Abstract
Objectives
Many orbital fracture patients are transferred to tertiary care centers for immediate ophthalmology consultation, though few require urgent ophthalmic evaluation or intervention. This overutilizes limited resources and overburdens patients and the health care system with travel and emergency department (ED) expenses. A simple, easy-to-use, clinical decision-making tool is needed to aid local EDs and triage services in effectively identifying orbital fracture patients who need urgent ophthalmic evaluation.
Design
Single center, retrospective cohort study.
Subjects
Orbital fracture patients aged ≥ 18 years who presented to the study institution’s emergency department and received an ophthalmology consultation.
Methods
Ocular injuries that required close monitoring or an intervention within the first few hours after presentation were termed urgent. Two Hawkeye Orbital Fracture Prioritization and Evaluation (HOPE) algorithms were developed to identify orbital fracture patients needing urgent evaluation; including 1 algorithm incorporating computerized tomography (CT) scans interpreted by ophthalmology (HOPE+CT). Algorithms were compared with 3 previously published protocols: the University of Texas Health Science Center at Houston (UTH), the South Texas Orbital Fracture Protocol (STOP), and Massachusetts Eye and Ear (MEE) algorithms.
Main Outcome Measures
Correct triage of patients with orbital fractures who have urgent ocular or orbital conditions.
Results
In the study institution’s ED, 134 adult patients (145 orbits) were seen with orbital fractures in 2019. Eighteen (13.4%) had ocular or orbital conditions categorized as urgent. The HOPE tool resulted in 100% sensitivity and 78.4% specificity. The HOPE+CT tool resulted in 100.0% sensitivity and 94.0% specificity. The UTH algorithm was 91.7% sensitive and 76.5% specific. South Texas Orbital Fracture Protocol and MEE were both 100% sensitive but only 35.1% and 32.8% specific, respectively.
Conclusions
The HOPE and HOPE+CT algorithms were superior or equal to the UTH, STOP, and MEE algorithms in terms of specificity while detecting all urgent cases. Implementation of a triage protocol that uses the HOPE or HOPE+CT algorithms could improve resource utilization and reduce health care costs through identification of orbital fracture patients needing urgent evaluation. An online tool that deploys the HOPE+CT algorithm in a user-friendly interface has been developed and is undergoing prospective validation before public dissemination.
Financial Disclosure(s)
Proprietary or commercial disclosure may be found in the Footnotes and Disclosures at the end of this article.
Keywords: Orbital fracture, Trauma, Ocular injury
Hawkeye Orbital Fracture Prioritization and Evaluation tools identify orbital fracture patients at risk of significant ocular injury with improved efficacy compared with published studies, offering a quick, simple clinical tool to triage patients.
Ophthalmic conditions account for nearly 2 million emergency department (ED) visits each year in the United States, with eye injuries comprising approximately 36.3% of these visits.1 Orbital fractures are one of the most common diagnoses in patients presenting to the ED with ocular trauma.2,3 Common mechanisms of injury resulting in orbital fractures include assault, motor vehicle accidents, and falls.4, 5, 6 Despite the potential for orbital fractures to cause ocular injury, only 12% to 19% require immediate evaluation and intervention for conditions that include orbital compartment syndrome (OCS), open globe injury, and extraocular muscle entrapment.7, 8, 9, 10, 11
Due to the concern for these injuries, many patients with orbital fractures are sent urgently to hospitals with consulting ophthalmology services. To reduce the number of unnecessary urgent transfers, several studies have attempted to identify examination findings and risk factors associated with significant ocular or periocular injury in patients with orbital fractures.7,9, 10, 11, 12, 13, 14, 15, 16 However, proposed algorithms have low specificity,7 involve unreliable or burdensome subjective and objective methods of testing,8, 9, 10 and/or are not routinely used in clinical practice.7, 8, 9, 10
Therefore, there is significant need for the development of a clinically useful algorithm that is efficient and simple with high sensitivity and specificity in identifying orbital fractures that result in ophthalmic injury requiring urgent evaluation. In this way, the algorithm can be implemented as a tool to triage patients with orbital fractures and reduce the burden on patients and the health care system of unneeded urgent transfers and/or urgent ophthalmology consults. Based on these goals, we conducted a retrospective review of patients with orbital fractures presenting to this institution’s ED to optimize an orbital fracture algorithm for referral of ophthalmic emergencies, termed the Hawkeye Orbital Fracture Prioritization and Evaluation (HOPE) algorithm.
Methods
A retrospective review was performed evaluating patients with orbital fractures who were seen in the University of Iowa Hospitals and Clinics ED, a level I trauma center, between January 1, 2019, and December 31, 2019. The University of Iowa Hospitals and Clinics institutional review board approval was obtained for this study and it adhered to the tenets of the Declaration of Helsinki. Due to the retrospective nature of the study, informed consent was not collected from all participants. However, every effort was made to maintain patient confidentiality throughout the research process.
Patient Identification Protocol/Inclusion/Exclusion
A search query of medical records in the Epic electronic health records system was performed to identify patients who received an ophthalmology consultation and were seen in the institution’s ED in 2019. Individual charts of the identified patients were reviewed to identify patients examined and diagnosed with an orbital fracture by radiologist interpretation of computerized tomography (CT) scans. All patients without the diagnosis of orbital fracture and those who were aged < 18 years were excluded from the study. Only the first ED visit was analyzed when patients had repeat ED visits for the same injuries.
Data Extraction
Individual outside hospital (OSH) ED notes and ED and ophthalmology notes from the University of Iowa were reviewed for data extraction. For each patient included in the study, demographic factors including date of consultation, age, gender, and mechanism of injury were documented. Subjective examination findings of presence of binocular diplopia and perceived change in vision were recorded for each patient. Additionally, objective examination findings were recorded, including visual acuity, presence of a relative afferent pupillary defect, ocular motility deficits, presence of subconjunctival heme or chemosis, and presence or type of ocular injury. Computerized tomography imaging was obtained for all patients and fracture patterns were categorized as follows: floor, medial, lateral (including zygomaticomaxillary complex fractures), and/or roof fractures. Radiologists’ CT interpretations as well as ophthalmologists’ interpretations of the CT scans were reviewed for notation of open globe, retrobulbar hemorrhage, and/or signs of extraocular muscle entrapment. Ophthalmologists included ophthalmology residents who had undergone orbital fracture interpretation training with an oculoplastic specialist; a publicly available tutorial on how to identify and assess orbital fractures is currently being developed and will be hosted on EyeRounds.org. Whether or not patients required surgical fracture repair was also documented. Patients were classified as requiring urgent ophthalmology evaluation if they potentially needed an immediate ophthalmic intervention, which included OCS, retrobulbar hemorrhage and/or significant hemorrhage within the orbital compartment, open globe injury, major corneal trauma, or extraocular muscle entrapment.
Patients who arrived directly at or were transferred to the study institution’s ED from an OSH had the mode of transportation recorded when available. The distance traveled by patients from the scene to the OSH(s) and from the OSH(s) to the study institution was calculated.
Algorithm Development and Application
Bayesian Information Criterion and Akaike Information Criterion model selection for logistic regression were used to identify variables predictive of patients with orbital fractures that required urgent ophthalmic evaluation using the stats and StepReg packages in R (open-source software available at http://www.r-project.org). Imputation of missing data was conducted using multivariate chained equations with the mice package in R. Once the models were determined, prediction and threshold testing were carried out to optimize sensitivity and specificity values of the algorithms, with an emphasis on sensitivity to not miss any urgent cases.
Comparison to Existing Orbital Fracture Triage Protocols
Algorithms developed in this study were compared with the screening tools for detecting and triaging ocular injuries developed at the Memorial Hermann Hospital–Texas Medical Center ED that is affiliated with The University of Texas Health Science Center at Houston (UTH),9 the South Texas Orbital Fracture Protocol (STOP),8 and the bedside orbital fracture algorithm developed at Massachusetts Eye and Ear (MEE; Table S1, available at www.ophthalmologyscience.org).7 The UTH, STOP, and MEE algorithms were retrospectively applied to assign patients in this study’s cohort to either be seen by ophthalmology in the ED or within a few hours of admission (urgent) or for a dilated ophthalmology examination within 48 hours (nonurgent).
Distance Traveled Assessment
To determine the total miles traveled by each patient, patient starting location and locations of all hospitals visited as part of the orbital fracture evaluation were geocoded into latitude and longitude coordinates using ggmap in R. The optimal driving distance between locations was determined using gmapsdistance and measurements packages in R, which utilizes Google’s Geocoding API to geocode locations. A geospatial map of the distance traveled and number of hospitals visited for the study population was generated using Kepler.gl.
Data Analysis
Descriptive statistics were performed using Excel statistical software (Microsoft Corporation) and R. Patients with bilateral fractures were counted as an individual patient demographically. For comparison of triage protocols, sensitivities, specificities, positive predictive values, and negative predictive values were calculated for the previously published algorithms and the HOPE algorithms.
Results
A total of 917 patients received an ophthalmology consultation and evaluation in the study institution’s ED in 2019. Of these, 134 adult patients with 145 orbital fractures were identified for inclusion in the final analysis. The average age of these patients was 49.9 years (standard deviation [SD] = 21.6). There were 99 males with orbital fractures and 35 females. The most frequent mechanisms of injury for each orbital fracture patient were falls or “found down” (39.6%), assault (27.6%), motor vehicle or bicycle accident (20.9%), object versus eye (9.7%), projectile injury (1.5%), and seizure (0.7%; Table 2).
Table 2.
Demographic Information of Patients with Orbital Fracture(s)
| Male patients (%) | 99 (73.9) |
| Female patients (%) | 35 (26.1) |
| Age (yrs), mean (SD) | 49.9 (21.6) |
| Mechanism of injury | |
| Fall or found down (%) | 53 (39.6) |
| Assault (%) | 37 (27.6) |
| Motor vehicle or bicycle crash (%) | 28 (20.9) |
| Object vs. eye (%) | 13 (9.7) |
| Projectile injury (%) | 2 (1.5) |
| Seizure (%) | 1 (0.7) |
n = 134.
SD = standard deviation.
Patients with Injury Requiring Urgent Ophthalmic Evaluation
Eighteen orbital fracture patients (13.4%) were identified to have ocular or orbital conditions considered to require urgent evaluation. Of these, 7 patients had OCS requiring canthotomy and cantholysis, 4 patients had retrobulbar hemorrhage or significant hemorrhage within the orbit that required close intraocular pressure monitoring, 4 patients had open globe injuries, 2 patients had extraocular muscle entrapment, and 1 patient had a corneal thermal injury. Patients with open globe injuries or extraocular muscle entrapment all underwent surgical repair. No patients with bilateral orbital fractures were found to have conditions requiring urgent evaluation by an ophthalmologist (Table 3).
Table 3.
Urgent Ophthalmic Conditions Observed in Patients with Orbital Fracture(s)
| Diagnosis | Patients with Fractured Orbits (%) |
|---|---|
| Orbital compartment syndrome | 7 (5.2) |
| Open globe | 4 (3.0) |
| Retrobulbar or significant orbital hemorrhage | 4 (3.0) |
| Extraocular muscle entrapment | 2 (1.5) |
| Corneal thermal injury | 1 (0.7) |
| Total | 18 (13.4) |
n = 134.
Building and Testing the HOPE Algorithms
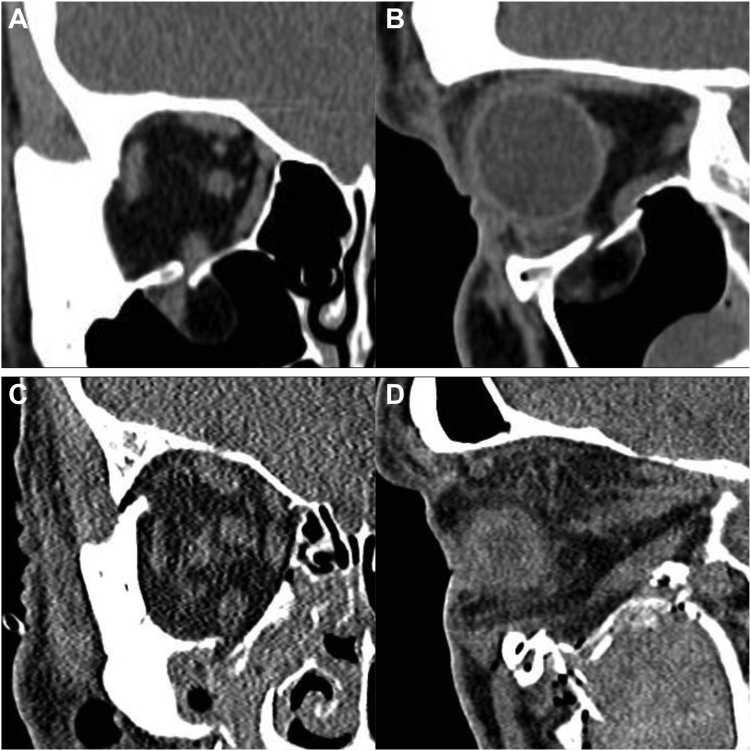
When analyzing all subjective and objective examination findings for the 134 patients, 2 different algorithms were developed to identify orbital fracture patients requiring urgent evaluation: the HOPE algorithm that included 11 variables (Table 4A) and the HOPE+CT algorithm with 6 variables, including CT scan interpretation by ophthalmology (Table 4B). The stepwise logistic regression analysis excluded radiologist interpretation of entrapment in favor of ophthalmology interpretation in the HOPE+CT algorithm because ophthalmology interpretation detected both entrapment cases with 4 false positives whereas radiology interpretation missed 1 of 2 entrapment cases with 23 false positives (Fig 1; Fig S2, available at www.ophthalmologyscience.org).
Table 4.
HOPE Algorithm (Top) and HOPE+CT (Bottom)
| HOPE∗ | Coefficient | Standard Error | Z Value | P (Z) |
|---|---|---|---|---|
| (Intercept) | −6.85 | 3.19 | −2.15 | 0.03 |
| Relative afferent pupillary defect | 25.23 | 2730.20 | 0.01 | 0.99 |
| Subconjunctival hemorrhage | 4.65 | 1.83 | 2.55 | 0.01 |
| Visual acuity† | 2.39 | 0.80 | 3.01 | 0.00 |
| Foreign body injury | 8.16 | 3.14 | 2.60 | 0.01 |
| Motility deficit | 3.12 | 1.58 | 1.98 | 0.05 |
| Medial wall fracture | 4.95 | 1.80 | 2.76 | 0.01 |
| Age | −0.12 | 0.05 | −2.30 | 0.02 |
| Number of fractured orbital walls | −2.16 | 1.14 | −1.90 | 0.06 |
| Gender | 3.14 | 1.69 | 1.85 | 0.06 |
| Eyelid laceration | 3.46 | 1.99 | 1.82 | 0.07 |
| Mechanism of injury‡ | −1.08 | 0.77 | −1.40 | 0.16 |
| Y' = −6.85 + 25.23(RAPD) + 4.65(SCH) + 2.39(VA)† + 8.16(FB) + 3.12(MD) + 4.95(MWF) – 0.12(Age) – 2.16(W) + 3.14(G) + 3.46(EL) – 1.08(MOI)‡ | ||||
| HOPE+CT∗ | Coefficient | Standard Error | Z Value | P value (Z) |
|---|---|---|---|---|
| (Intercept) | −39.21 | 8042.25 | −0.01 | 1.00 |
| Retrobulbar hemorrhage | 98.34 | 15 966.68 | 0.01 | 1.00 |
| Ability to count fingers at 3 feet | −77.63 | 13 411.37 | −0.01 | 1.00 |
| Extraocular muscle entrapment | 95.70 | 15 966.68 | 0.01 | 1.00 |
| Foreign body injury | 58.14 | 11 234.42 | 0.01 | 1.00 |
| Subconjunctival hemorrhage | 39.90 | 8042.25 | 0.01 | 1.00 |
| Orbital floor fracture | −20.15 | 5002.35 | −0.00 | 1.00 |
| Y' = −39.21 + 98.34(RBH) − 77.63(CF) + 95.70(EME) + 58.14(FB) + 39.90(SCH) − 20.15(FF) | ||||
CF = ability to count fingers at 3 feet; EL = eyelid laceration; EME = extraocular muscle entrapment; FB = foreign body injury; FF = orbital floor fracture; G = gender; HOPE = Hawkeye Orbital Fracture Prioritization and Evaluation; HOPE+CT = Hawkeye Orbital Fracture Prioritization and Evaluation with Computed Tomography interpretation by ophthalmology; MD = motility deficit; MOI = mechanism of injury; MWF = medial wall fracture; RAPD = relative afferent papillary defect; RBH = retrobulbar hemorrhage; SCH = subconjunctival hemorrhage; VA = visual acuity; W = number of fractured orbital walls.
All variables are input as either “1” (yes/present/male gender) or “0” (no/not present/female gender) unless otherwise stated below.
VA: 0 =20/20 or better; 1 = 20/25 to 20/40; 2 = 20/50 to 20/125; 3 = 20/200 to count fingers at 3’; 4 = count fingers at 1 to 2’ or worse; 5 = unable.
0 = fall or “found down;” 1 = assault; 2 = motor vehicle or bicycle accident; 3 = object vs. eye; 4 = projectile injury; 5 = seizure.
Figure 1.
Maxillofacial computerized tomography (CT) of 2 patients with orbital fractures. Patient with a right orbital floor fracture with clinical evidence of entrapment where both ophthalmology and radiology interpretations were concerned for entrapment (A, B). Patient with a left orbital floor fracture without entrapment where radiology CT interpretation noted concern for inferior rectus muscle entrapment but ophthalmology interpretation did not (C, D).
The HOPE algorithm resulted in a sensitivity of 100.0% and specificity of 78.4% for identifying patients needing urgent ophthalmic evaluation. No patients with urgent conditions were missed (Table 5), but 25 false-positive patients were sent for urgent evaluation. Application of the HOPE+CT algorithm resulted in 100.0% sensitivity with an improved 94.0% specificity, identifying all patients with urgent conditions and 7 false positives (Table 5).
Table 5.
Comparison of HOPE Algorithm and HOPE+CT to Published Algorithms in Identifying Orbital Fracture Cases Needing Urgent Ophthalmic Evaluation
| Algorithm | Total Number of Patients | Patients Transferred (%) | Patients Referred for Outpatient (%) | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | Missed Patients with Urgent Diagnoses |
|---|---|---|---|---|---|---|---|---|
| UTH | 110∗ | 34 (30.9) | 76 (69.1) | 91.7% | 76.5% | 32.4% | 98.7% | 1 (orbital compartment syndrome) |
| STOP | 132† | 92 (69.7) | 40 (30.3) | 100.0% | 35.1% | 19.6% | 100.0% | 0 |
| MEE | 134 | 96 (71.6) | 38 (28.4) | 100.0% | 32.8% | 18.8% | 100.0% | 0 |
| HOPE | 134 | 43 (32.1) | 91 (67.9) | 100.0% | 78.4% | 41.9% | 100.0% | 0 |
| HOPE+CT | 134 | 25 (18.7) | 109 (81.3) | 100.0% | 94.0% | 72.0% | 100.0% | 0 |
HOPE = Hawkeye Orbital Fracture Prioritization and Evaluation; HOPE+CT = Hawkeye Orbital Fracture Prioritization and Evaluation with Computed Tomography interpretation by ophthalmology; MEE = Massachusetts Eye and Ear; STOP = South Texas Orbital Fracture Protocol; UTH = University of Texas Health Science Center at Houston.
Twenty-four patients were excluded when the UTH tool was applied because they lacked information on positive or negative findings of blurry vision, pain with eye movement, visual acuity of 20/40 or worse, or extraocular muscle motility restriction.
Two patients were excluded when the STOP tool was applied. In 1 patient no slit lamp examination was documented so the STOP could not be applied and another patient was unresponsive so subjective findings were unavailable and no other findings suggested urgent evaluation.
Comparison with the UTH, STOP, and MEE Algorithms
Retrospective application of the UTH9 algorithm could be applied to 110 of the 134 patients in this cohort due to the ED not documenting all components of the algorithm, in particular documentation of pain with or without ocular movement. Of these patients, the UTH tool identified 34/110 (30.9%) for urgent ophthalmic evaluation and 76/110 (69.1%) for outpatient follow-up evaluation, which resulted in 91.7% sensitivity and 76.5% specificity (Table 5). Retrospective application of the STOP8 algorithm identified 92/132 patients (69.7%) for urgent ophthalmic evaluation and 40/132 patients (30.3%) for outpatient follow-up evaluation, achieving 100% sensitivity at the cost of 35.1% specificity (Table 5). Two patients were excluded due to incomplete data for STOP algorithm assessment. The MEE7 algorithm identified 96/134 patients (71.6%) for urgent ophthalmic evaluation and 38/134 patients (28.4%) for nonurgent evaluation, attaining 100.0% sensitivity with a 32.8% specificity (Table 5).
Transfer and Admission Data
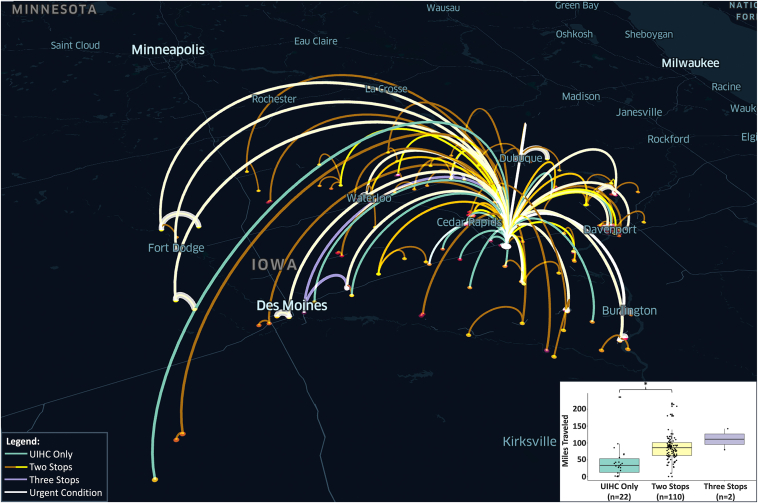
To determine the travel burden on the patient and health care system, total distance traveled, mode of transportation, and number of hospitals visited were calculated and determined for each individual patient (Table S6, available at www.ophthalmologyscience.org). The average distance traveled by all patients included in this study was 80 miles (SD = 43.5). Patients who presented directly to this institution’s ED traveled an average of 44 miles (SD = 50.8), patients who went to 1 OSH before this institution’s ED traveled an average of 87 miles (SD = 38.0), and patients who went to 2 OSHs before presentation at the study institution traveled an average of 111 miles (SD = 43.9). Visualization allowed for elucidation of several hot spot referral centers in Iowa (Fig 3).
Figure 3.
Geospatial mapping of distance traveled for all 134 patients presenting to the University of Iowa Hospitals and Clinics (UIHC) emergency department (ED) with orbital fractures in 2019. Mint green depicts patients who traveled directly to the UIHC ED. A gold-to-yellow gradient depicts patients who traveled to 1 outside hospital (OSH) before UIHC, with brighter yellow indicating multiple patients sharing the same travel path. Purple represents the travel paths of patients who went to 2 OSHs. The bottom right corner panel depicts the average distance traveled in miles by these 3 cohorts of patients. ∗ indicates P < 0.05.
Discussion
The HOPE and HOPE+CT algorithms were developed and successfully applied retrospectively to identify patients with urgent ophthalmic conditions secondary to orbital fractures with high sensitivity and improved specificity compared with existing algorithms.7, 8, 9 As observed in prior studies, the present study redemonstrates that most orbital fractures do not cause significant ocular or periorbital injury nor require urgent ophthalmic evaluation or intervention. However, the biggest risk of postponing a full ophthalmic examination is missing a critical diagnosis within the timeframe where permanent vision loss or diplopia could be avoided, which also poses medicolegal concerns. These risks need to be weighed against the health benefit and economic impact on individual patients and the hospital systems. Importantly, it is the policy at the University of Iowa that all orbital fracture patients, regardless of ocular risk profile, should have a dilated eye examination within 48 hours to ensure there are no intraocular injuries that need to be monitored or treated; all orbital fracture patients that are seen in local EDs are offered an outpatient follow-up appointment at the University of Iowa, if one is not available locally, and assuming there is not a need for urgent transfer for ophthalmic evaluation. Implementation of the HOPE and HOPE+CT algorithms at EDs and triage centers may significantly reduce the number of unnecessary urgent interhospital transfers and ophthalmology consultations for patients with orbital fractures while still identifying the patients requiring urgent intervention.
Further, for an orbital fracture algorithm to be used in a triage setting, it needs to be easily accessible and as simple as possible with both high sensitivity and specificity. Thus, the authors chose to focus on the HOPE+CT algorithm, which contains only 6 variables and had 100% sensitivity with the highest specificity of all the algorithms (94%). Of note, ophthalmology interpretation of CT scans is important, since ophthalmologists are clued into subtle radiologic findings present in cases of entrapment, as well as to help arrange outpatient follow-up. Each orbital fracture patient that may potentially be transferred to the University of Iowa for further assessment has their radiological imaging pushed to the electronic medical record system. This allows the “on call” ophthalmologist to have access to the outside scans when making a triage decision. Ideally, every hospital system should have a similar structure in place or alternatively allow for “on call” ophthalmology providers to have remote login to their systems to review these scans. However, in cases where this is not possible, the HOPE+CT algorithm cannot be used, offering the opportunity for systems level changes to improve the care of patients with orbital trauma.
Previously, 3 studies have developed algorithms to predict urgent conditions in patients with orbital fractures.7, 8, 9 The UTH tool was developed at Memorial Hermann Hospital–Texas Medical Center ED after retrospective evaluation of 512 patients who presented with orbital fractures to determine factors predictive of severe ocular injury.9 The STOP algorithm was developed by retrospectively evaluating 379 patients with orbital fractures who presented to the Brooke Army Medical Center’s ED, and the algorithm was created to identify patients with emergent ocular injuries and/or who require ophthalmic intervention, whether medical or surgical, including nonurgent procedures such as eyelid laceration repair.8 The MEE tool was developed through retrospective evaluation of 430 patients with orbital fractures presenting to either Massachusetts General ED or Brigham and Women’s ED. Their tool was made to identify patients at high risk for substantial ocular or orbital injury.7 When retrospectively applied to patients from the study institution, both the MEE and STOP algorithms identified all the urgent cases seen; however, they did so with low specificity and low positive predictive value. The UTH tool missed 1 urgent case with much higher specificity than MEE and STOP with the benefit of only requiring 4 findings in their tool, though 6 urgent cases were not able to be assessed using their algorithm. Markedly, HOPE and HOPE+CT achieved 100% sensitivity with higher specificity than all of the other algorithms, improving identification of which orbital fracture patients needed urgent transfer for ophthalmology consultation.
It is worth noting that the HOPE and HOPE+CT algorithms were developed for alert, responsive patients. In a trauma setting, ocular examination is a routine part of the secondary survey, including assessment for an open globe or chemical burn, as well as to assess pupillary response for evaluation of cortical function. During the survey, an inability to open the eyelids would raise suspicion and evaluation for OCS. However, in the acute emergency setting of an unresponsive patient, other medical issues take priority over the eye, including cortical function, breathing, and circulation. Hence, after ruling out ophthalmic emergencies as part of the normal trauma protocol, full ocular assessment can usually be postponed until the patient is stabilized.
In addition to evaluating orbital fracture triage protocols, this study examined geospatial mapping to understand regional and source-specific trends in the patients with orbital fractures seen at the University of Iowa, including identification of “hotspot” referral centers where a greater number of transferred patients originate. The average patient was seen at 1 outside hospital before transfer to the University of Iowa, typically traveling an average of 80 miles by ambulance. Though a full economic analysis and thorough evaluation of all available consultation services at referring hospitals is beyond the scope of this study, it is important to note that a 2021 study in Mississippi, where patients traveled a similar average of 76 miles to reach the study institution, estimated the average cost of ambulance travel and air ambulance travel were $784 and $15 585, respectively. Further, the same study estimated the average cost of each ED visit alone was $2763.75.17 In addition to patient and health care economic costs, overtransfer of patients with nonurgent conditions can create resource utilization dilemmas within the EDs where staffing and supply shortages already exist and can further strain resident workload and work hour restrictions. Of note, a 2019 study in Maryland suggested that outpatient ophthalmology appointments cost 37% less than ophthalmic care provided in the ED and do not require billable ED or hospital costs.18 Overall, it is clear that appropriate triage of patients with orbital fractures would reduce the financial burden of unnecessary ED visits and transport services for patients.
Limitations of this study include the small sample size and retrospective nature of the study. Identification of urgent cases was also dependent on the referring provider examination, such as in cases where high intraocular pressure may have been inaccurately measured at an outside institution and the patient received a canthotomy/cantholysis for possible OCS, though there was no radiological evidence. Additionally, a single institution study has inherent population biases with regional differences in transfer protocols and radiology reads, as well as proportions of high versus low acuity trauma, though these same limitations also exist in the published algorithms. The HOPE and HOPE+CT algorithms were not designed to identify all intraocular injuries and focused on those that potentially required urgent evaluation and intervention. As a result, conditions such as hyphema, traumatic iritis, and choroidal rupture, which some algorithms considered urgent, were not considered urgent in our analysis. These and other nonurgent conditions would be evaluated and treated as part of the outpatient dilated fundus examination within 48 hours of injury. It is important to note that these recommendations are at the discretion of the evaluating providers, and there may be certain situations where more immediate evaluation is indicated. Finally, it is important to note that timing of CT interpretations by ophthalmology occurred in a variable manner, occurring both before and after radiology interpretation and with and without knowledge of ocular examination findings.
Prospective validation of the HOPE+CT algorithm is currently underway at the study institution in collaboration with referring centers. An easily accessible, user-friendly online widget will be publicly available upon its validation (http://eyerounds.org/HOPE). The authors hope that the HOPE+CT algorithm will provide an efficient and simple clinical decision-making tool that clinicians can use to identify urgent ophthalmic conditions requiring immediate transfer.
Manuscript no. XOPS-D-23-00220R1.
Footnotes
Supplemental material available atwww.ophthalmologyscience.org.
Disclosure(s):
All authors have completed and submitted the ICMJE disclosures form.
The author(s) have made the following disclosure(s):
P.H.S.: Stock – Steris.
E.M.S.: Consultant –Horizon Therapeutics, Genentech; Advisory board – Horizon Therapeutics, Tarsus Pharmaceuticals.
K.D.C.: Consulting fees – Genentech; Travel support – ACGME; Leadership – ACGME.
C.P.: Stock or stock options – Edwards Life Sciences, Regeneron.
M.G.F.: Equity – OcuSciences, Inc.
The other authors have no proprietary or commercial interest in any materials discussed in this article.
Supported by an unrestricted grant from Research to Prevent Blindness to the University of Iowa Department of Ophthalmology and Visual Sciences.
HUMAN SUBJECTS: Human subjects were included in this study. The University of Iowa Hospitals and Clinics institutional review board approved this study and all research adhered to the tenets of the Declaration of Helsinki. Due to the retrospective nature of the study, informed consent was not collected from all participants. However, every effort was made to maintain patient confidentiality throughout the research process.
No animal subjects were used in this study.
Author Contributions:
Conception and design: Shriver, Diel, Field
Data collection: Sanchez, Strampe, Diel, Field
Analysis and interpretation: Sanchez, Shriver, Diel, Pham, Carter, Kemp, Field
Obtained funding: N/A
Overall responsibility: Sanchez, Shriver, Strampe, Diel, Pham, Carter, Kemp, Field
Supplementary Data
References
- 1.Channa R., Zafar S.N., Canner J.K., et al. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134:312–319. doi: 10.1001/jamaophthalmol.2015.5778. [DOI] [PubMed] [Google Scholar]
- 2.Scruggs D., Scruggs R., Stukenborg G., et al. Ocular injuries in trauma patients: an analysis of 28,340 trauma admissions in the 2003-2007 National Trauma Data Bank National Sample Program. J Trauma Acute Care Surg. 2012;73:1308–1312. doi: 10.1097/TA.0b013e31825c78d9. [DOI] [PubMed] [Google Scholar]
- 3.Iftikhar M., Latif A., Farid U.Z., et al. Changes in the incidence of eye trauma hospitalizations in the United States from 2001 through 2014. JAMA Ophthalmol. 2019;137:48–56. doi: 10.1001/jamaophthalmol.2018.4685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark T.J., Renner L.M., Sobel R.K., et al. Intimate partner violence: an underappreciated etiology of orbital floor fractures. Ophthal Plast Reconstr Surg. 2014;30:508–511. doi: 10.1097/IOP.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 5.Iftikhar M., Canner J.K., Hall L., et al. Characteristics of orbital floor fractures in the United States from 2006 to 2017. Ophthalmology. 2021;128:463–470. doi: 10.1016/j.ophtha.2020.06.065. [DOI] [PubMed] [Google Scholar]
- 6.Ray C.N., Marsh H.D., Gilmore J.E., et al. Review of 451 patients presenting with orbital wall fractures: a retrospective analysis. J Craniofac Surg. 2023;34:126–130. doi: 10.1097/SCS.0000000000008959. [DOI] [PubMed] [Google Scholar]
- 7.Rossin E.J., Szypko C., Giese I., et al. Factors associated with increased risk of serious ocular injury in the setting of orbital fracture. JAMA Ophthalmol. 2021;139:77–83. doi: 10.1001/jamaophthalmol.2020.5108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeffrey J., Nelson F., Hohlbein J., et al. South Texas orbital fracture protocol for emergency department evaluation of orbital fractures. Am J Emerg Med. 2022;57:42–46. doi: 10.1016/j.ajem.2022.04.025. [DOI] [PubMed] [Google Scholar]
- 9.Richani K., Do T.H., Merritt H.A., et al. Screening criteria for detecting severe ocular injuries in the setting of orbital fractures. Ophthal Plast Reconstr Surg. 2019;35:609–614. doi: 10.1097/IOP.0000000000001422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.al-Qurainy I.A., Titterington D.M., Dutton G.N., et al. Midfacial fractures and the eye: the development of a system for detecting patients at risk of eye injury. Br J Oral Maxillofac Surg. 1991;29:363–367. doi: 10.1016/0266-4356(91)90001-l. [DOI] [PubMed] [Google Scholar]
- 11.Nassrallah G., Dhillon J., Gaffar J., et al. Incidence of ophthalmologic pathology and associated risk factors in orbital fractures at a level I trauma centre. Can J Ophthalmol. 2023 doi: 10.1016/j.jcjo.2023.03.007. S0008-4182(23)00079-0. [DOI] [PubMed] [Google Scholar]
- 12.Zhong E., Chou T.Y., Chaleff A.J., et al. Orbital fractures and risk factors for ocular injury. Clin Ophthalmol. 2022;16:4153–4161. doi: 10.2147/OPTH.S391175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Layton C.J. Factors associated with significant ocular injury in conservatively treated orbital fractures. J Ophthalmol. 2014;2014 doi: 10.1155/2014/412397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ho T.Q., Jupiter D., Tsai J.H., Czerwinski M. The incidence of ocular injuries in isolated orbital fractures. Ann Plast Surg. 2017;78:59–61. doi: 10.1097/SAP.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 15.Andrews B.T., Jackson A.S., Nazir N., et al. Orbit fractures: identifying patient factors indicating high risk for ocular and periocular injury. Laryngoscope. 2016;126:S5–S11. doi: 10.1002/lary.25805. [DOI] [PubMed] [Google Scholar]
- 16.Akkina S.R., Saurey T.G., Middleton N.A., et al. Factors associated with ocular injury in orbital fracture patients: who requires urgent ophthalmic evaluation? Facial Plast Surg Aesthet Med. 2021 doi: 10.1089/fpsam.2021.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ray A., Curti S., Pegues J., et al. Secondary overtriage of isolated facial trauma. Am J Otolaryngol. 2021;42 doi: 10.1016/j.amjoto.2021.103043. [DOI] [PubMed] [Google Scholar]
- 18.Singman E.L., Smith K., Mehta R., et al. Cost and visit duration of same-day access at an academic ophthalmology department vs emergency department. JAMA Ophthalmol. 2019;137:729–735. doi: 10.1001/jamaophthalmol.2019.0864. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.