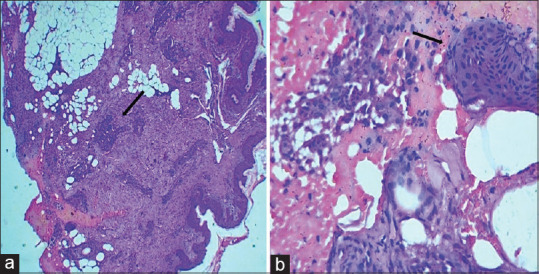
(a) Fibro-collagenous dermal stroma with adnexal structures and dense inflammatory infiltrate (Black arrow) (H & E stain, 10x); (b) Neutrophilic abscess and fibrin deposition (H and E Stain, 40x). Arrows indicate, a) dense inflammatory infiltrate and b) neutrophilic absces
Increased pro-inflammatory cytokines such as TNF-α, IL-1, IL-8, IL-12, IL-17, IL-23, and IL-6 are central to the pathogenesis of PG. COVID virus, too, causes cytokine storms releasing IL-1, IL-6, IL-8, IL-10, IL-12, TNF-α, and IFN-gamma. COVID vaccination triggers autoimmunity through molecular mimicry and hyperinflammation induced by adjuvants. Thus, the inflammatory cytokine profile of PG and COVID-19 disease/vaccination can be similar or may even overlap.[3] In pemphigus vulgaris, autoreactive T cells induce/maintain antidesmoglein-1 and antidesmoglein-3 autoantibodies. Serum levels of IFN-gamma are reduced and of IL-8, elevated, latter seen also in PG.[4] In systemic lupus erythematosus, genetic mutations, environmental factors, and gender predisposition generate proinflammatory milieu producing IFN-α, IL-6, and IL-10 causing activation of inflammasome and abnormal neutrophils.[5]
A review of English literature hitherto showed 150 reported cases of PG involving breast none in association with COVID-19 infection/vaccination. Preceding surgical intervention was reported in 70%, such pathergy followed incision and drainage of the probable breast abscess of our first case. Just one among the eight cases of PG reported after COVID-19 disease, and none of the 6 following its vaccination involved the breast. Systemic Lupus Erythematosus was reported in 23 cases and pemphigus vulgaris, in a single case. However, PG may have been independently associated with COVID-19 disease/vaccine and could have occurred probably, not conclusively, as a result of altered course of pre-existing autoimmune conditions. Still, cases vaccinated for COVID-19 as well as those with dysregulated immune status should have extended follow-up as a measure of abundant caution. Also, the occurrence of PG, even for sites other than those of vaccinations, should be monitored as induction of PG can augment potentially life-threatening COVID-19 disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Post ChAdOx1 nCoV-19 Corona Virus Vaccine Recombinant) (Covishield) Pulmonary thromboembolism with multiple intracranial ischemic infarcts. Neurol India. 2022;70:1287–8. doi: 10.4103/0028-3886.349719. [DOI] [PubMed] [Google Scholar]
- 2.Sarkar R, Vinay K, Bishnoi A, Poojary S, Gupta M, Kumaran MS, et al. A Delphi consensus on the nomenclature and diagnosis of lichen planus pigmentosus and related entities. Indian J Dermatol Venereol Leprol. 2023;89:41–6. doi: 10.25259/IJDVL_804_2021. [DOI] [PubMed] [Google Scholar]
- 3.Contractor A, Shivaprakash S, Tiwari A, Setia MS, Gianchandani T. Effectiveness of Covid-19 vaccines (CovishieldTM and Covaxin ®) in healthcare workers in Mumbai, India: A retrospective cohort analysis. PLoS One. 2022;17:e0276759. doi: 10.1371/journal.pone.0276759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SH, Hong WJ, Kim SC. Analysis of serum cytokine profile in pemphigus. Ann Dermatol. 2017;29:438–45. doi: 10.5021/ad.2017.29.4.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.González-Moreno J, Ruíz-Ruigomez M, Callejas Rubio JL, Ríos Fernández R, Ortego Centeno N. Pyoderma gangrenosum and systemic lupus erythematosus: A report of five cases and review of the literature. Lupus. 2015;24:130–7. doi: 10.1177/0961203314550227. [DOI] [PubMed] [Google Scholar]


